
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med., 08 February 2024
Sec. Cardiovascular Imaging
Volume 11 - 2024 | https://doi.org/10.3389/fcvm.2024.1303529
This article is part of the Research TopicEvaluation of Coronary Microvascular Dysfunction Based on Cardiovascular ImagingView all 9 articles
Background: In this study, we aim to investigate the relationship between the attenuation of peri-coronary adipose tissue (PCAT) in patients with suspected coronary artery disease (CAD) and the assessment of coronary vascular functions using coronary flow reserve (CFR).
Methods: We included 364 patients who underwent 13N-NH3 positron emission tomography/computed tomography and coronary computed tomography angiography (CCTA). We determined the relationship between fat attenuation index (FAI), PCAT volume, and other qualitative CT-derived anatomic parameters with CFR.
Results: We detected a decrease in CFR (<2.5) in 206 (57%) patients. At the patient level, those with reduced CFR showed a significantly higher prevalence of diffused atherosclerosis (41% vs. 23%; P < 0.001) and higher FAI (−75.5 HU vs. −77.1 HU; P = 0.014). In patients without obstructive CAD, FAI was significantly higher in those with reduced CFR (−75.5 HU vs. −77.7 HU, P = 0.026). On the vessel level, 1,092 vessels were analyzed, and 642 (59%) exhibited reduced CFR. The vessels with reduced CFR presented a significantly higher prevalence of obstructive CAD (37% vs. 26%; P < 0.001), diffused atherosclerosis (22% vs. 11%; P < 0.001), low-attenuation plaque (6% vs. 3%; P = 0.030), and positive remodeling (7% vs. 2%; P = 0.001). FAI was higher in vessels with reduced CFR (−80.8 HU vs. −81.8 HU; P = 0.045) than in normal CFR. In the patient-level analysis, obstructive CAD, diffused atherosclerosis, and FAI were independently linked with CFR. FAI was still associated with global CFR after adjusting for traditional risk factors (age, hypertension, diabetes, hyperlipidemia, and smoking). FAI remained independently associated with reduced CFR in patients without obstructive CAD.
Conclusions: Coronary perivascular inflammation evaluated by CCTA was independently associated with coronary vascular function. In patients without obstructive CAD, FAI was higher in the presence of reduced CFR. Altogether, FAI can help reveal microcirculatory damage in patients who do not exhibit epicardial artery stenosis.
Peri-coronary adipose tissue (PCAT) attenuation, derived from coronary computed tomography angiography (CCTA), is linked with coronary artery inflammation (1). The changes in the PCAT composition from lipid to aqueous can reveal inflammation in the surrounding coronary arteries.
Fat attenuation index (FAI) is a novel imaging biomarker for the presence of coronary artery inflammation (2). A study using two large cohorts reported the associations between increased cardiac mortality and higher FAI, confirming the prognostic value of FAI (3). In addition, FAI is also a novel parameter indicating changes in coronary artery hemodynamics. A previous study showed that perivascular FAI is significantly higher for flow-limiting lesions than non-flow-limiting lesions (4). Nevertheless, the specificity of perivascular FAI in identifying flow-limiting lesions is relatively low. Furthermore, the combination of perivascular FAI and other CCTA characteristics, such as diameter stenosis, can improve the accuracy of diagnosing ischemic coronary artery stenosis.
Positron emission tomography (PET) is the most accurate non-invasive method for evaluating myocardial blood flow (MBF), which can obtain MBF in both cardiac load and resting states. Coronary flow reserve (CFR) is the ratio of MBF during maximum coronary congestion to resting, which is considered a powerful indicator of the myocardial reserve capacity (5). The presence of abnormal CFR indicates the presence of coronary artery stenosis and coronary artery dysfunction (5, 6). CFR can reveal epicardial coronary artery stenosis and impaired vasodilatory capacity through diffused atherosclerotic (DA) changes (7). Nevertheless, it is challenging to determine whether reduced CFR is caused by epicardial coronary stenosis or microvascular dysfunction. A previous study showed that abnormal CFR (<2.5) indicates microvascular dysfunction in the absence of significant stenosis of the epicardial coronary artery (<50%) in patients (8). Presently, most studies focus on the effect and prediction of peri-coronary inflammation on the hemodynamics of epicardial coronary arteries. However, the effect of microvascular function is not well reported (9). In this study, we investigated the association between FAI and coronary vascular functions, particularly microvascular function.
We included consecutive patients with suspected coronary artery disease (CAD) who visited our institute from January 2021 to June 2023 and underwent 13N-NH3 positron emission tomography/computed tomography (PET/CT) and CCTA within 1 month. Patients with moderate to severe stenosis of any coronary artery revealed by CCTA required further invasive coronary angiography (ICA). The exclusion criteria were as follows: (I) patients with coronary artery variations, such as origin variation, conformational variation, and termination abnormality; or (II) patients with left dominant coronary artery; or (III) patients with concomitant cardiomyopathy; or (IV) patients with any previous coronary interventions or bypass surgery; or (V) patients with incomplete baseline clinical data; or (VI) patients with moderate to severe stenosis of any coronary artery in CCTA but without ICA; or (VII) patients with a significantly impaired image quality on CCTA. Lastly, 364 patients were enrolled in this study (Figure 1). The need for written informed consent was waived due to the retrospective design of the study. The hospital ethics committee approved this study.
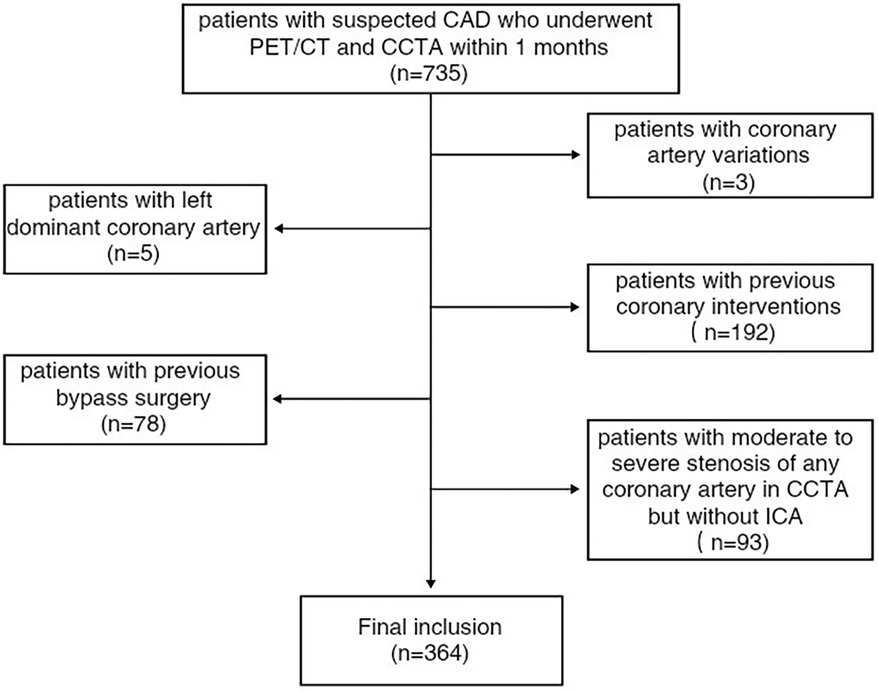
Figure 1. Inclusion and exclusion criteria for the study population. CAD, coronary artery disease; CCTA, coronary computed tomography angiography; ICA, invasive coronary angiography; PET/CT, positron emission tomography/computed tomography.
CCTA scans were performed using a GE 256-slice computed tomography scanner (Revolution, GE, USA). The CTA scan adopted a prospective electrocardiogram gating protocol, and the scan parameters were set as follows: tube voltage of 100 or 120 kV and tube current of 300–700 mA, which was based on the body mass index. Patients with elevated heart rates should have a heart rate below 75 beats/min prior to administering a contrast injection. A bolus of iodine contrast medium (Ioversol solution), 60–70 ml, was injected at a rate of 4.5–5 ml/s into the antecubital vein.
PCAT was defined as the radial distance from the vessel wall equal to the vessel diameter for all voxels in the range of −190 to −30 HU (10). PCAT attenuation was evaluated in the proximal 40-mm segment of the left anterior descending artery (LAD) and left circumflex artery (LCX) and the proximal 10- to 50-mm segment of the right coronary artery (RCA) (10). PCAT attenuation was calculated based on the average attenuation of the perivascular adipose tissue. Semiautomated software (CoronaryDoc, Shukun Technology, China) was used to perform PCAT attenuation analysis as previously described (11). The global FAI was defined as the lowest value among the three major coronary arteries, whereas the global PCAT volume was calculated as the average of the three arteries. FAI was considered high at >−70.1 HU.
Two radiologists (with 10 years and 3 years of diagnostic experience in cardiac imaging) independently analyzed all CCTA images. In cases of differences of opinion, consent was achieved after a joint discussion. The diagnosis of mild stenosis lesions was accurate due to the high negative predictive value of CCTA. A subsequent ICA examination was performed following the detection of ≥50% stenosis in the three major coronary arteries on CCTA. Furthermore, the final degree of stenosis was based on ICA. Curved planar reformation (CPR) and axial views were used to analyze the CCTA images. The stenosis severity was categorized into the following five groups: 0%, 1%–49%, 50%–69%, 70%–90%, and >90%. Obstructive CAD was considered when luminal stenosis was ≥50% (12). Simultaneously, we considered the effect of the presence of diffused atherosclerosis (DA). DA was defined as a single or tandem lesion measuring ≥2 cm or multifocal plaques diffusely distributed along the vascular wall with or without calcification (7). The characteristics of high-risk plaque were as follows: low-attenuation plaque (any voxel <30 HU), positive remodeling (ratio of cross-sectional lesion area by the area of a proximal reference point >1.1), spotty calcification (small calcified portion <3 mm length and presenting <90° of vessel circumference), and napkin ring sign (plaque core with low CT attenuation surrounded by a ring-like peripheral of higher CT attenuation) (13). Patients with at least two characteristics of high-risk plaque were considered to have high-risk plaques (14).
The patients underwent fasting for at least 4 h and refrained from caffeine for at least 24 h prior to the procedure. All patients received an adequate history inquiry and informed consent. An intravenous line was placed in the radial vein of the patients, and a low-dose CT scan (120 kV, 20 mA) was performed for attenuation correction. Subsequently, 10 mCi (370–555 MBq) of 13N-ammonia was injected intravenously as a bolus 10 s prior to the start of a 10 min dynamic PET acquisition in 3D list-mode format. After 13N-ammonia dynamic PET acquisition and a 2 min wait, ECG-gated perfusion 13N-ammonia PET with 8 frames per cardiac cycle was performed for 8 min. The interval between resting and stress imaging was at least 40 min, and 0.16 mg/kg/min of adenosine was intravenously infused for 6 min as a vasodilator. Then, 13N-ammonia was injected 3 min after the initiation of the infusion. Stress image acquisition was performed with the same dose and protocol as that for resting images. All PET scanning was performed using a PET/CT scanner (GE Discovery NM690).
QPET (Cedars-Sinai, LA, USA) was used for processing PET/CT images. We acquired the rest and stress MBF of three coronary artery perfusion regions and calculated the zoning and left ventricular coronary flow reserve (LV-CFR) (as the ratio of the stress/rest MBF). CFR was considered reduced when it was less than 2.5 (8, 15).
Baseline characteristics were retrospectively acquired from the electronic medical record system, which included the demographic characteristics (gender, age, and body mass index) and conventional high-risk factors of CAD (hyperlipidemia, hypertension, diabetes, and current smoking) of patients.
SPSS Statistics 23.0 software (IBM Corporation, Armonk, NY, USA) was used to perform statistical analyses. The continuous variables with a normal distribution are presented as mean ± standard deviation (SD), whereas the median (25th and 75th) is used to express non-normal distributions. The independent t-test or Mann–Whitney U test was performed to compare the quantitative parameters of the two groups. Categorical variables are expressed as absolute frequencies and percentages and compared using the χ2 test. In the patient-level analysis, logistic univariate and multivariate regression analyses were performed to determine the associations between global CFR and PCAT volume, FAI, diffused atherosclerosis, vulnerable plaques, and CAD risk factors. Pearson's correlation analysis was performed to evaluate the correlation between CFR, rest MBF, and stress MBF with FAI. The receiver operating characteristic (ROC) curve was performed to determine the optimal FAI cut-off value for defining reduced CFR in total, obstructive, and non-obstructive lesions. A P-value of <0.05 was considered statistically significant.
A total of 364 participants with 1,092 vessels were retrospectively reviewed in the present study, and their clinical and imaging characteristics are displayed in Table 1. The mean age of the included patients was 60 ± 11 years, and 179 patients (49%) were females. A total of 205 (56%) patients suffered from hypertension, and 69 (19%) patients had diabetes. A total of 205 (56%) patients presented obstructive CAD, and 122 (34%) presented DA. The global FAI was −76.2 ± 6.4 HU, and the PCAT volume was 1,866 ± 373 mm3.
At the patient level, a decrease in CFR was observed in 206 (56%) patients. The clinical and imaging characteristics of patients with a normal or reduced CFR are listed in Table 2. Compared with patients with normal CFR, those with reduced CFR showed a significantly higher prevalence of obstructive CAD (65% vs. 44%; P < 0.001) and DA (41% vs. 23%; P < 0.001). Moreover, the FAI was higher in patients with reduced CFR (−75.5 HU vs. −77.1 HU; P = 0.014) than in those with normal CFR (Figure 2A). No significant difference was observed in the rest MBF between the two groups, whereas the stress MBF of the reduced CFR group was significantly lower (1.45 vs. 2.68; P < 0.001) than that of the normal CFR group. A weak negative correlation was observed between the FAI and the stress MBF, whereas no significant correlation was observed between the rest MBF and the FAI (Figure 3).
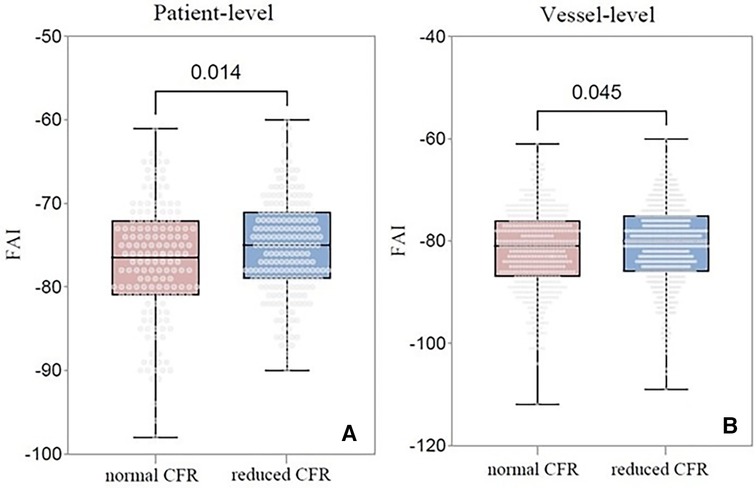
Figure 2. Comparison of the FAI between normal CFR group and reduced CFR group. (A) Comparison at the patient level; (B) Comparison at the vessel level. FAI, fat attenuation index; CFR, coronary flow reserve; CAD, coronary artery disease.
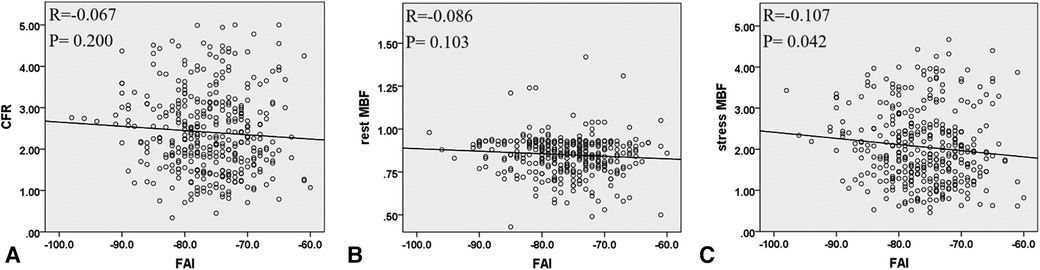
Figure 3. The correlation between FAI with CFR, rest MBF, and stress MBF at the patient level. (A) FAI and CFR, (B) FAI and rest MBF, and (C) FAI and stress MBF. FAI, fat attenuation index; CFR, coronary flow reserve; MBF, myocardial blood flow.
In patients with obstructive CAD, no significant difference was observed between the FAI of the patients with a normal and reduced CFR (−76.4 HU vs. −75.4 HU; P = 0.315) (Figure 4A). Conversely, in patients without obstructive CAD, FAI was significantly higher in patients with reduced CFR (−75.5 HU vs. −77.7 HU; P = 0.026) than in those with normal CFR (Figure 4B). However, no significant difference was observed between the global CFR of patients with high and low FAI among patients with or without obstructive CAD.

Figure 4. Comparison of the FAI between the normal CFR group and the reduced CFR group at the patient level. (A) Comparison in patients with obstructive CAD; (B) Comparison in patients without obstructive CAD. FAI, fat attenuation index; CFR, coronary flow reserve; CAD, coronary artery disease.
The results of the logistic regression analysis considering reduced CFR (<2.5) as a dependent variable in all patients are presented in Table 3. No significant correlation was observed among demographics (age, gender, and body mass index), CAD risk factors (hypertension, hyperlipidemia, diabetes, and smoking), high-risk plaques, PCAT volume, and reduced CFR. The univariate analysis results showed that obstructive CAD, DA, and FAI were related to reduced CFR. However, the multivariable analysis results showed that only obstructive CAD (P = 0.027) and FAI (P = 0.035) were independently related to reduced CFR.
The results of the logistic regression analysis considering reduced CFR (<2.5) as a dependent variable in patients without obstructive CAD are presented in Table 4. The univariate analysis results showed that only FAI was related to reduced CFR in patients without obstructive CAD (P = 0.029). Based on the univariate analysis results and existing knowledge, female sex, hyperlipidemia, smoking, and FAI were selected as independent variables for the multivariate analysis, which showed that FAI was independently related to reduced CFR (P = 0.045).
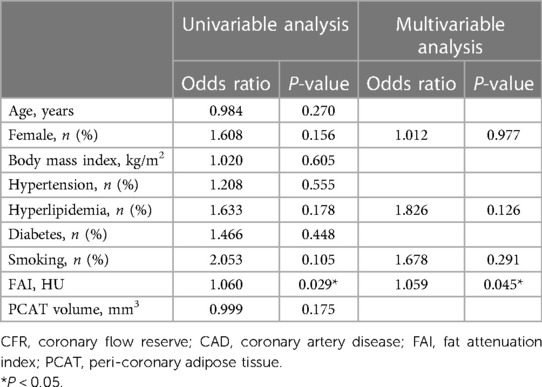
Table 4. Logistic regression analyses with CFR < 2.5 as a dependent variable in patients without obstructive CAD.
A total of 1,092 vessels were analyzed, of which 642 (59%) exhibited reduced CFR. The imaging results of these vessels are presented in Table 5. Compared with vessels with normal CFR, vessels with reduced CFR presented a significantly higher prevalence of obstructive CAD (37% vs. 26%; P < 0.001), diffused atherosclerosis (22% vs. 11%; P < 0.001), low-attenuation plaque (6% vs. 3%; P = 0.030), and positive remodeling (7% vs. 2%; P = 0.001). Moreover, vessels with reduced CFR showed a higher FAI (−80.8 HU vs. −81.8 HU; P = 0.045) than that showed by vessels with normal CFR (Figure 2B). A weak negative correlation was observed between the FAI and the rest and stress MBF (Figure 5).
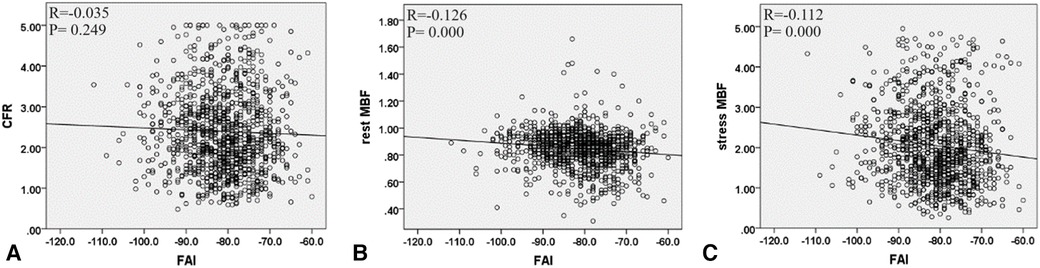
Figure 5. The correlation between FAI and CFR, rest MBF, and stress MBF at the vessel level. (A) FAI and CFR, (B) FAI and rest MBF, and (C) FAI and stress MBF. FAI, fat attenuation index; CFR, coronary flow reserve; MBF, myocardial blood flow.
An ROC curve was generated to determine the optimal FAI cut-off value in order to define CFR < 2.5. The Youden index showed that the optimal cut-off values of FAI for total, obstructive, and non-obstructive lesions were −84.5 HU, −87.5 HU, and −82.5 HU, respectively. Moreover, the ROC curve was used to analyze the diagnostic efficacy of anatomical stenosis, FAI, and their combination in identifying CFR < 2.5, and the results showed that the areas under the curve (AUCs) for anatomical stenosis, FAI, and their combination were 0.591 [95% confidence interval (CI), 0.561–0.621], 0.536 (95% CI, 0.506–0.566), and 0.606 (95% CI, 0.577–0.635), respectively (Figure 6). Although the AUC of the combination was higher than that of anatomical stenosis, no significant differences were observed between them (P = 0.067).
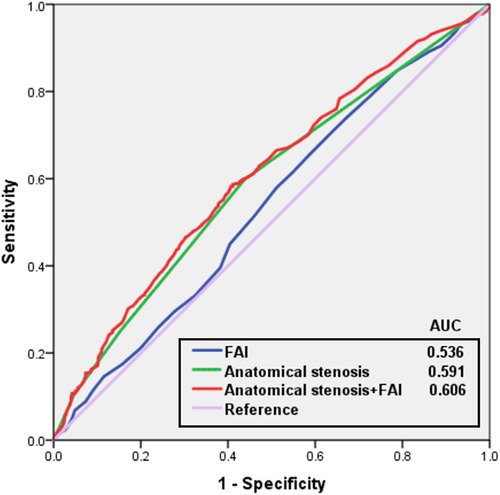
Figure 6. Receiver operating characteristic curves for anatomical stenosis and FAI in predicting reduced CFR. Cut-off value of −84.5 HU for FAI according to the Youden index. FAI, fat attenuation index; AUC, area under the curve.
The present study showed that the FAI was higher in the reduced CFR group than in the normal CFR group at both patient and vessel levels. Furthermore, the FAI was significantly higher in patients with reduced CFR than in those with normal CFR among patients without obstructive CAD. The FAI was independently related to reduced CFR among patients without obstructive CAD. Patients with microvascular dysfunction but without epicardial coronary stenosis showed a higher FAI. Moreover, a higher FAI was associated with reduced CFR after adjusting for the risk factors for CAD and the presence of obstructive CAD and DA. The results suggest that FAI is an independent factor for predicting reduced CFR among patients with suspected CAD. In addition, peri-coronary inflammation was associated with decreased stress MBF, which eventually affected CFR. To the best of our knowledge, this is the first study to investigate the relationship between coronary vascular function (particularly microcirculation function) evaluated by CFR and peri-coronary inflammation assessed by CCTA among many patients with suspected CAD.
Currently, most studies have focused on the effect and prediction of peri-coronary inflammation on the hemodynamics of epicardial coronary arteries; however, studies on the effect of coronary vascular functions, particularly microvascular functions, are lacking. Only one study has reported a correlation between CFR and peri-coronary inflammation, suggesting that PCAT attenuation may help identify myocardial ischemia specifically in patients who are traditionally considered not at a high risk of future cardiovascular events (13). However, this previous study included a relatively small sample size and did not include patients with obstructive CAD. Thus, further larger studies should be performed to verify differences in this subset in order to validate the relationship between FAI and microvascular function. Nevertheless, the present study compensated for the aforementioned limitations to some extent. Masahiro et al. (16) found that microcirculation dysfunction was not significantly correlated to the FAI and epicardial fat attenuation; however, it was significantly correlated with epicardial fat volumes in patients with moderate coronary stenosis (30%–80%) when invasive FFR and IMR values were considered as the gold standard. Herein, the reduced CFR group showed a higher FAI in patients without obstructive CAD, which indicated the association between microvascular dysfunction and FAI. However, no significant difference in FAI was observed between the reduced CFR group and the patient group without obstructive CAD. We consider that two possible reasons are the individual variations in FAI and a small sample size. Expanding the sample size would be valuable to enhance the precision of the conclusion.
PCAT supports and protects the surrounding coronary vessels. Previous studies have confirmed that FAI reflects peri-coronary inflammation and is associated with vulnerable plaques and inflammatory activities (1, 17). Moreover, the paracrine-mediated regulation of vascular homeostasis by PCAT has been reported in a study (18). In cases of CAD or microvascular dysfunction, radical oxygen species generated in response to regional ischemia can trigger the activation of EAT-driven inflammatory signals by releasing chemokines and inflammatory cytokines, which exert local effects on the underlying coronaries and myocardium (18). The possible mechanism is that coronary artery inflammation in patients with impaired coronary blood flow may disrupt the role of PCAT in regulating vascular tension caused by focal inflammation. Siasos et al. (19) reported an association between microvascular and epicardial endothelium dysfunction and local lower endothelial shear stress (ESS) during early-stage coronary atherosclerosis. Low ESS, the tangential stress produced by the friction of the circulating blood with the endothelial surface, is a focal proinflammatory stimulus associated with coronary atherosclerosis development and progression (19). Another probable reason for increased FAI in patients with reduced CFR is that microvascular endothelial dysfunction may reversibly decrease upstream local ESS, thereby exacerbating the inflammation of the upstream coronary artery endothelium. A bidirectional pathway between the vascular wall and the surrounding fat and the secretion of cytokines and inflammatory mediators may increase the density of peri-coronal fat (20).
Decreased CFR represents focal vascular stenosis and impaired vasodilation caused by diffused atherosclerosis. Similarly, herein, both obstructive CAD and DA were associated with reduced CFR. DA is related to a worse prognosis, irrespective of focal stenosis severity, and localized revascularization by stent insertion may not completely restore the hemodynamics impaired by DA (7), which suggests that attention should be paid to DA when evaluating the coronary circulation of patients with suspected CAD. Previous studies have shown the effects of CTA plaque characteristics on downstream myocardial perfusion evaluated by PET. A high disease burden was predicted by CFR and adverse plaque by hyperemic flow and resting flow. High-risk plaque characteristics and plaque burden were independently associated with cardiovascular events (21). Driessen et al. (22) showed that positive remodeling and non-calcified plaque volumes were related to detrimental downstream hyperemic blood flow in 208 patients with suspected CAD. They confirmed that compared with patients with normal CFR, patients with reduced CFR showed a significantly higher prevalence of low-attenuation plaques and positive remodeling, which is in line with the results of our study.
Nevertheless, the present study has several limitations. First, we included limited single-center retrospective data. Second, high-risk plaque characteristics were considered in the study, and plaque parameters such as plaque volumes and lesion lengths were not quantitatively measured. Third, the absence of epicardial diseases was presumed based on anatomical obstructive lesions owing to the lack of FFR data, which did not necessarily indicate true physiological microvascular dysfunction. Fourth, the absolute difference in FAI between the normal CFR group and the reduced CFR group was minuscule, which indicated that applying the index to clinical practice would be challenging. Hence, more studies should be performed to collect multicenter prospective data and quantitatively evaluate lesion parameters.
In conclusion, coronary perivascular inflammation evaluated by CCTA was found to be independently related to coronary vascular function. FAI was higher in patients without obstructive CAD in the presence of reduced CFR. Thus, FAI may help predict microcirculatory damage among patients who do not show epicardial artery stenosis.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the TEDA International Cardiovascular Hospital Research Project Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin due to the retrospective nature of the study.
MC: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. BL: Investigation, Methodology, Writing – review & editing. XL: Writing – review & editing, Investigation. DL: Conceptualization, Writing – review & editing. LF: Conceptualization, Funding acquisition, Resources, Writing – review & editing.
The authors declare financial support was received for the research, authorship, and/or publication of this article.
This study was supported by Tianjin Health Science and Technology Project (grant no. TJWJ2022ZD011), TEDA International Cardiovascular Hospital's Project (grant no. 2022-TD-012), Binhai New Area Health Commission Science and Technology Project (grant no. 2023BWKZ003) and Tianjin Science and Technology Plan Project (grant no. 21JCYBJ00530).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rosendael SE, Kuneman JH, Hoogen I, Kitslaar PH, Rosendael AR, Bijl P, et al. Vessel and sex differences in pericoronary adipose tissue attenuation obtained with coronary CT in individuals without coronary atherosclerosis. Int J Cardiovasc Imaging. (2022) 38(12):2781–9. doi: 10.1007/s10554-022-02716-7
2. Oikonomou EK, Marwan M, Desai MY, Mancio J, Alashi A, Centeno EH, et al. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data. Lancet. (2018) 392(10151):929–39. doi: 10.1016/S0140-6736(18)31114-0
3. Goeller M, Achenbach S, Cadet S, Kwan AC, Commandeur F, Slomka PJ, et al. Peri-coronary adipose tissue computed tomography attenuation and high-risk plaque characteristics in acute coronary syndrome compared with stable coronary artery disease. JAMA cardiology. (2018) 3(9):858–63. doi: 10.1001/jamacardio.2018.1997
4. Yu M, Dai X, Deng J, Lu Z, Shen C, Zhang J. Diagnostic performance of perivascular fat attenuation index to predict hemodynamic significance of coronary stenosis: a preliminary coronary computed tomography angiography study. Eur Radiol. (2020) 30(2):673–81. doi: 10.1007/s00330-019-06400-8
5. Assante R, Acampa W, Zampella E, Arumugam P, Nappi C, Gaudieri V, et al. Prognostic value of atherosclerotic burden and coronary vascular function in patients with suspected coronary artery disease. Eur J Nucl Med Mol Imaging. (2017) 44(13):2290–8. doi: 10.1007/s00259-017-3800-7
6. Crea F, Camici PG, Bairey Merz CN. Coronary microvascular dysfunction: an update. Eur Heart J. (2014) 35(17):1101–11. doi: 10.1093/eurheartj/eht513
7. Cho S, Park KS, Kim J, Kang S, Song H, Kim JH, et al. Coronary flow reserve and relative flow reserve measured by N-13 ammonia PET for characterization of coronary artery disease. Ann Nucl Med. (2017) 31(2):144–52. doi: 10.1007/s12149-016-1138-z
8. Marinescu MA, Löffler AI, Ouellette M, Smith L, Kramer CM, Bourque JM. Coronary microvascular dysfunction, microvascular angina, and treatment strategies. JACC Cardiovasc Imaging. (2015) 8(2):210–20. doi: 10.1016/j.jcmg.2014.12.008
9. Oikonomou EK, Desai MY, Marwan M, Kotanidis CP, Antonopoulos AS, Schottlander D, et al. Perivascular fat attenuation index stratifies cardiac risk associated with high-risk plaques in the CRISP-CT study. J Am Coll Cardiol. (2020) 76(6):755–7. doi: 10.1016/j.jacc.2020.05.078
10. Sugiyama T, Kanaji Y, Hoshino M, Hada M, Misawa T, Nagamine T, et al. Relationship of OCT-defined plaque characteristics with CCTA-derived coronary inflammation and CMR-derived global coronary flow reserve in patients with acute coronary syndrome. PLoS One. (2023) 18(5):e0286196. doi: 10.1371/journal.pone.0286196
11. Li N, Dong X, Zhu C, Shi K, Si N, Shi Z, et al. Model development and validation of noninvasive parameters based on coronary computed tomography angiography to predict culprit lesions in acute coronary syndromes within 3 years: value of plaque characteristics, hemodynamics and peri-coronary adipose tissue. Quant Imaging Med Surg. (2023) 3(7):4325–38. doi: 10.21037/qims-22-1045
12. Ma H, Dai X, Yang X, Zhao X, Wang R, Zhang J. Clinical and imaging predictors of impaired myocardial perfusion in symptomatic patients after percutaneous coronary intervention: insights from dynamic CT myocardial perfusion imaging. Quant Imaging Med Surg. (2021) 11(7):3327–37. doi: 10.21037/qims-20-977
13. Nomura CH, Assuncao AN Jr, Guimarães PO, Liberato G, Morais TC, Fahel MG, et al. Association between perivascular inflammation and downstream myocardial perfusion in patients with suspected coronary artery disease. Eur Heart J Cardiovasc Imaging. (2020) 21(6):599–605. doi: 10.1093/ehjci/jeaa023
14. Dai X, Hou Y, Tang C, Lu Z, Shen C, Zhang L, et al. Long-term prognostic value of the serial changes of CT-derived fractional flow reserve and perivascular fat attenuation index. Quant Imaging Med Surg. (2022) 12(1):752–65. doi: 10.21037/qims-21-424
15. Zhang X, Li H, Wu P, Yuan L, Wu Z, Liu H, et al. The diagnosis and prognosis of coronary microvascular disease using PET/CT. Clin Hemorheol Microcirc. (2022) 80(2):153–66. doi: 10.3233/CH-201034
16. Hoshino M, Yang S, Sugiyama T, Zhang J, Kanaji Y, Hamaya R, et al. Characteristic findings of microvascular dysfunction on coronary computed tomography angiography in patients with intermediate coronary stenosis. Eur Radiol. (2021) 31(12):9198–210. doi: 10.1007/s00330-021-07909-7
17. Kwiecinski J, Dey D, Cadet S, Lee S-E, Otaki Y, Huynh PT, et al. Peri-coronary adipose tissue density is associated with 18F-sodium fluoride coronary uptake in stable patients with high-risk plaques. JACC Cardiovasc Imaging. (2019) 12(10):2000–10. doi: 10.1016/j.jcmg.2018.11.032
18. Guaricci AI, Neglia D, Acampa W, Andreini D, Baggiano A, Bianco F, et al. Computed tomography and nuclear medicine for the assessment of coronary inflammation: clinical applications and perspectives. J Cardiovasc Med. (2023) 24(Suppl 1):e67–76. doi: 10.2459/JCM.0000000000001433
19. Siasos G, Sara JD, Zaromytidou M, Park KH, Coskun AU, Lerman LO, et al. Local low shear stress and endothelial dysfunction in patients with nonobstructive coronary atherosclerosis. J Am Coll Cardiol. (2018) 71(19):2092–102. doi: 10.1016/j.jacc.2018.02.073
20. Kanaji Y, Hirano H, Sugiyama T, Hoshino M, Horie T, Misawa T, et al. Pre-percutaneous coronary intervention peri-coronary adipose tissue attenuation evaluated by computed tomography predicts global coronary flow reserve after urgent revascularization in patients with non-ST-segment-elevation acute coronary syndrome. J Am Heart Assoc. (2020) 9(17):e016504. doi: 10.1161/JAHA.120.016504
21. Yang S, Hoshino M, Koo BK, Yonetsu T, Zhang J, Hwang D, et al. Relationship of plaque features at coronary CT to coronary hemodynamics and cardiovascular events. Radiology. (2022) 305(3):578–87. doi: 10.1148/radiol.213271
Keywords: coronary flow reserve, peri-coronary adipose tissue, fat attenuation index, coronary artery disease, perivascular inflammation
Citation: Chen M, Liu B, Li X, Li D and Fan L (2024) Relationship between peri-coronary inflammation and coronary vascular function in patients with suspected coronary artery disease. Front. Cardiovasc. Med. 11:1303529. doi: 10.3389/fcvm.2024.1303529
Received: 28 September 2023; Accepted: 25 January 2024;
Published: 8 February 2024.
Edited by:
Jie Zheng, Washington University in St. Louis, United StatesReviewed by:
Seokhun Yang, Seoul National University Hospital, Republic of Korea© 2024 Chen, Liu, Li, Li and Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dong Li ZHJfbGlkb25nQDE2My5jb20= Lijuan Fan TGlqdWFuZmFuMTExQHNpbmEuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.