
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Cardiovasc. Med. , 04 October 2023
Sec. Coronary Artery Disease
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1249924
 Boning Xu1*
Boning Xu1* Chunxin Zhang1†
Chunxin Zhang1† Wei Wei2†
Wei Wei2† Yun Zhan1
Yun Zhan1 Mingguo Yang1
Mingguo Yang1 Yanjun Wang1
Yanjun Wang1 Jiajian Zhao1
Jiajian Zhao1 Guiyang Lin1
Guiyang Lin1 Wen-wen zhang1
Wen-wen zhang1 Xing Huo1
Xing Huo1 Bin Shi1
Bin Shi1 Ling Fan2
Ling Fan2
Objective: To investigate the impact of optimized thrombus aspiration on myocardial perfusion, prognosis, and safety in patients with acute ST-segment elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention(primary PCI).
Methods: A total of 129 patients with STEMI were randomly allocated into control group (Subgroup A and B) and experimental group(Subgroup C and D). Control group received percutaneous transluminal coronary angioplasty (PTCA),thrombus aspiration and primary PCI. Experimental group received optimized thrombus aspiration and primary PCI. The number of thrombus aspiration was less than 4 times in Subgroup A and C. The number of thrombus aspiration was performed more than 4 times in Subgroups B and D. The classification of thrombi extracted, the TIMI flow grade, the incidence of no-reflow and slow flow, cTFC, TPI and CK-MB at 12 h and 24 h after stenting, ST segment resolution of ECG after stenting, NT-proBNP, LVEFat 24 h, 30 days and 180 days after stenting were compared between groups. The incidence of intraoperative and postoperative bleeding complications, stroke events and major cardiovascular events (MACE) were recorded and compared between groups.
Results: The classification of thrombi extracted in the experimental group was higher than that in the control group. The TIMI flow grade of the experimental group was better than the control group after thrombus aspiration. After stenting, the advantage still existed, but the difference was not statistically significant. On cTFC, the experimental group was lower than the control group, but the difference was not statistically significant; After stenting the experimental group was significantly lower than the control group. The CK-MB at 12 h and 24 h of the experimental group was lower than the control group. After thrombus aspiration the incidence of no-reflow in the experimental group was significantly lower than that in the control group; after stenting the incidence of no-reflow in the experimental group was still lower than the control group, but no statistically difference. After thrombus aspiration and stenting the incidence of slow flow in the experimental group were lower than that in the control group. After stenting, NT-proBNP at 24 h was lower in the experimental group than that in the control group, However, there was no statistical difference; after stenting, The NT-proBNP in the experimental group was lower than that in the control group at 30 days and 180 days. After stenting, LVEF of the experimental group was significantly higher than the control group at 24 h and 30 days; superiority remained after 180 days but no statistical difference. There was no statistical difference between two groups for intraoperative and postoperative bleeding complications, stroke events, and MACE events. In Subgroup analysis,there was no significant difference in the classification of thrombi extracted, TIMI flow grade, cTFC, CK-MB,NT-proBNP and LVEF between group C and D, but group A was better than group B. Analysis of variance showed that the optimal number of suction was 4–5 times.
Conclusions: Optimized thrombus aspiration can significantly improve myocardial perfusion and short-term and medium-term prognosis of STEMI patients after PCI, and reduce the incidence of slow flow and no-reflow. The optimal suction times were 4–5 times. Traditional aspiration method with more aspiration times is harmful to cardiac prognosis. Thrombus aspiration does not increase the incidence of stroke events and is safe.
Clinical Trial Registration: identifier, ChiCTR2300073410.
Acute myocardial infarction (AMI) has the highest mortality rate in cardiovascular diseases. The key to the treatment of AMI is to rapidly open the infarct-related artery (IRA), complete revascularization, and achieve effective reperfusion of the approaching necrotic myocardium. There are two commonly used clinical treatment methods, one is drug thrombolytic therapy; The second is primary percutaneous coronary intervention (PCI). Primary PCI is the most effective method for the treatment of acute myocardial infarction due to its high recanalization rate, sufficient and durable IRA recanalization and few bleeding complications. One of the more challenging aspects of primary PCI is thrombosis. The TAPAS study, presented at the EuroPCR meeting in 2008, was the first large randomized controlled study to demonstrate that thrombus aspiration vs. PCI alone significantly improves myocardial perfusion and outcomes in patients with STEMI. The 1-year follow-up showed that compared with the PCI group, the total death rate and the reinfarction rate in the thrombectomy group were significantly reduced (1). However, The TASTE study, published in 2013 in the New England Journal of Medicine, raised questions about thrombus aspiration when it showed no additional benefit of manual thrombus aspiration over PCI alone in reducing 30-day mortality in patients with STEMI. The results of the TOTAL trial, presented in 2015 at the ACC, showed that routine use of a manual aspiration catheter did not reduce the risk of cardiovascular death, recurrent myocardial infarction, cardiogenic shock, or heart failure at 180 days (similar to the results of the TASTE trial) but did increase the risk of embolic stroke at 30 days (different from the results of the TASTE trial) (2, 3).Thrombus aspiration has been downgraded from class ⅡA to Class Ⅱb in the guidelines in 2014 and 2017 years (4, 5). However, thrombus aspiration is recommended for patients with heavy thrombus burden during primary PCI, who are prone to coronary microcirculation dysfunction such as slow flow and no reflow, which aggravate myocardial injury and increase the incidence of heart failure and mortality (6, 7). In order to further search for the optimal treatment, this study adopted a randomized, parallel and controlled clinical trial design, to investigate whether the optimized thrombus aspiration method can improve the TIMI flow in patients with STEMI after primary PCI, and influence of cTFC, myocardial infarction size (ST segment resolution, TPI, CK-MB), clinical prognosis(NT-proBNP, LVEF) and the differences in safety were corrected. To further clarify whether optimizing thrombus aspiration can improve myocardial perfusion and prognosis in patients with STEMI, so as to provide new life and new perspective for the “ancient” method of thrombus aspiration therapy.
A total of 129 STEMI patients were selected in Bengang General Hospital from November 4, 2020 to January 25, 2022(males 101, females 28),the maximum age is 86, the minimum age is 34, the average age is(59.3 ± 10.7).
Inclusion criteria:(1) Patients with acute ST-segment elevation myocardial infarction within 12 h of onset according to the international common diagnostic criteria were enrolled. (2) Coronary angiography showed 100% occlusion of IRA,vessel diameter ≥2.Omm,no obvious tortuosity and calcification. (3) There was no contraindication of antiplatelet and anticoagulant therapy. (4) With a state of high thrombus burden should be aspirated. All enrolled subjects conform to four inclusion criteria.
The state of high thrombus burden: Coronary angiography showed long thrombus more than three times the diameter of the reference vessel; floating thrombus at the proximal end of the occluded vessel; the proximal end of the occluded vessel had >5 mm long strip thrombus; sudden complete occlusion of the proximal vessel without tapering; coronary artery occlusion-related vessels >4.0 mm;contrast agent was retained distal to the occluded vessel.
Exclusion criteria: (1) patients had undergone rescue PCI with intravenous thrombolysis; (2) history of intracranial hemorrhage; (3) ischemic stroke within 3 months; (4) suspected aortic dissection; (5) active bleeding or bleeding factors; (6) severe head and face injury within 3 months; (7) severe or poorly controlled hypertension; (8) severe trauma or major surgery or bleeding from vessels that could not be compressed within 3 weeks; (9) patients with malignant tumors; (10) complicated with severe liver and kidney dysfunction; (11) pregnant, lactating or at risk of becoming pregnant; (12)known allergies or contraindications to study drugs or contrast media; (13) patients had participated in other clinical trials at the same time; (14) patients after coronary artery bypass grafting; (15) Coronary angiography showed TIMI grade 3 blood flow in the culprit vessel without obvious signs of thrombosis. (16) patients with acute STEMI more than 12 h; (17) patients with acute non-STEMI;(18) The lesion was located in the left main coronary artery, the anterior trigeminal artery, the vessel was tortuous and calcified, the lesion was diffuse, and multiple stents were implanted more than 3 pieces; (19) blood pressure ≤90/60 mmHg;shock; Severe heart failure.
This study was approved and consented to participate by the Ethics Committee of China Resources Medical Group Bengang General Hospital (Approval No.:No.1,2020-010, Bengang General Hospital Ethical Review).This study has been registered in the Chinese Clinical Trial Registry (registration number: ChiCTR2300073410; Reg Date:10/07/2023).Informed consent was obtained from all subjects. This study was consented to publication.
A randomized, parallel, controlled design was used in this study, the random number table method was used for randomization. For STEAMI patients who conform to four inclusion criteria and did not meet the exclusion criteria, They were randomly divided into the control group(Subgroup A + B)(males 49, females 15)(average age 60.7 ± 11.7years)and experimental group (Subgroup C + D), (males52,females13) (average age57.9 ± 9.3years). Subgroup A included 32 patients(males 24, females 8) (average age 58.6 ± 8.3years).Subgroup B included 32 patients (males 25, females 7) (average age 62.8 ± 7years).Subgroup C included 33 patients (males 26, females 7)(average age 59.7 ± 10.2years).Subgroup D included 32 patients (males 26, females 6)(average age56.1 ± 9.7years).All patients underwent primary PCI, A loading dose of 300 mg aspirin (Bayer HealthCare Manufacturing S.r.l.Batch number: 3J71004) and Clopidogrel (Sanofi-aventis groupe, Batch number:BA992)300–600 mg or Ticagrelor (Astrazeneca Pharmaceuticals LTD. Batch number:2301050) 180 mg was given before surgery. In the control group, PTCA was performed before thrombus aspiration after emergency coronary angiography guide wire passage, Then, primary PCI was performed. In the experimental group, thrombus aspiration was performed directly after the emergency coronary angiography guide wire was passed, primary PCI was performed after thrombus aspiration was completed. Thrombus aspiration was Less than or equal to 4 times in groups A and C; Thrombus aspiration was performed more than 4 times in groups B and D. In the case of slow flow and no reflow during operation, Sodium Nitroprusside(Hainan Puli Pharmaceutical Co. LTD. Batch number:120721000) and Tirofiban[Broad Pharma (China) Co., LTD.Batch number:220802]can be injected into the coronary artery.
(1) TIMI flow grade and cTFC after thrombus aspiration and stenting,the incidence of no-reflow and slow reflow,frequency and dosage of drug intervention during stenting. (2) Evaluate the grade of classification of aspirated thrombus.Grading methods of thrombus: Grade 0:no thrombus visible to the naked eye;Grade 1: the total length of thrombus aspirated was less than 5 mm; Grade 2: total length of aspirated thrombus 5–10 mm; Grade 3: The total length of the aspirated thrombus was greater than 10 mm. (3)Evaluate the amplitude of ST-segment resolution on ECG at 2, 4, 6, 12 and 24 h after stenting;the peak values of serum TPI and CK-MB at 12 h and 24 h after stenting. (4) NT-proBNP and LVEF at 24 h, 30 days and 180 days after stenting. (5) Intraoperative and postoperative bleeding complications,stroke events and MACE events (death, reinfarction, target vessel revascularization) at 30 days and 180 days after stenting were recorded.
SPSS26.0 software was used for data processing. Measurement data were expressed as , T-test, analysis of variance and LSD post hoc test were used for comparison between groups. Count data were expressed as percentages, Rank sum test was used for comparison between groups. Logistic stepwise regression model was used for multivariate correlation. The cumulative incidence of stroke events and MACE events was detected by Kaplan-Meier method. P < 0.05 was considered statistically significant.
1. A total of 129 patients were enrolled, a total of 9 cases were lost to follow-up (2 cases in group A, 2 cases in group B, 3 cases in group C and 2 cases in group D), The total loss rate of follow-up was 6.98%. A total of 120 cases completed the follow-up, including 60 cases in the control group (30 cases in group A, 30 cases in group B) and 60 cases in the experimental group (30 cases in group C, 30 cases in group D). The shortest follow-up time was 6 months and the longest was 21 months, The average follow-up time was (13.92 ± 4.18) months, and the median follow-up time was 14 months. The average times of thrombus aspiration in the four groups were (3.80 ± 0.48) times in group A, (6.63 ± 1.30) times in group B, (3.77 ± 0.43) times in group C and (6.60 ± 1.07) times in group D.
2. The measurement data of 120 patients were in accordance with normal distribution. There was no significant difference in age, gender, BMI, SO2B (Symptom onset to balloon time), D2B (Door to balloon time), lesion location,number of stents, concomitant diseases, risk factors, preoperative medication between the two groups by homogeneity of variance test (P > 0.05).
3. Comparison of thrombus aspiration classification between groups.
3.1 Comparison of thrombus aspiration classification between control group and experimental group:After thrombus aspiration,the classification of thrombus in the experimental group was higher than that in the control group, and the difference was statistically significant (P = 0.008) (Table 1 and Figure 1A).
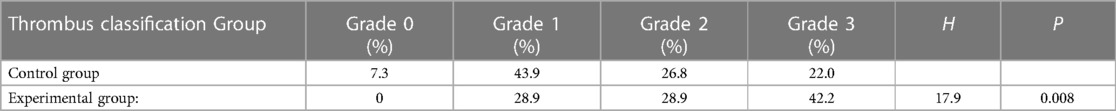
Table 1. Comparison of thrombus classification between the control group and the experimental group.
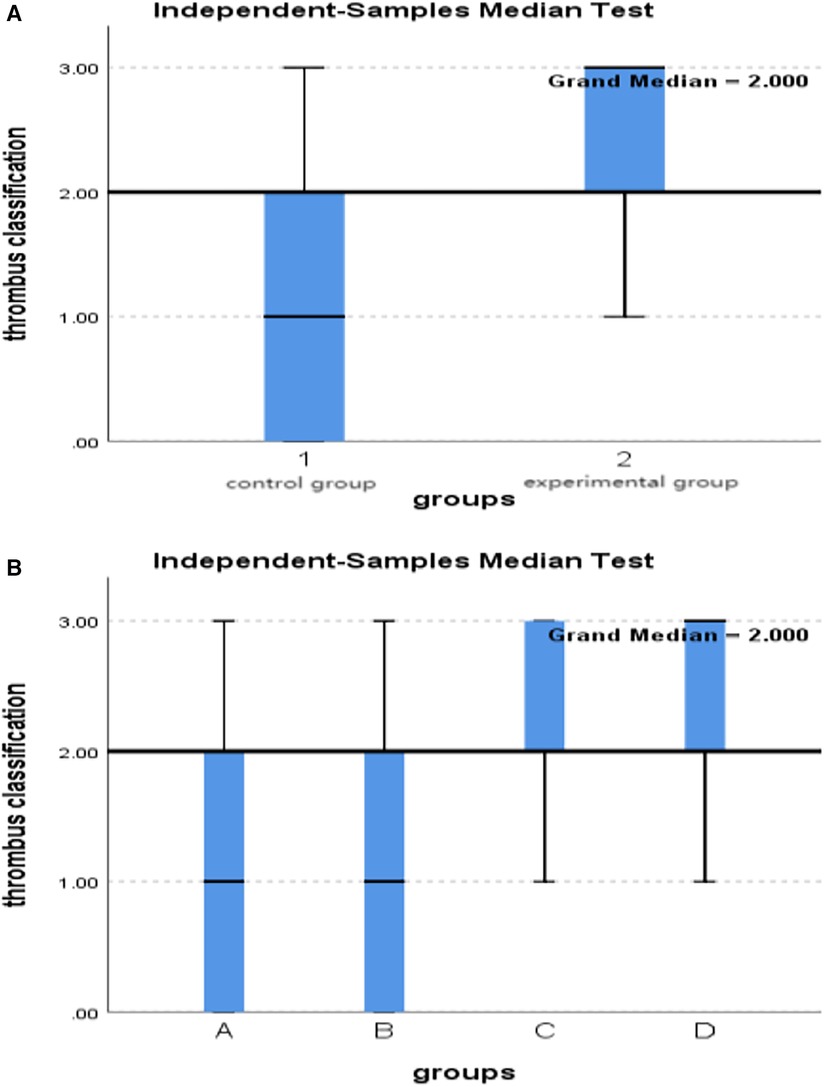
Figure 1. (A) Comparison of thrombus classification in two groups. (B) Comparison of thrombus classification among subgroups A, B, C and D.
3.2 Comparison of thrombus aspiration classification between subgroups A, B, C, and D:After thrombus aspiration,the classification of grade 2 and 3 thrombi extracted in groups C and D was higher than that in groups A and B, with statistically significant differences (P = 0.018) (Table 2 and Figure 1B).
4. Comparison of TIMI flow grade between-groups.
4.1 Comparison of TIMI flow grade between control group and experimental group: The TIMI flow grade after thrombus aspiration in the experimental group was better than that in the control group (P = 0.03). After stenting, there was no significant difference in TIMI flow grade between the two groups (P = 0.17) (Table 3 and Figures 2A,B).
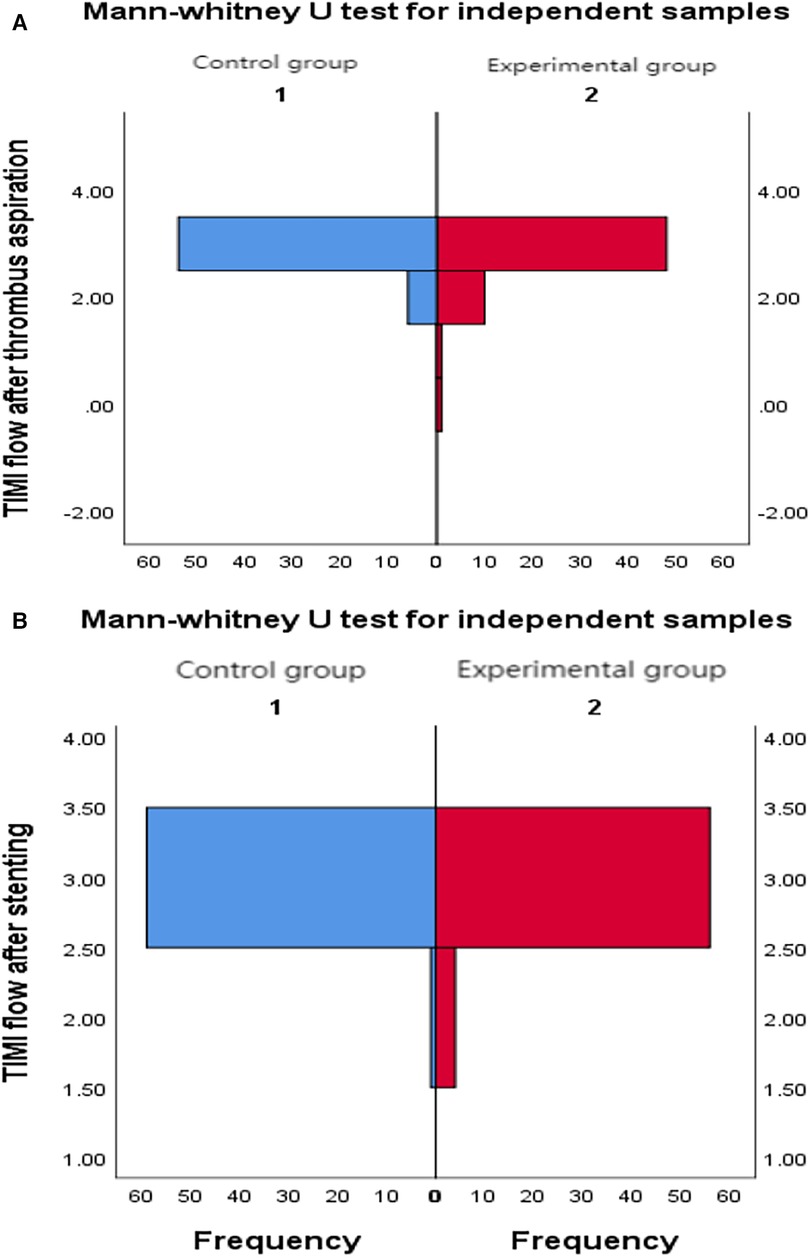
Figure 2. (A) Comparison of TIMI flow grade between two groups after thrombus aspiration. (B) Comparison of TIMI flow grade between two groups after stenting.
4.2 Comparison of TIMI flow grade between subgroups A, B, C, and D: after thrombus aspiration, TIMI flow grade in group B was lower than that in groups A, C, and D (P = 0.009); After stenting, the TIMI flow grade in group B was lower than that in groups A and D (P = 0.03) (Table 4).
5. Comparison of cTFC between groups
5.1 Comparison of cTFC between control group and experimental group: After thrombus aspiration, the cTFC of the experimental group was lower than that of the control group, and there was no significant difference between the two groups (P = 0.56). After stenting, the cTFC of the experimental group was lower than that of the control group, and the difference was statistically significant (P = 0.003) (Table 5).
5.2 Comparison of cTFC between subgroups A, B, C, and D: The cTFC of group B was higher than that of group A, C and D after thrombus aspiration, and the difference was not statistically significant(P = 0.37). After stenting, the cTFC of group B was higher than that of groups A, C, and D (P = 0.001), and the CTFC of group C was better than that of groups A and D(P = 0.94) (Table 6).
6. There was no significant difference in ST segment resolution between the control group and the experimental group, and among the four subgroups A, B, C, and D (Tables 7, 8).
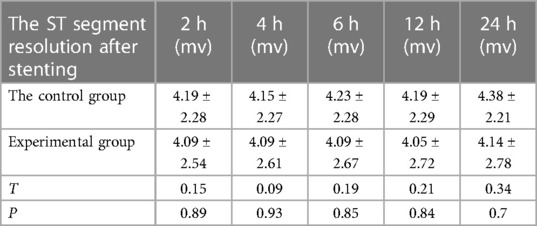
Table 7. Comparison of ST segment resolution after stenting between the control group and the experimental group.
7. There was no significant difference in TPI at 12 h and 24 h after stenting between the control group and the experimental group, and among the four subgroups A, B, C and D (Tables 9, 10). (TPI was detected by chemiluminescence method, and some values exceeded the limit range, which may affect the results of statistical data.)
8. Comparison of CK-MB between groups
8.1 Comparison of CK-MB between the control group and the experimental group: the peak value of CK-MB in the experimental group was lower than that in the control group at 12 h and 24 h after stenting,and the difference was statistically significant (P = 0.007, P = 0.016) (Table 11).
8.2 Comparison of CK-MB values between subgroups A, B, C and D: CK-MB values in group B were significantly higher than those in groups A, C and D at 12 h and 24 h after operation (P = 0.006, P = 0.016) (Table 12).
9. Comparison of no-reflow and slow flow rates between groups
9.1 Comparison of no-reflow and slow flow rates between the control group and the experimental group: The incidence of no-reflow in the experimental group was lower than that in the control group after thrombus aspiration (P = 0.04), and there was no significant difference between the two groups after stenting (P = 0.31).The incidence of slow flow in the experimental group was lower than that in the control group after thrombus aspiration and stenting (P = 0.03, P = 0.005) (Table 13 and Figures 3A–D).
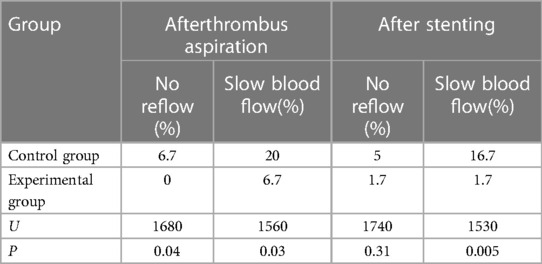
Table 13. Comparison of the incidence of no-reflow and slow blood flow between the experimental group and the control group.
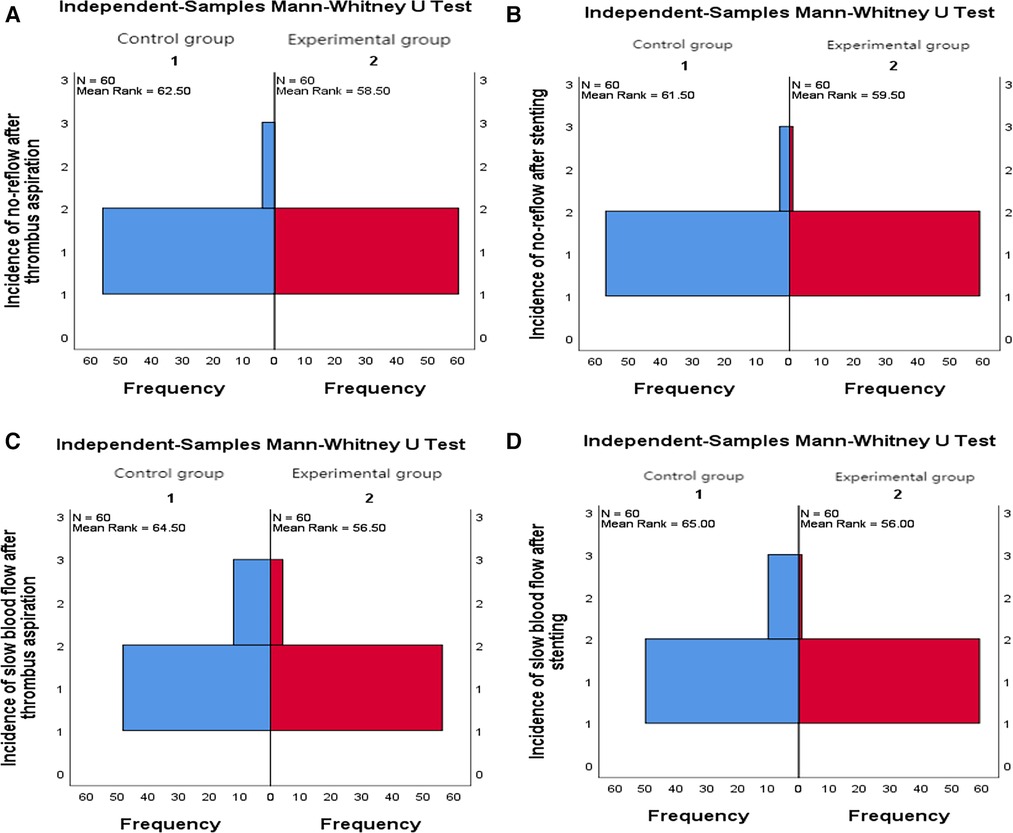
Figure 3. (A) Comparison of the incidence of no-reflow after thrombus aspiration between the two groups. (B) Comparison of the incidence of no-reflo after stenting between the two groups. (C) Comparison of the incidence of slow flow after thrombus aspiration between the two groups. (D) Comparison of the incidence of slow blood flow after stenting between the two groups.
9.2 Comparison of no-reflow and slow flow rates values between subgroups A, B, C and D: The incidence of slow flow in group B was higher than that in group C and group D after stenting (P = 0.029) (Table 14).
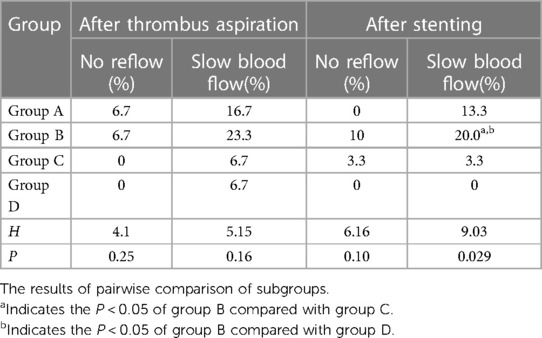
Table 14. Comparison of the incidences of no-reflow and slow biood flow among subgroups A, B, C and D.
10. Comparison of intraoperative drug intervention between the two groups: In order to obtain the same TIMI flow grade3 after stenting, the frequency of tirofiban in the experimental group was lower than that in the control group, and the difference was statistically significant (P = 0.002).The dosage of sodium nitroprusside in the experimental group was lower than that in the control group, and the difference was statistically significant (P = 0.001) (Table 15 and Figures 4A,B).
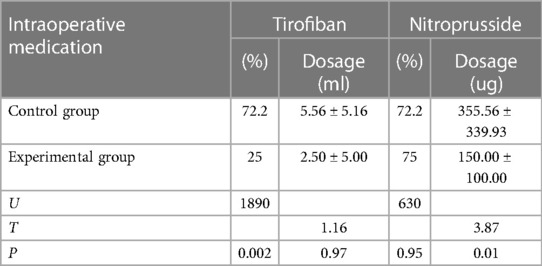
Table 15. Comparison of intraoperative medication between the control group and the experimental group.
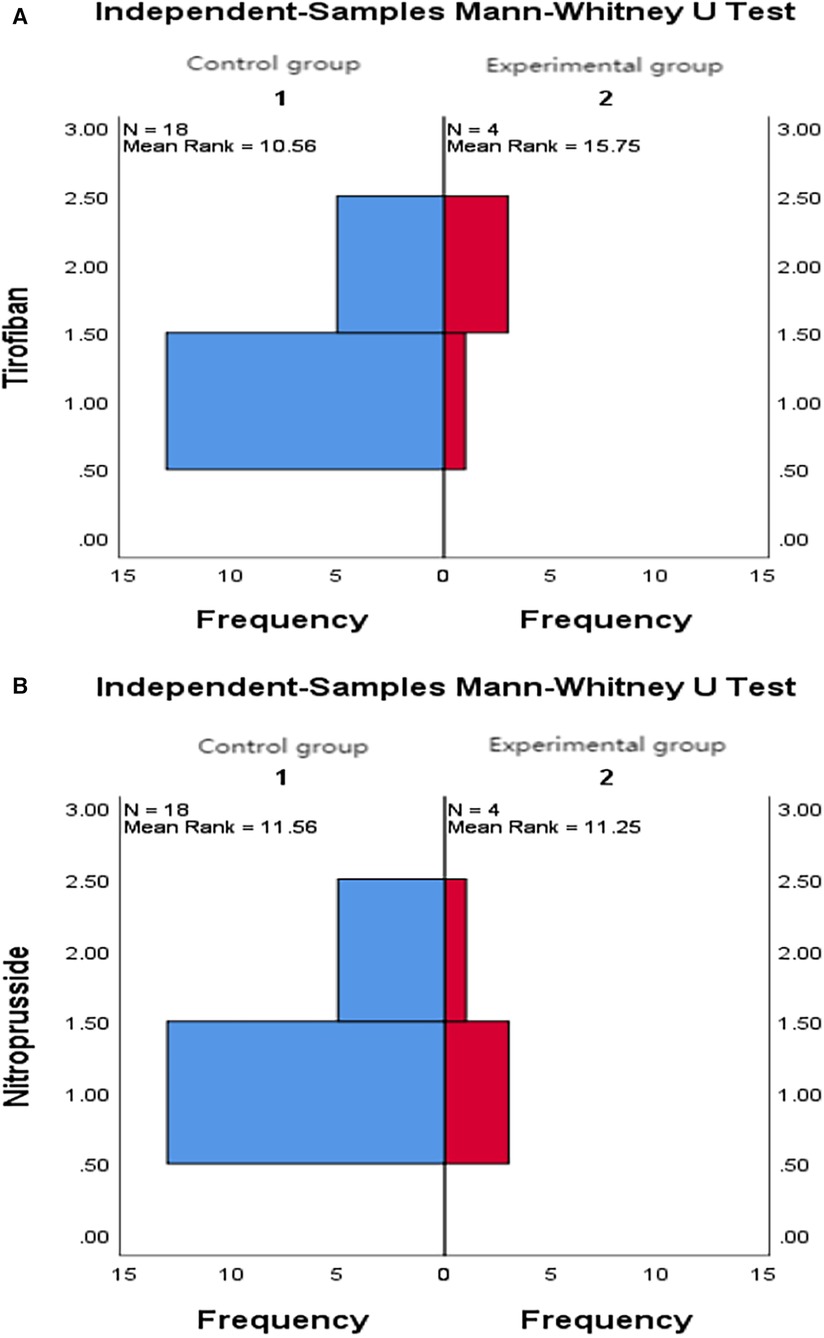
Figure 4. (A) Comparison of intraoperative tirofiban application between the two groups. (B) Comparison of intraoperative nitroprusside application between the two groups.
11. Comparison of NT-proBNP between groups
11.1 Comparison of NT-proBNP levels between the control group and the experimental group at 24 h, 30 days, and 180 days after stenting:The value of NT-proBNP in the experimental group was lower than that in the control group at 24 h after stenting, but the difference was not statistically significant (P = 0.156). The value of NT-proBNP in the experimental group was lower than that in the control group at 30 days and 180 days after stenting, and the difference was statistically significant (P = 0.002, P = 0.04) (Table 16 and Figure 5).
11.2 Comparison of NT-proBNP levels between subgroups A, B, C and D at 24 h, 30 days, and 180 days after stenting: The level of NT-proBNP in group B was significantly higher than that in group A and D at 24 h, 30 days and 180 days after stenting (P = 0.042). At 30 days after stenting, NT-proBNP in group B was significantly higher than that in group C and group D (P = 0.019), and NT-probnp in group A was significantly higher than that in group C and group D (P = 0.02). At 180 days after stenting, NT-proBNP in group B was significantly higher than that in group C and group D (P = 0.045) (Table 17 and Figure 6).
12. Comparison of LVEF between groups
12.1 Comparison of LVEF between the control group and the experimental group at 24 h, 30 days and 180 days after stenting: LVEF in the experimental group was significantly higher than that in the control group at 24 h and 30 days after stenting(P = 0.01, P = 0.04). LVEF in the experimental group was still higher than that in the control group at 180 days after stenting,but there was no significant difference between the two groups (P = 0.09) (Table 18 and Figure 7).
12.2 Comparison of LVEF between subgroups A, B, C and D at 24 h, 30 days and 180 days after stenting:Comparison of LVEF among subgroups A, B, C and D: LVEF in group A was lower than that in group C at 24 h after stenting(P = 0.03) (Table 19 and Figure 8).
13. Stepwise regression analysis of LVEF at 24 h, 30 days and 180 days after stenting, as shown in Table 20, LVEF at 24 h after stenting was highly correlated with the location of the lesion; LVEF at 30 days after stenting was highly correlated with lesion location, hypertension and smoking; LVEF at 180 days after stenting was highly correlated with SO2B, hypertension, smoking and BMI (Table 20 and Figures 9A–E).
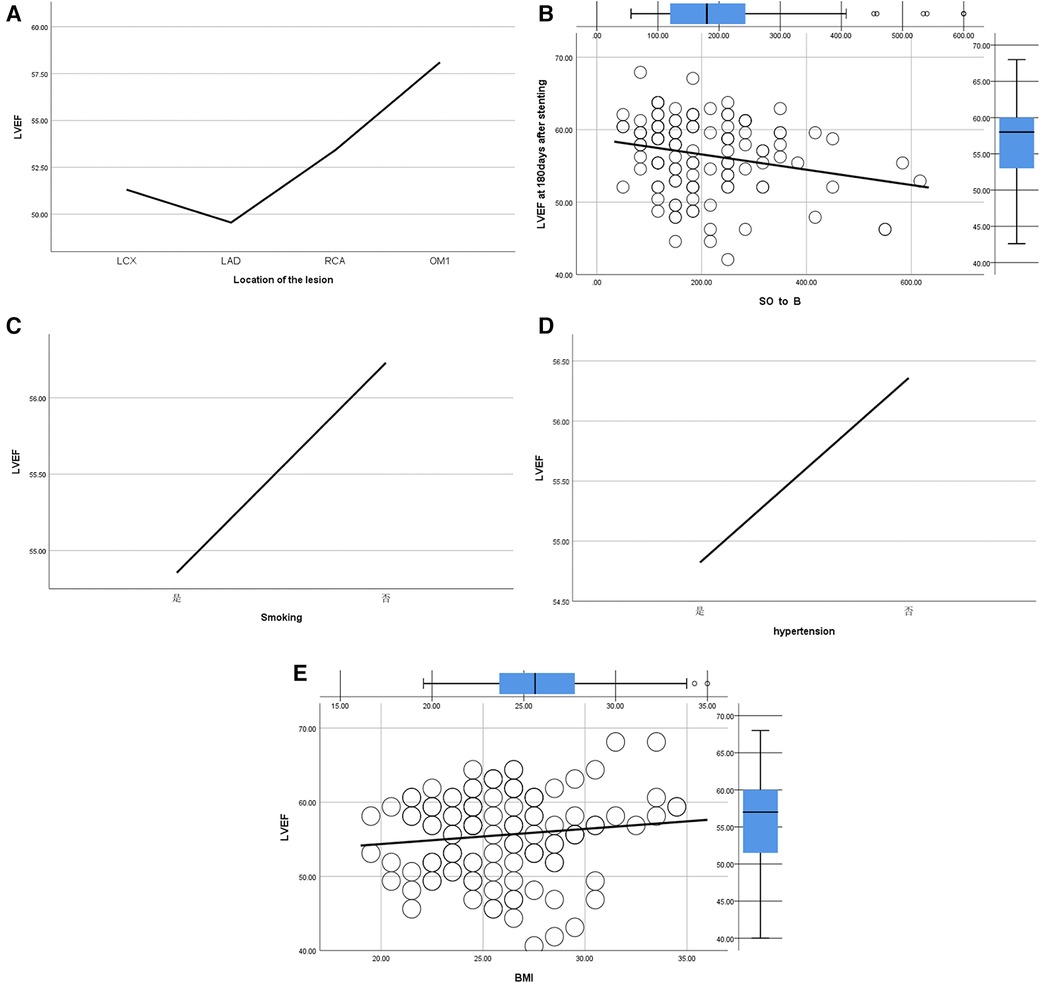
Figure 9. (A) Regression analysis of LVEF and location of the lesion. (B) Regression analysis of LVEF and SO2B. (C) Regression analysis of LVEF and smoking. (D) Regression analysis of LVEF and hypertension. (E) Regression analysis of LVEF and BMI.
14. By grading the suction times of 120 patients, the effects of different suction times on immediate myocardial blood flow, myocardial perfusion and cardiac function were analyzed, and the optimal suction times were analyzed. The influence of different suction times on myocardial perfusion and cardiac function prognosis was analyzed, and the optimal suction times was 4–5times (Table 21).
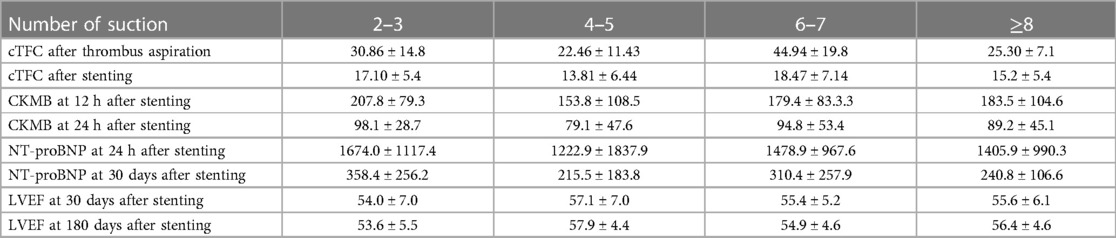
Table 21. Effects of different suction times on myocardial perfusion and cardiac function prognosis.
15. There was no significant difference in the cumulative incidence of intraoperative and postoperative bleeding events, stroke events and MACE events between the two groups by Kaplan-Meier analysis.
The preferred reperfusion strategy for STEMI is primary PCI. Coronary microcirculation dysfunction (CMD), such as slow flow and no-reflow, occurs in 5%–50% of patients when IRA is opened, which aggravate myocardial injury and increase the incidence of heart failure and mortality (6, 7). Relevant literature points out that the mechanism of CMD is related to a variety of factors, such as microcirculation embolism and spasm, ischemia/reperfusion injury, lack of ischemic preconditioning, and individual differences (8). During the interventional procedure for STEMI patients, thrombus and plaque on the vessel wall form tiny thrombus and plaque fragments under the mechanical action of catheters, guidewires, balloons and stents, which lead to embolism and spasm with the blood flow to the distal microcirculation (9). The degree of embolism and spasm is closely related to the accumulation of debris falling off during the operation. A decrease in myocardial perfusion is induced when coronary microcirculation is obstructed by more than 50%. Standardized surgical procedures can effectively reduce iatrogenic microcirculation embolism and spasm.
The treatment of CMD mainly includes drug therapy and non-drug therapy. Thrombus aspiration, as one of the non-drug treatment strategies, can effectively reduce the thrombus burden, reduce the incidence of CMD and improve myocardial perfusion. Meta-analysis studies have shown that patients with high thrombus burden can benefit from thrombus aspiration (10). In the subgroup analysis of the TOTAL study, the thrombus burden after thrombus aspiration in the direct thrombus aspiration group was compared with that after balloon dilation in the PCI group, and it was found that there was no significant difference between the two groups. It is believed that thrombus aspiration and balloon dilation can achieve the same effect of reducing thrombus burden (11). However, thrombus aspiration is to pull the thrombus out of the body to reduce the thrombus load. After balloon dilatation, some thrombus and plaque fragments fall off to the distal end of the blood vessel, which is bound to affect the microcirculation. In this study, optimized thrombus aspiration (experimental group) was performed in patients with TIMI0 blood flow and high thrombus burden, compared with the thrombus aspiration group after balloon dilation (control group). The results showed that the amount of thrombus aspirated in the experimental group was significantly more than that in the control group, and the thrombus load was reduced. In the control group, part of the thrombus fell off to the distal end of the blood vessel after balloon dilatation, and this part of the thrombus would cause obstacles to the vascular microcirculation. In this study, the incidence of slow flow and no-reflow in the experimental group was significantly lower than that in the control group, and the TIMI flow and cTFC after thrombus aspiration in the experimental group were better than those in the control group. Although there was no significant difference in TIMI flow grade after stent implantation between the two groups, the cTFC after thrombus aspiration and stent implantation in the experimental group was significantly lower than that in the control group, indicating that optimized thrombus aspiration can improve myocardial perfusion in patients with high thrombus burden and reduce the incidence of slow flow and no-reflow.
GPIIb/IIIa receptor antagonist and sodium nitroprusside can effectively prevent and improve the incidence of slow flow and no-reflow during PCI (12–15).In this study, the frequency of tirofiban and total dosage of sodium nitroprusside used in the control group were significantly higher than those in the experimental group. The incidence of slow flow and no-reflow in the control group was higher than that in the experimental group, indicating that the optimized thrombus aspiration can affect the immediate blood flow and reduce the incidence of slow flow and no-reflow. TIMI flow grade only represents epicardial blood perfusion and does not represent normal myocardial perfusion (16). This study showed that there was no significant difference in TIMI flow grade between the two groups after stent implantation, but the cTFC of the experimental group was significantly lower than that of the control group, indicating that optimized thrombus aspiration not only affected the immediate coronary flow, but also significantly improved the immediate myocardial perfusion. In TOTAL study, although TIMI flow grade 3 was achieved in both the thrombectomy group and the primary PCI group, microcirculatory disturbances such as cTFC or myocardial staining were not compared. In this study, even if the same TIMI flow grade 3 is achieved after stent implantation, optimized thrombus aspiration can better improve microcirculation and myocardial perfusion.
Related studies have shown that patients with low levels of cTFC have better cardiac function recovery after direct PCI and PTCA in IRA-related vessels (17). The results of this study showed that the CK-MB values of the experimental group at 12 h and 24 h after operation were significantly lower than those of the control group, indicating that the amount of myocardial necrosis in the experimental group was less than that in the control group. Compared with the control group, the optimized thrombus aspiration reduced the amount of myocardial necrosis and played a role in myocardial protection. The cTFC of the experimental group was significantly lower than that of the control group. The LVEF and NT-proBNP of the experimental group were significantly better than those of the control group at 24 h and 30 days after operation, and lasted for 180 days. It is suggested that the first optimization of thrombus aspiration is beneficial to the improvement of cardiac function in the short and medium term.
This study found that LVEF was significantly correlated with total ischemic time after myocardial infarction, smoking, hypertension, BMI and lesion location. Patients with long total ischemic time, smoking, hypertension, obesity and LAD lesions had lower left ventricular ejection fraction. Therefore, patients are advised to quit smoking, strictly control hypertension, lose weight and open the IRA as soon as possible after myocardial infarction to shorten the total ischemic time.
In order to ensure TIMI flow grade 3 after stenting, the amplitude of ST-segment resolution of electrocardiogram at 2 h, 4 h, 6 h, 12 h and 24 h after stenting was observed. There was no significant difference between the two groups, indicating that the electrical changes of necrotic myocardium may be later than myocardial perfusion.
The number of suctioning was stratified into 4 levels:2–3times,4–5times,6–7times and greater than or equal to 8 times. The effects of different levels of suctioning times on TIMI frame count, CK-MB, NT-ProBNP and LVEF were analyzed, concluding that the optimal number of suction was 4–5 times.
In this study, 120 patients were followed up for 6–21 months, and there were no stroke events. The follow-up results showed that there were no significant differences in the cumulative incidence of bleeding events, stroke and MACE events between the two groups. The thrombectomy procedure was standardized by experienced surgeons.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the Ethics Committee of China Resources Medical Group Bengang General Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Authors participated in paper topic selection and design, or participate in data analysis and interpretation; revised the key theories or other main contents in the paper; supported with work, including statistical analysis, technology or materials. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1249924/full#supplementary-material
1. Svilaas T, Vlaar PJ, van der Horst IC, Diercks GFH, de Smet BJGL, van den Heuvel AFM, et al. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. (2008) 358(6):557–67. doi: 10.1056/NEJMoa0706416
2. Fröbert O, Lagerqvist B, Olivecrona GK, Omerovic E, Gudnason T, Maeng M, et al. Thrombus aspiration during ST-segment elevation myocardial infarction. N Engl J Med. (2013) 369(17):1587–97; Erratum in: N Engl J Med.2014;371(8):786. doi: 10.1056/NEJMoa1308789
3. Jolly SS, Cairns JA, Yusuf S, Rokoss MJ, Gao P, Meeks B, et al. TOTAL Investigators.outcomes after thrombus aspiration for ST elevation myocardial infarction: 1-year follow-up of the prospective randomised TOTAL trial. Lancet. (2016) 387(10014):127–35. doi: 10.1016/S0140-6736(15)00448-1
4. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. ESC Scientific document group.2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC). Eur Heart J. (2018) 39(2):119–77. doi: 10.1093/eurheartj/ehx393
5. Kolh P, Windecker S, Alfonso F, Collet JP, Cremer J, Falk V, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European society of cardiology (ESC) and the European association for cardio-thoracic surgery (EACTS) Developed with the special contribution of the European association of percutaneous cardiovascular interventions (EAPCI). Eur Heart J. (2014) 35(37):2541–619. doi: 10.1093/eurheartj/ehu278
6. Durante A, Camici PG. Novel insights into an “old” phenomenon: the no reflow. Int J Cardiol. (2015) 187:273–80. doi: 10.1016/j.ijcard.2015.03.359
7. Cenko E, Ricci B, Kedev S, Kalpak O, Câlmâc L, Vasiljevic Z, et al. The no-reflow phenomenon in the young and in the elderly. Int J Cardiol. (2016) 222:1122–8. doi: 10.1016/j.ijcard.2016.07.209
8. Butler MJ, Chan W, Taylor AJ, Dart AM, Duffy SJ. Management of the no-reflow phenomenon. Pharmacol Ther. (2011) 132(1):72–85. doi: 10.1016/j.pharmthera.2011.05.010
9. Allencherril J, Jneid H, Atar D, Alam M, Levine G, Kloner RA, et al. Pathophysiology, diagnosis, and management of the no-reflow phenomenon. Cardiovasc Drugs Ther. (2019) 33(5):589–97. doi: 10.1007/s10557-019-06901-0
10. Bhindi R, Kajander OA, Jolly SS, Kassam S, Lavi S, Niemelä K, et al. Culprit lesion thrombus burden after manual thrombectomy or percutaneous coronary intervention-alone in ST-segment elevation myocardial infarction: the optical coherence tomography sub-study of the TOTAL (ThrOmbecTomy versus PCI ALone) trial. Eur Heart J. (2015) 36(29):1892–900. doi: 10.1093/eurheartj/ehv176
11. Jolly SS, James S, Džavík V, Cairns JA, Mahmoud KD, Zijlstra F, et al. Thrombus aspiration in ST-segment-elevation myocardial infarction: an individual patient meta-analysis: thrombectomy trialists collaboration. Circulation. (2017) 135(2):143–52. doi: 10.1161/CIRCULATIONAHA.116.025371
12. Su Q, Li L, Naing KA, Sun Y. Safety and effectiveness of nitroprusside in preventing no-reflow during percutaneous coronary intervention: a systematic review. Cell Biochem Biophys. (2014) 68(1):201–6. doi: 10.1007/s12013-013-9690-9
13. Zhao S, Qi G, Tian W, Chen L, Sun Y. Effect of intracoronary nitroprusside in preventing no reflow phenomenon during primary percutaneous coronary intervention: a meta-analysis. J Interv Cardiol. (2014) 27(4):356–64. doi: 10.1111/joic.12133
14. Prati F, Romagnoli E, Limbruno U, Pawlowski T, Fedele S, Gatto L, et al. Randomized evaluation of intralesion versus intracoronary abciximab and aspiration thrombectomy in patients with ST-elevation myocardial infarction: the COCTAIL II trial. Am Heart J. (2015) 170(6):1116–23. doi: 10.1016/j.ahj.2015.08.020
15. Ma Q, Ma Y, Wang X, Li S, Yu T, Duan W, et al. Intracoronary compared with intravenous bolus tirofiban on the microvascular obstruction in patients with STEMI undergoing PCI: a cardiac MR study. Int J Cardiovasc Imaging. (2020) 36(6):1121–32. doi: 10.1007/s10554-020-01800-0
16. Konijnenberg LSF, Damman P, Duncker DJ, Kloner RA, Nijveldt R, van Geuns R-JM, et al. Pathophysiology and diagnosis of coronary microvascular dysfunction in ST-elevation myocardial infarction. Cardiovasc Res. (2020) 116(4):787–805. doi: 10.1093/cvr/cvz301
17. Hamada S, Nishiue T, Nakamura S, Sugiura T, Kamihata H, Miyoshi H, et al. TIMI Frame count immediately after primary coronary angioplasty as a predictor of functional recovery in patients with TIMI 3 reperfused acute myocardial infarction. J Am Coll Cardiol. (2001) 38(3):666–71. doi: 10.1016/s0735-1097(01)01424-3
Keywords: optimized thrombus aspiration, ST-segment elevation myocardial infarction, microcirculation disturbance, myocardial perfusion, infarct-related artery
Citation: Xu B, Zhang C, Wei W, Zhan Y, Yang M, Wang Y, Zhao J, Lin G, zhang W-w, Huo X, Shi B and Fan L (2023) Effect of optimized thrombus aspiration on myocardial perfusion and prognosis in acute ST-segment elevation myocardial infarction patients with primary percutaneous coronary intervention. Front. Cardiovasc. Med. 10:1249924. doi: 10.3389/fcvm.2023.1249924
Received: 29 June 2023; Accepted: 6 September 2023;
Published: 4 October 2023.
Edited by:
Alessandro Sciahbasi, Sandro Pertini Hospital, ItalyReviewed by:
Simona Minardi, University of L'Aquila, Italy© 2023 Xu, Zhang, Wei, Zhan, Yang, Wang, Zhao, Lin, zhang, Huo, Shi and Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Boning Xu eGJuMTk2M0AxNjMuY29t
†Chunxin Zhang and Wei Wei are the co-first authors
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.