
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Cardiovasc. Med. , 07 July 2023
Sec. Cardiac Rhythmology
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1244294
This article is part of the Research Topic Atrial Fibrillation in Dementia View all 6 articles
Editorial on the Research Topic
Atrial fibrillation in dementia
Atrial fibrillation (AF) and dementia are diseases with a significantly increasing incidence worldwide, associated with increased morbidity and mortality and high costs for national health systems. One the one hand, the lifetime risk of developing AF affects one in three persons. On the other hand, ischemic strokes, a leading contributor to dementia, are caused by AF in 20%–30% (1).
Several pathological mechanisms are suspected to be responsible for the association between AF and cognitive decline (2). As AF has a strong association with stroke, there is an association between AF and vascular dementia (3–7).
In this special issue of Frontiers in Cardiovascular Medicine, Gao et al. performed a Mendelian randomization analysis to investigate the causal genetic association between AF and vascular dementia. The authors were unable to provide evidence for a causal relationship between atrial fibrillation and vascular dementia; nevertheless, this finding is important for understanding the pathophysiology of the two diseases (Gao et al.).
Several longitudinal studies in the past provided evidence that an association between AF and dementia may exist even without prior stroke (8). A meta-analysis included studies with more than 75,000 patients without a history of stroke and normal baseline cognitive function. In this meta-analysis, a total of 15% of all patients had AF. After a median observation period of approximately eight years, 6.5% developed dementia. Baseline AF was independently associated with the later occurrence of dementia (5). In addition, the effects of AF on cognitive function were evaluated by the Cardiovascular Health Study which included over 5,000 participants without prior stroke. AF occurred in 11% of patients and was associated with more rapid deterioration of mean cognitive function compared with patients in sinus rhythm (6).
In this special issue, Chen et al. highlight that AF is associated with a significantly worse prognosis even in patients who already have dementia. However, the authors suggest that oral anticoagulation and antiarrhythmic medication of AF is associated with a better outcome. The finding should motivate geriatricians and cardiologists to optimally treat AF also in patients with pre-existing dementia (Chen et al.).
In this special issue, Wang et al. address the question of whether atrial flutter carries a similar risk of dementia compared to AF. The question is of interest because atrial flutter carries a similar (but not identical) risk of stroke compared to AF. In this large epidemiological study, data from Taiwan’s National Health Insurance Research Database were analyzed over a 12-year period. Dementia occurred in 9.82% of patients with AF and in 6.88% of patients with atrial flutter (p < 0.001), a finding that remained significantly different even after propensity score matching (Wang et al. 9). The result could indicate that the deleterious effect of AF on cerebral function, irregular blood pressure amplitudes in AF may be an independent factor in the development of cognitive dysfunction. It has been described previously that altered cerebral perfusion (10) and hippocampal atrophy in patients with AF may be due to irregular R-R intervals, abnormal or rapid heart rate, and reduced blood pressure (11).
AF also appears to be associated with the risk of developing Alzheimer’s disease. Numerous studies suggest that the occurrence of Alzheimer’s disease is related to hypoperfusion, inflammation, oxidative stress, and endothelial dysfunction. In addition, several circulating biomarkers of oxidative stress, inflammation, and endothelial dysfunction have been demonstrated to be elevated in AF (12). As these factors are also associated with dementia, it seems conceivable that AF, through these pathways, may be related to cognitive decline and dementia.
Several studies are currently investigating primary or secondary effects of various therapies, including anticoagulation and interventions, on cognitive function in patients with AF (13).
Knowing the close association between AF and dementia, further studies on diagnosis and therapy are of extraordinary clinical importance. Pulmonary vein isolation is the most effective therapy for paroxysmal and persistent AF. According to positive studies in recent years, pulmonary vein isolation is also expected to prevent deterioration of neurocognitive function (1). This question is addressed by Zwimpfer et al. in their prospective, multicenter SwissAtrial Fibrillation Cohort study (Swiss-AF) in which patients who underwent pulmonary vein isolation were included and compared with patients who were treated conservatively. Neurocognitive analysis included several tests, including the Montreal Cognitive Assessment, and was performed at study inclusion and after one year. Notably, this study revealed no association between treatment by pulmonary vein isolation and neurocognitive function. The authors note that there have been studies in the past with contrary results. In addition, the number of patients with pulmonary vein isolation in the present study is low. Nonetheless, Zwimpfer et al. provide an important hint that influencing neurocognitive function with pulmonary vein isolation has to be questioned (Zwimpfer et al.).
Intervention studies that aim to investigate the benefit of pulmonary vein isolation, for example, have the fundamental problem that years and decades may pass between intervention and the onset of dementia. What is needed, therefore, are parameters of cognitive function that could measure subtle changes after just a few months or years. In this special issue, Lai et al. demonstrated that use of the telephone Montreal cognitive assessment in patients with AF is appropriate for screening mild cognitive impairment. The relatively simple telephone screening could be useful for further studies (Lai et al.).
Overall, this special issue of Frontiers in Cardiovascular Medicine provides an insight into the pathophysiology and epidemiology of AF and dementia. It also highlights the pitfalls and limitations of dementia prevention. Figure 1 illustrates the results of the discussed publications (Figure 1). As AF and dementia will increase in clinical importance in the future, further research is of utmost importance.
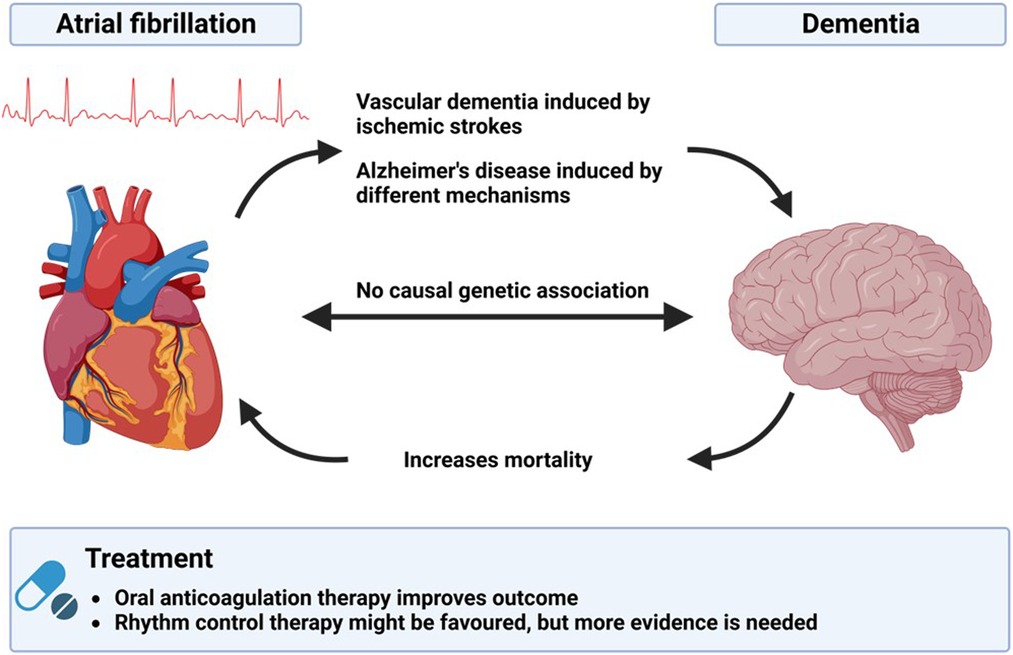
Figure 1. Illustration of the interactions between atrial fibrillation and demetia and possible therapeutic options.
Substantial contributions to the conception or design of the work provide approval for publication of the content agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European association for cardio-thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European society of cardiology (ESC) developed with the special contribution of the European heart rhythm association (EHRA) of the ESC. Eur Heart J. (2021) 42(5):373–498. doi: 10.1093/eurheartj/ehaa612; Erratum in: Eur Heart J. (2021 Feb 1) 42(5):507; Erratum in: Eur Heart J. (2021 Feb 1) 42(5):546–7; Erratum in: Eur Heart J. (2021).32860505
2. Anselmino M, Scarsoglio S, Ridolfi L, De Ferrari GM, Saglietto A. Insights from computational modeling on the potential hemodynamic effects of sinus rhythm versus atrial fibrillation. Front Cardiovasc Med. (2022) 9:844275. doi: 10.3389/fcvm.2022.844275
3. Ott A, Breteler MM, de Bruyne MC, van Harskamp F, Grobbee DE, Hofman A. Atrial fibrillation and dementia in a population-based study. The rotterdam study. Stroke. (1997) 28:316–21. doi: 10.1161/01.STR.28.2.316
4. Kilander L, Andren B, Nyman H, Lind L, Boberg M, Lithell H. Atrial fibrillation is an independent determinant of low cognitive function: a cross-sectional study in elderly men. Stroke. (1998) 29:1816–20. doi: 10.1161/01.STR.29.9.1816
5. Santangeli P, Di Biase L, Bai R, Mohanty S, Pump A, Cereceda Brantes M, et al. Atrial fibrillation and the risk of incident dementia: a meta-analysis. Heart Rhythm. (2012) 9:1761–8. doi: 10.1016/j.hrthm.2012.07.026
6. Thacker EL, McKnight B, Psaty BM, Longstreth W, Sitlani CM, Dublin S, et al. Atrial fibrillation and cognitive decline: a longitudinal cohort study. Neurology. (2013) 81:119–25. doi: 10.1212/WNL.0b013e31829a33d1
7. Singh-Manoux A, Fayosse A, Sabia S, Canonico M, Bobak M, Elbaz A, et al. Atrial fibrillation as a risk factor for cognitive decline and dementia. Eur Heart J. (2017) 38(34):2612–8. doi: 10.1093/eurheartj/ehx208
8. Saglietto A, Matta M, Gaita F, Jacobs V, Bunch TJ, Anselmino M. Stroke-independent contribution of atrial fibrillation to dementia: a meta-analysis. Open Heart. (2019) 6(1):e000984. doi: 10.1136/openhrt-2018-000984
9. Wang HT, Chen YL, Lin YS, Chen HC, Chong SZ, Hsueh S, et al. Differential risk of dementia between patients with atrial flutter and atrial fibrillation: a national cohort study. Front Cardiovasc Med. (2021) 8:787866. doi: 10.3389/fcvm.2021.787866; Erratum in: Front Cardiovasc Med. (2021) 8:819771.34869699
10. Saglietto A, Scarsoglio S, Canova D, Roatta S, Gianotto N, Piccotti A, et al. Increased beat-to-beat variability of cerebral microcirculatory perfusion during atrial fibrillation: a near-infrared spectroscopy study. Europace. (2021) 23(8):1219–26. doi: 10.1093/europace/euab070
11. Knecht S, Oelschlager C, Duning T, Lohmann H, Albers J, Stehling C, et al. Atrial fibrillation in stroke-free patients is associated with memory impairment and hippocampal atrophy. Eur Heart J. (2008) 29:2125–32. doi: 10.1093/eurheartj/ehn341
12. Goette A, Kalman JM, Aguinaga L, Akar J, Cabrera JA, Chen SA, et al. EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterization, and clinical implication. Europace. (2016) 18:1455–90. doi: 10.1093/europace/euw161
13. Dagres N, Chao TF, Fenelon G, Aguinaga L, Benhayon D, Benjamin EJ, et al. ESC Scientific document group. European heart rhythm association (EHRA)/heart rhythm society (HRS)/Asia pacific heart rhythm society (APHRS)/latin American heart rhythm society (LAHRS) expert consensus on arrhythmias and cognitive function: what is the best practice? Europace. (2018) 20(9):1399–421. doi: 10.1093/europace/euy046
Keywords: atrial fibrallation, atrial flutter, dementia, dementia after stroke, dementia alzheimer
Citation: Gotzmann M and Anselmino M (2023) Editorial: Atrial fibrillation in dementia. Front. Cardiovasc. Med. 10:1244294. doi: 10.3389/fcvm.2023.1244294
Received: 22 June 2023; Accepted: 28 June 2023;
Published: 7 July 2023.
Edited and Reviewed by: Elsayed Z. Soliman, Wake Forest University, United States
© 2023 Gotzmann and Anselmino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael Gotzmann bWljaGFlbC5nb3R6bWFubkBydWIuZGU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.