Abstract
Aims:
Cardiac decompensation (CD) in patients with aortic stenosis is a “red flag” for future adverse events. We classified patients undergoing transcatheter aortic valve implantation (TAVI) into those with acute, prior, or no prior CD at the timepoint of TAVI and compared their clinical presentation, prognosis, and effects of the prescribed medication during follow-up.
Methods:
Retrospective analysis of patients of one center fulfilling the criteria of 30-day device success after transfemoral TAVI.
Results:
From those patients with no CD (n = 1,985) ranging to those with prior CD (n = 497) and to those with acute CD (n = 87), we observed a stepwise increase in the proportion of patients in poor clinical condition, NYHA class III/IV, low psoas muscle area, fluid overload (rales, oedema, pleural effusion), reduced ejection fraction, renal insufficiency, and anemia. More diuretics but less renin-angiotensin system inhibitors (ACEI/ARB) were prescribed for patients with acute CD compared to other groups. Prior CD (hazard ratio and 95% CI 1.40; 1.02–1.91) and acute CD (1.72; 1.01–2.91), a reduced general condition (1.53; 1.06–2.20), fluid overload (1.54;1.14–2.08), atrial fibrillation (1.76; 1.32–2.33), and anemia (1.43;1.08–1.89) emerged as strong independent predictors of one-year mortality. In all three classes of CD, prescribing of ACEI/ARB was associated with a substantial improvement of survival.
Conclusions:
The clinical presentation of (acute or prior) cardiac decompensation in patients with AS overlapped substantially with that of patients with classical signs of heart failure. Our results may support an early treatment strategy in patients with left ventricular dysfuntion before clinical signs of congestion are manifest. Moreover, these patients require intensive medical attention after TAVI.
Introduction
A history of cardiac decompensation (CD) in patients with aortic stenosis (AS), due to increased afterload or myocardial malfunction, is one of the strongest predictors of outcomes, even after correction of afterload by surgical or transcatheter aortic valve implantation (TAVI) (1–5). The prompt treatment of severe AS in patients with acute CD may improve short-term outcomes and reduce hospital stay and treatment costs (6). While clinical signs and symptoms of patients with acute CD usually move clinicians towards a rapid diagnosis and treatment, it may be more challenging to identify and to interpret signs of cardiac congestion in patients with AS but without acute CD. Moreover, it remains unclear whether and to what extent the clinical presentation of decompensated patients with AS differs from that of patients with heart failure (HF) without concomitant AS and how these characteristics may impact further outcomes in the midterm after successful TAVI. We aimed to describe the clinical characteristics of patients with AS with or without a history of CD, determine their prognostic factors, and correlate clinical outcomes with the prescribed medication at hospital discharge.
Methods
Study design, participants, and setting
Patients undergoing transfemoral TAVI for symptomatic, severe AS (aortic valve area index <0.6 cm2/m2 or mean pressure gradient ≥40 mmHg) at a single, high-volume center were included consecutively in this retrospective, observational registry from January 2011 until January 2021. Only patients who were discharged from hospital with documented medication and who fulfilled the criteria of device success at 30 days post-TAVI according to the Valve Academic Research Consortium-3 (VARC-3) document (7) (freedom from mortality, surgery, or repeated device-related interventions, with intended performance of the valve) were included. Follow-up examinations were scheduled at 3 months (on an outpatient basis) followed by a one-year telephone follow-up call. Follow-up data were obtained from outpatient examinations, telephone interviews, or medical records from referring physicians.
Due to the retrospective nature of this study, a waiver of written informed consent was issued by the local ethics committee (University of Giessen), which approved the study protocol. The study complied with the Declaration of Helsinki.
Clinical parameters of interest
Medical reports of patients were screened for a history of CD, which was defined as an event of hospitalization due to fluid overload and accompanying dyspnea as documented in the medical history of the patient or as reported by the patient at the time of admission. Patients were then classified into one of three groups: no CD (no history of CD and patients never reported CD), prior CD (prior CD was documented, with timespan in months between last episode of CD and hospital admission for TAVI, or patients reported at least one episode of CD prior to admission, but presented in a stable and clinically compensated condition at admission), or acute CD (patients were referred to the hospital while suffering an episode of acute CD for urgent TAVI). Patients’ clinical condition (age-appropriate, reduced, or poor) and their signs (moist pulmonary rales, peripheral edema) and symptoms (NYHA classification) of cardiac congestion at the timepoint of hospital admission were documented. Type and dosage of the discharge medication after TAVI [angiotensin converting enzyme inhibitors or angiotensin receptor blockrs (ACEI/ARB), beta-blockers, mineralocorticoid antagonist, and statins] were assessed as described earlier (8). Fluid overload was defined in our study as the presence of any documented sign of congestion (pulmonary rales, peripheral edema, pleural effusion).
Computer tomographic parameters
Computed tomographic (CT) analysis was conducted retrospectively using imaging scans indicated for the planning of the TAVI procedure. Data analyses were performed on a dedicated workstation (syngo.via, Siemens Healthineers, Forchheim, Germany). The psoas muscle area (PMA) was measured in a single post-contrast axial slice using the freehand drawing tool. The slice was chosen at the level of L3 vertebrae in a way such that the lateral tips of both transverse processes were visible for better reproducibility. The left and right psoas muscle areas were carefully measured according to the pure geometrical anatomical boundaries. The areas of the left and right psoas muscle were added and the sum (in cm2) was indexed to the body surface area. The resulting PMAi was grouped in tertiles for women and men separately, resulting in sex-specific PMAi tertiles. CT scans were also screened for the presence of pleural effusion.
Outcome variables
The primary endpoint was death from any cause within one year post-intervention. Secondary endpoints were cardiovascular death according to the VARC-3 consensus document (7) and the combination of cardiovascular death and cardiac decompensation from the timepoint of discharge to one year after TAVI.
Statistical analysis
Continuous data are reported as median and interquartile range (IQR) and were compared by the Mann–Whitney Kruskal–Wallis test; categorical variables are reported as number and percent and were compared by the χ2 test. Survival curves were constructed using Kaplan–Meier estimates and were compared by the log-rank test. To account for covariates, univariate Cox proportional hazard models were used to calculate hazard ratios (HR). Variables with a statistically significant effect on the univariate analysis (p ≤ 0.01) were entered into a multivariable Cox proportional hazards model and underwent a stepwise bidirectional variable selection process. The following variables were included: body mass index, diabetes, atrial fibrillation, peripheral artery disease, Euroscore II, NYHA class III or IV, general condition, prior cardiac decompensation, fluid overload, glomerular filtration rate, anemia, ejection fraction <40%, mean transvalvular aortic pressure gradient <40%, moderate mitral or tricuspid regurgitation, indexed psoas muscle area tertiles, ACEI/ARB, statins. To appreciate the effect sizes of the predictors as well as the baseline hazard of the final Cox propotional hazards regression model, predictions from the model using clinically relevant prototypical values were constructed. All statistical analyses were performed using the SPSS statistical package version 26 (IBM Corp., Armonk, NY, USA) and R version 4.2.2 [R Core Team (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.]
Results
In this study population, 1,985 patients were assigned to the group that never experienced a CD (no CD), 497 patients were classified to have experienced at least one CD before hospital admission (prior CD), and 87 patients were diagnosed with a CD at the timepoint of hospital admission (acute CD). Patients with acute CD compared with those with prior CD or no CD had a higher prevalence of atrial fibrillation, anemia, chronic obstructive pulmonary disease, a worse renal function, and a higher calculated risk according to the EuroScore II (Table 1). They presented in a considerably worse clinical condition with significantly more symptoms and signs of fluid overload on clinical examination (pulmonary rales, peripheral edema) and exhibited most frequently the presence of pleural effusion as detected by CT. The ejection fraction was lowest in patients with acute CD, and these patients showed the highest rates of low-gradient aortic stenosis and significant atrio-ventricular valve regurgitation. The proportion of patients in the lowest sex-specific tertile of PMAi was highest among those with acute CD, indicating the highest prevalence of sarcopenia among this patient cohort. Slightly more patients with acute CD were treated with balloon-expandable valves.
Table 1
| No CD | Prior CD | Acute CD | P-Value | |
|---|---|---|---|---|
| n = 1,985 | n = 497 | n = 87 | ||
| Demographic data | ||||
| Female | 1,009 (50.8) | 281 (56.5) | 41 (47.1) | 0.050 |
| Age, year | 81.9 (78.6–84.9) | 82.5 (78.8–85.9) | 80.8 (77.3–84.7) | 0.032 |
| BMI, kg/m2 | 27.0 (24.3–30.4) | 26.8 (24.0–30.5) | 27.1 (23.8–32.2) | 0.634 |
| Cardiovascular and pulmonary disease | ||||
| Arterial hypertension | 1,796 (90.5) | 454 (91.3) | 73 (83.9) | 0.092 |
| Diabetes mellitus | 624 (31.4) | 204 (41.0) | 33 (37.9) | <0.001 |
| CAD | 1,202 (60.6) | 297 (59.8) | 51 (58.6) | 0.898 |
| Prior MI | 227 (11.4) | 73 (14.7) | 10 (11.5) | 0.136 |
| Atrial fibrillation | 740 (37.3) | 272 (54.8) | 55 (63.2) | <0.001 |
| Prior stroke | 262 (13.2) | 56 (11.3) | 8 (9.2) | 0.312 |
| Peripheral artery disease | 225 (11.3) | 59 (11.9) | 14 (16.1) | 0.390 |
| EuroScore II | 2.80 (2.01–4.32) | 3.91 (2.69–5.77) | 5.20 (3.59–7.99) | <0.001 |
| ICD at discharge | 32 (1.6) | 23 (4.6) | 10 (11.5) | <0.001 |
| COPD | 333 (16.8) | 111 (22.3) | 20 (23.0) | 0.008 |
| Clinical data | ||||
| NYHA class III/IV | 1,436 (72.3) | 439 (88.3) | 81 (93.1) | <0.001 |
| Reduced general condition | 1,193/1,952 (61.1) | 370/494 (74.9) | 62/86 (72.1) | <0.001 |
| Poor general condition | 21/1,952 (1.1) | 20/494 (4.0) | 23/86 (26.7) | |
| Frailty | 1,034 (52.1) | 312 (62.8) | 50 (57.5) | <0.001 |
| Moist rales | 43/1,947 (2.2) | 42/494 (8.5) | 26/86 (30.2) | <0.001 |
| Peripheral oedema | 323/1,936 (16.7) | 144/489 (29.4) | 53/84 (63.1) | <0.001 |
| Any congestion | 499/1,817 (27.5) | 250/464 (53.9) | 72/84 (85.7) | <0.001 |
| Laboratory data | ||||
| GFR, ml/min/1.73 m2 | 70 (51–89) | 55 (41–75) | 46 (34–74) | <0.001 |
| Anemia | 588/1,917 (30.7) | 198/486 (40.7) | 44/85 (51.8) | <0.001 |
| Echocardiographic data | ||||
| Ejection fraction, % | 65 (58–65) | 60 (45–65) | 50 (35–62) | <0.001 |
| Ejection fraction ≤40% | 125/1,917 (6.5) | 79/486 (16.3) | 26/85 (30.6) | <0.001 |
| MPG <40 mmHg | 677/1,917 (35.3) | 228/486 (46.9) | 54/85 (63.5) | <0.001 |
| Moderate MR or TR | 271 (13.7) | 129 (20.0) | 34 (39.1) | <0.001 |
| CT data | ||||
| Pleural effusion | 221/1,830 (12.1) | 147/458 (32.1) | 47/81 (58.0) | <0.001 |
| PMAi, cm2/m2 | 8.19 (6.92–9.85) | 7.88 (6.68–9.50) | 7.97 (6.61–9.35) | <0.001 |
| Lowest PMAi tertile | 572/1,795 (31.9) | 159/146 (34.9) | 39/81 (48.1) | 0.031 |
| Procedural data | ||||
| Balloon-expandable valve | 720 (36.3) | 181 (36.4) | 43 (49.4) | 0.044 |
Patient characteristics.
The percentage of patients with prescribed ACEI/ARB at discharge declined significantly when moving from those with no CD to those with acute CD, and even in those patients with acute CD treated by ACEI/ARB, the proportion of patients with a target dose ≥50% was half that of patients with no CD (Table 2). In contrast, beta-blockers, mineralocorticoid antagonists, and loop diuretics were more frequently prescribed in patients with acute CD. The prescribing of statins was slightly less frequent in patients with acute CD compared with the other groups.
Table 2
| No CD | Prior CD | Acute CD | P-Value | |
|---|---|---|---|---|
| n = 1,985 | n = 496 | n = 87 | ||
| ACEI/ARB | 1,591 (80.2) | 373 (75.2) | 57 (65.5) | <0.001 |
| ≥50% target dose | 1,042 (52.5) | 217 (43.8) | 22 (25.3) | <0.001 |
| Beta-blockers | 1,423 (71.7) | 425 (85.7) | 73 (83.9) | <0.001 |
| ≥50% target dose | 748 (37.7) | 231 (46.6) | 41 (47.1) | <0.001 |
| MR antagonists | 289 (14.6) | 136 (27.4) | 40 (46.0) | <0.001 |
| ≥50% target dose | 260 (13.1) | 121 (24.3) | 34 (39.1) | <0.001 |
| Loop diuretics | 1,040 (52.4) | 427 (86.1) | 84 (96.6) | <0.001 |
| Statins | 1,445 (72.8) | 327 (65.9) | 55 (63.2) | 0.003 |
| High-intensity statins | 171 (8.6) | 50 (10.1) | 11 (12.6) | 0.002 |
Discharge medication.
Data shown as number (%). ACEI/ARB, angiotensin converting enzyme inhibitors/angiogtensin receptor antagonists; MR antagonists, mineralocorticoid antagonists.
We further analyzed the patient group with prior CD. In this group, information on the timespan between the last CD and admission as well as information on fluid overload was available for 379 patients. The timespan ranged from 1 to 108 months: 190 patients (50.1%) reported the last CD 1 month before admission; 154 patients (40.6%) reported the last CD 2–6 months before admission; 35 patients (9.2%) reported the last CD >6 months before the last CD. Manifest fluid overload was documented in 117 (61.6%), 74 (48.1%), and 19 (54.3%) of patients with a timespan of 1, 2–6, or >6 months, respectively (0.042), which was mainly due to the presence of pleural effusion in 67/181 (37.0%), 47/153 (30.7%), and 5/34 (14.7%) patients, respectively (p = 0.033).
One-year all-cause mortality rates for patients with no, prior, or acute CD were 7.4%, 14.5%, and 28.7% (log-rank <0.001), and cardiovascular mortality was 4.1%, 9.3%, and 23.0%, (log-rank p < 0.001, Figure 1); the event rates for the combination of cardiovascular death or new CD were 7.1%, 15.7% and 33.3% (p < 0.001). In the subgroup of patients with prior CD only, patients with 1, 2–6 months, or >6 months timespan between CD and TAVI had all-cause one-year mortality rates of 16.3%, 12.3%, and 11.4%, respectively (log-rank = 0.625). Cardiovascular one-year mortality rates were 10.0%, 6.5%, and 8.6%, respectively (log-rank = 0.573).
Figure 1
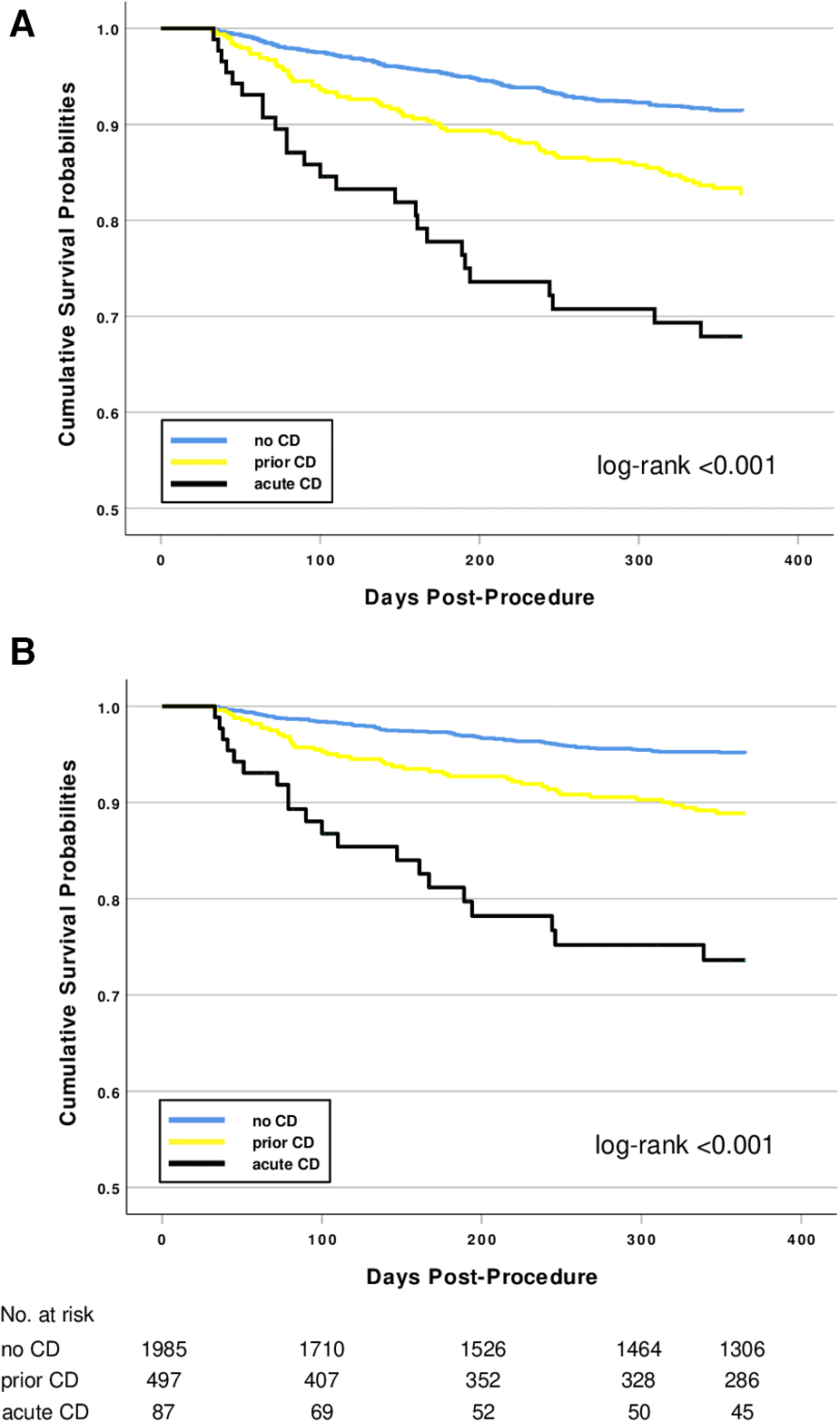
Kaplan–Meier survival curves after TAVI for patients with no, prior, or acute CD before hospital admission. (A) All-cause mortality. (B) Cardiovascular mortality.
Univariate predictors of one-year all-cause mortality in the overall study population included parameters of body physique (low BMI, low PMAi), cardiovascular diseases (diabetes mellitus, atrial fibrillation, peripheral arterial disease, EuroScore II), clinical parameters (highly symptomatic patients in NYHA class III and IV, a reduced general condition, prior or acute CD, fluid overload), echocardiographic parameters (low ejection fraction, low transvalvular gradients, mitral or tricuspid valve regurgitation), laboratory parameters (anemia, renal insufficiency), and the absence of prescribed discharge medication (ACEI/ARB and statins). A summary of the results of the univariate Cox regression analysis is given in Table 3.
Table 3
| Variable | HR | CI 95% | p | |
|---|---|---|---|---|
| Lower | Upper | |||
| Female | 0.960 | 0.746 | 1.235 | 0.751 |
| Age | 1.024 | 1.000 | 1.049 | 0.053 |
| BMI | 0.954 | 0.928 | 0.981 | 0.001 |
| COPD | 1.051 | 0.764 | 1.445 | 0.760 |
| Cardiovascular disease | ||||
| Arterial hypertension | 0.627 | 0.433 | 0.910 | 0.014 |
| Diabetes mellitus | 1.527 | 1.183 | 1.970 | 0.001 |
| CAD | 1.031 | 0.796 | 1.335 | 0.817 |
| Prior MI | 0.703 | 0.454 | 1.090 | 0.115 |
| Atrial fibrillation | 2.450 | 1.889 | 3.176 | <0.001 |
| Prior stroke | 1.176 | 0.825 | 1.675 | 0.371 |
| Peripheral artery disease | 1.567 | 1.120 | 2.192 | 0.009 |
| EuroScore II | 1.069 | 1.047 | 1.091 | <0.001 |
| ICD at discharge | 1.690 | 0.897 | 3.182 | 0.104 |
| Clinical data | ||||
| NYHA class III/IV | 1.875 | 1.305 | 2.695 | <0.001 |
| General condition (Steps 1–3) | ||||
|
– | – | – | – |
|
2.298 | 1.648 | 3.203 | <0.001 |
|
5.055 | 2.809 | 9.099 | <0.001 |
| Frailty | 1.262 | 0.977 | 1.631 | 0.075 |
| Cardiac decompensation | ||||
|
– | – | – | – |
|
2.102 | 1.585 | 2.788 | <0.001 |
|
4.525 | 2.960 | 6.917 | <0.001 |
| Moist rales | 2.192 | 1.414 | 3.398 | <0.001 |
| Peripheral oedema | 1.870 | 1.420 | 2.462 | <0.001 |
| Fluid overload | 2.534 | 1.950 | 3.293 | <0.001 |
| Laboratory Data | ||||
| GFR | 0.989 | .0985 | 0.994 | <0.001 |
| Anemia | 1.895 | 1.470 | 2.444 | <0.001 |
| Echocardiographic data | ||||
| Ejection fraction | 0.982 | 0.973 | 0.991 | <0.001 |
| Ejection fraction ≤40% | 2.089 | 1.492 | 2.924 | <0.001 |
| MPG <40 mmHg | 1.947 | 1.508 | 2.513 | <0.001 |
| Moderate MR or TR | 1.649 | 1.234 | 2.204 | <0.001 |
| CT data | ||||
| Pleural effusion | 2.909 | 2.211 | 3.826 | <0.001 |
| PMAi | 0.903 | 0.846 | 0.963 | 0.002 |
| PMAi tertiles (1–3) | 0.816 | 0.695 | 0.958 | 0.013 |
| Procedural data | ||||
| Balloon-expandable valve | 0.853 | 0.654 | 1.113 | 0.241 |
| Medication at hospital discharge | ||||
| ACEI/ARB | 0.542 | 0.414 | 0.710 | <0.001 |
| Beta-blockers | 1.423 | 1.032 | 1.961 | 0.031 |
| Mineralocorticoid antagonists | 1.273 | 0.935 | 1.734 | 0.126 |
| Statins | 0.626 | 0.484 | 0.810 | <0.001 |
Univariate Cox regression analysis with 1-year all-cause mortality as the outcome variable.
The following parameters emerged as independent predictors of one-year all-cause mortality in the multivariable analysis (Table 4): low BMI, diabetes mellitus, atrial fibrillation, a reduced general condition, prior or acute CD, fluid overload, anemia, a low-flow AS, and the lack of prescribed ACEI/ARB and of statins.
Table 4
| Variable | HR | CI 95% | p | |
|---|---|---|---|---|
| Lower | Upper | |||
| BMI | 0.951 | 0.923 | 0.979 | <0.001 |
| Diabetes mellitus | 1.434 | 1.074 | 1.014 | 0.015 |
| Atrial fibrillation | 1.756 | 1.322 | 2.334 | <0.001 |
| EuroScore II | 1.035 | 1.007 | 1.063 | 0.015 |
| General condition (Steps 1–3) | ||||
|
reference | – | – | – |
|
1.529 | 1.062 | 2.202 | 0.022 |
|
1.201 | 0.575 | 2.509 | 0.627 |
| Cardiac decompensation | ||||
|
reference | – | – | – |
|
1.396 | 1.023 | 1.906 | 0.036 |
|
1.715 | 1.011 | 2.911 | 0.046 |
| Fluid overload | 1.537 | 1.136 | 2.079 | 0.005 |
| Anemia | 1.432 | 1.088 | 1.886 | 0.010 |
| MPG <40 mmHg | 1.436 | 1.084 | 1.902 | 0.012 |
| ACEI/ARB | 0.597 | 0.445 | 0.799 | <0.001 |
| Statins | 0.659 | 0.498 | 0.872 | 0.003 |
Multivariate Cox regression analysis with 1-year all-cause mortality as the outcome variable.
HR, hazard ratio; CI, confidence interval; BMI, body mass index; MPG, mean pressure gradient; ACEI/ARB, angiotensin converting enzyme inhibitors or angiotensin receptor blocker.
Figure 2 illustrates the effect of prescribed ACEI/ARB medication on the hazards of one-year mortality on patients of all three CD classes. ACEI/ARB were associated with a reduction of mortality by around one third, and this effect was consistent throughout all three CD classes.
Figure 2
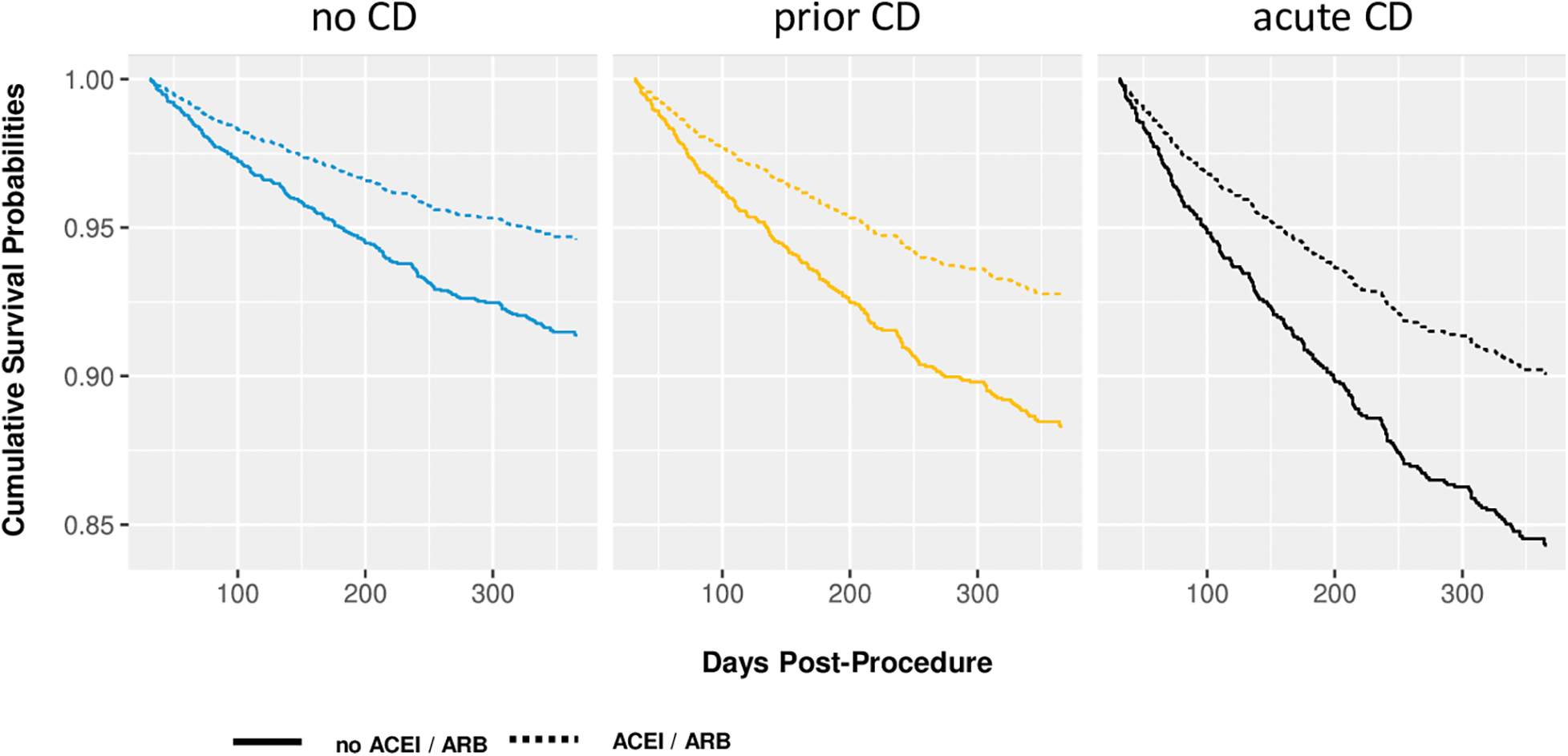
Adjusted survival curves illustrating the effect of both a history of cardiac decompensation and the effects of ACEI/ARB on one-year mortality. Predictions of the multivariate Cox proportional hazard model for prototypical values: BMI = 27.7 kg/m2, diabetes, atrial fibrillation, Euroscore II = 4.14%, reduced general condition, no fluid overload, no anemia, MPG >40 mmHg, statins.
We finally analyzed patients with an EF ≤40% (n = 323) and those with an EF ≥50% (n = 2,121) in analogy to patients with heart failure with reduced or preserved EF, respectively (Table 5). Both groups revealed a significant increase in mortality rates from patients without CD over those with a prior to those with an acute CD. In patients with an EF ≤40%, prescribed ACEI/ARB therapy was associated with a numerically 50% reduction of mortality rates in patients with a prior and in those with an acute CD, however due to small patient numbers, the significance level was not achieved. In patients with an EF ≥50%, ACEI/ARB was associated with a significant survival benefit in patients with a prior CD while no effect could be observed in those patients with an acute CD.
Table 5
| Class of CD | ACEI/ARB | EF ≤40% | log-rank | EF ≥50% | log-rank |
|---|---|---|---|---|---|
| n = 323 | n = 2,121 | ||||
| no CD | 16/178 (9.0) | <0.001 | 124/1,720 (7.2) | <0.001 | |
| prior CD | 21/108 (19.4) | 45/355 (12.7) | |||
| acute CD | 13/37 (35.1) | 10/46 (21.7) | |||
| prior CD | yes | 13/82 (15.9) | 0.088 | 27/267 (10.1) | 0.010 |
| no | 8/26 (30.8) | 18/87 (20.7) | |||
| acute CD | yes | 7/26 (26.9) | 0.087 | 6/28 (21.4) | 0.879 |
| no | 6/11 (54.5) | 4/18 (22.2) |
All-cause one-year mortality rates of patients with EF ≤40% vs. EF ≥50% .
Data shown as number (%). ACEI/ARB, angiotensin converting enzyme inhibitors/angiogtensin receptor antagonists; CD, cardiac decompensation.
Discussion
The classification of this all-comers population of patients with severe AS into those with no, prior, or acute CD and the thorough evaluation of signs of cardiac congestion and evaluation of their prognostic impact may lead to a better understanding of the prevalence and clinical manifestation of concomitant HF in patients with AS. While almost 90% of all patients presenting with acute CD had documented cardiac congestion, fluid overload was also manifest in more than 50% of the patients with prior CD and even in more than 25% of those patients with no reported CD, suggesting the presence of manifest or subclinical HF among the whole spectrum of patients with AS referred for TAVI.
We chose to include only patients fulfilling the criteria of 30-day device success, because we explicitly wanted to exclude the impact of procedural and technical aspects of TAVI that could influence further results, thereby attempting to investigate outcomes and the effect of the prescribed medication in apparently stable patients after successful TAVI. Our model allowed for a stepwise comparison of patient cohorts with increasing intensity of signs and symptoms of cardiac congestion, and it is intriguing to observe similarities to those of classic HF patients. Indeed, the loss of left ventricular systolic function as reflected by a reduction of ejection fraction and an increase in the frequency of low-gradient aortic stenosis, alongside with a higher prevalence of atrio-ventricular valve dysfunction, a functional decline of other organ systems manifested by a reduced renal function and anemia, and a clear accumulation of extravascular fluid in different body compartments are clearly compatible with signs of HF. However, even when our data suggest at first the presence of HF with reduced EF as the main origin of CD, more detailed analysis of our data revealed that CD-related mortality rates are similar in patients with reduced and preserved EF. This observation allows to conclude that mechanisms described in patients with HF with preserved EF are present in our patient population and that a part of those with an EF ≥50% might bear the (most probably masked) diagnosis of HF with preserved EF. Sarcopenia, though common in older patients, is a characteristic of patients with HF with a prevalence of around 34% (9), contributes to exercise intolerance and ventilatory inefficiency, and is associated with longer hospitalizations and worsened prognosis in these patients (10). Although we did not measure functional parameters of sarcopenia, it is interesting to observe an increased percentage of patients in the sex-specific lowest range of PMAi in the patient groups with prior and acute CD, which appears to be similar to patients with HF. Accordingly, more patients with prior or acute CD presented in a poor general clinical condition. Interestingly, each of the individual signs of volume overload (moist pulmonary rales, peripheral edema, pleural effusion) emerged as a strong univariate predictor of prognosis, and any fluid overload proved to be an independent prognostic indicator of one-year mortality.
Fluid overload, interpreted as residual clinical congestion, could be part of a pathophysiologic model that would explain the rather high mortality in the intermediate group of patients with prior CD. Of almost 8,000 patients with acute HF included in the ESC-EORP-HFA Heart Failure Long-Term Registry (11), 31% of those discharged alive from hospital still had signs of residual congestion, which is in line with the results of other studies (12), all of which demonstrated the strong negative predictive value of residual fluid overload in re-compensated HF patients for future re-hospitalizations or death (13). It seems plausible to decode the presence of fluid overload in patients with prior CD as a remnant of incomplete recompensation or subclinically manifested HF, presenting only the end results of fundamentally and persistently disrupted hemodynamics that obviously affect outcomes even after TAVI. Indeed, once symptomatic patients are diagnosed with severe AS, the aim of clinical management is for symptom improvement and improvement of prognosis; however, once the AS has been corrected by TAVI and symptoms have improved, the complete recompensation of patients might not be documented, and one could speculate that patients still have a lingering degree of cardiac congestion that is associated with higher rehospitalization rates and worse outcomes. Our analysis revealed that the shorter the timespan between CD and TAVI was, the more fluid overload in those patients was present, which could have translated into higher mortality rates in these patients with a very recent CD. However, no significant impact of the timespan on mortality could be observed. We speculate that this lacking relationship might be due to the different levels of cardiac recompensation that could be achieved during the hospital stay. Unfortunately, we cannot provide data on fluid overload at the timepoint of hospital discharge, information that might have contributed to a further understanding of the clinical status of HF in these patients.
From a clinical point of view, our results are consistent with the concept of an early treatment of patients with left ventricular dysfunction, even for those with a less-than-severe degree of aortic stenosis (14). The idea of this concept is that an early unloading of the left ventricle in these patients might avoid further deterioration of left ventricular function and avoid cardiac decompensations, a concept that is currently being tested in a multicenter study (15). In fact, one could conclude that an early treatment, most likely consisting of aortic valve replacement, should be initiated before signs of cardiac congestion are manifest.
The beneficial effect of targeted medication at hospital discharge has already been demonstrated for ACEI/ARB (8, 16) and statins (17) and demonstrates parallels to the effect in patients with HF. It is interesting to note that the ACEI/ARB regimen might be effective not only in stable patients without any prior CD but also in those with prior CD and even in those hospitalized for acute CD. Given the similarities to patients with HF with reduced EF, it is not surprising to see substantial effects of ACEI/ARB in these patients. However, it is interesting to note that significant effects of ACEI/ARB prescription could be observed in patients with probably masked HF with preserved EF who suffered a previous CD, even more because this medication has not been proven to be effective in this condition. Obviously additional/complementary pathophysiological mechanisms should play a role in patients with AS that make those patients amenable for the beneficial effects of ACEI/ARB.
Given that these results might hold true in prospective and controlled trials, such a therapy might comprise a potential treatment to deal with the excess mortality observed in patients with AS and HF after TAVI.
One limitation of this retrospective analysis may be the lack of a systemic, serial documentation of left ventricular function and fluid status during follow-up. Moreover, the knowledge of natriuretic peptide levels could have given important insights into myocardial wall stress. Regarding the prescribed medication of our patients, we cannot comment on true compliance during the observational period, and the prescribing of ACEI/ARB might have reflected a better overall clinical condition of those patients, translating into a better outcome per se.
Taken together, the results of our study help to better understand the clinical condition of patients with AS, in particular of those with or without a history of CD. In parallel to patients with HF, those patients of our registry with documented fluid overload had a worse prognosis compared with those without. The classification into acute, prior, or no CD additionally determined prognosis. These results may contribute to the discussion about an early treatment strategy in patients with AS and left ventricular dysfunction. Moreover, medical treatment post-TAVI might be a crucial part of the postinterventional treatment.
Statements
Data availability statement
The datasets presented in this article are not readily available because according to local restrictions no patient data, even anonymized, can be shared with other people outside our institution. Requests to access the datasets should be directed to www.kerckhoff-klinik.de.
Ethics statement
The studies involving humans were approved by the ethics committee of the University of Giessen. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin due to the retrospective nature of this study, a waiver of written informed consent was issued by the local ethics committee (University of Giessen), which approved the study protocol.
Author contributions
Conception and design of the work: UF-R, MS and W-KK Substantial contribution to the acquisition of data: MR, MS, JT, W-KK and EC. Substatial contribution to the analysis of data: UF-R, EC, AR and MW. Substatial contribution to the interpretation of data: AR, MW, Y-HC, CH and W-KK. Drafting the work: UF-R and EC. Revising the draft and important intellectual content: MR, EC, AR, MW, Y-HC, CH and W-KK. All authors contributed to the article and approved the submitted version.
Conflict of interest
UF-R: none. EC: proctor fees from Boston Scientific. MR: speaker fees from St. Jude Medical/Abbott. CS: none. JT: none. AR: none. MW: speaker fees from Boston Scientific. Y-HC: proctor/speaker/scientific advisor fees from Getinge, Jotec/CryoLife, Cytosorbents. CH: advisory board Medtronic. W-KK: proctor/speaker fees from Abbott, Boston Scientific, Edwards Lifesciences, Medtronic, Meril Life Sciences, Shockwave Medical.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Chen S Redfors B Crowley A Ben-Yehuda O Summers M Hahn RT et al Impact of recent heart failure hospitalization on clinical outcomes in patients with severe aortic stenosis undergoing transcatheter aortic valve replacement: an analysis from the PARTNER 2 trial and registries. Eur J Heart Fail. (2020) 22(10):1866–74. 10.1002/ejhf.1841
2.
Schmidt T Bohne M Schluter M Kitamura M Wohlmuth P Schewel D et al The impact of biventricular heart failure on outcomes after transcatheter aortic valve implantation. Clin Res Cardiol. (2019) 108(7):741–8. 10.1007/s00392-018-1400-6
3.
Nagao K Taniguchi T Morimoto T Shiomi H Ando K Kanamori N et al Acute heart failure in patients with severe aortic stenosis - insights from the CURRENT AS registry. Circ J. (2018) 82(3):874–85. 10.1253/circj.CJ-17-0610
4.
Jalava MP Laakso T Virtanen M Niemela M Ahvenvaara T Tauriainen T et al Transcatheter and surgical aortic valve replacement in patients with recent acute heart failure. Ann Thorac Surg. (2020) 109(1):110–7. 10.1016/j.athoracsur.2019.05.044
5.
Fischer-Rasokat U Renker M Liebetrau C Weferling M Rieth A Rolf A et al Predictive value of overt and non-overt volume overload in patients with high- or low-gradient aortic stenosis undergoing transcatheter aortic valve implantation. Cardiovasc Diagn Ther. (2021) 11(5):1080–92. 10.21037/cdt-21-286
6.
Patel KP Mukhopadhyay S Bedford K Richards R Queenan H Jerrum M et al Rapid assessment and treatment in decompensated aortic stenosis (ASTRID-AS study)- A pilot study. Eur Heart J Qual Care Clin Outcomes. (2022) 15:qcac074. 10.1093/ehjqcco/qcac074 [Epub ahead of print].
7.
Généreux P Piazza N Alu MC Nazif T Hahn RT Pibarot P et al Valve academic research consortium 3: updated endpoint definitions for aortic valve clinical research. Eur Heart J. (2021) 42(19):1825–57. 10.1093/eurheartj/ehaa799
8.
Fischer-Rasokat U Bansch C Renker M Rolf A Charitos EI Weferling M et al Effects of renin-angiotensin system inhibitor type and dosage on survival after transcatheter aortic valve implantation. Eur Heart J Cardiovasc Pharmacother. (2022) 8(8):815–24. 10.1093/ehjcvp/pvac027
9.
Zhang Y Zhang J Ni W Yuan X Zhang H Li P et al Sarcopenia in heart failure: a systematic review and meta-analysis. ESC Heart Fail. (2021) 8(2):1007–17. 10.1002/ehf2.13255
10.
Lena A Anker MS Springer J . Muscle wasting and sarcopenia in heart failure-the current state of science. Int J Mol Sci. (2020) 21(18):6549. 10.3390/ijms21186549
11.
Chioncel O Mebazaa A Maggioni AP Harjola VP Rosano G Laroche C et al Acute heart failure congestion and perfusion status - impact of the clinical classification on in-hospital and long-term outcomes; insights from the ESC-EORP-HFA heart failure long-term registry. Eur J Heart Fail. (2019) 21(11):1338–52. 10.1002/ejhf.1492
12.
Pugliese NR Mazzola M Bandini G Barbieri G Spinelli S De Biase N et al Prognostic role of sonographic decongestion in patients with acute heart failure with reduced and preserved ejection fraction: a multicentre study. J Clin Med. (2023) 12(3):773. 10.3390/jcm12030773
13.
Rubio-Gracia J Demissei BG Ter Maaten JM Cleland JG O'Connor CM Metra M et al Prevalence, predictors and clinical outcome of residual congestion in acute decompensated heart failure. Int J Cardiol. (2018) 258:185–91. 10.1016/j.ijcard.2018.01.067
14.
Samad Z Vora AN Dunning A Schulte PJ Shaw LK Al-Enezi F et al Aortic valve surgery and survival in patients with moderate or severe aortic stenosis and left ventricular dysfunction. Eur Heart J. (2016) 37(28):2276–86. 10.1093/eurheartj/ehv701
15.
Spitzer E Van Mieghem NM Pibarot P Hahn RT Kodali S Maurer MS et al Rationale and design of the transcatheter aortic valve replacement to UNload the left ventricle in patients with ADvanced heart failure (TAVR UNLOAD) trial. Am Heart J. (2016) 182:80–8. 10.1016/j.ahj.2016.08.009
16.
Wang S Lin X Guan Y Huang J . The clinical outcomes of reni-angiotensin system inhibitors for patients after transcatheter aortic valve replacement: a systematic review and meta-analysis. Front Cardiovasc Med. (2022) 9:963731. 10.3389/fcvm.2022.963731
17.
Fischer-Rasokat U Renker M Bansch C Weferling M Liebetrau C Herrmann E et al Effects of statins after transcatheter aortic valve implantation in key patient populations. J Cardiovasc Pharmacol. (2021) 78(5):e669–e74. 10.1097/FJC.0000000000001114
Summary
Keywords
transcatheter aortic valve implantation (TAVI), aortic stenosis, heart failure, cardiac decompensation, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, prognosis
Citation
Fischer-Rasokat U, Renker M, Charitos EI, Strunk C, Treiber J, Rolf A, Weferling M, Choi Y-H, Hamm CW and Kim W-K (2023) Cardiac decompensation of patients before transcatheter aortic valve implantation—clinical presentation, responsiveness to associated medication, and prognosis. Front. Cardiovasc. Med. 10:1232054. doi: 10.3389/fcvm.2023.1232054
Received
31 May 2023
Accepted
10 October 2023
Published
23 October 2023
Volume
10 - 2023
Edited by
Hendrik Tevaearai Stahel, University Hospital of Bern, Switzerland
Reviewed by
Fabio Lima, University of California, San Francisco, United States Marcel Weber, University Hospital Bonn, Germany
Updates
Copyright
© 2023 Fischer-Rasokat, Renker, Charitos, Strunk, Treiber, Rolf, Weferling, Choi, Hamm and Kim.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Ulrich Fischer-Rasokat fischer-rasokat@gmx.de
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.