
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 03 November 2023
Sec. Heart Valve Disease
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1228258
This article is part of the Research Topic Individualized Treatment of Mitral and Aortic Valve Disease View all 8 articles
 Yunfeng Yan†
Yunfeng Yan† Jing Yao†
Jing Yao† Fei Yuan
Fei Yuan Xinmin Liu
Xinmin Liu Taiyang Luo
Taiyang Luo Zhinan Lu
Zhinan Lu Sanshuai Chang
Sanshuai Chang Qian Zhang
Qian Zhang Ran Liu
Ran Liu Chengqian Yin
Chengqian Yin Guangyuan Song*
Guangyuan Song*
Background: Transcatheter aortic valve replacement (TAVR) potentially may be significantly simplified by using the single artery access (SA) technique, which does not require a secondary artery access. Nevertheless, the safety and efficacy of this technique remains unclear. Our goal was to determine if single artery access TAVR (without upgrading the sheath size) is a feasible, minimally invasive procedure.
Methods: Patients with symptomatic severe aortic stenosis who underwent TAVR via the femoral artery were consecutively enrolled in this study. Eligible individuals were divided into 2 groups: the SA group and the dual artery access (DA) group. The primary end point was device success (defined by the valve academic research consortium 3, VARC 3). A 6-month follow-up and propensity score matching analyses were performed.
Results: After propensity score matching analysis, a total of 130 patients were included: 65 in the SA group and 65 in the DA group. The SA procedure achieved similar device success (95.4% vs. 87.7%; P = 0.115) compared with the DA procedure. The SA procedure shortened the operating time (102 min vs. 125 min; P = 0.001) but did not increase the x-ray time or dose. Both a 20 Fr and a 22 Fr sheath (without upgrading the sheath size) could be used for the SA procedure. There was no major vascular complication occurred in both groups. The incidence of minor main vascular and access complications in the SA group was comparable to those of the DA procedure (0.0% vs. 3.1%; P = 0.156).
Conclusions: The SA access procedure is a promising minimally invasive TAVR technique with a low incidence of vascular complications and a high incidence of device success. It is safe and possibly applicable in all TAVR procedures.
Since the first aortic valve prosthesis percutaneously implanted in 2002 (1), the evolution of transcatheter aortic valve replacement (TAVR) has been astonishing. Currently, TAVR is recommended for treating symptomatic severe aortic stenosis (AS) regardless of the surgical risk (2–4). The feasibility of a simplified TAVR has been explored extensively and is regarded as another revolution in the development of this technique (5).
As major vascular complications of approximately 10% are reported from current all-comers cohorts (6, 7), improvements in vascular access are required to improve the outcome of TAVR. In contrast to the fact that the transfemoral approach is recommended as the first choice for primary access (3, 8), the choice of secondary access is widely debated. Conventionally, the contralateral femoral artery has been the first choice. However, as many as 25% of all vascular/access complications are associated with a transfemoral secondary access (9, 10). A radial artery access can be applied and has been proven to be a useful alternative that results in fewer complications (9, 11, 12). Previous studies have also proven the safety of the unilateral femoral access (13). However, secondary access complications still occurred.
Previous studies have explored the possibility of eliminating secondary access. Some researchers compared the effects of puncturing only 1 femoral artery as the primary access with the effects of conventional dual artery (DA) access and reported promising results (14). However, they used aortic root calcifications as landmarks to avoid the use of angiography, which requires rigorous patient selection and is rarely used. Other researchers who conducted a 1-arm study reported that they placed both the delivery system and the pigtail into the sheath, thereby achieving promising outcomes (15).
In the present study, we analyzed our modified TAVR process with a single femoral artery puncture and assessed whether this technique was safer and more effective than the DA procedure.
This trial was an all-comer, single-center, retrospective cohort study that was performed at the Beijing Anzhen Hospital between June 2021 and September 2022. The protocol was approved by the clinical research ethics committee of Beijing AnZhen Hospital (No.: 2021008X). An adjudication board blinded to the patient groups was responsible for enrollment, judgment about end points, quality control, and other related issues.
All individuals with symptomatic severe AS who had TAVR via the femoral artery were consecutively enrolled in this study. The inclusion criteria comprised (1) patients with severe AS; (2) patients with symptoms associated with AS: dyspnea related to heart failure (New York Heart Association Functional class ≥II), angina, syncope/presyncope, and others; (3) aortic root anatomy that was suitable for TAVR that was assessed by contrast-enhanced multidetector computerized tomography; (4) patients ≥60 years old (4); and (5) suitable iliofemoral access diameter assessed by contrast-enhanced multidetector computerized tomography.
The exclusion criteria included (1) a myocardial infarction within ≤1 month; (2) hypertrophic cardiomyopathy with obstruction; (3) evidence of an intracardiac mass, thrombus, or vegetation; (4) inability to tolerate antithrombotic/anticoagulation therapy; (5) evidence of septicemia or endocarditis; (6) life expectancy <12 months; (7) significant aortic or other diseases requiring surgical intervention: aortic dissection, aortic aneurysm (especially if >5 cm); (8) the use of a sheath or a transcatheter heart valve (THV) delivery system did not permit the insertion of 2 instruments [for example, an e-sheath (Edwards Lifesciences, Irvine, CA, USA)].
Based on the SA technology applied, eligible patients were assigned to 1 of 2 groups: the SA group or the conventional DA group. That is: patients were assigned to different groups according to their final treatment strategy.
The key point of the SA procedure is to avoid using a secondary artery (without upgrading the sheath size). A brief description of the SA procedure is provided below (Figure 1):
1. Establish femoral access: perform an ultrasound-guided precision puncture, preset 2 Perclose ProGlide devices (Abbott Laboratory, Chicago, IL, USA), and insert the sheath.
2. Aortogram: insert a pigtail catheter into the aortic root for the aortogram.
3. Balloon predilation: After predilating the balloon, remove the pigtail catheter.
4. Delivery of the THV: (i) Insert the THV delivery system into the descending aorta; (ii) insert the pigtail catheter from the single femoral access point to the bottom of aortic root; and (iii) deliver the THV to the aortic root.
5. Deployment of the THV: Using the pigtail catheter and the aortogram as guides, release the THV.
6. Removal of the sheath and suturing: Inject the contrast agent slowly while removing the sheath to detect potential vascular injury. Use 2 Perclose ProGlide devices to lock the puncture orifice.
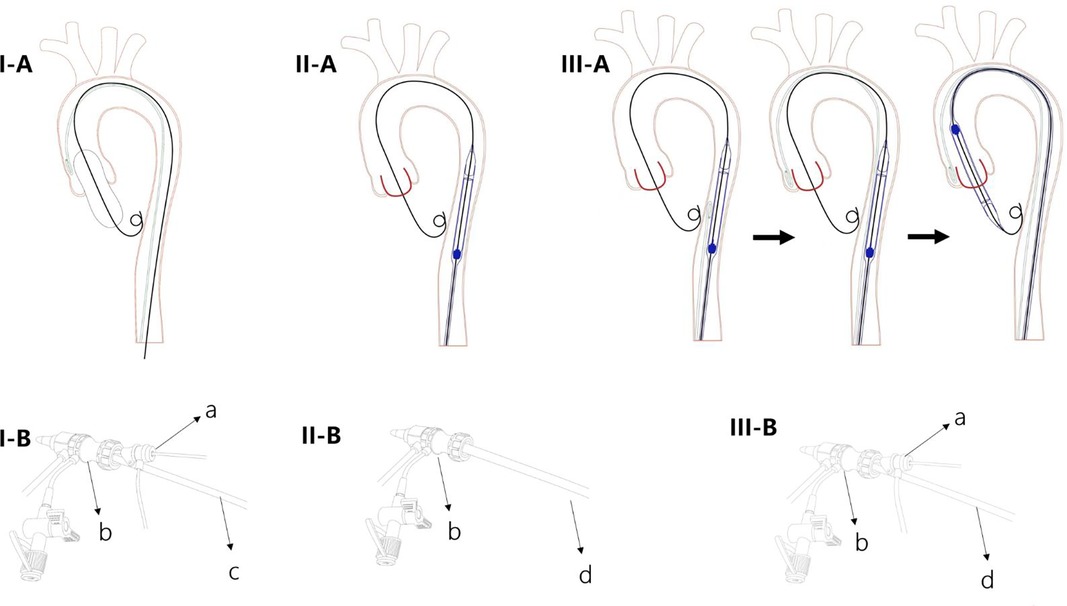
Figure 1. Diagram of the single artery access technique. I (A,B) A 5 Fr pigtail catheter is inserted into the aortic root for an aortogram with the 5 Fr sheath inside the large sheath; balloon dilation occurs through the same sheath. II (A,B) After the 5 Fr pigtail and the balloon are removed, the transcatheter heart valve (THV) delivery system is inserted into the descending aorta. III (A,B) The pigtail catheter is inserted from the single femoral access up to the bottom of the aortic root; then the THV is delivered to the aortic root. (a) A 5F sheath with pigtail catheter; (b) large sheath; (c) balloon; (d) THV delivery system.
It should also be noted that rapid cardiac pacing is performed through either the left ventricular wire or a preinstalled temporary pacemaker wire via the femoral vein.
Traditionally, two arteries are punctured: the primary access used for valve delivery and the secondary access for aortic root aortogram. That is the DA access procedural.
The following data were extracted from the hospital information system by trained researchers: baseline clinical history (such as: age, sex, hypertension, and dyslipidemia), examination and laboratory information, medical information, and data on endpoints.
Severe AS was defined according to transthoracic echocardiographic results: (1) jet velocity ≥400 cm/s or mean gradient ≥40 mmHg; and/or (2) aortic valve area ≤1.0 cm2 or aortic valve area index ≤0.6 cm2/m2 (2–4).
The primary end point was device success, which was defined according to the Valve Academic Research Consortium 3 (VARC−3) criteria: a composite of technical success, freedom from mortality, freedom from surgery or intervention related to the device/ complications, and intended performance of the valve during 30 days follow-up (16). Secondary end points included death; cardiac death; major main vascular/access-related complications; minor vascular/access-related complications; major secondary vascular/access-related complications; minor secondary vascular/access-related complications; myocardial infarction; acute kidney injury; moderate/severe paravalvular regurgitation; new permanent pacemaker; new left bundle branch block; rehospitalization; and disabling stroke.
The following procedural data were also extracted: operating time, x-ray time, x-ray dose, concurrent percutaneous transluminal coronary intervention, valve-in-valve implant, sheath size, and bioprosthetic valve type. The definition of operating duration was the time from the introduction of anesthesia until the patient left the operating room. x-ray time and dose were collected directly by a digital subtraction angiography device.
The follow-up procedures were performed by trained researchers who were blinded to the patients’ groups. Data were collected at 1 month and 6 months during clinical visits and by phone calls and the We-chat application.
The continuous variables with normal distributions were presented as the means ± standard deviations and were compared using the Student t-test or the analysis of variance test. Those variables without normal distributions were presented as medians with interquartile ranges, and differences between the groups were analyzed using the Mann–Whitney U-test or the Kruskal–Wallis test. The categorical data were presented as numbers and percentages and were compared using the χ2 test or the Fisher exact test, where applicable.
All end points were presented as numbers and percentages and were analyzed by using the χ2 test or the Fisher exact test, where applicable.
To balance selection biases and other confounding items, a propensity score matched analysis was performed, based on the patients’ baseline characteristics, which are listed in Table 1. We completed a nonparsimonious model. Patients were matched 1:1 using a nearest-neighbor algorithm, with a caliper of 0.05. The absolute standardized differences were used to evaluate the imbalance of each variable. The propensity score matched baseline characteristics of the patients were then compared again using the Student t-test, a Wilcoxon rank-sum test, a χ2 test, or the Fisher exact test, where applicable. The end points of the propensity score matched population were analyzed using the χ2 test or the Fisher exact text, where applicable.
All analyses were performed using SPSS 24.0 (SPSS Inc., Chicago, IL, USA) and Stata 14.0 (Stata, College Station, TX, USA). A two-tailed p-value ≤ 0.05 was considered statistically significant.
From June 2021 to September 2022, a total of 213 patients with severe AS were consecutively enrolled in the present study (Figure 2). Of these patients, 113 (53.05%) were treated by SA (the SA group), and 100 (46.95%) were treated by conventional DA (the DA group).
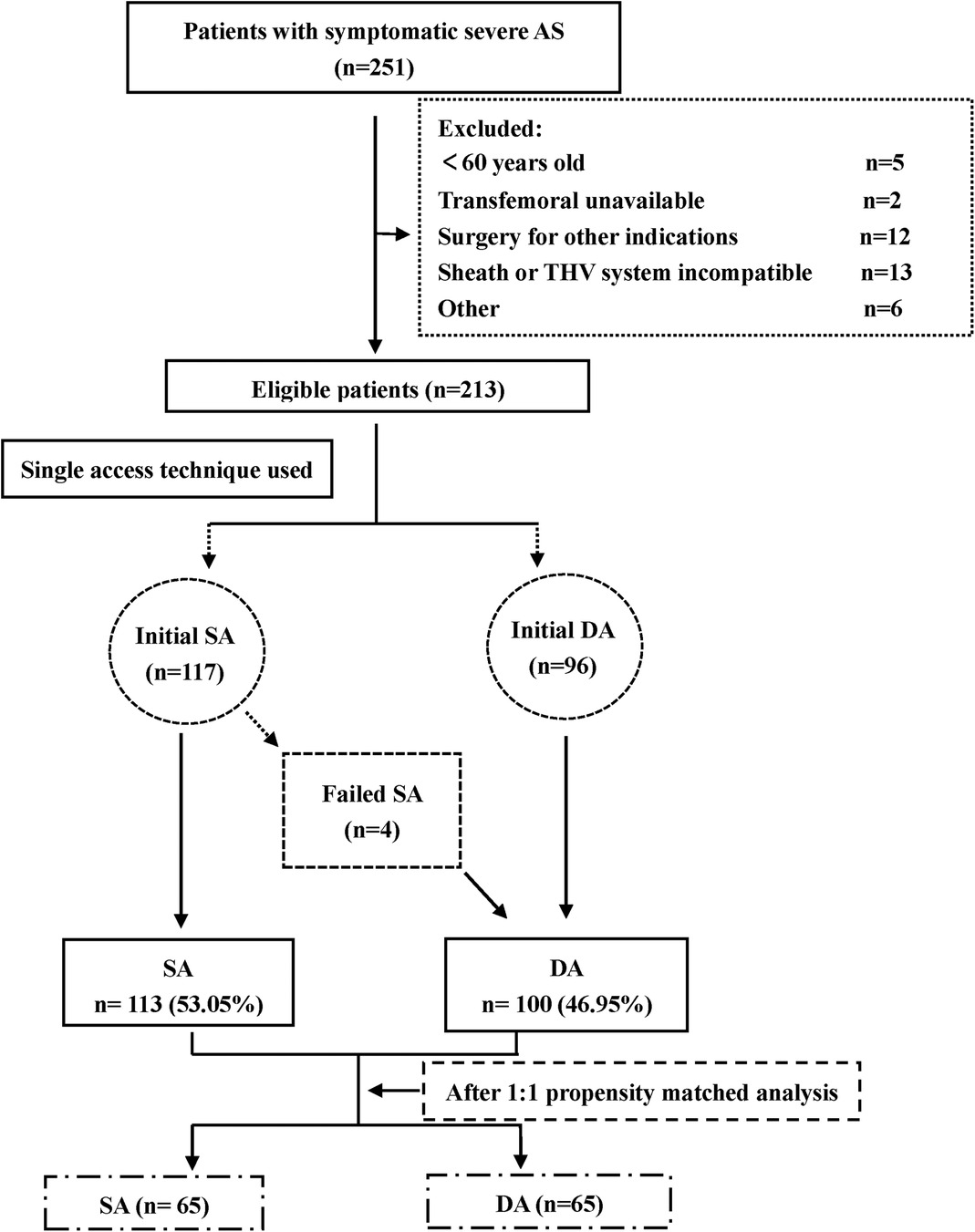
Figure 2. Flow chart. AS, aortic stenosis; DA, dual artery access; SA, single artery access; THV, transcatheter heart valve.
The baseline clinical, ultrasound cardiographic, and contrast-enhanced multidetector computerized tomography characteristics are listed in Table 1. To reiterate, patients who were treated with SA had a higher prevalence of right bundle branch block and a lower prevalence of prior stroke compared with the DA group. The perimeters of the annulus and the areas in patients with SA were statistically smaller. No significant differences existed between the groups for the other variables.
After a 1:1 propensity matched analysis, 65 individuals were included in each group. The absolute standard differences after the matching were all less than 10.0% (Figure 3) except for the body surface area (BSA), body mass index (BMI) and aortic valve calcification (HU850), which showing a good matching balance. None of the baseline items showed statistical differences (Table 1).
Procedural outcomes are listed in Table 2. In summary, the end points for x-ray time and x-ray dose for patients in the SA group were comparable to those in the DA group, as were the end points of concurrent PCI, sheath usage, bioprosthetic valve type, sheath to femoral artery ratio (SFAR) and valve-in-valve implants. The operating times for the DA group were longer than those for the SA group (102 min vs. 125 min; P = 0.001).
Table 3 lists all clinical outcomes. Device success was observed in 119 individuals: 62 (95.4%) in the SA group and 57 (87.7%) in the DA group. Although the SA procedure was superior numerically, there were no statistical differences between the groups (P = 0.115). As to the secondary clinical end points—death; cardiac death; myocardial infarction; new permanent pacemaker and disabling stroke—those in the SA group were comparable to those in the DA group, both perioperatively and at the 1-month and 6-month follow-up examinations. There were also no statistical differences in the end points of acute kidney injury and new left bundle branch block when analyzed perioperatively. Moderate/severe paravalvular regurgitation results were also comparable between groups both perioperatively and at the 1-month follow-up, as were rehospitalizations at both the 1-month and the 6-month follow-up examinations.
Only two vascular/access complications occurred. All those complications were in the DA group and minor main vascular/access events. There was no statistical significance between groups (0.0% vs. 3.1%, P = 0.156) (Table 3).
We analyzed a modified minimally invasive TAVR procedure in which only one artery was punctured (without upgrading the sheath size). To the best of our knowledge, this is a most innovative attempt. After comparing the outcomes of our procedure with those of the DA procedure and applying the method of propensity matched analysis, our main findings are as follows: (1) The SA procedure achieved similar device success compared with the DA procedure. (2) The SA procedure shortened the operating time and did not increase the x-ray time or dose. (3) The 20 Fr and 22 Fr sheaths could be used for the SA procedure with a low incidence of vascular/access complications that was comparable to the results achieved with the DA procedure.
Previous studies have contributed useful suggestions for simplifying the TAVR approach. Secondary access was the primary focus. The radial artery was a reasonable alternative. Curran and colleagues enrolled 87 patients (11) and by comparing the radial artery access with the collateral femoral access, they proved the safety and efficiency of the radial access (major vascular complication: 4.3% vs. 7.3%, P = 0.553). Other researchers reported similar results (9, 17, 18). Khubber and colleagues reported their experience with the unilateral access technique (13). They punctured both the main and secondary access points in the same femoral artery. A significant decline (6.3%) in the incidence of vascular complications was observed after they applied the unilateral access technique. However, vascular complications related to secondary access still occurred. Gianluca and colleagues published a case report in which they did not mark a secondary access point (19). With the help of visible aortic root calcification, a prosthetic aortic valve was successfully implanted. Nicholas and colleagues also reported an analysis of such SA techniques (14). A total of 100 patients were enrolled consecutively. When compared with conventional DA, the SA technique showed a high incidence of technical success (100% vs. 100%, P = 1.000) and a low incidence of complications. However, they used anatomical calcification as a landmark to obviate the need for a secondary access. This SA technique requires a rigorous protocol for patient selection and is difficult to extrapolate to all patients with AS. Stefan and colleagues shared their experience with a modified SA TAVR procedure (15): By placing both the delivery system and the pigtail into the sheath, they achieved promising procedural and clinical outcomes. However, they reported only the results of a single arm study and did not compare their results with those from the DA procedure. We reported our experience with a modified SA procedure. When we compared the results of the modified SA procedure with those of the DA procedure, we found that the SA procedure achieved similar device success. The operating time was shorter. At the same time, it did not increase the x-ray time or dose. We believe that such an SA technique is promising and can be extrapolated to all TAVR procedures. Larger randomized controlled trials are needed to further prove the safety and efficiency of the SA technique.
The incidence of major/minor vascular/access-related complications in this study was low. Previous studies and all-comer cohort studies reported a vascular complication incidence of approximately 10%-20% (6, 20–22). More recent reports (mainly RCTs) have shown an incidence of 4% or less (23–26). Possible explanations for these results are as follows: (1) Real-time ultrasound-guided needle puncture helps interventionists clearly distinguish calcifications, the anterior wall of an artery, the branch artery, and the vein. Previous studies have proven that, compared to fluoroscopy guidance and anatomical landmark guidance, ultrasound guidance during femoral catheterization can significantly reduce the incidence of access-related complications (27–29). In our centre, when we evaluated an approach using contrast-enhanced multidetector computerized tomography, the distance between the femoral bifurcation and the ideal femoral artery puncture site was premeasured. Thus, interventionists were more likely to achieve a precise puncture, which might help keep vascular complications to a minimum. (2) We performed a diligent preprocedural evaluation of the vascular access. (3) We used a percutaneous closure device. In the present study, two ProGlide closure devices were used to suture the artery. The haemostatic efficiency of this technique has been reported by previous researchers (30, 31). (4) We had a small sample of only 213 patients. The small sample size might also explain the lower incidence.
We reported herein our modification of the SA technique. Some key techniques should be highlighted: (1) As described previously, ultrasound-guided puncture contributed to a decrease in the incidence of vascular complications. (2) The entry and exit of the 5 Fr pigtail catheter should be repeated to ensure the trafficability of the devices. (3) We introduced another new technique in which contrast agent was slowly injected while the sheath was removed to avoid causing a vascular injury. Traditionally, angiography was performed from the secondary approach to detect the potential for vascular injury even though, to our knowledge, this manual injection technique is safe and efficient. Further studies are needed to prove this hypothesis.
The present study has some limitations: (1) Because the sample size is small, it is difficult to draw definitive conclusions. Further studies with a large sample are needed to verify the feasibility of the modified SA technique. (2) Some sheath or THV delivery systems could not be used to perform the SA technique. The construction of the e-sheath (Edwards Lifesciences) did not permit the insertion of 2 instruments. Thus, the SAPIEN (Edwards Lifesciences) valves were excluded from the present study. Further studies are needed to confirm that the SAPIEN is suitable for the modified SA technique. This study was a single-center, retrospective study, although we did perform propensity score matched analyses. Our evidence grade was indeed lower than that of multicenter randomized controlled trials. (4) Patients with aortic regurgitation were not enrolled in the present study.
The SA procedure is a promising minimally invasive TAVR technique with a low incidence of vascular complications and a high incidence of device success. Such an innovative technique is safe and might be suitable for application in all TAVR procedures.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The protocol was approved by the clinical research ethics committee of Beijing AnZhen Hospital (No.: 2021008X). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because This trial was an retrospective study.
Designed the studies: GS, YY and JY Performed the studies: JY, YY, FY, XL, RL and TL Analyzed the data: YY, ZL, SC, CY and QZ Drafted the manuscript: YY and JY Revised the manuscript: all authors. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cribier A, Eltchaninoff H, Bash A, Borenstein N, Tron C, Bauer F, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation. (2002) 106:3006–8. doi: 10.1161/01.cir.0000047200.36165.b8
2. Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. J Am Coll Cardiol. (2021) 77:e25–e197. doi: 10.1016/j.jacc.2020.11.018
3. Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. ESC/EACTS scientific document group. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. (2022) 43:561–632. doi: 10.1093/eurheartj/ehab395
4. Structural cardiology committee of cardiovascular physicians branch, Chinese medical doctor association, expert consensus on clinical pathway for transcatheter aortic valve replacement in China. Chinese J Interventional Cardiol. (2022) 30:7–16.
5. Leclercq F, Meunier PA, Gandet T, Macia JC, Delseny D, Gaudard P, et al. Simplified TAVR procedure: how far is it possible to go? J Clin Med. (2022) 11:2793. doi: 10.3390/jcm11102793
6. Ruge H, Burri M, Erlebach M, Lange R. Access site related vascular complications with third generation transcatheter heart valve systems. Catheter Cardiovasc Interv. (2021) 97:325–32. doi: 10.1002/ccd.29095
7. Rheude T, Pellegrini C, Lutz J, Alvarez-Covarrubias HA, Lahmann AL, Mayr NP, et al. Transcatheter aortic valve replacement with balloon-expandable valves: comparison of SAPIEN 3 ultra versus SAPIEN 3. JACC Cardiovasc Interv. (2020) 13:2631–8. doi: 10.1016/j.jcin.2020.07.013
8. Watanabe M, Takahashi S, Yamaoka H, Sueda T, Piperata A, Zirphile X, et al. Comparison of transcarotid vs. transfemoral transcatheter aortic valve implantation. Circ J. (2018) 82:2518–22. doi: 10.1253/circj.CJ-18-0530
9. Fernandez-Lopez L, Chevalier B, Lefèvre T, Spaziano M, Unterseeh T, Champagne S, et al. Implementation of the transradial approach as an alternative vascular access for transcatheter aortic valve replacement guidance: experience from a high-volume center. Catheter Cardiovasc Interv. (2019) 93:1367–73. doi: 10.1002/ccd.28024
10. Allende R, Urena M, Cordoba JG, Ribeiro HB, Amat-Santos I, DeLarochellière R, et al. Impact of the use of transradial versus transfemoral approach as secondary access in transcatheter aortic valve implantation procedures. Am J Cardiol. (2014) 114:1729–34. doi: 10.1016/j.amjcard.2014.09.009
11. Curran H, Chieffo A, Buchanan GL, Bernelli C, Montorfano M, Maisano F, et al. A comparison of the femoral and radial crossover techniques for vascular access management in transcatheter aortic valve implantation: the milan experience. Catheter Cardiovasc Interv. (2014) 83:156–61. doi: 10.1002/ccd.24913
12. Wynne DG, Rampat R, Trivedi U, de Belder A, Hill A, Hutchinson N, et al. Transradial secondary arterial access for transcatheter aortic valve implantation: experience and limitations. Heart Lung Circ. (2015) 24:682–5. doi: 10.1016/j.hlc.2014.12.011
13. Khubber S, Bazarbashi N, Mohananey D, Kadri A, Gad MM, Kaur M, et al. Unilateral access is safe and facilitates peripheral bailout during transfemoral-approach transcatheter aortic valve replacement. JACC Cardiovasc Interv. (2019) 12:2210–20. doi: 10.1016/j.jcin.2019.06.050
14. Aroney NP, Patterson T, Kalogeropoulos A, Allen CJ, Hurrell H, Chehab O, et al. Clinical outcomes following single access transfemoral transcatheter aortic valve implantation. Catheter Cardiovasc Interv. (2022) 100:227–32. doi: 10.1002/ccd.30246
15. Toggweiler S, Bagur R, Agatiello CR, Giuliani C, Moccetti F, Diamantouros P, et al. Transcatheter aortic valve replacement through a single femoral access: a multicenter experience. J Invasive Cardiol. (2022) 34:E739–42.36121924
16. VARC-3 WRITING COMMITTEE: Généreux P, Piazza N, Alu MC, Nazif T, Hahn RT, Pibarot P, et al. Valve academic research consortium 3: updated endpoint definitions for aortic valve clinical research. J Am Coll Cardiol. (2021) 77:2717–46. doi: 10.1016/j.jacc.2021.02.038
17. Jhand A, Apala DR, Dhawan R, Katta N, Aronow HD, Daniels MJ, et al. Meta-analysis comparing transradial versus transfemoral secondary access in transcatheter aortic valve implantation. Am J Cardiol. (2020) 131:74–81. doi: 10.1016/j.amjcard.2020.06.032
18. Das TM, Shin J, Czarny MJ, Nanavati J, Resar JR, Hasan RK. Radial versus femoral secondary access for transcatheter aortic valve replacement: a systematic review and meta-analysis. Catheter Cardiovasc Interv. (2022) 99:1225–33. doi: 10.1002/ccd.30009
19. Lucchese G, Montarello N, Bapat V. Modified single-puncture technique for transcatheter aortic valve implantation in patients without peripheral vascular access. Thorac Cardiovasc Surg. (2017) 65:231–3. doi: 10.1055/s-0036-1586494
20. Hayashida K, Lefèvre T, Chevalier B, Hovasse T, Romano M, Garot P, et al. Transfemoral aortic valve implantation new criteria to predict vascular complications. JACC Cardiovasc Interv. (2011) 4:851–8. doi: 10.1016/j.jcin.2011.03.019
21. Gurvitch R, Toggweiler S, Willson AB, Wijesinghe N, Cheung A, Wood DA, et al. Outcomes and complications of transcatheter aortic valve replacement using a balloon expandable valve according to the valve academic research consortium (VARC) guidelines. EuroIntervention. (2011) 7:41–8. doi: 10.4244/EIJV7I1A10
22. Van Mieghem NM, Tchetche D, Chieffo A, Dumonteil N, Messika-Zeitoun D, van der Boon RM, et al. Incidence, predictors, and implications of access site complications with transfemoral transcatheter aortic valve implantation. Am J Cardiol. (2012) 110:1361–7. doi: 10.1016/j.amjcard.2012.06.042
23. Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. (2019) 380:1695–705. doi: 10.1056/NEJMoa1814052
24. Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O'Hair D, et al. Evolut low risk trial investigators. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. (2019) 380:1706–15. doi: 10.1056/NEJMoa1816885
25. Abdelaziz HK, Megaly M, Debski M, Rahbi H, Kamal D, Saad M, et al. Meta-analysis comparing percutaneous to surgical access in trans-femoral transcatheter aortic valve implantation. Am J Cardiol. (2020) 125(8):1239–48. doi: 10.1016/j.amjcard.2020.01.021
26. Beurtheret S, Karam N, Resseguier N, Houel R, Modine T, Folliguet T, et al. Femoral versus nonfemoral peripheral access for transcatheter aortic valve replacement. J Am Coll Cardiol. (2019) 74:2728–39. doi: 10.1016/j.jacc.2019.09.054
27. Rashid MK, Sahami N, Singh K, Winter J, Sheth T, Jolly SS. Ultrasound guidance in femoral artery catheterization: a systematic review and a meta-analysis of randomized controlled trials. J Invasive Cardiol. (2019) 31:E192–8.31257213
28. Sobolev M, Slovut DP, Lee Chang A, Shiloh AL, Eisen LA. Ultrasound-guided catheterization of the femoral artery: a systematic review and meta-analysis of randomized controlled trials. J Invasive Cardiol. (2015) 27:318–23.26136279
29. Seto AH, Abu-Fadel MS, Sparling JM, Zacharias SJ, Daly TS, Harrison AT, et al. Real-time ultrasound guidance facilitates femoral arterial access and reduces vascular complications: FAUST (femoral arterial access with ultrasound trial). JACC Cardiovasc Interv. (2010) 3:751–8. doi: 10.1016/j.jcin.2010.04.015
30. Tchetche D, Dumonteil N, Sauguet A, Descoutures F, Luz A, Garcia O, et al. Thirty-day outcome and vascular complications after transarterial aortic valve implantation using both edwards sapien and medtronic CoreValve bioprostheses in a mixed population. EuroIntervention. (2010) 5:659–65. doi: 10.4244/eijv5i6a109
Keywords: transcatheter aortic valve replacement, simplification, single artery access procedure, propensity matched analysis, transfemoral
Citation: Yan Y, Yao J, Yuan F, Liu X, Luo T, Lu Z, Chang S, Zhang Q, Liu R, Yin C and Song G (2023) Single femoral artery access is safe and feasible during transcatheter aortic valve replacement: a propensity score matched analysis. Front. Cardiovasc. Med. 10:1228258. doi: 10.3389/fcvm.2023.1228258
Received: 24 May 2023; Accepted: 5 October 2023;
Published: 3 November 2023.
Edited by:
Paolo Denti, San Raffaele Hospital (IRCCS), ItalyReviewed by:
Hendrik Ruge, Technical University Munich, Germany© 2023 Yan, Yao, Yuan, Liu, Luo, Lu, Chang, Zhang, Liu, Yin and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guangyuan Song c29uZ2d5X2FuemhlbkBWSVAuMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.