- 1Division of Vascular Surgery, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China
- 2Private Medical Service & Healthcare Center, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China
Objective: Spontaneous isolated abdominal aortic dissection (SIAAD) is a rare aortic emergency and not yet fully understood. This study aims to report the characteristics and treatments of 31 patients with SIAAD in the past 12 years.
Methods: A total of 31 consecutive patients with SIAAD between 2010 and 2022 were included. The clinical manifestations, treatment strategies, and outcomes were reviewed. Following the SVS/STS reporting standard, we compared the clinical characteristics with different locations of primary entry, or different numbers of dissected zones. Furthermore, we compared the effects of surgical and conservative therapies on the outcome during the follow-up.
Results: Among the 31 patients with SIAAD, 16 (51.6%) were in the acute phase on admission. The primary entry of SIAAD was mainly located in Zone 9 (67.7%). Most patient presented with dissection involving 1 or 2 aortic zones (61.3%). In addition, 35.5% and 64.5% of SIAADs involved the visceral and iliac arteries, respectively. Compared with asymptomatic SIAADs, the symptomatic ones had longer dissection lengths (P = 0.008) and tended to involve iliac artery more frequently (P = 0.098). There were differences in the number of dissected aortic zones (P = 0.005) among patients with primary entry located in Zone 5 (Supraceliac aorta), Zone 6–8 (Paravisceral aorta) and Zone 9 (Infrarenal aorta). The involvement of visceral artery (P = 0.039) and iliac artery (P = 0.006) was significantly different between the subgroups of SIAAD involving one, two, and three or more aortic zones. The cumulative incidence of adverse false lumen progression events was significantly lower (P = 0.000) and the rate of false lumen thrombogenesis or disappearance was higher in patients receiving surgery (P = 0.001). The cumulative all-cause mortality was 9.7% at 1-year, and 19.7% at 5-year, with no significant difference between surgical and conservative therapies.
Conclusions: Clinical features of SIAAD vary depending on the location of the primary entry and the number of dissected aortic zones. Although surgery was not associated with a lower all-cause mortality compared with conservative therapy, it was associated with a lower incidence of adverse false lumen progression and a higher rate of aortic remodeling.
Introduction
Aortic dissection (AD) is a rare but fatal cardiovascular emergency mainly involving the ascending and descending aorta. Isolated abdominal aortic dissection accounts for 1%–4% of AD (1–3), with lesions limited to the abdominal aorta, as initially reported by Shekelton in 1822 (4). Currently, only small numbers of spontaneous isolated abdominal aortic dissection (SIAAD) were reported in several centers (5–10), and the characteristics and prognosis of SIAAD remain incompletely understood.
The symptoms of SIAAD are atypical, with abdominal or back pain as the main manifestation, while few patients present with limb ischemia. Notably, 10%–15% of the SIAAD may lead to aortic rupture (11, 12). Treatments of SIAAD include open surgery, endovascular aortic repair (EVAR), and conservative therapy. A meta-analysis of 491 cases showed that surgical treatments including open surgery and EVAR does not lower the early and late mortality compared to the conservative management (13). However, a more recent report argued that operation facilitated aortic remodeling and reduced adverse false lumen progression (14). The optimal treatment of SIAAD remains controversial.
This study aims to report the characteristics of 31 patients with SIAAD and to summarize the treatment outcomes in the patients managed with conservative or surgical treatments.
Methods
Enrollment of patients
SIAAD was defined as a spontaneous AD confined to the abdominal aorta below the aortic fissure and above the aortic bifurcation, regardless of its extension to visceral or iliac arteries. Patients with SIAAD were retrieved in the electronic medical record system, with exclusion of AD secondary to iatrogenic or traumatic causes, and intermural aortic hematomas or ulcers. The study was approved by the Ethics Committee for Clinical Research and Laboratory Animal Trials of the First Affiliated Hospital of Sun Yat-sen University, and all patients were informed and exempted from the informed consent due to the retrospective design.
Data collection and definition
Demographic data, stages, symptoms, comorbidity and risk factors were collected through the electronic medical record system. The stages of acute, subacute and chronic phase were defined as 1–14 days, 15–90 days and >90 days from the onset of symptoms, respectively. Aortic features, including direction of the entry tear (12–3 o’clock; 3–6 o’clock; 6–9 o’clock; 9–12 o’clock), length of the dissection, total aortic diameter, true lumen diameter, false lumen diameter, status of false lumen (patent, partial thrombosis, complete thrombosis), involvement of visceral or iliac artery, coexisting abdominal aortic aneurysm (AAA), were evaluated based on the imaging.
The abdominal aorta and iliac arteries can be divided into zones 5–11 (Supplementary Table S1), according to the Society for Vascular Surgery (SVS)/Society for Thoracic Surgery (STS) (SVS/STS) reporting standard published in 2020 (15). In this study, the SIAAD patients with lesion confined to the abdominal aorta were classified into three subgroups based on the location of primary entry tear according to SVS/STS reporting standard: Group 1 with primary entry tear located in Zone 5 (from superior border of T12 to the celiac trunk artery), Group 2 with primary entry tear located between Zone 6 and Zone 8 (from the celiac trunk artery to the lowest renal artery), and Group 3 with primary entry tear located between Zone 9 (from the lowest renal artery to the aorto-iliac bifurcation). In addition, patients were categorized into three subgroups based on the initial number of dissected zones: Group A with dissection involving one aortic zone, Group B with dissection involving two aortic zones, and Group C with dissection involving three or more aortic zones.
Treatment strategy
Treatment strategies were determined based on patients' clinical and anatomical features. Criteria for surgical treatment include: (1) presence of aortic rupture or pending rupture, (2) presence of organ or limb ischemia, (3) abdominal aortic diameter ≥30 mm, (4) symptoms did not relieve after standard medical treatment. For patients appropriate for endovascular repair, aortography was performed to determine the primary entry tear site, and the location and extent of the dissection. Endovascular repair including standard EVAR, EVAR with chimney technique to reconstruct visceral arteries, straight stent graft to cover the tears, kissing stent graft technique (16), and hybrid strategy was applied to individual patients depending on the anatomical features. Patients without surgical indications were treated with conservative therapy including strict control of blood pressure and heart rate.
Follow-up
The patients were followed up by CTA at 1 month, 3 months, 6 months and 12 months after surgery or discharge with conservative therapy, and annually thereafter. Symptoms, complications, and survivals were recorded, while progression of the false lumen was evaluated by the CTA.
Statistical analysis
Normal distribution variables were expressed as mean ± standard deviation, and comparisons were performed using t-test or ANOVA. Non-normal distribution variables were expressed as median (IQR, P25–P75) and compared using the Mann–Whitney U test or Kruskal–Wallis H test. Kaplan–Meier analysis was used to compare the cumulative outcomes during follow-up, and log-rank tests were used for comparisons within groups. All statistical analyses were performed using SPSS 26.0 software, with P < 0.05 being considered as statistically significant.
Results
Demographics
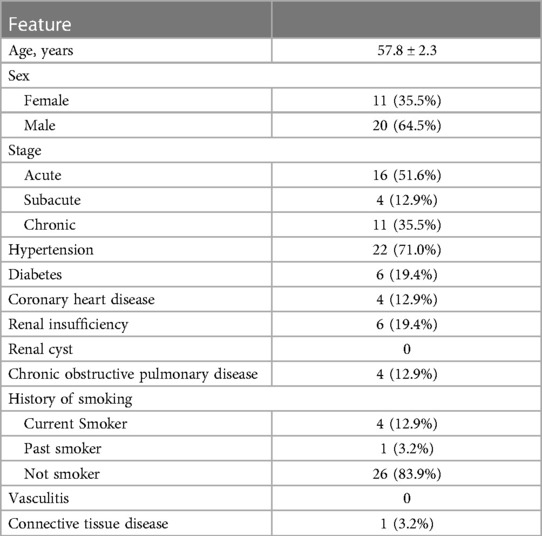
From 2010 to 2022, a total of 31 patients with SIAAD were included in the study. The mean age was 57.8 ± 2.3 years. On admission, 16 (51.6%), 4 (12.9%), and 11 (35.5%) patients were in the acute, subacute, and chronic phases, respectively. Hypertension were found in 71.0% of SIAAD patients. Only 19.4% and 12.9% patients presented with diabetes and coronary artery disease, respectively. Five cases had a history of smoking. One patient had a connective tissue disease (Table 1).
Clinical presentation
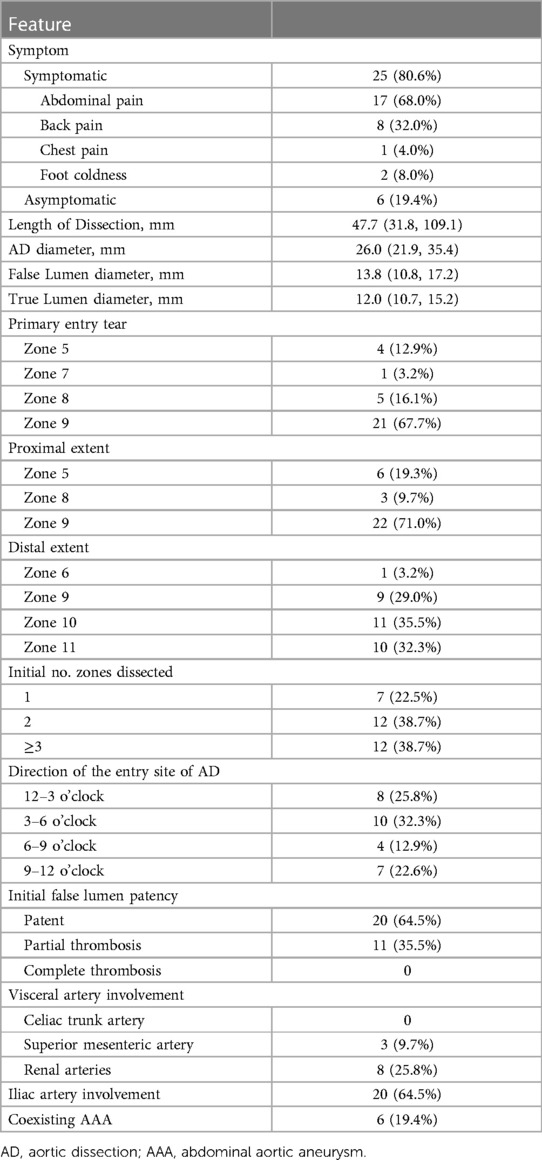
Of the 31 patients with SIAAD, 25 (80.6%) were symptomatic, with abdominal pain (17 cases, 68.0%) and back pain (8 cases, 32.0%) as the main symptoms. The primary entry tear was mainly located in Zone 9 (21 cases, 67.7%), with proximal extent mainly in Zone 9 (22 cases, 71.0%) and distal extent mostly in Zone 10–11 (21 cases, 67.8%). There were 3 (9.7%), 8 (25.8%), and 20 (64.5%) cases with dissection involving the superior mesenteric artery, renal artery, and iliac artery, respectively (Table 2).
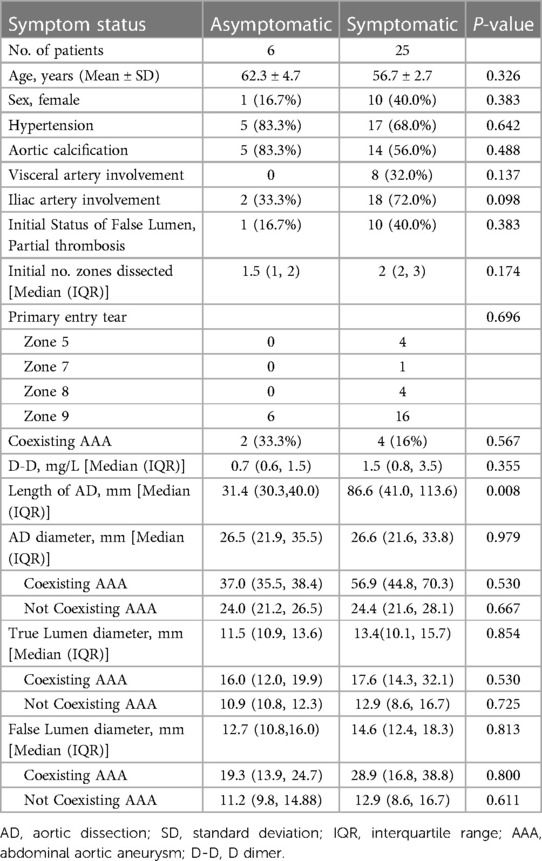
Compared with asymptomatic SIAAD, patients with symptomatic SIAAD had younger ages (56.7 ± 2.7 vs. 62.3 ± 4.7) and higher percentage of female gender (40.0% vs. 16.7%). Visceral artery involvement (32.0% vs. 0%) and iliac artery involvement (72.0% vs. 33.3%) were higher in symptomatic patients than that in asymptomatic patients, although the results did not reach a statistical significance. Length of dissection was significantly longer in symptomatic patients compared to asymptomatic patients (P = 0.008, Table 3), and the number of dissected zones in symptomatic patients tended to be larger than that in asymptomatic patients (Table 3). All asymptomatic patients had primary entry tears in Zone 9, while symptomatic patients had primary entry tears in multiple aortic zones.
None of the patients with primary entry tears in Group 3 (Zone 9) had a retrograde extension to the aorta in Zone 5–8. Visceral artery involvement was present in the patients with primary entry tears in either Group 1 (Zone 5) or Group 2 (Zone 6–8). The length of dissection tended to be longer in the SIAAD with primary entry tears in Group 2 (Zone 6–8) than Group1 (Zone 5) and Group 3 (Zone 9) (P = 0.051) (Table 4). Moreover, the initial number of dissected zones showed a significant difference among the three subgroups (P = 0.005). Comparison between subgroups showed that the initial number of dissected zones for patients with primary entry tears in Group 1 (Zone 5) and Group 2 (Zone 6–8) was both significantly greater than Group 3 (Zone 9) (P = 0.030, P = 0.039) (Table 4).
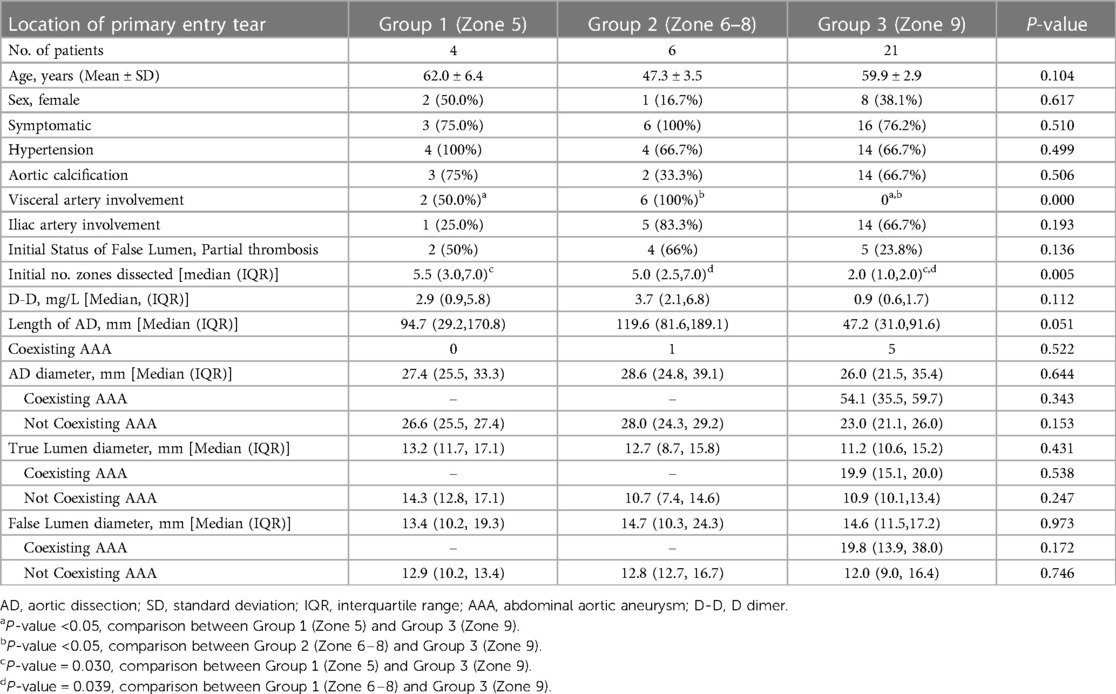
Table 4. Comparison of patients’ characteristics and morphologic features by the location of primary entry tear.
The distribution of visceral arterial involvement was significantly different among the three subgroups (Group A, Zone = 1; Group B, Zone = 2; Group C, Zone ≥3) (P = 0.039), but the dissection extent of SIAAD in the Group A (Zone = 1) was all confined to Zone 9 (Table 5). For iliac artery involvement, it occurred in 83.3% cases in the Group C (Zone ≥3), 75.0% cases in the Group B (Zone =2), and only 14.3% cases in the Group A (Zone =1), with a significantly different distribution among the three subgroups (P = 0.006), and the incidence of iliac artery involvement in the Group B (Zone = 2) and Group C (Zone ≥3) was both significantly higher than that in Group A (Zone = 1) (Table 5). In addition, the false lumen diameter tended to be larger in the Group C (Zone ≥3) than both the Group A (Zone = 1) and Group B (Zone = 2) (P = 0.102). After excluding the cases coexisting with AAA, there was a significant difference in false lumen diameter among the three subgroups (P = 0.025), and the false lumen diameter was significantly larger in the Group C (Zone ≥3) than that in the Group B (Zone = 2) (Table 5).
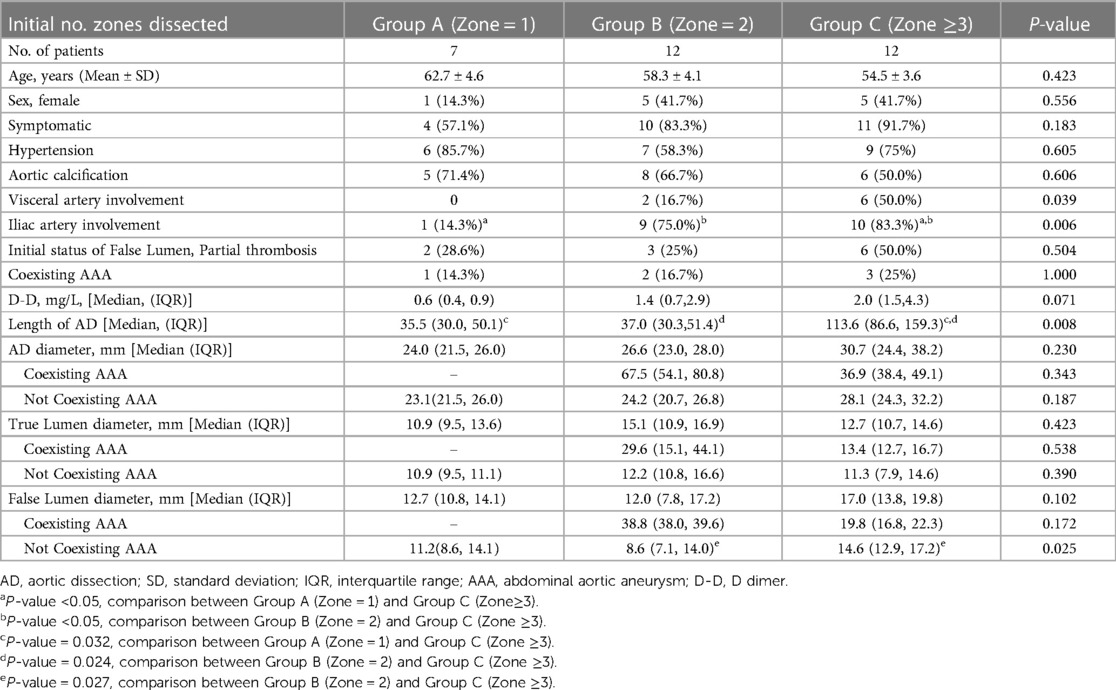
Table 5. Comparison of patients’ characteristics and morphologic features by initial number of aortic zones dissected.
Treatment outcomes
Eight patients received conservative treatment, while 23 patients underwent surgical treatment. including one hybrid surgery and 22 endovascular repair. Type I–III endoleaks were observed in 5, 1, and 1 patients in completion angiography, respectively (Supplementary Table S2). For one case involving Zone 5-Zone 8, the celiac trunk artery was intentionally covered to gain a sufficient landing zone. For patients with lesions involving all the paravisceral and infrarenal aorta (Zone 5-Zone 11), one was treated by straight stent graft combined with chimney stenting, one with entry tear in a collateral renal artery was sealed with aortic stent graft, and one with small entry tear in renal artery was left untreated and the infrarenal lesion was treated with aortic stent graft. For lesions involving Zone 9, straight aortic stent grafts were used in 2 cases, and bifurcated stent grafts were used for lesions near aortic bifurcation or involving the iliac artery in 3 cases. For SIAAD involving Zone 9–11, bifurcated stent graft was applied in 7 cases. When the diameter of the true lumen at the aortic bifurcation was less than 15 mm, straight stent graft combined with unilateral iliac stent graft was used in 1 case with unilateral iliac artery involved, while the kissing stent technique was used in 3 cases with bilateral iliac artery involved.
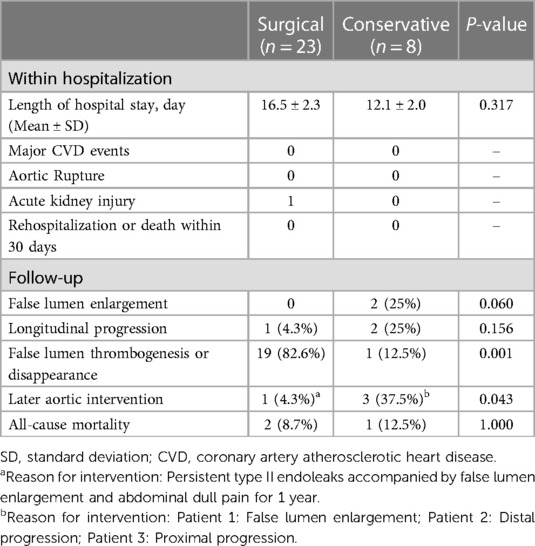
There was no significant difference in the length of hospital stay between conservative and surgical treatments. Furthermore, no major cardiovascular events or aortic rupture occurred during hospitalization after either treatment (Table 6). One patient receiving surgery developed acute renal injury, which fully recovered after rehydration therapy (Table 6). No patient died within 30 days for either treatment.
All patients were followed up with a median time of 37.5 months (IQR, 18.9–61.4 months). During the follow-up period, two cases (25%) developed false lumen enlargement and two cases (25.0%) developed longitudinal progression in patients receiving conservative treatment. In contrast, no false lumen enlargement and one case (4.3%) with longitudinal progression were observed in patients receiving surgery (Table 6). The Kaplan-Meier analysis in Figure 1A showed the cumulative incidence of adverse false lumen progression in patients receiving surgery was significantly lower than that in patients receiving conservative treatment (P = 0.000). The rate of false lumen thrombogenesis or disappearance was higher (82.6% vs. 12.5%, P = 0.001), while the aortic intervention rate was lower (4.3% vs. 37.5%, P = 0.043) in patients receiving surgery compared to patients receiving conservative treatment. In Figure 1B, the cumulative all-cause mortality was 9.5% at 1 year, and 19.5% at 5 years. No significant difference was found between surgical and conservative therapies (P = 0.320). In patients treated by surgery, one died of chronic heart failure 8 months after surgery, and one died of myocardial infarction 5 years later. In patients receiving conservative treatment, one died 6 months after discharge from hospital for unknown reason.
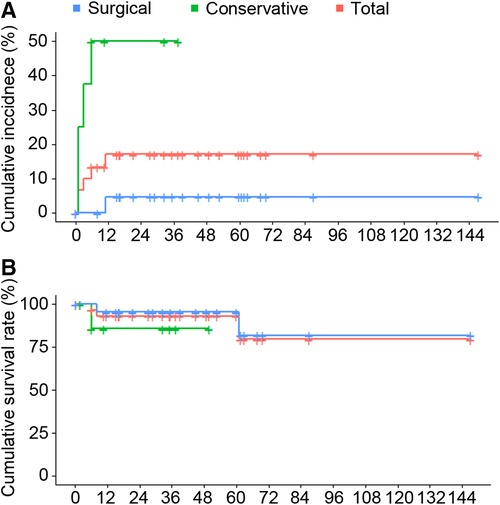
Figure 1. (A) Kaplan–Meier curves of the cumulative incidence of adverse aortic pathology during the follow-up of conservative versus surgical treatment in patients with SIAAD. (Log-Rank test: P-value = 0.000). (B) Kaplan–Meier curve of cumulative survival rate of conservative versus surgical treatment in SIAAD patients. (Log-Rank test: P-value = 0.320).
Discussion
This study described the clinical characteristics and treatment outcomes of 32 patients with SIAAD in a single center. Symptomatic patients had longer dissection length and were more likely to involve the iliac artery. SIAAD with entry tear in Zone 6-Zone 8 tended to have a longer dissection length and involve much more aortic zones, and proned to involve visceral arteries or iliac artery. Different treatment options did not affect the incidence of adverse events and all-cause mortality within hospitalization. Surgical treatment was associated with a lower incidence of false lumen progression and a higher rate of false lumen thrombosis and aortic remodeling compared with conservative treatment.
Symptoms are important for identifying SIAAD and may vary from asymptomatic to abdominal pain, back pain, chest pain, or foot coldness, depending on the extent of SIAAD. According to previous studies including the International Registry of Acute Aortic Dissection (IRAD) study, 21%–72% patients with SIAAD were symptomatic (5, 13, 17, 18). Of note, 81.3% patients were symptomatic in this study. Identification of asymptomatic patients mainly relies on the use of enhanced CT in patients with various abdominal symptoms. In this study, a total of 6 asymptomatic cases were found under examination for abdominal diseases. SIAAD should be suspected in the presence of symptoms such as abdominal pain, limb or visceral ischemia. In our study, symptomatic SIAAD had a longer length of dissection and was more likely to involve the iliac artery.
Morphological features of SIAAD can be updated and renewed in accordance with SVS/STS guidelines. Traditionally, SIAAD was divided into the infrarenal and suprarenal types to guide the choice of open surgery. New classifications composed of supraceliac, paravisceral and infrarenal SIAAD have been proposed, but the definition varied (7, 9). SVS/STS reporting standard provided a detailed description of anatomical aortic zones (15), which could help us renew the recognition of SIAAD morphological features. Consistent with previous reports, female gender, presence of symptoms, and visceral artery involvement were more likely to occur in patients with suprarenal (Zone 5–8) SIAAD (9). In addition, we found that the SIAAD with entry tear in Zone 9 were less extensive than those with entry tear in Zone 5–8 in terms of dissection length and number of dissected aortic zones, similar to previous studies (7). Meanwhile, none of patients with primary entry tear in Zone 9 had retrograde tears proximal to suprarenal aorta, suggesting that SIAAD with more distal primary entry tears may have less severe lesions. In addition, the false lumen diameter was larger in patients with the number of dissected aortic Zones ≥3 compared to 1 or 2. The results remained consistent after excluding cases with AAA, in line with a previous study which suggested patients with more extensive length of SIAAD had greater false lumen (7).
The optimal treatment of SIAAD is currently inconclusive. In patients receiving conservative treatment, no death within 30-day occurred, similar to previous reports of 1% (13). All-cause mortality was 12.5% at long-term follow-up, and 37.5% patients needed aortic-related intervention, all of them were slightly higher than previous report (13, 14). Of the 23 patients who received surgical treatment, the 30-day all-cause mortality was 0%, consistent with previous reports of 0%–3% (13, 14).In addition, all-cause mortality at follow-up was 8.7%, and the incidence of aortic intervention was 4.3%, in line with previous reports of 5–11.4% and 6%–9.1%, respectively (13, 14, 17). A network meta-analysis found that conservative treatment was superior to open surgery and EVAR in terms of early mortality and late mortality (18). Su Sheng et al. reported that the adverse false lumen progression was higher for conservative treatment. Our study found that the all-cause mortality rate of conservative treatment was slightly but not significantly higher than that of surgical treatment. Furthermore, the adverse false lumen progression was significantly higher for conservative treatment than surgical treatment. Moreover, Mozes et al. (19) reviewed 41 cases of SIAAD and found that aortic rupture occurred in 14% cases overall. In a study that included 79% patients with SIAAD, aortic rupture was found in 10% cases, and all-cause mortality and complication were higher in patients who received conservative treatment (2). This suggests that SIAAD receiving conservative therapy remains at a higher risk of adverse progression and aortic rupture. Endovascular repair may promote aortic remodeling, reduce the risk of false lumen progression and decrease aortic rupture.
There were several limitations in this study. First, our cohort was a single-center retrospective study, which might increase selection bias. Second, the small sample size of the subgroups might decrease the statistical confidence.
Conclusion
The clinical features of SIAAD vary depending on the location of the primary entry tear and the number of dissected aortic zones. Although surgical treatment was not associated with higher survival rate of SIAAD, it associated with a lower incidence of false lumen progression and a higher rate of aortic remodeling.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee for Clinical Research and Laboratory Animal Trials of the First Affiliated Hospital of Sun Yat-sen University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
ZZ, JL, and YL performed the project and drafted the original manuscript. JL provided statistical support. ZZ, YL, and KH contributed to electronic image analysis. MW, RW, ZH, and CY contributed to operation performance and clinical data collection. This project led by ZL and GC, who contributed to the design of this project and critically reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1214377/full#supplementary-material
References
1. Trimarchi S, Tsai T, Eagle KA, Isselbacher EM, Froehlich J, Cooper JV, et al. Acute abdominal aortic dissection: insight from the international registry of acute aortic dissection (IRAD). J Vasc Surg. (2007) 46(5):913–9. doi: 10.1016/j.jvs.2007.07.030
2. Jonker FH, Schlösser FJ, Moll FL, Muhs BE. Dissection of the abdominal aorta. Current evidence and implications for treatment strategies: a review and meta-analysis of 92 patients. J Endovasc Ther. (2009) 16(1):71–80. doi: 10.1583/08-2601.1
3. Handa N, Nishina T, Nishio I, Asano M, Noda K, Ueno Y. Endovascular stent-graft repair for spontaneous dissection of infra-renal abdominal aorta. Ann Vasc Surg. (2010) 24(7):955.e1–4. doi: 10.1016/j.avsg.2010.03.033
4. Doyle L. Three important early case reports on dissecting aneurysm of the aorta: one each from Dublin, Paris and York. J R Soc Med. (1992) 85(3):169–72.1556723
5. Faries CM, Tadros RO, Lajos PS, Vouyouka AG, Faries PL, Marin ML. Contemporary management of isolated chronic infrarenal abdominal aortic dissections. J Vasc Surg. (2016) 64(5):1246–50. doi: 10.1016/j.jvs.2016.04.030
6. Tayfur K, Senel Bademci M, Yazman S, Canyigit M. Endovascular approach in isolated abdominal aortic dissections. Vascular. (2018) 26(5):477–82. doi: 10.1177/1708538118760941
7. Zhu QQ, Li DL, Lai MC, Chen XD, Jin W, Zhang HK, et al. Endovascular treatment of isolated abdominal aortic dissection and postoperative aortic remodeling. J Vasc Surg. (2015) 61(6):1424–31. doi: 10.1016/j.jvs.2015.01.027
8. Böckler D, Bianchini Massoni C, Geisbüsch P, Hakimi M, von Tengg-Kobligk H, Hyhlik-Dürr A. Single-center experience in the management of spontaneous isolated abdominal aortic dissection. Langenbeck’s Arch Surg. (2016) 401(2):249–54. doi: 10.1007/s00423-015-1335-6
9. Kang JH, Kim YW, Heo SH, Woo SY, Park YJ, Kim DI, et al. Treatment strategy based on the natural course of the disease for patients with spontaneous isolated abdominal aortic dissection. J Vasc Surg. (2017) 66(6):1668–78.e3. doi: 10.1016/j.jvs.2017.03.435
10. Zlatanovic P, Dragas M, Cvetkovic S, Dimic A, Mitrovic A, Vujcic A, et al. Open surgical treatment of acute spontaneous isolated abdominal aortic dissection. Ann Vasc Surg. (2021) 74:525.e13–.e21. doi: 10.1016/j.avsg.2021.02.035
11. Farber A, Lauterbach SR, Wagner WH, Cossman DV, Long B, Cohen JL, et al. Spontaneous infrarenal abdominal aortic dissection presenting as claudication: case report and review of the literature. Ann Vasc Surg. (2004) 18(1):4–10. doi: 10.1007/s10016-003-0100-4
12. Graham D, Alexander JJ, Franceschi D, Rashad F. The management of localized abdominal aortic dissections. J Vasc Surg. (1988) 8(5):582–91. doi: 10.1016/0741-5214(88)90309-6
13. Liu Y, Han M, Zhao J, Kang L, Ma Y, Huang B, et al. Systematic review and meta-analysis of current literature on isolated abdominal aortic dissection. Eur J Vasc Endovasc Surg. (2020) 59(4):545–56. doi: 10.1016/j.ejvs.2019.05.013
14. Su S, Liu J, Wang C, Chen R, Liu Y, Huang W, et al. Optimal medical treatment versus endovascular aortic repair in uncomplicated isolated abdominal aortic dissection. J Vasc Surg. (2022) 77:1028–36.e2. doi: 10.1016/j.jvs.2022.10.036
15. Lombardi JV, Hughes GC, Appoo JJ, Bavaria JE, Beck AW, Cambria RP, et al. Society for vascular surgery (SVS) and society of thoracic surgeons (STS) reporting standards for type B aortic dissections. J Vasc Surg. (2020) 71(3):723–47. doi: 10.1016/j.jvs.2019.11.013
16. Yao C, Ning J, Li Z, Wang M, Wu R, Wang S, et al. Parallel covered stents technique in the treatment of abdominal aortic diseases. J Vasc Interv Radiol. (2020) 31(5):771–7. doi: 10.1016/j.jvir.2019.09.022
17. Sen I, D'Oria M, Weiss S, Bower TC, Oderich GS, Kalra M, et al. Incidence and natural history of isolated abdominal aortic dissection: a population-based assessment from 1995 to 2015. J Vasc Surg. (2021) 73(4):1198–204.e1. doi: 10.1016/j.jvs.2020.07.090
18. Wu J, Zafar M, Qiu J, Huang Y, Chen Y, Yu C, et al. A systematic review and meta-analysis of isolated abdominal aortic dissection. J Vasc Surg. (2019) 70(6):2046–53.e6. doi: 10.1016/j.jvs.2019.04.467
Keywords: spontaneous isolated abdominal aortic dissection, manifestation, conservative therapy, endovascular aortic repair, outcome
Citation: Zhao Z, Liu J, Liu Y, Huang K, Wang M, Wu R, Hu Z, Yao C, Li Z and Chang G (2023) Clinical characteristics and therapeutic strategy for patients with spontaneous isolated abdominal aortic dissection. Front. Cardiovasc. Med. 10:1214377. doi: 10.3389/fcvm.2023.1214377
Received: 29 April 2023; Accepted: 8 August 2023;
Published: 25 August 2023.
Edited by:
Tal Hörer, Örebro University Hospital, SwedenReviewed by:
Emily Spangler, University of Alabama at Birmingham, United StatesXiaobing Liu, Shanghai Jiao Tong University, China
Ding Yuan, Sichuan University, China
© 2023 Zhao, Liu, Liu, Huang, Wang, Wu, Hu, Yao, Li and Chang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zilun Li bGl6aWx1bkBtYWlsLnN5c3UuZWR1LmNu Guangqi Chang Y2hhbmdncUBtYWlsLnN5c3UuZWR1LmNu
†These authors have contributed equally to this work
 Zhengde Zhao
Zhengde Zhao Jiawei Liu2,†
Jiawei Liu2,† Yunchong Liu
Yunchong Liu Kan Huang
Kan Huang Chen Yao
Chen Yao Zilun Li
Zilun Li