
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 07 September 2023
Sec. Heart Failure and Transplantation
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1210278
This article is part of the Research Topic Methods in Treating Heart Failure - Device and Surgery Approach View all 16 articles
 Qiang Shen1,†
Qiang Shen1,† Dingyi Yao1,†
Dingyi Yao1,† Yang Zhao1,2,†
Yang Zhao1,2,† Xingyu Qian1
Xingyu Qian1 Yidan Zheng1
Yidan Zheng1 Li Xu1,2,3,4
Li Xu1,2,3,4 Chen Jiang1,2,3,4
Chen Jiang1,2,3,4 Qiang Zheng1
Qiang Zheng1 Si Chen1,2,3,4*
Si Chen1,2,3,4* Jiawei Shi1,2,3,4*
Jiawei Shi1,2,3,4* Nianguo Dong1,2,3,4*
Nianguo Dong1,2,3,4*
Background: The purpose of this study was to investigate the prognostic significance of serum albumin to creatinine ratio (ACR) in patients receiving heart transplantation of end-stage heart failure.
Methods: From January 2015 to December 2020, a total of 460 patients who underwent heart transplantation were included in this retrospective analysis. According to the maximum Youden index, the optimal cut-off value was identified. Kaplan-Meier methods were used to describe survival rates, and multivariable analyses were conducted with Cox proportional hazard models. Meanwhile, logistic regression analysis was applied to evaluate predictors for postoperative complications. The accuracy of risk prediction was evaluated by using the concordance index (C-index) and calibration plots.
Results: The optimal cut-off value was 37.54 for ACR. Univariable analysis indicated that recipient age, IABP, RAAS, BB, Hb, urea nitrogen, D-dimer, troponin, TG, and ACR were significant prognostic factors of overall survival (OS). Multivariate analysis showed that preoperative ACR (HR: 0.504, 95% = 0.352–0.722, P < 0.001) was still an independent prognostic factor of OS. The nomogram for predicting 1-year and 5-year OS in patients who underwent heart transplantation without ACR (C-index = 0.631) and with ACR (C-index = 0.671). Besides, preoperative ACR level was a significant independent predictor of postoperative respiratory complications, renal complications, liver injury, infection and in-hospital death. Moreover, the calibration plot showed good consistency between the predictions by the nomogram for OS and the actual outcomes.
Conclusion: Our research showed that ACR is a favorable prognostic indicator in patients of heart transplantation.
Heart failure is one of the most common cardiovascular manifestations (1). More than 26 million people worldwide are affected by heart failure (2). Heart transplantation (HTx) is the most effective and reliable treatment for end-stage heart failure (3). Over the past decades, the selection of HTx candidates and improvements in preoperative care have led to a steady improvement in outcomes after early HTx. Meanwhile, studies have shown that preoperative specific risk factors can predict survival after HTx, such as preoperative obesity, single-ventricle congenital heart disease, history of multiple thoracotomies, and renal replacement therapy (4–6). Therefore, it is very meaningful to study predictors of adverse HTx outcomes, as they may allow for closer monitoring and early intervention of patients at risk.
Human serum albumin is a key plasma protein and has important physiological functions such as immune regulation, endothelial stability, antioxidant effects, and binding to a variety of drugs, toxins, and other molecules (7). There is increasing evidence that serum albumin levels are closely associated with cardiovascular diseases, such as myocardial fibrosis, adverse pulsing aortic hemodynamics, heart failure, and coronary heart disease (8, 9). Furthermore, the serum albumin level before HTx is a useful marker for estimating post-transplantation survival (10). In addition, previous studies have pointed out that serum creatinine levels can affect prognosis in cardiac surgery (11). Importantly, glomerular filtration rate (GFR) is also often measured by serum creatinine level and can affect the prognosis of heart transplantation (9).
The definition of the ratio of serum albumin to creatinine (ACR) was proposed by Liu H (12). Recent studies have pointed out that it can be used to predict renal outcomes in diabetic patients. Meanwhile, ACR is also used in predicting the outcome of cardiovascular diseases, such as asymptomatic coronary artery disease and acute myocardial infarction (12–14). Nevertheless, its role in heart transplantation has not been investigated.
Therefore, in this retrospective study, we aimed to analyze the association of preoperative ACR levels with complications and overall survival (OS) after HTx.
Between 2015 and 2020, a total of 568 patients scheduled to undergo heart transplantation at Wuhan Union Medical College Hospital were included in this study. Age less than 18 years, retransplants, and patients with missing data were excluded. Ultimately 460 patients were recruited to the study and were divided into two groups of ACR > 37.54 (n = 262), and ACR ≤ 37.54 (n = 198), according to the optimal cut-off value of ACR (Figure 1). This retrospective study has been approved by the Committee of Tongji Medical College. The use and collection of patient data complied with the Declaration of Helsinki principles in our study.
Information on all survivors was collected through visits and telephone calls. OS was defined as the interval between surgery and death or last contact. The follow-up ended on December 31, 2020.
Demographic variables of all patients included sex, age, blood type, body mass index (BMI), and diagnosis. Additionally, the recipients' information also included the history of smoking, diabetes mellitus, previous cardiac surgery, hypertension, left ventricular ejection fraction (LVEF), and waiting time. The preoperative therapy data included extracorporeal membrane oxygenation (ECMO), implantable intra-aortic balloon pump (IABP), renin-angiotensin-aldosterone system (RAAS) antagonist, beta-blockers (BB), calcium channel blocker (CCB) and diuretics. Preoperative blood biochemical indexes included hemoglobin (Hb), white blood cell count (WBC), blood platelet (PLT), albumin, creatinine (Cr), bilirubin, glutamic oxaloacetic transaminase (AST), alanine aminotransferase (ALT), low-density lipoprotein (LDL), troponin and triglyceride (TG). Preoperative hematological and biochemical indicators are the first results of the first admission of a heart transplant patient.
We compared several postoperative clinical events between the high and low ACR groups, including postoperative ICU stay time, total postoperative hospital stay time, the use of postoperative CRRT, IABP, and ECMO, respiratory complications, neurological complications, hematological complications, hyperglycemia, hypertension, infection, renal injury, liver injury, septic shock, secondary thoracotomy, and death in hospital.
As previously reported in the literature, ACR was calculated from the ratio of serum albumin (mg/dl) to creatinine (mg/dl) (15). Postoperative infection is defined as an infection of soft tissues and organs after surgery and arises when the balance between host defense mechanisms and bacterial load or virulence is disrupted (16, 17).
In this study, continuous variables are expressed as mean ± standard deviation or median [interquartile range] according to their normality, whereas categorical variables are expressed as percentages. Different ACR groups were compared at baseline concerning participants' characteristics and outcome measures using Mann–Whitney U tests for continuous variables, which were tested to be non-normal distributions, and χ2 tests for categorical variables. The Cox proportional hazards regression model was used to determine independent predictors of mortality after heart transplantation. Besides, univariate and multivariable logistic regression was employed to identify predictors of postoperative clinical events. Survival analysis was performed using the Kaplan-Meier method, and significance was assessed by the log-rank test. Two-tailed P values < 0.05 were considered significant. The statistical analysis was performed with SPSS 23.0 and R-software v.4.2.1.
According to the inclusion and exclusion criteria, a total of 460 patients were included in the study. The median age was 50.00 years (38.00–57.00) and 359 (78%) of the patients were male. The median ACR of the samples was 39.32 (31.96–47.95). The histogram curve of ACR distribution is shown in Figure 2.
The association between ACR and survival is shown in the ROC curve (Figure 3). During the process, the area under the curve (AUC) for survival was 0.584 (P = 0.006). According to the maximum Youden index, it revealed that 37.54 was an optimal cut-off value of the ACR index for predicting the survival rate. By the optimal cut-off value of ACR, the patients were divided into two groups (high, ≥37.54, and low, <37.54).
Table 1 showed baseline patients' characteristics based on ACR. Patients with higher ACR levels tended to have a less proportion of males (P < 0.001) and chronic kidney disease (P < 0.001), younger age (P < 0.001), less hypertension (P = 0.017), more use of spironolactone (P = 0.002) and thiazides (P = 0.010), higher preoperative level of blood platelet (P = 0.033) and albumin (P < 0.001), lower preoperative levels of white blood cells (P = 0.001), creatinine (P < 0.001) and AST (P = 0.025), and a different proportions of Donor/recipient sex (P = 0.001).
At the end of follow-up, 121 (26.3%) patients had died and 339 (73.7%) patients were alive. The Kaplan-Meier curve (Figure 4) shows the association between OS and ACR for all patients. Patients with high ACR levels had better survival than those with low ACR levels (P < 0.001). To identify the risk factors affecting postoperative OS, the Cox proportional hazard model was applied to the analysis. Univariable analysis indicated that recipient age (P < 0.001), the preoperative use of IABP (P = 0.004), RAAS (P = 0.001), and BB (P = 0.016), preoperative level of Hb (P < 0.001), BUN (P = 0.004), D-dimer (P = 0.018), Troponin (P = 0.014), TG (P = 0.043) and ACR (P < 0.001) were significant prognostic factors of OS (Table 2). Nextly, significant prognostic factors identified by univariate analysis were entered into the multivariate Cox proportional hazards model. The results showed that recipient age (P = 0.005), the use of IABP (P = 0.008) and RAAS (P = 0.014), preoperative level of D-dimer (P = 0.041) and ACR (P = 0.019) were significant independent predictors of OS (Table 2).
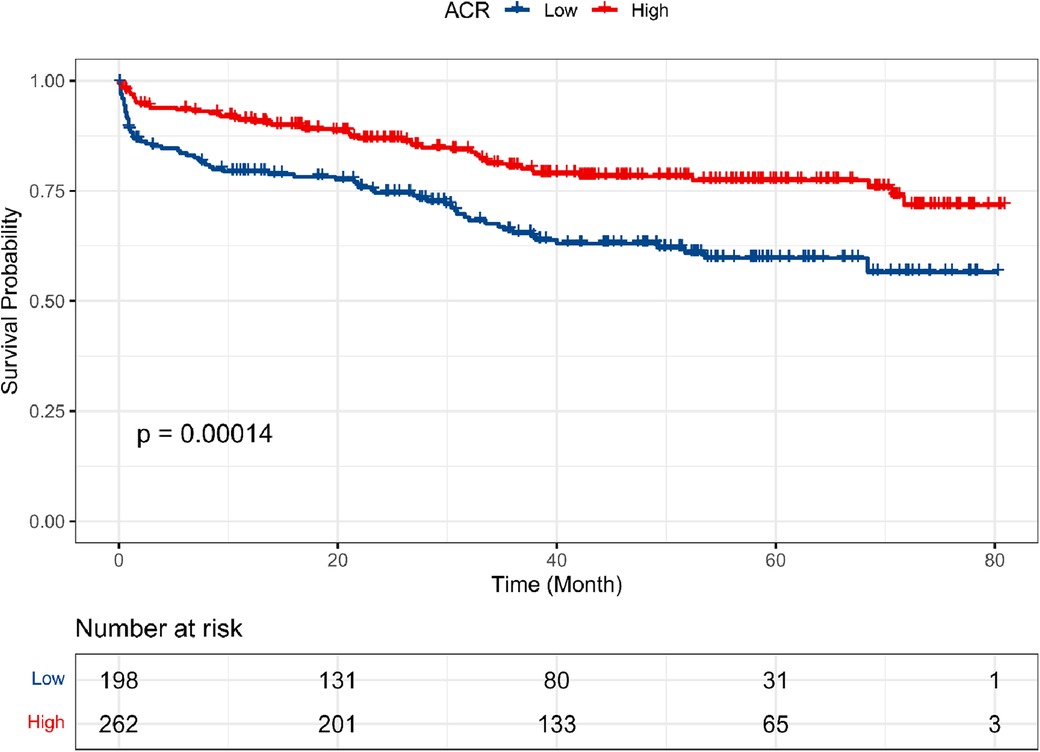
Figure 4. Kaplan–Meier survival curves for OS according to ACR. The low-ACR value group. Exhibited worse OS than high-ACR value group (P < 0.001).
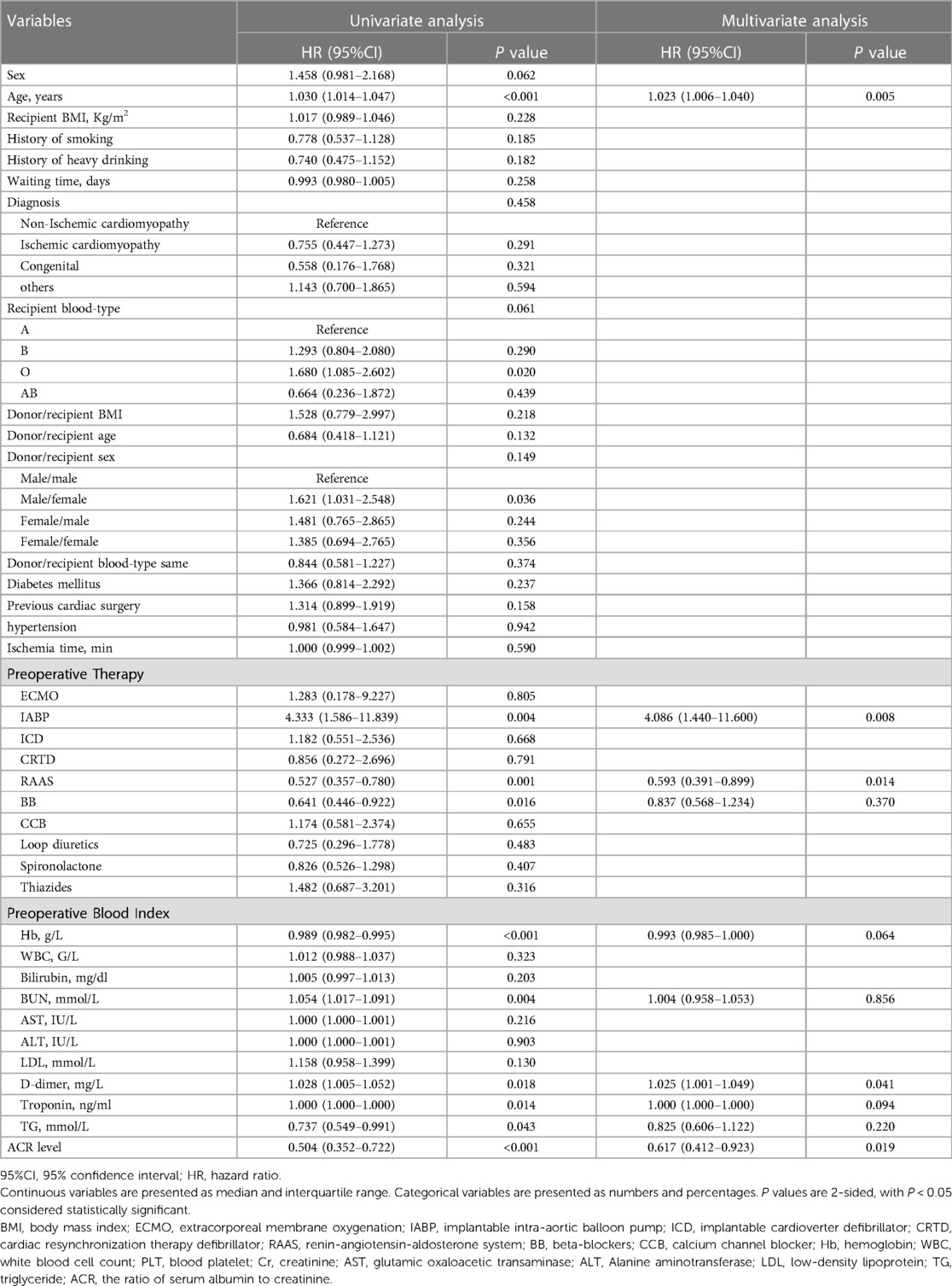
Table 2. Univariate and multivariate Cox proportional hazards regression models for overall survival in patients with heart transplantation.
A total of 17 surgery-related adverse clinical events occurred during the in-hospital posttransplant period, listed in Table 3. The result showed that lower levels of ACR tended to lead to more use of postoperative CRRT (P < 0.001) and IABP (P = 0.001), more respiratory complications (P = 0.001), liver injury (P = 0.005), kidney injury (P = 0.001), postoperative infection (P = 0.001), septic shock (P = 0.012), and in-hospital death (P = 0.001). We next performed univariate logistic regression analysis for these adverse clinical events (Supplementary Schedules S1–S8), and then the factors with P < 0.05 in univariate analysis were applied to multivariate logistic regression analysis. The results showed that lower preoperative ACR level was a significantly independent predictor of respiratory complications (P = 0.043), renal complications (P = 0.007), liver injury (P = 0.019), postoperative infection (P= 0.003) and in-hospital death (P = 0.028) (Table 4). What's more, higher age, less preoperative RAAS use and lower TG were independent risk factors of respiratory complication. Women and less RAAS use were independent risk factors of kidney injury. And less preoperative RAAS use was also associated with postoperative liver injury. Longer waiting time, diabetes mellitus and preoperative IABP were independently associated with in-hospital death. Moveover, smoking was an independent risk factor postoperative infection.
A nomogram (Figure 5) integrating was constructed based on five prognostic variables (age, IABP, RAAS, D-dimer, and ACR) from the univariate and multivariate Cox regression results. A Nomogram with ACR had a concordance index (C-index) of 0.671 compared with 0.631 without ACR. The calibration plot (Figure 6) showed good consistency between the nomogram predictions and actual observations of survival at 1- or 5- years.
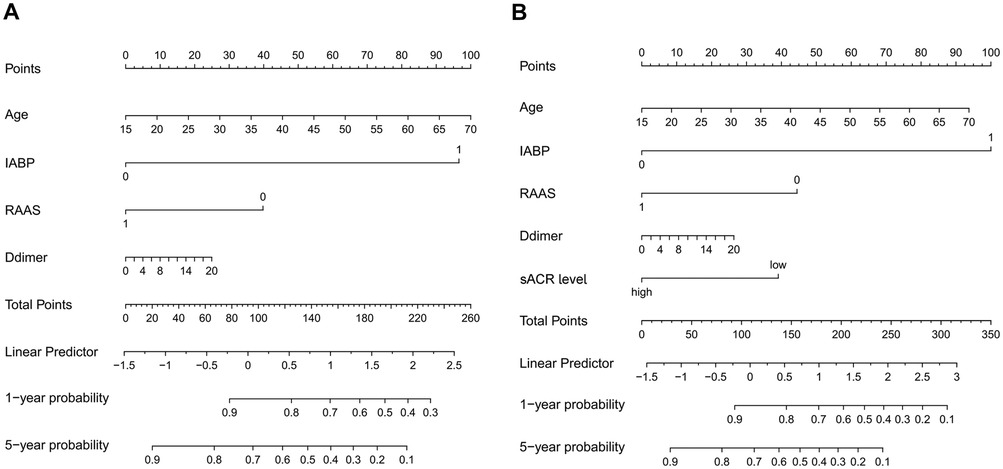
Figure 5. The nomogram for predicting 1-year and 5-year OS in patients who underwent HTx without ACR [(A), C-index = 0.631] and with ACR [(B), C-index = 0.671].
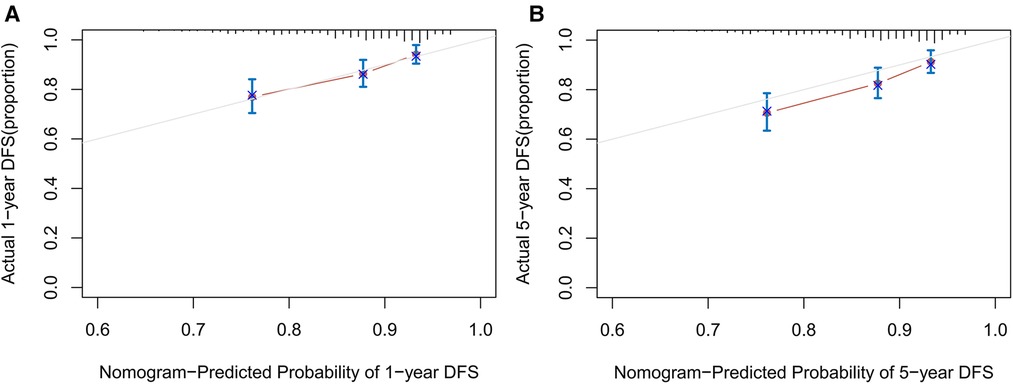
Figure 6. The calibration curves for predicting 1-year (A) and 5-year (B) OS of patients after HTx. Each point in the plot represents a group of patients, with the nomogram predicted probability of survival shown on x-axis and actual survival proportion shown on y-axis.
Heart failure is a common disease and the best treatment for patients with end-stage heart failure is HTx (1, 3). Meanwhile, many factors can predict the outcomes of HTx. For example, recent studies have pointed out that ACR as a preoperative indicator can predict the prognosis of cardiovascular disease (12–14). In this retrospective study, we evaluated the effect of ACR on the prognosis of HTx and found that high levels of ACR were a protective factor after HTx. Meanwhile, five possible prognostic factors (age, the use of IABP, RAAS, D-dimer, and ACR) were identified according to multivariable Cox regression analysis. Furthermore, multivariate logistic regression analysis showed that low levels of ACR are associated with several post-transplant complications, including respiratory complications, renal complications, liver injury, and in-hospital death. In addition, a visual nomogram was created in light of clinical variables and ACR, which helped to improve individual prognosis prediction accuracy.
Albumin is an important serum protein and has a wide range of physiological functions, such as immune regulation, endothelial stabilization, antioxidant effects, and binding to a variety of drugs, toxins, and other molecules (7). Albumin can also be used as a biomarker for many diseases, such as cancer, ischemia, obesity, severe acute graft-vs.-host disease, and diseases requiring monitoring of glycemic control (18). Specifically, numerous studies have demonstrated a strong association between serum albumin levels and the prognosis of cardiovascular diseases, such as atherosclerosis, myocardial infarction, and heart failure (19, 20). Moreover, Tomoko et al. proposed the effect of pre-transplant albumin levels on 1-year survival after heart transplantation in a retrospective study (21).
Creatinine was used as an index of renal function, which reflects not only renal excretion but also creatinine production (22, 23). In most genome-wide association studies, creatinine-based assessment of renal function (eGFR crea) has been used to define renal disease (24). Since the link between chronic kidney disease and cardiovascular disease was first described, numerous research suggested that chronic kidney disease greatly increases the risk of cardiovascular disease. This is partly because abnormal renal function leads to abnormal blood pressure, lipids, inflammatory responses, and increased activity of the renin-angiotensin system (25). Apart from preoperative renal disease, acute kidney injury is often a common complication after heart transplantation (26). It is associated with increased short- and long-term morbidity and mortality (27). Therefore, an important next step will be to investigate preoperative factors affecting AKI after heart transplantation.
The possibility of the correlation between ACR and the prognosis of HTx might be as follows: Firstly, Low serum albumin is often a marker of poor liver function (28). Likewise, in our study, we found that the preoperative ACR level was closely related to the occurrence of postoperative liver injury. In addition, albumin can improve the prognosis of heart transplantation by regulating systemic inflammatory response and immune response (7). Physiological concentrations of albumin attenuate inflammation by selectively inhibiting TNFα-induced upregulation of VCAM-1 expression and monocyte adhesion (29). Moreover, albumin inhibits histone-induced platelet aggregation and thrombus formation by binding to histones (30). These help explain why a low preoperative ACR level is associated with a higher incidence of septic shock. Besides, it is well established that oxidative stress is a common risk factor in various diseases, such as diabetes, inflammation, and cardiovascular disease. Oxidative stress generated by excessive reactive oxygen species (ROS) promotes cardiovascular disease (31). For example, starting point of atherosclerosis is considered to be oxidative stress, which facilitates key molecular events, such as oxidative modification of lipoproteins and phospholipids, endothelial cell activation, and macrophage infiltration/activation (32). Importantly, albumin exerts its antioxidant function by binding and neutralizing free metals such as copper and iron at its N-terminal site and specifically regulates cellular glutathione levels (7). Secondly, creatinine is a waste product of muscle metabolism (33). Produced at a continuous rate by creatine metabolism and excreted without tubular reabsorption, it is used as a marker of GFR (34). It is well-known that the reduction of GFR is now a recognized risk factor for cardiovascular disease (CVD) and chronic kidney disease (35, 36). Similarly, our results showed that low preoperative ACR levels are associated with a higher risk for postoperative Kidney Complications and In-hospital death. Besides, many studies have pointed out that chronic kidney disease often leads to dyslipidemia and inflammation, which leads to the hardening of the aorta and the reduction of coronary reserve (25, 37). Furthermore, kidney disease may cause remodeling of the ventricle through hypertension, renal anemia, and vascular stiffness, thus leading to hypertrophy of the left ventricle (25, 37). These biological processes may help explain associations between the level of ACR and the prognosis of HTx.
As far as we know, it is the first study to assess the role of ACR in HTx outcomes. Our study confirmed that preoperative ACR was a novel and promising indicator that independently predicts the outcomes of HTx. This investigation gives us some clues about preoperative interventions to reduce postoperative complications, such as albumin supplements (38–40).
However, there are some limitations of this study that should be considered. Firstly, this is a retrospective and observational study, which ignores the progression of the disease and has inherent risks of information bias. Secondly, the sample size of this study was small (n = 460) and the follow-up period was relatively short. Thirdly, preoperative frailty may have effect on the study results. Future studies about heart transplantation should consider this issue. What's more, null of the subjects in our study developed early graft failure, so the evaluation of early graft failure could not be performed. Lastly, we did not obtain cytokines, markers of glucose metabolism, or serum inflammatory markers, all of which may affect the prognosis of heart transplantation.
The data analyzed in this study is subject to the following licenses/restrictions: a portion of the data, models, or code generated or used during the study is proprietary or confidential in nature and may only be provided with restrictions (e.g., anonymized data). Requests to access these datasets should be directed to Dong N,MTk4NnhoMDY5NEBodXN0LmVkdS5jbg==.
This retrospective study has been approved by the Committee of Tongji Medical College. All patients signed the informed consent in light of the Declaration of Helsinki.
QS, DY and YZ: were in charge of collecting and analyzing data and writing this manuscript. XQ, YZ, LX, CJ and QZ: contributed to the discussion and provided additional advice. SC, JS and ND: gave their valuable and professional suggestions and guidance in organizing and drafting this manuscript. All authors contributed to the article and approved the submitted version.
This study was supported by the National Natural Science Foundation of China (81974034).
This research is attributed to the Department of Cardiovascular Surgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology. We are grateful to Guohua Wang, Jing Zhang, and Xiusi Xiongti for their generous assistance.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1210278/full#supplementary-material
1. Bansal N, Szpiro A, Reynolds K, Smith DH, Magid DJ, Gurwitz JH, et al. Long-term outcomes associated with implantable cardioverter defibrillator in adults with chronic kidney disease. JAMA Intern Med. (2018) 178(3):390–8. doi: 10.1001/jamainternmed.2017.8462
2. Abraham WT, Ponikowski P, Brueckmann M, Zeller C, Macesic H, Peil B, et al. Rationale and design of the EMPERIAL-preserved and EMPERIAL-reduced trials of empagliflozin in patients with chronic heart failure. Eur J Heart Fail. (2019) 21(7):932–42. doi: 10.1002/ejhf.1486
3. Tatum R, Briasoulis A, Tchantchaleishvili V, Massey HT. Evaluation of donor heart for transplantation. Heart Fail Rev. (2022) 27(5):1819–27. doi: 10.1007/s10741-021-10178-7
4. Grady KL, White-Williams C, Naftel D, Costanzo MR, Pitts D, Rayburn B, et al. Are preoperative obesity and cachexia risk factors for post heart transplant morbidity and mortality: a multi-institutional study of preoperative weight-height indices. Cardiac transplant research database (CTRD) group. J Heart Lung Transplant. (1999) 18(8):750–63. doi: 10.1016/S1053-2498(99)00035-2
5. O'Connor MJ, Glatz AC, Rossano JW, Shaddy RE, Ryan R, Ravishankar C, et al. Cumulative effect of preoperative risk factors on mortality after pediatric heart transplantation. Ann Thorac Surg. (2018) 106(2):561–6. doi: 10.1016/j.athoracsur.2018.03.044
6. Kim D, Choi JO, Cho YH, Sung K, Oh J, Cho HJ, et al. Impact of preoperative renal replacement therapy on the clinical outcome of heart transplant patients. Sci Rep. (2021) 11(1):13398. doi: 10.1038/s41598-021-92800-0
7. Spinella R, Sawhney R, Jalan R. Albumin in chronic liver disease: structure, functions and therapeutic implications. Hepatol Int. (2016) 10(1):124–32. doi: 10.1007/s12072-015-9665-6
8. Prenner SB, Pillutla R, Yenigalla S, Gaddam S, Lee J, Obeid MJ, et al. Serum albumin is a marker of myocardial fibrosis, adverse pulsatile aortic hemodynamics, and prognosis in heart failure with preserved ejection fraction. J Am Heart Assoc. (2020) 9(3):e014716. doi: 10.1161/JAHA.119.014716
9. Habib PJ, Patel PC, Hodge D, Chimato N, Yip DS, Hosenpud JD, et al. Pre-orthotopic heart transplant estimated glomerular filtration rate predicts post-transplant mortality and renal outcomes: an analysis of the UNOS database. J Heart Lung Transplant. (2016) 35(12):1471–9. doi: 10.1016/j.healun.2016.05.028
10. Kato TS, Lippel M, Naka Y, Mancini DM, Schulze PC. Post-transplant survival estimation using pre-operative albumin levels. J Heart Lung Transplant. (2014) 33(5):547–8. doi: 10.1016/j.healun.2014.01.921
11. Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol. (2004) 15(6):1597–605. doi: 10.1097/01.ASN.0000130340.93930.DD
12. Liu H, Zhang J, Yu J, Li D, Jia Y, Cheng Y, et al. Prognostic value of serum albumin-to-creatinine ratio in patients with acute myocardial infarction: results from the retrospective evaluation of acute chest pain study. Medicine. (2020) 99(35):e22049. doi: 10.1097/MD.0000000000022049
13. Sanchez RA, Sanchez MJ, Ramirez AJ. Renal function, albumin-creatinine ratio and pulse wave velocity predict silent coronary artery disease and renal outcome in type 2 diabetic and prediabetic subjects. Curr Hypertens Rev. (2021) 17(2):131–6. doi: 10.2174/1573402116999201210194817
14. Turkyilmaz E, Ozkalayci F, Birdal O, Karagoz A, Tanboga IH, Tanalp AC, et al. Serum albumin to creatinine ratio and short-term clinical outcomes in patients with ST-elevation myocardial infarction. Angiology. (2022) 73(9):809–17. doi: 10.1177/00033197221089423
15. Arar NH, Voruganti VS, Nath SD, Thameem F, Bauer R, Cole SA, et al. A genome-wide search for linkage to chronic kidney disease in a community-based sample: the SAFHS. Nephrol Dial Transplant. (2008) 23(10):3184–91. doi: 10.1093/ndt/gfn215
16. Alverdy JC, Hyman N, Gilbert J. Re-examining causes of surgical site infections following elective surgery in the era of asepsis. Lancet Infect Dis. (2020) 20(3):e38–43. doi: 10.1016/S1473-3099(19)30756-X
17. Steeg L T, Dominguez-Andres J, Netea MG, Joosten LAB, van Crevel R. Trained immunity as a preventive measure for surgical site infections. Clin Microbiol Rev. (2021) 34(4):e0004921. doi: 10.1128/CMR.00049-21
18. Fanali G, di Masi A, Trezza V, Marino M, Fasano M, Ascenzi P. Human serum albumin: from bench to bedside. Mol Aspects Med. (2012) 33(3):209–90. doi: 10.1016/j.mam.2011.12.002
19. Ronit A, Kirkegaard-Klitbo DM, Dohlmann TL, Lundgren J, Sabin CA, Phillips AN, et al. Plasma albumin and incident cardiovascular disease: results from the CGPS and an updated meta-analysis. Arterioscler Thromb Vasc Biol. (2020) 40(2):473–82. doi: 10.1161/ATVBAHA.119.313681
20. Deo R, Norby FL, Katz R, Sotoodehnia N, Adabag S, DeFilippi CR, et al. Development and validation of a sudden cardiac death prediction model for the general population. Circulation. (2016) 134(11):806–16. doi: 10.1161/CIRCULATIONAHA.116.023042
21. Kato TS, Cheema FH, Yang J, Kawano Y, Takayama H, Naka Y, et al. Preoperative serum albumin levels predict 1-year postoperative survival of patients undergoing heart transplantation. Circ Heart Fail. (2013) 6(4):785–91. doi: 10.1161/CIRCHEARTFAILURE.111.000358
22. Nielsen LR, Damm P, Mathiesen ER. Improved pregnancy outcome in type 1 diabetic women with microalbuminuria or diabetic nephropathy: effect of intensified antihypertensive therapy? Diabetes Care. (2009) 32(1):38–44. doi: 10.2337/dc08-1526
23. Levey AS, Perrone RD, Madias NE. Serum creatinine and renal function. Annu Rev Med. (1988) 39:465–90. doi: 10.1146/annurev.me.39.020188.002341
24. Ko YA, Yi H, Qiu C, Huang S, Park J, Ledo N, et al. Genetic-variation-driven gene-expression changes highlight genes with important functions for kidney disease. Am J Hum Genet. (2017) 100(6):940–53. doi: 10.1016/j.ajhg.2017.05.004
25. Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, Jafar TH, Heerspink HJ, Mann JF, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. (2013) 382(9889):339–52. doi: 10.1016/S0140-6736(13)60595-4
26. Goren O, Matot I. Perioperative acute kidney injury. Br J Anaesth. (2015) 115(Suppl 2):ii3–14. doi: 10.1093/bja/aev380
27. Lei C, Berra L, Rezoagli E, Yu B, Dong H, Yu S, et al. Nitric oxide decreases acute kidney injury and stage 3 chronic kidney disease after cardiac surgery. Am J Respir Crit Care Med. (2018) 198(10):1279–87. doi: 10.1164/rccm.201710-2150OC
28. Brahmer JR, Dahlberg SE, Gray RJ, Schiller JH, Perry MC, Sandler A, et al. Sex differences in outcome with bevacizumab therapy: analysis of patients with advanced-stage non-small cell lung cancer treated with or without bevacizumab in combination with paclitaxel and carboplatin in the eastern cooperative oncology group trial 4599. J Thorac Oncol. (2011) 6(1):103–8. doi: 10.1097/JTO.0b013e3181fa8efd
29. Zhang WJ, Frei B. Albumin selectively inhibits TNF alpha-induced expression of vascular cell adhesion molecule-1 in human aortic endothelial cells. Cardiovasc Res. (2002) 55(4):820–9. doi: 10.1016/S0008-6363(02)00492-3
30. Lam FW, Cruz MA, Leung HC, Parikh KS, Smith CW, Rumbaut RE. Histone induced platelet aggregation is inhibited by normal albumin. Thromb Res. (2013) 132(1):69–76. doi: 10.1016/j.thromres.2013.04.018
31. Shao D, Oka S, Liu T, Zhai P, Ago T, Sciarretta S, et al. A redox-dependent mechanism for regulation of AMPK activation by Thioredoxin1 during energy starvation. Cell Metab. (2014) 19(2):232–45. doi: 10.1016/j.cmet.2013.12.013
32. Forstermann U, Xia N, Li H. Roles of vascular oxidative stress and nitric oxide in the pathogenesis of atherosclerosis. Circ Res. (2017) 120(4):713–35. doi: 10.1161/CIRCRESAHA.116.309326
33. Bulka CM, Mabila SL, Lash JP, Turyk ME, Argos M. Arsenic and obesity: a comparison of urine dilution adjustment methods. Environ Health Perspect. (2017) 125(8):087020. doi: 10.1289/EHP1202
34. Nedergaard A, Sun S, Karsdal MA, Henriksen K, Kjaer M, Lou Y, et al. Type VI collagen turnover-related peptides-novel serological biomarkers of muscle mass and anabolic response to loading in young men. J Cachexia Sarcopenia Muscle. (2013) 4(4):267–75. doi: 10.1007/s13539-013-0114-x
35. Chronic Kidney Disease Prognosis C, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. (2010) 375(9731):2073–81. doi: 10.1016/S0140-6736(10)60674-5
36. Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO controversies conference report. Kidney Int. (2011) 80(1):17–28. doi: 10.1038/ki.2010.483
37. Pannier B, Guerin AP, Marchais SJ, Safar ME, London GM. Stiffness of capacitive and conduit arteries: prognostic significance for end-stage renal disease patients. Hypertension. (2005) 45(4):592–6. doi: 10.1161/01.HYP.0000159190.71253.c3
38. Hsich EM, Thuita L, McNamara DM, Rogers JG, Valapour M, Goldberg LR, et al. Variables of importance in the scientific registry of transplant recipients database predictive of heart transplant waitlist mortality. Am J Transplant. (2019) 19(7):2067–76. doi: 10.1111/ajt.15265
39. Lee EH, Kim WJ, Kim JY, Chin JH, Choi DK, Sim JY, et al. Effect of exogenous albumin on the incidence of postoperative acute kidney injury in patients undergoing off-pump coronary artery bypass surgery with a preoperative albumin level of less than 4.0 g/dl. Anesthesiology. (2016) 124(5):1001–11. doi: 10.1097/ALN.0000000000001051
Keywords: heart failure, heart transplantation, albumin/creatinine ratio, prognosis, nomogram
Citation: Shen Q, Yao D, Zhao Y, Qian X, Zheng Y, Xu L, Jiang C, Zheng Q, Chen S, Shi J and Dong N (2023) Elevated serum albumin-to-creatinine ratio as a protective factor on outcomes after heart transplantation. Front. Cardiovasc. Med. 10:1210278. doi: 10.3389/fcvm.2023.1210278
Received: 22 April 2023; Accepted: 22 August 2023;
Published: 7 September 2023.
Edited by:
Jamshid Karimov, Cleveland Clinic, United StatesReviewed by:
Dorin Ionescu, Carol Davila University of Medicine and Pharmacy, Romania© 2023 Shen, Yao, Zhao, Qian, Zheng, Xu, Jiang, Zheng, Chen, Shi and Dong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Si Chen U2ljaGVuQGh1c3QuZWR1LmNu Jiawei Shi MTk5OXhoMDUyMkBodXN0LmVkdS5jbg== Nianguo Dong MTk4NnhoMDY5NEBodXN0LmVkdS5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.