- 1Nursing Department, The Second Affiliated Hospital of Zhejiang University School of Medicine (SAHZU), Hangzhou, China
- 2Public Health Department, Changxing County People’s Hospital, Huzhou, China
- 3Emergency Department, Changxing County People’s Hospital, Huzhou, China
- 4Nursing Department, Lishui University School of Medicine, Lishui, China
Background: There is currently a pervasive prevalence of cardiovascular disease (CVD) risk worldwide and an inadequate amount of action is being taken to promote healthy lifestyle habits. The risk perception attitude (RPA) framework, which classifies individuals based on their risk perception and efficacy belief, enables us to predict their preventive behaviors. We applied the RPA framework to analyze CVD prevention behaviors among Chinese adults and extended its application to CVD objective risk.
Methods: A cross-sectional survey was performed in two sites in Zhejiang Province, from March to August 2022, which contained self-reported CVD risk perception, objective CVD risk, efficacy belief, physical activity, healthy diet, and covariates. We used the RPA framework to categorize participants into four groups, then analysis was conducted to estimate inter-group differences in healthy behaviors. We further conducted a hierarchical logistic regression analysis with individuals' health behaviors as the dependent variable, using three blocks of independent variables.
Results: Among 739 participants, healthy physical activity and healthy diet had significant differences among four RPA groups, post hoc tests clarified that the proportion of respondents with healthy PA in the responsive group (61.6%) was significantly higher than that in the other three groups. Risk perception and efficacy belief significantly predicted health behavior against CVD; the relationship between absolute CVD risk and health behavior was moderated by efficacy belief.
Conclusions: Early CVD risk screening is crucial, but tailored support and a proper understanding of personal risk are essential to promote healthy behaviors. Developing communication and behavioral counseling intervention strategies on the basis of the RPA framework has the potential to promote healthy behaviors for CVD prevention.
Background
Cardiovascular diseases (CVDs) are the leading cause of disease burden in the world, and cardiometabolic, behavioral, environmental, and social risk factors are major drivers of CVDs (1, 2). In China, CVDs were the leading cause of death (36%) (3). Furthermore, metabolic risk factors accounted for the largest proportion of CVD (41.7%), among which the largest risk factor was hypertension (25.0%), followed by high non-HDL-cholesterol (7.8%), abdominal obesity (6.9%), and diabetes (2.0%) (3). That means the CVD burden resulting from modifiable risk factors continues to increase globally. There is a pressing need to focus on controlling metabolic risk factors and improving education to address this severe public health threat.
Lifestyle modification is the foundation of both primary and secondary prevention of CVDs to reduce cardiometabolic risk, which has been emphasized by major evidence-based guidelines (4–6), such as physical activity (PA), healthy diet (HD), and smoking cessation. Despite this, the current status of lifestyle management remains suboptimal (7, 8). Only 39.6% of adults adopt at least three kinds of low-risk lifestyles from the China Nutrition and Health Surveillance (CNHS) (9), likewise, only 11.1% of adults aged 35–75 years follow a healthy diet and only 23.6% have sufficient physical activity according to the China PEACE Million Persons project (10).
Behavior change is difficult and challenging since it requires making changes to deeply ingrained habits and routines. People may experience multiple barriers to adopting healthy lifestyles, including access to care, knowledge, cost, cultural tradition, time constraints, and social pressure (11–13). As we know, the understanding of CVD risk is a prerequisite for adopting a healthy lifestyle and habits (14). Hence, a positive correlation could be found between individual risk perception and health behaviors (15). Risk perception is widely recognized as a dependable indicator of individuals' inclination to adopt precautionary behaviors, as expounded in various theories (e.g., protective motivation theory, health belief model). Nonetheless, the causal connection between risk perception and CVD prevention behavior has been shown to be relatively weak (16–18). On the other hand, people who possess the competency and confidence to manage their own health may be more inclined to believe that adopting a healthy lifestyle can enhance their health status, thus reinforcing their willingness to comply with health behaviors (19). In addition, the propensity to engage in health behaviors will increase as health self-efficacy increases (20). However, there is limited research on the effects of individual perceptions of CVD risk and health self-efficacy on health behaviors among populations with CVD risk.
Risk perception attitude framework
To understand the relationship between risk perception, health self-efficacy, and health behaviors, we applied the risk perception attitude (RPA) framework in this study. Specifically, the RPA framework proposes that risk perception and efficacy belief not only have a direct impact but also a moderating effect on individuals' health-related behavior (21). According to the RPA framework, people can be categorized into one of four distinct groups based on risk perception and efficacy level. The “Responsive” category refers to individuals who have high levels of both perceived risk and self-efficacy; individuals with a high level of perceived risk but low self-efficacy were labeled as “Avoidant”; individuals with a low level of perceived risk but high self-efficacy were categorized into the “Proactive” group; and individuals with both a low level of perceived risk and self-efficacy were labeled as “Indifferent”. The RPA framework suggests that individuals in the “Proactive” and “Indifferent” categories may not be as likely to actively change their behaviors due to their lower level of perceived risk. However, the “Responsive” group, who have high levels of both perceived risk and self-efficacy, are more likely to be active actors in changing their health behaviors. On the other hand, the “Avoidant” group, who also have high levels of perceived risk but low levels of self-efficacy, may be less likely to take action towards changing their behaviors compared to the “responsive” group. This highlights the importance of considering both risk perception and self-efficacy when understanding health behavior change comprehensively (21).
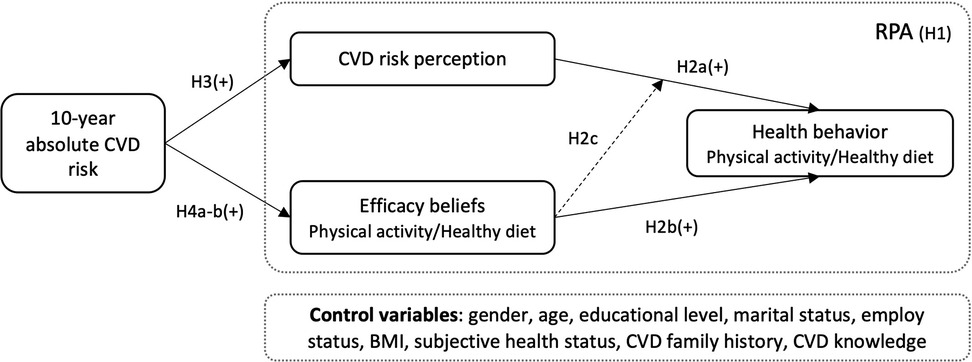
Several studies have indeed tested the effectiveness of the RPA framework in promoting health behavior changes related to the prevention of HIV or HPV (22–24), cancer (25, 26), diabetes (27, 28), and COVID-19 (29, 30), as well as pregnancy leisure-time physical activity (31, 32), information seeking (33, 34), safety behavior while driving (35), or using chemical household products (36). However, the RPA framework has yet to be applied to understand health behaviors in response to CVD risk reduction. Furthermore, cultural norms and values can influence how people perceive and respond to risk (37), so it is essential to explore the application of the RPA framework in a non-Western cultural context. The following hypotheses were proposed: (Figure 1)
H1: Differences exist among the four RPA categories in health behaviors (physical activity, healthy diet). Participants in “Responsive” and “Proactive” groups will present higher levels of health behaviors (physical activity, healthy diet) than participants in “Indifferent” and “Avoidant” groups. In addition, the four RPA groups differ in their demographic characteristics.
H2: Participants’ (a) perceived risk, (b) efficacy belief, and (c) their interaction would positively predict health behaviors (physical activity, healthy diet) toward CVD prevention.
Cardiovascular disease risk appraisal
Current guidelines for CVD prevention all apply objective absolute estimates of an individual's risk of developing CVD to guide treatment decisions and hierarchical prevention strategies (5, 38, 39). Specifically, lifestyle change was needed for individuals of low risk; moderate-risk individuals should adhere to lifestyle change initially, medication should be considered unless additional risk factors were present or lifestyle modification was inefficacy, and high-risk individuals should accept both blood pressure or cholesterol-lowering medication and lifestyle modification. Risk appraisal provides a platform for healthcare professionals and patients to discuss the absolute CVD risk and potential treatment options, then allows patients to make informed health decisions leading to improved adherence to medication and healthy behaviors (40). CVD risk estimation tools are commonly used to calculate the 10-year or lifetime risk of individuals and directly reflect the impact of multicomponent interventions in large randomized controlled trials (41). However, such hierarchical risk intervention strategies are likely to be effective only if individuals understand their own risks and potential benefits of prevention interventions first, then they are more likely to identify the need for change (42). Several studies reported that mismatch widely occurred between objective calculated CVD risk and individual perceived risk, which in turn affects one's willingness to use or consider preventive medication and adopt healthy lifestyles (15, 43, 44). Some studies reported no correlation found between absolute CVD risk, an individual's perceived risk, and healthy behaviors (16, 45, 46). People with high-perceived CVD risk were more likely to adopt healthy behaviors compared with under-perceived ones, but the effect path was unclear. In addition, there is a limited amount of study to certify the relationship between CVD objective risk, risk perception, efficacy belief, and health behaviors. Examining the prediction role of objective absolute risk on an individual's healthy behaviors, along with their risk perception and efficacy belief, will expand our knowledge of the RPA framework in CVD prevention scenarios. Based on the logical de deduction and literature review, we propose the following hypothesis (Figure 1):
H3: 10-year absolute CVD risk is positively associated with CVD risk perception.
H4: 10-year absolute CVD risk is positively associated with healthy physical activity efficacy belief (a) and healthy diet efficacy belief (b).
Methods
Sampling and procedure
A cross-sectional survey with convenience sampling was conducted in two sites of Zhejiang Province, from March to August 2022. The inclusion criteria were: (1) enrolled as a Zhejiang citizen in the District of Hangzhou or Changxing area; (2) being 20–80 years of age; (3) having no previous diagnosis of CVD; (4) having full medical examination report within at last three months; and (5) being able to read and speak in Mandarin. Participants with critical illness or intellectual disability, or who were pregnant or undergoing treatment for a psychiatric disorder were excluded.
The sample size calculation considers the requirements of regression models and mediating effect analysis, the required sample size should be 10 to 15 times the number of observed variables (47, 48). A total of 9 demographic factors and 7 scale-related dimensions were considered independent variables in our study, assuming an attrition rate of 20%, at least (9 + 7) × 10 × (1 + 20%) = 192.
Data were collected through standardized protocol and questionnaires administered by well-trained researchers. Both a paper-based questionnaire and an online survey platform powered by WJX (www.wjx.com) were provided and anonymized, and participants could choose the survey they preferred. Prior to beginning the questionnaire, a paragraph detailed the research purpose, data usage, and privacy protection. After agreeing to these terms, participants proceeded to the questionnaire page and filled it out independently. The questionnaire included general information, 10-year CVD absolute risk appraisal, CVD risk perception, healthy diet-related efficacy belief, physical activity-related efficacy belief, healthy diet score, and self-reported physical activity. The items were self-assessed by participants except for the 10-year CVD risk appraisal. The 10-year absolute CVD risk was calculated using an online calculator by the investigator after obtaining the indicators from the health check report, with the permission of the participants. If participants were unable to write, the investigator read each item to them, then the questionnaire was completed according to the statements of the participants. The research was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine (No. 2022-0280). After the exclusion of 43 responses with incomplete or invalid answers to the questionnaire, a total of 739 participants were included in the final analysis.
Measurements
General information
Demographic data contained age, gender, height (cm), weight (kg), marital status (coded as married or single), education level (coded as less than junior school, middle school/high school, college school, and above), employment status (coded as employed or unemployed), family history of CVD, and subjective health status. Body mass index (BMI) was determined by dividing weight (kg) by height (m) squared. Family history of CVD was defined as the presence of at least one immediate relative (parent or sibling) with myocardial infarction or stroke (49). Subjective health status was assessed by the response to the question, “In general, how would you rate your health status?” (1 = very poor, 2 = poor, 3 = fair, 4 = good, 5 = excellent) (50).
10-year CVD absolute risk appraisal
The 10-year CVD absolute risk was calculated using the China-PAR (Prediction for Atherosclerotic cardiovascular disease Risk) equation (51) which was developed from the gender-specific Cox proportional hazards model (49). The estimation items included sex, age, geographic region (Northern China/Southern China), urbanization (urban/rural), treated or untreated Systolic blood pressure (mmHg), total cholesterol (mmol/L), high-density lipoprotein cholesterol (HDL-C; mmol/L), currently smoking (yes/no), diabetes (yes/no), waist circumference (WC; cm), and family history of CVD (yes/no). Based on the cut-off value recommended in the Chinese guideline (38), participants were divided into three classes: low risk (<5%), moderate risk (5%–9.9%), and high risk (≥10%). The risk score was obtained through an online calculator (https://www.cvdrisk.com.cn/ASCVD/Eval).
CVD risk perception
The Attitude and Beliefs about Cardiovascular Disease (ABCD) Risk Questionnaire (52) was employed to measure people's CVD risk perception, which has confirmed validity in the Chinese population (ABCD-C) (53). The scale contains 26 items of four dimensions: CVD-related knowledge (8 items), risk perception (8 items), perceived benefits and intention to change physical activity (6 items), and perceived benefits and intention to change dietary habits (4 items). For knowledge items, 1 = right answer, 0 = wrong or “I don’t know” answer. Values were summed to a total score, with a higher score indicating a higher level of CVD-related knowledge. Answer options for another three dimensions were presented on a Likert 4-point scale ranging from 1 (strongly disagree) to 4 (strongly agree); a “not applicable” option was added, with a value of 0. Items 15, 21, and 26 were reverse-coded. In the present study, the Cronbach's α for the four dimensions was 0.668, 0.936, 0.894, 0.846, respectively.
Physical activity and healthy diet efficacy belief
According to social cognitive theory, and following recommendations by Rimal et al. (26), efficacy belief comprises (a) self-efficacy indicating an individual perceived ability to exert personal control, and (b) response efficacy which are the perceived benefits from engaging in a particular behavior (healthy diet, physical activity) (36). For self-efficacy, we used the single item “I am confident that I can exercise at least 150 min a week/ eat at least 500 g per day of fresh fruit and vegetables within the next two months”. For response efficacy, respondents answered the following question: “When I exercise for at least 150 min a week/eat at least 500 g per day of fresh fruit and vegetables, I am doing something good for the health of my heart”. Answer options for both constructs used a 4-point Likert scale (1 = strongly disagree to 4 = strongly agree). These items were extracted from ABCD-C (53). Efficacy beliefs were calculated as the average of self-efficacy and response efficacy. Based on a median split method recommended by Lee et al (36), a high- and a low-efficacy belief group was created.
Healthy diet score
A semi-quantitative food frequency questionnaire (FFQ) was used to collect habitual dietary intake through the response to the frequency of eating 18 food types during the past year (54). For each food type, seven frequency classes were presented (“more than 3 times per day”, “1–2 times per day”, “5–6 days per week”, “3–4 days per week”, “1–2 days per week”, “1–3 days per month”, “never or almost never”) (Supplementary Table S1). Based on the recommendations in the updated Chinese Dietary Guideline (55), the healthy diet score was computed based on the weekly intake of six food groups. These groups include fresh fruit, fresh vegetables, whole grains, eating fish and other seafood (more than once per week), beans and bean foods (at least four times per week), and red meat (less than seven times per week). A response that met the criterion scored 1 for each food group, and the total score was summed (full score = 6). The healthy group was defined as those with a total score ≥4 (10, 56).
Self-reported physical activity
Self-reported weekly physical activity was assessed through the International Physical Activity Questionnaire-short version (IPAQ) (57). Participants were asked to report the frequency and duration of their engagement in vigorous physical activity, moderate physical activity, walking, and sedentary behavior per week. The IPAQ guidelines for Chinese were used to process and aggregate the responses (58). The test-retest reliability was 0.71–0.93 in the Chinese population, and the criterion-related validity to the accelerometer was 0.60 (59). Participants who engaged in at least 150 min of moderate-intensity physical activities or 75 min of vigorous-intensity physical activities per week were deemed to have met the requirements for sufficient physical activity (38), which was considered healthy in this study.
Formation of four risk perception attitude groups
The participants were categorized into four RPA groups based on their scores in risk perception, efficacy belief for healthy physical activity, and healthy diet, respectively. We employed the segment approach reported in previous relevant studies (27, 32, 36) to identify RPA groups. A median split of both risk perception and efficacy belief was used to produce four groups, then the groups were classified as high (≥16.82) and low (<16.82) risk perception groups. For efficacy belief, the median value for physical activity and healthy diet was 3.09 and 3.23, respectively; therefore, we split the respondents into high (≥3.09/3.23) and low (<3.09/3.23) efficacy belief groups. Afterward, we created a bi-plot that categorized each risk classification into its respective quadrant: responsive (high risk perception + high efficacy), proactive (low risk perception + high efficacy), avoidant (high risk perception + low efficacy), and indifferent (low risk perception + low efficacy).
Statistical analysis
SPSS 26.0 and the SPSS macro program process plug-in were used to process the data for statistical analysis. The chi-square test and ANOVA were conducted to compare the difference in demographics, risk perception, efficacy belief, healthy physical activity, and healthy diet ratio among four RPA groups. Post hoc analyses used Tukey's HSD or adjusted Bonferroni method. The correlations of the study variables were analyzed by Spearman's correlation. To test the hypotheses, we performed a hierarchical logistic regression analysis with individuals' health behaviors (physical activity and healthy diet, respectively) as the dependent variable. The blocks of indicators were entered into the regression through three steps: (1) the control variables including age, gender, education level, marital status, employment status, BMI, subjective health status, CVD family history, CVD related knowledge; (2) CVD risk perception and efficacy belief; (3) risk perception × efficacy belief. The interaction term was mean-centered to reduce potential multi-collinearity (60). Path analysis was conducted to test the relationships among 10-year absolute CVD risk, CVD risk perception, efficacy belief, and healthy behaviors. Mediating effect tests were conducted following the procedure suggested by Zhonglin Wen et al. (61). P < 0.05 was considered statistically significant.
Results
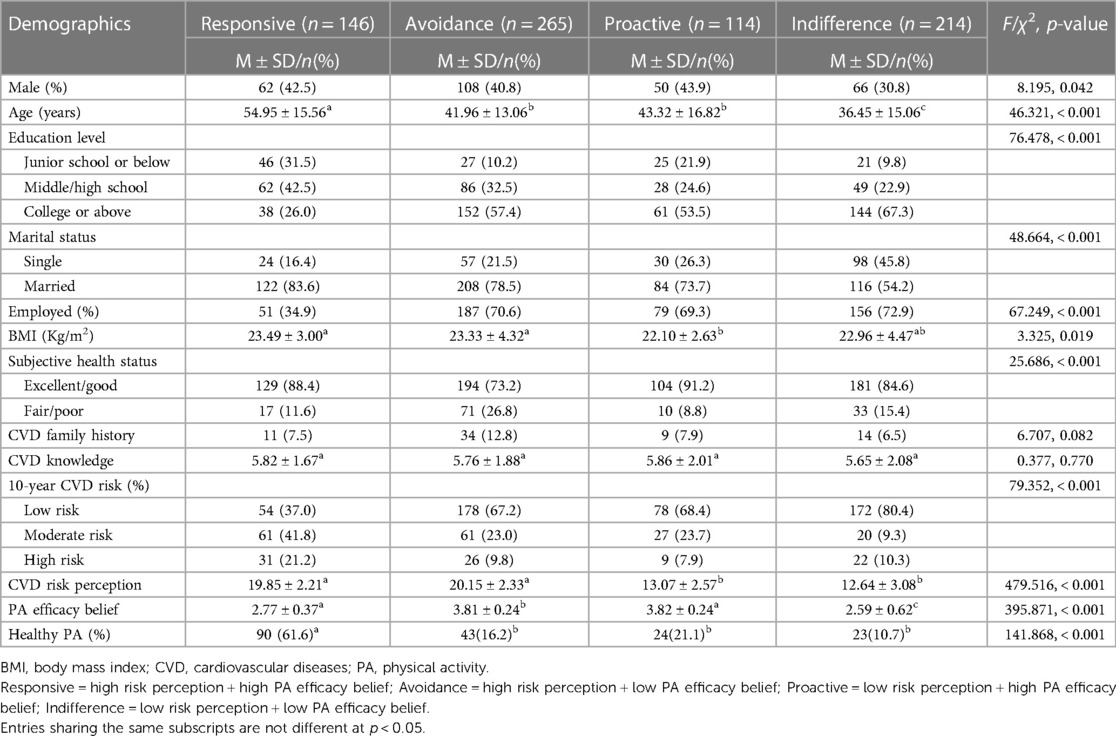
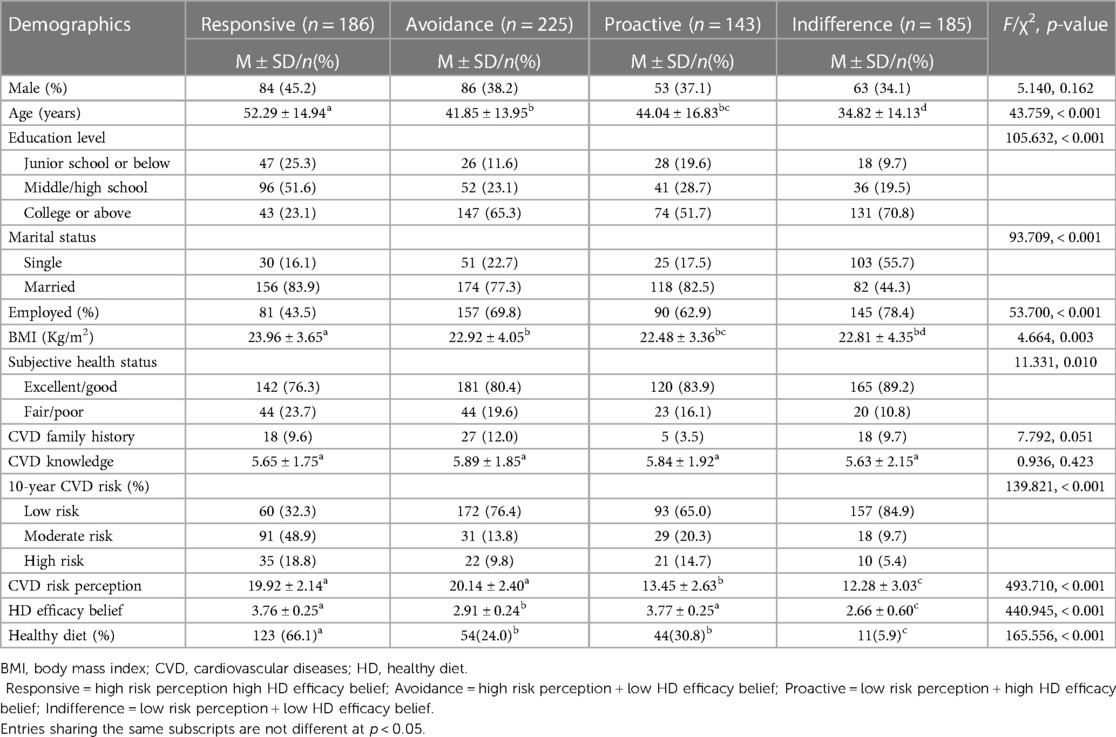
Participants’ characteristics among the four RPA groups
The participants were classified into four distinct groups according to their CVD risk perception and healthy PA efficacy belief scores: responsive (n = 146), avoidance (n = 265), proactive (n = 114), and indifference (n = 214), as shown in Table 1; similarly, the RPA groups for healthy diet are shown in Table 2. H1 proposed that responsive individuals show the highest level of health behaviors while the indifferent group presented the lowest. To examine H1, we performed Chi-square tests to explore the difference in physical activity and healthy diet among the four RPA groups. The results showed a significant difference in healthy physical activity (χ2 = 141.868, p < 0.001) and diet (χ2 = 165.556, p < 0.001) across groups. Post hoc tests clarified that the proportion of participants who engaged in healthy physical activity in the responsive group (61.6%) was significantly higher than that in the other three groups, with no significant difference between these three groups. The proportion of participants with a healthy diet in the responsive group (66.1%) was significantly higher than that in the other three groups and the proactive group and avoidance group were significantly higher than the indifference group. Thus, the results were partly consistent with H1.
Also, we examined the differences in demographic characteristics across the RPA groups. The results showed a significant difference except for CVD family history and CVD-related knowledge among RPA groups of healthy physical activity, while a significant difference was also found among RPA groups of healthy diet except for gender, CVD family history, and CVD-related knowledge (Tables 1, 2).
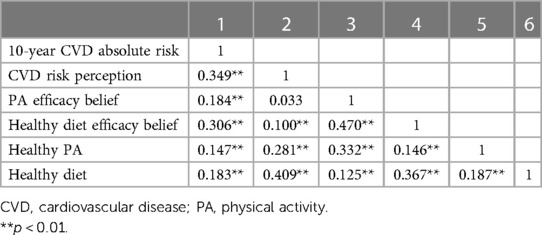
Correlation analysis
The distribution of 10-year CVD absolute risk, CVD risk perception, PA efficacy belief, and healthy diet efficacy belief was non-normal (Shaprio-Wilk test, P < 0.001); additionally, healthy PA and healthy diet data were ordinal in nature. Consequently, Spearman's correlation analysis was performed. The correlations between variables are shown in Table 3, which provides the basis for further testing the hypotheses. Ten-year CVD absolute risk, CVD risk perception, PA efficacy, healthy diet efficacy belief, healthy PA, and healthy diet were in pairwise correlation with each other significantly, except for no relationship being found between CVD risk perception and PA efficacy belief.
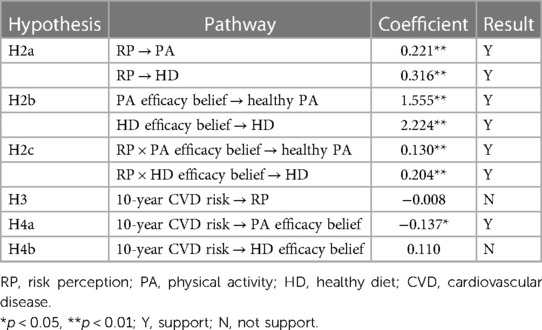
Verification results of hierarchical regressions
The effects of control variables were examined first (block 1), Subsequently, the main factors containing CVD risk perception and efficacy belief (block 2), the interaction of risk perception and efficacy belief (block 3) were added to test the main and moderating effects. The results of multiple regression for risk perception, efficacy belief and health behaviors are shown in Table 4. We found that risk perception was positively associated with healthy PA (OR = 1.247, 95% CI = 1.178,1.321), and healthy diet (OR = 1.372, 95% CI = 1.290,1.460). In addition, the efficacy belief was positively associated with healthy PA (OR = 4.734, 95% CI = 3.200,7.005), and healthy diet (OR = 9.244, 95% CI = 5.698,14.995). The results were consistent with H2a and H2b.
H2c predicted interaction effects between CVD risk perception and efficacy belief on health behaviors, namely that the relationship among risk perception and health behaviors would strengthen along with efficacy belief. The results revealed an interaction effect exist between risk perception and efficacy belief on healthy PA (OR = 1.138, 95% CI = 1.043,1.242), as well as healthy diet (OR = 1.226, 95% CI = 1.090,1.380).
Path analysis by means of regression was used to test the relationships among 10-year absolute CVD risk, CVD risk perception, efficacy belief, and healthy behaviors, so as to verify the hypothesis. The results are shown in Table 5. The findings indicated that only a 10-year CVD risk affects PA efficacy belief positively. The results of multiple regression are shown in the Supplementary Tables S2, S3.
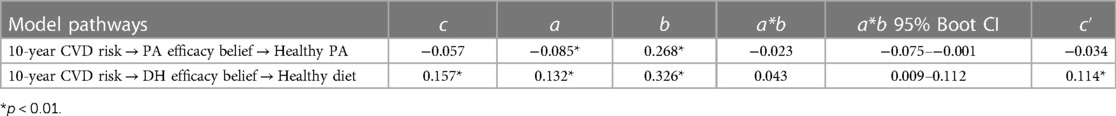
Mediating effect test
The mediating effect was conducted on the condition of controlling variables. The 95% confidence intervals were obtained by Bootstrap 5,000 times sampling correction (Table 6). The results suggested that 10-year CVD risk predicts a healthy diet, while there was no significance for PA efficacy belief. After the mediating variable HD efficacy belief was included, the predictive effect remained significant. Besides the direct effect of a 10-year CVD risk on healthy diet, the mediating effect of efficacy belief was non-zero, which indicates that a 10-year CVD risk predicts healthy diet not only directly but also indirectly through the mediating effect of efficacy belief. Thus, efficacy belief partially mediates the effect of 10-year CVD risk on a healthy diet. As for healthy PA, after the mediating effect HD efficacy belief was included, the direct effect of 10-year CVD risk on healthy PA decreased while the efficacy belief had a significant positive predictive effect on healthy PA. Therefore, efficacy belief fully mediates the effect of 10-year CVD risk on healthy PA.
Discussion
As we know, this study is the first to investigate the relationship between CVD risk perception, efficacy belief, and healthy behaviors containing healthy physical activity and healthy diet under the RPA framework among the Chinese population at risk for CVD. Consistent with RPA, CVD risk perception and efficacy belief were positively associated with healthy physical activity and healthy diet behaviors. Moreover, an interaction effect between CVD risk perception and efficacy belief in healthy physical activity/healthy diet behaviors was confirmed. In detail, there was a significant association between CVD risk perception and healthy behaviors, but only when the individual had a higher level of efficacy belief. We also verified that the actual health behavior difference was significant among RPA groups, and the responsive group was higher than the other three groups in healthy physical activity and healthy diet. In extending the RPA framework from an individual actual CVD risk perspective, our findings revealed that efficacy belief mediates the predictive effect of 10-year CVD risk on health behavior. This compensation addressed the previously identified lack of individual correlation resulting from the absence of actual CVD risk in a previous study (31). In summary, our findings not only contribute to the current literature on the role of the RPA framework in promoting cardiovascular disease (CVD) prevention behaviors, but also offer valuable insights for developing communication strategies that effectively target the CVD-risk population, particularly adults with a younger age and higher education level, and promote healthy behaviors for CVD prevention.
Efficacy belief of the original RPA framework refers to an individual's confidence and competence to engage in preventive behaviors to avert the threat, as well as their belief in the effectiveness of these behaviors to reduce it (21). The preventive behaviors of CVD include not only lifestyle changes, but also preventive medication adherence and self-health monitoring (38), while individuals may have varying levels of commitment toward different types of behavior depending on their personal values and priorities (62). Thus, we specifically designated the efficacy belief of physical activity and a healthy diet to ensure correct measurement, and then RPA groups on healthy PA and a healthy diet were created respectively. In addition, we classified individuals into four distinct groups based on their CVD risk perception and PA/healthy diet efficacy belief and compared their actual physical activity and healthy diet behavior. The results showed a significant difference in healthy physical activity (χ2 = 141.868, p < 0.001) and healthy diet (χ2 = 165.556, p < 0.001) across groups. In particular, the responsive group reported the highest ratio of healthy PA and healthy diet, whereas the indifference group reported the lowest. Our findings were consistent with the RPA framework's prediction.
We also observed different profiles of four RPA groups on individuals’ characteristics, such as age, education level, marital status, employment status, BMI, and subjective health status. In particular, the indifference group had the highest proportion of younger, better educated, single, employed, and poor health status, meaning that these individuals were likely to perceive low CVD risk and efficacy belief toward both PA and healthy diet, as well as rarely engaged in healthy behaviors. Those findings suggest that more attention should be focused on young people with CVD risk to improve their understanding of CVD risk and belief in behavior change, through effective risk communication and behavior counseling interventions to promote adherence to a healthy lifestyle (63, 64). However, we did not find significant differences in CVD family history among the four groups. The avoidance group shared the highest proportion of CVD family history indicating that individuals with a family member diagnosed with CVD could heighten their perception of risk, but perceived efficacy was insufficient to motivate them to perform preventive behaviors (65). Some individuals may perceive that their predisposition to certain health conditions is inescapable, and modifying their lifestyle choices may not alter their family history. While there were no significant differences in CVD-related knowledge among the four RPA groups, we found that the indifference group had the lowest level of knowledge as well as the lowest likelihood of engaging in CVD prevention behaviors. These results suggest that increasing CVD-related knowledge may not be sufficient in motivating individuals to engage in preventive behaviors, particularly for those who are indifferent. Our study also highlights the importance of assessing an individual's family CVD history and CVD-related knowledge, that information could provide valuable insight for effective prevention strategies (66).
In examining the core premise of the RPA framework, namely the interaction effect of risk perception and efficacy belief on healthy behavior, we detected a significant interaction effect between risk perception and efficacy belief. That is to say, individuals were more likely to act upon their perceived risk engaging in healthy physical activity and healthy diet against CVD when they perceived higher efficacy, as theorized by Rimal et al. (21). Previous RPA investigations have verified the risk perception/efficacy belief interactions for HIV prevention (24), cancer prevention (25, 26), and self-precaution against COVID-19 (30), although the interaction effect of pregnancy risk perception and leisure-time physical activity efficacy belief was not found, the results also suggested that efficacy belief appeared important in facilitating greater levels of pregnancy leisure-time physical activity (32). In addition, Rains et al. tailored messages for diabetes screenings according to baseline RPA groups, and the results revealed that participants who received matching messages reported greater willingness to engage in self-protective behavior (27). These researches revealed the theoretical and practical value as a guidance to promote self-protective behavior.
We also tested the relationships among 10-year absolute CVD risk, CVD risk perception, efficacy belief, and healthy behaviors, and the results showed that efficacy belief mediated the effect of 10-year CVD risk on healthy PA/diet. However, we did not find a similar mediating effect for risk perception, though they were all positively correlated with each other. These results suggest that early CVD risk screening is crucial, but simply identifying objective risks is not enough. It is equally important to ensure individuals have a proper understanding of their personal risk and are provided tailored support that meets their needs and preferences to encourage healthy behaviors. Particularly, the prevalence of cardiovascular metabolic risk is on the rise for young individuals; providing risk education and behavioral counseling during the early stages of college education or workforce transition can enable young individuals to engage in preventative measures and adopt healthy habits for their overall well-being (31).
Implications and limitations
Implication for future research
Our findings provide some valuable clues for future studies. There is a pervasive prevalence of cardiovascular disease risk worldwide and an inadequate amount of action is being taken to promote healthy lifestyle habits. Our study confirms that risk perception and efficacy beliefs positively influence individuals' health-promoting behavior. Additionally, efficacy beliefs play a significant mediating role in the relationship between objective risk scores and health behaviors. On one hand, the study enhances our understanding of the link between objective CVD risk, risk perception, efficacy beliefs, and health behavior. On the other hand, from the perspective of the RPA framework, this study illuminated specific factors that influence individuals' health behaviors, such as age, education level, and health status, thereby providing valuable insights for further research on the practical application of the theory.
Findings from primary care practice
Our research findings have important guidance for the primary prevention practice of CVD. A large number of guidelines have recommended that lifestyle modification is the foundation of CVD prevention to reduce cardiometabolic risk (4–6). However, encouraging the public to engage in self-health management and health promotion is one of the most challenging tasks. Our findings certified that the responsive group had the highest ratio of physical activity meeting the guideline and the healthy diet, and the indifferent group had the lowest. Therefore, primary health care should design communication and behavioral counseling intervention strategies that target the CVD risk population, so as to promote healthy behaviors for preventing CVD. In addition, we reported the characteristics in the indifferent group, and those findings suggest that more attention should be given to young people at CVD risk to improve their understanding of CVD risk and belief in behavior change, through effective interventions to promote adherence to a healthy lifestyle.
Limitations
The current study has several limitations. First, the web-based online survey used in our study accounted for the fact that the enrolled sample had a high proportion of young/high-education level respondents, so older participants without smartphones or computers were not included in our study. This may be an important source of potential sample bias. Further study will be conducted to verify the study's conclusion in a broader range of people. In addition, we did not exclude individuals who were unable to write or experienced difficulty in writing, the investigator read each question one by one aloud, and the subjects responded accordingly. The accuracy of the results would be enhanced if the subjects completed the questionnaire themselves, although we designed structured options to improve the accuracy, misclassification of some self-reported psychological measurements is possible and could have led to an overestimation of their attributable effect for behavior. Second, the cross-sectional design may capture only a snapshot of an individual's behavioral and psychosocial status. However, it is possible that the relationship between risk perception, efficacy belief, and healthy behaviors may change over time along with an individual's life circumstances, environmental factors, and exposure to health information. To address this, future research may conduct a longitudinal study with these factors on healthy behaviors at a follow-up stage. Third, although the China-PAR is a well-established and validated CVD risk prediction model in China, it does not include LDL-cholesterol. It is well-known that LDL-cholesterol is an important causal factor for CVD (67). Therefore, future studies could apply alternative risk appraisal models to verify the robustness of the results. Finally, we did not test the RPA framework for all forms of CVD prevention behaviors, such as medication adherence, health monitoring, and stress management. Future research should explore the feasibility and effectiveness of utilizing RPA in these areas to determine whether the framework can be extended beyond other CVD prevention behaviors.
Conclusion
In the current study, risk perception and efficacy belief have not only main effects but also moderating roles in predicting individuals' behavior against CVD; efficacy belief plays a moderating role in the relationship between actual CVD risk and healthy physical activity and healthy diet. Further, designing communication and behavioral counseling intervention strategies on the basis of the RPA framework has the potential to promote healthy behaviors for preventing CVD.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of the second affiliated hospital of Zhejiang University School of Medicine. The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conceptualization and Methodology: GZ and JJ; Investigation: GZ, CY, DC, LM, and XL; Data curation: CY, DC, LM, and XL; Formal analysis: GZ and ZY; paper writing: GZ; paper review: JJ. All authors contributed to the article and approved the submitted version.
Funding
This study received funding from the Health Commission of Zhejiang Province (Grant No. 2023KY759). The funder was not involved in the study design, collection, analysis, interpretation of data, writing of this paper, or decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1201789/full#supplementary-material
References
1. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. (2020) 76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010
2. Crea F. The burden of cardiovascular risk factors: a global perspective. Eur Heart J. (2022) 43(30):2817–20. doi: 10.1093/eurheartj/ehac430
3. Li S, Liu Z, Joseph P, Hu B, Yin L, Tse LA, et al. Modifiable risk factors associated with cardiovascular disease and mortality in China: a PURE substudy. Eur Heart J. (2022) 43(30):2852–63. doi: 10.1093/eurheartj/ehac268
4. Millen BE, Wolongevicz DM, de Jesus JM, Nonas CA, Lichtenstein AH. 2013 American heart association/American college of cardiology guideline on lifestyle management to reduce cardiovascular risk: practice opportunities for registered dietitian nutritionists. J Acad Nutr Diet. (2014) 114(11):1723–9. doi: 10.1016/j.jand.2014.07.037
5. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. (2019) 74(10):e177–232. doi: 10.1016/j.jacc.2019.03.010
6. Chu P, Pandya A, Salomon JA, Goldie SJ, Hunink MGM. Comparative effectiveness of personalized lifestyle management strategies for cardiovascular disease risk reduction. J Am Heart Assoc. (2016) 5(3):e002737. doi: 10.1161/JAHA.115.002737
7. van Trier TJ, Mohammadnia N, Snaterse M, Peters RJG, Jørstad HT, Bax WA. Lifestyle management to prevent atherosclerotic cardiovascular disease: evidence and challenges. Neth Heart J. (2022) 30(1):3–14. doi: 10.1007/s12471-021-01642-y
8. Xia S, Du X, Guo L, Du J, Arnott C, Lam CSP, et al. Sex differences in primary and secondary prevention of cardiovascular disease in China. Circulation. (2020) 141(7):530–9. doi: 10.1161/CIRCULATIONAHA.119.043731
9. Sun Q, Yu D, Fan J, Yu C, Guo Y, Pei P, et al. Healthy lifestyle and life expectancy at age 30 years in the Chinese population: an observational study. Lancet Public Health. (2022) 7(12):e994–e1004. doi: 10.1016/S2468-2667(22)00110-4
10. Zhang X, Lu J, Wu C, Cui J, Wu Y, Hu A, et al. Healthy lifestyle behaviours and all-cause and cardiovascular mortality among 0.9 million Chinese adults. Int J Behav Nutr Phys Act. (2021) 18(1):162. doi: 10.1186/s12966-021-01234-4
11. Neate SL, Donald A, Jelinek GA, Nag N. Experiences of and attitudes to lifestyle modification for the management of multiple sclerosis: a qualitative analysis of free-text survey data. Health Expect. (2022) 25(1):214–22. doi: 10.1111/hex.13364
12. Seear KH, Lelievre MP, Atkinson DN, Marley JV. It’s important to make changes.’ insights about motivators and enablers of healthy lifestyle modification from young aboriginal men in western Australia. Int J Environ Res Public Health. (2019) 16(6):1063. doi: 10.3390/ijerph16061063
13. Patel N, Ferrer HB, Tyrer F, Wray P, Farooqi A, Davies MJ, et al. Barriers and facilitators to healthy lifestyle changes in minority ethnic populations in the UK: a narrative review. J Racial Ethn Health Disparities. (2017) 4(6):1107–19. doi: 10.1007/s40615-016-0316-y
14. Homko CJ, Santamore WP, Zamora L, Shirk G, Gaughan J, Cross R, et al. Cardiovascular disease knowledge and risk perception among underserved individuals at increased risk of cardiovascular disease. J Cardiovasc Nurs. (2008) 23(4):332–7. doi: 10.1097/01.JCN.0000317432.44586.aa
15. Thakkar J, Heeley EL, Chalmers J, Chow CK. Inaccurate risk perceptions contribute to treatment gaps in secondary prevention of cardiovascular disease. Intern Med J. (2016) 46(3):339–46. doi: 10.1111/imj.12982
16. Vörös K, Márkus B, Hargittay C, Sisak O, Kalabay L. Perceived cardiovascular risk and attitude towards lifestyle change. Fam Pract. (2018) 35(6):712–7. doi: 10.1093/fampra/cmy028
17. Cioe PA, Crawford SL, Stein MD. Cardiovascular risk-factor knowledge and risk perception among HIV-infected adults. J Assoc Nurses AIDS Care. (2014) 25(1):60–9. doi: 10.1016/j.jana.2013.07.006
18. Ammouri AA, Neuberger G, Mrayyan MT, Hamaideh SH. Perception of risk of coronary heart disease among Jordanians. J Clin Nurs. (2011) 20(1-2):197–203. doi: 10.1111/j.1365-2702.2010.03192.x
19. Jackson ES, Tucker CM, Herman KC. Health value, perceived social support, and health self-efficacy as factors in a health-promoting lifestyle. J Am Coll Health. (2007) 56(1):69–74. doi: 10.3200/JACH.56.1.69-74
20. Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull. (2014) 140(2):511–43. doi: 10.1037/a0033065
21. Rimal RN. Perceived risk and efficacy beliefs as motivators of change: use of the risk perception attitude (RPA) framework to understand health behaviors. Hum Commun Res. (2003) 29(3):370–99. doi: 10.1111/j.1468-2958.2003.tb00844.x
22. Pask EB, Rawlins ST. Men’s intentions to engage in behaviors to protect against human papillomavirus (HPV): testing the risk perception attitude framework. Health Commun. (2016) 31(2):139–49. doi: 10.1080/10410236.2014.940670
23. Sewell WC, Patel RR, Blankenship S, Marcus JL, Krakower DS, Chan PA, et al. Associations among HIV risk perception, sexual health efficacy, and intent to use PrEP among women: an application of the risk perception attitude framework. AIDS Educ Prev. (2020) 32(5):392–402. doi: 10.1521/aeap.2020.32.5.392
24. Rimal RN, Brown J, Mkandawire G, Folda L, Böse K, Creel AH. Audience segmentation as a social-marketing tool in health promotion: use of the risk perception attitude framework in HIV prevention in Malawi. Am J Public Health. (2009) 99(12):2224–9. doi: 10.2105/AJPH.2008.155234
25. Su Y, Shi J. Extending the risk perception attitude framework to predict Individuals’ engagement in collective actions against cancer. Health Commun. (2021) 38(1):1–10. doi: 10.1080/10410236.2021.1935540
26. Rimal RN, Juon H-S. Use of the risk perception attitude framework for promoting breast cancer prevention. J Appl Soc Psychol. (2010) 40(2):287–310. doi: 10.1111/j.1559-1816.2009.00574.x
27. Rains SA, Hingle MD, Surdeanu M, Bell D, Kobourov S. A test of the risk perception attitude framework as a message tailoring strategy to promote diabetes screening. Health Commun. (2019) 34(6):672–9. doi: 10.1080/10410236.2018.1431024
28. Simonds VW, Omidpanah A, Buchwald D. Diabetes prevention among American Indians: the role of self-efficacy, risk perception, numeracy and cultural identity. BMC Public Health. (2017) 17(1):763. doi: 10.1186/s12889-017-4766-x
29. Cheng Y, Liu RW, Foerster TA. Predicting intentions to practice COVID-19 preventative behaviors in the United States: a test of the risk perception attitude framework and the theory of normative social behavior. J Health Psychol. (2022) 27(12):2744–62. doi: 10.1177/13591053211057382
30. Wang RN, Zhang YC, Wu RK, Li B, Li CW, Yu BT, et al. A study of self-precaution against the background of the COVID-19 pandemic from the perspective of risk perception attitude theory and social support. BMC Public Health. (2021) 21(1):1527. doi: 10.1186/s12889-021-11597-9
31. Napolitano MA, Tjaden AH, Bailey CP, DiPietro L, Rimal R. What moves young people? Applying the risk perception attitude framework to physical activity behavior and cardiometabolic risk. Transl Behav Med. (2022) 12(6):742–51. doi: 10.1093/tbm/ibac012
32. Connolly CP, Pivarnik JM, Mudd LM, Feltz DL, Schlaff RA, Lewis MG, et al. The influence of risk perceptions and efficacy beliefs on leisure-time physical activity during pregnancy. J Phys Act Health. (2016) 13(5):494–503. doi: 10.1123/jpah.2015-0358
33. Yang Q, Wu S. Air pollution in China: health information seeking and protective behaviors. Health Promot Int. (2020) 35(6):1495–506. doi: 10.1093/heapro/daaa017
34. Yang B, Jiang S. Intentions to seek information about E-cigarettes: perceived risk, efficacy, and smoking identity. J Health Commun. (2021) 26(5):339–49. doi: 10.1080/10810730.2021.1943728
35. Dillow MR, Walsh AG, Spellman F, Quirk M. Testing the risk perception attitude framework in the context of texting while driving. Commun Res Rep. (2015) 32(2):132–42. doi: 10.1080/08824096.2015.1016144
36. Lee M, You M. Safety behaviors to reduce risk of using chemical household products: an application of the risk perception attitude framework. Int J Environ Res Public Health. (2020) 17(5):1–14. doi: 10.3390/ijerph17051528
37. Siaki LA, Loescher LJ, Trego LL. Synthesis strategy: building a culturally sensitive mid-range theory of risk perception using literary, quantitative, and qualitative methods. J Adv Nurs. (2013) 69(3):726–37. doi: 10.1111/j.1365-2648.2012.06096.x
38. Hu D, Han Y, Ning G, Ma C. Guidelines for primary prevention of cardiovascular diseases in China. Chin J Cardiovasc Dis. (2020) 48(12):1000–38. doi: 10.3760/cma.j.cn112148-20201009-00796
39. Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. Br Med J. (2017) 357:j2099. doi: 10.1136/bmj.j2099
40. Zhang Y, Miao H, Chia Y-C, Buranakitjaroen P, Siddique S, Shin J, et al. Cardiovascular risk assessment tools in Asia. J Clin Hypertens (Greenwich). (2022) 24(4):369–77. doi: 10.1111/jch.14336
41. Jafar TH, Gandhi M, de Silva HA, Jehan I, Naheed A, Finkelstein EA, et al. A community-based intervention for managing hypertension in rural south Asia. N Engl J Med. (2020) 382(8):717–26. doi: 10.1056/NEJMoa1911965
42. Navar AM, Wang TY, Mi X, Robinson JG, Virani SS, Roger VL, et al. Influence of cardiovascular risk communication tools and presentation formats on patient perceptions and preferences. JAMA Cardiol. (2018) 3(12):1192–9. doi: 10.1001/jamacardio.2018.3680
43. Navar AM, Wang TY, Li S, Mi X, Li Z, Robinson JG, et al. Patient-perceived versus actual risk of cardiovascular disease and associated willingness to consider and use prevention therapy. Circ Cardiovasc Qual Outcomes. (2021) 14(1):e006548. doi: 10.1161/CIRCOUTCOMES.120.006548
44. Wu Z, Li ZR, Dai YQ, Zhu FY, Tan JX, Wan LH. Relationship between risk perception and lifestyle in ischemic stroke patients with H-type hypertension. Ann Palliat Med. (2020) 9(6):3731–41. doi: 10.21037/apm-20-2012
45. Zweiker D, Zweiker R, Winkler E, Roesch K, Schumacher M, Stepan V, et al. Association between subjective risk perception and objective risk estimation in patients with atrial fibrillation: a cross-sectional study. BMJ Open. (2017) 7(9):e018242. doi: 10.1136/bmjopen-2017-018242
46. Robinson N, Miller A, Wilbur J, Fogg L. Subjective versus objective estimated cardiovascular disease risk and adherence to physical activity in African American women. J Cardiovasc Nurs. (2018) 33(2):111–7. doi: 10.1097/JCN.0000000000000437
47. Kline R, Kline RB, Kline R. Principles and practice of structural equation modeling. J Am Stat Assoc. (2011) 101(12). doi: 10.1002/0470013192.bsa655
48. Hair JF, Black B, Babin BJ, Anderson R. Multivariate Data Analysis: Multivariate Data Analysis. (2011).
49. Yang X, Li J, Hu D, Chen J, Li Y, Huang J, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-PAR project (prediction for ASCVD risk in China). Circulation. (2016) 134(19):1430–40. doi: 10.1161/CIRCULATIONAHA.116.022367
50. Shmueli A. Subjective health status and health values in the general population. Med Decis Making. (1999) 19(2):122–7. doi: 10.1177/0272989X9901900202
51. Zhiting G, Jiaying T, Haiying H, Yuping Z, Qunfei Y, Jingfen J. Cardiovascular disease risk prediction models in the Chinese population- a systematic review and meta-analysis. BMC Public Health. (2022) 22(1):1608. doi: 10.1186/s12889-022-13995-z
52. Woringer M, Nielsen JJ, Zibarras L, Evason J, Kassianos AP, Harris M, et al. Development of a questionnaire to evaluate patients’ awareness of cardiovascular disease risk in England’s national health service health check preventive cardiovascular programme. BMJ Open. (2017) 7(9):e014413. doi: 10.1136/bmjopen-2016-014413
53. Guo Z, Ding C, Gao W, Hong J, Tang J, Zhang Y, et al. Psychometric properties of the Chinese version of attitudes and beliefs about cardiovascular disease risk perception questionnaire. Sci Rep. (2022) 12(1):20241. doi: 10.1038/s41598-022-24620-9
54. Yingyi L. Design of food frequency questionnaire and international physical activity questionnaire and their applications in different populations. Shanghai: Medical School of Tongji University (2007).
56. Lv J, Yu C, Guo Y, Bian Z, Yang L, Chen Y, et al. Adherence to healthy lifestyle and cardiovascular diseases in the Chinese population. J Am Coll Cardiol. (2017) 69(9):1116–25. doi: 10.1016/j.jacc.2016.11.076
57. Bassett DR. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. (2003) 35(8):1396. doi: 10.1249/01.MSS.0000078924.61453.FB
58. Fan M, Lyu J, He P. Chinese Guidelines for data processing and analysis concerning the international physical activity questionnaire. Zhonghua Liu Xing Bing Xue Za Zhi. (2014) 35(8):961–4. doi: 10.1260/1750-9548.6.4.365
59. Qu N-N, Li K-J. Study on the reliability and validity of international physical activity questionnaire (Chinese vision, IPAQ). Zhonghua Liu Xing Bing Xue Za Zhi. (2004) 25(3):265–8. doi: 10.1016/j.csr.2003.12.006
60. Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the social sciences. New York: Routledge (2003).
61. Zhonglin W, Baojuan Y. Analyses of mediating effects: the development of methods and models. Adv Psychol Sci. (2014) 22(5):731–45. doi: 10.3724/SP.J.1042.2014.00731
62. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. (1983) 51(3):390–5. doi: 10.1037/0022-006X.51.3.390
63. Patnode CD, Redmond N, Iacocca MO, Henninger M. Behavioral counseling interventions to promote a healthy diet and physical activity for cardiovascular disease prevention in adults without known cardiovascular disease risk factors: updated evidence report and systematic review for the US preventive services task force. JAMA. (2022) 328(4):375–88. doi: 10.1001/jama.2022.7408
64. Laddu D, Ma J, Kaar J, Ozemek C, Durant RW, Campbell T, et al. Health behavior change programs in primary care and community practices for cardiovascular disease prevention and risk factor management among midlife and older adults: a scientific statement from the American heart association. Circulation. (2021) 144(24):e533–49. doi: 10.1161/CIR.0000000000001026
65. Acheson LS, Wang C, Zyzanski SJ, Lynn A, Ruffin MTT, Gramling R, et al. Family history and perceptions about risk and prevention for chronic diseases in primary care: a report from the family healthware impact trial. Genet Med. (2010) 12(4):212–8. doi: 10.1097/GIM.0b013e3181d56ae6
66. Vornanen M, Konttinen H, Kääriäinen H, Männistö S, Salomaa V, Perola M, et al. Family history and perceived risk of diabetes, cardiovascular disease, cancer, and depression. Prev Med. (2016) 90:177–83. doi: 10.1016/j.ypmed.2016.06.027
67. Mortensen MB, Dzaye O, Bøtker HE, Jensen JM, Maeng M, Bentzon JF, et al. Low-density lipoprotein cholesterol is predominantly associated with atherosclerotic cardiovascular disease events in patients with evidence of coronary atherosclerosis: the western Denmark heart registry. Circulation. (2023) 147(14):1053–63. doi: 10.1161/CIRCULATIONAHA.122.061010
Keywords: cardiovascular disease, risk perception attitude framework, health behaviors, risk perception, efficacy belief, primary prevention
Citation: Guo Z, Chen Y, Zhang Y, Ding C, Li M, Xu L and Jin J (2023) Associations among risk perception, health efficacy, and health behaviors for cardiovascular disease: an application of risk perception attitude framework. Front. Cardiovasc. Med. 10:1201789. doi: 10.3389/fcvm.2023.1201789
Received: 7 April 2023; Accepted: 25 August 2023;
Published: 13 September 2023.
Edited by:
Redhwan Ahmed Al-Naggar, National University of Malaysia, MalaysiaReviewed by:
Anan Jarab, Jordan University of Science and Technology, JordanRoberto Volpe, National Research Council (CNR), Italy
© 2023 Guo, Chen, Zhang, Ding, Li, Xu and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jingfen Jin enJqemtobEB6anUuZWR1LmNu
 Zhiting Guo
Zhiting Guo Yun Chen2
Yun Chen2 Chuanqi Ding
Chuanqi Ding Jingfen Jin
Jingfen Jin