- 1College of Traditional Chinese Medicine, Changchun University of Chinese Medicine, Changchun, China
- 2Department of Cardiology, Affiliated Hospital of Changchun University of Chinese Medicine, Changchun, China
- 3Department of Geriatrics, Henan Provincial Veteran Cadres Rehabilitation Hospital, Zhengzhou, China
- 4Department of Internal Medicine, Longkou Traditional Chinese Medicine Hospital, Yantai, China
Background: The association between high-density lipoprotein cholesterol (HDL-C) and adverse cardiovascular outcomes is understudied. Based on cohort studies, the current study aimed to investigate the association of extremely high HDL-C with all-cause, atherosclerotic cardiovascular disease (CVD) mortality, and stroke risk.
Methods: A systematic literature search in Embase, PubMed, Cochrane Library, and Web of Science was performed to collect relevant cohort studies published before August 20, 2022. A random-effects model was used to pool relative risks (RRs) and 95% confidence intervals (CIs).
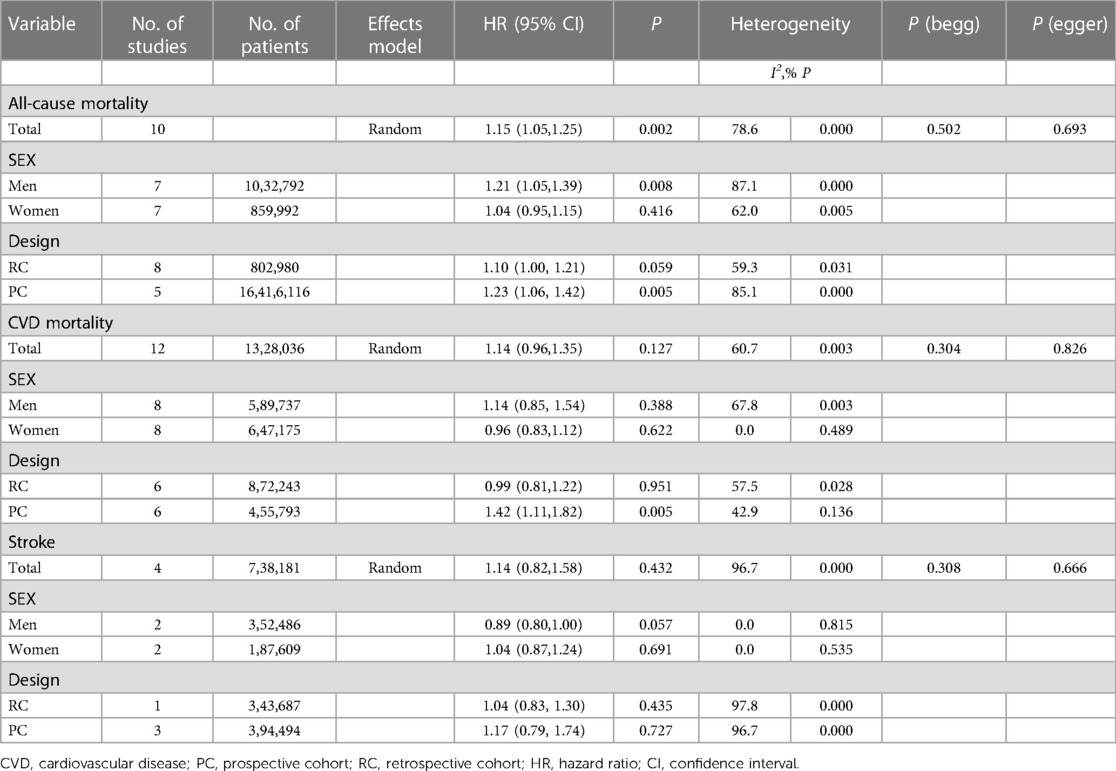
Results: A total of 17 cohort studies involving 19,630,829 participants were included, encompassing 18,547,132 total deaths (1,328,036 CVD deaths). All-cause mortality, CVD mortality, and stroke risk in the extremely high HDL-C group were increased by 15% (RR = 1.15, 95% CI:1.05–1.25), 14% (RR = 1.14, 95% CI:0.96–1.35) and 14% (RR = 1.14, 95% CI:0.82–1.58), compared to the normal HDL-C group. In subgroup analyses, extremely high HDL-C was associated with a reduced risk of CVD mortality in women and a lower risk of stroke in men compared to normal HDL-C levels.
Conclusions: The extremely high levels of HDL-C were associated with elevated risks of all-cause mortality, CVD mortality, and stroke. More well-designed studies are needed to confirm our findings.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=370201, identifier: CRD42022370201.
1. Introduction
High-density lipoprotein cholesterol (HDL-C) has been identified as a risk factor for atherosclerotic cardiovascular disease (CVD), and a close association has been demonstrated between HDL-C and adverse cardiovascular outcomes (including all-cause mortality, cardiac vascular disease death, stroke, heart failure or myocardial infarction). Traditionally, HDL-C is believed to have an inverse correlation with CVD or mortality, and it is often called as “good cholesterol” (1–3). Unfortunately, its protective effect is increasingly questioned as the latest evidence accumulates gradually. A recent study found a non-linear dose-response relationship between HDL-C levels and cause-specific mortality, which is inconsistent with previous findings (4). An extremely high level of HDL-C paradoxically increases cardiovascular morbidity or mortality, rather than protecting the heart (4–7). In clinical trials, elevated HDL-C levels after cholesteryl ester transfer protein (CETP) inhibitor administration cannot reduce the incidence of cardiovascular events (8), and average high levels of HDL-C are intimately associated with a higher risk of overall stroke, ischemic stroke and hemorrhagic stroke (9). Furthermore, a heredity study indicated that high HDL-C levels did not reduce the risk of myocardial infarction (MI) (10). However, some published articles reported no significant association between HDL-C and all-cause mortality, cardiovascular death, stroke, and MI (11–13). Therefore, the clinical significance of HDL-C for assessing cardiovascular risk remains inconclusive and debatable.
However, HDL-C is still an essential variable in cardiovascular risk prediction models. Thus, the current study aimed to investigate the association between extremely high HDL-C and all-cause mortality, CVD mortality and stroke risk using a systematic review and meta-analysis based on cohort studies.
2. Materials and methods
2.1. Literature search
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. We performed a systematic literature search in Embase, PubMed, Cochrane Library, and Web of Science to collect cohort studies investigating the association between extremely high HDL-C levels and adverse cardiovascular outcomes published before August 20, 2022. The search terms included “HDL/High Density Lipoprotein Cholesterol” AND “Mortality/Death” OR “Stroke” OR “MACE” OR “Myocardial Infarction” OR “Heart Attacks” OR” Strokes” OR” Heart Failure” AND “Cohort Studies/prospective cohort/retrospective cohort”.
2.2. Inclusion and exclusion criteria
Cohort studies were included if they (a) assessed the association between extremely high HDL-C levels and risks of all-cause and cardiovascular death, stroke, MI, and heart failure; (b) reported relative risks (RR), hazard ratios (HR), or odds ratios (OR) of 95% confidence intervals (CI); (c) included estimates of at least three categories of HDL-C measurements in the analysis; (d) considered the normal levels of HDL-C as the reference range.
Meanwhile, the following studies were excluded: case-control studies, animal experiments, irrelevant outcomes, studies with no extremely high levels of HDL-C, duplicate publications, reviews, meta-analyses, non-English language, abstracts, letters, case reports, and articles for which the full texts were not available. Besides, if several studies were published based on an identical cohort, including HDL-C levels, we included the one that reported the most abundant data and had the largest sample sizes.
2.3. Data extraction and quality assessment
Two authors (Guanwei Zhang and Jiajuan Guo) extracted the following data: first authors, year of publication, geographic location, length of follow-up, sample size, participant gender, participant age, outcome type, stated HDL-C exposure levels, number of cases with HDL-C exposure of each category, total number or person/year of HDL-C exposure of each category, RR/HR/OR with 95% CI, and potential confounders adjusted in multivariate analysis. Any disagreements were resolved through discussion. The quality of included studies was assessed using the Newcastle-Ottawa Scale, which involved the selection of study groups, the comparability of the groups, and the ascertainment of outcomes of interest (14). Each study was scored up to nine 9 stars, and those scored >7 stars were considered as having high quality.
2.4. Statistical analysis
We assumed that the HR or OR for the risk of adverse cardiovascular outcomes was roughly the same as the RR (15) in the cohort study. Multivariate-adjusted RRs with 95% CI were extracted and used for data analysis. When heterogeneity (I2) < 50%, the combined RR and 95% CI were estimated using a fixed-effects model; otherwise, a random-effects model was applied. Subgroup analysis by gender was performed, and the data reported separately were pooled using a fixed-effects model.
Cochran Q and I2 statistics were applied to assess heterogeneity (16), and P < 0.05 was considered statistically significant. Subgroup analyses by gender and experimental design were conducted. Sensitivity analysis was performed by excluding one study at a time to assess whether the results were strongly influenced by a single study. Additionally, potential publication bias was assessed using Begg's and Egger's tests.
All analyses were performed using Stata 15.1 (Stata Corp, College Station, TX, USA), and a two-sided P < 0.05 was considered statistically significant.
3. Results
3.1. Literature retrieval and study characteristics
A total of 16 reports were included in this meta-analysis (7, 9, 13, 17–29), involving 17 cohort studies. The main characteristics of the included studies are presented in Table 1. Thirteen articles (7, 13, 17–19, 21–25, 28, 29) provided estimates of all-cause mortality; eleven articles (7, 13, 17, 18, 20–24, 28, 29) reported CVD mortality estimates; four (9, 21, 26, 27) reported estimates of stroke incidence, and one reported (21) estimates of MI incidence. Overall, this meta-analysis included 19 630 829 participants and 18 547 132 deaths (1 328 036 from CVD), with a median follow-up time over 7 years.
In the entire cohort, all-cause mortality and CVD mortality were 9.05% and 6.8%, respectively, and all studies mainly involved adult populations. A total of seventeen studies included both females and males; eleven were stratified by gender (7, 13, 17, 19, 21–25, 27, 28) and one was analyzed by stroke type. Of the seventeen studies, two were from UK (17, 18), three from the US (17, 22, 23), three from Korea (19, 21, 24), four from Japan (7, 13, 27, 28), and five from China (9, 20, 25, 26, 29). Of these studies, nine mentioned the adjustment for variables such as lipid-lowering drug usage, and eight did not report information on drug usage. Analysis of study quality yielded a mean score greater than 7 on the Newcastle-Ottawa scale (ranging from 7 to 9).
3.2. Extremely high HDL-C levels and risk of all-cause mortality
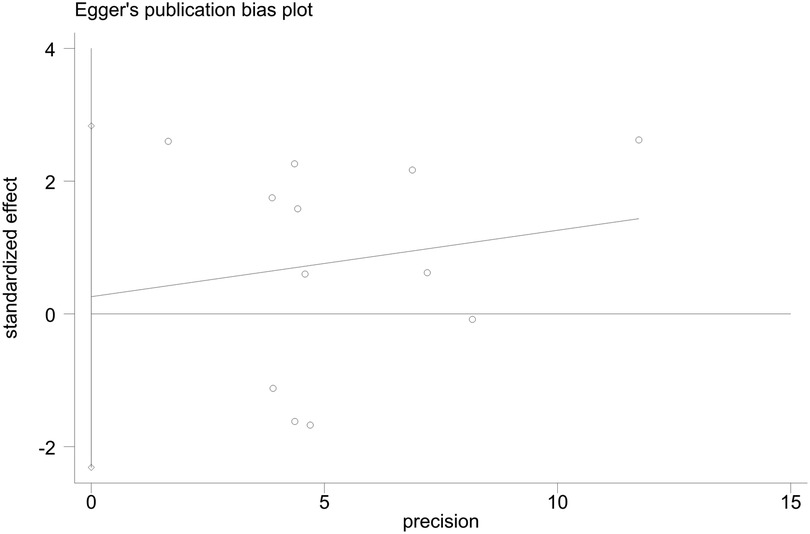
A total of 13 publications were included in the binary analysis. Extremely high levels of HDL-C were associated with a 15% increased risk of all-cause mortality, compared with normal HDL-C (RR = 1.15, 95% CI: 1.05–1.25), with significant heterogeneity (I2 = 78.6%, Pheterogeneity < 0.001, Figure 1), as shown in Tables 1, 2.
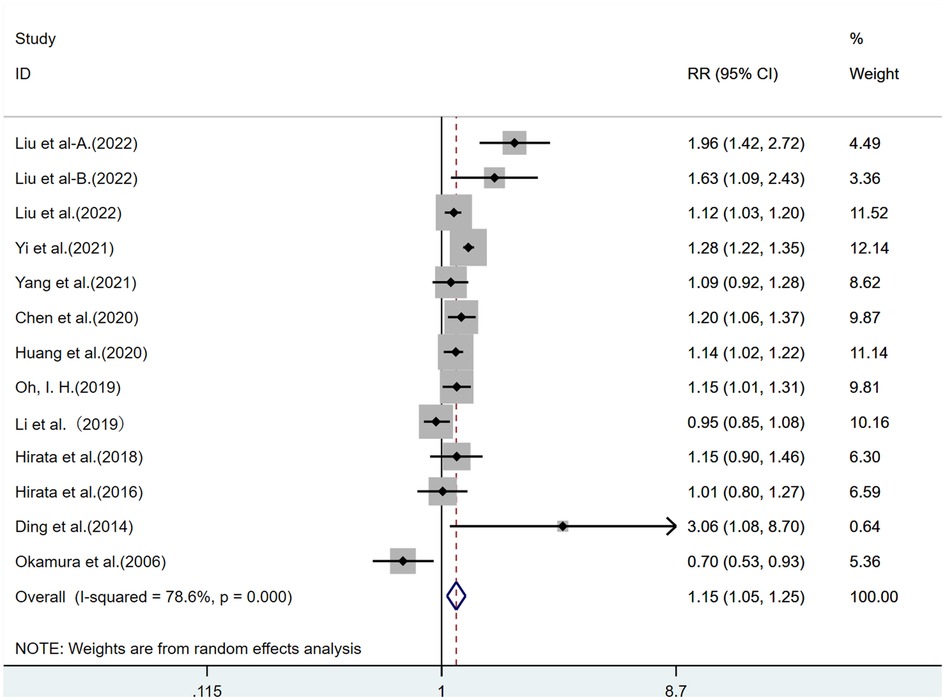
Figure 1. Risk of all-cause mortality for extremely high HDL-C levels. (CI: confidence interval; RR: relative risk. (A and B) in Liu et al-A and Liu et al-B in the figure refer to different cohort studies by Liu et al., involving different regions and populations, with independent cohort study results.).
Furthermore, to explore the source of heterogeneity, we performed subgroup analyses. In the subgroup analysis by gender, the risk of all-cause mortality of extremely high HDL-C was 1.21 times higher than that of normal HDL-C (RR = 1.21, 95% CI: 1.05–1.39) in men, and extremely high levels of HDL-C had a 1.04-fold higher risk of all-cause mortality than normal HDL-C (RR = 1.04, 95% CI: 0.94–1.15) in women. Both had significant heterogeneity (I2 > 50%, Pheterogeneity < 0.001, Supplementary Figure S1). In the subgroup analysis by Asian and Western populations, the risk of all-cause mortality of extremely high HDL-C was 1.24 times higher than that of normal HDL-C (RR = 1.24, 95% CI:1.10–1.40) in the Western population, while the risk of all-cause mortality of extremely high HDL-C is 1.04 times that of normal HDL-C (RR = 1.07, 95% CI:0.93–1.23) in the Asian population. Both had significant heterogeneity (I2 > 50%, Pheterogeneity < 0.001, Supplementary Figure S2). In the subgroup analysis by trial design, there was no substantial difference in the risk of all-cause mortality (Supplementary Figure S3).
3.3. Extremely high HDL-C levels and risk of CVD mortality
A total of 10 publications were included. The extremely high HDL-C group had a 14% increased risk of CVD mortality than the normal HDL-C group (RR = 1.14, 95% CI: 0.96–1.35), with significant heterogeneity (I2 = 60.7%, Pheterogeneity < 0.005, Table 2, Figure 2).
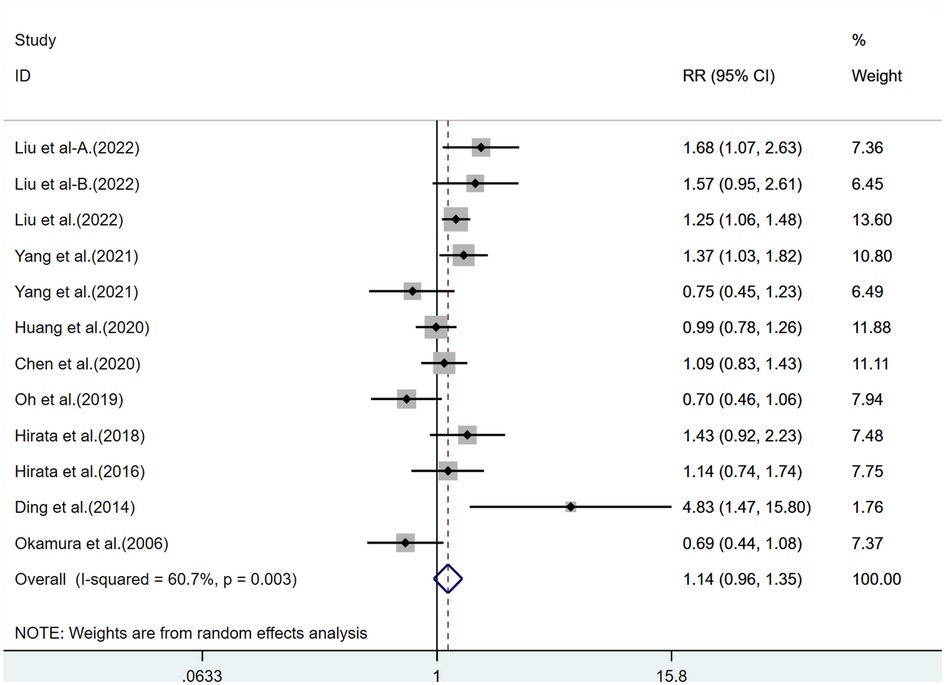
Figure 2. CVD mortality risk of extremely high HDL-C levels. (CVD: cardiovascular disease; CI: confidence interval; RR: relative risk.).
In the subgroup analysis by gender, extremely high levels of HDL-C were associated with a 14% increased risk of CVD mortality in men as compared with normal HDL-C levels (RR = 1.14, 95% CI: 0.85–1.54), with significant heterogeneity (I2 > 50%, Pheterogeneity < 0.005); Meanwhile, extremely high levels of HDL-C were associated with a 4% lower risk of CVD mortality in women as compared with normal HDL-C levels (RR = 0.96, 95% CI: 0.83–1.12), with low heterogeneity (I2 < 50%, Pheterogeneity > 0.001, Supplementary Figure S4). In the subgroup analysis by Asian and Western populations, extremely high levels of HDL-C were associated with an elevated risk of all-cause mortality in both Asian and Western populations. The heterogeneity was low in the Western population (I2 < 50%, Pheterogeneity > 0.001) but significant in the Asian population (I2 > 50%, Pheterogeneity < 0.005, Supplementary Figure S5). In the subgroup analysis by trial design, the risk of all-cause mortality in the extremely high HDL-C group was significantly increased in prospective cohort studies but decreased in retrospective cohort studies (Supplementary Figure S6).
3.4. Extremely high HDL-C levels and stroke risk
Four studies were included. Extremely high HDL-C was associated with a 14% increased risk of stroke (RR = 1.14, 95% CI: 0.82–1.58) as compared with normal HDL-C levels, with significant heterogeneity (I2 = 60.7%, Pheterogeneity < 0.001, Figure 3).
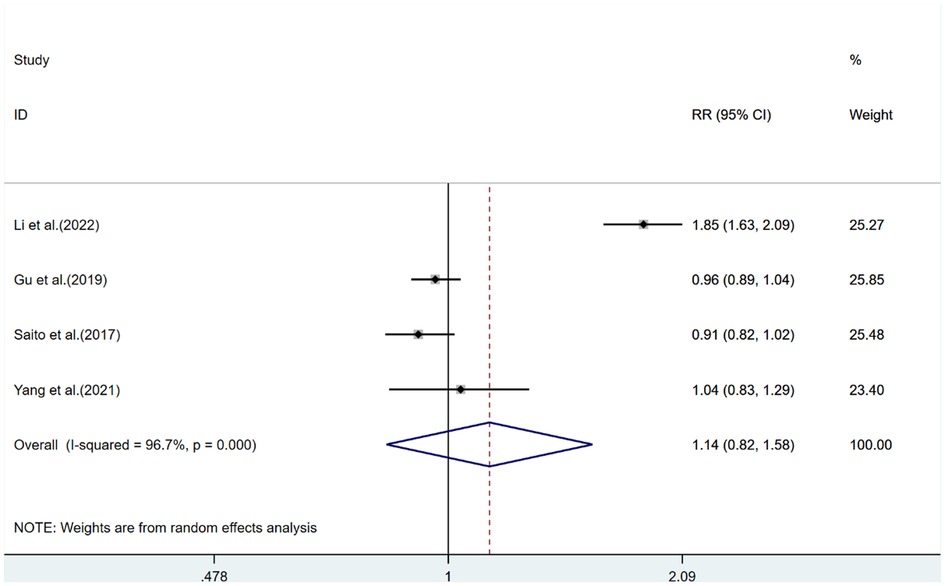
Figure 3. Stroke risk analysis for extremely high HDL-C levels. (CI: confidence interval; RR: relative risk.).
In the subgroup analysis by gender, extremely high levels of HDL-C were associated with a lower risk of stroke in men (RR = 0.89, 95% CI: 0.80–1.00) compared with normal HDL-C levels, with relatively low heterogeneity (I2 < 50%, Pheterogeneity > 0.001); women with extremely high levels of HDL-C had a stroke risk of 1.04 as compared to those with normal HDL-C (RR = 1.04, 95% CI: 0.87–1.24), with low heterogeneity (I2 < 50%, Pheterogeneity > 0.001, Supplementary Figure S7). In subgroup analysis by trial design, the risk of stroke increased in both groups (Supplementary Figure S8).
3.5. Sensitivity analysis and publication bias
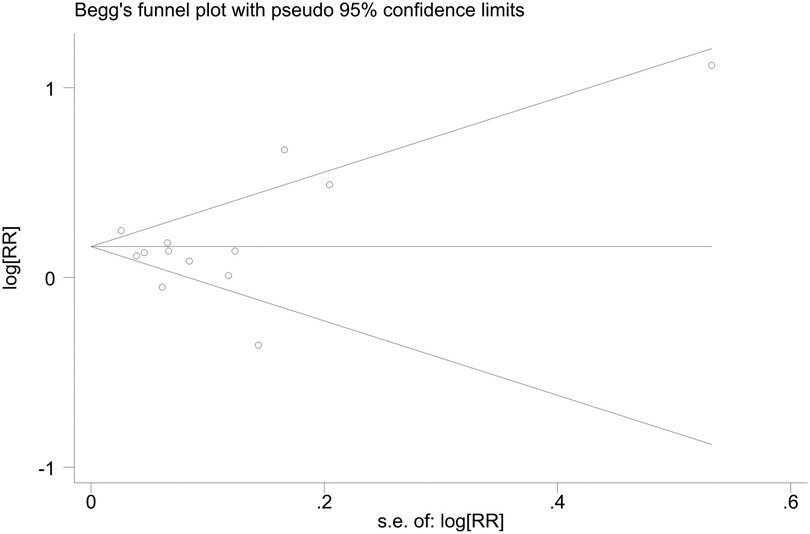
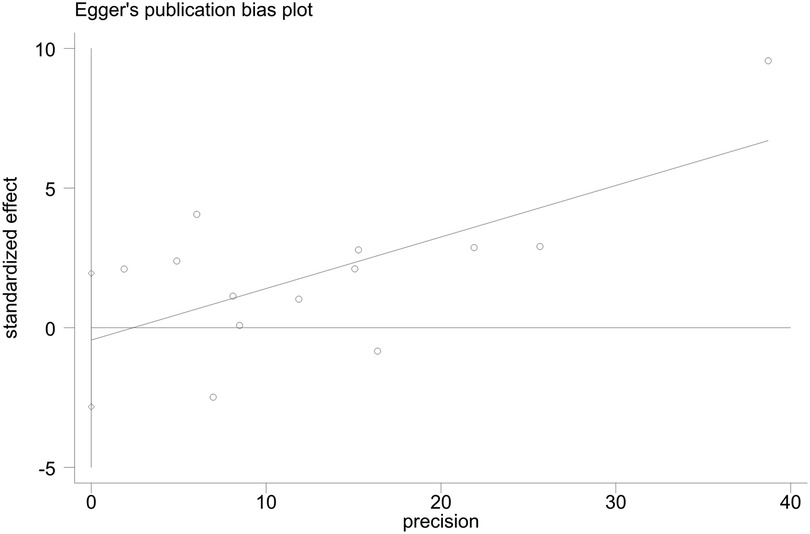
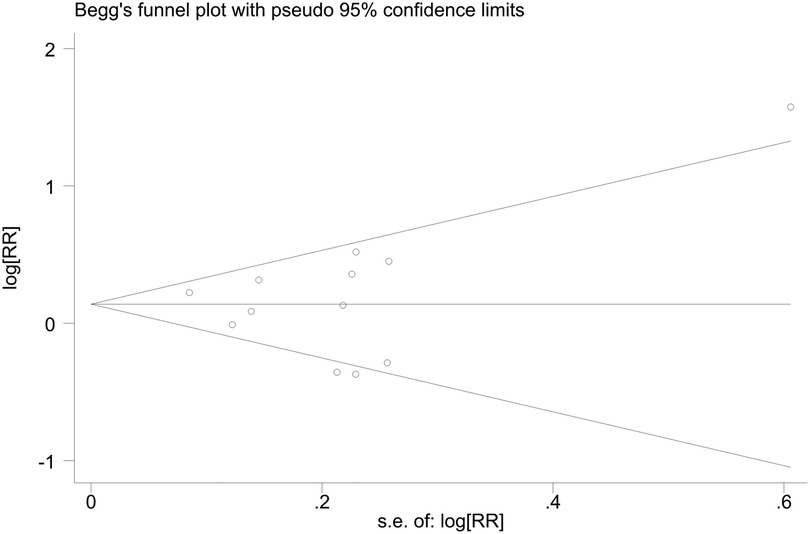
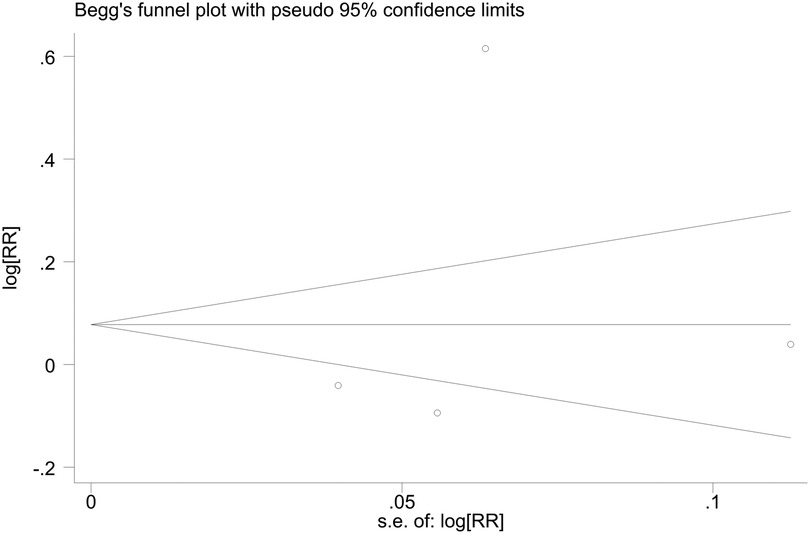
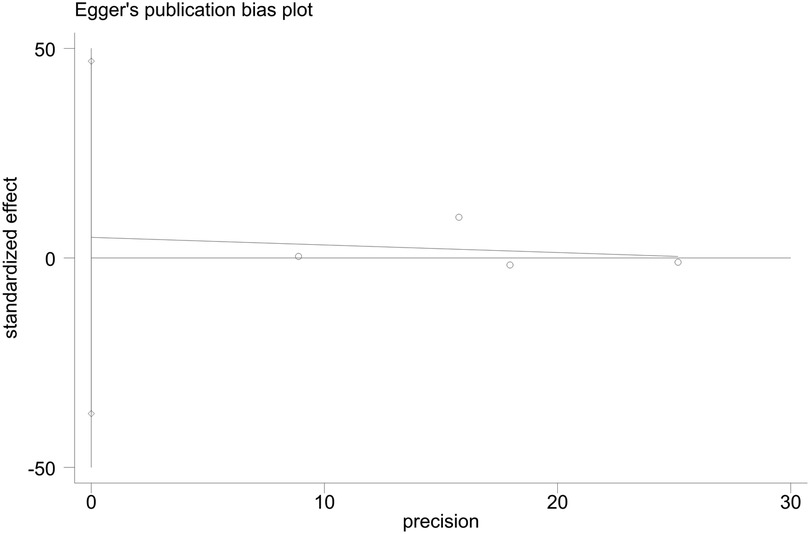
Sensitivity analyses indicated consistent results after the exclusion of each individual study (Supplementary Figures S9–S11). Neither Begger's test nor Egger's test revealed evidence of publication bias. For all-cause mortality of extremely high levels of HDL-C, Begger's test indicated P = 0.502, and Egger's test showed P = 0.693, as shown in Figures 4, 5. For CVD death of extremely high levels of HDL-C, Begger's test indicated P = 0.304 and Egger's test showed P = 0.826, as shown in Figures 6, 7. For the risk of stroke, Begger's test indicated P = 0.308 and Egger's test showed P = 0.666, as shown in Figures 8, 9.
4. Discussion
4.1. Summary of evidence
The current meta-analysis comprehensively assessed the association between extremely high HDL-C levels and adverse cardiovascular outcomes based on cohort studies. The results revealed that the risks of all-cause mortality, CVD mortality, and stroke increased by 15%, 14%, and 14% in the extremely high HDL-C group, respectively. Subgroup analysis revealed that extremely high levels of HDL-C showed differences in CVD mortality and stroke risks in men and women. Women with extremely high HDL-C had a lower risk of CVD mortality, compared with those with normal HDL-C. However, men with extremely high HDL-C had a significantly higher risk of CVD mortality. Meanwhile, the risk of stroke in women was proportional to extremely high levels of HDL-C and was higher than that in men, and the risk of stroke in men was inversely correlated with extremely high levels of HDL-C. Asian and Western populations with extremely high levels of HDL-C had an increased risk of all-cause mortality and CVD mortality, according to the subgroup analysis of Asian and Western populations.
4.2. Recent studies on the association of extremely high levels of HDL-C-mortality with adverse cardiovascular outcomes
Extremely high levels of HDL-C are found to be associated with an increased risk of all-cause and CVD mortality and stroke; however, their association has not been fully elucidated. Some studies revealed a positive association between HDL-C and CVD mortality (4, 5, 30), whereas some studies indicated no significant association between the two (12, 13, 28, 31–33). A pooled analysis of nine Japanese cohort studies including 43,407 participants aged 40–89 indicated that extremely high levels of HDL-C were highly associated with increased risks of all-cause mortality, CHD mortality, and ischemia stroke (7). Furthermore, gender differences have also been reported in previous studies, and another pooled dataset from six cohorts, including 24,440 participants aged 54–60 years, showed that the mortality of men was proportional to the level of HDL-C as compared to normal HDL-C, whereas the mortality of women increased after > 70 mg/dl, and the incidence of coronary heart disease events decreased with the increase of HDL-C level (30). Besides, a pooled analysis of 17 Canadian cohorts including 631,762 participants aged 40–105 years has indicated that a higher risk of cardiac/non-cardiac mortality was observed in individuals with extremely high HDL-C levels, and such risks remained elevated after adjustment for alcohol drinking (4).
4.3. Implications for research and practice compared with previous meta-analyses
Previous meta-analyses on HDL-C mostly applied the lowest or high levels of HDL-C as the reference range. Conversely, the current study utilized the normal level as the reference range to investigate the relationship between extremely high levels of HDL-C and adverse cardiovascular outcomes. Thus, it is possible to more clearly analyze the impact of extremely high levels of HDL-C on adverse cardiovascular outcomes, in the hope of offering some guidance for the prevention of CVD. Furthermore, the current meta-analysis involved several countries and multiple age groups, and it included the general population as the major research subject. Several subgroup analyses were performed by gender of the participants (male and female), trial design (prospective and retrospective cohort studies), and different populations (Asian and Western populations). The results of this meta-analysis provided updated summary evidence of the association between extremely high HDL-C and all-cause mortality, CVD mortality, and stroke. Subgroup analyses indicated differences in CVD mortality and stroke risks between men and women. Further verification revealed that extremely high HDL-C exerted no protective effect on cardiovascular and cerebrovascular as compared with normal levels of HDL-C, providing a reference for minimizing the risk of all-cause mortality and CVD mortality by adjusting HDL-C levels.
4.4. Underlying mechanisms
As HDL-C can reversely transport cholesterol, it can effectively reduce the accumulation of excess cholesterol. Thus, the formation of atherosclerosis is avoided (34, 35), which produces a protective effect on the cardiovascular system. However, HDL-C may have a biphasic effect. As the level of HDL-C increases, the corresponding contents or functions of HDL-C may also change. This is the reason why a higher concentration of HDL-C is not always better. The specific mechanisms underlying how elevated HDL-C levels increase the risks of all-cause mortality, CVD mortality, and stroke are still unclear. Some studies have pointed out that it may be related to genetic variation, but other studies have shown that associated genes CETP, LIPC, SCARB1, and ABCA1 (5, 36–38) can not only elevate HDL-C concentrations but also increase the risk of adverse outcomes. Another explanation is the complicated composition of HDL-C. As the concentration of HDL-C increases, the particle size, number, shape, and function or content of HDL-C may change. Such differences can produce different effects on the predictive ability of vascular events. Besides, high concentrations may not only damage and accelerate endothelial cell senescence (10), but may also lead to the retention of low-density lipoprotein particles in the arterial intima, which in turn reversely accelerates the development of atherosclerosis (39). Mendelian genetic randomization has failed to demonstrate a causal relationship between HDL and coronary heart disease, and several pharmacological trials that applied increased HDL-C levels have failed to reduce the risk of ASCVD (40–43). Several pathological conditions, such as genetic inflammatory diseases, genetic alterations, liver diseases, and endocrine diseases, may be contributing factors to extremely high HDL-C levels and cardiovascular risk [1, 38]. The pathophysiological role of extremely high HDL-C levels in the risk of adverse cardiovascular outcomes remains to be fully elucidated.
4.5. Limitations
This study also has several limitations. First, given the observational studies included in this meta-analysis, it is impossible to demonstrate a causal relationship between extremely high HDL-C and adverse cardiovascular outcomes. Second, there were limited data on the relationship between extremely high HDL-C levels and the risk of MI and heart failure in previous general population-based cohort studies, it was hard for the current work to perform corresponding analyses. Finally, residual confounding bias may be unavoidable due to unmeasured and under-measured variables.
5. Conclusions
This systematic review and meta-analysis indicated that extremely high HDL-C levels were inversely associated with all-cause mortality, CVD mortality, and the risk of stroke. Lifestyle interventions and prevention and control strategies are necessary to minimize the risks of HDL-C-related all-cause mortality, CVD mortality, and stroke. More studies are warranted to validate the inverse role of extremely high HDL-C levels in the risk of death from all-cause and CVD. Furthermore, the range of extremely high levels of HDL-C or the optimal threshold needs further exploration, which has favorable guiding significance for reducing cardiovascular risk using HDL-C intervention.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
Conceptualization: GWZ, YSH; Data curation: GWZ, HGJ, XJW; Formal analysis: GWZ, YSH, JJG, HGJ; Funding acquisition: JJG, YSH; Investigation: GWZ, HGJ, XZ; Methodology: GWZ, YSH; Project administration: JJG, GWZ, YSH; Resources: GWZ, JJG, YSH; Software: GWZ, WTJ; Supervision: YSH; Validation: GWZ, YSH; Visualization: GWZ; Roles/Writing—original draft: GWZ; Writing—review & editing: YSH All authors contributed to editorial changes in the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was funded by the project of Department of Science and Technology of JiLin Province, grant number 20200403102SF; and the Administration of Traditional Chinese Medicine of JiLin Province, grant number 2020094.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1201107/full#supplementary-material
SUPPLEMENTARY FIGURE S1
Subgroup analysis of all-cause mortality risk in men and women with very high HDL-C levels.
SUPPLEMENTARY FIGURE S2
Subgroup analysis of all-cause mortality risk in Asian and Western populations with very high HDL-C levels.
SUPPLEMENTARY FIGURE S3
Prospective and retrospective cohorts subgroup analysis of all-cause mortality risk in patients with very high HDL-C levels.
SUPPLEMENTARY FIGURE S4
Subgroup analysis of CVD mortality risk in men and women with very high HDL-C levels.
SUPPLEMENTARY FIGURE S5
Subgroup analysis of CVD mortality risk in Asian and Western populations with very high HDL-C levels.
SUPPLEMENTARY FIGURE S6
Prospective and retrospective cohorts subgroup analysis of CVD mortality risk in patients with very high HDL-C levels.
SUPPLEMENTARY FIGURE S7
Subgroup analysis of stroke risk in men and women with very high HDL-C levels.
SUPPLEMENTARY FIGURE S8
Prospective and retrospective cohorts subgroup analysis of stroke risk in patients with very high HDL-C levels.
SUPPLEMENTARY FIGURE S9
Sensitivity analysis of all-cause mortality.
SUPPLEMENTARY FIGURE S10
Sensitivity analysis of CVD mortality.
SUPPLEMENTARY FIGURE S11
Sensitivity analysis of Stroke.
SUPPLEMENTARY TABLE S1
Systematic literature review search terms and strategy.
SUPPLEMENTARY TABLE S2
Characteristics of studies included in the meta-analysis.
SUPPLEMENTARY TABLE S3
Newcastle-Ottawa Scale table.
Abbreviations
HDL-C, high-density lipoprotein cholesterol; CVD, cardiovascular disease; CETP, cholesteryl ester transfer protein; MI, myocardial infarction; RR, relative risks; HR, hazard ratios; OR, odds ratios; CI, confidence intervals; CVD, cardiovascular disease; PC, prospective cohort; RC, retrospective cohort; HR, hazard ratio.
References
1. Wu Z, Huang Z, Lichtenstein AH, Jin C, Chen S, Wu S, et al. Different associations between HDL cholesterol and cardiovascular diseases in people with diabetes mellitus and people without diabetes mellitus: a prospective community-based study. Am J Clin Nutr. (2021) 114:907–13. doi: 10.1093/ajcn/nqab163
2. Wilson PW, Abbott RD, Castelli WP. High density lipoprotein cholesterol and mortality. The framingham heart study. Arteriosclerosis. (1988) 8:737–41. doi: 10.1161/01.atv.8.6.737
3. Pekkanen J, Linn S, Heiss G, Suchindran CM, Leon A, Rifkind BM, et al. Ten-year mortality from cardiovascular disease in relation to cholesterol level among men with and without preexisting cardiovascular disease. N Engl J Med. (1990) 322:1700–7. doi: 10.1056/nejm199006143222403
4. Ko DT, Alter DA, Guo H, Koh M, Lau G, Austin PC, et al. High-density lipoprotein cholesterol and cause-specific mortality in individuals without previous cardiovascular conditions: the CANHEART study. J Am Coll Cardiol. (2016) 68:2073–83. doi: 10.1016/j.jacc.2016.08.038
5. Madsen CM, Varbo A, Nordestgaard BG. Extreme high high-density lipoprotein cholesterol is paradoxically associated with high mortality in men and women: two prospective cohort studies. Eur Heart J. (2017) 38:2478–86. doi: 10.1093/eurheartj/ehx163
6. Bowe B, Xie Y, Xian H, Balasubramanian S, Zayed MA, Al-Aly Z. High density lipoprotein cholesterol and the risk of all-cause mortality among U. S. Veterans. Clin J Am Soc Nephrol. (2016) 11:1784–93. doi: 10.2215/cjn.00730116
7. Hirata A, Sugiyama D, Watanabe M, Tamakoshi A, Iso H, Kotani K, et al. Association of extremely high levels of high-density lipoprotein cholesterol with cardiovascular mortality in a pooled analysis of 9 cohort studies including 43,407 individuals: the EPOCH-JAPAN study. J Clin Lipidol. (2018) 12:674–684.e5. doi: 10.1016/j.jacl.2018.01.014
8. Otocka-Kmiecik A, Mikhailidis DP, Nicholls SJ, Davidson M, Rysz J, Banach M. Dysfunctional HDL: a novel important diagnostic and therapeutic target in cardiovascular disease? Prog Lipid Res. (2012) 51:314–24. doi: 10.1016/j.plipres.2012.03.003
9. Li H, Qian F, Zuo Y, Yuan J, Chen S, Wu S, et al. U-shaped relationship of high-density lipoprotein cholesterol and incidence of total, ischemic and hemorrhagic stroke: a prospective cohort study. Stroke. (2022) 53:1624–32. doi: 10.1161/strokeaha.121.034393
10. Huang CY, Lin FY, Shih CM, Au HK, Chang YJ, Nakagami H, et al. Moderate to high concentrations of high-density lipoprotein from healthy subjects paradoxically impair human endothelial progenitor cells and related angiogenesis by activating rho-associated kinase pathways. Arterioscler Thromb Vasc Biol. (2012) 32:2405–17. doi: 10.1161/atvbaha.112.248617
11. Woodward M, Barzi F, Feigin V, Gu D, Huxley R, Nakamura K, et al. Associations between high-density lipoprotein cholesterol and both stroke and coronary heart disease in the Asia pacific region. Eur Heart J. (2007) 28:2653–60. doi: 10.1093/eurheartj/ehm427
12. Psaty BM, Anderson M, Kronmal RA, Tracy RP, Orchard T, Fried LP, et al. The association between lipid levels and the risks of incident myocardial infarction, stroke, and total mortality: the cardiovascular health study. J Am Geriatr Soc. (2004) 52:1639–47. doi: 10.1111/j.1532-5415.2004.52455.x
13. Okamura T, Hayakawa T, Kadowaki T, Kita Y, Okayama A, Ueshima H. The inverse relationship between serum high-density lipoprotein cholesterol level and all-cause mortality in a 9.6-year follow-up study in the Japanese general population. Atherosclerosis. (2006) 184:143–50. doi: 10.1016/j.atherosclerosis.2005.03.042
14. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford (2000). https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
15. Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. (2012) 175:66–73. doi: 10.1093/aje/kwr265
16. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
17. Liu C, Dhindsa D, Almuwaqqat Z, Ko YA, Mehta A, Alkhoder AA, et al. Association between high-density lipoprotein cholesterol levels and adverse cardiovascular outcomes in high-risk populations. JAMA Cardiol. (2022) 7:672–80. doi: 10.1001/jamacardio.2022.0912
18. Liu C, Dhindsa D, Almuwaqqat Z, Sun YV, Quyyumi AA. Very high high-density lipoprotein cholesterol levels and cardiovascular mortality. Am J Cardiol. (2022) 167:43–53. doi: 10.1016/j.amjcard.2021.11.041
19. Yi SW, Park SJ, Yi JJ, Ohrr H, Kim H. High-density lipoprotein cholesterol and all-cause mortality by sex and age: a prospective cohort study among 15.8 million adults. Int J Epidemiol. (2021) 50:902–13. doi: 10.1093/ije/dyaa243
20. Yang ZM, Wu MY, Lu JM, Zhu Y, Li D, Yu ZB, et al. HDL-C, longitudinal change and risk of mortality in a Chinese cohort study. Nutr Metab Cardiovasc Dis. (2021) 31:2669–77. doi: 10.1016/j.numecd.2021.06.004
21. Yang Y, Han K, Park SH, Kim MK, Yoon KH, Lee SH. High-density lipoprotein cholesterol and the risk of myocardial infarction, stroke, and cause-specific mortality: a nationwide cohort study in Korea. J Lipid Atheroscler. (2021) 10:74–87. doi: 10.12997/jla.2021.10.1.74
22. Huang YQ, Liu XC, Lo K, Liu L, Yu YL, Chen CL, et al. The U shaped relationship between high-density lipoprotein cholesterol and all-cause or cause-specific mortality in adult population. Clin Interv Aging. (2020) 15:1883–96. doi: 10.2147/cia.S271528
23. Chen CL, Liu XC, Liu L, Lo K, Yu YL, Huang JY, et al. U-shaped association of high-density lipoprotein cholesterol with all-cause and cardiovascular mortality in hypertensive population. Risk Manag Healthc Policy. (2020) 13:2013–25. doi: 10.2147/rmhp.S272624
24. Oh IH, Hur JK, Ryoo JH, Jung JY, Park SK, Yang HJ, et al. Very high high-density lipoprotein cholesterol is associated with increased all-cause mortality in south Koreans. Atherosclerosis. (2019) 283:43–51. doi: 10.1016/j.atherosclerosis.2019.01.035
25. Li X, Guan B, Wang Y, Tse G, Zou F, Khalid BW, et al. Association between high-density lipoprotein cholesterol and all-cause mortality in the general population of northern China. Sci Rep. (2019) 9:14426. doi: 10.1038/s41598-019-50924-4
26. Gu X, Li Y, Chen S, Yang X, Liu F, Li Y, et al. Association of lipids with ischemic and hemorrhagic stroke: a prospective cohort study among 267 500 Chinese. Stroke. (2019) 50:3376–84. doi: 10.1161/strokeaha.119.026402
27. Saito I, Yamagishi K, Kokubo Y, Yatsuya H, Iso H, Sawada N, et al. Association of high-density lipoprotein cholesterol concentration with different types of stroke and coronary heart disease: the Japan public health center-based prospective (JPHC) study. Atherosclerosis. (2017) 265:147–54. doi: 10.1016/j.atherosclerosis.2017.08.032
28. Hirata A, Okamura T, Sugiyama D, Kuwabara K, Kadota A, Fujiyoshi A, et al. The relationship between very high levels of serum high-density lipoprotein cholesterol and cause-specific mortality in a 20-year follow-up study of Japanese general population. J Atheroscler Thromb. (2016) 23:800–9. doi: 10.5551/jat.33449
29. Ding D, Li X, Qiu J, Li R, Zhang Y, Su D, et al. Serum lipids, apolipoproteins, and mortality among coronary artery disease patients. Biomed Res Int. (2014) 2014:709756. doi: 10.1155/2014/709756
30. Wilkins JT, Ning H, Stone NJ, Criqui MH, Zhao L, Greenland P, et al. Coronary heart disease risks associated with high levels of HDL cholesterol. J Am Heart Assoc. (2014) 3:e000519. doi: 10.1161/jaha.113.000519
31. Nomikos T, Panagiotakos D, Georgousopoulou E, Metaxa V, Chrysohoou C, Skoumas I, et al. Hierarchical modelling of blood lipids’ profile and 10-year (2002-2012) all cause mortality and incidence of cardiovascular disease: the ATTICA study. Lipids Health Dis. (2015) 14:108. doi: 10.1186/s12944-015-0101-7
32. Umeki Y, Adachi H, Enomoto M, Fukami A, Nakamura S, Nohara Y, et al. Serum albumin and cerebro-cardiovascular mortality during a 15-year study in a community-based cohort in tanushimaru, a cohort of the seven countries study. Intern Med. (2016) 55:2917–25. doi: 10.2169/internalmedicine.55.6931
33. Ghasemzadeh Z, Abdi H, Asgari S, Tohidi M, Khalili D, Valizadeh M, et al. Divergent pathway of lipid profile components for cardiovascular disease and mortality events: results of over a decade follow-up among Iranian population. Nutr Metab (Lond). (2016) 13:43. doi: 10.1186/s12986-016-0102-1
34. Mineo C, Shaul PW. Novel biological functions of high-density lipoprotein cholesterol. Circ Res. (2012) 111:1079–90. doi: 10.1161/circresaha.111.258673
35. Lüscher TF, Landmesser U, von Eckardstein A, Fogelman AM. High-density lipoprotein: vascular protective effects, dysfunction, and potential as therapeutic target. Circ Res. (2014) 114:171–82. doi: 10.1161/circresaha.114.300935
36. Frikke-Schmidt R. Genetic variation in the ABCA1 gene, HDL cholesterol, and risk of ischemic heart disease in the general population. Atherosclerosis. (2010) 208:305–16. doi: 10.1016/j.atherosclerosis.2009.06.005
37. Genga KR, Trinder M, Kong HJ, Li X, Leung AKK, Shimada T, et al. CETP Genetic variant rs1800777 (allele A) is associated with abnormally low HDL-C levels and increased risk of AKI during sepsis. Sci Rep. (2018) 8:16764. doi: 10.1038/s41598-018-35261-2
38. Zanoni P, Khetarpal SA, Larach DB, Hancock-Cerutti WF, Millar JS, Cuchel M, et al. Rare variant in scavenger receptor BI raises HDL cholesterol and increases risk of coronary heart disease. Science. (2016) 351:1166–71. doi: 10.1126/science.aad3517
39. Li ZH, Lv YB, Zhong WF, Gao X, Byers Kraus V, Zou MC, et al. High-density lipoprotein cholesterol and all-cause and cause-specific mortality among the elderly. J Clin Endocrinol Metab. (2019) 104:3370–8. doi: 10.1210/jc.2018-02511
40. Holmes MV, Asselbergs FW, Palmer TM, Drenos F, Lanktree MB, Nelson CP, et al. Mendelian Randomization of blood lipids for coronary heart disease. Eur Heart J. (2015) 36:539–50. doi: 10.1093/eurheartj/eht571
41. Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, Koprowicz K, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. (2011) 365:2255–67. doi: 10.1056/NEJMoa1107579
42. Lincoff AM, Nicholls SJ, Riesmeyer JS, Barter PJ, Brewer HB, Fox KAA, et al. Evacetrapib and cardiovascular outcomes in high-risk vascular disease. N Engl J Med. (2017) 376:1933–42. doi: 10.1056/NEJMoa1609581
Keywords: high-density lipoprotein cholesterol, meta-analysis, cohort studies, adverse cardiovascular outcomes, the extremely high level
Citation: Zhang G, Guo J, Jin H, Wei X, Zhu X, Jia W and Huang Y (2023) Association between extremely high-density lipoprotein cholesterol and adverse cardiovascular outcomes: a systematic review and meta-analysis. Front. Cardiovasc. Med. 10:1201107. doi: 10.3389/fcvm.2023.1201107
Received: 6 April 2023; Accepted: 15 June 2023;
Published: 27 June 2023.
Edited by:
Mohamad Navab, UCLA Health System, United StatesReviewed by:
Roberto Scicali, University of Catania, ItalyTetsuro Miyazaki, Juntendo University Urayasu Hospital, Japan
© 2023 Zhang, Guo, Jin, Wei, Zhu, Jia and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongsheng Huang bGluZ3hpMTYyMkAxNjMuY29t
 Guanwei Zhang1
Guanwei Zhang1 Yongsheng Huang
Yongsheng Huang