
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Cardiovasc. Med. , 10 July 2023
Sec. Cardio-Oncology
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1195582
Invasive cardiac lipoma is a rare type of primary cardiac tumor that is composed of adipose tissue but infiltrating the adjacent structures. It is a benign tumor that can cause significant morbidity and mortality due to its size and location within the heart. We describe a giant invasive intracardiac lipoma across atrial wall extending to the ascending aorta and the superior vena cava. This review will provide an overview of invasive cardiac lipoma, including its clinical presentation, diagnosis, and management.
Invasive cardiac lipoma is a rare, benign tumor that originates from adipose tissue and can develop within the heart. Although benign, these tumors can pose significant clinical challenges due to their infiltration to adjacent structure causing obstruction, arrhythmias, and hemodynamic instability (1, 2). The incidence of cardiac lipoma is 2.4% of all primary cardiac tumors from the report of Japanese Circulation Society, and the invasive cardiac lipoma is rarer (3). However, due to its potential for adverse outcomes, timely diagnosis and management are critical for optimal patient outcomes.
Despite its rarity, invasive cardiac lipoma remains an important clinical entity that requires prompt recognition and management (1). We report a case of typical invasive cardiac lipoma and provide an overview of the epidemiology, clinical presentation, diagnostic modalities, and management of invasive cardiac lipoma, with a focus on recent advances in surgical techniques and outcomes. By enhancing our understanding of this condition, we can improve patient outcomes and optimize management strategies for patients with invasive cardiac lipoma.
A 52-year-old female patient was admitted to the hospital due to recurring episodes of palpitations that were relieved by rest. Prior to this admission, the patient had visited a local hospital where echocardiography had suggested right atrial occupancy. Physical examination conducted after admission was non-specific. However, the electrocardiogram indicated frequent premature atrial pulses. Further evaluation by echocardiography revealed a 7.0 cm × 9.0 cm hypoechoic mass with limited motion in the right atrium, attached to the upper part of the interatrial septum with a wide base and partially protruding into the left atrium (Figure 1A). Mild tricuspid regurgitation was also noted. Computed tomography confirmed the presence of a massive intrapericardial mass occupying the interstitial space between the ascending aorta and the superior vena cava, which was poorly delineated from the right atrium (Figure 1B). The density of the mass was similar to that of subcutaneous fat, and a lipoma was suspected, although liposarcoma could not be ruled out. Due to the patient's symptomatic presentation and the potential for long-term complications, surgical removal of the mass was decided upon with the consent of the patient and family. During surgery, a large fatty tumor was discovered on the surface of the heart, almost entirely covering the right atrium and aortic root (Figure 2A). The mass was suspended for exposure of right atrium (Figure 2B). The right atrium was excised, exposing an intracardiac tumor that was attached to the atrial septum with a wide base, and infiltrated upward, penetrating the right atrial wall to form a large epicardial mass around the superior vena cava-right atrial junction and the aortic root (Figure 2C). As extensive resection was required, the defective atrium was patched using bovine pericardium (Figure 2D).The excised fatty mass was yellowish and soft, measuring approximately 7.9 cm × 8 cm (Figures 3A,B). Histopathological analysis of the specimen showed that the mass consisted predominantly of adipocytes (lipid droplets) with a moderate amount of fibrous tissue (Figure 3C). Immunohistochemical analysis revealed that the tumor was CK(−), MDM2(−), CDK-4(−), S-100(+), CD34(+), HNB45(−), Mela-A(−), 1% ki67(1%+), focal Desmin(+), and focal SMA(−), indicating a differentiated mature lipoma with mild fibrosis (Figure 4). Following surgery, the patient's palpitations subsided, and she made a rapid recovery, being discharged on the fifth postoperative day. At the six-month follow-up, there was no evidence of recurrence of the lipoma.
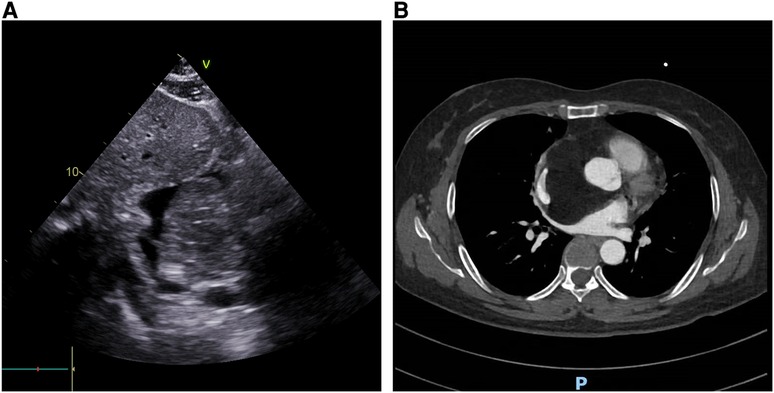
Figure 1. The imaging feature of the cardiac mass. (A) Echocardiography revealed a large mass attached to the interatrial septum; (B) CT revealed a low-density mass within the atrium, which compressed the superior vena cava and ascending aorta.
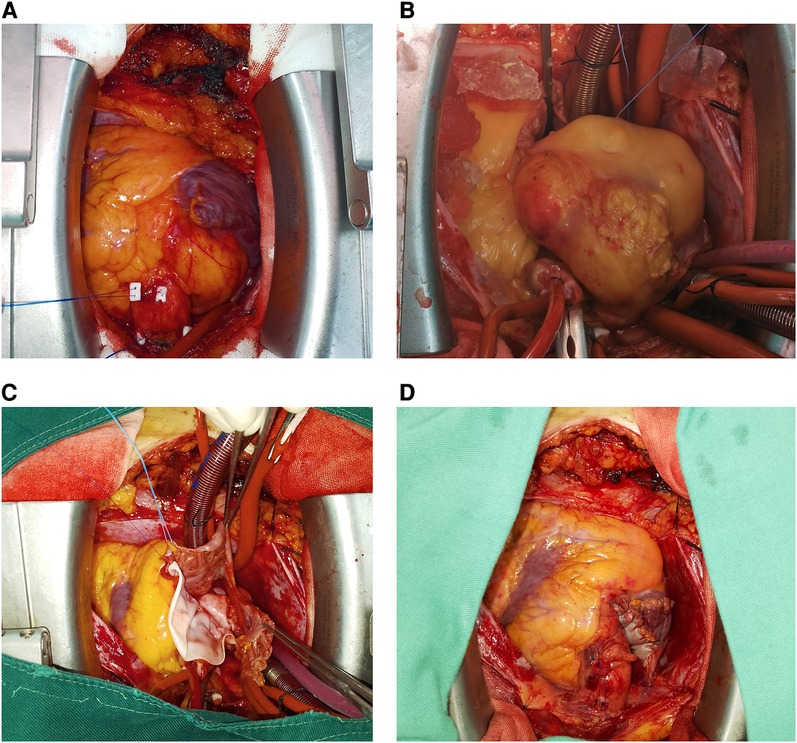
Figure 2. The surgical view of the mass. (A) A large yellow mass covering the superior vena cava and the root of the ascending aorta; (B) the mass was dissected by suspending it via surgical sutures; (C) the mass was found to originate from the interatrial septum after exposing the right atrium; (D) the right atrium was sutured.
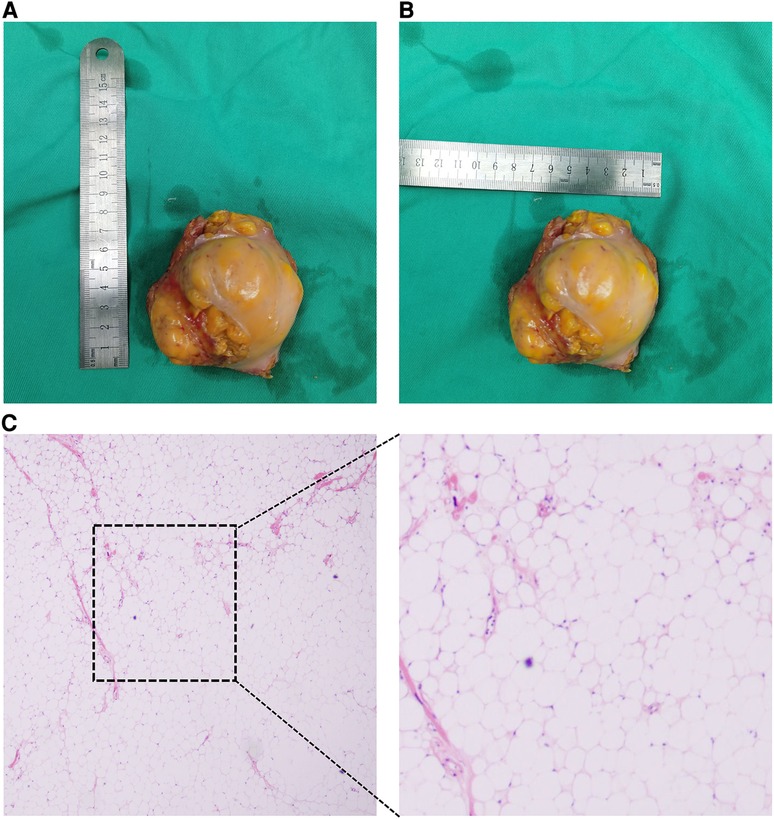
Figure 3. The macroscopical view and HE staining of resected mass. (A) Horizontal diameter of resected mass; (B) vertical diameter of resected mass; (C) HE staining result of resected mass.
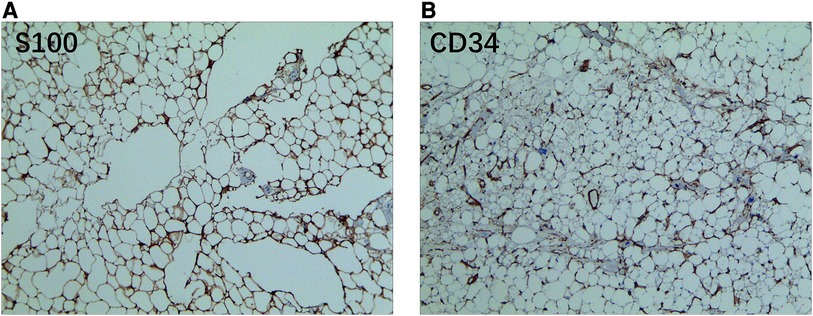
Figure 4. The immunohistochemical staining result of resected mass. (A) The mass exhibited a positive reaction to S100 staining; (B) the mass is positive to CD34 staining.
Cardiac lipomas are rare benign tumors that occur within the heart. They are composed of mature adipose tissue but are invasive like malignant tumor. This invasive lipoma originated from interatrial septum and across atrial wall form a giant lipoma covering super vena cava and root of aorta (Figure 5). Cardiac lipomas are rare tumors that account for 0.5% of primary cardiac tumors from 1976 to 1993 AFIP data (3). Invasive cardiac lipomas are even rarer, with only a few cases reported in the literatures (Table 1).
The incidence of invasive cardiac lipomas is difficult to determine, as most cases are diagnosed incidentally during autopsy or surgery. The median age at diagnosis is around 50 years, and there is a slight female predominance (1, 17).
Invasive cardiac lipomas are characterized by their ability to invade the myocardium and infiltrate surrounding structures (6, 10, 15, 22). The mechanism of invasion is not well understood, but it is thought to be related to the ability of the tumor to secrete proteolytic enzymes that break down the extracellular matrix. Invasive cardiac lipomas may also be associated with a high degree of vascularity, which can facilitate tumor growth and invasion. Based on MalaCards database, invasive lipoma, or infiltrating lipoma, is related to mesenchymal cell neoplasm and well-differentiated liposarcoma. An important gene associated with invasive lipoma is MDM2 (MDM2 Proto-Oncogene) (Figure 6). However, the majority of intracardiac lipoma is negative for MDM2 amplification (12, 39). Among its related pathways are Cellular Senescence and Regulation of retinoblastoma protein (Figure 7).
The clinical presentation of invasive cardiac lipomas is variable and often nonspecific. Patients may present with symptoms such as chest pain, dyspnea, or palpitations, which can be attributed to the tumor's effect on cardiac function (7, 21, 31). Invasive cardiac lipomas can also cause arrhythmias, valvular dysfunction, or obstruction of blood flow, depending on their location within the heart (16). In some cases, the tumor may be asymptomatic and discovered incidentally during imaging studies (32).
The diagnosis of invasive cardiac lipomas is challenging, and a high degree of suspicion is required. The initial workup usually involves a comprehensive history and physical examination, including a detailed cardiac evaluation. Imaging studies such as echocardiography, cardiac magnetic resonance imaging (MRI), and computed tomography (CT) can provide valuable information about the size, location, and extent of the tumor (6, 24). In some cases, a biopsy may be necessary to confirm the diagnosis (1, 12, 17).
The management of invasive cardiac lipomas depends on several factors, including the size and location of the tumor, the patient's clinical presentation, and the degree of invasion. In general, small tumors that are asymptomatic and do not invade the myocardium may be monitored with periodic imaging studies. However, larger tumors or those that are causing significant symptoms or hemodynamic compromise may require surgical intervention. Surgical resection is the treatment of choice for invasive cardiac lipomas (11, 31). The surgical approach may vary depending on the location of the tumor and the degree of invasion. In some cases, a partial or complete excision of the tumor may be possible, while in others, the tumor may need to be debulked to relieve symptoms or prevent further invasion (25). In rare cases, a heart transplant may be necessary if the tumor is unresectable or has caused significant damage to the heart (40).
The prognosis for patients with invasive cardiac lipomas is generally good if the tumor is diagnosed and treated early. However, the prognosis may be poor if the tumor is large, invasive, or has caused significant damage to the heart (40). In some cases, the tumor may recur after surgical resection, and long-term surveillance is necessary (7, 40).
Generally speaking, invasive cardiac lipoma is an infrequent form of primary cardiac tumor, which can give rise to substantial morbidity and mortality. The accurate identification of invasive cardiac lipoma necessitates a heightened level of suspicion, along with comprehensive imaging investigations. Surgical intervention represents the preferred therapeutic approach for managing invasive cardiac lipoma; however, the intricacies associated with tumor localization and the potential for damage to adjacent structures can pose considerable surgical challenges. Consequently, a meticulous assessment of the potential risks and benefits associated with surgery becomes imperative in the management of patients diagnosed with invasive cardiac lipoma.
Conceived and designed the study: XZ, ZC, SW Analyzed the data: XZ, XC Contributed reagents/materials/analysis tools: XZ, GL, XL Wrote the paper: XZ. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bai R, Zhang Y, Wang H, Yang J, Sun D. Invasive cardiac lipoma diagnosis based on echocardiography: case report and literature review. J Clin Ultrasound. (2021) 49(4):408–12. doi: 10.1002/jcu.22893
2. Shu S, Yuan H, Kong X, Wang J, Wang J, Zheng C. The value of multimodality imaging in diagnosis and treatment of cardiac lipoma. BMC Med Imaging. (2021) 21(1):71. doi: 10.1186/s12880-021-00603-6
3. Amano J, Nakayama J, Yoshimura Y, Ikeda U. Clinical classification of cardiovascular tumors and tumor-like lesions, and its incidences. Gen Thorac Cardiovasc Surg. (2013) 61(8):435–47. doi: 10.1007/s11748-013-0214-8
4. Nepal S, Deshmane SB, Donovan K, May A, Chaudhuri D. Invasive lipoma of the interventricular septum, a rare benign cardiac mass with atypical presentation and management. J Investig Med High Impact Case Rep. (2022) 10:23247096221104469. doi: 10.1177/23247096221104469
5. Fan W, Liao B, Li X. Lipoma across the wall of the right atrium. J Card Surg. (2021) 36(9):3390–2. doi: 10.1111/jocs.15753
6. Kadosaka T, Tsujinaga S, Iwano H, Oyama-Manabe N, Anzai T. Invasive cardiac lipoma complicating visceral inversion. JACC Case Rep. (2020) 2(10):1570–1. doi: 10.1016/j.jaccas.2020.05.061
7. Vriz O, Ahmed MM, Kharabsheha S, Aladmawi M, Alamro B, AlSomali A, et al. Ventricular tachycardia: beginning and ending fate of a benign invasive cardiac lipoma. Monaldi Arch Chest Dis. (2020) 90(3):1288. doi: 10.4081/monaldi.2020.1288
8. Shah OA, Badran A, Kaarne M, Velissaris T. Right atrial and SVC infiltrating mass-the entity of infiltrating lipoma. J Cardiothorac Surg. (2019) 14(1):210. doi: 10.1186/s13019-019-1015-7
9. Naseerullah FS, Javaiya H, Murthy A. Cardiac lipoma: an uncharacteristically large intra-atrial mass causing symptoms. Case Rep Cardiol. (2018) 2018:3531982. doi: 10.1155/2018/3531982
10. Kong F, Zhang W, Guo Q. Multiple well-differentiated cardiac liposarcoma with a concomitant myocardial lipoma: a case report. Mol Clin Oncol. (2018) 9(6):617–21. doi: 10.3892/mco.2018.1741
11. Kim YS, Lee KH, Choi SJ, Baek WK. Cardiac lipoma arising from left ventricular papillary muscle: resect or not? J Thorac Cardiovasc Surg. (2018) 156(1):244–6. doi: 10.1016/j.jtcvs.2018.01.040
12. D'Souza J, Shah R, Abbass A, Burt JR, Goud A, Dahagam C. Invasive cardiac lipoma: a case report and review of literature. BMC Cardiovasc Disord. (2017) 17(1):28. doi: 10.1186/s12872-016-0465-2
13. Saito C, Arai K, Ashihara K, Saito S, Yamazaki K, et al. Multiple synchronous ventricular lipomas. J Echocardiogr. (2016) 14(2):85–6. doi: 10.1007/s12574-016-0280-x
14. Yuan SM. Postperfusion lung syndrome and related sequelae. J Thorac Dis. (2016) 8(5):E340–4. doi: 10.21037/jtd.2016.03.44
15. Sakamoto H, Tokunaga C, Hiramatsu Y. Intramyocardial lipoma. J Card Surg. (2016) 31(11):689. doi: 10.1111/jocs.12854
16. Zhang HW, Zhong MH, Meng W, Zhang EY, Gu J, Hu J, et al. Intramuscular lipoma as an unusual cause of right ventricular outflow tract obstruction. Echocardiography. (2016) 33(2):328–9. doi: 10.1111/echo.13082
17. Fang L, He L, Chen Y, Xie M, Wang J. Infiltrating lipoma of the right ventricle involving the interventricular septum and tricuspid valve: report of a rare case and literature review. Medicine (Baltimore). (2016) 95(3):e2561. doi: 10.1097/MD.0000000000002561
18. Tanaka Y, Yoshimuta T, Yamagishi M, Sakata K. Video-assisted transmitral resection of primary cardiac lipoma originated from the left ventricular apex. Eur Heart J Cardiovasc Imaging. (2015) 16(4):401. doi: 10.1093/ehjci/jeu326
19. Barbuto L, Ponsiglione A, Del Vecchio W, Altiero M, Rossi G, De Rosa D, et al. Humongous right atrial lipoma: a correlative CT and MR case report. Quant Imaging Med Surg. (2015) 5(5):774–7. doi: 10.3978/j.issn.2223-4292.2015.01.02
20. Kilic ID, Alur I, Alihanoglu YI, Yildiz BS, Bir F, Ozcan AV. Lipoma in the right atrium. Herz. (2015) 40(1):150–2. doi: 10.1007/s00059-013-3966-0
21. Zhu J, Liu Y, Xi EP, Zhu SB. A giant symptomatic cardiac lipoma recurring at the fifth year. Int J Clin Exp Med. (2015) 8(8):14173–5.26550390
22. Wang Y, Ma C, Yang J, Gu T. Incomplete excision or postoperative hematoma: primary right ventricular intramyocardial lipoma involving the right ventricular outflow tract. J Med Ultrason (2001). (2015) 42(4):541–5. doi: 10.1007/s10396-015-0632-6
23. Girrbach F, Mohr FW, Misfeld M. Epicardial lipoma–a rare differential diagnosis in cardiovascular medicine. Eur J Cardiothorac Surg. (2012) 41(3):699–701. doi: 10.1093/ejcts/ezr020
24. Domoto S, Nakano K, Kodera K, Sasaki A, Asano R, Ikeda M, et al. Cardiac lipoma originating from the left ventricular apex diagnosed using the magnetic resonance imaging fat suppression technique: report of a case. Surg Today. (2010) 40(9):871–3. doi: 10.1007/s00595-009-4146-y
25. Joaquim MR, Braile DM, Arruda MVFD, Soares MJF. Right atrial lipoma resection and partial reconstruction using bovine pericardium. Rev Bras Cir Cardiovasc. (2009) 24(2):239–41. doi: 10.1590/S0102-76382009000200022
26. Reddy VK, Faulkner M, Bandarupalli N, Nanda NC, Singh P, Dutta R, et al. Incremental value of live/real time three-dimensional transthoracic echocardiography in the assessment of right ventricular masses. Echocardiography. (2009) 26(5):598–609. doi: 10.1111/j.1540-8175.2009.00952.x
27. Kitami A, Suzuki S, Suzuki T. Giant intrapericardial extracavitary lipoma: report of a case. Surg Today. (2005) 35(9):789–91. doi: 10.1007/s00595-005-3002-y
28. Agacdiken A, Gurbuz Y, Ciftci E, Omay O, Vural A, Ural D. Cardiac lipoma in a patient with proven arrhythmogenic right ventricular dysplasia: a case report. A huge intramyocardial lipoma. Int J Cardiovasc Imaging. (2005) 21(4):463–7. doi: 10.1007/s10554-004-7024-0
29. Yoshitatsu M, Nomura F, Katayama A, Tamura K, Katayama K, Ihara K. Intraoperative view of cardiac lipoma by using a compact camera. Asian Cardiovasc Thorac Ann. (2004) 12(1):89. doi: 10.1177/021849230401200123
30. Courtis J, Marani L, Amuchastegui LM, Rodeiro J. Cardiac lipoma: a rare cause of right-to-left interatrial shunt with normal pulmonary artery pressure. J Am Soc Echocardiogr. (2004) 17(12):1311–4. doi: 10.1016/j.echo.2004.06.031
31. Schrepfer S, Deuse T, Detter C, Treede H, Koops A, Boehm DH, et al. Successful resection of a symptomatic right ventricular lipoma. Ann Thorac Surg. (2003) 76(4):1305–7. doi: 10.1016/S0003-4975(03)00523-X
32. Chen HM, Chiu CC, Lee CS, Lai WD, Lin YT. Intractable ventricular tachycardia in a patient with left ventricular epicardial lipoma. J Formos Med Assoc. (2001) 100(5):339–42.11432314
33. Bonamini R, Rosettani E, Mangiardi L, Pinneri F, Cirillo S. A large false aneurysm of the right ventricle within a giant epicardial lipoma. Chest. (2000) 117(2):601–3. doi: 10.1378/chest.117.2.601
34. Cooper MJ, deLorimier AA, Higgins CB, Van Hare GF, Enderlein MA. Atrial flutter-fibrillation resulting from left atrial compression by an intrapericardial lipoma. Am Heart J. (1994) 127(4 Pt 1):950–1. doi: 10.1016/0002-8703(94)90573-8
35. King SJ, Smallhorn JF, Burrows PE. Epicardial lipoma: imaging findings. AJR Am J Roentgenol. (1993) 160(2):261–2. doi: 10.2214/ajr.160.2.8424329
36. Anderson DR, Gray MR. Mitral incompetence associated with lipoma infiltrating the mitral valve. Br Heart J. (1988) 60(2):169–71. doi: 10.1136/hrt.60.2.169
37. Zingas AP, Carrera JD, Murray III CA, Kling GA. Lipoma of the myocardium. J Comput Assist Tomogr. (1983) 7(6):1098–100. doi: 10.1097/00004728-198312000-00034
38. Harada K, Seki I, Kobayashi H, Okuni M, Sakurai I. Lipoma of the heart in a child. Clinical, echocardiographic, angiographic, and pathological features. Jpn Heart J. (1980) 21(6):903–10. doi: 10.1536/ihj.21.903
39. Bois MC, Bois JP, Anavekar NS, Oliveira AM, Maleszewski JJ. Benign lipomatous masses of the heart: a comprehensive series of 47 cases with cytogenetic evaluation. Hum Pathol. (2014) 45(9):1859–65. doi: 10.1016/j.humpath.2014.05.003
Keywords: cardiac, cardiac tumor, cardiac lipoma, invasive cardiac lipoma, cardiac tumor diagnosis
Citation: Zhu X, Cheng Z, Wang S, Chen X, Lu G and Li X (2023) The characteristics of invasive cardiac lipoma: case report and literature review. Front. Cardiovasc. Med. 10:1195582. doi: 10.3389/fcvm.2023.1195582
Received: 28 March 2023; Accepted: 9 June 2023;
Published: 10 July 2023.
Edited by:
Reto Asmis, Wake Forest University, United StatesReviewed by:
Nilda Espinola-Zavaleta, National Institute of Cardiology Ignacio Chavez, Mexico© 2023 Zhu, Cheng, Wang, Chen, Lu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiliang Zhu cnV6aG91emh1QGhvdG1haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.