- 1Department of Internal Medicine, College of Medicine, Ewha Womans University, Seoul, Republic of Korea
- 2Clinical Trial Center, Ewha Womans University Mokdong Hospital, Seoul, Republic of Korea
Background and aims: This study aimed to examine the association between dynamic smoking habit change and cardiovascular risk in a population newly diagnosed with hypertension, diabetes, and dyslipidemia.
Methods: This study included 49,320 individuals who had received health examinations provided by the Korea National Health Insurance Service. To determine the hazard ratios (HRs) and 95% confidence intervals (CIs) for incident major adverse cardiac events (MACE) and all-cause mortality based on dynamic smoking habit changes for 2 years, multivariable Cox proportional hazard models were utilized.
Results: During the follow-up, there were 1,004 (2.2%), 3,483 (7.6%), and 334 (0.7%) cases of myocardial infarction, stroke events, and cardiovascular death, respectively. The group with worsening smoking habits had an increased risk of cardiovascular events and death (HR: 1.33, 95% CI: 1.26–1.40) compared to improved smoking habits. The robustness of the results determined by a series of sensitivity analyses further strengthened the main findings.
Conclusions: Our findings suggest that worsening of smoking habits, even for a short period of time, may increase the risk of myocardial infarction, stroke, and cardiovascular death in patients diagnosed with hypertension, diabetes, and dyslipidemia. For the primary prevention of cardiovascular events in patients with underlying diseases, dynamic modification of smoking habits should be actively considered.
Introduction
Cardiovascular diseases (CVDs) have a notable impact on global health, leading to high rates of illness and mortality. The inadequate adoption of preventive measures and suboptimal management of risk factors associated with atherosclerotic cardiovascular disease (ASCVD) significantly contribute to this burden among adults (1, 2). According to data from the World Health Organization, smoking accounts for 10% of all CVD cases (3). Smoking increases the risk of all-cause mortality and is a cause of ASCVD (4, 5). According to the guidelines on CVD prevention, smoking cessation is recommended as the 1st step and Class I regardless of the established ASCVD status and age (6, 7). Studies on CVD risk reduction after smoking cessation have been widely conducted in persistent smokers and former smokers (8–13).
CVD risk estimates among newly diagnosed patients with hypertension, diabetes, or dyslipidemia could be improved by dynamic changing smoking habits, as well as by an objective and time-updated assessment of other CVD risk factors. We evaluated the relationship between dynamic changes in smoking habits during two biennial screenings after the diagnosis of chronic conditions, such as diabetes, hypertension, and dyslipidemia, and subsequent CVD events using large, population-based data. The data comprised of records on sociodemographic factors, health surveys, examinations, and medical claims from the National Health Insurance Service (NHIS) in the Republic of Korea. Additionally, we explored whether this relationship varied by age, body mass index, and blood pressure.
Materials and methods
Study population
For this study, we used a database provided by the Korean NHIS, which is a mandatory and universal health insurance system that covers 97% of the South Korean population. The remaining 3% with the lowest income are covered by the Medical Aid Program. As the NHIS database contains information on medical aid subjects, it represents the entire Korean population. The NHIS provides biennial health screenings for all insured South Koreans, including blood tests, chest x-ray examinations, physical examinations, and lifestyle questionnaires. We utilized data from the National Health Insurance Service-Health Screening Cohort (NHIS-HEALS Cohort), a nationwide retrospective cohort spanning from 2002 to 2015, to conduct this study. Further information regarding the NHIS cohort design, methods, and the validity of records can be found in prior research (14).
The purpose of this study was to investigate the association between dynamic changes in smoking habits during a 4-year follow-up period (from 2002 to 3 to 2006–7) and CVD (myocardial infarction, stroke, cardiovascular death) in patients newly diagnosed with chronic diseases such as HTN, DM, or dyslipidemia. The NHIS-HEALS cohort enrolled 514,795 men and women who underwent national health screenings provided by the NHIS from 2002 to 2003. Among them, this study excluded participants without national health screening data from 2002 to 2007 and a history of heart failure or CVD (myocardial infarction, stroke) or cancer. Then, during the 4-year follow-up period, we included those with newly identified HTN, DM, or dyslipidemia. Finally, a population of 49,320 patients was included in the analysis (Figure 1).
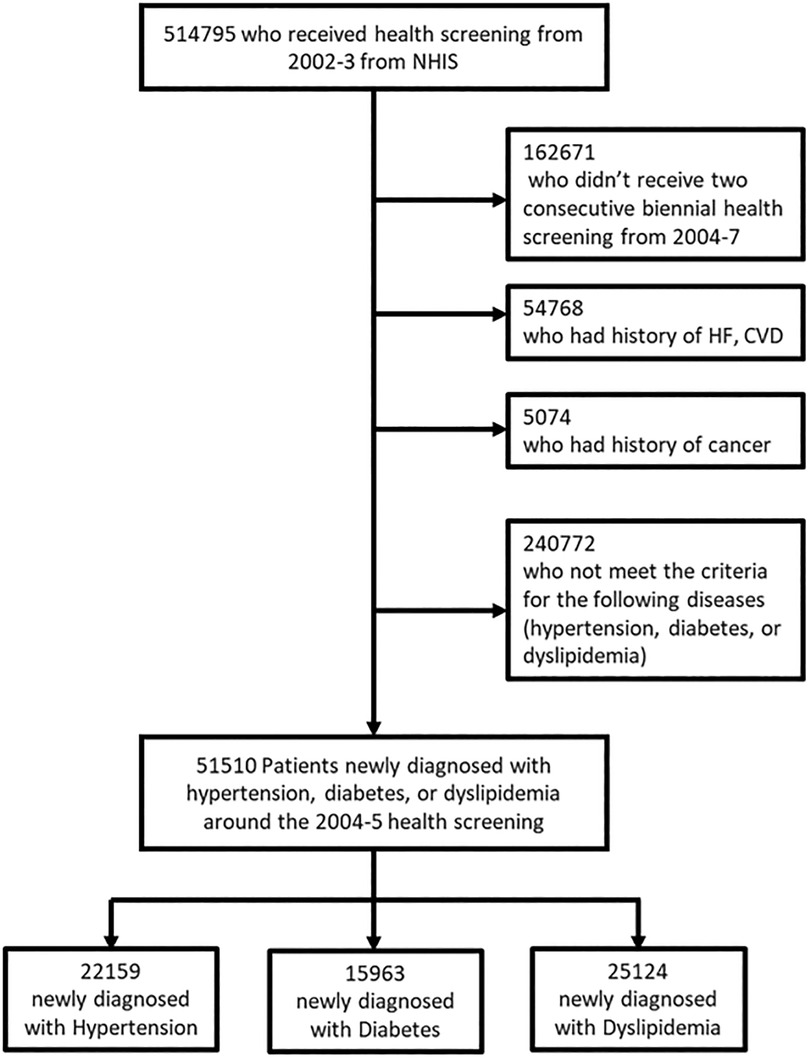
Figure 1. Flow diagram of the study population selection from the national health insurance service database.
The Institutional Review Board (IRB) at the Ewha Womans Medical College Mokdong Hospital (IRB no. EUMC-2021-11-029) and the NHIS Big Data Steering Department (NHIS-2022-2-197) approved this study. We were exempted from obtaining written consent from the participants because the NHIS data contains strictly anonymized clinical data that follow the guidelines of the Personal Data Protection Act.
ICD 10 code definition
To assess behavioral changes in smoking before and after disease diagnosis, the incident diseases were confirmed for a period of ±1year from the date of the second health check-up. According to the International Classification of Diseases, 10th revision (ICD-10), newly diagnosed patients were defined as subjects who had 2 or more outpatient visits or at least 1 hospitalization with the diagnosis code for hypertension (ICD-10: I10-I15), diabetes (ICD-10: E10-E14), or dyslipidemia (ICD-10: E78) (15, 16).
We confirmed information on the medical claims records of the NHIS to identify CVD events during the follow-up period up to December 31, 2015. We used hospitalization records to identify the causes for all cardiovascular events (composite CVD events including myocardial infarct (MI) (ICD-10: I21), stroke (ICD-10: I60–I69), and cardiovascular death (I20–I25, I71–I72, and I60–I69)).
Definition of smoking status
During each national health screening period, NHIS cohort participants completed self-administered questionnaires about their smoking habits and other lifestyle behaviors. Based on their responses from the first to third health check-up periods, participants in the biennial health checkup were categorized as current smokers or non-smokers. For the subgroup analysis, non-smokers at the time of examination were classified into never-smokers and past smokers according to whether they had a history of smoking. Accordingly, the smoking status investigated at the first health check-up was considered as the status before the disease diagnosis, and the smoking status at the third health check-up was regarded as the status after the disease diagnosis. Dynamic changes in smoking habits were defined as improved, worsened, or unchanged through the combination of smoking status at two-time points. Improvement in smoking habit was defined as quitting smoking, and worsening in smoking habit was defined as current smoking status from non-smoking or past smoking.
Key variables
As covariates, age (continuous, years), income (continuous, quintiles), body mass index status (categorical, <23.0, 23.0–24.9, and ≥25.0 kg/m2), systolic blood pressure (continuous, mmHg), total cholesterol (continuous, mg/dl), fasting serum glucose (continuous, mg/dl), cigarette smoking (categorical, non-smoker and current smoker), alcohol consumption (categorical, 0, 1–2, 3–4, and ≥5 times per week), physical activity (categorical, 0, 1–2, 3–4, and ≥5 times per week), medication use (aspirin, antihypertensive medication, antidiabetic medication, and statin; categorical, yes or no), and Charlson Comorbidity Index (continuous) at the first check-up were considered. The Charlson Comorbidity Index is a method of categorizing the comorbidities of patients based on the ICD diagnosis codes found in administrative data, such as hospital abstract data. Each comorbidity category has an associated weight (from 1 to 6), based on the adjusted risk of mortality or resource use, and the sum of all the weights results in a single comorbidity score for a patient. A score of zero indicates that no comorbidities were found. The higher the score, the more likely the predicted outcome will result in mortality or higher resource us (16). Socioeconomic factors (age, sex, income) and medical factors (medication use and comorbidity; Charlson Comorbidity Index) were obtained from the NHIS insurance eligibility and medical claims databases, respectively (17). The annual income level was classified into five groups using quintile ratios (from Q1, the lowest, to Q5, the highest). Lifestyle behaviors (physical activity and alcohol consumption), laboratory results (total cholesterol, and fasting serum glucose), and measurement (body mass index, blood pressure) were determined from the NHIS national health screening database.
Statistical analyses
The study participants’ characteristics at the beginning of the study were evaluated by expressing categorical variables as numbers and percentages and continuous variables as means and standard deviations. We determined the incidence rate (IR) by calculating the incidence per 10,000 person-years (PY) based on the number of total cardiovascular events and PY in each group, as per changes in smoking habits. The Cox proportional hazard model was used to calculate the hazard ratio (HR) and 95% confidence intervals (CIs) for CVD outcomes according to the dynamic changes in smoking habits between the two national health screening periods (2002–3 and 2006–7). In the Cox regression model, the following variables were adjusted for calculating the adjusted HRs and 95% CIs for CVD outcomes: age, income, body mass index, systolic blood pressure, total cholesterol, fasting serum glucose, cigarette smoking, alcohol consumption, physical activity, medication use (aspirin, antihypertensive medication, antidiabetic medication, statin), and comorbidity (Charlson Comorbidity Index). Multicollinearity was assessed using variance inflation factors and confirmed when the value was lower than 3. All data collection, mining, and statistical analyses were performed using SAS software (ver. 9.4; SAS Institute, Cary, NC, USA). The statistical significance was two-sided, and a P-value <0.05 was considered significant for all analyses.
Results
Baseline characteristics
Among the 49,320 participants, the mean (SD) age was 53.6 ± 8.9 years and 26,139 (53.0%) were men. About two-thirds of the individuals at the first (2002–3) and third (2006–7) health screening periods responded that they were never smokers (69.0% in the first and 69.7% in the third period, respectively). Other characteristics of the participants who underwent the two health screenings between 2002 and 2007 are listed in Table 1. Mean follow up duration was 10.9 years [interquartile range; 10.4–11.5yrs] after the screening in 2006–7.

Table 1. Characteristics of participants with a newly-diagnosed chronic disease (hypertension, diabetes, dyslipidemia) in the national health insurance service cohort who received two national health screening in 2002–3 and 2006–7.
Dynamic change in smoking habits
Of the 34,012 participants who were never smokers at the first health screening period (2002–3), most of the participants were continuously never smokers (96.3%) and only 3.7% started smoking. About 36.6% of the current smokers at the first health screening period quit smoking after a diagnosis of chronic disease, and 91.2 percent of those with aggravated smoking habits were men. Compared to the first examination, at the second examination, 3,566 patients (7.5%) showed an improvement in smoking habits, 1,345 (2.8%) had aggravated habits, and 42,832 people had no change in smoking habits.
Association of dynamic changes in smoking habits with total CVD
During 535,771 PY of follow-up, there were 5,021 total cardiovascular events, 1,122 myocardial infarctions, 3,927 stroke events, and 373 cardiovascular deaths. Smoking cessation was associated with a decline in myocardial infarction, stroke, and cardiovascular death vs. continued smoking (Table 2) in men. Similarly, cardiovascular events increased significantly during the follow-up period in the group with worsening smoking habits—new smoker or increasing the amount of smoking (adjusted HR (95% CI) myocardial infarct; 1.87 (1.35–2.59), stroke; 1.34 (1.09–1.65), cardiovascular death; 2.05 (1.19–3.55). However, there was no significant relationship between dynamic changes in smoking habits and cardiovascular events in women.
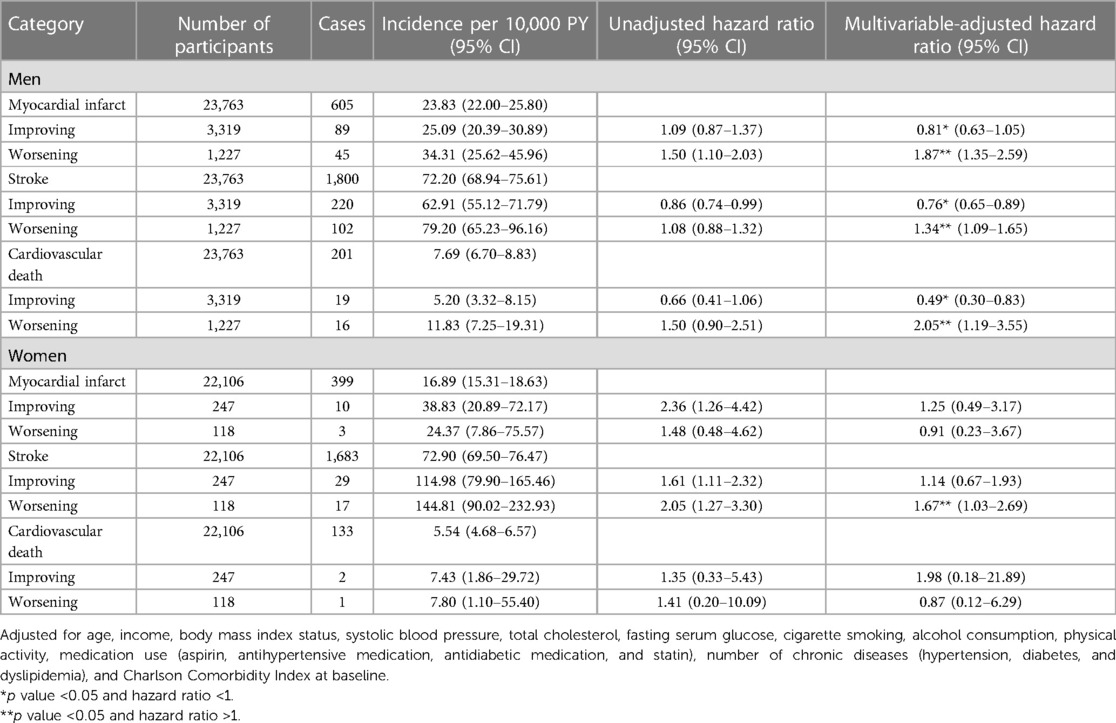
Table 2. Association of dynamic changes in smoking habit between the two biennial health screening periods (2002–3 and 2006–7) with subsequent risk of total cardiovascular disease events in the national health insurance service cohort.
A worsening smoking habit was defined as the current smoking status from non-smoking or past smoking, so cases of a worsening smoking habit can be classified as non-smoking or past smoking at baseline. Therefore, an additional analysis was conducted according to whether there was no smoking or past agreement at baseline (Table 3). For former smokers, the amount of smoking (pack*years) was corrected for analysis. Similar to the overall results, improvement in smoking habits showed a decrease in cardiovascular events and vice versa, an increase in cardiovascular events (Table 3).
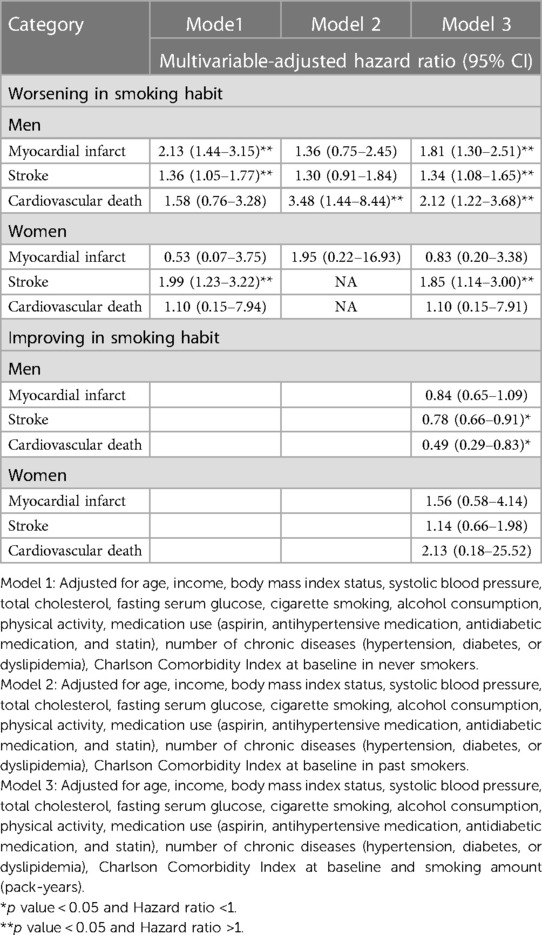
Table 3. Association between dynamic changes in smoking habits and cardiovascular events according to the smoking status (never-smoker or past-smoker) before diagnosis and smoking amount.
Subgroup analysis
A newly diagnosed hypertension male, with worsening smoking status, had increased cardiovascular events. There was a trend in decreased cardiovascular events when the smoking habit was improved, but this was not statistically significant. In male patients newly diagnosed with diabetes, both the exacerbation and improvement of smoking habits were significantly associated with stroke risk. A similar trend was observed in women diagnosed with diabetes, and stroke increased when the smoking habit worsened. In men diagnosed with dyslipidemia, improvement in smoking habits significantly reduced stroke and cardiovascular death (Figure 2, Supplementary Tables S1–3).
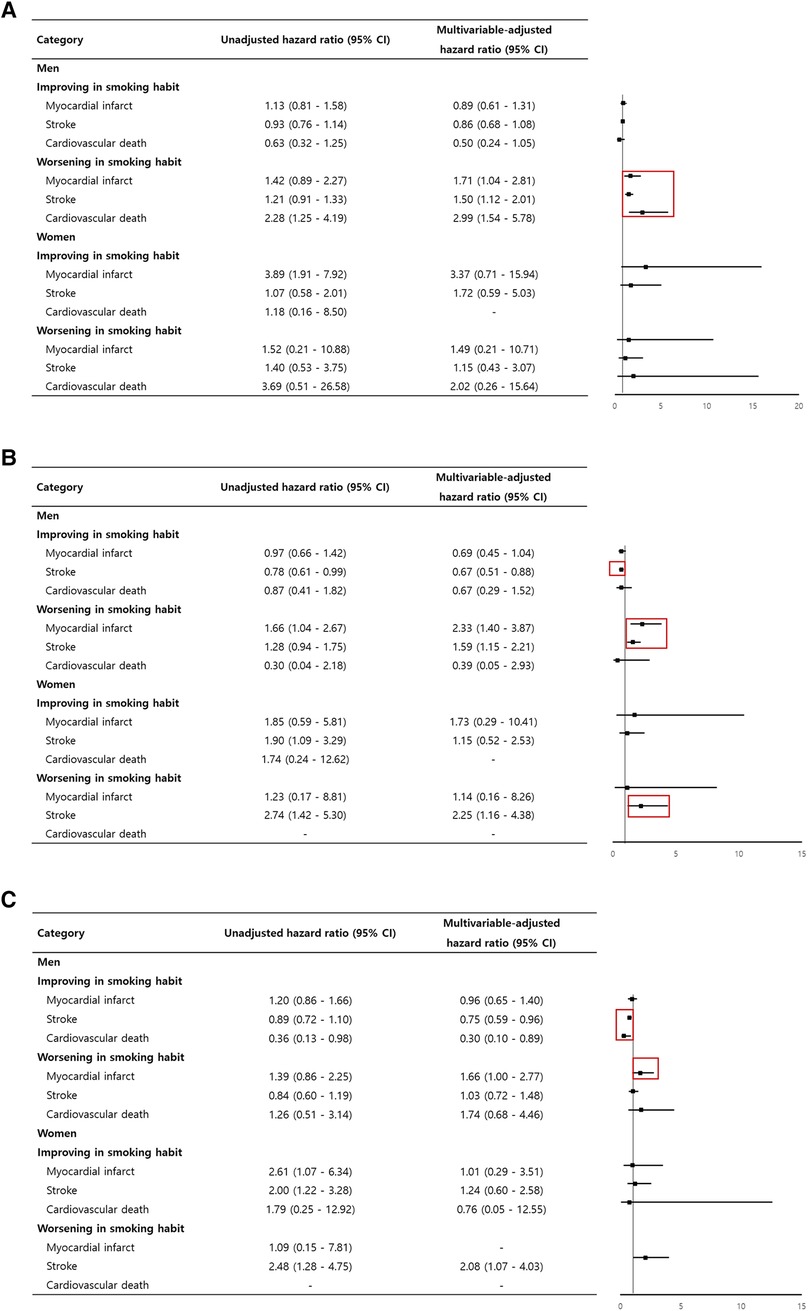
Figure 2. Adjusted hazard ratio for cardiovascular events according to dynamic changes in smoking habits in newly diagnosed (A) hypertension, (B) diabetes, (C) and dyslipidemia patients.
Discussion
This study found that compared with current smoking, smoking cessation among a newly-diagnosed disease population with higher cardiovascular risk with worsening smoking habit reaffirmed the cardiovascular benefit of smoking cessation demonstrated by others (8, 10, 11, 18, 19). It also revealed differences in statistical significance between sexes. Compared to non-smokers, the risk of stroke more than doubled in women with diabetes who started smoking in a relatively short period. The significance of this study is that it is real-world data showing the effect of changing smoking habits in patients newly diagnosed with hypertension, diabetes, or hyperlipidemia, even for a short period. Lifestyle modification for primary prevention is recommended as class I in several guidelines (AHA/ESC/ADA). The effect of lifestyle modification on diabetic patients was strongly recommended through the results obtained through randomized control and meta-analyses (20, 21).
In hypertensive patients, a randomized control trial showed that lifestyle modification was effective at preventing CVD by having a positive effect on blood pressure control. This has also been proven in several other studies, which also provided strong recommendations and high-quality evidence related to the guidelines (22–27).
In the real world, an improvement in everything in a positive direction may be limited, but other cohorts have shown that minimal improvement was sufficiently effective for cardiovascular adverse outcomes. It has been shown that the optimal correction of all aspects of lifestyle does not have a maximal effect; however, only minimal improvement is effective in low-risk subjects (28). Although this study was followed up for 10.9 years after diagnosis, it may be relatively short to confirm the cardiovascular adverse effects that can be obtained through the improvement of insulin resistance by improving exercise habits or weight control.
However, in subjects newly diagnosed with hypertension and diabetes during this period, a smoking-related lifestyle had a significant relationship with cardiovascular adverse events in newly diagnosed male patients with hypertension, and the worsening of smoking habit increased all-cause death, cardiovascular death, fatal and nonfatal myocardial infarct, and stroke. Also, in men and women diagnosed with diabetes, an increase in smoking significantly increased the risk of myocardial infarction and stroke.
A sub-analysis of overall lifestyle was also performed. For each of four items, smoking, exercise, weight control, and alcohol intake, improvements and deteriorations were evaluated (improvement plus 1, worsening minus 1), and a simple sum was calculated. If the value was positive, the overall lifestyle was seen to have improved. In this case, the relationship between lifestyle and cardiovascular events showed that the composite cardiovascular event increased in men (HR 1.16 95% CI 1.04–1.29) when the lifestyle worsened. In women, an improvement in overall lifestyle resulted in a 39% reduction in cardiovascular death (HR 0.61 95% CI 0.39–0.97). Generally, in women, overall lifestyle and especially smoking showed different associations with cardiovascular events. The reason may be that the number of analyzable numbers is small due to the small number of women who smoke.
We expected that overall lifestyle changes would lower the risk of cardiovascular events, but we did not observe such a trend. The reason can be explained as follows. In the evaluation of overall lifestyle, improvements were calculated by adding 1 point and deteriorations by subtracting 1 point. The proportion of each item involved in lifestyle improvement may vary from individual to individual. Therefore, evaluating improvement or deterioration by a simple summation method may be limited.
In the case of body weight, increases and decreases were not proportional to increases and decreases in the risk of cardiovascular events. Previous studies have demonstrated that weight gain had a protective effect on the cardiovascular system and that being slightly overweight rather than underweight had the lowest cardiovascular risk. For this reason, there are theories including lean body and muscle weight related to cardiovascular accidents that are not properly reflected in the body weight and obesity paradox (29, 30).
It is well known from previous studies that smoking contributes to an increased cardiovascular risk. These studies have demonstrated that smoking has adverse effects on cardiovascular events even when considering underlying conditions, race, and age. Conversely, it is also widely recognized that the opposite is true. Although the observation period for changes in smoking habits differs from study to study, the results of this study that worsening smoking habits in the short term after diagnosis, such as hypertension, diabetes, and hyperlipidemia, have negative effects on cardiovascular health are not only the subject of this study, but also more generally.
Limitations
First, smoking status information was obtained through a self-reported survey, which is prone to reporting bias and potential misclassification. Secondly, the NHIS database lacked additional sources of information to assess cardiovascular outcomes, such as dietary factors and left ventricular ejection fraction. In addition, as the use of administrative databases becomes more common in clinical research, there is a potential for coding inaccuracies that may introduce errors into these studies. To mitigate this issue, we employed a previously validated definition based on previous studies that utilized a sample cohort from the Korean NHIS. Also, since our study relied on real-world data, we were unable to ascertain the specific reasons behind the participants’ lifestyle modifications. Another limitation is the small number of female smokers in the study, resulting in a relatively low rate of changes in smoking habits. Additionally, compared to men, women have a lower incidence of cardiovascular events. As a result, the occurrence of cardiovascular events based on changes in smoking habits did not show statistical significance or exhibited extremely wide 95% confidence intervals for incidence rates and hazard ratios. Finally, a limitation of this study is the restricted assessment of the duration of previous smoking and the period of cessation in past smokers. Therefore, further studies with different intervention strategies for lifestyle improvement to prevent cardiovascular events are needed.
Conclusion
Our findings suggest that worsening smoking habits may increase the risk of myocardial infarction, stroke, and cardiovascular death in patients diagnosed with hypertension, diabetes, or dyslipidemia. Smoking is a risk factor for mortality and coronary heart disease in patients with hypertension, diabetes, or dyslipidemia, especially in men. Furthermore, the risk for stroke was more consistent in the hypertension male group and the newly diagnosed diabetes female group. For the primary prevention of cardiovascular events, lifestyle modifications should be actively considered.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://nhiss.nhis.or.kr.
Ethics statement
The studies involving human participants were reviewed and approved by Ewha Womans Medical College Mokdong Hospital (IRB no. EUMC-2021-11-029) and the NHIS Big Data Steering Department (NHIS-2022-2-197). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
SS and JP contributed to conception and design of the study. HL organized the database and performed the statistical analysis. SS wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2022R1A2C1093352), and by Institute of Information & communications Technology Planning & Evaluation (IITP) grant funded by the Korea government (MSIT) [No. RS-2022-00155966, Artificial Intelligence Convergence Innovation Human Resources Development (Ewha Womans University)].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1190227/full#supplementary-material
References
1. Weir HK, Anderson RN, King SM, Soman A, Thompson TD, Hong Y, et al. Peer reviewed: heart disease and cancer deaths—trends and projections in the United States, 1969–2020. Prev Chronic Dis. (2016) 13. doi: 10.5888/pcd13.160211 external icon
2. Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA. CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005–2013.
4. Mons U, Müezzinler A, Gellert C, Schöttker B, Abnet CC, Bobak M, et al. Impact of smoking and smoking cessation on cardiovascular events and mortality among older adults: meta-analysis of individual participant data from prospective cohort studies of the CHANCES consortium. Br Med J. (2015) 350. doi: 10.1136/bmj.h1551
5. Pan A, Wang Y, Talaei M, Hu FB. Relation of smoking with total mortality and cardiovascular events among patients with diabetes mellitus: a meta-analysis and systematic review. Circulation. (2015) 132(19):1795–804. doi: 10.1161/CIRCULATIONAHA.115.017926
6. Visseren FL, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice: developed by the task force for cardiovascular disease prevention in clinical practice with representatives of the European society of cardiology and 12 medical societies with the special contribution of the European Association of Preventive Cardiology (EAPC). Eur Heart J. (2021) 42(34):3227–337. doi: 10.1093/eurheartj/ehab484
7. American Heart Association. Guideline on the primary prevention of cardiovascular disease. Circulation. (2019);140:e596–646. doi: 10.1161/CIR.0000000000000678
8. Kawachi I, Colditz GA, Stampfer J, Willett WC, Manson JE, Rosner B, et al. Smoking cessation and time course of decreased risks of coronary heart disease in middle-aged women. Arch Intern Med. (1994) 154(2):169–75. doi: 10.1001/archinte.1994.00420020075009
9. Thun MJ, Carter BD, Feskanich D, Freedman ND, Prentice R, Lopez AD, et al. 50-year Trends in smoking-related mortality in the United States. N Engl J Med. (2013) 368:351–64. doi: 10.1056/NEJMsa1211127
10. Rosenberg L, Kaufman DW, Helmrich SP, Shapiro S. The risk of myocardial infarction after quitting smoking in men under 55 years of age. N Engl J Med. (1985) 313(24):1511–4. doi: 10.1056/NEJM198512123132404
11. Rosenberg L, Palmer JR, Shapiro S. Decline in the risk of myocardial infarction among women who stop smoking. N Engl J Med. (1990) 322(4):213–7. doi: 10.1056/NEJM199001253220401
12. Cook DG, Pocock SJ, Shaper AG, Kussick SJ. Giving up smoking and the risk of heart attacks: a report from the British regional heart study. Lancet. (1986) 328(8520):1376–80. doi: 10.1016/S0140-6736(86)92017-9
13. Centers for Disease Control and Prevention (CDC). Smoking-attributable mortality, years of potential life lost, and productivity losses–United States, 2000-2004. MMWR Morb Mortal Wkly Rep. (2008) 57(45):1226–8.19008791
14. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the national health insurance service-national health screening cohort (NHIS-HEALS) in Korea. BMJ open. (2017) 7(9):e016640. doi: 10.1136/bmjopen-2017-016640
15. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the national health insurance service–national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol. (2017) 46(2):e15. doi: 10.1093/ije/dyv319
16. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. (2005) 43:1130–9. doi: 10.1097/01.mlr.0000182534.19832.83
17. Noh J, Han KD, Ko SH, Ko KS, Park CY. Trends in the pervasiveness of type 2 diabetes, impaired fasting glucose and co-morbidities during an 8-year-follow-up of nationwide Korean population. Sci Rep. (2017) 7(1):1–7. doi: 10.1038/s41598-016-0028-x
18. Cook DG, Pocock SJ, Shaper AG, Kussick SJ. Giving up smoking and the risk of heart attacks: a report from the British regional heart Study. Lancet. (1986):328(8520):1376–80. doi: 10.1016/S0140-6736(86)92017-9
19. Ahmed AA, Patel K, Nyaku MA, Kheirbek RE, Bittner V, Fonarow GC, et al. Risk of heart failure and death after prolonged smoking cessation: role of amount and duration of prior smoking. Circulation. (2015) 8(4):694–701. doi: 10.1161/CIRCHEARTFAILURE.114.001885
20. Chen L, Pei JH, Kuang J, Chen HM, Chen Z, Li ZW, et al. Effect of lifestyle intervention in patients with type 2 diabetes: a meta-analysis. Metab Clin Exp. (2015) 64(2):338–47. doi: 10.1016/j.metabol.2014.10.018
21. Lin X, Zhang X, Guo J, Roberts CK, McKenzie S, Wu WC, et al. Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. (2015) 4(7):e002014. doi: 10.1161/JAHA.115.002014
22. Whelton PK, Kumanyika SK, Cook NR, Cutler JA, Borhani NO, Hennekens CH, et al. Efficacy of nonpharmacologic interventions in adults with high-normal blood pressure: results from phase 1 of the trials of hypertension prevention. Trials of hypertension prevention collaborative research group. Am J Clin Nutr. (1997) 65(2):652S–60S. doi: 10.1093/ajcn/65.2.652S
23. Whelton PK, Appel L, Charleston J, Dalcin AT, Ewart C, Fried L, et al. The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels: results of the trials of hypertension prevention, phase I. JAMA. (1992) 267(9):1213–20. doi: 10.1001/jama.1992.03480090061028
24. Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. (2003) 42(5):878–84. doi: 10.1161/01.HYP.0000094221.86888.AE
25. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. (2002) 136(7):493–503. doi: 10.7326/0003-4819-136-7-200204020-00006
26. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OS, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. (2017) 2(2):e108–20. doi: 10.1016/S2468-2667(17)30003-8
27. Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. (2001) 38(5):1112–7. doi: 10.1161/hy1101.093424
28. Chlabicz M, Jamiołkowski J, Łaguna W, Dubatówka M, Sowa P, Łapińska M, et al. Effectiveness of lifestyle modification vs. therapeutic, preventative strategies for reducing cardiovascular risk in primary prevention—a cohort study. J Clin Med. (2022) 11(3):688. doi: 10.3390/jcm11030688
29. Patnode CD, Evans CV, Senger CA, Redmond N, Lin JS. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults without known cardiovascular disease risk factors: updated evidence report and systematic review for the US preventive services task force. JAMA. (2017) 318(2):175–93. doi: 10.1001/jama.2017.3303
Keywords: smoking habits, cardiovascular risk, hypertension, diabetes mellitus, dyslipidemia
Citation: Song S, Lee HA, Kim Y, Jeon BK, Moon CM and Park J (2023) Dynamic changing smoking habits and cardiovascular events in patients newly diagnosed with hypertension, diabetes, or dyslipidemia: a national cohort study. Front. Cardiovasc. Med. 10:1190227. doi: 10.3389/fcvm.2023.1190227
Received: 20 March 2023; Accepted: 19 June 2023;
Published: 28 June 2023.
Edited by:
Gen-Min Lin, Hualien Armed Forces General Hospital, TaiwanReviewed by:
Michael Mussolino, National Institutes of Health (NIH), United StatesYu-Jin Kwon, Yonsei University College of Medicine, Republic of Korea
© 2023 Song, Lee, Kim, Jeon, Moon and Park. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chang Mo Moon bW9vbmNtMjdAZXdoYS5hYy5rcg== Junbeom Park bmV3cmlzZXJAbmF2ZXIuY29t
†These authors share first authorship
‡These authors share last authorship
 Shinjeong Song1,†
Shinjeong Song1,† Hye Ah Lee
Hye Ah Lee Chang Mo Moon
Chang Mo Moon Junbeom Park
Junbeom Park