
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Cardiovasc. Med. , 05 July 2023
Sec. Cardiovascular Epidemiology and Prevention
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1186330
This article is part of the Research Topic Global Excellence in Cardiovascular Medicine: Asia and Australasia View all 11 articles
 Qianhang Xia1,2,†
Qianhang Xia1,2,† Yuquan Chen1,2,†
Yuquan Chen1,2,† Zijing Yu1,2,†
Zijing Yu1,2,† Zhongyue Huang1,2
Zhongyue Huang1,2 Yujie Yang1,2*
Yujie Yang1,2* Ayan Mao1,2
Ayan Mao1,2 Wuqi Qiu1,2
Wuqi Qiu1,2
Background: Researchers have conducted a considerable number of epidemiological studies on dyslipidemia in China over recent years. Nevertheless, a representative study to comprehensively appraise for the epidemiological status of dyslipidemia is still lacked. This meta-analysis is intended to explore the pooled prevalence, rates of awareness, treatment, and control of dyslipidemia among adults in Chinese Mainland.
Materials and methods: A systematic review was performed on relevant cross-sectional studies published since January 2012 by searching six authoritative literature databases. Meta-analyses were conducted in included studies based on a random-effect model to summarize the epidemiological status of dyslipidemia in China. A potential source of heterogeneity was detected by subgroup analysis and meta-regression. Publication bias was assessed by Egger's test and funnel plots. A sensitivity analysis was conducted to examine the study quality's influence on the pooled estimate of prevalence and rates of awareness, treatment, and control.
Results: Forty-one original researches with a total of 1,310,402 Chinese participants were finally included in the meta-analysis. The prevalence, rates of awareness, treatment, and control of dyslipidemia were 42.1%, 18.2%, 11.6%, and 5.4%, respectively. With a pooled prevalence estimate at 24.5%, low HDL-C was the most prevalent among various dyslipidemia types, followed by hypertriglyceridemia (TG) (15.4%), hypercholesterolemia (TC) (8.3%), and high LDL-C (7.1%). The pooled prevalence of elevated serum lipoprotein(a) [Lp(a)] was 19.4%. By gender, the prevalence of dyslipidemia was 47.3% in males and 38.8% in females. Subgroup analyses revealed that the prevalence in southern and urban areas were higher than their counterparts. Females and population in urban areas tended to possess higher rates of awareness, treatment, and control. Meta-regression analyses suggested that the year of screening influenced prevalence estimates for dyslipidemia. The impact of the study's quality on the pooled estimates is insignificant.
Conclusion: Our study suggested a severe epidemic situation of dyslipidemia among adults in Chinese Mainland. More importantly, the awareness, treatment, and control rates were extremely low, revealing that dyslipidemia is a grave health issue. Consequently, we should attach more importance to the management of dyslipidemia, especially in economically underdeveloped areas.
Systematic review registration: PROSPERO [CRD42022366456].
Cardiovascular disease (CVD) is one of the prior sources of global disease burden, as well as the main cause of premature death for Chinese residents (1–3). In China, cardiovascular disease is the leading cause of total deaths among residents while its prevalence and mortality are still increasing (4, 5). In 2019, cardiovascular diseases were responsible for 46.76% of the total deaths in rural areas and 44.26% in urban areas of China (6), which means that approximately two in five deaths were caused by cardiovascular diseases on average. Against the background of population aging trend and progressively prevalent metabolic risk factors such as hypertension, hyperglycemia, central adiposity, and dyslipidemia (7, 8), the disease burden caused by cardiovascular diseases kept increasing, which has developed into a critical concerning public health issue (9–12). Atherosclerotic cardiovascular disease (ASCVD) includes ischemic heart disease and ischemic stroke (13–15). Because of the same arterial pathological characteristics and risk factors, ASCVD is increasingly regarded as a special type of cardiovascular disease in Chinese and international cardiovascular disease prevention guidelines (16–20). In addition, ASCVD is the pattern that causes the most deaths among all kinds of cardiovascular diseases. In 2016, it caused about 2.4 million deaths in China, which amounts to more than 60% of all cardiovascular disease deaths as well as 25% of all causes of death (21, 22). Therefore, prevention and treatment of ASCVD are the top priorities of management for cardiovascular disease.
Characterized by hypercholesterolemia (high TC), hypertriglyceridemia (high TG), low HDL-C, or high LDL-C, dyslipidemia is a crucial risk factor for ASCVD and one of the three major risk factors that the Healthy China 2030 plan focuses on (23–27), which emphasizes the strategic role of health in China's development and outlines the major principles to achieve this. The disease burden caused by dyslipidemia in China has shown a significant growth trend in recent years (28–30). In 2017, a study showed that 862,759 deaths in China could be attributed to high LDL-C, accounting for 8.25% of all causes of death and 19.71% of cardiovascular disease deaths (31). Economist Intelligence Unit (EIU) report (2018) indicated that CVD had the economic burden of USD 21.7 billion in direct and indirect costs annually in China, of which more than 12% is due to dyslipidemia (32).
Although “co-management of hypertension, diabetes, and hyperlipidemia” was clearly proposed in the Healthy China 2030 plan, the management of dyslipidemia is far from ideal for hypertension and diabetes. The 2017 China Cardiovascular Health Index study showed the prevalence of dyslipidemia (33.7%) exceeded hypertension (26.0%), and diabetes (9.7%), while its awareness rate (14.5%), treatment rate (7.9%), and control rate (5.4%) were all below the corresponding levels of hypertension and diabetes (33). Compared with the standardized management of hypertension and hyperglycemia, that of dyslipidemia is still in a neglected position, and the public's awareness and attention to it need to be strengthened (34–38).
In recent years, researchers have carried out surveys on the epidemiological status of dyslipidemia in China, and many related data have been disclosed. Due to divergent research backgrounds and other reasons, the results varied widely between different studies (39). A comprehensive evaluation on the dyslipidemia epidemiology nationwide in China which may promote our understanding of the epidemiological status of dyslipidemia as well as benefit future research and policy formulation is needed. Consequently, we performed the meta-analyses to comprehensively synthesize the prevalence and management status of dyslipidemia among adults in Chinese Mainland.
Based on and Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines (40) and the PRISMA statement (41), we conducted the systematic review. Studies on dyslipidemia from six databases were searched, including Web of Science, Embase, PubMed, WanFang, CNKI, and Chinese BioMedical Literature Database. The search strategy was based on a conjunction of “dyslipidemias,” “hyperlipidemias,” “epidemiology,” “prevalence,” “awareness rate,” “treatment rate,” “control rate,” “cross-sectional study,” and so on. The detailed literature retrieval strategy for each database can be found in Supplementary Material. Only studies published in English and Chinese between 1 January 2012 and 31 January 2023 were included.
The following information concerning dyslipidemia in Chinese population must be included in eligible studies: prevalence, awareness rate, treatment rate, and control rate. In addition, studies reported that the prevalence of elevated lipoprotein(a) [Lp(a)] was also included.
Eligibility criteria were set as followed: (1) research types: original cross-sectional studies; (2) study participants: Chinese adults; (3) the criteria of prevalence, awareness, treatment, and control rates of dyslipidemia were set based on the latest guideline of Prevention and Treatment for Dyslipidemia in Chinese adults (42).
The exclusion criteria we applied were the following: (1) animal research, (2) non-cross-sectional study, (3) study with a sample size lower than 500, and (4) study on specific occupational groups.
After combining all searched articles in EndNote X9 and removing duplicates, two reviewers (QX and YC) independently scanned the titles and abstracts of the retrieved studies for possible eligible studies. Then, the two reviewers independently evaluated the full texts of all potential eligible studies. After discussing and determining the final list of the included studies, QX and YC extract the relevant information by a standardized data collection form, respectively. The extracted information was cross-checked, and a third reviewer (ZY) was responsible for determining any unsettled discrepancies.
The two reviewers (QX and YC) independently extracted the data from studies including but not limited to regular information (such as title, author, and the publication year), characteristics of study (such as study area and number of participants), and characteristics of participants (such as age range, gender, and residential area). Then, the core information was extracted, i.e., the prevalence and rates of awareness, treatment, and control reported in each study. We also extracted these data stratified by age group, sex, region area, and year of screening.
According to the observational study criteria recommended by AHRQ, QX and YC independently evaluated the quality of the included studies (43). With a full score at 11 points, each study was grouped according to its own score. The grouping rules are as follows: good (above 7 points), medium (4–7 points), and poor (below 4 points). In addition, the risk of bias (ROB) of the included studies was evaluated based on the results' quality.
We calculated the pooled rates of prevalence, awareness, treatment, and control and corresponding 95% confidence intervals (95% CI) with a systematic analysis approach. Heterogeneity among studies was examined by Cochran's Q test and I2 statistic. The I2 statistic value at 25%, 50%, and 75% indicated a low, moderate, and high degree of heterogeneity, respectively (44, 45). The random-effect model will be used if the result suggested a high degree of heterogeneity (I2 > 50%). Otherwise, the fixed-effect model will be used (46).
To address heterogeneity between studies, subgroup analyses by age group, sex, geographic region, and the year of screening were performed. Afterward, a meta-regression was conducted, and the added variables include sex ratio (males vs. females), the year of screening, geographic area (southern vs. northern China), studies' quality score, and sample size. Finally, we performed a sensitivity analysis by evaluating the influence of the study's quality on the pooled estimates. Funnel plots and Egger's test were used to assess the risk of publication bias. We set the significance level at a P < 0.05. Stata and SPSS software were used to perform statistical analyses.
A total of 10,379 studies from all databases were searched and gathered in EndNote X9 software. Initially, 3,674 duplicates were removed, and then 6,161 studies were eliminated after reading the titles and abstracts, leaving 544 possibly qualified articles. Studies using other diagnostic criteria, reporting incomplete data or with a sample size of <500, were further excluded after referring to the full text. Finally, 41 studies (47–87) were included for analysis which involved a total of 1,310,402 Chinese adults. The search selection process is displayed in Figure 1.
Table 1 represented the characteristics of all included studies. Among all included 41 studies, 30 were published in Chinese (47–60, 63, 64, 68–70, 73–79, 81, 85–87), and 11 were in English (61, 62, 65–67, 71, 72, 80, 82–84). All studies were published between 2012 and 2023. As for study area, 14 studies (47, 49, 50, 58, 61, 63, 69, 70, 72, 75–77, 83, 85) were conducted on the populations of northern China, while 17 studies (48, 51–57, 59, 68, 71, 73, 74, 78, 84, 86, 87) focused on southern counterparts, and 10 nationwide studies (60, 62, 64–67, 79–81, 82) were conducted.
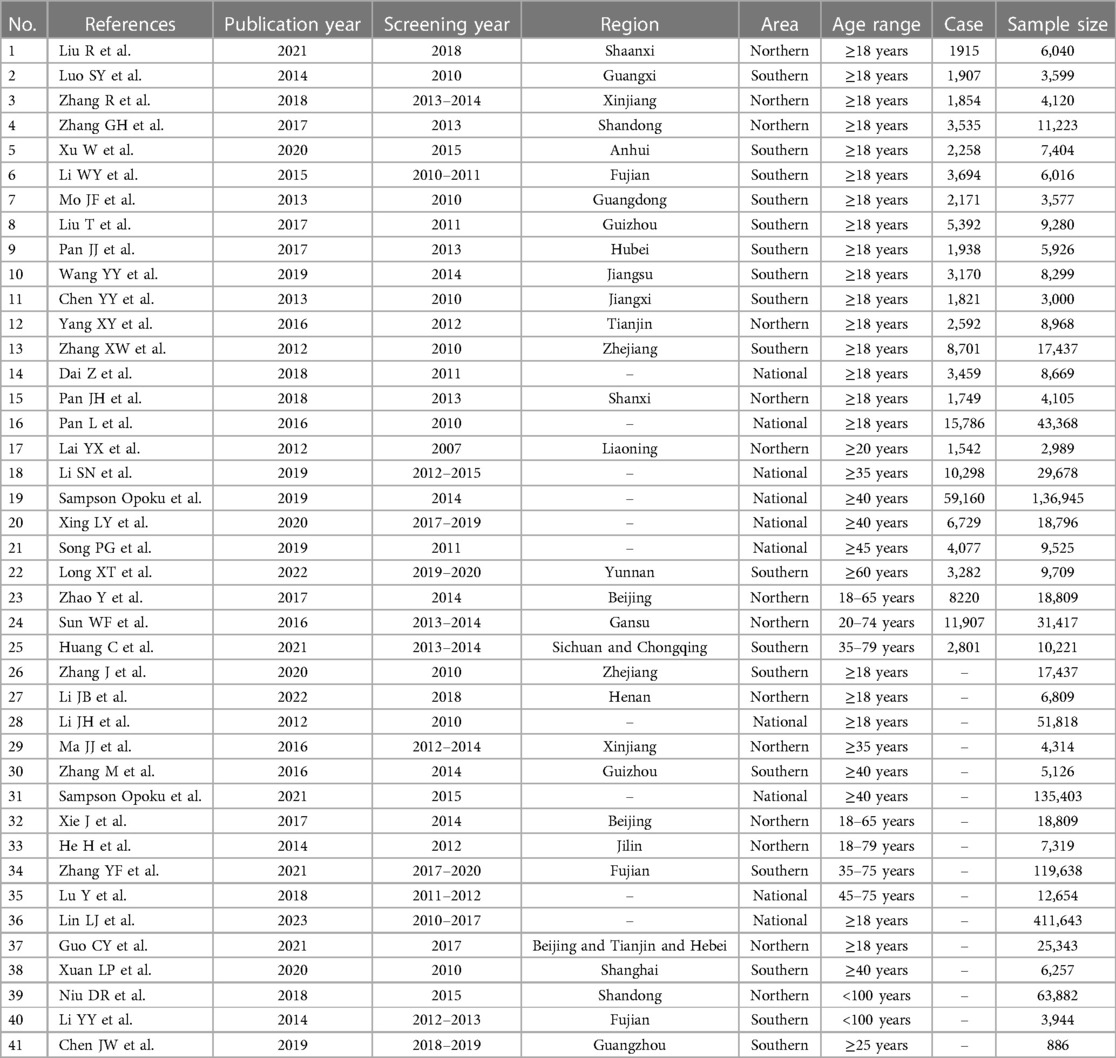
Table 1. Characteristic of 41 included studies of the epidemiology of dyslipidemia in Chinese adults.
The results of quality evaluation of the included studies were displayed in Table 2. A total of 29 studies scored above 7 and were consequently rated as high-quality, while 12 studies were rated as medium-quality, and no studies of low-quality were observed. The studies' average quality score was 8.07, while the standard deviation was 1.09. Since no study was evaluated as low-quality, all studies were included for further analyses. Figure 2 showed the summary plots of assessment for risk bias.
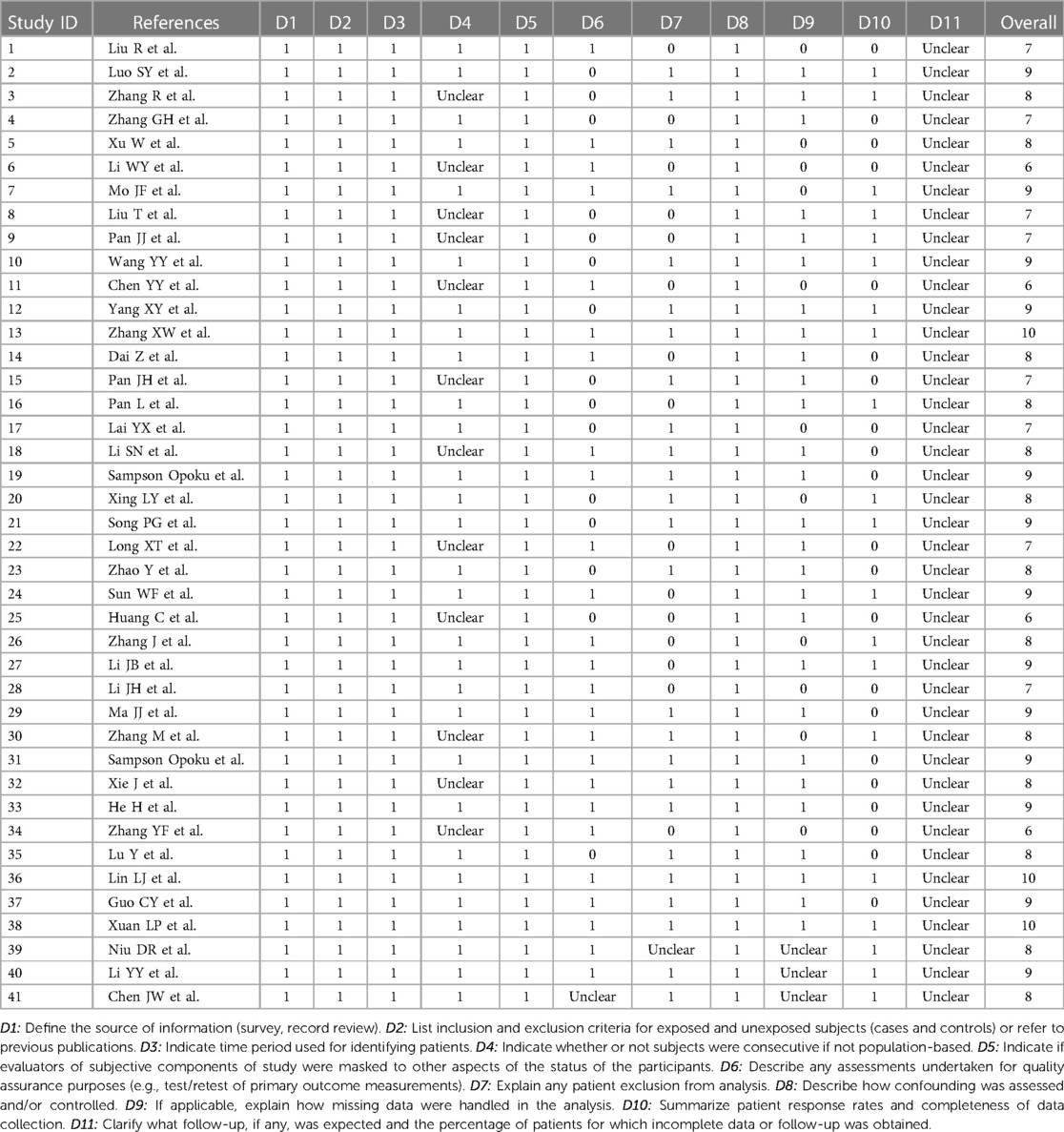
Table 2. Quality evaluation results of systematic review of epidemiology of dyslipidemia in Chinese adults.
Twenty-five articles detailed the dyslipidemia prevalence of their population (see Table 3). The meta-analysis suggested that the pooled prevalence of dyslipidemia among adults in Chinese Mainland was 42.1% (95% CI: 39.2%– 44.9%), while the heterogeneity between studies was extremely high (I2 = 99.8%, P < 0.001). The forest plots of the pooled prevalence and rates of awareness, treatment, and control were displayed in Figure 3, and the corresponding funnel plots were shown in Figure 4. The Egger's test and funnel plots (Figure 3A) demonstrated that no significant publication bias on the prevalence of dyslipidemia was found (P = 0.996).
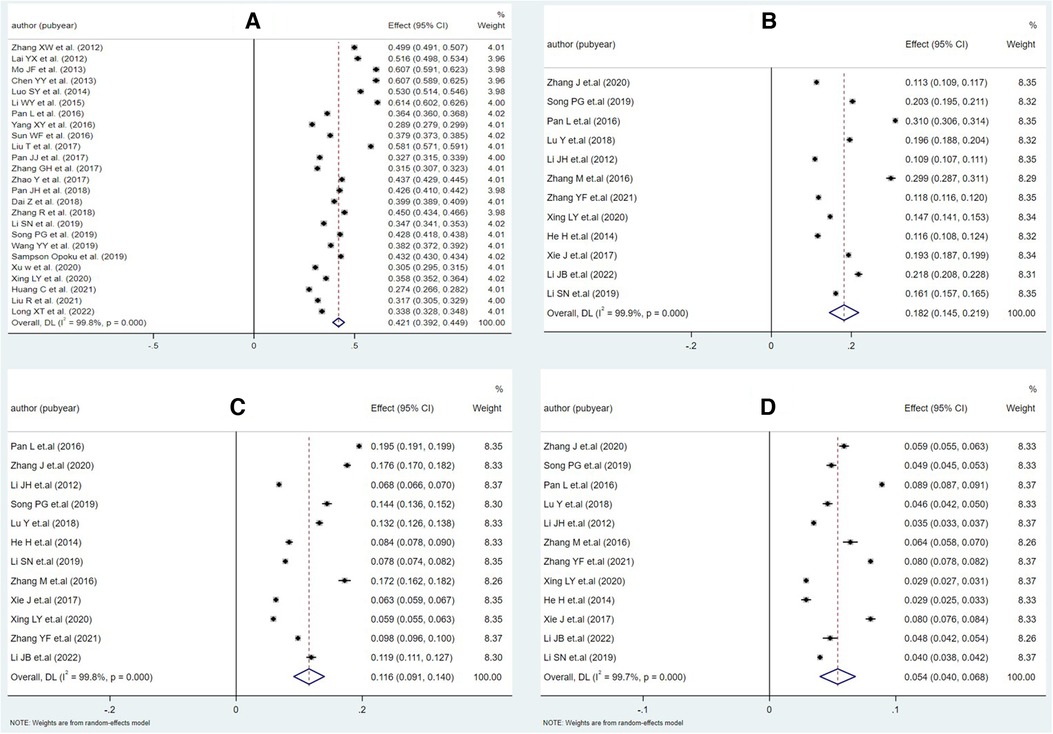
Figure 3. Forest plot of meta-analysis for each part of epidemiology of dyslipidemia in Chinese adults. (A) Prevalence, (B) awareness rate, (C) treatment rate, and (D) control rate.
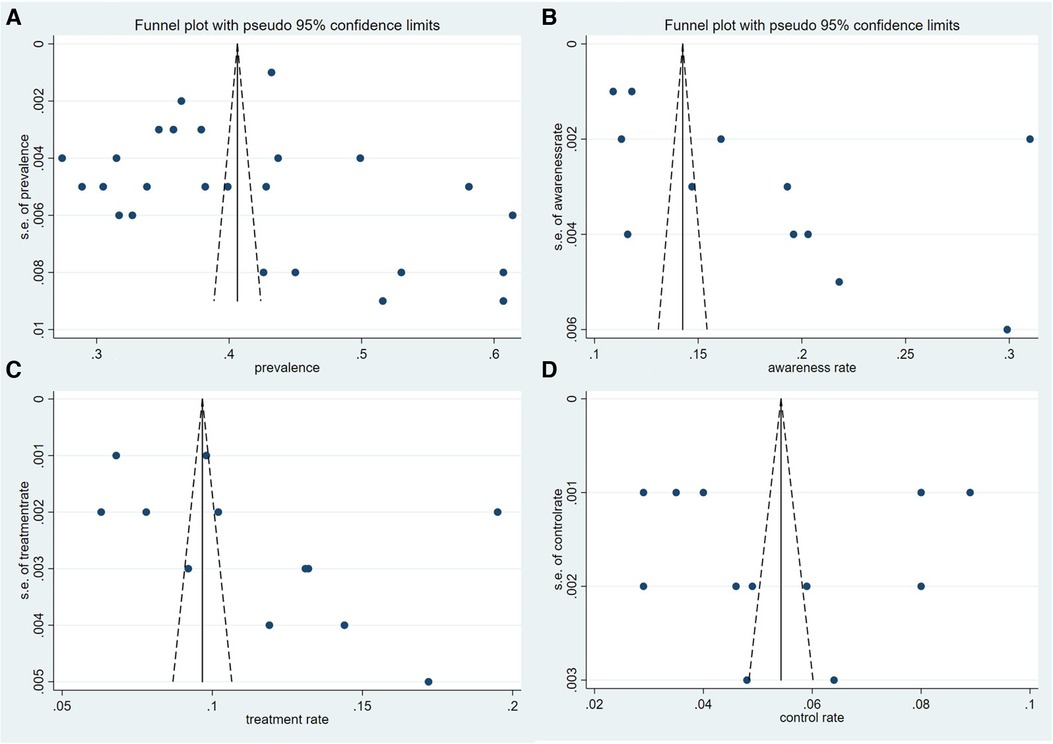
Figure 4. Funnel plot of each theme. (A) Prevalence, (B) awareness rate, (C) treatment rate, and (D) control rate.
Table 3 detailed the results of subgroup analysis stratified by gender, age group, geographic area, year of screening, and types of dyslipidemia. Males had higher pooled prevalence (47.3%, 95% CI: 44.0%–50.6%) of dyslipidemia than females (38.8%, 95% CI: 34.3%–43.3%), and the difference was statistically significant (P < 0.001). The pooled prevalence for specific age ranges was 45.2% (95% CI: 39.7%–50.7%) for subjects aged 45–59 years, which was the highest and similar to that of subjects aged ≥60 years (44.9%, 95% CI: 38.8%–50.9%), and subjects aged 18–44 years had the lowest pooled prevalence (40.1%, 95% CI: 33.1%–47.1%). Populations living in the southern area of China had higher pooled prevalence of dyslipidemia (46.0%, 95% CI: 38.2%–53.9%) than those living in northern China (39.1%, 95% CI: 34.5%–43.7%). In addition, the pooled prevalence of urban residents (46.3%, 95% CI: 43.2%–49.5%) was high than that of rural residents (41.3%, 95% CI: 37.3%–45.2%). In addition, the pooled prevalence of dyslipidemia decreased with time, which was 53.4% (95% CI: 44.2%–62.6%) during 2007–2010, decreasing to 38.9% (95% CI: 32.7%–45.1%) during 2011–2013, and decreasing further to 36.7% (95% CI: 33.0%–40.5%) during 2014–2020.
The pooled prevalence of different types of dyslipidemia varied widely. HDL-C was the highest at 24.5% (95% CI: 21.0%–28.1%), followed by hypertriglyceridemia at 15.4% (95% CI: 12.5%–18.3%), and the pooled prevalence of hypercholesterolemia and LDL-C were lower at 8.3% (95% CI: 6.9%–9.6%) and 7.1% (95% CI: 5.9%–8.2%), respectively. The forest plots for the pooled prevalence of different types of dyslipidemia were displayed in Figure 5. Corresponding funnel plots were shown in Figure 6. We also calculated the pooled prevalence of elevated Lp(a), which was defined as a serum Lp(a) value of >30 mg/dl according to the latest guideline of Prevention and Treatment for Dyslipidemia in Chinese adults (42). The results showed a pooled prevalence between that of HDL-C and hypertriglyceridemia at 19.4% (95% CI: 16.8%–22.1%). Forest plot and funnel plot for the prevalence of elevated Lp(a) could be searched in Supplementary Material.
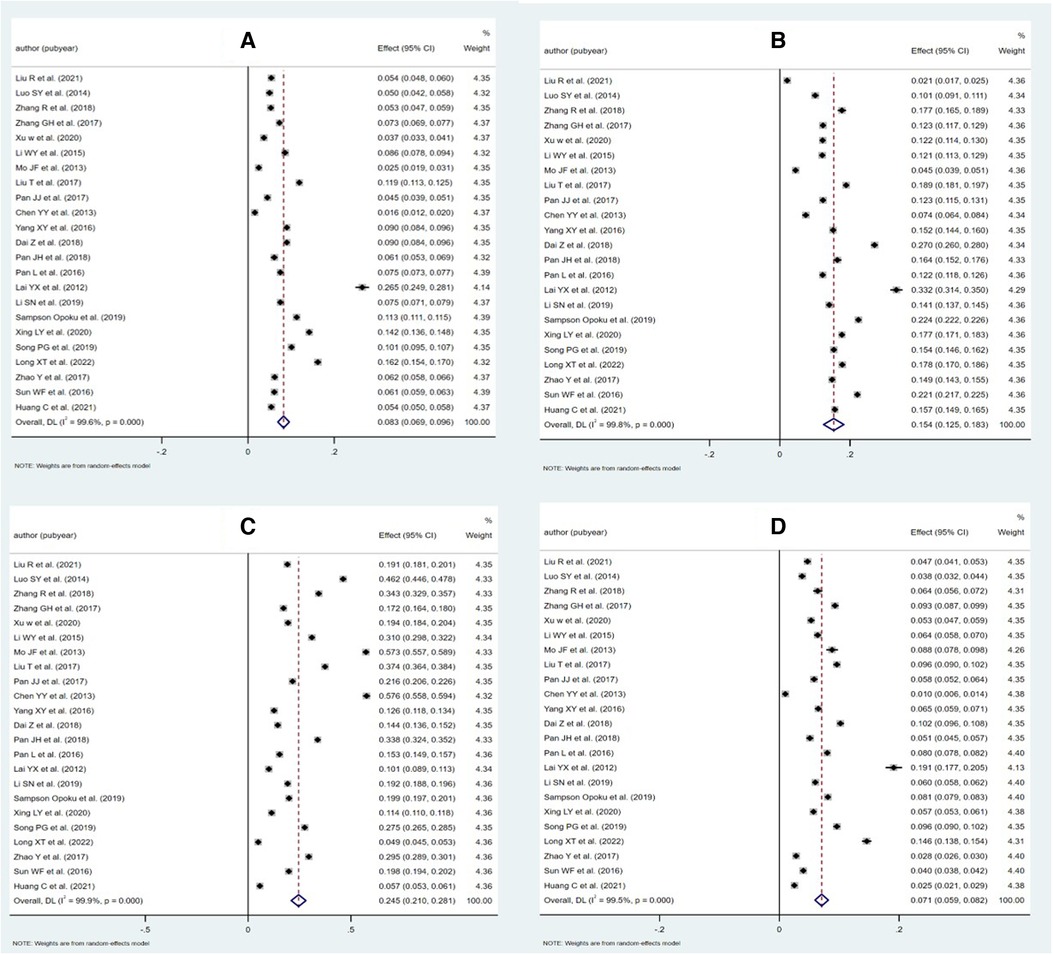
Figure 5. Forest plots for the pooled prevalence of different types of dyslipidemia. (A) Hypercholesterolemia (TC), (B) hypertriglyceridemia (TG), (C) low levels of high-density lipoprotein cholesterol (HDL-C), and (D) high levels of low-density lipoprotein cholesterol (LDL-C).
According to the related information released in 12 surveys, we arrived at pooled rates of awareness, treatment, and control of dyslipidemia at 18.2%, 11.6%, and 5.4%, respectively (see Table 4). The funnel plots (see Figure 4) and the Egger's tests demonstrated that no significant publication bias on the rates was observed (P = 0.072, 0.110 and 0.958, respectively).
The pooled rates of awareness, treatment, and control in females (18.5%, 12.3%, and 6.4%, respectively) were higher than those in males (15.7%, 9.7%, and 4.2%, respectively). Urban residents had higher pooled rates of awareness, treatment, and control than the rural residents (P < 0.001). Southern residents had higher pooled rates of treatment and control (13.3% and 6.8%, respectively) than the northern populations (9.4% and 4.6%, respectively), while the difference of awareness rates was not statistically significant among them (P = 0.055). The pooled rates of awareness and control increased with time. The pooled rates are 17.4% and 5.1%, respectively, during 2009–2013, increasing to 18.9% and 5.7% during 2014–2020. However, the pooled rate of treatment dropped from 12.7% to 10.5% over the same period.
In the sensitivity analysis, we excluded four citations with a quality score of 6 which was the lowest among all studies. After omitting these studies, we discovered a slight decrease in the pooled prevalence (from 42.1% to 41.0%, P = 0.653). Funnel plot combined with Egger's test (P = 0.639) indicated that no significant publication bias was noted. The pooled prevalence of hypercholesterolemia, hypertriglyceridemia, HDL-C, and LDL-C changed to 8.7%, 15.9%, 23.5%, and 7.6% from 8.3%, 15.4%, 24.5%, and 7.1%, respectively. The pooled rates of awareness, treatment, and control also changed slightly (from 18.2%, 11.6%, and 5.4% to 18.8%, 11.8%, and 5.2%, respectively) after omitting these studies. The results indicated that the pooled prevalence and rates of awareness, treatment, and control had good stability.
Finally, a meta-regression was performed to address the high level of heterogeneity between studies (I2 = 98.7%–100.0%). Five variables (sex ratio, the year of screening, geographic area, studies' quality score, and sample size) were included in the analyses. The results of meta-regression demonstrated that only the year of screening variable had a significant impact on the heterogeneity (P = 0.011) (see Table 5).
For the first time, this study comprehensively summarized and analyzed the epidemiological studies on dyslipidemia in recent years and explored its potential influencing factors. With a total number of 1,310,402 participants from different cross-sectional studies, our systematic review incorporated 41 studies conducted in multiple provinces of Chinese Mainland over the past decade. The results of the meta-analyses suggested a high-degree of prevalence of dyslipidemia in Chinese adults along with unacceptably low rates of awareness, treatment, and control. Results from this study would be a timely alarm since a comprehensive evaluation on the dyslipidemia epidemiology nationwide in China which may promote our understanding of its epidemiological status and benefit future research and policy formulation is still lacking. In 2014, the pooled prevalence of dyslipidemia among adults in Chinese Mainland is 42.1%, which is very close to the research results of Huang et al. (41.9%) (88). The deepening of aging population degree and the great changes in residents' living habits (including but not limited to diet and physical activity) could lead to the highly prevalent dyslipidemia in recent years (89–94). By comparison with other developed countries, the dyslipidemia prevalence in Chinese adults was still lower than that reported in the United States (54.9%) (95) but much higher than that reported in Korea (16.6%) (96) and Japan (27.1%) (97). Among all types of dyslipidemia, HDL-C was the most prevalent, with a pooled estimate of 24.5%, followed by hypertriglyceridemia (15.4%), hypercholesterolemia (8.3%), and LDL-C (7.1%). In accordance with the results from surveys of Chinese Mainland in 2008–2019 (65, 98, 99), the more prevalent types of dyslipidemia in China were still HDL-C and hypertriglyceridemia. As the risk of ASCVD will be increased by all types of dyslipidemia, it is essential to treat them with applicable interventions, both clinical and non-clinical (25, 88).
The pooled estimates of dyslipidemia prevalence between different genders, age groups, and regions were calculated and analyzed. We found that males had higher pooled prevalence than females (47.3% vs. 38.8%; P < 0.001), which is consistent with the previous studies' results (100–103). Many factors can attribute to such difference, for instance, males are more likely to possess unhealthy behaviors than females, including but not limited to lack of vegetables and fruits in diet and fewer physical activity. Such factors could contribute to higher prevalence of many metabolic diseases in males than females, including dyslipidemia (104–108). Researches showed that estrogen changes the vascular permeability by increasing nitrous oxide production which retains a healthful lipoprotein profile (109, 110). Nonetheless, such protective mechanisms will disappear after menopause, resulting in an ascending risk for suffering cardiovascular diseases. For example, the levels of TC, TG, LDLC, and VLDL-C aming postmenopausal women appear an upward trend, while that of HDL-C significantly decreases. Consequently, the prevalence of dyslipidemia in women often showed a dramatic increase after menopause, even surpassing that of men of the same age (60, 62, 65, 99). The systematic review revealed that southern and urban residents were more likely to suffer from dyslipidemia than their counterparts, which was a result in line with previous findings (111, 112). Another study in China suggested that economically developed areas (e.g., southeast area of China) tend to possess higher burden of dietary chronic conditions, such as dyslipidemia and obesity (113). In addition, healthcare facilities are more accessible for residents in highly urbanized and economically vibrant cities, resulting in more diagnosis and hence higher reporting rate of dyslipidemia in urban and southern areas. It is worth noting that in recent years, dyslipidemia has become more and more prevailing in Chinese youngsters. A cross-sectional study conducted in Wenzhou, Zhejiang Province, showed a prevalence at 34.11% among 7,859 young adults (114), which was much higher than the figure in Mainland China 10 years before that, as well as other Asian developing countries (115, 116). In Beijing, a study of 3,249 children aged 6–18 years showed that the prevalence of dyslipidemia was 28.9%, higher than 18.8% in 2004 (117). The younger trend of dyslipidemia may be partly attributed to the westernization of young people's lifestyle, such as dietary patterns (114). It is indisputable that corresponding risk factor intervention project should be developed based on the characteristics of young people and further screening and management programs should be strengthened.
One of the key findings of this study is a summary estimation of the pooled prevalence of elevated Lp(a) in Chinese adults, although it is not included in the definition of dyslipidemia. According to the latest guideline of Prevention and Treatment for Dyslipidemia in Chinese adults (42), we set the cutoff value at >30 mg/dl and got a pooled prevalence at 19.4%, which was much lower than that in the United States (35%) (118). As a novel lipid biomarker which could promote the formation of atherosclerosis and thrombosis, Lp(a) was considered the core pathogenesis of ASCVD and deemed as a reversible risk factor (119). Based on seven randomized controlled trials and 29,069 patients taking statin medication, one meta-analysis found that elevated Lp(a) can still increase the risk of CVD, despite a controlled LDL-C level (120). Due to the fact that the concentration level of Lp (a) in plasma is mainly caused by genetic factors, it is relatively stable throughout life (121). Chinese researchers recommended that people consider at least once measurement of Lp(a) to identify individuals who have inherited extremely increased levels of Lp(a) (≥180 mg/dl), which may bring an extremely high lifetime risk of ASCVD (119).
Publicizing the harm of dyslipidemia to the general public along with encouraging a healthier lifestyle is the basic strategy to prevent dyslipidemia and ASCVD. For patients with dyslipidemia, the focus is to control the blood lipid level to the normal range through therapeutic approaches, such as taking statins. Therefore, improving residents' awareness, treatment, and control of dyslipidemia is the key to effective management of dyslipidemia. The pooled rates of awareness, treatment, and control of dyslipidemia among Chinese adults are 18.2%, 11.6%, and 5.4%, respectively, which are slightly higher than the research results of Zhao et al. (10.9%, 6.8%, and 3.5%, respectively) in Chinese Mainland in 2010 but much lower than that reported in the United States (73.3%, 54.1%, and 35.7%) and also lower than the results from Argentina (37.3%, 36.6%, and 20.0%) and South Korea (29.4%, 17.0%, and 13.9%, respectively) (79, 122, 123). In accordance with previous studies (80, 88), our study suggested that women had higher awareness rates of dyslipidemia than men and tend to receive corresponding treatment, which further contributed to better control of their condition. Various factors can account for such phenomenon, for instance, studies demonstrated that women more frequently seek medical services than men (124). In addition, women are more likely to have a health insurance as well as an ongoing source for primary care than men (125). Therefore, we suggested strengthening the promotion and management of dyslipidemia among male residents in China. In line with the previous studies (62, 80), our results showed that urban residents had significantly higher rates of awareness, treatment, and control than rural residents. Similarly, such urban–rural difference was found in a couple of findings from other countries (119, 126, 127). The differences in rates between urban and rural areas may be partly attributed to the gap between residents' economy and education level (128). A prior study suggested a gap in statin availability between urban and rural areas, which may support evidence that rural residents generally have difficulty accessing health care, especially in developing countries (129, 130). Therefore, it is suggested to attach more importance to the dyslipidemia management in rural areas, such as increasing the availability of drugs. The significance of this study has been highlighted by the extremely low rates of awareness, treatment, and control discovered, which may imply some disparities and deficiencies in dyslipidemia management in China. The results of a study on 99,655 patients with dyslipidemia who had prescribed statins in Tianjin showed that although high adherence to medications can reduce the risk of major adverse cardiovascular events, only 5.4% of the patients insist on taking statins for more than 50% of the days (131). Results of China Dyslipidemia Survey (DYSIS) signified that among the outpatients in China who had regularly taken lipid-lowering drugs, statin monotherapy accounted for 97.96%, while combination therapy accounted for only 2.04%. In addition, despite the steady lipid-lowering therapy, the vast majority of patients still had at least one manifestation of dyslipidemia (132). China PEACE Million Persons Project investigated the accessibility of lipid-lowering drugs in primary healthcare institutions of China. Only 49.7% of total number of 3,041 primary care institutions stocked statins, while 19.2% stored non-statin lipid-lowering drugs. The poor drug availability was particularly serious in rural medical institutions (129). The PURE study evaluated the usage of secondary prevention drugs for patients with CVD in communities of countries with different income levels (133). Results signified a positive relation between the rates of use for statins and the economic level of country. In addition, the use rate of statins in patients with coronary heart disease or stroke in China was the lowest (1.7%) among all secondary prevention drugs, which is lower than the level in North America, Europe, the Middle East, South America, Malaysia, and South Asia and only slightly higher than the level in Africa.
Consequently, at the first step, we suggested to determine a patient journey of dyslipidemia with clear process and easy understanding and operation. Second, by improving the allocation of manpower and resources in primary medical institutions, it may help in making up for their vacancy in the management of dyslipidemia and gradually play their role in patient screening, initial diagnosis, referral, and follow-up management. Finally, a comprehensive management system should be established to prevent and control various cardiovascular diseases and their risk factors.
The quality of the studies included in this systematic review is generally high; consequently, the results of sensitivity analysis revealed that when the lowest score studies were excluded, only a slight impact on the results was achieved. Data from multiple provinces in Chinese Mainland with a large sample size was incorporated in our meta-analysis. However, some limitations in this study are shown as well. Firstly, due to limitations in data availability, the relationship between the prevalence of dyslipidemia and some factors cannot be explored by subgroup analyses and meta-regression. Therefore, this study is limited in exploring the influencing factors of dyslipidemia. Secondly, only epidemiological studies were included in our systematic review and meta-analysis, and the high degree of heterogeneity between studies is inevitable (134). However, subgroup analysis and meta-regression alleviate this issue to some extent. Finally, we cannot infer causality between dyslipidemia and other factors due to the cross-sectional design in all included studies.
Nearly half of Chinese adults suffered from dyslipidemia, while the most prevalent type of dyslipidemia was low levels of high-density lipoprotein cholesterol. Males and urban residents had a higher prevalence of dyslipidemia than their counterparts. This study further suggested extremely low rates of awareness, treatment, and control for dyslipidemia in Chinese adults. The government should increase the financial and manpower support for primary medical institutions and implement effective programs to prevent and control dyslipidemia.
The original contributions presented in the study are included in the article/Supplementary Material, and further inquiries can be directed to the corresponding author.
Conceptualization, QX. Methodology, QX and YC. Material search: QX and ZY. Data extraction: QX, YC, and ZY. Data analysis: QX, ZH, WQ, and AM. Writing—original draft preparation: QX. Writing—review and editing: QX, YC, ZY, ZH, AM, WQ, and YY. Supervision: YY. Project administration: YY. Funding acquisition: YY. All authors contributed to the article and approved the submitted version.
This research was funded by the Capital health development scientific research project (2021-1g-4251). The funding bodies did not play any role in the design of the study and collection, analysis, and interpretation of data and in writing this manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at https://www.frontiersin.org/articles/10.3389/fcvm.2023.1186330/full#supplementary-material
1. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. (2019) 16:203–12. doi: 10.1038/s41569-018-0119-4
2. Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the global burden of disease study 2013. Lancet. (2016) 387:251–72. doi: 10.1016/s0140-6736(15)00551-6
3. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study (vol 76, pg 2982, 2020). J Am Coll Cardiol. (2021) 77:1958–9. doi: 10.1016/j.jacc.2021.02.039
4. The writing committee of the report on cardiovascular health and diseases in China. Overview of China cardiovascular health and disease report 2021. Chin J Cardio-Vascular Res. (2022) 20:577–96. doi: 10.3969/j.issn.1672-5301.2022.07.001
5. China’s National Health Commission. China Health statistics yearbook. Beijing: China Union Medical University Press (2020).
6. Interpretation of Report on Cardiovascular health and diseases in China 2021. Chin J Cardiovasc Med. (2022) 27:305–18. doi: 10.3969/j.issn.1007-5410.2022.04.001
7. Isomaa B, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. (2001) 24:683–9. doi: 10.2337/diacare.24.4.683
8. Cai H, Huang J, Xu G, Yang Z, Liu M, Mi Y, et al. Prevalence and determinants of metabolic syndrome among women in Chinese rural areas. PLoS One. (2012) 7:e36936. doi: 10.1371/journal.pone.0036936
9. Liu S, Li Y, Zeng X, Wang H, Yin P, Wang L, et al. Burden of cardiovascular diseases in China, 1990-2016: findings from the 2016 global burden of disease study. JAMA Cardiol. (2019) 4:342–52. doi: 10.1001/jamacardio.2019.0295
10. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/s0140-6736(19)30427-1
11. Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. (2016) 176:524–32. doi: 10.1001/jamainternmed.2016.0190
12. Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE million persons project). Lancet. (2017) 390:2549–58. doi: 10.1016/s0140-6736(17)32478-9
13. Wang CY, Chen YQ, Jin JY, Du R, Fan LL, Xiang R. A novel nonsense mutation of ABCA8 in a Han-Chinese family with ASCVD leads to the reduction of HDL-c levels. Front Genet. (2020) 11:755. doi: 10.3389/fgene.2020.00755
14. Chamberlain AM, Cohen SS, Weston SA, Fox KM, Xiang P, Killian JM, et al. Relation of cardiovascular events and deaths to low-density lipoprotein cholesterol level among statin-treated patients with atherosclerotic cardio-vascular disease. Am J Cardiol. (2019) 123:1739–44. doi: 10.1016/j.amjcard.2019.02.043
15. Zhou L, Mai J, Li Y, Guo M, Wu Y, Gao X, et al. Triglyceride to high-density lipoprotein cholesterol ratio and risk of atherosclerotic cardiovascular disease in a Chinese population. Nutr Metab Cardiovasc Dis. (2020) 30:1706–13. doi: 10.1016/j.numecd.2020.05.009
16. Okamura M, Takekawa H, Sjsum , Okabe R, Suzuki K, Hirata K. Vertebral artery Doppler waveform patterns for exclusive diagnosis of basilar artery stenosis and occlusion. J Med Ultrason (2001). (2016) 43:83–9. doi: 10.1007/s10396-015-0669-6
17. Volgman AS, Palaniappan LS, Aggarwal NT, Gupta M, Khandelwal A, Krishnan AV, et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American heart association. Circulation. (2018) 138:e1–e34. doi: 10.1161/CIR.0000000000000580
18. Nordestgaard BG. Triglyceride-Rich lipoproteins and atherosclerotic cardiovascular disease: new insights from epidemiology, genetics, and biology. Circ Res. (2016) 118:547–63. doi: 10.1161/CIRCRESAHA.115.306249
19. Zeng Y, Zhu S, Yu X, Wang S, Yu K, Qi H. Expert consensus on grassroots management path of adult atherosclerotic cardiovascular disease in China (draft). Chin J Gen Pract Med. (2017) 20:251–61.
20. Zhang M, Zhao Y, Tian S, Gao X, Yang J, Su S, et al. Risk stratification of atherosclerotic cardiovascular disease in Chinese patients with acute myocardial infarction. Chin J Circ. (2021) 36:852–7. doi: 10.3969/j.issn.1000-3614.2021.09.004
21. GBD results tool. GHDx http://ghdx.healthdata.org/gbd-results-tool (2018).
22. Liu S, Yuan H, Jiang C, Xu J, Qiu X, Luo J. The blood pressure control and arteriosclerotic cardiovascular risk among Chinese community hypertensive patients. Sci Rep. (2021) 11:19066. doi: 10.1038/s41598-021-98745-8
23. Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European atherosclerosis society consensus panel. Eur Heart J. (2017) 38:2459–72. doi: 10.1093/eurheartj/ehx144
24. Barter PJ, Ballantyne CM, Carmena R, Castro Cabezas M, Chapman MJ, Couture P, et al. Apo B versus cholesterol in estimating cardiovascular risk and in guiding therapy: report of the thirty-person/ten-country panel. J Intern Med. (2006) 259:247–58. doi: 10.1111/j.1365-2796.2006.01616.x
25. Jacobson TA, Ito MK, Maki KC, Orringer CE, Bays HE, Jones PH, et al. National lipid association recommendations for patient-centered management of dyslipidemia: part 1—executive summary. J Clin Lipidol. (2014) 8:473–88. doi: 10.1016/j.jacl.2014.07.007
26. Stevens W, Peneva D, Li JZ, Liu LZ, Liu G, Gao R, et al. Estimating the future burden of cardiovascular disease and the value of lipid and blood pressure control therapies in China. BMC Health Serv Res. (2016) 16:175. doi: 10.1186/s12913-016-1420-8
27. Patel AP, Wang M, Pirruccello JP, Ellinor PT, Ng K, Kathiresan S, et al. Lp(a) [lipoprotein(a)] concentrations and incident atherosclerotic cardiovascular disease: new insights from a large national biobank. Arterioscler Thromb Vasc Biol. (2021) 41:465–74. doi: 10.1161/ATVBAHA.120.315291
28. Chen P, Zhang M, Zhang Y, Su X, Chen J, Xu B, et al. Economic burden of myocardial infarction combined with dyslipidemia. Front Public Health. (2021) 9:648172. doi: 10.3389/fpubh.2021.648172
29. Mendoza-Herrera K, Pedroza-Tobias A, Hernandez-Alcaraz C, Avila-Burgos L, Aguilar-Salinas CA, Barquera S. Attributable burden and expenditure of cardiovascular diseases and associated risk factors in Mexico and other selected mega-countries. Int J Environ Res Public Health. (2019) 16:4041. doi: 10.3390/ijerph16204041
30. Yuan KJ, Zhao CY, Yang Y, Yan DH, Zhou GQ. Analysis on the trend of disease burden attributable to high level of LDL-C in Chinese population from 1990 to 2019. Chin J Evid Based Med. (2022) 22:444–9. doi: 10.7507/1672-2531.202112052
31. Xu XH, Yang JJ, Wang LJ, Yin P, Liu JM, Dong WL, et al. Study on disease burden attributable to high level of LDL-C in Chinese population in 2017. Chin J Epidemiol. (2020) 41:839–44. doi: 10.3760/cma.j.cn112338-20191205-00861
33. Fan M, Yingying J, Yunning L, Zhenping Z, Limin W, Linhong W, et al. Status of cardiovascular disease epidemics and its risk factors prevention and control in China: an evaluation based on China cardiovascular health Index of 2017. Chin J Prev Med. (2021) 55:1280–6. doi: 10.3760/crna.j.cn112150-20210822-00817
34. Peng W, Li K, Yan AF, Shi Z, Zhang J, Cheskin LJ, et al. Prevalence, management, and associated factors of obesity, hypertension, and diabetes in Tibetan population compared with China overall. Int J Environ Res Public Health. (2022) 19:8787. doi: 10.3390/ijerph19148787
35. Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. China Hypertension survey I. Status of hypertension in China: results from the China hypertension survey, 2012-2015. Circulation. (2018) 137:2344–56. doi: 10.1161/CIRCULATIONAHA.117.032380
36. Li MZ, Su L, Liang BY, Tan JJ, Chen Q, Long JX, et al. Trends in prevalence, awareness, treatment, and control of diabetes mellitus in mainland China from 1979 to 2012. Int J Endocrinol. (2013) 2013:753150. doi: 10.1155/2013/753150
37. Mao F, Jiang YY, Liu YN, Zhao ZP, Wang LM, Wang LH, et al. Prevalence and risk factors analysis of cardiovascular and cerebrovascular diseases among Chinese residents: based on the 2017 China cardiovascular health index study. Chin J Prev Med. (2021) 55:1280–6. doi: 10.3760/cma.j.cn112150-20210822-00817
38. Wang X, Li X, Zhang YB, Zhang F, Sun L, Lin J, et al. Genome-Wide linkage scan of a pedigree with familial hypercholesterolemia suggests susceptibility loci on chromosomes 3q25-26 and 21q22. Plos One. (2011) 14:10. doi: 10.1371/journal.pone.0024838
39. Chu JR, Gao RL, Zhao SP, Lu GP, Zhao D, Li JJ. Guidelines for the prevention and treatment of dyslipidemia in Chinese adults (revised in 2016). Chin J Circ. (2016) 31:937–53. doi: 10.3969/j.issn.1000-3614.2016.10.001
40. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
41. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
42. The writing committee of the report on cardiovascular health diseases in China. Interpretation of report on cardiovascular health and diseases in China 2021. Chin J Cardiovasc Med. (2022) 27:305–18.
43. Rostom A, Dubé C, Cranney A. Celiac disease. Evidence Report/Technology Assessment No. 104. AHRQ Publication No. 04-E029-2. Rockville, MD: Agency for Healthcare Research and Quality. Appendix D. Quality Assessment Forms.; 2004. (2013). Available from: https://www.ncbi.nlm.nih.gov/books/NBK35156/. [Accessed 05 March 2023].
44. Huedo-Medina TB, Sanchez-Meca J, Marin-Martinez F, Botella J. Assessing heterogeneity in meta-analysis: q statistic or I2 index? Psychol Methods. (2006) 11:193–206. doi: 10.1037/1082-989X.11.2.193
45. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327(7414):557–60. doi: 10.1136/bmj.327.7414.557
46. Schmidt FL, Oh IS, Hayes TL. Fixed- versus random-effects models in meta-analysis: model properties and an empirical comparison of differences in results. Br J Math Stat Psychol. (2009) 62:97–128. doi: 10.1348/000711007X255327
47. Liu R, Wang YP, Qiu L, Sa RN, Tao YL. Cross-sectional survey on dyslipidemia among adults in Shaanxi, 2010—2018. Mod Prev Med. (2021) 48:3081–3087 + 3109.
48. Luo SY, Yang H, Meng XY, Huang T, Xu JJ, Huang Y. Prevalence rate and risk factors of dyslipidemia among adults in Guangxi Province. Appl Prev Med. (2014) 20:129–33.
49. Zhang R, Zhang WJ, Pu E, Liao PH, Zhe W, Liu LX, et al. Analysis on epidemiological characteristics and related factors of dyslipidemia am ong adult residents of Xinjiang uygur autonomous region during 2013—2014. Chin J Prev Me. (2018) 52:1152–7. doi: 10.3760/cma.j.issn.02539624.2018.11.011
50. Zhang GH, Tang JL, Chen X, Guo XL, Xu CX, Gao CC, et al. Cross-sectional survey on dyslipidemia among residents aged 18 and above in Shandong Province, 2013. Chin J Dis Control Prev. (2017) 21:457–60. doi: 10.16462/j.cnki.zhjbkz.2017.05.007
51. Xu W, Xing XY, He Q, Dai D, Li R, Xu JQ, et al. A cross-sectional study on the prevalence and related factors of dyslipidemia among adults in Anhui province, in 2015. Chin J Epidemiol. (2020) 41:195–200. doi: 10.3760/cma.j.issn.0254-6450.2020.02.011
52. L WY, Chen TH, Zhong WL, Lin SG, Lin XQ, Ye Y, et al. Epidemic characteristics and influencing factors of dyslipidemia in Fujian residents. Strait J Prve Med. (2015) 21:1–3.
53. Mo JF, Song XL, Xu YJ, Xu XJ, He Q, Cai QM, et al. Association study of prevalence of dyslipidemia and its risk factors among adults in Guangdong Province. South China J Prev Med. (2013) 39:11–7.
54. Liu T, Guo SQ, Guo M, Li L, Liu D, Zhou J, et al. Prevalence and risk factors of dyslipidemia among adult residents in Guizhou province. Chin J Public Health. (2017) 33:88–91. doi: 10.11847/zgggws2017-33-01-22
55. Pan JJ, He TJ, Zhang L, Tang Y, Li Q, Zhang Q. Dyslipidemia prevalence and serum lipid profiles and ratios among urban and rural residents in Hubei province, 2013: a comparison analysis. Chin J Public Health. (2017) 33:1439–44. doi: 10.11847/zgggws2017-33-10-06
56. Wang Y, Dai Y, Wang S, Zhang J, Zhu Q, Xie W. Prevalence and related factors of dyslipidemia among the adult residents in Jiangsu province in 2014. J Hyg Res. (2019) 48:945–52. doi: 10.19813/j.cnki.weishengyanjiu.2019.06.014
57. Chen Y, Zhu L, Li A, Luo W, Liu J, Yan W, et al. Epidemic characteristics of dyslipidemia among adults in Jiangxi Province. Pract Prev Med. (2013) 20:234–6. doi: 10.3969/j.issn.1006-3110.2013.02.039
58. Yang X, Wang T, Wang Y. Prevalence and influencing factors of dyslipidemia among adult residents in Tianjin city: a cross-sectional study. Chin J Public Health. (2016) 32:286–90. doi: 10.3969/j.issn.1006-3110.2013.02.039
59. Zhang X, Ye Z, Zhou D, Zhang J, Wang H, He Q, et al. Prevalence of dyslipidemia and its distribution among adults, a cross-sectional study in Zhejiang. Dis Surveill. (2012) 27:395–9. doi: 10.3784/j.issn.1003-9961.2012.5.019
60. Dai J, Min J, Yang Y. A study on the epidemic characteristics of dyslipidemia in adults of nine provinces of China. Chin J Cardiol. (2019) 27:300. doi: 10.3760/cma.j.issn.0253-3758.2018.02.00
61. Pan J, Ren Z, Li W, Wei Z, Rao H, Ren H, et al. Prevalence of hyperlipidemia in Shanxi Province, China and application of Bayesian networks to analyse its related factors. Sci Rep. (2018) 8:3750. doi: 10.1038/s41598-018-22167-2
62. Pan L, Yang Z, Wu Y, Yin R-X, Liao Y, Wang J, et al. The prevalence, awareness, treatment and control of dyslipidemia among adults in China.. Atherosclerosis. (2016) 248:2–9. doi: 10.1016/j.atherosclerosis.2016.02.006
63. Lai Y, Li C, Teng X, Chen Y, Shan Z. The prevalence and risk factors of dyslipidemia among urban and rural adults in Liaoning province. J China Med Univ. (2012) 41:151–4. CNKI:21-1227/R.20120117.1122.008
64. Li S, Zhang L, Wang X, Chen Z, Dong Y, Zheng C, et al. Status of dyslipidemia among adults aged 35 years and above in China. Chin Circ J. (2019) 34:681–97. doi: 10.3969/j.issn.1000-3614.2019.07.011
65. Opoku S, Gan Y, Fu W, Chen D, Addo-Yobo E, Trofimovitch D, et al. Prevalence and risk factors for dyslipidemia among adults in rural and urban China: findings from the China national stroke screening and prevention project (CNSSPP). Bmc Public Health. (2019) 19:1500. doi: 10.1186/s12889-019-7827-5
66. Xing L, Jing L, Tian Y, Yan H, Zhang B, Sun Q, et al. Epidemiology of dyslipidemia and associated cardiovascular risk factors in northeast China: a cross-sectional study. Nutr Metab Cardio-Vascular Dis. (2020) 30:2262–70. doi: 10.1016/j.numecd.2020.07.032
67. Song P, Zha M, Yang X, Xu Y, Wang H, Fan Z, et al. Socioeconomic and geographic variations in the prevalence, awareness, treatment and control of dyslipidemia in middle-aged and older Chinese. Atherosclerosis. (2019) 282:57–66. doi: 10.1016/j.atherosclerosis.2019.01.005
68. Long X, Ye A, Chen J, Mao Y, Wang X, Pu H, et al. Prevalence and influencing factors of dyslipidemia among the elderly in Anning City from 2019 to 2020. J Prev Med Inf. (2022) 38:965–71.
69. Zhao Y, Ma A, Fang K, Li H, Xie J, Zhou Y, et al. Study on the prevalence of dyslipidemia and its risk factors among residents aged 18-65 in Beijing in 2014. Chin. J. Clin. (2017) 45:25–8. doi: 10.3969/j.issn.2095-8552.2017.11.009
70. Sun W. Epidemiological investigation of dyslipidemia in adults in Gansu province. Lanzhou University (2016).
71. Huang C, Zhang W, Tang W, Liu Y, Liu J, Xu R, et al. Prevalence and related factors of dyslipidemia among urban adults aged 35 to 79 years in Southwestern China. Sci Rep. (2021) 11:17579. doi: 10.1038/s41598-021-96864-w
72. He H, Yu YQ, Li Y, Kou CG, Li B, Tao YC, et al. Dyslipidemia awareness, treatment, control and influence factors among adults in the Jilin province in China: a cross-sectional study. Lipids Health Dis. (2014) 3:122. doi: 10.1186/1476-511X-13-122
73. Zhang J, He Q, Wang L, Zhao M-H, Su D, Lu F, et al. Analysis of influencing factors on awareness rate, treatment rate and control rate of dyslipidemia among adults in zhejiang province. Prev Med. (2020) 32:1230–5. doi: 10.19485/j.cnki.issn2096-5087.2020.12.010
74. Zhang Y, Li X, Fang X, Chen T, Chen J, Yang Z, et al. Analysis of awareness, treatment and control rate of dyslipidemia in adults in Fujian Province. Prev Med Trib. (2021) 27:892–6. doi: 10.16406/j.pmt.issn.1672-9153.2021.12.005
75. Ma J, Gao J, Luo J, Liu F, Yang Y. The prevalence rate, awareness rate, treatment rate and control rate of dyslipidemia in Uygur people over 35 years old in Akesu area of Xinjiang. Chin J Arterioscler. (2016) 24:1050–4.
76. Xie J, Dong Z, Li H, Ma A, Fang K, Dong J, et al. The awareness rate, treatment rate, control rate of dyslipidemia and the influencing factors in the residents (18-65 years old) of Beijing. Chin J Prev Contr Chron Dis. (2017) 25:489–93. doi: 10.16386/j.cjpccd.issn.1004-6194.2017.07.003
77. Li J, Liu J, Wu E. Analysis on the status quo of awareness, treatment and control of dyslipidemia among adult residents in Zhengzhou and its influencing factors. Chin J Prev Contr Chron Dis. (2022) 30:525–9. doi: 10.16386/j.cjpccd.issn.1004-6194.2022.07.010
78. Zhang M, Zhang Y, Shi L, Zhang Q, Peng N, Hu Y. Awareness, treatment and control of dyslipidemia in middle-aged and older population in Guiyang: a three-year follow-up study. J Diagn J Diagn Concepts Pract. (2016) 15:487–91. doi: 10.16150/j.1671-2870.2016.05.011
79. Lu Y, Wang P, Zhou T, Lu J, Spatz ES, Nasir K, et al. Comparison of prevalence, awareness, treatment, and control of cardiovascular risk factors in China and the United States. J Am Heart Sociation. (2018) 7:e007462. doi: 10.1161/jaha.117.007462
80. Opoku S, Gan Y, Yobo EA, Tenkorang-Twum D, Yue W, Wang Z, et al. Awareness, treatment, control, and determinants of dyslipidemia among adults in China. Sci Rep. (2021) 11:10056. doi: 10.1038/s41598-021-89401-2
81. Li J, Wang L, Mi S, Zhang M, Li Y, Jiang Y, et al. Awareness rate, treatment rate and control rate of dyslipidemia in Chinese adults, 2010. Chin J Prev Me. (2012) 2012:08. doi: 10.3760/cma.j.issn.0253-9624.2012.08.004
82. Lin L, Deng KQ, Chen Z, Lei F, Qin JJ, Huang X, et al. Lipoprotein(a) distribution and its association with carotid arteriopathy in the Chinese population. Atherosclerosis. (2023) 372:1–9. doi: 10.1016/j.atherosclerosis.2023.03.007
83. Guo C, Cao H, Shan G, Zhao W, Zhang H, Niu K, et al. Elevated lipoprotein(a) and risk of coronary heart disease according to different lipid profiles in the general Chinese community population: the CHCN-BTH study. Ann Transl Med. (2021) 9:26. doi: 10.21037/atm-20-3899
84. Xuan L, Wang T, Dai H, Wang B, Xiang J, Wang S, et al. Serum lipoprotein (a) associates with a higher risk of reduced renal function: a prospective investigation. J Lipid Res. (2020) 61:1320–7. doi: 10.1194/jlr.RA120000771
85. Niu DR, Liu YQ, Ju Y, Shao J, Wang ZJ, Fan WH. Investigation and analysis of serum lipoprotein (a) levels in the population of Shandong province. Int J Lab Med. (2018) 39:354–6. doi: 10.3969/j.issn.1673-4130.2018.03.030
86. Li YY, Li QL, Huang W. Investigation and comprehensive analysis on serum Lipoprotein (a) reference ranges in Chinese health population. Fujian Med J. (2014) 36:128–30.
87. Chen JW, Chen BJ, Lu CH. Investigation on Serum lipoprotein (a) levels in healthy population in Guangzhou province. Psychologies Magazine. (2019) 14:235–7. doi: 10.19738/j.cnki.psy.2019.24.215
88. Huang Y, Gao L, Xie X, Tan SC. Epidemiology of dyslipidemia in Chinese adults: meta-analysis of prevalence, awareness, treatment, and control. Popul Health Metr. (2014) 12:28. doi: 10.1186/s12963-014-0028-7
89. Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, et al. A re-search agenda for aging in China in the 21st century. Ageing Res Rev. (2015) 24:197–205. doi: 10.1016/j.arr.2015.08.003
90. Li R, Cheng X, Schwebel DC, Yang Y, Ning P, Cheng P, et al. Disability-adjusted life years associated with population ageing in China, 1990-2017. BMC Geriatr. (2021) 21:369. doi: 10.1186/s12877-021-02322-7
91. Liu S, Zhang M, Yang L, Li Y, Wang L, Huang Z, et al. Prevalence and patterns of tobacco smoking among Chinese adult men and women: findings of the 2010 national smoking survey. J Epidemiol Community Health. (2017) 71:154–61. doi: 10.1136/jech-2016-207805
92. Han A, Sun T, Ming J, Chai L, Liao X. Are the Chinese moving toward a healthy diet? Evidence from macro data from 1961 to 2017. Int J Environ Res Public Health. (2020) 17:5294. doi: 10.3390/ijerph17155294
93. Menhas R, Dai J, Ashraf MA, Noman SM, Khurshid S, Mahmood S, et al. Physical inactivity, non-communicable diseases and national fitness plan of China for physical activity. Risk Manag Healthc Policy. (2021) 14:2319–31. doi: 10.2147/RMHP.S258660
94. Zhu B, Zhou J, Chen Y, Xu K, Wu Y, Wang Y, et al. Incidence rate, risk factors and behaviour changes for alcohol drinking: findings from a community-based cohort study in southwest China. BMJ Open. (2022) 12:e060914. doi: 10.1136/bmjopen-2022-060914
95. Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. (2010) 140:226–35. doi: 10.1016/j.ijcard.2008.11.033
96. Boo S, Yoon YJ, Oh H. Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database: a cross-sectional analysis. Medicine (Baltimore). (2018) 97:e13713. doi: 10.1097/MD.0000000000013713
97. Fujiyoshi N, Arima H, Satoh A, Ojima T, Nishi N, Okuda N, et al. Associations between socioeconomic Status and the prevalence and treatment of hypercholesterolemia in a general Japanese population: nIPPON DATA2010. J Atheroscler Thromb. (2018) 25:606–20. doi: 10.5551/jat.42531
98. Wu Y, Huxley R, Li L, Anna V, Xie G, Yao C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China national nutrition and health survey 2002. Circulation. (2008) 118:2679–86. doi: 10.1161/CIRCULATIONAHA.108.788166
99. Yang W, Xiao J, Yang Z, Ji L, Jia W, Weng J, et al. Serum lipids and lipoproteins in Chinese men and women. Circulation. (2012) 125:2212–21. doi: 10.1161/circulationaha.111.065904
100. Song P, Wang H, Xia W, Chang X, Wang M, An L. Prevalence and correlates of hyperuricemia in the middle-aged and older adults in China. Sci Rep. (2018) 8(1):4314. doi: 10.1038/s41598-018-22570-9
101. Zhao W, Zhang J, You Y, Man QQ, Li H, Wang CR, et al. Epidemiologic characteristics of dyslipidemia in people aged 18 years and over in China. Chin J Pre Me. (2005) 5:12–6.
102. Dai J, Min JQ, Yang YJ. Epidemic characteristics of dyslipidemia among adults in nine provinces and cities of China. Chin J Hypertens. (2019) 27:300. doi: 10.16439/j.cnki.1673-7245.2019.03.033
103. Li S, Zhang L, Wang X, Chen Z, Dong Y, Zheng C, et al. Status of dyslipidemia among adults aged 35 years and above in China. Chin Circ J. (2019) 34:681–7.
104. Liu X, Wu W, Mao Z, Huo W, Tu R, Qian X, et al. Prevalence and influencing factors of overweight and obesity in a Chinese rural population: the Henan rural cohort study. Sci Rep. (2018) 8: 13101. doi: 10.1038/s41598-018-31336-2
105. Chen H, Zhang X, Feng Q, Zeng Y. The effects of “diet-smoking-gender” three-way interactions on cognitive impairment among Chinese older adults. Nutrients. (2022) 14:2144. doi: 10.3390/nu14102144
106. Xu SH, Qiao N, Huang JJ, Sun CM, Cui Y, Tian SS, et al. Gender differences in dietary patterns and their association with the prevalence of metabolic syndrome among Chinese: a cross-sectional study. Nutrients. (2016) 8:180. doi: 10.3390/nu8040180
107. Li ZR, Ruan HF, Shen LP, Zhang XP, Wan LH. Gender difference in the association between stroke knowledge and health behavior before the onset of stroke among Chinese hypertensive patients. J Neurosci Nurs. (2021) 53:160–5. doi: 10.1097/JNN.0000000000000599
108. Mao Z, Wu B. Urban-rural, age and gender differences in health behaviours in the Chinese population: findings from a survey in Hubei, China. Public Health. (2007) 121:761–4. doi: 10.1016/j.puhe.2007.02.015
109. Reddy Kilim S, Chandala SR. A comparative study of lipid profile and oestradiol in pre- and post-menopausal women. J Clin Diagn Res. (2013) 7:1596–8. doi: 10.7860/JCDR/2013/6162.3234
110. Saha KR, Rahman MM, Paul AR, Das S, Haque S, Jafrin W, et al. Changes in lipid profile of postmenopausal women. Mymensingh Med J. (2013) 22:706–11.24292300
111. Li Q, Wu H, Yue W, Dai Q, Liang H, Bian H, et al. Prevalence of stroke and vascular risk factors in China: a nationwide community-based study. Sci Rep. (2017) 7:6402. doi: 10.1038/s41598-017-06691-1
112. Xi Y, Niu L, Cao N, Bao H, Xu X, Zhu H, et al. Prevalence of dyslipidemia and associated risk factors among adults aged >= 35 years in northern China: a cross-sectional study. Bmc Public Health. (2020) 20:1068. doi: 10.1186/s12889-020-09172-9
113. C CM. Overview of obesity in mainland China. Obes Rev. (2008) 9(Suppl 1):14–21. doi: 10.1111/j.1467-789X.2007.00433.x
114. Zhang H, Kwapong WR, Shao MM, Yan JY, Lin XD, Chen BB, et al. Predictors of the prevalence of dyslipidemia and influencing factors for young health examination cohort: a cross-sectional survey. Front Public Health. (2020) 8:400. doi: 10.3389/fpubh.2020.00400
115. Islam N, Rahman MZ, Choudhury S, Afrin L, Rahman S, Aftabuddin M. Prevalence of dyslipidemia and associated factors among the sub-urban Bangladeshi population. Univ Heart J. (2012) 8:15–9. doi: 10.3329/uhj.v8i1.11662
116. Sharma U, Kishore J, Garg A, Garg A, Anand T, Chakraborty M, et al. Dyslipidemia and associated risk factors in a resettlement colony of Delhi. J Clin Lipidol. (2013) 7:653–60. doi: 10.1016/j.jacl.2013.06.003
117. Ding W, Cheng H, Yan Y, Zhao X, Chen F, Huang G, et al. 10-Year Trends in Serum lipid levels and dyslipidemia among children and adolescents from several schools in Beijing, China. J Epidemiol. (2016) 26(12):637–45. doi: 10.2188/jea.JE20140252
118. Varvel S, McConnell JP, Tsimikas S. Prevalence of elevated lp(a) mass levels and patient thresholds in 532 359 patients in the United States. Arterioscler Thromb Vasc Biol. (2016) 36(11):2239–45. doi: 10.1161/ATVBAHA.116.308011
119. Li JJ, Ma CS, Zhao D, Yan XW, Beijing Heart Society and Expert Committee. Lipoprotein(a) and cardiovascular disease in Chinese population: a Beijing heart society expert scientific statement. JACC Asia. (2022) 2(6):653–65. doi: 10.1016/j.jacasi.2022.08.015
120. Willeit P, Ridker PM, Nestel PJ, Simes J, Tonkin AM, Pedersen TR, et al. Baseline and on-statin treatment lipoprotein(a) levels for prediction of cardiovascular events: individual patient-data meta-analysis of statin outcome trials. Lancet. (2018) 392:1311–20. doi: 10.1016/S0140-6736(18)31652-0.
121. Dubé JB, Boffa MB, Hegele RA, Koschinsky ML. Lipoprotein(a): more interesting than ever after 50 years. Curr Opin Lipidol. (2012 Apr) 23(2):133–40. doi: 10.1097/MOL.0b013e32835111d8
122. Lee J, Son H, Ryu OH. Management Status of cardiovascular disease risk factors for dyslipidemia among Korean adults. Yonsei Med J. (2017) 58:326–38. doi: 10.3349/ymj.2017.58.2.326
123. Sadler AE, Belcastro F, Yarleque CR. Hypertension and dyslipidaemia in Argentina: patient journey stages. Int J Gen Med. (2022) 15:7799–808. doi: 10.2147/IJGM.S358476
124. Goff DC, Bertoni AG, Kramer H, Bonds D, Blumenthal RS, Tsai MY, et al. Dyslipidemia prevalence, treatment, and control in the multi-ethnic study of atherosclerosis (MESA)—gender, ethnicity, and coronary artery calcium. Circulation. (2006) 113:647–56. doi: 10.1161/circulationaha.105.552737
125. Zhang X, Dupre ME, Qiu L, Zhou W, Zhao Y, Gu D. Age and sex differences in the association between access to medical care and health outcomes among older Chinese. BMC Health Serv Res. (2018) 18:1004. doi: 10.1186/s12913-018-3821-3
126. de la Sierra A, Pinto X, Guijarro C, Miranda JL, Callejo D, Cuervo J, et al. Prevalence, treatment, and control of hypercholesterolemia in high cardiovascular risk patients: evidences from a systematic literature review in Spain. Adv Ther. (2015) 32:944–61. doi: 10.1007/s12325-015-0252-y
127. Joshi SR, Anjana RM, Deepa M, Pradeepa R, Bhansali A, Dhandania VK, et al. Prevalence of dyslipidemia in urban and rural India: the ICMR-INDIAB study. PLoS One. (2014) 9:e96808. doi: 10.1371/journal.pone.0096808
128. Supiyev A, Nurgozhin T, Zhumadilov Z, Peasey A, Hubacek JA, Bobak M. Prevalence, awareness, treatment and control of dyslipidemia in older persons in urban and rural population in the Astana region, Kazakhstan. BMC Public Health. (2017) 17:651. doi: 10.1186/s12889-017-4629-5
129. Lu Y, Zhang H, Lu J, Ding Q, Li X, Wang X, et al. Prevalence of dyslipidemia and availability of lipid-lowering medications among primary health care settings in China. Jama Network Open. (2021) 4:e2127573. doi: 10.1001/jamanetworkopen.2021.27573
130. Janus ED, Tideman PA, Dunbar JA, Kilkkinen A, Bunker SJ, Philpot B, et al. Dyslipidaemia in rural Australia: prevalence, awareness, and adherence to treatment guidelines in the greater green tri-angle risk factor study. Med J Aust. (2010) 192:127–32. doi: 10.5694/j.1326-5377.2010.tb03449.x
131. Zhao B, He X, Wu J, Yan S. Adherence to statins and its impact on clinical outcomes: a retrospective population-based study in China. BMC Cardiovasc Disord. (2020) 20:282. doi: 10.1186/s12872-020-01566-2
132. Zhao S, Wang Y, Mu Y, Yu B, Ye P, Yan X, et al. Prevalence of dyslipidaemia in patients treated with lipid-lowering agents in China: results of the DYSlipidemia international study (DYSIS). Atherosclerosis. (2014) 235:463–9. doi: 10.1016/j.atherosclerosis.2014.05.916
133. Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, et al. Prospective urban rural epidemiology (PURE) study investigators. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE study): a prospective epidemiological survey. Lancet. (2011) 378(9798):1231–43. doi: 10.1016/S0140-6736(11)61215-4
Keywords: dyslipidemia, prevalence, awareness rate, treatment rate, control rate, Mainland China, meta-analysis
Citation: Xia Q, Chen Y, Yu Z, Huang Z, Yang Y, Mao A and Qiu W (2023) Prevalence, awareness, treatment, and control of dyslipidemia in Chinese adults: a systematic review and meta-analysis. Front. Cardiovasc. Med. 10:1186330. doi: 10.3389/fcvm.2023.1186330
Received: 14 March 2023; Accepted: 14 June 2023;
Published: 5 July 2023.
Edited by:
Zhonghua Sun, Curtin University, AustraliaReviewed by:
Aoming Jin, Capital Medical University, China© 2023 Xia, Chen, Yu, Huang, Yang, Mao and Qiu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yujie Yang eWFuZy55dWppZUBpbWljYW1zLmFjLmNu
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.