1. Introduction
The diameter of the main vessel (MV) tapers at the bifurcation segment, and the stent size is chosen according to the diameter of the distal MV when performing bifurcation lesion stenting. If post-dilation is conducted using a balloon stent of nominal size, the proximal segment of the stent cannot appose adequately to the vessel wall. The proximal optimization technique (POT), proposed by Darremont et al., effectively addresses this problem. During POT, a non-compliant balloon consistent with the proximal diameter of the MV is located precisely at the carina tip cut-plane and dilated at nominal pressure (Figure 1A). Stent under-expansion, malapposition, and deformation can be, therefore, perfectly corrected (Figure 1B). In addition, the stent cell at the side branch (SB) ostium can be enlarged, making rewiring the distal cell plausible. Results from the e-ULTIMASTER registry revealed that POT could reduce the incidence of target lesion failure (TLF) from 6.0% to 4.0% (P < 0.01) (1). Based on these, POT is regarded as a routine maneuver after stenting in a bifurcation lesion (2).
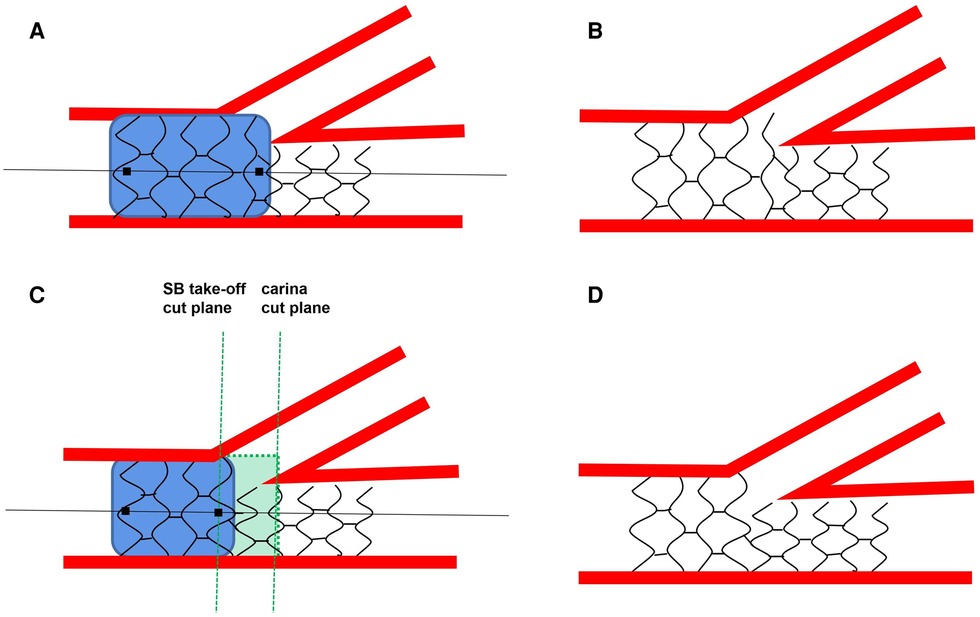
Figure 1. (A,B) the standard method for the proximal optimization technique proposed by the European bifurcation club consensus; (C,D)the protocol for the proximal optimization technique recommended by us.
Multiple bench tests have shown that an accurate POT positioning is crucial to hemodynamics status at the bifurcation site, stent formation, and SB fate. However, achieving an absolutely accurate POT position is often difficult due to the different operators' skills, designs of the POT balloons, and SB ostium residue areas. According to our experience, patients without an absolutely accurate POT also benefited well in the long-term follow-up. Additionally, newly published clinical studies indirectly supported the unnecessity of the strict criterion (3). In this article, we discuss this issue through a comprehensive review of the literature and our experiences in percutaneous coronary intervention for bifurcation lesions.
2. In vitro tests revealed that any inaccuracy was significant
Wu et al. analyzed the effects of three different distal shoulder positionings of POT balloons with a finite element simulation method. The carina cut-plane, “proximal” 1 mm before the carina cut-plane, and “distal” 1 mm after the carina cut-plane were tested. The results showed that the “proximal” 1 mm before the carina cut-plane location yielded the best result in reducing the area of stent strut obstruction at the SB ostium and enlarging the distal stent cell. The “distal” 1 mm after the carina cut-plane location performed worst by increasing the area of high-stress distribution on the vessel's inner surface. In addition, the study concluded that the distal shoulder of the balloon should be located between two stent rings to achieve an enlargement of the distal cell with less resistance (4).
However, a computational test by Zuin et al. reached the opposite conclusion. They suggested that the shoulder of the balloon should be located 1 mm after the carina cut plane to achieve higher wall shear stress and to facilitate neointimal formation (5).
Dérimay et al. conducted a bench test with a fractal model. The optical coherence tomography (OCT) and micro-computed tomography (CT) results favored the carina cut plane since the “proximal” 1 mm before the carina cut-plane location failed to improve SB obstruction, and the “distal” 1 mm before the carina cut-plane location overstretched the distal main vessel (6).
A bench test by Andreasen et al. demonstrated that the final POT after SB dilation or double balloon kissing should be at the proximal SB take-off level because POT beyond the take-off level reduced the stent cell area over the SB ostium (7).
Regardless of the different conclusions drawn from these in vitro tests, they all pointed out that a discrepancy of even 1 mm was significant. In vitro tests provide important instructions for clinical interventions, especially for bifurcation lesions. For example, a bench test of a kissing balloon inflation explained why it could not produce clinical benefits (8). Bench tests of re-POT showed that a second POT was essential to revise stent malapposition caused by SB dilation (9). The FDA has demanded that the safety of all new techniques should be certified through in vitro tests before being applied in the real world. However, gaps remain between in vitro tests and clinical applications (10).
3. Clinical experiences told us absolutely precise positioning of a POT balloon was scarcely possible
Clinical experiences told us that an absolutely precise positioning of a POT balloon is scarcely possible. In most cases, the balloon was adjusted under the guidance of fluoroscopic imaging. Exact locating should be conducted under a projection vertical to the SB take-off, which cannot be achieved all the time. Tu et al. revealed that an optimal projection could only be reached in roughly half of the cases due to the mechanical constraints of the current x-ray systems (11).
Moreover, the location of the balloon shoulder before dilation is unknown. The relationship between distal opaque markers and balloon shoulders varies among brands. If an operator is unfamiliar with a particular brand, it is difficult to achieve ideal positioning. When the shoulders are long outside the marker, unwanted dilation could overstretch the distal MV and cause a carina shift. When the shoulders are inside the marker, insufficient dilation might occur. Besides, it is difficult for an operator to millimetrically control a balloon. Finally, it could slide backward over the wire if the distal part meets resistance when dilating the balloon.
4. Our viewpoint and proposed protocol
POT optimizes stent apposition and expansion, prevents accidental MV abluminal rewiring, and facilitates SB recrossing, which has been validated by bench tests and clinical application of OCT or intravascular ultrasound (IVUS). POT reduced incidences of major adverse cardiac events. Therefore, POT is deemed as standard procedure for the treatment of all coronary bifurcation lesions. POT balloon positioning varies according to bifurcation intervention strategies. For provisional stenting, the distal end of the POT balloon should be placed at the carina plane to open the stent cell covering the SB ostium in the first POT and re-POT. For double stenting, the first POT balloon position is the same as in provisional stenting. However, the balloon should be limited in the proximal MV in double stenting, in case it might influence the middle position of the metal carina formed by the two stents.
Regarding how to perform POT in provisional stenting, several studies have suggested that the stent should be expanded from the carina cut-plane to the proximal stent edge. The 15th EBC consensus document stated, “Of note, bench tests demonstrated that superior results from POT are obtained when the balloon is positioned immediately proximal to the carina. Incorrect placement of the POT balloon too proximal or distal is associated with suboptimal results” (2). Through a review of published in vitro tests, we concluded that any error in the balloon position would lead to unsatisfactory outcomes.
However, in practice, the exact maneuver cannot be achieved in all cases, even under the guidance of IVUS or OCT by a skilled operator. Continuous adjustment is time- and contrast-consuming. A real-world study is needed to validate the in vitro conclusions. Operators must balance the benefits and risks of delicate POT positioning according to the complexity and patient clinical conditions during clinical practice. Besides, we thought that POT positions from the carina tip cut-plane to the SB take-off cut-plane are all reasonable if SB rewiring is not planned (Figures 1C,D). Finally, the importance of using intravascular imaging must be emphasized when dealing with a bifurcation lesion, since it helped to evaluate the lesion severity, make strategy choices, and appraise the stent status. As a result, it helps to reduce adverse events during the procedures and long-term follow-up (12, 13).
5. Conclusions
The previous declaration of precise POT from carina cut-plane was difficult to be realized in clinical practice. We propose that POT positions from the carina tip cut-plane to the SB take-off cut-plane are all reasonable if SB rewiring is not planned. Intravascular imaging is recommended to achieve optimal outcomes. More clinical evidence is needed to validate these viewpoints.
Author contributions
WG is the first corresponding author. WG and DL conceived this opinion. DL wrote the manuscript. JL revised the manuscript. CG, HD, and HL composed the figure and provided insight for this work. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Tangdu Innovative Development Project (2021LCYJ044). The funder played no role in study conception, literature review, or manuscript drafting.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chevalier B, Mamas MA, Hovasse T, Rashid M, Gómez-Hospital JA, Pan M, et al. Clinical outcomes of the proximal optimisation technique (POT) in bifurcation stenting. EuroIntervention. (2021) 17(11):e910–8. doi: 10.4244/EIJ-D-20-01393
2. Burzotta F, Lassen JF, Lefèvre T, Banning AP, Chatzizisis YS, Johnson TW, et al. Percutaneous coronary intervention for bifurcation coronary lesions: the 15th consensus document from the European bifurcation club. EuroIntervention. (2021) 16(16):1307–17. doi: 10.4244/EIJ-D-20-00169
3. Lee CH, Nam C-W, Cho Y-K, Yoon H-J, Kim K-B, Gwon H-C, et al. 5-Year Outcome of simple crossover stenting in coronary bifurcation lesions compared with Side branch opening. JACC Asia. (2021) 1(1):53–64. doi: 10.1016/j.jacasi.2021.04.002
4. Wu H, Li M, Lin C. Influence of balloon location during proximal optimization technique (POT): a finite element analysis. J Biomech. (2021) 127:110703. doi: 10.1016/j.jbiomech.2021.110703
5. Zuin M, Rigatelli G, Chiastra C. Optimal site for proximal optimization technique in Complex coronary bifurcation stenting: a computational fluid dynamics study. Cardiovasc Revasc Med. (2020) 21(7):826–32. doi: 10.1016/j.carrev.2019.12.015
6. Dérimay F, Rioufol G, Nishi T, Kobayashi Y, Fearon WF, Veziers J, et al. Optimal balloon positioning for the proximal optimization technique? An experimental bench study. Int J Cardiol. (2019) 292:95–7. doi: 10.1016/j.ijcard.2019.05.041
7. Andreasen LN, Holm NR, Webber B, Ormiston JA. Critical aspects of balloon position during final proximal optimization technique (POT) in coronary bifurcation stenting. Catheter Cardiovasc Interv. (2020) 96(1):31–9. doi: 10.1002/ccd.28801
8. Finet G, Derimay F, Motreff P, Guerin P, Pilet P, Ohayon J, et al. Comparative analysis of sequential proximal optimizing technique versus kissing balloon inflation technique in provisional bifurcation stenting. JACC Cardiovasc Interv. (2015) 8(10):1308–17. doi: 10.1016/j.jcin.2015.05.016
9. Çetinkal G, Balaban Koçaş B, Keskin K, Kilci H, Ser ÖS, Kılıçkesmez K. Comparison of sequential POT-side-POT and kissing balloon techniquesin patients with coronary bifurcation lesions treated with single-stent strategy; which one is simple and safe? Propensity score analysis[J]. Anatol J Cardiol. (2022) 26(7):559–66. doi: 10.5152/AnatolJCardiol.2022.1136
10. Ormiston J, Kassab G, Finet G, Chatzizisis Y, Foin N, Mickley T, et al. Bench testing and coronary artery bifurcations: a consensus document from the European bifurcation club. EuroIntervention. (2018) 13(15):e1794–1803. doi: 10.4244/EIJ-D-17-00270
11. Tu S, Jing J, Holm NR, Onsea K, Zhang T, Adriaenssens T, et al. In vivo assessment of bifurcation optimal viewing angles and bifurcation angles by three-dimensional (3D) quantitative coronary angiography. Int J Cardiovasc Imaging. (2012) 28(7):1617–25. doi: 10.1007/s10554-011-9996-x
12. Onuma Y, Katagiri Y, Burzotta F, Holm NR, Amabile N, Okamura T, et al. Joint consensus on the use of OCT in coronary bifurcation lesions by the European and Japanese bifurcation clubs. EuroIntervention. (2019) 14(15):e1568–77. doi: 10.4244/EIJ-D-18-00391
Keywords: bench test, coronary bifurcation lesion, in vitro test, proximal optimization technique, PCI
Citation: Li D, Gao C, Dai H, Liu H, Li J and Guo W (2023) Must absolutely accurate balloon position be achieved during POT? More in vitro tests, but less clinical evidence. Front. Cardiovasc. Med. 10:1166020. doi: 10.3389/fcvm.2023.1166020
Received: 14 February 2023; Accepted: 28 April 2023;
Published: 17 May 2023.
Edited by:
Hiroki Teragawa, JR Hiroshima Hospital, JapanReviewed by:
Dobrin Vassilev, University of Ruse, BulgariaToru Naganuma, New Tokyo Hospital, Japan
Satoru Mitomo, New Tokyo Hospital, Japan
© 2023 Li, Gao, Dai, Liu, Li and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinjing Li bGpqMTk5MTAyMDNAMTYzLmNvbQ== Wangang Guo d2dfZ3VvQGZtbXUuZWR1LmNu
†These authors have contributed equally to this work
Abbreviations MV, main vessel; POT, proximal optimization technique; SB, side branch; TLF, target lesion failure; CT, computed tomography; OCT, optical coherence tomography; IVUS, intravascular ultrasound.
 Dongdong Li
Dongdong Li Chuncheng Gao†
Chuncheng Gao† Hao Liu
Hao Liu Jinjing Li
Jinjing Li