
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Cardiovasc. Med., 10 May 2023
Sec. Cardiac Rhythmology
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1165011
This article is part of the Research TopicMethods in Treating Heart Failure - Device and Surgery ApproachView all 16 articles
Background: The benefit of catheter ablation vs. medical treatment has been reported to be inconsistent in randomized controlled trials (RCTs) for patients with atrial fibrillation (AF) and heart failure (HF) due to different enrollment criteria. This meta-analysis aimed to decipher the differential outcomes stratified by different left ventricular ejection fractions (LVEFs) and AF types.
Methods: We searched PubMed, Embase, ProQuest, ScienceDirect, Cochrane Library, ClinicalKey, Web of Science, and ClinicalTrials.gov databases for RCTs comparing medical treatment and catheter ablation in patients with AF and HF published before March 31, 2023. Nine studies were included.
Results: When patients were stratified by LVEF, improved LVEF and 6-min walk distance, less AF recurrence, and lower all-cause mortality in favor of catheter ablation were observed in patients with LVEF ≤50% but not in patients with LVEF ≤35%, and short HF hospitalization was observed in patients with LVEF ≤50% and LVEF ≤35%. When patients were stratified by AF types, improved LVEF and 6-min walk distance, better HF questionnaire score, and short HF hospitalization in favor of catheter ablation were observed both in patients with nonparoxysmal AF and mixed AF (paroxysmal and persistent) and less AF recurrence and lower all-cause mortality in favor of catheter ablation were observed in only patients with mixed AF.
Conclusions: This meta-analysis showed improved LVEF and 6-min walk distance, less AF recurrence, and lower all-cause mortality in favor of catheter ablation vs. medical treatment in AF patients with HF and LVEF of 36%–50%. Compared with medical treatment, catheter ablation improved LVEF and had better HF status in patients with nonparoxysmal AF and mixed AF; however, AF recurrence and all-cause mortality in favor of catheter ablation were observed in only HF patients with mixed AF.
The prevalence of atrial fibrillation (AF) and heart failure (HF) has increased globally (1). Advanced age and underlying structural heart disease are risk factors for AF and HF, which may develop sequentially or coincidentally (2). Patients with both conditions have worse outcomes and a higher risk of adverse clinical events (3, 4). Therefore, appropriate management of AF and HF is important to reduce morbidity and mortality in patients with AF and HF. One randomized controlled study showed that catheter ablation had a low reported rate of restoring sinus rhythm and did not improve N-terminal pro-B-type natriuretic peptide, 6-min walk distance, or quality of life in patients with persistent AF and HF when compared with rate control (5). However, several randomized controlled studies showed significant benefits from catheter ablation vs. rate control in terms of objective exercise performance, clinical symptoms, neurohormonal status, left ventricular ejection fraction (LVEF), unplanned hospitalization, and mortality in patients with persistent AF and HF (6–8). One randomized controlled trial (RCT) reported that catheter ablation was associated with a significantly lower rate of all-cause mortality or hospitalization for worsening HF than rhythm and rate control therapy in patients with paroxysmal and persistent AF and HF, especially in patients with LVEF ≥ 25% (9). One study reported that timely treatment of arrhythmia-mediated cardiomyopathy might minimize irreversible ventricular remodeling in patients with persistent AF and HF related to LV systolic dysfunction (LVEF ≤ 45%) (10). However, another RCT reported that catheter ablation did not improve LVEF compared with the best medical treatment in HF patients with persistent AF and LVEF ≤ 35% (11). In the subgroup analysis of the CABANA study, catheter ablation produced clinically important improvements in survival, freedom from AF recurrence, and quality of life compared with drug therapy in patients with paroxysmal or persistent AF and clinically stable heart failure with a mean LVEF of 55% (12). However, another open-label study showed no difference in all-cause mortality or HF events between catheter ablation and rate control in patients with high-burden paroxysmal AF or persistent AF and HF symptoms (13). Therefore, the benefit of catheter ablation vs. medical treatment has been reported to be inconsistent in patients with AF and HF regarding clinical symptoms and outcomes. The discrepancy in outcomes between catheter ablation and medical treatment in patients with AF and HF may be due to different inclusion criteria in terms of HF diagnostic criteria and LVEF and AF types. Therefore, this meta-analysis aimed to decipher the differential outcomes of catheter ablation vs. medical treatment in patients with AF and HF, stratified by different LVEFs, New York Heart Association (NYHA) class ≥ II, and different AF types.
Two cardiologists (W-CL and H-YF) performed a systematic literature search of the PubMed, Embase, ProQuest, ScienceDirect, Cochrane Library, ClinicalKey, Web of Science, and ClinicalTrials.gov databases for articles published before March 31, 2023. The databases were searched for relevant studies without language restrictions using the key terms “atrial fibrillation,” “heart failure,” “catheter ablation,” and “medical treatment.” Disagreements were resolved by a third reviewer (P-JW). This study included different RCTs that compared the efficacies of catheter ablation and medical treatment in patients with AF and HF. The inclusion criteria were a human study with parallel design and comparison of the efficacy of catheter ablation and medical treatment in patients with AF and HF. The exclusion criteria were case reports or series, animal studies, review articles, conference abstracts, unpublished data, and observational studies. We did not set language limitations to increase the number of eligible articles. Supplementary Figure S1 illustrates the literature search and screening protocol.
The outcomes of interest in this study were the change in LVEF, 6-min walk distance, HF questionnaire score, change in brain natriuretic peptide (BNP), AF recurrence, HF hospitalization, and all-cause mortality.
The frequency of each evaluated outcome was extracted from each study, and the data were presented as cumulative rates. A random-effects model was employed to pool the individual odds ratio (OR), and all analyses were performed using Comprehensive Meta-Analysis software version 3 (Biostat, Englewood, NJ, United States). To assess the heterogeneity across trials, we used the chi-squared test (values of p ≤ 0.10 were considered significant) and I2 statistics to examine each outcome from low to high heterogeneity (25%–75%, respectively). Potential publication bias was assessed using Egger's test via funnel plots, and statistical significance was set at p ≤ 0.10. Statistical significance was set at p < 0.05 to compare the catheter ablation and medical treatment groups.
The study selection process is illustrated in Supplementary Figure S1. Nine studies met our inclusion criteria. The study design, study period, participant characteristics, AF type, HF criteria, mean LVEF, and follow-up period are described in Table 1. A total of 2,074 participants (mean age, 65 ± 7.6 years; 70.9% men) were included. Most participants in these studies had nonparoxysmal AF (68%–100%). The enrollment criterion for HF trial patients in four studies was LVEF ≤ 35% (5, 6, 9, 11). In another three studies, different LVEF values were used to enroll HF patients, including ≤50% (7), ≤40% (8), and ≤45% (10). The remaining two studies did not declare the LVEF cutoff value for enrollment and used only a history of NYHA functional classification ≥II as the enrollment criteria (12, 13).
Table 2 describes the details of patients’ demographics between the medical treatment and catheter ablation groups of the enrolled study patients. The mean age, sex, NYHA functional classification, prevalence of diabetes mellitus, hypertension, prior stroke, ischemic cardiomyopathy, implantable cardioverter defibrillator, cardiac resynchronization therapy placement, nonparoxysmal AF, AF duration, mean LVEF, and use of HF medications did not differ significantly between the medical treatment and catheter ablation groups.
Pooled results from the random-effects model showed that catheter ablation for AF, compared with medical treatment, was associated with an increased LVEF from baseline [mean difference 6.22%; 95% confidence interval (CI), 3.59%–8.86%] with high heterogeneity (Cochran's Q, 294.657; df, 7; I2, 97.624%; p < 0.001) (Figure 1A). Egger's test revealed nonsignificant publication bias in the change in LVEF (t, 0.309; df, 6; p = 0.767). The funnel plot of the change in LVEF is shown in Supplementary Figure S2. Pooled results from the random-effects model showed that catheter ablation vs. medical treatment was associated with an increased 6-min walk distance from baseline (mean difference, 0.97 m; 95% CI, 0.27–1.67 m), with high heterogeneity (Cochran's Q, 94.559; df, 5; I2, 94.712%; p < 0.001) (Figure 1B). Egger's test revealed a nonsignificant publication bias regarding the change in the 6-min walk distance (t, 0.782; df, 4; p = 0.478). The funnel plot for the change in the 6-min walk distance is shown in Supplementary Figure S3. Pooled results from the random-effects model showed that catheter ablation vs. medical therapy was associated with an improved HF questionnaire score from baseline (mean difference, 0.86; 95% CI, 0.35–1.37) with high heterogeneity (Cochran's Q, 55.150; df, 5; I2, 90.934%; p < 0.001) (Figure 1C). Egger's test showed a nonsignificant publication bias in the change in the HF questionnaire score (t, 0.028; df, 4; p = 0.979). The funnel plot for the change in HF questionnaire score is shown in Supplementary Figure S4. Pooled results from the random-effects model showed that catheter ablation vs. medical treatment was associated with significant change in the BNP level from baseline (mean difference, 2.58 pg/ml, 95% CI, 0.97–4.20 pg/ml) with high heterogeneity (Cochran's Q, 233.478; df, 5; I2, 97.858%; p < 0.001) (Figure 1D). Egger's test revealed a nonsignificant publication bias for the change in the BNP level (t, 0.392; df, 4; p = 0.715). The funnel plot for the change in the BNP level is shown in Supplementary Figure S5. The overall OR of the recurrence of AF of the catheter ablation group vs. medical treatment was 4.26 (95% CI, 1.34–13.55) in favor of catheter ablation (Figure 1E) with high heterogeneity (Cochran's Q, 112.389; df, 4; I2, 96.441%; p < 0.001). Egger's test revealed nonsignificant publication bias regarding the overall OR of AF recurrence (t, 0.382; df, 3; p = 0.728). A funnel plot for the log OR of AF recurrence is shown in Supplementary Figure S6. The overall OR of the HF hospitalization of catheter ablation vs. medical treatment was 1.72 (95% CI, 1.22–2.42) in favor of catheter ablation (Figure 1F) with moderate heterogeneity (Cochran's Q, 7.991; df, 4; I2, 49.946%; p = 0.092). Egger's test revealed a nonsignificant publication bias regarding the overall OR of hospitalization for HF (t, 0.180; df, 3; p = 0.869). A funnel plot for the log OR of HF hospitalization is shown in Supplementary Figure S7. The overall OR of the incidence of all-cause mortality of catheter ablation vs. medical treatment was 1.65 (95% CI, 1.25–2.20) in favor of catheter ablation (Figure 1G) with low heterogeneity (Cochran's Q, 3.622; df, 4; I2, 0%; p = 0.460). Egger's test revealed a nonsignificant publication bias regarding the overall OR of all-cause mortality (t, 0.215; df, 3; p = 0.844). The funnel plot for the log OR of all-cause mortality is shown in Supplementary Figure S8.
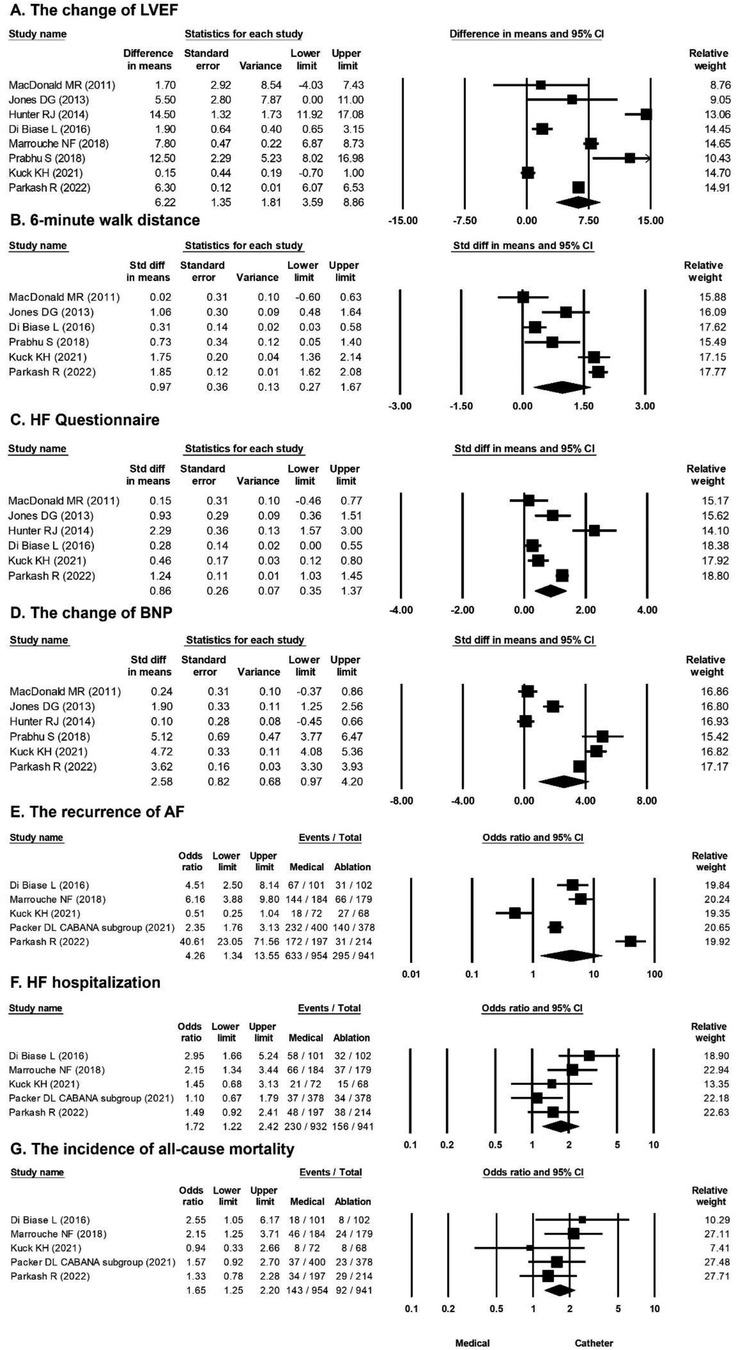
Figure 1. Forest plots comparing the changes in LVEF, 6-min walk distance, HF questionnaire score, BNP level, odds ratio for AF recurrence, odds ratio for HF hospitalization, and odds ratio for all-cause mortality of medical treatment versus catheter ablation. (A) Change of LVEF in eight studies. (B) 6-min walk distance in six studies. (C) HF questionnaire in six studies. (D) Change of BNP level in six studies. (E) AF recurrence rate in five studies. (F) HF hospitalization rate in five studies. (G) All-cause mortality rate in five studies. AF, atrial fibrillation; BNP, B-type natriuretic peptide; HF, heart failure; LVEF, left ventricular ejection fraction.
A greater improvement in LVEF in favor of catheter ablation vs. medical treatment was observed in the population with LVEF ≤50% (mean difference, 9.54%; 95% CI, 0.04%–19.04%) but not in the population with LVEF ≤35% (Figure 2A). A longer 6-min walk distance in favor of catheter ablation vs. medical treatment was observed in the population with LVEF ≤50% (mean difference, 0.40 m; 95% CI, 0.03–0.75 m), but not in the population with LVEF ≤35% (Figure 2B). Interestingly, a greater improvement in HF questionnaire scores in favor of catheter ablation vs. medical treatment was observed in the population with LVEF ≤35% (mean difference, 0.51; 95% CI, 0.14–0.89) but not in the population with LVEF ≤50% (Figure 2C). There was no significant difference in the change in the BNP level between catheter ablation and medical treatment in the population with LVEF ≤35% (mean difference, 2.29 pg/ml; 95% CI, −0.30 to 4.87 pg/ml) and in the population with LVEF ≤50% (mean difference, 2.57 pg/ml; 95% CI, −2.34 to 7.48 pg/ml) (Figure 2D). The risk of recurrence of AF was significantly lower by catheter ablation compared with medical treatment in the population with LVEF ≤50% (OR, 4.51; 95% CI, 2.50–8.14) but not in the population with LVEF ≤35% (Figure 2E). The overall OR values of HF hospitalization were 1.93 (95% CI, 1.29–2.88), in favor of catheter ablation vs. medical treatment in the population with LVEF ≤35%, and 2.95 (95% CI, 1.66–5.24), also in favor of catheter ablation vs. medical treatment in the population with LVEF ≤50% (Figure 2F). The incidence of all-cause mortality was significantly lower by catheter ablation compared with medical treatment in the population with LVEF ≤50% (OR, 2.55; 95% CI, 1.05–6.17) but not in the population with LVEF ≤35% (Figure 2G).
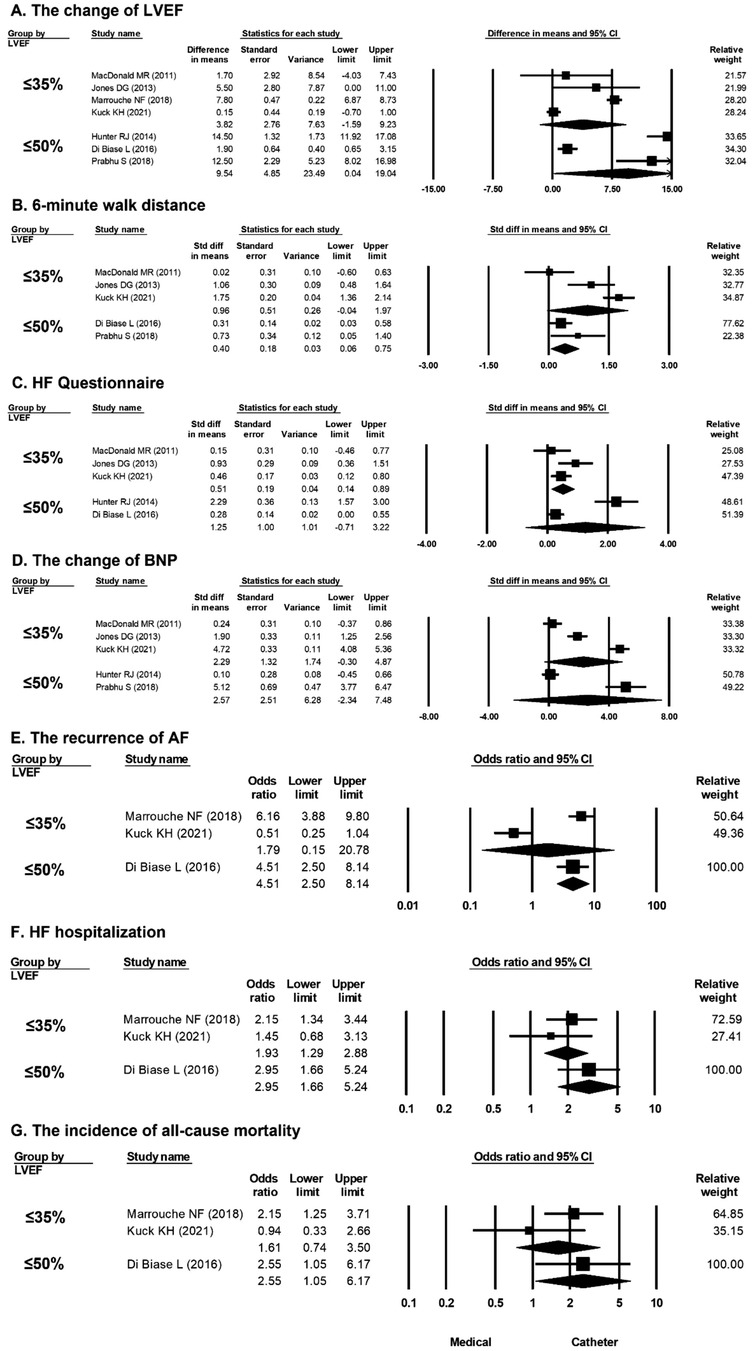
Figure 2. Forest plots comparing the changes in LVEF, 6-min walk distance, HF questionnaire score, BNP level, odds ratio for AF recurrence, odds ratio for HF hospitalization, and odds ratio for all-cause mortality of medical treatment versus catheter ablation in patients stratified by LVEF (LVEF ≤ 35% and LVEF ≤ 50%). (A) Change in LVEF in seven studies (≤35% in four, ≤50% in three). (B) 6-min walk distance in five studies (LVEF ≤ 35% in three, LVEF ≤ 50% in two). (C) HF questionnaire score in five studies (LVEF ≤ 35% in three, LVEF ≤ 50% in two). (D) BNP level in five studies (LVEF ≤ 35% in three, LVEF ≤ 50% in two). (E) AF recurrence in three studies (LVEF ≤ 35% in two, LVEF ≤ 50% in one). (F) HF hospitalization in three studies (LVEF ≤ 35% in two, LVEF ≤ 50% in one). (G) All-cause mortality rate in three studies (LVEF ≤ 35% in two, LVEF ≤ 50% in one). AF, atrial fibrillation; BNP, B-type natriuretic peptide; HF, heart failure; LVEF, left ventricular ejection fraction.
A greater improvement in LVEF in favor of catheter ablation vs. medical treatment was observed in the population with HF history (mean difference, 6.30%; 95% CI, 6.07%–6.53%) (Figure 3A). A longer 6-min walk distance in favor of catheter ablation vs. medical treatment was observed in the population with HF history (mean difference, 1.85 m; 95% CI, 1.62–2.08 m) (Figure 3B). A greater improvement in HF questionnaire scores in favor of catheter ablation vs. medical treatment was observed in the population with HF history (mean difference, 1.24; 95% CI, 1.03–1.45) (Figure 3C). A significant difference in the change in the BNP level in favor of catheter ablation vs. medical treatment was observed in the population with HF history (mean difference, 3.62 pg/ml; 95% CI, 3.30–3.93 pg/ml) (Figure 3D). There was no significant difference in the recurrence of AF, HF hospitalization, and all-cause mortality between catheter ablation and medical treatment in the population with HF history of NYHA ≥II (Figures 3E–G).
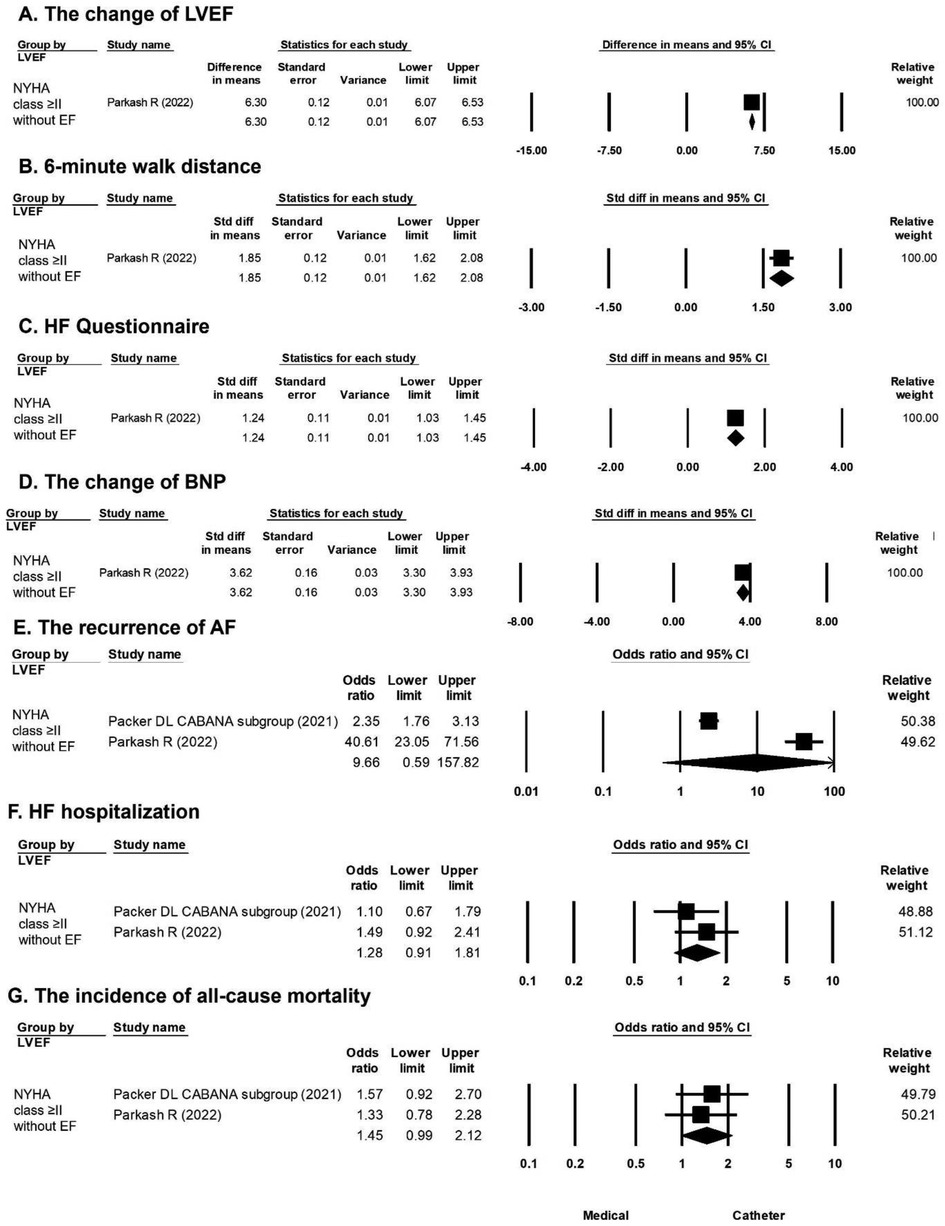
Figure 3. Forest plots comparing the changes in LVEF, 6-min walk distance, HF questionnaire score, BNP level, odds ratio for AF recurrence, odds ratio for HF hospitalization, and odds ratio for all-cause mortality of medical treatment versus catheter ablation in patients stratified by NYHA ≥ II without LVEF. (A) Change in LVEF in one study. (B) 6-min walk distance in one study. (C) HF questionnaire score in one study. (D) BNP level in one study. (E) AF recurrence in two studies. (F) HF hospitalization in two studies. (G) All-cause mortality rate in two studies. AF, atrial fibrillation; BNP, B-type natriuretic peptide; HF, heart failure; LVEF, left ventricular ejection fraction.
Mixed AF was defined as the study population with paroxysmal and persistent AF (14). A greater improvement in LVEF in favor of catheter ablation vs. medical treatment was observed in the population with nonparoxysmal AF (mean difference, 3.68%; 95% CI, 0.82%–6.54%) and mixed AF (mean difference, 9.07%; 95% CI, 6.46%–11.69%) (Figure 4A). A longer 6-min walk distance in favor of catheter ablation vs. medical treatment was observed in the population with nonparoxysmal AF (mean difference, 0.78 m; 95% CI, 0.11–1.45 m) and mixed AF (mean difference, 1.85 m; 95% CI, 1.62–2.08 m) (Figure 4B). A greater improvement in HF questionnaire scores in favor of catheter ablation vs. medical treatment was observed in the population with nonparoxysmal AF (mean difference, 0.42; 95% CI, 0.16–0.68) and mixed AF (mean difference, 1.70; 95% CI, 0.68–2.72) (Figure 4C). A significant difference in the change in the BNP level in favor of catheter ablation vs. medical treatment was observed in the population with nonparoxysmal AF (mean difference, 2.96 pg/ml; 95% CI, 0.68–5.24 pg/ml) but not in the population with mixed AF (Figure 4D). The risk of recurrence of AF was significantly lower by catheter ablation compared with medical treatment in the population with mixed AF (OR, 8.25; 95% CI, 1.74–39.19) but not in the population with nonparoxysmal AF (Figure 4E). The overall OR values of HF hospitalization in favor of catheter ablation vs. medical treatment were 2.17 (95% CI, 1.09–4.32) in the population with nonparoxysmal AF and 1.53 (95% CI, 1.04–2.23) in the population with mixed AF (Figure 4F). The incidence of all-cause mortality was significantly lower by catheter ablation compared with medical treatment in the population with mixed AF (OR, 1.65; 95% CI, 1.21–2.25) but not in the population with nonparoxysmal AF (Figure 4G).
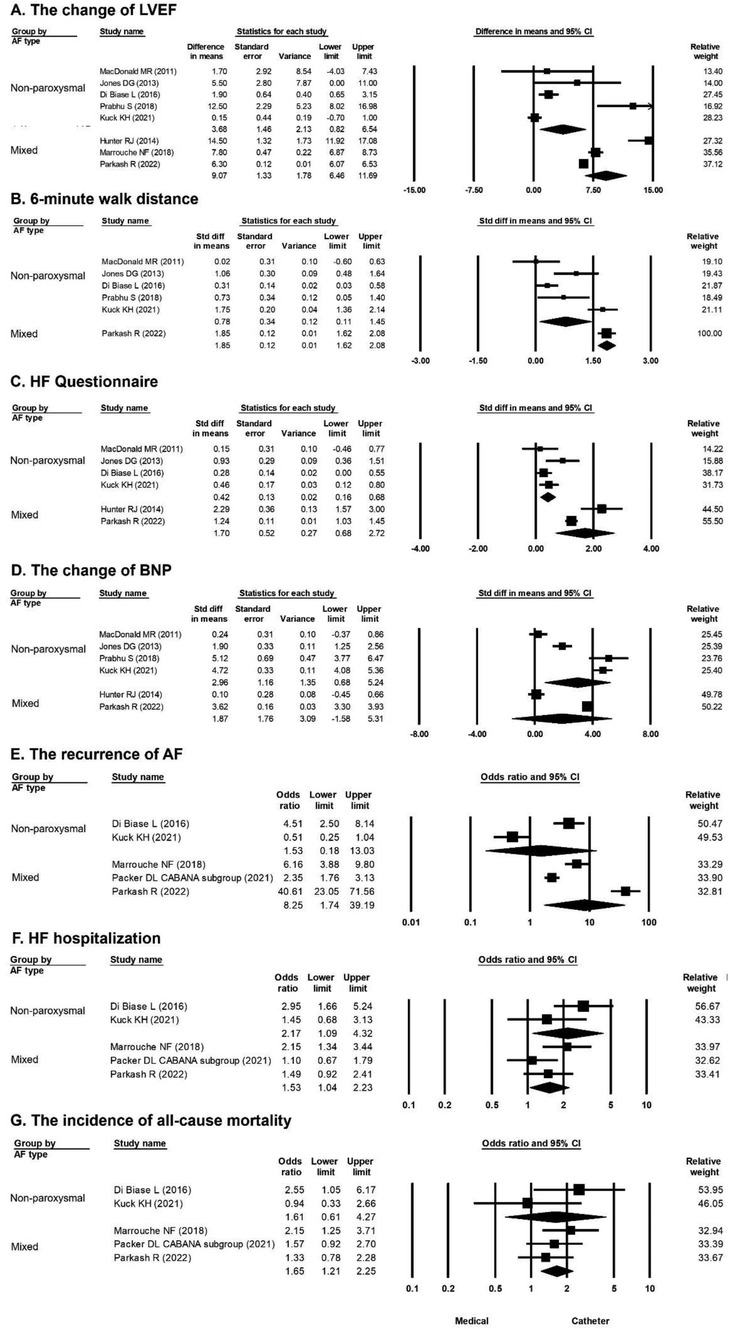
Figure 4. Forest plots comparing the changes of LVEF, 6-min walk distance, HF questionnaire score, BNP level, odds ratio for AF recurrence, odds ratio for HF hospitalization, and odds ratio for all-cause mortality of medical treatment versus catheter ablation in patients stratified by different AF types (nonparoxysmal and mixed AF). (A) Change in LVEF in eight studies (nonparoxysmal AF in five, mixed AF in three). (B) 6-min walk distance in six studies (nonparoxysmal AF in five, mixed AF in one). (C) HF questionnaire score in six studies (nonparoxysmal AF in four, mixed AF in two). (D) BNP level in six studies (nonparoxysmal AF in four, mixed AF in two). (E) AF recurrence rate in five studies (nonparoxysmal AF in two, mixed AF in three). (F) HF hospitalization rate in five studies (nonparoxysmal AF in two, mixed AF in three). (G) All-cause mortality rate in five studies (nonparoxysmal AF in two, mixed AF in three). AF, atrial fibrillation; BNP, B-type natriuretic peptide; HF, heart failure; LVEF, left ventricular ejection fraction.
In the whole study population of this meta-analysis, improved LVEF, improved 6-min walk distance, better HF questionnaire score, significantly decreased BNP level, less AF recurrence, less HF hospitalization, and lower all-cause mortality were observed after catheter ablation vs. medical treatment. When the study population was stratified by LVEF, improved LVEF, improved 6-min walk distance, less AF recurrence, and lower all-cause mortality in favor of catheter ablation vs. medical treatment were observed in the population with LVEF ≤50% but not in the population with LVEF ≤35%; however, less HF hospitalization was observed both in the population with LVEF ≤50% and LVEF ≤35%. When the study population was stratified by HF NYHA ≥II, improved LVEF, improved 6-min walk distance, and better HF questionnaire score in favor of catheter ablation vs. medical treatment were observed in the population with HF NYHA ≥II. When the study population was stratified by AF types, improved LVEF, improved 6-min walk distance, better HF questionnaire score, and less HF hospitalization in favor of catheter ablation vs. medical treatment were observed both in the population with nonparoxysmal AF and mixed AF; however, less AF recurrence and lower all-cause mortality in favor of catheter ablation vs. medical treatment were observed only in the population with mixed AF.
The criteria for HF in the enrolled studies differed in LVEF cutoff values, ranging from LVEF ≤35% (5, 6, 9, 11) to ≤40% (8), ≤45% (10), and ≤50% (7) or differed in only enrolling patients with a history of HF with NYHA functional classification ≥II without mention LVEF (12, 13). According to our meta-analysis, improved LVEF, improved 6-min walk distance, less AF recurrence, and lower all-cause mortality in favor of catheter ablation vs. medical treatment were observed in the population with LVEF of 36%–50% and less HF hospitalization was observed both in the population with LVEF ≤ 50%, and LVEF ≤35%.
In patients with HF and reduced LVEF, a high prevalence of persistent AF exists and is closely related to underlying heart disease severity and HF functional classes (15). In the enrolled studies of this meta-analysis, the prevalence of nonparoxysmal AF was 68%–100%. Previous meta-analyses comparing catheter ablation vs. medical treatment in terms of clinical outcomes in patients with AF and HF did not specifically stratify the study subjects by different AF types (16, 17). However, the long-term efficacy of catheter ablation vs. medical treatment for different AF types on clinical outcomes may differ and may require more than one catheter ablation procedure for different AF types (18). In this meta-analysis, improved LVEF, improved 6-min walk distance, better HF questionnaire score, and less HF hospitalization in favor of catheter ablation vs. medical treatment were observed both in the population with nonparoxysmal AF and mixed AF; however, AF recurrence and all-cause mortality in favor of catheter ablation vs. medical treatment were only observed in the population with mixed AF but not in the population with nonparoxysmal AF. Nonparoxysmal AF may contribute to more atrial and ventricular structural remodeling and atrial fibrosis, reducing the benefit of catheter ablation for AF, especially in HF patients. Therefore, catheter ablation could achieve more clinical benefits in patients with mixed AF than in patients with nonparoxysmal AF.
This study had several limitations. First, the enrollment criteria for HF differed among the nine enrolled studies, and high heterogeneity was found in the analyses of the whole population. Therefore, we performed subgroup analyses, and patients were stratified by different LVEFs, HF history of NYHA ≥ II, and AF types. Second, the use of HF biomarkers differed among six studies, three (6, 7, 10) used serum BNP and the other three (5, 11, 13) used N-terminal proBNP. Third, although nine studies were included, over one-third of the 2,074 participants enrolled in this meta-analysis were derived from the HF subgroup of the CABANA study, which contributes a large number of patients with LVEF >50% (12). Fourth, the baseline characteristics of all participants in the enrolled studies were not completely available. Fifth, the enrolled studies had different follow-up periods, while HF hospitalization and all-cause mortality might need longer follow-up periods to show a significant difference between catheter ablation and medical treatment.
This meta-analysis showed improved LVEF, improved 6-min walk distance, less AF recurrence, and lower all-cause mortality in favor of catheter ablation vs. medical treatment in AF patients with HF and LVEF of 36%–50%, and less HF hospitalization was observed both in AF patients with HF and LVEF ≤50%, and LVEF ≤35%. Compared with medical treatment, catheter ablation improved LVEF, improved 6-min walk distance, and had better HF questionnaire score and less HF hospitalization in patients with nonparoxysmal AF and mixed AF; however, AF recurrence and all-cause mortality in favor of catheter ablation were observed only in HF patients with mixed AF.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
W-CL and P-JW reviewed the articles and wrote the manuscript. Y-NF and H-CC prepared figures. M-CC did the final revision. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1165011/full#supplementary-material.
SUPPLEMENTARY FIGURE 1
Flowchart of the study selection strategy and inclusion and exclusion criteria for this meta-analysis. AF, atrial fibrillation; HF, heart failure
SUPPLEMENTARY FIGURE 2
Funnel plot showing non-significant publication bias using Egger's test (t, 0.309; df, 6; p = 0.767).
SUPPLEMENTARY FIGURE 3
Funnel plot showing non-significant publication bias using Egger's test (n t, 0.782; df, 4; p = 0.478).
SUPPLEMENTARY FIGURE 4
Funnel plot showing non-significant publication bias using Egger's test (t, 0.028; df, 4; p = 0.979).
SUPPLEMENTARY FIGURE 5
Funnel plot showing non-significant publication bias using Egger's test (t, 0.392; df, 4; p = 0.715).
SUPPLEMENTARY FIGURE 6
Funnel plot showing non-significant publication bias using Egger's test (t, 0.382; df, 3; p = 0.728).
SUPPLEMENTARY FIGURE 7
Funnel plot showing non-significant publication bias using Egger's test (t, 0.180; df, 3; p = 0.869).
SUPPLEMENTARY FIGURE 8
Funnel plot showing non-significant publication bias using Egger's test (t, 0.215; df, 3; p = 0.844).
1. Anter E, Jessup M, Callans DJ. Atrial fibrillation and heart failure: treatment considerations for a dual epidemic. Circulation. (2009) 119(18):2516–25. doi: 10.1161/CIRCULATIONAHA.108.821306
2. Heck PM, Lee JM, Kistler PM. Atrial fibrillation in heart failure in the older population. Heart Fail Clin. (2013) 9(4):451–9, viii–ix. doi: 10.1016/j.hfc.2013.07.007
3. Batul SA, Gopinathannair R. Atrial fibrillation in heart failure: a therapeutic challenge of our times. Korean Circ J. (2017) 47(5):644–62. doi: 10.4070/kcj.2017.0040
4. Gopinathannair R, Chen LY, Chung MK, Cornwell WK, Furie KL, Lakkireddy DR, et al. Managing atrial fibrillation in patients with heart failure and reduced ejection fraction: a scientific statement from the American heart association. Circ Arrhythm Electrophysiol. (2021) 14(6):HAE0000000000000078. doi: 10.1161/HAE.0000000000000078
5. MacDonald MR, Connelly DT, Hawkins NM, Steedman T, Payne J, Shaw M, et al. Radiofrequency ablation for persistent atrial fibrillation in patients with advanced heart failure and severe left ventricular systolic dysfunction: a randomised controlled trial. Heart. (2011) 97(9):740–7. doi: 10.1136/hrt.2010.207340
6. Jones DG, Haldar SK, Hussain W, Sharma R, Francis DP, Rahman-Haley SL, et al. A randomized trial to assess catheter ablation versus rate control in the management of persistent atrial fibrillation in heart failure. J Am Coll Cardiol. (2013) 61(18):1894–903. doi: 10.1016/j.jacc.2013.01.069
7. Hunter RJ, Berriman TJ, Diab I, Kamdar R, Richmond L, Baker V, et al. A randomized controlled trial of catheter ablation versus medical treatment of atrial fibrillation in heart failure (the CAMTAF trial). Circ Arrhythm Electrophysiol. (2014) 7(1):31–8. doi: 10.1161/CIRCEP.113.000806
8. Di Biase L, Mohanty P, Mohanty S, Santangeli P, Trivedi C, Lakkireddy D, et al. Ablation versus amiodarone for treatment of persistent atrial fibrillation in patients with congestive heart failure and an implanted device: results from the AATAC multicenter randomized trial. Circulation. (2016) 133(17):1637–44. doi: 10.1161/CIRCULATIONAHA.115.019406
9. Marrouche NF, Brachmann J, Andresen D, Siebels J, Boersma L, Jordaens L, et al. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med. (2018) 378(5):417–27. doi: 10.1056/NEJMoa1707855
10. Prabhu S, Costello BT, Taylor AJ, Gutman SJ, Voskoboinik A, McLellan AJA, et al. Regression of diffuse ventricular fibrosis following restoration of sinus rhythm with catheter ablation in patients with atrial fibrillation and systolic dysfunction: a substudy of the CAMERA MRI trial. JACC Clin Electrophysiol. (2018) 4(8):999–1007. doi: 10.1016/j.jacep.2018.04.013
11. Kuck KH, Merkely B, Zahn R, Arentz T, Seidl K, Schlüter M, et al. Catheter ablation versus best medical therapy in patients with persistent atrial fibrillation and congestive heart failure: the randomized AMICA trial. Circ Arrhythm Electrophysiol. (2019) 12(12):e007731. doi: 10.1161/CIRCEP.119.007731
12. Packer DL, Piccini JP, Monahan KH, Al-Khalidi HR, Silverstein AP, Noseworthy PA, et al. Ablation versus drug therapy for atrial fibrillation in heart failure: results from the CABANA trial. Circulation. (2021) 143(14):1377–90. doi: 10.1161/CIRCULATIONAHA.120.050991
13. Parkash R, Wells GA, Rouleau J, Talajic M, Essebag V, Skanes A, et al. Randomized ablation-based rhythm-control versus rate-control trial in patients with heart failure and atrial fibrillation: results from the RAFT-AF trial. Circulation. (2022) 145(23):1693–1704. doi: 10.1161/CIRCULATIONAHA.121.057095
14. Weinmann K, Aktolga D, Pott A, Bothner C, Rattka M, Stephan T, et al. Impact of re-definition of paroxysmal and persistent atrial fibrillation in the 2012 and 2016 European society of cardiology atrial fibrillation guidelines on outcomes after pulmonary vein isolation. J Interv Card Electrophysiol. (2021) 60(1):115–23. doi: 10.1007/s10840-020-00710-4
15. Schönbauer R, Duca F, Kammerlander AA, Aschauer S, Binder C, Zotter-Tufaro C, et al. Persistent atrial fibrillation in heart failure with preserved ejection fraction: prognostic relevance and association with clinical, imaging and invasive haemodynamic parameters. Eur J Clin Invest. (2020) 50(2):e13184. doi: 10.1111/eci.13184
16. Chen S, Pürerfellner H, Meyer C, Acou WJ, Schratter A, Ling Z, et al. Rhythm control for patients with atrial fibrillation complicated with heart failure in the contemporary era of catheter ablation: a stratified pooled analysis of randomized data. Eur Heart J. (2020) 41(30):2863–73. doi: 10.1093/eurheartj/ehz443
17. Pan KL, Wu YL, Lee M, Ovbiagele B. Catheter ablation compared with medical therapy for atrial fibrillation with heart failure: a systematic review and meta-analysis of randomized controlled trials. Int J Med Sci. (2021) 18(6):1325–31. doi: 10.7150/ijms.52257
Keywords: atrial fibrillation, heart failure, left ventricular ejection fraction, medical treatment, catheter ablation
Citation: Lee W-C, Fang H-Y, Wu P-J, Chen H-C, Fang Y-N and Chen M-C (2023) Outcomes of catheter ablation vs. medical treatment for atrial fibrillation and heart failure: a meta-analysis. Front. Cardiovasc. Med. 10:1165011. doi: 10.3389/fcvm.2023.1165011
Received: 13 February 2023; Accepted: 18 April 2023;
Published: 10 May 2023.
Edited by:
Faisal Syed, University of North Carolina at Chapel Hill, United StatesReviewed by:
David Zweiker, Klinik Ottakring, Austria© 2023 Lee, Fang, Wu, Chen, Fang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mien-Cheng Chen Y2hlbm1pZW5AbXM3Ni5oaW5ldC5uZXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.