- 1Department of Cardiac Surgery, Lanzhou University Second Hospital, Lanzhou University, Lanzhou, China
- 2Health Science Center of Lanzhou University, Lanzhou University, Lanzhou, China
- 3Dongguan Tungwah Hospital, Dongguan, China
Objectives: Ruptured sinus of Valsalva aneurysm (RSVA) often has an abrupt onset, and can chest pain, acute heart failure, and even sudden death. The effectiveness of different treatment modalities remains controversial. Thus, we completed a meta-analysis to evaluate the efficiency and safety of traditional surgery vs. percutaneous closure (PC) for RSVA.
Methods: We carried out a meta-analysis using PubMed, Embase, Web of Science, Cochrane Library, China National Knowledge Infrastructure (CNKI), WanFang Data, and the China Science and Technology Journal Database. The primary outcome was comparing in-hospital mortality between the two procedures, and the secondary outcome was documenting postoperative residual shunts, postoperative aortic regurgitation, and length of hospital stay in the two groups. Differences were expressed as odds ratios (ORs) with 95% confidence intervals (CIs) to assess the relationships between predefined surgical variables and clinical outcomes. This meta-analysis was conducted using Review Manager software (version 5.3).
Results: The final qualifying studies included 330 patients from 10 trials (123 in the percutaneous closure group, and 207 in the surgical repair group). When PC was compared to surgical repair, there were no statistically significant differences in in-hospital mortality (overall OR: 0.47, 95%CI 0.05–4.31, P = 0.50). However, percutaneous closure did significantly decrease the average length of hospital stay (OR: −2.13, 95% CI −3.05 to −1.20, P < 0.00001) when compared to surgical repair, but there were no significant between-group differences in the rates of postoperative residual shunts (overall OR: 1.54, 95%CI 0.55–4.34, P = 0.41) or postoperative aortic regurgitation (overall OR: 1.54, 95%CI 0.51–4.68, P = 0.45).
Conclusion: PC may become a valuable alternative to surgical repair for RSVA.
Introduction
Sinus of Valsalva aneurysm is an uncommon aberration that is typically brought on by a congenital lack of elastic and muscular tissue in the aorta wall or acquired as a result of periaortic inflammation, atherosclerosis, trauma, and/or aortic dissection. Patients who have undergone corrective surgery for congenital heart conditions may also experience it (1). In Eastern populations, rupture incidence is higher in patients who are adolescents or older (2). Ruptured sinus of Valsalva aneurysm (RSVA) necessitate immediate medical attention and can cause rapid heart failure, cardiac tamponade, hemodynamic compromise, and possibly sudden cardiac death (3).
Surgical correction is widely used to treat RSVA, and has low death rates. Unfortunately, it may also increase the risks of incisional infections, post-pericardiotomy syndrome, and scar tissue formation (4). Several different devices have been used to treat RSVA, but occluders have received the most attention and have demonstrated positive outcomes in single-case reports and short-case series (5). However, relatively few studies have compared clinical outcomes between surgical and percutaneous closure (PC) for RSVA. Thus, we conducted a meta-analysis to compare clinical results of PC and surgical repair amongst RSVA patients.
Material and methods
The components of this meta-analysis were reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (6). The research protocol has also been submitted to the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY2022110131).
Search strategy
The following seven electronic databases were comprehensively searched: WanFang Data, China Science and Technology Journal Database, China national knowledge infrastructure (CKNI), Web of Science, Cochrane Library, PubMed, and Embase. There were no restrictions set on the language or date of the literature search. The searches began on November 30, 2022. Studies detailed the results of patients over the age of 18 who underwent PC surgery or surgical repair for RSVA. The search was developed based on the PICOS method, and the search terms were (“Ruptured sinus of valsalva aneurysm” OR “Sinus of Valsalva aneurysm”) AND (“surgery” OR“percutaneous closure surgery” OR “treatment”). We also manually searched reference lists of retrieved publications (including reviews) to find studies that might be eligible.
Study selection and inclusion criteria
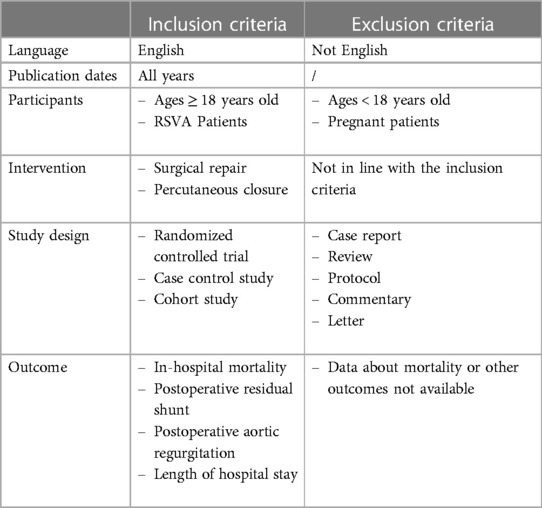
After deleting duplicates and importing all citations into EndNote, two reviewers (YM and XYW) evaluated the titles and abstracts with consideration of the qualifying standards (shown in Table 1). We only included studies written in English. Full papers that were evaluated and determined to be “included” or “uncertain” were then evaluated once again with consideration of the inclusion criteria. Only studies with the most comprehensive data and that had consistently been published were chosen. The papers were selected through discussion, and the disagreements were finally resolved by a third-party reviewer (CTW).
Data extraction
A specialized extraction form was used to gather information about each study's author(s), publication year, methodological design, control and treatment interventions, sample size, and findings. If more information was needed, the authors were contacted.
Quality assessment
The caliber of all included studies was independently assessed by two reviewers (YM and XYW). Nonrandomized control trials were assessed using the Newcastle-Ottawa Scale(NOS) (7). The “star system” was used to grade each included study. A total score of 5 or less was considered low, 6 or 7 was considered moderate, and 8 or 9 was considered high. Disputes were settled by discussion and consensus between the other two reviewers (YNL and CTW). A comparison of in-hospital mortality for the two treatments served as the primary outcome. The secondary outcome was documenting postoperative residual shunts, postoperative aortic regurgitations, and length of hospital stays.
Statistical analysis
Review Manager 5.3 was used for the meta-analysis and Egger's regression test. For dichotomous variables, the Mantel-Haenszel (MH) model was used to obtain Odds Ratio (OR) and 95% CI. Heterogeneity between studies was assessed by I2 statistics. I2 Values of 25, 50, and 75% were reported as low, moderate, and high degrees of heterogeneity, respectively. A subgroup analysis in the meta-analysis (focused on different study designs such as randomized controlled trials, prospective cohort studies, and retrospective studies) was conducted to lessen the heterogeneity. A P < 0.05 was considered to be statistically significant. Egger's regression model was used to detect publication bias when the number of studies analyzed was enough.
Results
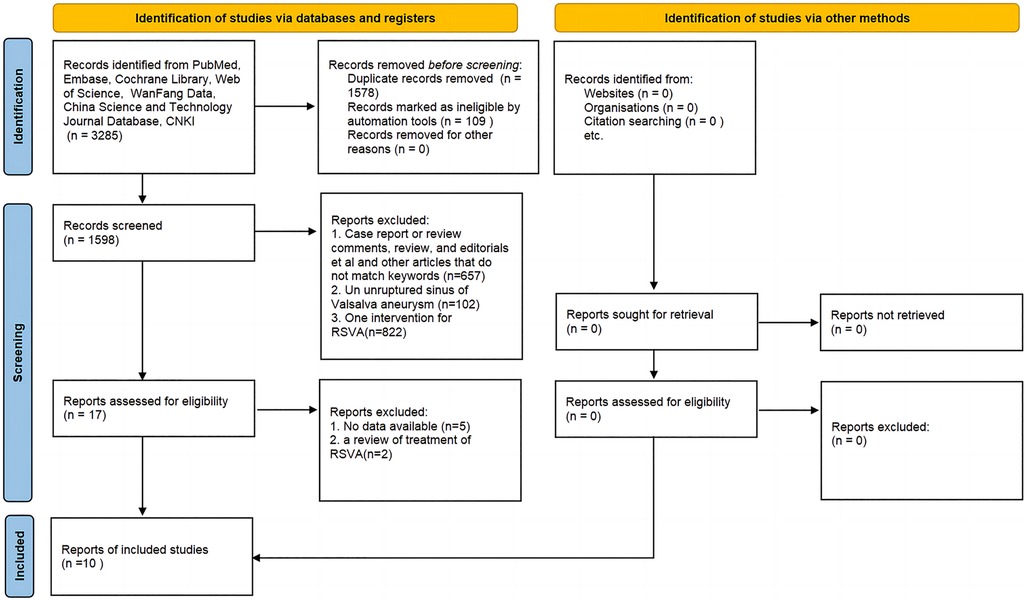
A summary of the study selection process is presented in Figure 1. A total of 3,285 citations were found through our literature search. Of these, 1,687 articles were eliminated for various reasons, including duplication. After reviewing the paper titles and abstracts, 1,581 articles were eliminated for PI-VSR or other reasons, depending on the type of article. Six papers were found to be invalid after the full-text versions of 17 publications were reviewed. A total of 10 papers (8–17) were deemed suitable for final analysis.
General characteristics of the included studies
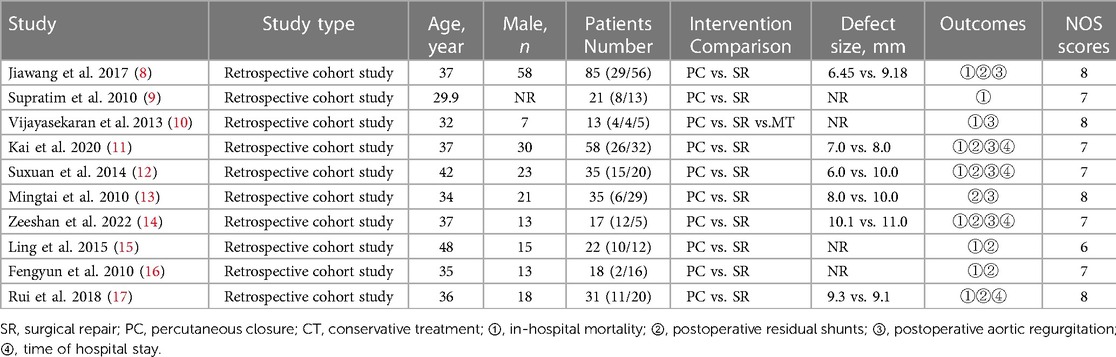
The key characteristics of the studies that fit the inclusion criteria are presented in Table 2. A total of 330 patients were included across these 10 papers. 123 of them were in the PC group, and 207 were in the surgical repair group. Nine studies compared surgical treatment and PC for RSVA. The other study compared surgical treatment, PC, and medical treatment for RSVA. Nine of the studies evaluated in-hospital mortality, and eight evaluated the rates of residual shunts following surgery, five evaluated rates of postoperative aortic regurgitation, and four evaluated the length of hospital stay.
Primary outcome
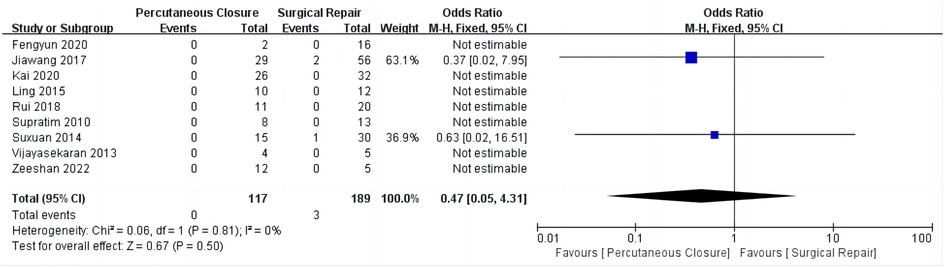
In-hospital mortality
There were no significant differences observed in in-hospital mortality rates between the two treatment groups (overall OR: 0.47, 95%CI 0.05–4.31, P = 0.50) (Figure 2). Additionally, no heterogeneity was observed (I2 = 0%).
Secondary outcomes
Rates of postoperative residual shunt
There were no significant differences in incidence rates of postoperative residual shunt between the two treatment groups (overall OR: 1.54, 95%CI 0.55–4.34, P = 0.41) (Figure 3), and no heterogeneity was observed (I2 = 0%).
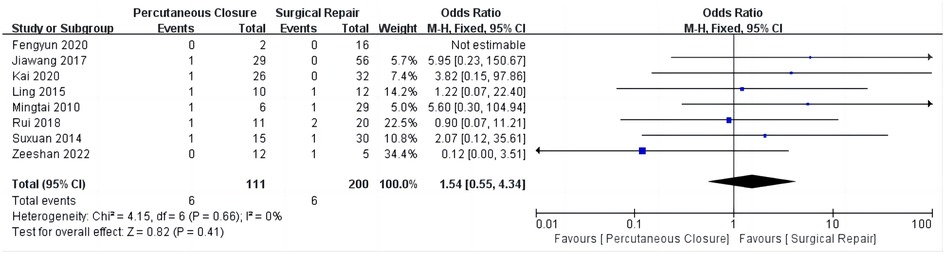
Figure 3. Comparison of postoperative residual shunt rates between percutaneous closure and surgical repair.
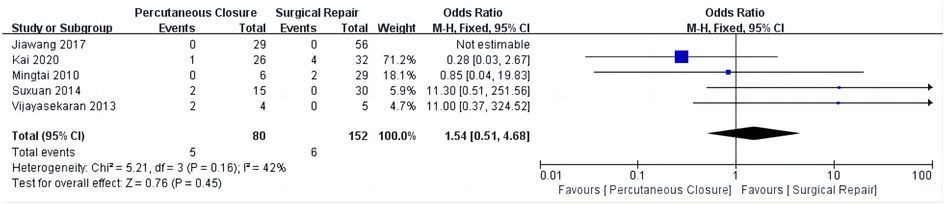
Rates of postoperative aortic regurgitation
There were no significant differences in the incidence rates of postoperative aortic regurgitation between the treatment groups (overall OR: 1.54, 95%CI 0.51–4.68, P = 0.45) (Figure 4), and no heterogeneity was observed (I2 = 0%).
Length of hospital stay
The PC group had significantly shorter lengths of hospital stay when compared to the surgical treatment group (overall OR: −2.13, 95%CI −3.05–1.20, P < 0.00001) (Figure 5). However, high heterogeneity was observed in this category (I2 = 85%).
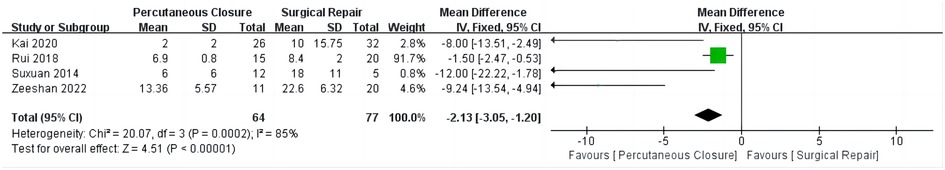
Figure 5. Comparing length of postoperative hospital stay between percutaneous closure and surgical repair.
Discussion
Although the actual prevalence of SOVAs is unknown, it is estimated that 0.09 percent of the population is affected. Between 0.1% to 3.5% of all congenital heart abnormalities are SOVA (3). Hemodynamic disturbances and/or sudden cardiac death are frequently present in SOVA patients. There have also been reports of rupture into the interventricular septum, leading to occlusion of the left ventricular outflow system (18). This investigation demonstrated that PC treatment for RSVA was associated with a shorter length of hospital stay compared to surgical treatment. However, there were no statistically significant differences in in-hospital mortality rates, incidence rates of postoperative residual shunts, or incidence rates of postoperative aortic regurgitation between the two strategies.
Surgical treatment is widely used to treat RSVA, especially in patients with combined intracardiac malformations. The literature reports a long history of surgical treatment for RSVA, with the first surgical treatment performed by Lillehei in 1957 (19). Surgical treatment has several advantages, including complete correction of the deformity and maturity of practice. However, surgical treatment can increase other risks and even cause death. Additionally, patients will often opt for an interventional approach if it can achieve the same results as surgery. Cullen et al. described the first instance of PC in 1994, and this less invasive approach has been increasingly used (20). Liu reported on 25 patients from a single center and found that trivial residual shunts developed in three patients, and mild occluder-related AR occurred in five patients. During a median follow-up time period of 19 months (6–96 months), however, all of the trivial residual shunts vanished, and mild occluder-related AR disappeared in four out of the five patients (21). In addition, studies from several centers have shown that interventions can be used to treat PDA, ASD, and VSD in combination with RSVA (12, 22). However, there are still no universal guidelines for RSVA treatment, so we completed a meta-analysis and systematic review of this disease.
The effectiveness of percutaneous intervention and surgical repair have not been previously compared in a meta-analysis. Kuriakose compared 34 studies detailing PC treatments with 16 studies on surgical closure, including 877 patients treated for aortic sinus aneurysm ruptures between 1,956 and 2014. He concluded that PC might be safe, effective, and practical in patients who are too ill for bypass surgery and who have mild or no aortic regurgitation and simple associated defects (e.g.,myxomatous ventricular septal defects, secondary foramen ovale septal defects, and small patent ductus arteriosus) (23). His conclusions are generally consistent with ours. The prolonged length of hospital stay amongst patients in the surgical group in our study may be related to factors such as extracorporeal circulation and the more invasive nature of the procedure.
This meta-analysis had several limitations. First, the included studies were all retrospective, and it was not possible to control for potential confounding factors. In addition, The location of Additionally, the precise location of the ruptures may have differed (see Table 3).
Conclusions
RSVA is a rare cardiac malformation that can result in large left-to-right shunts and severe congestive heart failure. We conducted a meta-analysis and concluded that, for RSVA, PC might become a valuable alternative to surgical repair. However, large-scale randomized controlled trials are required to confirm the effects of PC and surgical repair for treating RSVA.
Author contributions
All of the authors have made important contributions to the manuscript. Study conception and design: XYW and YM; Analysis and interpretation: XYW, YM, CTW, and YNL; Manuscript preparation: XYW and YM; Data collection and statistical expertise: YM, CTW, YNL, XQG, YPZ; Attainment of funding: XYW. All authors contributed to the article and approved the submitted version.
Funding
The study was funded by the Cuiying Graduate Supervisor Applicant Training Program of Lanzhou University Second Hospital (201709).
Acknowledgments
We thank MedEditing LCC. for the scientific editing of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ishizaka N, Sohmiya K, Miyamura M, Umeda T, Tsuji M, Katsumata T, et al. Infected aortic aneurysm and inflammatory aortic aneurysm—in search of an optimal differential diagnosis. J Cardiol. (2012) 59:123–31. doi: 10.1016/j.jjcc.2011.10.006
2. Chu SH, Hung CR, How SS, Chang H, Wang SS, Tsai CH, et al. Ruptured aneurysms of the sinus of valsalva in oriental patients. J Thorac Cardiovasc Surg. (1990) 99:288–98. doi: 10.1016/S0022-5223(19)37013-8
3. Feldman DN, Roman MJ. Aneurysms of the sinuses of valsalva. Cardiology. (2006) 106:73–81. doi: 10.1159/000092635
4. Jaswal V, Kumar V, Thingnam SKS, Puri GD. Surgical repair of ruptured sinus of valsalva aneurysm: 13-year single center experience. J Card Surg. (2021) 36(4):1264–9. doi: 10.1111/jocs.15358
5. Kumar P, Banerji A. Transcatheter closure of ruptured sinus of valsalva aneurysm. Catheter Cardiovasc Interv. (2010) 76:774–6. doi: 10.1002/ccd.22353
6. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
7. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25(9):603–5. doi: 10.1007/s10654-010-9491-z
8. Xiao JW, Wang QG, Zhang DZ, Cui CS, Han X, Zhang P, et al. Clinical outcomes of percutaneous or surgical closure of ruptured sinus of valsalva aneurysm. Congenit Heart Dis. (2018) 13(2):305–10. doi: 10.1111/chd.12572
9. Supratin S, Biswajit B, Amitabha C, Mily R. Clinical profile and management options of ruptured sinus of valsalva. Cardiol Young. (2010) 20(suppl. 1):292.
10. Vijayasekaran B, Majella CM, Venkatesan S, Ramesh R, Dhandapani VE. Clinical profile of 13 cases of rupture sinus of valsalva aneurysm. Indian Heart J. (2013) 65:S77.
11. Yang K, Luo X, Tang Y, Hu H, Sun H. Comparison of clinical results between percutaneous closure and surgical repair of ruptured sinus of valsalva aneurysm. Catheter Cardiovasc Interv. (2021) 97(3):E354–61. doi: 10.1002/ccd.29216
12. Liu S, Xu X, Ding X, Liu G, Zhao Z, Zhao X, et al. Comparison of immediate results and mid-term follow-up of surgical and percutaneous closure of ruptured sinus of valsalva aneurysm. J Cardiol. (2014) 63(3):239–43. doi: 10.1016/j.jjcc.2013.08.011
13. Lin M, Chiu S, Chen C, Wu E, Wang J, Wu M, et al. Repair of ruptured sinus of valsalva aneurysm without VSD: comparisons between transcatheter closure and surgery. Cardiol Young. (2010) 20:385.
14. Mumtaz ZA, Sagar P, Rajendran M, Sivakumar K. Transcatheter versus surgical closure of acute ruptured sinus of valsalva aneurysms with associated ventricular septal defects. Pediatr Cardiol. (2022) 43(7):1494–501. doi: 10.1007/s00246-022-02873-5
15. Cui L, Na J, Qin Y. Efficacy and safety of interventional closure and surgical of ruptured sinus of valsalva aneurysm. Chin J Interv Imaging Ther. (2015) 12(4):223–5.
16. Zhang F, Yang R, Shang P. Analysis of 18 cases of ruptured aortic sinus aneurysm. Chin J Misdiagn. (2010) 13(10):3332–3.
17. Niu R, Wang C, Xia Y, Liu J, Cheng S, Wang G, et al. Transcatheter closure versus surgical closure for ruptured aortic sinus aneurysm; a comparative study. J Intervent Radiol. (2018) 27(1):9–12.
18. Lee DH, Kang EJ, Park TH, Woo JS, Hong SH, Kim YD. A case of right sinus of valsalva rupture with dissection into interventricular septum causing left ventricular outflow tract obstruction. Korean Circ J. (2013) 43(11):770–3. doi: 10.4070/kcj.2013.43.11.770
19. Weinreich M, Yu PJ, Trost B. Sinus of valsalva aneurysms: review of the literature and an update on management. Clin Cardiol. (2015) 38(3):185–9. doi: 10.1002/clc.22359
20. Cullen S, Somerville J, Redington A. Transcatheter closure of a ruptured aneurysm of the sinus of valsalva. Br Heart J. (1994) 71:479–80. doi: 10.1136/hrt.71.5.479
21. Liu S, Xu X, Zhao X, Chen F, Bai Y, Li W, et al. Percutaneous closure of ruptured sinus of valsalva aneurysm: results from a multicentre experience. EuroIntervention. (2014) 10(4):505–12. doi: 10.4244/EIJV10I4A87
22. Kerkar PG, Lanjewar CP, Mishra N, Nyayadhish P, Mammen I. Transcatheter closure of ruptured sinus of valsalva aneurysm using the amplatzer duct occluder: immediate results and mid-term follow-up. Eur Heart J. (2010) 31:2881–7. doi: 10.1093/eurheartj/ehq323
Keywords: percutaneous closure, surgical repair, ruptured sinus of valsalva aneurysm, meta-analysis, effects of treatment
Citation: Mao Y, Wang C, Li Y, Guan X, Zhang X and Wu X (2023) Percutaneous closure versus surgical repair for ruptured sinus of valsalva aneurysm: A systematic review and meta-analysis. Front. Cardiovasc. Med. 10:1158906. doi: 10.3389/fcvm.2023.1158906
Received: 4 February 2023; Accepted: 13 March 2023;
Published: 17 April 2023.
Edited by:
Eustaquio Maria Onorato, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), ItalyReviewed by:
Serban Mihai Balanescu, Carol Davila University of Medicine and Pharmacy, RomaniaOsman Baspinar, University of Gaziantep, Türkiye
Aleksejus Zorinas, Vilnius University, Lithuania
© 2023 Mao, Wang, Li, Guan, Zhang and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiangyang Wu d3V4eW9rQDE2My5jb20=
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Structural Interventional Cardiology, a section of the journal Frontiers in Cardiovascular Medicine
 Yong Mao1,†
Yong Mao1,† Xiangyang Wu
Xiangyang Wu