
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Cardiovasc. Med. , 24 May 2023
Sec. Cardiac Rhythmology
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1156658
This article is part of the Research Topic Sudden Cardiac Death From Channelopathies and Cardiomyopathies View all 6 articles
Introduction: While pacing has been used for long QT syndrome (LQTs), the optimal pacing modality is controversial.
Case: We report a woman with bradycardia and a recently implanted single-chamber pacemaker experienced multiple syncope. No device dysfunction was found. Multiple Torsade de Pointes (TdP) induced by the bigeminy result from retrograde ventriculoatrial (VA) activation in VVI pacing were demonstrated in the scenario of previously unidentified LQTs. Replacement for a dual-chamber ICD and intentional atrial pacing eliminated the VA conduction and symptoms.
Conclusion: Pacing without atrioventricular sequence might be catastrophic in LQTs. Atrial pacing and atrioventricular synchrony should be highlighted.
Pacemakers have been routinely used for treating bradycardia. For patients with long QT syndrome (LQTs), the pacing is also helpful for those who remain symptomatic despite being on beta-blockers, especially when bradycardia facilitates TdP (1, 2). While guidelines have established recommendations for permanent pacing in patients with LQTS and suggest ICD therapy for patients with risk factors for sudden cardiac death, formal recommendations for optimal device choice and programming for LQTS are not available.
We reported a case of a 62-year-old woman who was admitted for intermittent dizziness and syncope. One month earlier, the patient received single-chamber pacemaker implantation for significant fatigue due to sinus bradycardia and asystole at a local hospital. No improvement in her symptoms was noted, and multiple syncope attacks prompted her visit. No dysfunction of the device was found during interrogation. However, telemetric ECG monitoring and EGM demonstrated Torsade de Pointes induced by the bigeminy result from repetitive retrograde ventriculoatrial (VA) activation in VVI pacing and sequential atrial impulses conducted to the ventricles through intact conduction systems (Figure 1).
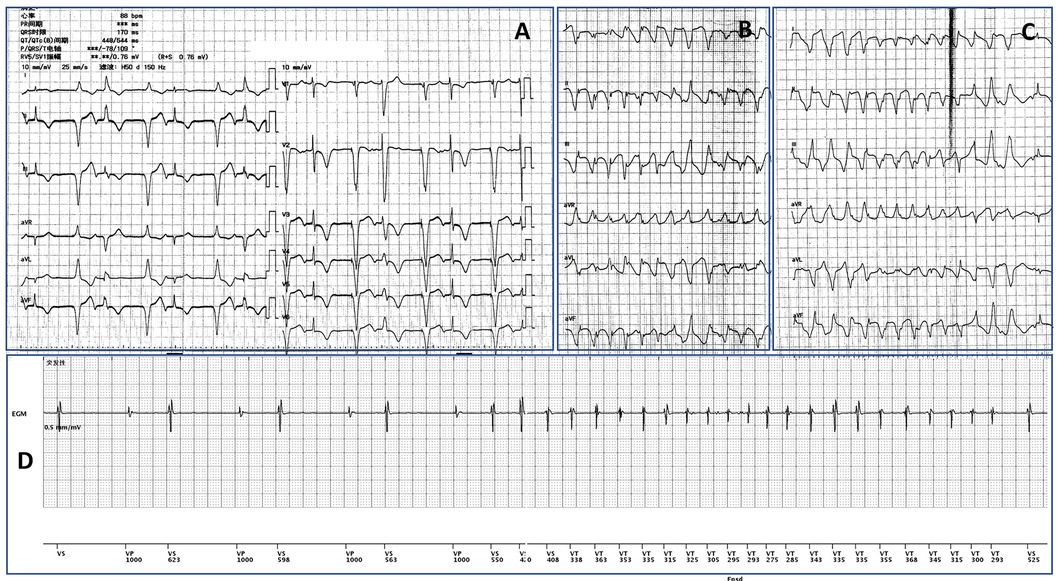
Figure 1. (A) VVI pacing led to repetitive VA retrograde conduction and the subsequent atrial activation conducted to capture the ventricle. The bigeminy led to short-long cycles and resulted in multiple Torsade de Pointes (TdP) shown in (B and C). (D) The EGM recorded the onset of one episode of the TdP, indicating the sequential relationship between the bigeminy and the malignant arrhythmia.
In the scenario of previously unidentified LQTs (Figure 2A), the bigeminy pattern created short-long cycles which contributed to the malignant arrhythmia attacks. Electrolyte disturbances and coronary artery disease as the reversible cause of the LQTs were ruled out, and a beta-blocker was initiated. Replacement of the device for a dual-chamber implantable cardiac defibrillator (ICD) and intentional atrial pacing eliminated the VA retrograde activation. Also, the higher base rate of 70 bpm helps to shorten the QTc (Figure 2B). In the follow-up, the patient reported significant improvement in her life quality with no syncope recurrence. No malignant arrhythmia was recorded by the ICD either. One missense variant in α-1,2-glucosyltransferase (ALG10c.1247G > A; p.Arg416His) of the patient was identified by whole-exome sequencing, which was furtherly verified by Sanger sequencing.
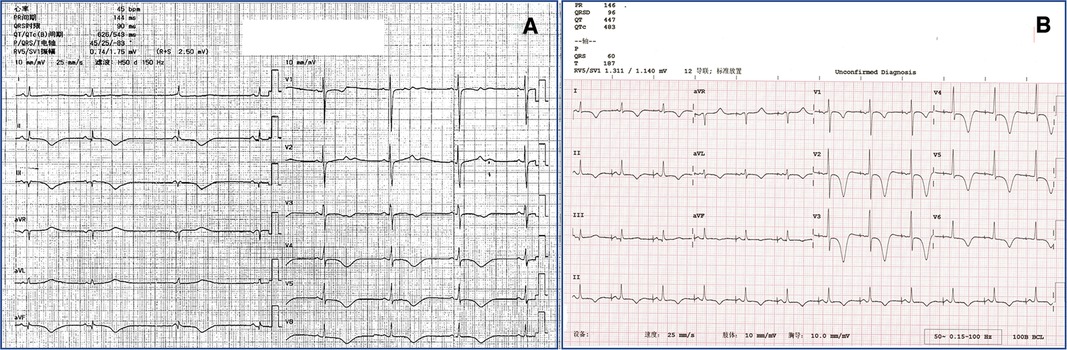
Figure 2. (A) Baseline 12-lead ECG of the patient before the single-chamber pacemaker implantation showed significant sinus bradycardia, junctional escape rhythm, and long QTc of 543 ms. (B) Replacement for a dual-chamber implantable cardiac defibrillator and intentionally higher atrial base rate of 70 bpm resulted in eliminating VA retrograde conduction and shortened QTc of 483 ms.
Our case suggests the pivotal clinical significance of understanding the whole picture of an arrhythmia syndrome in decision-making. Although pacing is suggested as one of the treatment measures for LQTs, inappropriate device and setting might lead to unwanted outcomes.
The patient's story began with the implantation of a single-chamber pacemaker for sinus bradycardia. In patients with sinus node dysfunction (SND), however, studies have found that dual-chamber AV sequential pacing was superior to single-chamber ventricular-based pacing in reducing the risk of atrial fibrillation, stroke, and pacemaker syndrome (3, 4). Potential exceptions are those with advanced age and/or frail patients with infrequent pauses who have limited functional capacity and/or a short life expectancy (2). The patient did not fall into the exceptional category, and a single-chamber device might not be appropriate.
Notably, pacemaker syndrome has been reported to occur in ∼25% of patients with SND in VVI pacing (5, 6) and is associated with a reduced quality of life (6, 7). The patient had shown the predisposing characteristic for pacemaker syndrome with spontaneous VA retrograde conduction (8). It is natural to speculate that pacemaker syndrome was the culprit of the exacerbation of the symptoms. The base rate of the pacemaker was once set to 45 bpm at the local hospital to decrease the retrograde conduction. With no clinical improvement, insufficient correction of the bradycardia was suspected instead, and the base rate was changed to 70 bpm. The alteration could not alleviate the symptoms either. In fact, a higher programmed base rate was associated with the development of pacemaker syndrome, and a higher percentage of paced beats was an independent predictor (6).
When we continued to focus on the pre-assumption of pacemaker syndrome, findings in EGM and concurrent symptoms and telemetry suggested Tdp as the cause of the patient's loss of consciousness. With no prior cardiac arrest attack or associated family history, the prolonged QTc in the 12-lead ECG was attributed to the significant bradycardia and neglected. The bigeminy resulting from repetitive retrograde VA activation in VVI pacing created the short-long cycles contributing to the increased repolarization dispersion and enhanced early after-depolarizations. Both mechanisms are key to arrhythmia initiation in LQTs. Furthermore, the missense mutant of ALG10 identified in this case exhibits sequence homology with KCR1, therefore, might modulate IKr sensitivity (9). The multi-hit model (10), with the mutation serving as a genetic predisposition and bigeminy as the trigger, might result in the occurrence of Tdp.
ICD combined pacing is considered reasonable in patients with LQTS (7, 8) while no specific recommendations for the pacing modalities and programming were suggested in the guidelines. Meanwhile, pacing at an increased rate has been proposed as an essential treatment in LQTS because the modality shortens QT interval and the window of vulnerability for reinduction of Tdp (2). In our case, though, rapid ventricular pacing did not help if it did not accelerate the syncope attacks. It is not only because this pacing mode can cause heterogeneous ventricular depolarization that can be proarrhythmic (7), but also because the increased bigeminies and short-long couplings could further strengthen the vicious cycle.
The problem seemingly comes down to eliminating the retrograde VA activation as an initiation factor for both potential pacemaker syndrome and Tdp. Slow pathway ablation was an apparent approach. However, the AV desynchrony would not be solved as the sinus arrest and irregularity persists when only ventricular sensing and pacing exist. Also, ablation at the AV junction would have limited influence on the ventricular repolarization process, which defines the QT interval. On the other hand, increased-rate atrial pacing has been reported to shorten the QTc and reduce the risk of recurrent arrhythmia breakthroughs (7, 11, 12). Traditional right ventricular pacing, as shown in our case, should be minimized. The novel conduction system pacing (CSP) would be a promising modality for physiological ventricular activation in patients who need ventricular pacing (13, 14), although the sole adoption of CSP would not solve VA retrograde conduction. For our patient with sinus node dysfunction instead of atrioventricular block (AVB), dual-chamber ICD with minimized ventricular pacing algorism by using defibrillation RV lead implanted on the septum would be an optimal choice. Indeed, the intentional atrial pacing at 70 pm served as overdrive and effectively prevented the AV desynchrony. QTc was also significantly shortened.
Loss of atrioventricular sequence in LQTs might be catastrophic. Atrial pacing and atrioventricular synchrony should be highlighted as pacing strategies for LQTs.
As in our case, patients with channelopathies often act as candidates for cardiac implantable electronic devices. ICD has often been recommended for the prevention of sudden cardiac death in this population (15, 16). Consensus on the need for pacing and/or the optimal device selection, though, has not been obtained in most current guidelines. For instance, high-risk AVB has been reported in Brugada syndrome, especially in patients with baseline long PR interval (16). Considering this, a transvenous ICD with pacing capabilities should be considered instead of a simplified subcutaneous ICD. Future studies will be necessary to provide more evidence and recommendation on the tailored devices selection strategy.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Ethics Committee on Clinical Investigation of Peking University First Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
S-YC, Q-HS, LW, and JZ formed the conception and drafted the manuscript. Q-PS, LQ analyzed and interpreted the data. All authors contributed to the article and approved the submitted version.
National Key Research and Development Project: Screening, Prevention, and Health Economic Evaluation for High-Risk Population of Cardio and Cerebrovascular Disease (2017YFC1307700) and the Youth Clinical Research Project of Peking University First Hospital (No. 2017CR20).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Viskin S. Cardiac pacing in the long QT syndrome: review of available data and practical recommendations. J Cardiovasc Electrophysiol. (2000) 11(5):593–600. doi: 10.1111/j.1540-8167.2000.tb00015.x
2. Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IM, et al. 2021 ESC guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. (2021) 42(35):3427–520. doi: 10.1093/eurheartj/ehab364
3. Connolly SJ, Kerr CR, Gent M, Roberts RS, Yusuf S, Gillis AM, et al. Effects of physiologic pacing versus ventricular pacing on the risk of stroke and death due to cardiovascular causes. Canadian trial of physiologic pacing investigators. N Engl J Med. (2000) 342(19):1385–91. doi: 10.1056/NEJM200005113421902
4. Healey JS, Toff WD, Lamas GA, Andersen HR, Thorpe KE, Ellenbogen KA, et al. Cardiovascular outcomes with atrial-based pacing compared with ventricular pacing: meta-analysis of randomized trials, using individual patient data. Circulation. (2006) 114(1):11–7. doi: 10.1161/CIRCULATIONAHA.105.610303
5. Lamas GA, Lee KL, Sweeney MO, Silverman R, Leon A, Yee R, et al. Ventricular pacing or dual-chamber pacing for sinus-node dysfunction. N Engl J Med. (2002) 346(24):1854–62. doi: 10.1056/NEJMoa013040
6. Link MS, Hellkamp AS, Estes NA 3rd, Orav EJ, Ellenbogen KA, Ibrahim B, et al., High incidence of pacemaker syndrome in patients with sinus node dysfunction treated with ventricular-based pacing in the mode selection trial (MOST). J Am Coll Cardiol. (2004) 43(11):2066–71. doi: 10.1016/j.jacc.2003.10.072
7. Rhodes T, Weiss R. Device therapy in the setting of long QT syndrome. Card Electrophysiol Clin. (2015) 7(3):479–86. doi: 10.1016/j.ccep.2015.05.018
8. Wilkoff BL, Fauchier L, Stiles MK, Morillo CA, Al-Khatib SM, Almendral J, et al. 2015 HRS/EHRA/APHRS/SOLAECE expert consensus statement on optimal implantable cardioverter-defibrillator programming and testing. Heart Rhythm. (2016) 13(2):e50–86. doi: 10.1016/j.hrthm.2015.11.018
9. Nakajima T, Hayashi K, Viswanathan PC, Kim MY, Anghelescu M, Barksdale KA, et al. HERG Is protected from pharmacological block by alpha-1,2-glucosyltransferase function. J Biol Chem. (2007) 282(8):5506–13. doi: 10.1074/jbc.M605976200
10. El-Sherif N, Turitto G, Boutjdir M. Acquired long QT syndrome and electrophysiology of torsade de pointes. Arrhythm Electrophysiol Rev. (2019) 8(2):122–30. doi: 10.15420/aer.2019.8.3
11. Fruh A, Siem G, Holmstrom H, Dohlen G, Haugaa KH. The Jervell and Lange-Nielsen syndrome, atrial pacing combined with ss-blocker therapy, a favorable approach in young high-risk patients with long QT syndrome? Heart Rhythm. (2016) 13(11):2186–92. doi: 10.1016/j.hrthm.2016.07.020
12. Kowlgi GN, Giudicessi JR, Barake W, Bos JM, Ackerman MJ. Efficacy of intentional permanent atrial pacing in the long-term management of congenital long QT syndrome. J Cardiovasc Electrophysiol. (2021) 32(3):782–9. doi: 10.1111/jce.14920
13. Senes J, Mascia G, Bottoni N, Oddone D, Donateo P, Grimaldi T, et al. Is his-optimized superior to conventional cardiac resynchronization therapy in improving heart failure? Results from a propensity-matched study. Pacing Clin Electrophysiol. (2021) 44(9):1532–9. doi: 10.1111/pace.14336
14. Katta MR, Abouzid MRA, Hameed M, Kaur J, Balasubramanian S. Approach to left bundle branch pacing. Cardiol Rev. (2023). Online ahead of print. doi: 10.1097/CRD.0000000000000545
15. Mascia G, Bona RD, Ameri P, Canepa M, Porto I, Parati G, et al. Brugada syndrome and syncope: a practical approach for diagnosis and treatment. Europace. (2021) 23(7):996–1002. doi: 10.1093/europace/euaa370
Keywords: long QT syndrome (LQTS), torsade de pointes (TdP), pacemaker, implantable cardioversion defibrillator, atrioventricular sequential pacing
Citation: Chu S-Y, Sheng Q-H, Shi Q-P, Qiu L, Wu L and Zhou J (2023) Case report: Torsade de pointes induced by the bigeminy result from retrograde ventriculoatrial activation in VVI pacing and resolved by intentional atrial pacing. Front. Cardiovasc. Med. 10:1156658. doi: 10.3389/fcvm.2023.1156658
Received: 1 February 2023; Accepted: 4 May 2023;
Published: 24 May 2023.
Edited by:
Ehud Chorin, Tel Aviv Sourasky Medical Center, IsraelReviewed by:
Giuseppe Mascia, University of Genoa, Italy© 2023 Chu, Sheng, Shi, Qiu, Wu and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Zhou ZHJ6aG91amluZzEyM0AxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.