- 1University Medical Center Mainz, Department of Cardiology, Mainz, Germany and German Center for Cardiac and Vascular Research (DZHK), Standort Rhein-Main, Germany
- 2Department of Cardiovascular Medicine, Assiut University Heart Hospital, Assiut, Egypt
Background: There is a debate regarding the best stent strategy for unprotected distal left main (LM) bifurcation disease. Among two-stent techniques, double-kissing and crush (DKC) is favored in current guidelines but is complex and requires expertise. Reverse T and Protrusion (rTAP) was shown to be a comparable strategy regarding short-term efficacy and safety, but with reduced procedural complexity.
Aim: To compare rTAP vs. DKC by optical coherence tomography (OCT) on the intermediate term.
Methods: 52 consecutive patients with complex unprotected LM stenoses (Medina 0,1,1 or 1,1,1) were randomized to either DKC or rTAP and followed-up for a median of 189[180–263] days for clinical and OCT outcomes.
Results: At follow-up OCT showed similar change in the side branch (SB) ostial area (primary endpoint). The confluence polygon showed a higher percentage of malapposed stent struts in the rTAP group that did not reach statistical significance (rTAP: 9.7[4.4–18.3] % vs. DKC: 3[0.07–10.9] %; p = 0.064). It also showed a trend towards larger neointimal area relative to the stent area (DKC: 8.8 [6.9 to 13.4] % vs. rTAP: 6.5 [3.9 to 8.9] %; p = 0.07), and smaller luminal area (DKC: 9.54[8.09–11.07] mm2 vs. rTAP: 11.21[9.53–12.42] mm²; p = 0.09) in the DKC group. The minimum luminal area in the parent vessel distal to the bifurcation was significantly smaller in the DKC group (DKC: 4.64 [3.64 to 5.34] mm² vs. rTAP: 6.76 [5.20 to 7.29] mm²; p = 0.03). This segment also showed a trend for smaller stent areas (p = 0.05 to 0.09), and a bigger neointimal area relative to the stent area (DKC: 8.94 [5.43 to 10.5]% vs. rTAP: 4.75 [0.08 to 8.5]%; p = 0.06) in the DKC patients. The incidence of clinical events was comparably low in both groups.
Conclusion: At 6-months, OCT showed a similar change in the SB ostial area (primary endpoint) in rTAP compared to DKC. There was also a trend for smaller luminal areas in the confluence polygon and the distal parent vessel, and a larger neointimal area relative to the stent area, in DKC, along with a tendency for more malapposed stent struts in rTAP.
Clinical Trial Registration: https://clinicaltrials.gov/ct2/show/NCT03714750, identifier: NCT03714750.
1. Introduction
Although distal left main (LM) disease has been treated with coronary artery bypass grafting for several decades, the advances in stent designs, adjunctive pharmacotherapy, and the evolution of intravascular imaging to guide and optimize percutaneous coronary interventions (PCI), make interventional treatment a viable alternative in cases with low to intermediate syntax score (1). In an attempt to improve immediate and long-term clinical outcomes, multiple stenting techniques have been proposed, and disagreement exists on whether an upfront single- or two-stent strategy is superior (2). In cases of severe disease in both branches, where an upfront 2-stent strategy is planned, guidelines recommend the DK-Crush (DKC) technique based on evidence from trials comparing the outcomes of this strategy to classic Crush (3) and Culotte stenting (4, 5). Although the discussion regarding the relative merits of different strategies remains open, 2-stent techniques involve many technical steps and demand expertise (6). Consequently, any efforts at simplifying these processes, including reducing procedural times, contrast and x-ray exposure while preserving patient outcomes are welcome. In a recently published paper, we reported the outcomes of a randomized trial comparing DKC with a simplified variant involving a shorter stent crush length and only one rewiring. We reported that this variation, which we called reverse-T-and-protrusion (rTAP) and which resembles a previously reported technique named “cone flare DKC”(7), was non-inferior to DKC in terms of side branch (SB) ostial expansion and was associated with shortened procedural times (8). In the present study, we compare the intermediate-term outcomes assessed by optical coherence tomography (OCT) of patients with LM bifurcation disease, randomized to either the DKC technique or rTAP. The purpose of the new proposed technique is to minimize procedural time and complexity without compromising patient outcomes.
2. Materials and methods
2.1. Study design
In this 1:1 randomized controlled trial (NCT03714750), 52 consecutive patients with unprotected complex distal LM bifurcation disease (Medina 0,1,1 or 1,1,1) and a heart team recommendation for PCI treatment were randomly assigned to either of 2 strategies: DKC or rTAP (26 patients in each arm). The inclusion and exclusion criteria as well as the details of both stenting techniques were previously described (9) (Figure 1 depicts the critical step specific to rTAP). Randomization was performed by a computer-generated random sequence (MedCalc Statistical Software version 15.1 (MedCalc Software bvba, Ostend, Belgium)). The study was approved by the local ethics committee and all enrolled patients provided written informed consent.
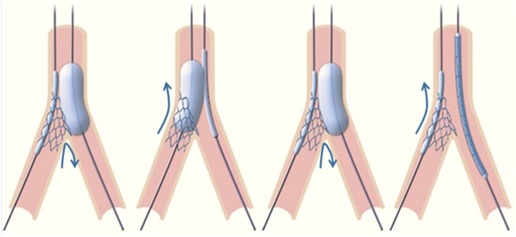
Figure 1. Reverse TAP alternate high-pressure balloon inflations as in the “standard” TAP technique, the goal of these dilatations is to progressively flare the proximal SB stent at the ostium, so that the struts are spread across its circumference. As compared to crush techniques, this approach is designed to avoid double layers of struts on one side. The high-pressure dilations are designed to optimize SB ostium expansion.
2.2. End points
The primary purpose of the current study is to compare the OCT-assessed change in the SB ostial area between the two study arms at 6-months follow-up. As secondary endpoints, we also compared stent and luminal areas, as well as neointimal areas relative to the respective stent areas, in all segments of the bifurcation, in addition to the percentage of malapposed and uncovered stent struts in the confluence polygon.
2.2.1. Optical coherence tomography (OCT)
Patients were scheduled for follow-up diagnostic coronary angiography at 6 months. OCT was performed using the DragonflyTM Duo ILUMIENTM catheter (St. Jude Medical, St. Paul, MN, USA). Two pullbacks were performed from the main branch (MB; parent distal artery), and from the SB to the LM stem, at the speed of 18 mm/second (high resolution mode), to examine the different bifurcation segments. Offline analysis of the acquired data sets was then carried out using QCU-CMS Version 4–69 (Leiden University Medical Center and MEDIS, Leiden, the Netherlands) by a cardiologist blinded to the patient allocation, to the initial post-PCI results as well as to the patients' clinical outcome.
Analysis was performed at 1-mm intervals except for the so-called confluence polygon (carina-anticarina zone, Figure 2), which was analyzed on a frame-by-frame basis. The cross-sectional images were examined in the confluence polygon for the mean stent area, mean luminal area, absolute mean neointimal area (=mean stent area-mean luminal area). The mean neointimal area normalized to the mean stent area was then derived. In other bifurcation segments, the maximum, and minimum stent areas, as well as the minimum luminal area were noted. The mean neointimal area normalized to the mean stent area was again derived. The stent struts were automatically detected by the software on the frames of interest, and the stent and luminal contours were automatically traced (with manual corrections if needed). The percentages of malapposed and uncovered stent struts were calculated. All malapposed struts were counted regardless of the severity/distance of the malapposition.
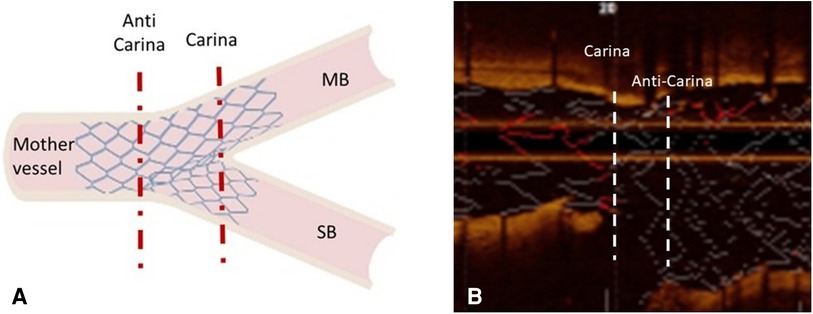
Figure 2. Confluence polygon (carina-anticarina zone) (A) is a schematic depicting the region of the confluence polygon contained between the two dashed red lines. (B) is an example of an OCT longitudinal view showing the confluence polygon confined by the 2 dashed white lines. MB: main branch; SB: side branch.
The change in the SB ostial area from baseline to follow-up was also calculated.
2.2.2. Clinical end points
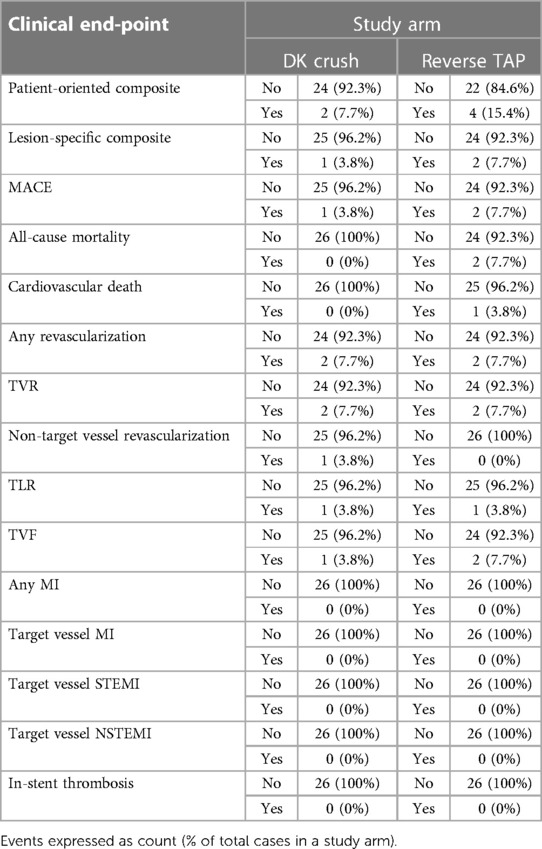
Patients were followed-up by office visits or telephone contact for standardized clinical endpoints (10) including: a patient-oriented composite of all-cause mortality, any revascularization, and any myocardial infarction (MI), in addition to a lesion-specific composite of cardiovascular (CV) death, target lesion revascularization (TLR) (non-protocol-driven), and target vessel MI.
2.3. Statistical analysis
IBM SPSS Statistics Version 23.0.0.2 (2015) and MedCalc Statistical Software version 15.8 (MedCalc Software bvba, Ostend, Belgium; 2015) were used. Continuous variables are presented as medians with interquartile ranges. Categorical variables are presented as counts and percentages. Mann-Whitney U test was used to compare continuous variables between the 2 study arms. A p value < 0.05 was considered statistically significant. The Benjamini Hochberg method was used to adjust for multiple comparisons.
3. Results
The baseline clinical characteristics, procedural characteristics, and procedural outcomes, as well as OCT analysis results, of the 52 enrolled patients were previously reported (8). There were no differences between groups in any of the clinical, procedural, or imaging variables except for ostial side branch expansion, which was significantly larger in the rTAP at the end of the procedure (8).
3.1. Clinical outcomes
Clinical follow-up was available in all patients at 6 months in both groups (Table 1). The lesion-specific endpoint was achieved in only 1 patient in the DKC group (TLR due to unstable angina) and 2 patients in the rTAP group (1 CV death by cardiogenic pulmonary edema, and 1 TLR due to unstable angina). None of the patients had in-stent thrombosis nor STEMI or NSTEMI.
The patient-oriented endpoint was achieved in 2 patients (7.7%) in the DKC arm, who received revascularization vs. 4 patients (15.4%) in the rTAP arm (2 deaths and 2 patients who received revascularization). The Two deaths in the rTAP group included 1 CV death (cardiogenic pulmonary edema at 147 days), and 1 non-CV death (prostatic cancer at 77 days).
Per-protocol coronary angiography was performed in 24 patients at a median of 188.5 days (133 to 337) after index PCI in the DKC group and in 21 patients at a median of 181 days (113 to 378) in the rTAP group. Four patients refused the control coronary angiography, and three others died before scheduled control. None of these patients had symptoms or non-invasive evidence of ischemia.
3.2. OCT analysis results
Of the 45 patients with control coronary angiography, OCT was available in 38 patients (except for SB pullback in a single patient where the OCT catheter failed to cross into the SB).
Baseline clinical characteristics of the patients with follow-up OCT are reported in Supplementary Table S1, and procedural details are reported in Supplementary Table S2. Pre-defined protocol and procedural success was achieved in all patients in both arms (definitions previously reported (8, 9)), with no difference in peak post-procedural troponin between the 2 arms.
3.2.1. Change in side branch ostial area
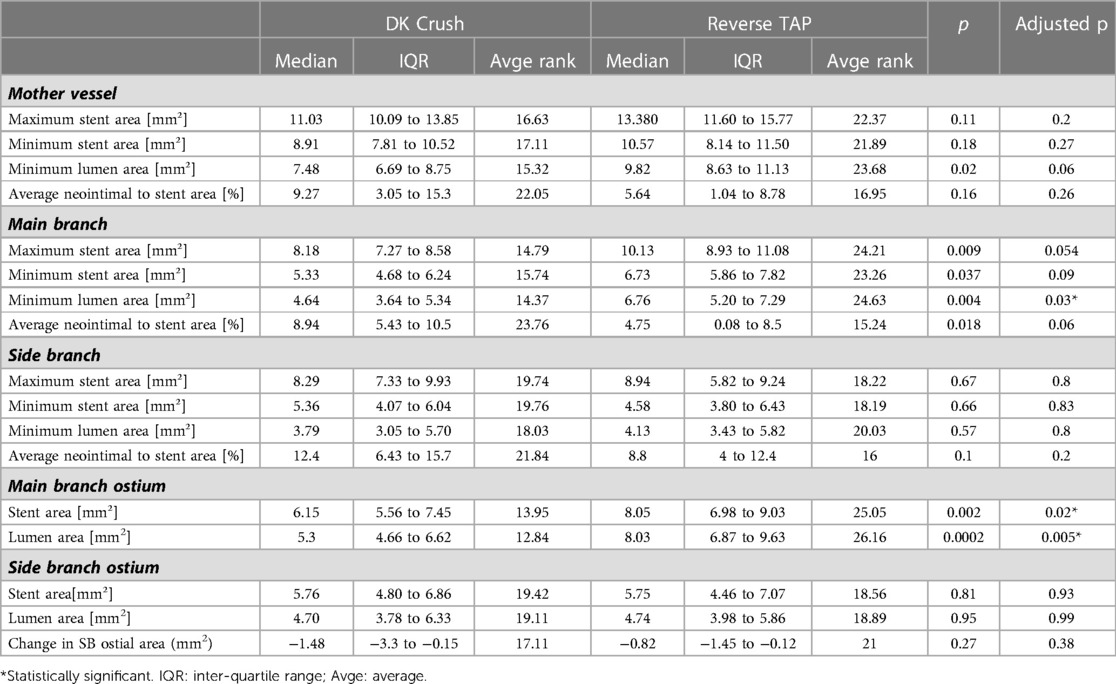
No significant difference was found regarding the change in the SB ostial area from baseline to follow-up in the 2 groups (−1.48[−3.3 to −0.15] mm2 in DKC vs. −0.82[−1.45 to −0.12] mm2 in rTAP; p = 0.38) (Table 3, Figure 3).
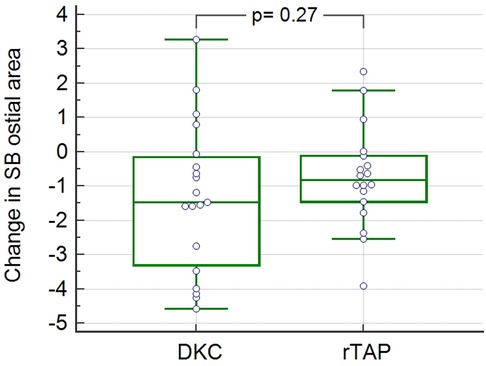
Figure 3. Change in side branch ostial area by OCT in the two study groups OCT: optical coherence tomography; SB: side branch; DKC: double kissing and crush; rTAP: reverse T and protrusion.
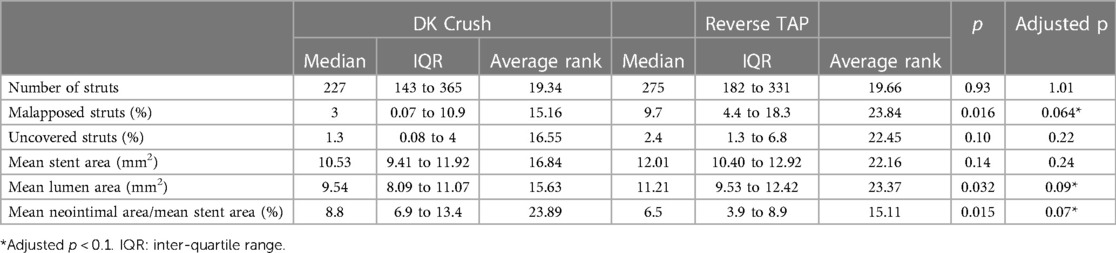
3.2.2. Confluence polygon analysis results
There was a trend for a higher percentage of malapposed stent struts in the rTAP group (rTAP: 9.7 [4.4–18.3] % vs. DKC: 3 [0.07–10.9] %; p = 0.064) that did not reach statistical significance (Figure 4A). However, there was no difference regarding the percentage of uncovered struts (p = 0.22) (Table 2).
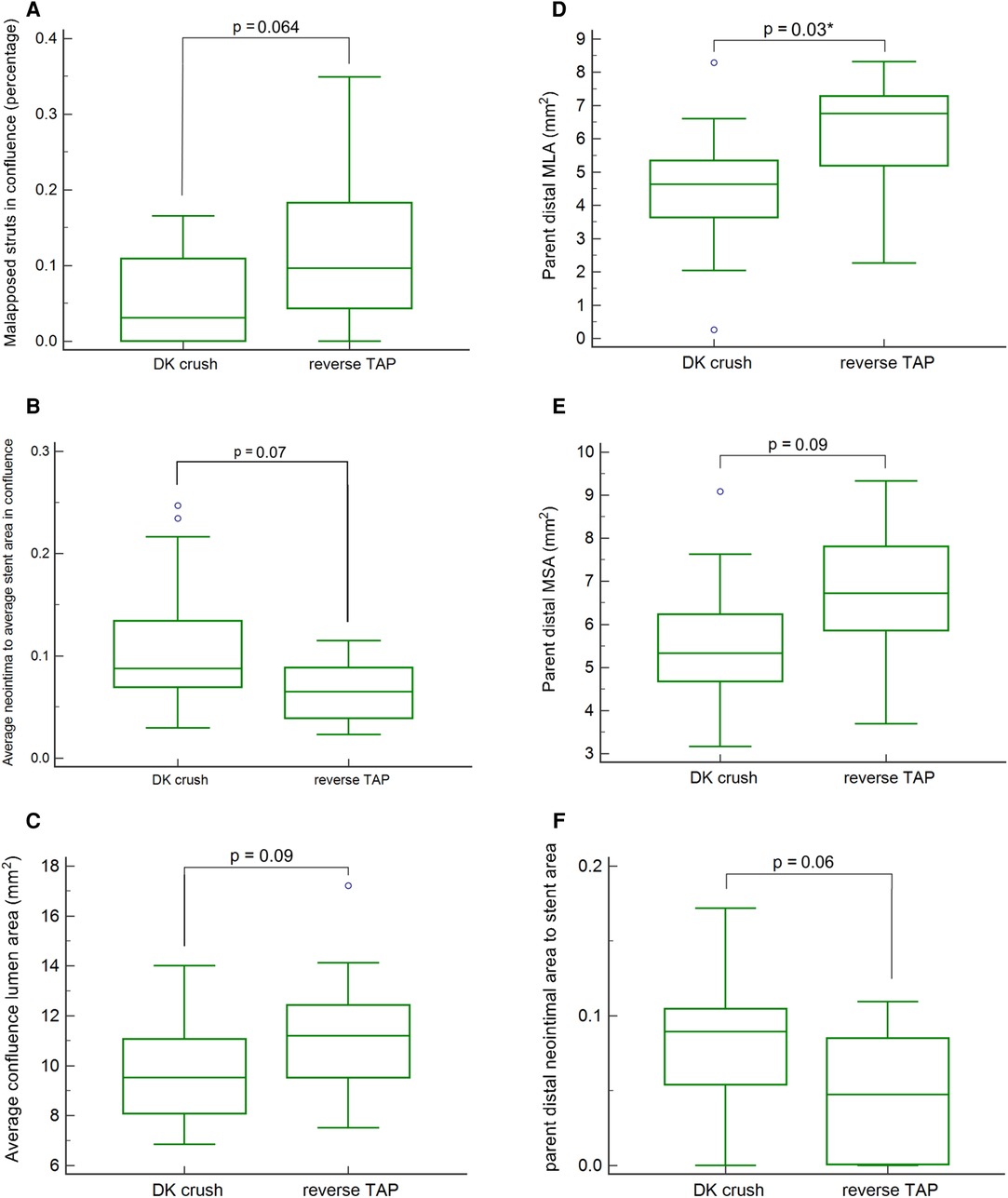
Figure 4. (A) malapposed stent strut percentage in the confluence polygon in the two study groups. (B). Mean neointimal area normalized to mean stent area in the confluence polygon in the two study groups. (C) Mean luminal area in the confluence polygon in the two study groups. (D) Minimal luminal area (MLA) in the main branch distal to the bifurcation in the two study groups *statistically significant. (E) Minimal stent area (MSA) in the main branch distal to the bifurcation in the two study groups. (F) Mean neointimal area normalized to mean stent area in the main branch in the two study groups.
There was also a non-statistically significant trend towards larger neointimal area relative to the stent area (DKC: 8.8 [6.9 to 13.4] % vs. rTAP: 6.5 [3.9 to 8.9] %; p = 0.07), and smaller luminal area (DKC: 9.54[8.09–11.07]mm2 vs. rTAP: 11.21[9.53–12.42]mm²; p = 0.09) in the DKC group (Figures 4B, C respectively), despite no difference in the stent area (10.53 [9.41 to 11.92] mm2 in DKC vs. 12.01 [10.4 to 12.92] mm2 in rTAP; p = 0.2).
3.2.3. Other bifurcation segment analysis results
The minimum luminal area in the parent vessel distal to the bifurcation was significantly smaller in the DKC group (DKC: 4.64 [3.64 to 5.34] mm² vs. rTAP: 6.76 [5.20 to 7.29] mm²; p = 0.03) (Figure 4D). This segment also showed a trend for smaller stent areas (p = 0.05 to 0.09), and a bigger neointimal area relative to the stent area (DKC: 8.94 [5.43 to 10.5] mm2 vs. rTAP: 4.75 [0.08 to 8.5] mm2; p = 0.06) in the DKC patients (Figures 4E, F respectively) (Table 3).
The main branch ostium had a significantly smaller stent and luminal area in the DKC group (6.15 [5.56 to 7.45] mm2 in DKC vs. 8.05 [6.98 to 9.03] mm2 in rTAP; p = 0.02, and 5.3 [4.66 to 6.62] mm2 in DKC vs. 8.03 [6.87 to 9.63] mm2 in rTAP; p = 0.004, respectively).
There was no significant difference in the SB stent or luminal areas between the 2 study groups.
4. Discussion
The differences between rTAP and DKC have been extensively described in a previous paper and are summarized in Figure 1 (8). The major differences include the use of a systematic alternate high-pressure inflation of MB and SB balloons following SB stent implantation and the need for one rewiring in rTAP (instead of two in DKC). In rTAP, this alternate balloon dilation results in the splaying of the proximal SB stent struts along the circumference of the SB ostium. In DKC, the first MB balloon inflation followed by the first rewiring and kissing results in crushing of the proximal SB stent struts on one side.
In our previous publication, the rTAP technique proved to be non-inferior to the gold standard DKC technique in terms of short-term efficacy and safety in the treatment of complex unprotected LM bifurcation lesions. As compared to DKC, rTAP reduced procedural time and improved side branch ostial expansion (8). The current study aims to compare the outcomes, as assessed by OCT, of both techniques at the intermediate term, i.e., 6-months follow-up.
The primary endpoint that we sought to examine is the serial change in the side branch ostial area in the 2 groups. No significant difference was detected in that respect between the 2 study arms (Table 3). Despite that a significantly better SB ostial stent expansion was achieved in rTAP vs. DKC at baseline, both groups had a similar ostial stent area at the end of the procedure (median >5 mm2 in both groups) (8). It is also crucial to note that a follow-up duration of 6 months does not cover the typical time-frame for restenosis in drug-eluting stents, and thus it is critical to observe how this plays out on the longer-term. Different authors have previously pointed out that multiple factors can influence such serial change, including features assessed by 3D-OCT: the SB jailing configuration by the MB stent struts, the site of crossing through the MB stent struts into the SB to perform the KBI (11, 12). These aspects warrant examination in further studies with 3D-OCT reconstruction.
From another perspective, stent strut apposition, tissue coverage, and the extent of neointimal growth are key elements to evaluate in the follow-up of different stenting techniques. The higher percentage of malapposed struts shown by follow-up OCT (including in part SB-ostium-jailing struts) in rTAP compared to DKC, albeit not reaching statistical significance, was not observed immediately after implantation. This can signify a higher incidence of late acquired malapposition. However, since the same stent type and similar deployment pressures were used in the two groups, the mechanisms of this phenomenon are unclear, but it might be hypothesized that the repeated high-pressure inflations might have resulted in more extensive vascular trauma. A more plausible explanation though is that the numerically fewer major malappositions detected at baseline in the DKC group (8), aided neointimal bridging of lesser degrees of malapposition (13–15) in this group as opposed to rTAP.
This tendency for a higher percentage of malapposed struts raises concern because of the unsettled relationship with stent thrombosis. However, it is important to note that the percentage of uncovered stent struts was not different between the 2 study groups, with the caveat that it can be difficult to discern neointima from fibrin depositions on malapposed struts by OCT. Interestingly, none of the patients in the 2 study arms had in-stent thrombotic events, or any kind of MI so far. However, as patients emerge from the protective umbrella of DAPT beyond 1 year, and should this malapposition remain unbridged, there is a higher theoretical risk of late and very late stent thrombosis.
On the other hand, the trend for larger neointimal area relative to the stent area in DKC could be explained by the repeated kissing, which creates more arterial wall stress and trauma, as previously shown by computer simulation, which may in turn trigger an excessive healing response (16). Another interesting finding was the significantly smaller luminal areas in the main branch distal to the bifurcation in DKC, associated with a tendency for smaller stent area, and larger neointimal area relative to the stent area, despite no difference in the used stent or post dilation-balloon diameters. This could be accounted for by the higher burden of calcification (as qualitatively judged on angiography—Supplementary Table S1) in the DKC group, precluding the parent artery stent from expanding to the same extent as in the rTAP group.
Although the current study was not powered to detect differences in clinical outcomes, it is worth noting that both groups showed low rates of target vessel failure which is reassuring from a safety standpoint.
4.1. Limitations
This was a small single-center study performed in a real-life setting, and the rate of loss to invasive follow-up was unfortunately relatively high. Further, the scope of the study was to investigate mid-term OCT parameters and not clinical outcomes, which would have required a much larger sample size.
A number of iterations of the protocol for DK-crush have been published, and we used the one proposed in the EBC consensus of 2018. This limitation obviously applies to any interventional study.
The current study involves only an intermediate-term follow-up. Given that in-stent restenosis typically needs more time to develop in drug-eluting stents, and that patients are still protected by DAPT at 6-months, longer-term follow-up is still needed to observe the impact of the OCT-detected differences on the clinical outcomes in the two study groups.
5. Conclusions
At 6-months, OCT showed a comparable change in the SB ostial area (primary endpoint) in rTAP vs. DKC. There were non-statistically significant trends for smaller luminal areas in the confluence polygon and the distal parent vessel, and larger neointimal areas relative to the stent areas, in DKC, as opposed to more malapposed stent struts in rTAP. The clinical impact of such signals is yet to be seen on longer term follow-up, as well as in other studies adequately powered to examine clinical endpoints.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethikkommission der Landesärztekammer Rheinland Pfalz (Ethics committee of the Rhineland-Palatinate Chamber of Physicians). The patients/participants provided their written informed consent to participate in this study.
Author contributions
TG, MA, HU, and MK conceptualized and designed the study. MO and GM contributed to patient recruitment. AA, GM, and MO contributed to data collection and organization. AA and TG performed the statistical analysis. AA wrote the first draft of the manuscript. TG, TM, and AA were responsible for manuscript revisions and amendments. All authors contributed to the article and approved the submitted version.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study received funding from the Deutsches Zentrum für Herz und Kreislauf Forschung through the professorship of TG.
Acknowledgments
TG and TM receive funding from the Center for Translational Vascular Biology, Mainz.
Conflict of interest
TG has received speaker fees and grant support from Abbott Vascular, Boston Sci., SMT (not in relationship with this research). TG is principal investigator of the DZHK, funded by the Ministry of Research, Germany.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1153652/full#supplementary-material.
Abbreviations
LM, left main; DKC, double kissing and crush:rTAP, reverse T and protrusion; OCT, optical coherence tomography; SB, side branch; PCI, percutaneous coronary intervention; MB, main branch (parent distal artery).
References
1. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. (2019) 40:87–165. doi: 10.1093/eurheartj/ehy394
2. Burzotta F, Lassen JF, Lefevre T, Banning AP, Chatzizisis YS, Johnson TW, et al. Percutaneous coronary intervention for bifurcation coronary lesions: the 15(th) consensus document from the European bifurcation club. EuroIntervention. (2021) 16:1307–17. doi: 10.4244/EIJ-D-20-00169
3. Chen SL, Zhang JJ, Ye F, Chen YD, Patel T, Kawajiri K, et al. Study comparing the double kissing (DK) crush with classical crush for the treatment of coronary bifurcation lesions: the DKCRUSH-1 bifurcation study with drug-eluting stents. Eur J Clin Invest. (2008) 38:361–71. doi: 10.1111/j.1365-2362.2008.01949.x
4. Chen SL, Xu B, Han YL, Sheiban I, Zhang JJ, Ye F, et al. Comparison of double kissing crush versus culotte stenting for unprotected distal left main bifurcation lesions: results from a multicenter, randomized, prospective DKCRUSH-III study. J Am Coll Cardiol. (2013) 61:1482–8. doi: 10.1016/j.jacc.2013.01.023
5. Chen SL, Xu B, Han YL, Sheiban I, Zhang JJ, Ye F, et al. Clinical outcome after DK crush versus culotte stenting of distal left main bifurcation lesions: the 3-year follow-up results of the DKCRUSH-III study. JACC Cardiovasc Interv. (2015) 8:1335–42. doi: 10.1016/j.jcin.2015.05.017
6. Zhang JJ, Chen SL. Classic crush and DK crush stenting techniques. EuroIntervention. (2015) 11(Suppl V):V102–5. doi: 10.4244/eijv11sva23
7. Peverill WT, Incani A, Worthley SG, Singbal Y, Garrahy PJ, McCann AB, et al. The cone flare crush modified-T (CFCT) stenting technique for coronary artery bifurcation lesions. Int J Cardiol Heart Vasc. (2020) 30:100643. doi: 10.1016/j.ijcha.2020.100643
8. Olschewski M, Ullrich H, Knorr M, Makmur G, Ahoopai M, Munzel T, et al. Randomized non-inferiority TrIal comParing reverse T and protrusion versus double-kissing and crush stenting for the treatment of complex left main bifurcation lesions. Clin Res Cardiol. (2021) (7):750–760. doi: 10.1007/s00392-021-01972-2
9. Rakhimov K, Buono A, Anadol R, Ullrich H, Knorr M, Ahoopai M, et al. Randomised, non-inferiority, controlled procedural outcomes TrIal comParing reverse T and protrusion versus double-kissing and crush stenting: protocol of the TIP TAP I randomised trial. BMJ Open. (2020) 10:e034264. doi: 10.1136/bmjopen-2019-034264
10. Garcia-Garcia HM, McFadden EP, Farb A, Mehran R, Stone GW, Spertus J, et al. Standardized End point definitions for coronary intervention trials: the academic research consortium-2 consensus document. Circulation. (2018) 137:2635–50. doi: 10.1161/CIRCULATIONAHA.117.029289
11. Nakamura T, Okamura T, Fujimura T, Yamada J, Nao T, Tateishi H, et al. Serial changes in the three-dimensional aspect of the side-branch ostium jailed by a drug-eluting stent assessed by optical coherence tomography. Int J Cardiovasc Imaging. (2017) 33:797–806. doi: 10.1007/s10554-017-1080-8
12. Fujimura T, Okamura T, Tateishi H, Nakamura T, Yamada J, Oda T, et al. Serial changes in the side-branch ostial area after main-vessel stenting with kissing balloon inflation for coronary bifurcation lesions, assessed by 3D optical coherence tomography. Eur Heart J Cardiovasc Imaging. (2018) 19:1117–25. doi: 10.1093/ehjci/jex213
13. Gutierrez-Chico JL, Wykrzykowska J, Nuesch E, van Geuns RJ, Koch KT, Koolen JJ, et al. Vascular tissue reaction to acute malapposition in human coronary arteries: sequential assessment with optical coherence tomography. Circ Cardiovasc Interv. (2012) 5:20–9. S1-8. doi: 10.1161/CIRCINTERVENTIONS.111.965301
14. Shimamura K, Kubo T, Akasaka T, Kozuma K, Kimura K, Kawamura M, et al. Outcomes of everolimus-eluting stent incomplete stent apposition: a serial optical coherence tomography analysis. Eur Heart J Cardiovasc Imaging. (2015) 16:23–8. doi: 10.1093/ehjci/jeu174
15. Sotomi Y, Onuma Y, Dijkstra J, Miyazaki Y, Kozuma K, Tanabe K, et al. Fate of post-procedural malapposition of everolimus-eluting polymeric bioresorbable scaffold and everolimus-eluting cobalt chromium metallic stent in human coronary arteries: sequential assessment with optical coherence tomography in ABSORB Japan trial. Eur Heart J Cardiovasc Imaging. (2018) 19:59–66. doi: 10.1093/ehjci/jew329
Keywords: left main, bifurcation, optical coherence tomography (OCT), reverse t and protrusion, double kissing and crush
Citation: Abouelnour AE, Olschewski M, Makmur G, Ullrich H, Knorr M, Ahoopai M, Münzel T and Gori T (2023) Six-months clinical and intracoronary imaging follow-up after reverse T and protrusion or double-kissing and crush stenting for the treatment of complex left main bifurcation lesions. Front. Cardiovasc. Med. 10:1153652. doi: 10.3389/fcvm.2023.1153652
Received: 29 January 2023; Accepted: 12 April 2023;
Published: 27 April 2023.
Edited by:
Gianluca Caiazzo, Azienda Sanitaria Locale Caserta, ItalyReviewed by:
Rocco Vergallo, University of Genoa, ItalyLuigi Di Serafino, Federico II University Hospital, Italy
© 2023 Abouelnour, Olschewski, Makmur, Ullrich, Knorr, Ahoopai, Münzel and Gori. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tommaso Gori dG9tbWFzby5nb3JpQHVuaW1lZGl6aW4tbWFpbnouZGU=
 Amr EI Abouelnour
Amr EI Abouelnour Maximilian Olschewski
Maximilian Olschewski Giulio Makmur1
Giulio Makmur1 Helen Ullrich
Helen Ullrich Thomas Münzel
Thomas Münzel Tommaso Gori
Tommaso Gori