
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 16 March 2023
Sec. Coronary Artery Disease
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1143509
This article is part of the Research Topic Management of Ischemic Cardiomyopathy View all 4 articles
Background: Current guidelines recommend potent P2Y12 inhibitors for patients after acute coronary syndrome. However, the data on the efficacy and safety of potent P2Y12 inhibitors in elderly Asian populations was limited. We aimed to investigate the major adverse cardiovascular events (MACE), bleeding events, and net adverse clinical events (NACE) with ticagrelor and clopidogrel in Taiwanese patients aged 65 and older after acute myocardial infarction (AMI).
Methods: This retrospective population-based cohort study was conducted using data from the National Health Insurance Research Database. The AMI patients aged ≥65 years who underwent percutaneous coronary intervention (PCI) and survived after 1 month were included. The patients were separated into 2 cohorts depending on the type of dual antiplatelet therapy (DAPT) they received: ticagrelor plus aspirin (T + A) or clopidogrel plus aspirin (C + A). We used inverse probability of treatment weighting to balance the difference between these 2 study groups. The outcome included all-cause mortality, MACE (cardiovascular death, nonfatal ischemic stroke, and nonfatal myocardial infarction), intracerebral hemorrhage, major bleeding, and NACE which is composed of cardiovascular death, ischemic and hemorrhagic events. The follow-up period was up to 12 months.
Results: From 2013 to 2017, a total of 14,715 patients who met the eligibility criteria were separated into 2 groups: 5,051 for T + A and 9,664 for C + A. Compared to patients with C + A, patients who received T + A had a lower risk of cardiovascular death and all-cause death, with an adjusted HR of 0.57 [95% confidence interval (CI), 0.38–0.85, p = 0.006] and 0.58 (95% CI 0.45–0.74, p < 0.001), respectively. No differences were found in MACE, intracranial and major bleeding between the 2 groups. In addition, the patients with T + A had a lower risk of NACE with an adjusted HR of 0.86 (95% CI 0.74–1.00, p = 0.045)
Conclusion: Among elderly AMI patients receiving DAPT after successful PCI, ticagrelor was a more favorable P2Y12 inhibitor than clopidogrel because of lowering the risk of death and NACE without increasing the risk of severe bleeding. Ticagrelor is an effective and safe P2Y12 inhibitor in Asian elderly survivors after PCI.
The Asia-Pacific region is populated by more than 4.2 billion inhabitants, equivalent to 60% of the world's population. Acute coronary syndrome (ACS) is now a major cause of death and disability in this region as the Western conturies (1). Dual antiplatelet therapy (DAPT), consisting of aspirin combined with a P2Y12 inhibitor, has been the standard of care in preventing coronary and cerebrovascular thrombotic events in patients with chronic coronary syndrome and ACS, but choosing the optimal treatment combination and balance between the ischemic and bleeding risk of treatment duration have become difficult challenges (2–4). Current guidelines recommend using risk stratification instruments for tailoring treatment duration and composition (5–9).
In the global randomized controlled Phase III PLATO trial, ticagrelor, a more potent P2Y12 receptor antagonist, has been demonstrated to reduce the composite end-point of myocardial infarction (MI), stroke, and death from cardiovascular causes across different age groups (10). However, potent P2Y12 inhibitor-related bleeding occurred more frequently in elder ACS patients, than clopidogrel-related bleeding in real-world practice (11). And yet, no guideline suggests the choice of DAPT by age group. To fill in the knowledge gap, our study aimed to examine the effectiveness and safety of ticagrelor or clopidogrel combined with aspirin as dual antiplatelet therapy among AMI patients aged 65 years and older who underwent percutaneous coronary intervention (PCI).
This retrospective population-based cohort study was conducted by using data from the National Health Insurance Research Database (NHIRD) that was maintained by the Health and Welfare Data Science Center, Ministry of Health and Welfare. The NHIRD was a claims-based database that covered healthcare utilization and costs for 99% of residents in Taiwan. The NHIRD files included inpatient, outpatient, and pharmaceutical claims. The data of disease diagnosis was coded by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), and the Tenth Version (ICD-10-CM) after 2016. The data of prescription drugs can be classified based on Anatomical Therapeutic Chemical (ATC) classification. In addition, the enrollment files of beneficiaries and providers were included. The data period used in this study was from 2013 to 2017. The study protocol had been reviewed and approved by Taipei Medical University Joint Institutional Review Board (N202205097).
Patients first diagnosed with AMI, including ST elevation (STEMI) and non-ST elevation myocardial infarction (NSTEMI), and who underwent PCI between 2013 and 2017 were included. The period was chosen to follow the regulations of the National Health Insurance Administration because ticagrelor was first reimbursed for treating patients with AMI after July 1st, 2013. The reimbursed DAPT duration was 9 months after AMI. Of these patients, we added several exclusion criteria to ensure that the patients were eligible for the current study, including (1) age less than 65 years, sex information missing, or not a resident in Taiwan; (2) did not have heparin or antiplatelet agents during the AMI admission; (3) had anticoagulant drugs or had aspirin only during the AMI admission; (4) died within a month after the index AMI; and (5) had a history of coronary artery bypass graft during the study period. Of the patients, we excluded those who had no prescription claim of DAPT, switched the type of DAPT, or had a medication possession ratio (MPR) <0.8 within a month after AMI discharge. MPR is defined as the total number of days covered by filled prescriptions divided by a predefined period (i.e., 30 days). The value of MPR ≥0.8 suggests a significantly higher adherence (12). Figure 1 depicts the process of patient selection in detail.
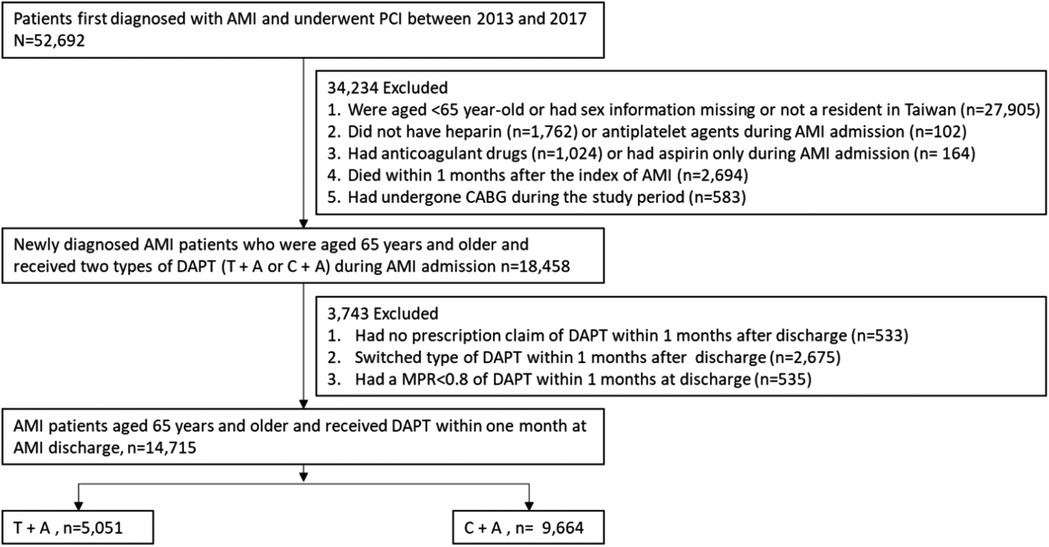
Figure 1. Patient selection process. A, aspirin; AMI, acute myocardial infraction; C, clopidogrel; CABG, coronary artery bypass graft; DAPT, dual antiplatelets therapy; MPR, medication possession ratio; PCI, percutaneous coronary intervention; T, ticagrelor.
The disease diagnosis codes for baseline comorbidities and ATC codes for medications were provided in Supplementary Table S1. Baseline cardiovascular and bleeding risks were assessed at the time of inclusion. We considered the risk of hypertension, diabetes, hyperlipidemia, heart failure, and prior stroke/transient ischemic stroke. Also, we combined comorbidity information into the CHA2DS2-VASC score (congestive heart failure, hypertension, age ≥75 years, diabetes, stroke/TIA, vascular disease, age 65–74 years, sex category) for quantifying thromboembolic risk (13). To assess the risk of bleeding, a history of anemia, bleeding, the ORBIT score (age ≥74 years, anemia, bleeding history, GFR <60 ml/min/1.73 m2, treatment with antiplatelet therapy), and HAS-BLED score (hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, age >65 years, drugs/alcohol concomitantly) were used (14, 15). Both the ORBIT score and HAS-BLED score can predict major bleeding better than other risk scores and were validated in large studies. To control the confounding effect due to the medication history that might associate with cardiovascular outcomes or bleeding events additionally, we considered whether patients had DAPT or NSAIDs more than 3 months within a year before the AMI admission (16, 17).
The outcomes of interest included major adverse cardiovascular events (MACE), cardiovascular death, and all-cause death to evaluate the effectiveness of therapy. MACE is defined as a composite of nonfatal ischemic stroke nonfatal MI, and cardiovascular death. The events of intracerebral hemorrhage (ICH) and major bleeding were considered to assess the safety of the treatment. The definition of major bleeding was hospitalized due to bleeding, symptomatic bleeding in a critical area or organ, or bleeding leading to transfusion of more than 2 units of packed red blood cells. We also analyzed the net adverse clinical events (NACE), composed of cardiovascular death, ischemic events (recurrent nonfatal MI or nonfatal ischemic stroke), and hemorrhagic events (Intracerebral hemorrhage or major bleeding). The follow-up period was up to 12 months. The disease diagnosis codes for study outcomes are provided in Supplementary Table S1.
Baseline characteristics were analyzed using standardized mean difference. A standardized mean difference of greater than 0.1 indicates the non-negligible difference between the two groups. Inverse probability of treatment weighted (IPTW) analysis was conducted to adjust for differences in baseline characteristics between the two cohorts. Cox proportional hazard regression adjusted for baseline covariates and medications listed in Table 1 were used to estimate the hazard ratio (HR) between two treatment regimens. Each patient was followed from the date of AMI discharge to the date of the event of interest or up to 1 year of follow-up. All the variables were included in multivariable Cox analyses. All analyses were performed using SAS/STAT 9.4 (SAS Institute Inc., Cary, NC) and STATA 14 (Stata Corp LP, College Station, TX). A p value <0.05 was considered significant.
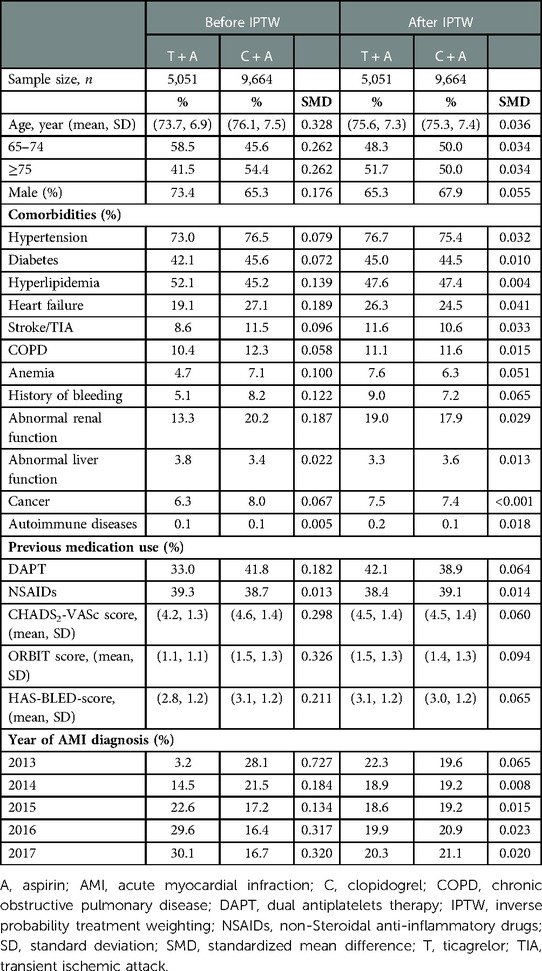
Table 1. Baseline characteristics of the elderly AMI patients who received aspirin with ticagrelor or clopidogrel before and after IPTW.
Among 52,692 patients first diagnosed with AMI and underwent PCI between 2013 and 2017, a total of 14,715 patients, including STEMI (49.7%) and NSTEMI (50.3%) met the eligibility criteria. The patients were separated into two cohorts depending on the type of DAPT: 5,051 for ticagrelor plus aspirin (T + A) and 9,664 for clopidogrel plus aspirin (C + A) (Figure 1).
Baseline characteristics are shown in Table 1. Before IPTW, patients who received T + A were younger and had a higher percentage of males but a lower percentage of comorbidities, CHA2DS2-VASc, ORBIT, and HAS-BLED scores. Also, more patients had received T + A in more recent years. The mean (±standard deviation) DAPT duration of T + A and C + A was 7.1 (±3.9) and 7.9 (±3.7) months (p = 0.218), respectively. After IPTW, baseline characteristics were well-balanced between the 2 groups.
The incidence and relative risks of MACE, cardiovascular death, and all-cause death are shown in Figure 2. Compared to patients with C + A, patients with T + A had a lower risk of cardiovascular death and all-cause death, with an adjusted HR of 0.57 (95% confidence interval 0.38–0.85, p = 0.006) and 0.58 (95% confidence interval 0.45–0.74, p < 0.001). The MACE events rate was lower in the T + A group, although the p-value was insignificant. The recurrent MI and ischemic stroke events rate were comparable in 2 groups (Supplementary Figure S1). After stratifying the analysis into different age groups, the protective effect on cardiovascular death and all-cause death was observed in patients aged 75 years and over in the T + A group.
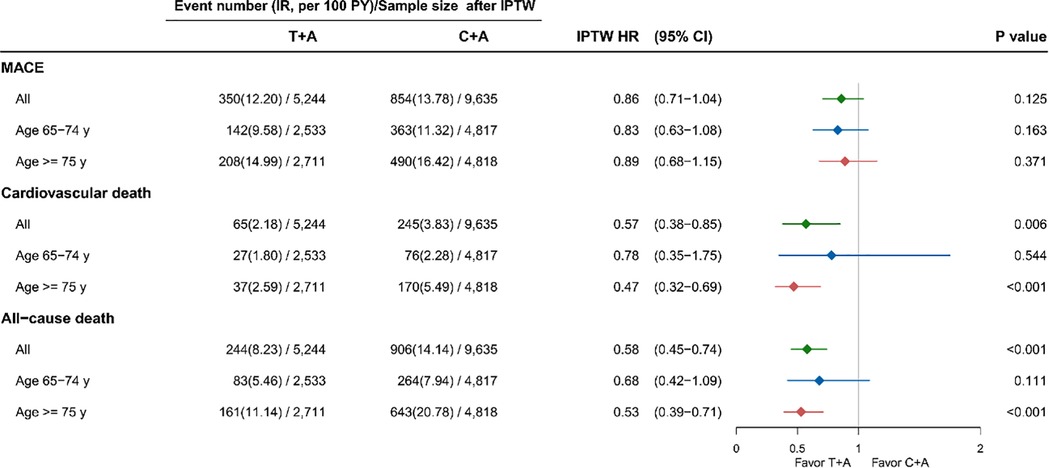
Figure 2. Effectiveness of ticagrelor and clopidogrel on MACE, cardiovascular death and all-cause death among AMI patients. A, aspirin; AMI, acute myocardial infraction; C, clopidogrel; HR, hazard ratio; IPTW, inverse probability treatment weighting; MACE, major adverse cardiovascular events; T, ticagrelor; y, years.
The incidence and relative risks of ICH and major bleeding are shown in Figure 3. No differences were found in ICH and major bleeding between the 2 groups. The results were also similar in both age groups. The Figure 4 revealed the patient with T + A had lower risk of NACE, with an adjusted HR of 0.86 (95% confidence interval 0.74–1.00, p = 0.045) while no different in age groups.
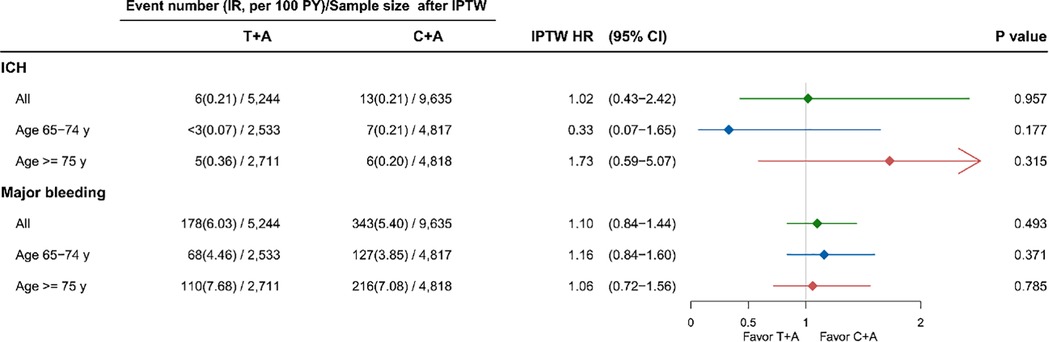
Figure 3. Safety of ticagrelor and clopidogrel on ICH and major bleeding among AMI patients. A, aspirin; AMI, acute myocardial infraction; C, clopidogrel; HR, hazard ratio; ICH, intracerebral hemorrhage; IPTW, inverse probability treatment weighting; T, ticagrelor; y, years.
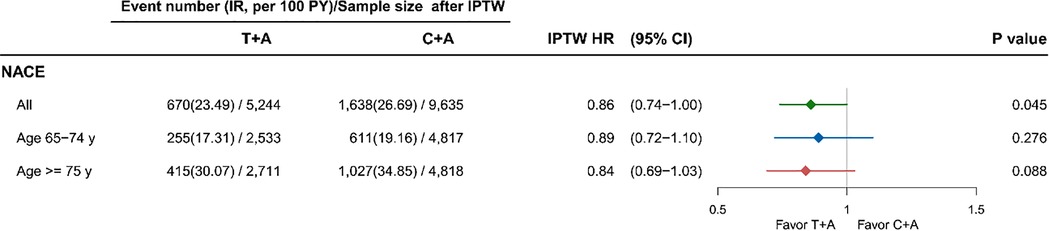
Figure 4. Outcome of ticagrelor and clopidogrel on NACE among AMI patients. A, aspirin; AMI, acute myocardial infraction; C, clopidogrel; HR, hazard ratio; ICH, intracerebral hemorrhage; IPTW, inverse probability treatment weighting; NACE, net adverse clinical event; STEMI, ST segment elevation myocardial infarction; T, ticagrelor; y, years.
This nationwide population-based cohort study found that ticagrelor was superior to clopidogrel in lowering the risk of death and NACE while not increasing the risk of marjor bleeding among elderly AMI patients after PCI. The phenomenon was found in those aged 65 years and older.
Studies have shown that compared to clopidogrel, the more potent P2Y12 inhibitors, including prasugrel and ticagrelor, further reduced the risk of death, MI, and stroke in ACS patients (18, 19). But, an increase in non-critical major bleeding risk was found in the patients with these more potent P2Y12 inhibitors, which might indicate a trade-off between the anti-thrombotic benefit and the bleeding side effects (20). The hemorrhagic risk rises exponentially from the seventh decade, leading to prolonged hospital stay, increased medical expenses, and disproportionate risk of death (21). A previous Taiwanese retrospective national cohort study revealed a similar cardiovascular benefit of ticagrelor while limited to NSTEMI patients (22). In our study, we included both STEMI and NSTEMI patients and focused our study populations on the elderly because of both high ischemic and bleeding risk in this vulnerable population (23). Furthermore, we analyzed the risk of NACE to weigh the gains and losses of different DAPT strategy. Fortunately, the current large-scale study found the effectiveness and safety of ticagrelor were comparable with clopidogrel in elderly AMI patients based on real-world data.
The fear of increased bleeding risk and the intrinsic frailty of this aging population often lead physicians to prescribe a less potent P2Y12 inhibitor. As a result, those patients might be potentially undertreated and exposed to a higher incidence of thrombotic complications (24–26). According to our data, the percentage of ticagrelor plus aspirin as a DAPT regimen was lower in those aged 75 and older, which was one-third of elderly AMI patients; however, the trend has been increasing gradually recently. One of the possible reasons might be the international and domestic guidelines’ recommendation of ticagrelor over clopdogrel in ACS patients (27–29).
This current study confirmed the significant survival benefit of ticagrelor over clopidogrel and similar major bleeding risk between treatment groups. The similar findings were observed in the PLATO trial although a recent randomized open-label study, POPular-AGE study, including patients aged ≥70 years with non-ST elevation ACS showed similar thrombotic events between ticagrelor and clopidogrel but less bleeding in the clopidogrel group (11). The possible reason for the discrepancy might be due to the less adherence to ticagrelor. A recent analysis from the PARIS (Patterns of Non-Adherence to Anti-Platelet Regimens in Stented Patients) registry suggested that those patients who stop DAPT therapy due to “disruption” (nonadherence or bleeding), have the highest risk of major cardiovascular events (30). In the POPular-AGE trials, the adherence to ticagrelor was lower than that to clopidogrel, with only 53% of patients continuing the more potent P2Y12 inhibitor compared with 78% for clopidogrel during the 12-month follow-up. We only included the patients with a medication possession ratio (MPR) ≥ 0.8 for both DAPT treatment groups; therefore, the benefit of ticagrelor in preventing major cardiovascular events might not be neutralized by the early disruption of this potent P2Y12 inhibitor.
Meanwhile, ticagrelor might have pleiotropic effects that go beyond antiplatelet action. A recent study has indicated that ticagrelor may have antimicrobial activity in a mouse model (31). But, only a few clinical studies have been focused on the potential bactericidal effect (32, 33). We additionally examined the risk of infection events, including pneumonia, urinary tract infection (UTI), and cellulitis after AMI discharge. A decreased risk of pneumonia hospitalization was observed in patients with T + A (Supplementary Figure S2) Compared to patients with C + A, those with T + A had a lower risk of pneumonia (adjusted HR of 0.7, 95% confidence interval 0.56–0.86, p = 0.001). These pleomorphic effects of ticagrelor beyond what we know about the platelet inhibition might provide some hypothesis for our study's survival benefit of ticagrelor over clopidogrel (34, 35). Further studies should be launched and investigated the anti-infective or anti-inflammatory activity of ticagrelor.
Although short duration or de-escalated DAPT strategy might reduce bleeding without increasing cardiovascular events in some studies, but current guideline still recommend DAPT consisting of a potent P2Y12 receptor inhibitor in addition to aspirin for 12 months in acute coronary syndrome patients after PCI, irrespective of the stent type, unless there are contraindications adequate (36–38). Studies are deserved to evaluate the effiicacy and safety of short duration DAPT in elder population.
There were some limitations in this study. First, the NHIRD does not have certain patient information, such as risk behaviors, diet, and physical activities, which might be associated with the outcomes of interest. Second, the NHIRD does not contain clinical information, such as angiographic findings during PCI, the extent of coronary artery disease, and the severity of AMI at admission. Consequently, we could not adjust for the severity of AMI nor could we know whether the AMI admission was planned or not, which might induce non-differential misclassification bias. We did not follow BARC or GUSTO, or TIMI criteria for bleeding classification because of the limitation of NHIRD that laboratory data like the hemoglobin or other exact clinical records was unable to obtain. Therefore, some outcome measurement like minor bleeding might be underestimated. In this study, we defined the major bleeding as being hospitalized due to bleeding, bleeding in a critical organ, or bleeding leading to transfusion that were comparable to the major bleeding of TIMI or BARC 2–3 bleeding criteria. The similar method has been used in the claim-based studies (20, 39). Third, only observed variables were considered in the IPTW; therefore, hidden bias was possible. Finally, we only included Taiwanese patients and we did not include patients with known coronary artery disease or acute coronary syndrome history because they are usually more complicated in clinical condition that may interfere the physicians’ decision on DAPT stategies. Therefore, the results might not be generalizable to other patient populations.
Using the nationwide cohort study, we found that in Asian patients aged 65 years or older presenting with AMI, ticagrelor provided a more favorable outcome than clopidogrel, because it was associated with a lower cumulative rate of all-cause mortality, cardiovascular death and NACE without an increase of intracranial or major bleeding.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
L-NC contributed to conception and design of the study. W-TC and J-SY organized the database. L-NC and W-TC performed the statistical analysis. J-SY and L-NC wrote the first draft of the manuscript. BT wrote sections of the manuscript. J-SY and W-CT submitted the manuscript. All authors contributed to the article and approved the submitted version.
Open access publication fees: Taipei Medical University Wan-Fang Hospital 112-wf-eva-40.
This study was supported by the Health Data Analytics and Statistics Center, Office of Data Science, Taipei Medical University.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1143509/full#supplementary-material.
Supplement Figure 1
Effectiveness of ticagrelor and clopidogrel on MI and ischemic stroke among AMI patients Abbreviation: A=aspirin, AMI=acute myocardial infraction, C=clopidogrel, HR=hazard ratio, IPTW=inverse probability treatment weighting, MI=myocardial infarction, T=ticagrelor, y=years.
Supplementary Figure 2
Effectiveness of ticagrelor and clopidogrel on pneumonia, UTI and Cellulitis among AMI patients after the AMI discharge Abbreviation: A=aspirin, AMI=acute myocardial infraction, C=clopidogrel, HR=hazard ratio, IPTW=inverse probability treatment weighting, T=ticagrelor, UTI= urinary tract infection, y=years.
1. Chan MY, Du X, Eccleston D, Ma C, Mohanan PP, Ogita M, et al. Acute coronary syndrome in the Asia-pacific region. Int J Cardiol. (2016) 202:861–9. doi: 10.1016/j.ijcard.2015.04.073
2. Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, et al. 2017 Esc focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with eacts: the task force for dual antiplatelet therapy in coronary artery disease of the European society of cardiology (Esc) and of the European association for cardio-thoracic surgery (Eacts). Eur Heart J. (2018) 39(3):213–60. doi: 10.1093/eurheartj/ehx419
3. Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. 2016 Acc/aha guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. (2016) 68(10):1082–115. doi: 10.1016/j.jacc.2016.03.513
4. Bianco M, D'Ascenzo F, Raposeiras Roubin S, Kinnaird T, Peyracchia M, Ariza-Solé A, et al. Comparative external validation of the precise-dapt and Paris risk scores in 4424 acute coronary syndrome patients treated with prasugrel or ticagrelor. Int J Cardiol. (2020) 301:200–6. doi: 10.1016/j.ijcard.2019.11.132
5. van der Sangen NMR, Rozemeijer R, Chan Pin Yin D, Valgimigli M, Windecker S, James SK, et al. Patient-tailored antithrombotic therapy following percutaneous coronary intervention. Eur Heart J. (2021) 42(10):1038–46. doi: 10.1093/eurheartj/ehaa1097
6. Costa F, van Klaveren D, James S, Heg D, Räber L, Feres F, et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (precise-dapt) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet. (2017) 389(10073):1025–34. doi: 10.1016/s0140-6736(17)30397-5
7. Yeh RW, Secemsky EA, Kereiakes DJ, Normand SL, Gershlick AH, Cohen DJ, et al. Development and validation of a prediction rule for benefit and harm of dual antiplatelet therapy beyond 1 year after percutaneous coronary intervention. J Am Med Assoc. (2016) 315(16):1735–49. doi: 10.1001/jama.2016.3775
8. Angiolillo DJ, Capodanno D, Danchin N, Simon T, Bergmeijer TO, Ten Berg JM, et al. Derivation, validation, and prognostic utility of a prediction rule for nonresponse to clopidogrel: the abcd-gene score. JACC Cardiovasc Interv. (2020) 13(5):606–17. doi: 10.1016/j.jcin.2020.01.226
9. Tarantini G, Cirillo P, De Servi S, Parodi G, Capodanno D, D'Amico G, et al. Dual antiplatelet therapy in elderly patients with acute coronary syndrome: does age make the difference?. G Ital Cardiol. (2018) 19(7):420–8. doi: 10.1714/2938.29538
10. Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. (2009) 361(11):1045–57. doi: 10.1056/NEJMoa0904327
11. Gimbel M, Qaderdan K, Willemsen L, Hermanides R, Bergmeijer T, de Vrey E, et al. Clopidogrel versus ticagrelor or prasugrel in patients aged 70 years or older with non-st-elevation acute coronary syndrome (popular age): the randomised, open-label, non-inferiority trial. Lancet. (2020) 395(10233):1374–81. doi: 10.1016/s0140-6736(20)30325-1
12. Sperber CM, Samarasinghe SR, Lomax GP. An upper and lower bound of the medication possession ratio. Patient Prefer Adherence. (2017) 11:1469–78. doi: 10.2147/ppa.s136890
13. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. (2010) 137(2):263–72. doi: 10.1378/chest.09-1584
14. O'Brien EC, Simon DN, Thomas LE, Hylek EM, Gersh BJ, Ansell JE, et al. The orbit bleeding score: a simple bedside score to assess bleeding risk in atrial fibrillation. Eur Heart J. (2015) 36(46):3258–64. doi: 10.1093/eurheartj/ehv476
15. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (has-bled) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the euro heart survey. Chest. (2010) 138(5):1093–100. doi: 10.1378/chest.10-0134
16. Graham DJ, Campen D, Hui R, Spence M, Cheetham C, Levy G, et al. Risk of acute myocardial infarction and sudden cardiac death in patients treated with cyclo-oxygenase 2 selective and non-selective non-steroidal anti-inflammatory drugs: nested case-control study. Lancet. (2005) 365(9458):475–81. doi: 10.1016/s0140-6736(05)17864-7
17. Mellemkjaer L, Blot WJ, Sørensen HT, Thomassen L, McLaughlin JK, Nielsen GL, et al. Upper gastrointestinal bleeding among users of nsaids: a population-based cohort study in Denmark. Br J Clin Pharmacol. (2002) 53(2):173–81. doi: 10.1046/j.0306-5251.2001.01220.x
18. Fujisaki T, Kuno T, Ando T, Briasoulis A, Takagi H, Bangalore S. Potent P2y12 inhibitors versus clopidogrel in elderly patients with acute coronary syndrome: systematic review and meta-analysis. Am Heart J. (2021) 237:34–44. doi: 10.1016/j.ahj.2021.03.009
19. Jacobsen MR, Engstrøm T, Torp-Pedersen C, Gislason G, Glinge C, Butt JH, et al. Clopidogrel, prasugrel, and ticagrelor for all-comers with st-segment elevation myocardial infarction. Int J Cardiol. (2021) 342:15–22. doi: 10.1016/j.ijcard.2021.07.047
20. You SC, Rho Y, Bikdeli B, Kim J, Siapos A, Weaver J, et al. Association of ticagrelor vs clopidogrel with net adverse clinical events in patients with acute coronary syndrome undergoing percutaneous coronary intervention. J Am Med Assoc. (2020) 324(16):1640–50. doi: 10.1001/jama.2020.16167
21. Mehran R, Pocock S, Nikolsky E, Dangas GD, Clayton T, Claessen BE, et al. Impact of bleeding on mortality after percutaneous coronary intervention results from a patient-level pooled analysis of the replace-2 (randomized evaluation of pci linking angiomax to reduced clinical events), acuity (acute catheterization and urgent intervention triage strategy), and horizons-ami (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trials. JACC Cardiovasc Interv. (2011) 4(6):654–64. doi: 10.1016/j.jcin.2011.02.011
22. Lee CK, Wang TD, Juang HT, Chang SC, Pan HY, Lin DS, et al. Efficacy and safety of ticagrelor versus clopidogrel in patients with non-st-elevation myocardial infarction in Taiwan. Sci Rep. (2021) 11(1):14150. doi: 10.1038/s41598-021-93712-9
23. Avezum A, Makdisse M, Spencer F, Gore JM, Fox KA, Montalescot G, et al. Impact of age on management and outcome of acute coronary syndrome: observations from the global registry of acute coronary events (grace). Am Heart J. (2005) 149(1):67–73. doi: 10.1016/j.ahj.2004.06.003
24. De Luca L, Leonardi S, Cavallini C, Lucci D, Musumeci G, Caporale R, et al. Contemporary antithrombotic strategies in patients with acute coronary syndrome admitted to cardiac care units in Italy: the eyeshot study. Eur Heart J Acute Cardiovasc Care. (2015) 4(5):441–52. doi: 10.1177/2048872614560505
25. Tegn N, Abdelnoor M, Aaberge L, Endresen K, Smith P, Aakhus S, et al. Invasive versus conservative strategy in patients aged 80 years or older with non-st-elevation myocardial infarction or unstable angina pectoris (after eighty study): an open-label randomised controlled trial. Lancet. (2016) 387(10023):1057–65. doi: 10.1016/s0140-6736(15)01166-6
26. Tarantini G, Ueshima D, D'Amico G, Masiero G, Musumeci G, Stone GW, et al. Efficacy and safety of potent platelet P2y12 receptor inhibitors in elderly versus nonelderly patients with acute coronary syndrome: a systematic review and meta-analysis. Am Heart J. (2018) 195:78–85. doi: 10.1016/j.ahj.2017.09.012
27. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2015 Acc/aha/scai focused update on primary percutaneous coronary intervention for patients with st-elevation myocardial infarction: an update of the 2011 accf/aha/scai guideline for percutaneous coronary intervention and the 2013 accf/aha guideline for the management of st-elevation myocardial infarction. J Am Coll Cardiol. (2016) 67(10):1235–50. doi: 10.1016/j.jacc.2015.10.005
28. Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. 2015 Esc guidelines for the management of acute coronary syndromes in patients presenting without persistent st-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent st-segment elevation of the European society of cardiology (esc). Eur Heart J. (2016) 37(3):267–315. doi: 10.1093/eurheartj/ehv320
29. Li YH, Wang YC, Wang YC, Liu JC, Lee CH, Chen CC, et al. 2018 Guidelines of the Taiwan society of cardiology, Taiwan society of emergency medicine and Taiwan society of cardiovascular interventions for the management of non st-segment elevation acute coronary syndrome. J Formos Med Assoc. (2018) 117(9):766–90. doi: 10.1016/j.jfma.2018.06.002
30. Mehran R, Baber U, Steg PG, Ariti C, Weisz G, Witzenbichler B, et al. Cessation of dual antiplatelet treatment and cardiac events after percutaneous coronary intervention (Paris): 2 year results from a prospective observational study. Lancet. (2013) 382(9906):1714–22. doi: 10.1016/s0140-6736(13)61720-1
31. Lancellotti P, Musumeci L, Jacques N, Servais L, Goffin E, Pirotte B, et al. Antibacterial activity of ticagrelor in conventional antiplatelet dosages against antibiotic-resistant gram-positive bacteria. JAMA Cardiol. (2019) 4(6):596–9. doi: 10.1001/jamacardio.2019.1189
32. Winning J, Reichel J, Eisenhut Y, Hamacher J, Kohl M, Deigner HP, et al. Anti-platelet drugs and outcome in severe infection: clinical impact and underlying mechanisms. Platelets. (2009) 20(1):50–7. doi: 10.1080/09537100802503368
33. Vicent L, Bruña V, Devesa C, Sousa-Casasnovas I, Juárez M, Alcalá L, et al. Ticagrelor and infection risk in patients with coronary artery disease. Cardiology. (2021) 146(6):698–704. doi: 10.1159/000519285
34. Kubisa MJ, Jezewski MP, Gasecka A, Siller-Matula JM, Postuła M. Ticagrelor—toward more efficient platelet inhibition and beyond. Ther Clin Risk Manag. (2018) 14:129–40. doi: 10.2147/tcrm.s152369
35. Sexton TR, Zhang G, Macaulay TE, Callahan LA, Charnigo R, Vsevolozhskaya OA, et al. Ticagrelor reduces thromboinflammatory markers in patients with pneumonia. JACC Basic Transl Sci. (2018) 3(4):435–49. doi: 10.1016/j.jacbts.2018.05.005
36. Tsigkas G, Apostolos A, Trigka A, Chlorogiannis D, Katsanos K, Toutouzas K, et al. Very short versus longer dual antiplatelet treatment after coronary interventions: a systematic review and meta-analysis. Am J Cardiovasc Drugs. (2023) 23(1):35–46. doi: 10.1007/s40256-022-00559-0
37. Yeh JS, Hsu CY, Huang CY, Chen WT, Hsieh YC, Chien LN. The effect of de-escalation of P2y12 receptor inhibitor therapy after acute myocardial infarction in patients undergoing percutaneous coronary intervention: a nationwide cohort study. PLoS One. (2021) 16(1):e0246029. doi: 10.1371/journal.pone.0246029
38. Collet J-P, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, et al. 2020 Esc guidelines for the management of acute coronary syndromes in patients presenting without persistent st-segment elevation: the task force for the management of acute coronary syndromes in patients presenting without persistent st-segment elevation of the European society of cardiology (esc). Eur Heart J. (2020) 42(14):1289–367. doi: 10.1093/eurheartj/ehaa575
Keywords: acute myocardial infarction, clopidogrel, elder, net adverse clinical events, percutaneous coronary intervention, ticagrelor
Citation: Yeh J, Chen W, Tomlinson B, Tam W and Chien L (2023) Comparing the effectiveness and safety of dual antiplatelet with ticagrelor or clopidogrel in elderly Asian patients with acute myocardial infraction. Front. Cardiovasc. Med. 10:1143509. doi: 10.3389/fcvm.2023.1143509
Received: 13 January 2023; Accepted: 27 February 2023;
Published: 16 March 2023.
Edited by:
Grigorios Tsigkas, University of Patras, GreeceReviewed by:
Anna Olasinska-Wisniewska, Poznan University of Medical Sciences, Poland© 2023 Yeh, Chen, Tomlinson, Tam and Chien. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li-Nien Chien bGluaWVuLmNoaWVuQG55Y3UuZWR1LnR3
Specialty Section: This article was submitted to Coronary Artery Disease, a section of the journal Frontiers in Cardiovascular Medicine
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.