
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 05 May 2023
Sec. Hypertension
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1137706
This article is part of the Research Topic Insights in Hypertension: 2022 View all 9 articles
 Valentina Trimarco1,†
Valentina Trimarco1,† Maria Virginia Manzi2,†
Maria Virginia Manzi2,† Raffaele Izzo2
Raffaele Izzo2 Pasquale Mone3,4
Pasquale Mone3,4 Maria Lembo2
Maria Lembo2 Daniela Pacella5
Daniela Pacella5 Giovanni Esposito2
Giovanni Esposito2 Angela Falco1
Angela Falco1 Carmine Morisco2,4
Carmine Morisco2,4 Paola Gallo2
Paola Gallo2 Gaetano Santulli2,3,4,6*
Gaetano Santulli2,3,4,6* Bruno Trimarco2,4
Bruno Trimarco2,4
Background: Adverse drug reactions (ADRs) remain among the leading causes of therapy-resistant hypertension (TRH) and uncontrolled blood pressure (BP). We have recently reported beneficial results in BP control in patients with TRH adopting an innovative approach, defined as therapeutic concordance, in which trained physicians and pharmacists reach a concordance with patients to make them more involved in the therapeutic decision-making process.
Methods: The main scope of this study was to investigate whether the therapeutic concordance approach could lead to a reduction in ADR occurrence in TRH patients. The study was performed in a large population of hypertensive subjects of the Campania Salute Network in Italy (ClinicalTrials.gov Identifier: NCT02211365).
Results: We enrolled 4,943 patients who were firstly followed-up for 77.64 ± 34.44 months, allowing us to identify 564 subjects with TRH. Then, 282 of these patients agreed to participate in an investigation to test the impact of the therapeutic concordance approach on ADRs. At the end of this investigation, which had a follow-up of 91.91 ± 54.7 months, 213 patients (75.5%) remained uncontrolled while 69 patients (24.5%, p < 0.0001) reached an optimal BP control. Strikingly, during the first follow-up, patients had complained of a total of 194 ADRs, with an occurrence rate of 68.1% and the therapeutic concordance approach significantly reduced ADRs to 72 (25.5%).
Conclusion: Our findings indicate that the therapeutic concordance approach significantly reduces ADRs in TRH patients.
While health care systems are known to be highly incentivized to provide care for acute illnesses such as myocardial infarction and stroke, they are not well designed for preventive care (1–3). Primary prevention of cardiovascular disease may potentially be better managed in a system non-centered on the acute care model (4–6). Hence, it is time to acknowledge that standard strategies for blood pressure (BP) management in clinical practice are failing to achieve ideal BP control rates (7–11). New approaches are needed, ideally requiring multifaceted personalized solutions tailored to the needs of specific patients, communities, and health care professionals (12, 13).
Therapy-resistant hypertension (TRH) is defined by BP targets not achieved despite treatment with at least 3 anti-hypertensive drugs of different classes, including a blocker of the renin-angiotensin system, a diuretic, and a long-acting Ca2+ channel blocker (14, 15). TRH is currently observed in more than 10% of hypertensive patients. We have recently reported (16) the favorable results in BP control obtained in a population of patients with TRH applying a clinical approach in which a trained pharmacist was responsible for evaluating the medical pharmacological history, in order to remove drug-drug negative interactions, and the physicians aimed at reaching a concordance with the patients in order to make them better informed, actively engaged, and somehow more gratified. We have demonstrated that therapeutic concordance allows to reach a satisfactory BP control in 25% of patients with uncontrolled TRH (16).
Substantial evidence indicates that 20%–90% of patients can experience adverse events attributable to their antihypertensive therapies (17–20); hence, adverse drug reactions (ADRs) are listed among the main causes of uncontrolled BP by reducing patients' compliance (18, 21–29). On these grounds, we designed the present study to investigate whether the therapeutic concordance approach could induce a reduction in ADR occurrence. The principles of the concordance are centered on better communication and engaging patients in treatment decisions. Etymology may help understanding the meaning of therapeutic concordance: the word concordance comes from the Latin term “concordare”, which means with the same heart, inferring mutual trust and consensus between two parties in the decision-making process.
The approach of concordance that allows patient autonomy was conceived in the UK in 1997, when the Royal Pharmaceutical Society of Great Britain published a report entitled “From Compliance to Concordance: Achieving Shared Goals in Medicine Taking” (30), describing the new model of therapeutic concordance, in which patients and doctors work together towards shared therapeutic goals. Initially limited to the consultation process, in which doctor and patient agree on therapeutic decisions that incorporate their respective views, the definition of therapeutic concordance also includes prescribing communication and patient support in medicine taking. Concordance should not be confused with compliance or adherence (31–33). Indeed, compliance is “the extent to which the patient's behavior matches the prescriber's recommendations”, whilst adherence is defined as “the extent to which the patient's behavior matches agreed recommendations from the prescriber”.
Health-care professionals adapt their style to meet the individual needs of patients and to make information about chronic conditions and their treatment as accessible as possible. They enquire sympathetically about side-effects and ask patients whether they realize the merits of treatment. They counsel patients on the importance of concordance and how to organize their medication, enlisting the help of family members and reiterate the potential risk of sudden unauthorized withdrawal of medications.
The study was performed in a population of hypertensive patients of the Campania Salute Network (CSN), which is an open electronic registry [currently including more than 15,000 hypertensive subjects (34)] that fosters the interaction between the Hypertension Research Center of “Federico II” University Hospital in Naples and primary physicians as well as hypertension clinics within the Campania region in Italy (ClinicalTrials.gov: NCT02211365) (34–37).
Patients with uncontrolled office BP (OBP ≥ 140/90 mmHg) and home BP (HBP > 135/85 mmHg), were included in a long-term follow-up. At the end of this procedure, the patients that despite taking 3 antihypertensive drugs including a diuretic, showed uncontrolled office BP and HBP were included in the arm of true TRH (tTRH); instead, patients with uncontrolled office BP but with optimal HBP (white coat effect) were entered in the arm of apparent (aTRH) (38, 39).
Thereafter, tTRH patients were included in the intervention arm of therapeutic concordance, with follow-up visits scheduled at 6-month intervals. Details about the therapeutic concordance approach have been previously described (16).
Demographics, relevant risk factors, and main clinical characteristics were acquired at enrollment, including age, race, sex, smoking status, weight, diabetes, history of stroke and heart attack history.
For each patient, the physician registered the types of antihypertensive drugs, their dosage, and the use of other drugs alongside with information about the actual length of the anti-hypertensive treatment and the adverse events spontaneously reported by the patients. The term ADRs implies a causal relationship with the anti-hypertensive treatment; so, ADRs were confirmed using the Liverpool Algorithm (40), consisting of the following scale of 4: “Unlikely”, “Possible”, “Probable”, and “Definite”.
Following current guidelines (41), BP was measured after five minutes resting in the sitting position, three times at one-minute interval; all enrolled subjects were also encouraged to measure their HBP utilizing validated devices (41). Follow-up BP and HBP were defined as optimally controlled if the average OBP values was <140/90 mmHg or if the average HBP self-reported value was <135/85 mmHg, respectively (42). The estimated glomerular filtration rate was achieved by means of the Chronic Kidney Disease Epidemiology Collaboration equation, as described (43).
Our primary endpoint was to assess whether the use of a therapeutic concordance approach could reduce ADRs. Secondary endpoint was whether a reduction in ADRs, if any, correlates with an improvement in BP control.
Data were analyzed using Jamovi and SPSS (version 25.0; IBM, Armonk, NY) and expressed as mean ± SD. The normal distribution of values was confirmed applying the Shapiro-Wilk test. Continues variables were analyzed using the Student's t test. We rejected the null hypothesis at a two-tailed p < 0.05.
From the initial CSN cohort of 5,331 hypertensive subjects with ascertained HBP measurements, and absence of coronary heart disease, we excluded patients with secondary hypertension as well as individuals with a follow-up of less than twelve months, obtaining 4,943 subjects. These patients were firstly monitored for 77.64 + 34.44 months, yielding to the identification of 322 patients with a white coat effect (aTRH, i.e., uncontrolled OBP and optimal HBP) and 4,057 subjects without TRH.
Therefore, from the first follow-up study, we obtained 564 tTRH subjects with uncontrolled OBP (BP ≥ 140/90 mmHg) and HBP (BP > 135/85 mmHg) according to the above-mentioned definition. Since some of these patients did not accept to participate in our study testing the therapeutic concordance approach, we obtained a population of two-hundred eighty-two tTRH patients who in the first follow-up did not display any significant change in BP. The baseline characteristics of these patients are reported in Table 1.
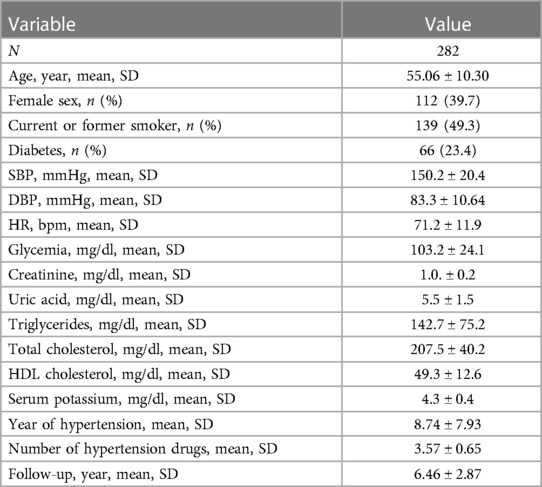
Table 1. Baseline characteristics of patients with true therapy-resistant hypertension enrolled in the study.
During the first follow-up period, 194 ADRs were recorded (Table 2) with an occurrence rate of 68.8%. Thereafter, the hypertensive subjects were monitored according to the therapeutic concordance protocol for a second follow-up period, which lasted 91.91 + 54.7 months.
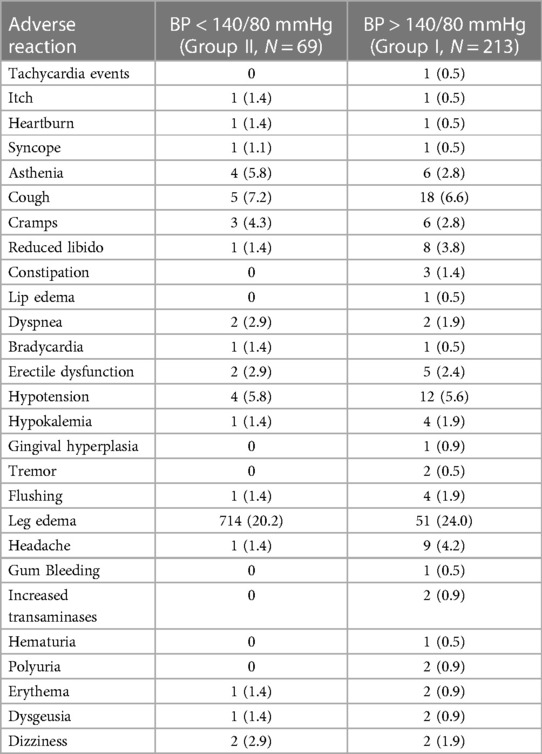
Table 2. Percentage of adverse reactions recorded before the concordance therapeutic approach. The population has been divided in subgroups according to the BP response during the second follow-up period (Group 1 without, Group II with optimal BP control). Data are expressed as number (%).
After the therapeutic concordance approach 213 patients (Group I: 75.5%) remained uncontrolled (uncontrolled tTRH) whereas 69 patients (Group II: 24.5%) were able to reach an optimal BP control (defined as an average BP inferior to 140/90 mmHg in >50% of the follow-up visits). During this second follow-up 72 ADRs were recorded (Table 3), with an occurrence rate of 25.5%, which was statistically lower as compared to the percentage recorded in the first follow-up (Figure 1) despite thefact that there was no statistically significant reduction in the mean daily number of antihypertensive drugs and in the percentage of use of the main classes of antihypertensive medications (Table 4).
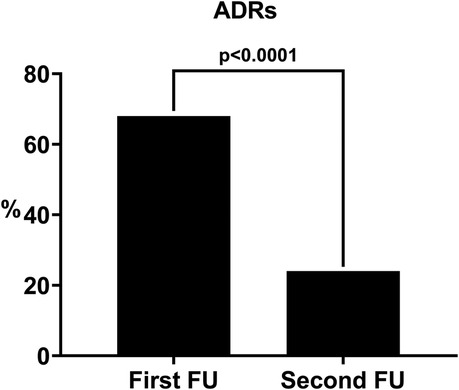
Figure 1. Percentage of patients with ADRs before (first FU) and after (second FU) the therapeutic concordance approach. FU: follow-up.
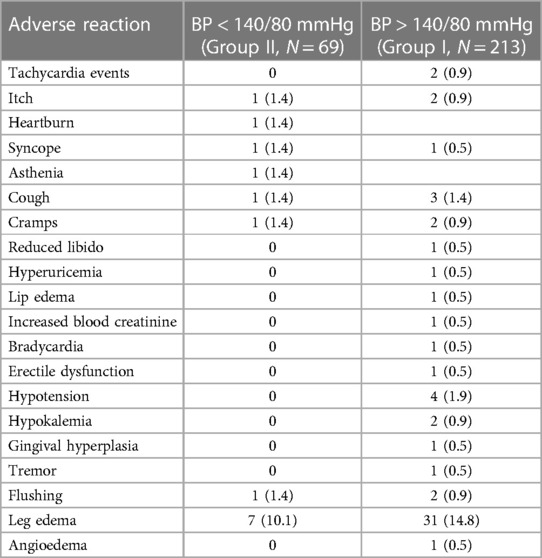
Table 3. Type of adverse reactions recorded during the follow-up period after therapeutic concordance approach. The population has been divided in subgroups according to the BP response during the second follow-up period (Group 1 without, Group II with optimal BP control). Data are expressed as number (%).
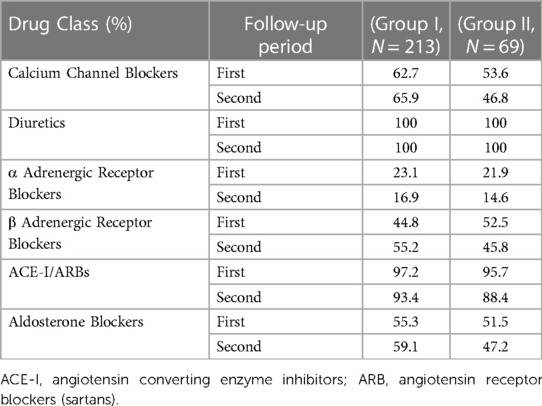
Table 4. Antihypertensive drugs used before (first follow-up period) and after (second follow-up period) the application of the therapeutic concordance approach. The population has been divided in subgroups according to the BP response during the second follow-up period (Group I without optimal BP control, Group II with optimal BP control). Statistical analysis was performed comparing the percentage of each class of drug used in the two follow-up periods in the same group of patients, and no significant differences were observed (all p values were >0.05).
A statistically significant difference in the rate of occurrence of ADRs was detected between males and females (rate of ADR occurrence 20.5% vs. 30.3%, respectively, p = 0.037), such a difference was not seen in the first follow-up (females 73%, males 65.8%. n.s.). Further, we divided the patients into four age quartiles (<47.7 years; 47.8–55.1 years; 55.2–61.9 years; >70 years) and we observed that ADRs due to antihypertensive treatments were more common in third age quartile: ADRs in this age group were 26 (37.5%). Individuals who developed ADRs in the other age groups were 11 (15.7%), 19 (26.8%), and 16 (22.5%) in the first, second, and fourth quartiles, respectively (p for trend < 0.05). On the contrary, during the first follow-up period we did not detect any significant difference in the rate of ADRs occurrence between the four age groups: 46 (65,7%), 54 (76,0%), 53 73,6%) and 41 (57,7%), respectively from the first to the fourth quartile).
According to the Liverpool scale, 3 (4.1%) ADRs recorded during the second follow-up were “Unlikely”, 16 (22.2%) “Possible”, 10 (13.9%) “Probable”, and 43 (59,7%) were “Definite”, a distribution which was not different from that observed during the first follow-up when 18 (9.3%) were “Unlikely”, 50 (25,8%) “Possible”, 34 (17.5%) “Probable” and 92 (47.4%) “Definite” (Figure 2).
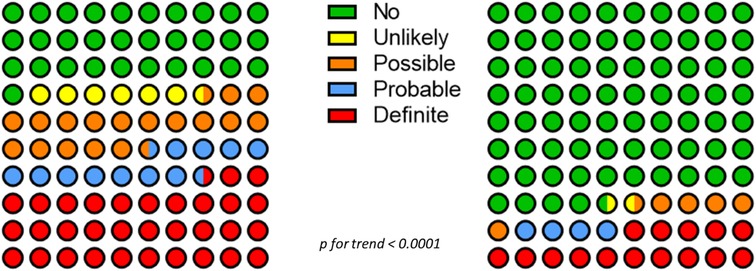
Figure 2. Distribution of ADRs before (first follow-up, right panel) and after (second follow-up, left panel) therapeutic concordance according to the Liverpool algorithm.
During both follow-up periods no serious ADRs were recorded. Of the 282 patients who successfully completed the second follow-up study, 69 obtained a satisfactory BP control with 2.9 + 1.0 antihypertensive drugs/day, 27 (9.57%) reached BP control with <3 antihypertensive drugs (including a full dose diuretic), while 42 (14.9%) patients required more than 3 antihypertensive drugs and were thereby considered patients with difficult-to-control tTRH. The remaining 212 patients (75.5%) were tTRH since they failed to obtain a satisfactory BP control despite a greater daily number of antihypertensive drugs 4.25 + 1.0 (p < 0.01 vs. 2.9 + 1.04).
However, no significant difference in ADR occurrence rate was detected between Group I (n = 210) and Group II (n = 69) (25.8% vs. 20.3%, p < 0.353), notwithstanding the lower number of antihypertensive drugs in Group II.
In the present study we investigated whether an evaluation of the pharmacological history of the patient and a more empathetic approach that actively involves the patient in the choice of her/his antihypertensive treatment could improve the tolerability of the antihypertensive therapy.
Our findings indicate a significant reduction in the rate of occurrence of ADRs, which in about 25% of the population of patients defined as tTHR hypertensives is associated with an improved BP control, so that they were no longer defined as resistant to the treatment or at least became difficult to control hypertensives, who required more than three drugs to achieve a good BP control. Howbeit, a comparable reduction in the rate of ADR occurrence was recorded in the remaining 3/4 of our population who failed to obtain any improvement in BP control, so it seems likely that the reduction in ADR occurrence improves BP control but not vice versa.
Although physician-related barriers for concordance have been considerably minimized by the introduction of clearer guidelines, physicians may not be sufficiently insistent in the management of hypertension, especially in older adults (44–49). In this regard, it is important to emphasize that most of the side effects declared by the patients have no relationship with antihypertensive drugs, while other adverse effects, including reduced libido and hypokalemia have a reduced incidence as compared to the one expected, probably on account of a correct use of drug combination.
Since all patients received more than one single drug, our findings do not consent speculations on the tolerability of single antihypertensive drugs, albeit some ADRs are considered specific for one class of drugs, such as leg edema for calcium channel blockers (50). Finally, although we did not measure adherence and persistence of the prescribed treatment, the finding that a reduction in ADRs is accompanied by an improvement in BP control allows the speculation that the presence of ADRs may impair these two parameters. Nevertheless, since no difference in ADR rate occurrence could be detected between patients with and without a satisfactory BP control, ADRs cannot be considered the only responsible of unsatisfactory BP control by reducing the adherence to the antihypertensive regimen, at least when the pharmacologic prescription has taken into account possible drug to drug interactions and has been agreed with the patient, as in the concordance protocol. The usefulness of this global approach is further demonstrated by the observation that in a population requiring a large number of antihypertensive drugs we have observed a very low rate of ADR occurrence so that we have been able to detect some characteristics of ADR occurrence, such as the higher rate of ADRs in females and in subjects ageing 55–62 years, which seem to be peculiar of antihypertensive monotherapy.
The major limitation of our study is that it has not been planned and performed according to a double-blind placebo-controlled protocol. Notwithstanding, the use of two very long follow-up periods and the choice to perform the study in patients with tTRH may allow to overcome this limitation. Furthermore the availability of two very long follow-up periods, each lasting more than 6 years, and the choice to perform the study in patients with tTRH minimize the role of other factors, such as changes in BMI or in physical activity as well progressive familiarization of patients with the staff, in the improvement of antihypertensive treatment tolerability.
In summary, our data indicate that the therapeutic concordance approach is able to significantly reduce the occurrence of ADRs in tTRH patients. Our findings support a thorough rearrangement of current health care systems in order to emulate rigorous management strategies used in clinical trials proven to provide better BP control rates than traditional approaches.
The raw data supporting the conclusions of this article will be made available by the first authors, upon reasonable request, without undue reservation.
The studies involving human participants were reviewed and approved by Federico II University Hospital. The patients/participants provided their written informed consent to participate in this study.
VT: had full access to the raw data in this clinical study and takes full responsibility for the integrity and accuracy of the data. Study conceptualization and design: VT, RI, GS, and BT. Acquisition and interpretation of data: MM, RI, PM, ML, DP, AF, PG, and GS. Writing: VT, MM, and GS. Editing: CM, GS, and BT. Statistical analysis: VT, MM, RI, and DP. Technical support: PM, AF, GE, and PG. Study supervision: VT and GS. All authors contributed to the article and approved the submitted version.
The Santulli's Lab is supported in part by the National Institutes of Health (NIH): National Heart, Lung, and Blood Institute (NHLBI: R01-HL164772, R01-HL159062, R01-HL146691, T32-HL144456), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK: R01-DK123259, R01-DK033823), National Center for Advancing Translational Sciences (NCATS: UL1-TR002556-06, UM1-TR004400) to GS, by the Diabetes Action Research and Education Foundation (to GS), and by the Monique Weill-Caulier and Irma T. Hirschl Trusts (to GS). This study was also supported by Grant 00014Prin_2017 ID43237 to VT.
The authors thank X. Wang for the valuable support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ADRs, adverse drug reactions; BP, blood pressure; CSN, campania salute network; HBP, home blood pressure; OBP, office blood pressure; TRH, therapy-resistant hypertension.
1. Parati G, Goncalves A, Soergel D, Bruno RM, Caiani EG, Gerdts E, et al. New perspectives for hypertension management: progress in methodological and technological developments. Eur J Prev Cardiol. (2023) 30:48–60. doi: 10.1093/eurjpc/zwac203
2. Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health. (2018) 6:e1196–252. doi: 10.1016/S2214-109X(18)30386-3
3. Batarseh FA, Ghassib I, Chong DS, Su PH. Preventive healthcare policies in the US: solutions for disease management using big data analytics. J Big Data. (2020) 7:38. doi: 10.1186/s40537-020-00315-8
4. April-Sanders AK, Golestaneh L, Zhang L, Swett K, Meissner P, Rodriguez CJ. Hypertension treatment and control in a New York city health care system. J Am Heart Assoc. (2022) 11:e026077. doi: 10.1161/JAHA.122.026077
5. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. (2020) 76:2982–3021. doi: 10.1016/j.jacc.2020.11.010
6. Campos CL, Rodriguez CJ. High blood pressure in hispanics in the United States: a review. Curr Opin Cardiol. (2019) 34:350–8. doi: 10.1097/HCO.0000000000000636
7. Cushman WC, Ringer RJ, Rodriguez CJ, Evans GW, Bates JT, Cutler JA, et al. Blood pressure intervention and control in SPRINT. Hypertension. (2022) 79:2071–80. doi: 10.1161/HYPERTENSIONAHA.121.17233
8. Parati G, Lombardi C, Pengo M, Bilo G, Ochoa JE. Current challenges for hypertension management: from better hypertension diagnosis to improved patients’ adherence and blood pressure control. Int J Cardiol. (2021) 331:262–9. doi: 10.1016/j.ijcard.2021.01.070
9. Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, et al. Trial of intensive blood-pressure control in older patients with hypertension. N Engl J Med. (2021) 385:1268–79. doi: 10.1056/NEJMoa2111437
10. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. International society of hypertension global hypertension practice guidelines. Hypertension. (2020) 75:1334–57. doi: 10.1161/HYPERTENSIONAHA.120.15026
11. Liu X, Byrd JB, Rodriguez CJ. Use of physician-recommended non-pharmacological strategies for hypertension control among hypertensive patients. J Clin Hypertens. (2018) 20:518–27. doi: 10.1111/jch.13203
12. Kitt J, Fox R, Tucker KL, McManus RJ. New approaches in hypertension management: a review of current and developing technologies and their potential impact on hypertension care. Curr Hypertens Rep. (2019) 21:44. doi: 10.1007/s11906-019-0949-4
13. Braun SE, Kinser PA, Rybarczyk B. Can mindfulness in health care professionals improve patient care? An integrative review and proposed model. Transl Behav Med. (2019) 9:187–201. doi: 10.1093/tbm/iby059
14. Jackson AM, Jhund PS, Anand IS, Dungen HD, Lam CSP, Lefkowitz MP, et al. Sacubitril-valsartan as a treatment for apparent resistant hypertension in patients with heart failure and preserved ejection fraction. Eur Heart J. (2021) 42:3741–52. doi: 10.1093/eurheartj/ehab499
15. Dimeo F, Pagonas N, Seibert F, Arndt R, Zidek W, Westhoff TH. Aerobic exercise reduces blood pressure in resistant hypertension. Hypertension. (2012) 60:653–8. doi: 10.1161/HYPERTENSIONAHA.112.197780
16. Trimarco V, Izzo R, Mone P, Lembo M, Manzi MV, Pacella D, et al. Therapeutic concordance improves blood pressure control in patients with resistant hypertension. Pharmacol Res. (2023) 187:106557. doi: 10.1016/j.phrs.2022.106557
17. Tedla YG, Bautista LE. Drug side effect symptoms and adherence to antihypertensive medication. Am J Hypertens. (2016) 29:772–9. doi: 10.1093/ajh/hpv185
18. Lowry KP, Dudley TK, Oddone EZ, Bosworth HB. Intentional and unintentional nonadherence to antihypertensive medication. Ann Pharmacother. (2005) 39:1198–203. doi: 10.1345/aph.1E594
19. Jowett S, Kodabuckus S, Ford GA, Hobbs FDR, Lown M, Mant J, et al. Cost-effectiveness of antihypertensive deprescribing in primary care: a markov modelling study using data from the OPTiMISE trial. Hypertension. (2022) 79:1122–31. doi: 10.1161/HYPERTENSIONAHA.121.18726
20. Kostis WJ, Cabrera J. Fear of adverse events should not prevent the use of appropriate antihypertensive drug therapy. J Am Soc Hypertens. (2018) 12:756–8. doi: 10.1016/j.jash.2018.09.002
21. Kulkarni S, Rao R, Goodman JDH, Connolly K, O'Shaughnessy KM. Nonadherence to antihypertensive medications amongst patients with uncontrolled hypertension: a retrospective study. Medicine. (2021) 100:e24654. doi: 10.1097/MD.0000000000024654
22. Trimarco V, de Simone G, Izzo R, De Luca N, Giudice R, Marino M, et al. Persistence and adherence to antihypertensive treatment in relation to initial prescription: diuretics versus other classes of antihypertensive drugs. J Hypertens. (2012) 30:1225–32. doi: 10.1097/HJH.0b013e328353398b
23. Gebreyohannes EA, Bhagavathula AS, Abebe TB, Tefera YG, Abegaz TM. Adverse effects and non-adherence to antihypertensive medications in university of Gondar comprehensive specialized hospital. Clin Hypertens. (2019) 25:1. doi: 10.1186/s40885-018-0104-6
24. Morimoto T, Gandhi TK, Fiskio JM, Seger AC, So JW, Cook EF, et al. An evaluation of risk factors for adverse drug events associated with angiotensin-converting enzyme inhibitors. J Eval Clin Pract. (2004) 10:499–509. doi: 10.1111/j.1365-2753.2003.00484.x
25. Black HR, Graff A, Shute D, Stoltz R, Ruff D, Levine J, et al. Valsartan, a new angiotensin II antagonist for the treatment of essential hypertension: efficacy, tolerability and safety compared to an angiotensin-converting enzyme inhibitor, lisinopril. J Hum Hypertens. (1997) 11:483–9. doi: 10.1038/sj.jhh.1000482
26. Curb JD, Borhani NO, Blaszkowski TP, Zimbaldi N, Fotiu S, Williams W. Long-term surveillance for adverse effects of antihypertensive drugs. JAMA. (1985) 253:3263–8. doi: 10.1001/jama.1985.03350460063022
27. Fletcher AE, Bulpitt CJ, Chase DM, Collins WC, Furberg CD, Goggin TK, et al. Quality of life with three antihypertensive treatments. Cilazapril, atenolol, nifedipine. Hypertension. (1992) 19:499–507. doi: 10.1161/01.HYP.19.6.499
28. Israili ZH, Hall WD. Cough and angioneurotic edema associated with angiotensin-converting enzyme inhibitor therapy. A review of the literature and pathophysiology. Ann Intern Med. (1992) 117:234–42. doi: 10.7326/0003-4819-117-3-234
29. Saunders E, Weir MR, Kong BW, Hollifield J, Gray J, Vertes V, et al. A comparison of the efficacy and safety of a beta-blocker, a calcium channel blocker, and a converting enzyme inhibitor in hypertensive blacks. Arch Intern Med. (1990) 150:1707–13. doi: 10.1001/archinte.1990.00040031707020
30. From compliance to concordance: Achieving shared goals in medicine taking. London: Royal Pharmaceutical Society of Great Britain (1997).
31. Settineri S, Frisone F, Merlo EM, Geraci D, Martino G. Compliance, adherence, concordance, empowerment, and self-management: five words to manifest a relational maladjustment in diabetes. J Multidiscip Healthc. (2019) 12:299–314. doi: 10.2147/JMDH.S193752
32. Aronson JK. Compliance, concordance, adherence. Br J Clin Pharmacol. (2007) 63:383–4. doi: 10.1111/j.1365-2125.2007.02893.x
33. Jeong SM, Kim S, Wook Shin D, Han K, Hyun Park S, Hyuk Kim S, et al. Persistence and adherence to antihypertensive drugs in newly treated hypertensive patients according to initial prescription. Eur J Prev Cardiol. (2021) 28:e1–4. doi: 10.1177/2047487319900326
34. Trimarco V, Izzo R, Morisco C, Mone P, Virginia Manzi M, Falco A, et al. High HDL (high-density lipoprotein) cholesterol increases cardiovascular risk in hypertensive patients. Hypertension. (2022) 79:2355–63. doi: 10.1161/HYPERTENSIONAHA.122.19912
35. Manzi MV, Mancusi C, Lembo M, Esposito G, Rao MAE, de Simone G, et al. Low mechano-energetic efficiency is associated with future left ventricular systolic dysfunction in hypertensives. ESC Heart Fail. (2022) 9:2291–300. doi: 10.1002/ehf2.13908
36. Ciccarelli M, Finelli R, Rivera N, Santulli G, Izzo R, De Luca N, et al. The possible role of chromosome X variability in hypertensive familiarity. J Hum Hypertens. (2017) 31:37–42. doi: 10.1038/jhh.2016.9
37. Mancusi C, Manzi MV, de Simone G, Morisco C, Lembo M, Pilato E, et al. Carotid atherosclerosis predicts blood pressure control in patients with hypertension: the campania salute network registry. J Am Heart Assoc. (2022) 11:e022345. doi: 10.1161/JAHA.121.022345
38. Judd E, Calhoun DA. Apparent and true resistant hypertension: definition, prevalence and outcomes. J Hum Hypertens. (2014) 28:463–8. doi: 10.1038/jhh.2013.140
39. Wang Q, Wang Y, Wang J, Zhang L, Zhao MH. Chinese cohort study of chronic kidney D. White-coat hypertension and incident end-stage renal disease in patients with non-dialysis chronic kidney disease: results from the C-STRIDE study. J Transl Med. (2020) 18:238. doi: 10.1186/s12967-020-02413-w
40. Gallagher RM, Kirkham JJ, Mason JR, Bird KA, Williamson PR, Nunn AJ, et al. Development and inter-rater reliability of the liverpool adverse drug reaction causality assessment tool. PLoS One. (2011) 6:e28096. doi: 10.1371/journal.pone.0028096
41. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of cardiology and the European society of hypertension: the task force for the management of arterial hypertension of the European society of cardiology and the European society of hypertension. J Hypertens. (2018) 2018(36):1953–2041. doi: 10.1097/HJH.0000000000001940
42. Mone P, Varzideh F, Jankauskas SS, Pansini A, Lombardi A, Frullone S, et al. SGLT2 inhibition via empagliflozin improves endothelial function and reduces mitochondrial oxidative stress: insights from frail hypertensive and diabetic patients. Hypertension. (2022) 79(8):1633–43. doi: 10.1161/HYPERTENSIONAHA.122.19586
43. Wilson S, Mone P, Jankauskas SS, Gambardella J, Santulli G. Chronic kidney disease: definition, updated epidemiology, staging, and mechanisms of increased cardiovascular risk. J Clin Hypertens. (2021) 23:831–4. doi: 10.1111/jch.14186
44. Bowling CB, Lee A, Williamson JD. Blood pressure control among older adults with hypertension: narrative review and Introduction of a framework for improving care. Am J Hypertens. (2021) 34:258–66. doi: 10.1093/ajh/hpab002
45. Bilen O, Wenger NK. Hypertension management in older adults. F1000Res. (2020) 9:F1000 Faculty Rev-1003. doi: 10.12688/f1000research.20323.1
46. Pansini A, Lombardi A, Morgante M, Frullone S, Marro A, Rizzo M, et al. Hyperglycemia and physical impairment in frail hypertensive older adults. Front Endocrinol. (2022) 13:831556. doi: 10.3389/fendo.2022.831556
47. Feldman R, Bacher M, Campbell N, Drover A, Chockalingam A. Adherence to pharmacologic management of hypertension. Can J Public Health. (1998) 89:I16–8. doi: 10.1007/BF03404494
48. Brown MJ, Cruickshank JK, Dominiczak AF, MacGregor GA, Poulter NR, Russell GI, et al. Better blood pressure control: how to combine drugs. J Hum Hypertens. (2003) 17:81–6. doi: 10.1038/sj.jhh.1001511
49. Sinnott SJ, Tomlinson LA, Root AA, Mathur R, Mansfield KE, Smeeth L, et al. Comparative effectiveness of fourth-line anti-hypertensive agents in resistant hypertension: a systematic review and meta-analysis. Eur J Prev Cardiol. (2017) 24:228–38. doi: 10.1177/2047487316675194
50. Galappatthy P, Waniganayake YC, Sabeer MI, Wijethunga TJ, Galappatthy GK, Ekanayaka RA. Leg edema with (S)-amlodipine vs conventional amlodipine given in triple therapy for hypertension: a randomized double blind controlled clinical trial. BMC Cardiovasc Disord. (2016) 16:168. doi: 10.1186/s12872-016-0350-z
Keywords: adherence, adverse drug reactions, blood pressure, compliance, concordance, hypertension, pharmacologic resistance, resistant hypertension
Citation: Trimarco V, Manzi MV, Izzo R, Mone P, Lembo M, Pacella D, Esposito G, Falco A, Morisco C, Gallo P, Santulli G and Trimarco B (2023) The therapeutic concordance approach reduces adverse drug reactions in patients with resistant hypertension. Front. Cardiovasc. Med. 10:1137706. doi: 10.3389/fcvm.2023.1137706
Received: 4 January 2023; Accepted: 11 April 2023;
Published: 5 May 2023.
Edited by:
Elise Peery Gomez-Sanchez, University of Mississippi Medical Center, UnitedStatesReviewed by:
Luis Miguel Ruilope, University Hospital October 12, Spain© 2023 Trimarco, Manzi, Izzo, Mone, Lembo, Pacella, Esposito, Falco, Morisco, Gallo, Santulli and Trimarco. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gaetano Santulli Z3NhbnR1bGxpMDAxQGdtYWlsLmNvbQ==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.