- Department of Vascular Surgery, Beijing Jishuitan Hospital, Beijing, China
Background: The permanent placement of inferior vena cava (IVC) filters may lead to numerous complications and their removal is recommended once the risk of pulmonary embolism is reduced. Removal of IVC filters by endovenous means is preferred. But failure of endovenous removal happens when recycling hooks penetrate the vein wall and filters are left in place for too long time. In these scenarios, open surgery may be effective for removal of IVC filters. We aimed to describe the surgical approach, outcomes, and 6-month follow-up of the removal of IVC filter by open surgery, after the failure of removal via the endovenous method.
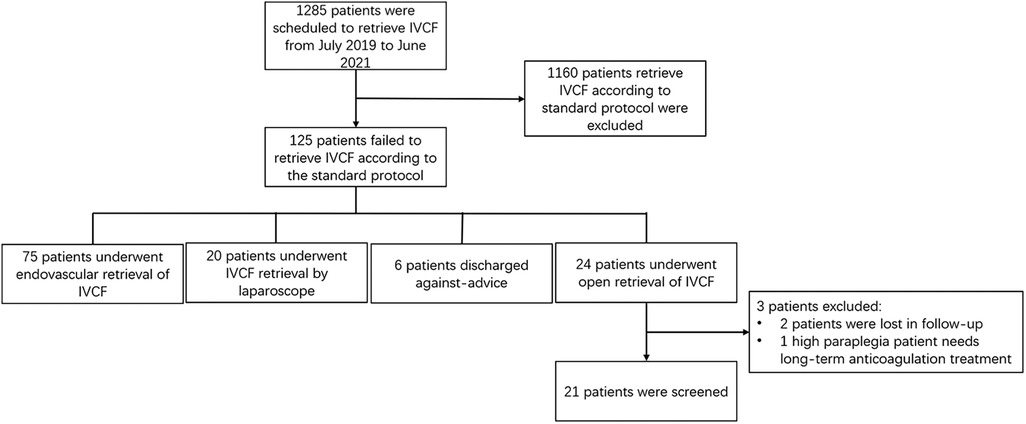
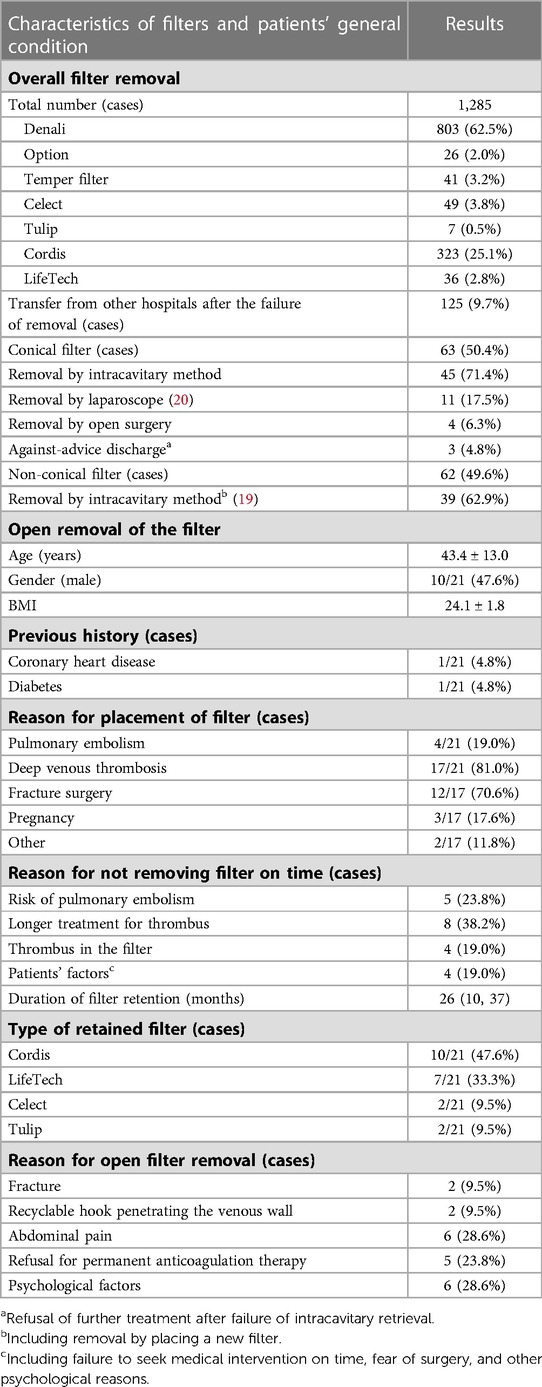
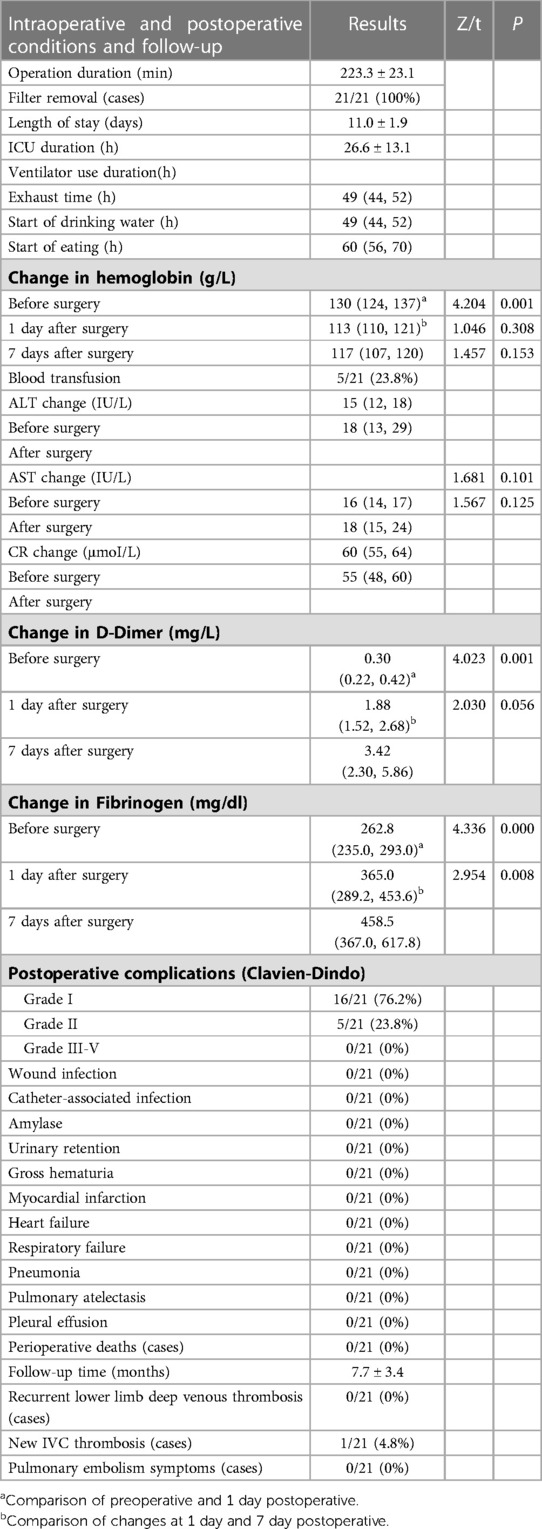
Methods: A total of 1,285 patients with retrievable IVC filters were admitted from July 2019 to June 2021, including 1,176 (91.5%) endovenous filter removals, and 24 (1.9%) open surgical IVC filter removals after the failure by endovenous method, of whom 21 (1.6%) were followed-up and eligible for analysis of the study. Patient characteristics, filter type, filter removal rate, IVC patency rate, and complications were retrospectively analyzed.
Results: Twenty-one patients were left with IVC filters for 26 (10, 37) months, of which 17 (81.0%) patients had non-conical filters and 4 (19.0%) had conical filters; all 21 filters were successfully removed, with a 100% removal rate, no deaths, no serious complications, and no symptomatic pulmonary embolism. At the 3rd month follow-up after surgery and 3rd month follow-up after discontinuation of anticoagulation therapy, only 1 case (4.8%) had IVC occlusion, but without any occurrence of new lower limb deep venous thrombosis and silent pulmonary embolism.
Conclusion: Open surgery can be used for the removal of IVC filters after failure of removal by endovenous method or when accompanied by complications without symptoms of pulmonary embolism. Open surgical approach can be used as an adjunctive clinical intervention for the removal of such filters.
Background
Lower limb deep venous thrombosis (DVT) is a common condition, requiring prompt treatment, and the dislodged thrombus may lead to a pulmonary embolism that is a life-threatening condition (1–3). It has an incidence of approximately 1–2/1,000 people (4–6). Currently, inferior vena cava (IVC) filters are used clinically to prevent fatal pulmonary embolism during the perioperative period (7–9). Indications for vena cava filter placement in the Chinese guidelines (10) are floating thrombus in the iliac, femoral or inferior vena cava, acute DVT that needs thrombectomies such as catheter-directed thrombolysis (CDT), pharmacomechanical thrombectomy (PMT), or surgical thrombectomy, and abdominal, pelvic, or lower limb surgery with high-risk factors for acute DVT and pulmonary embolism (PE). Permanent placement of IVC filters, however, may lead to numerous complications (11–13), and therefore, it is recommended (8, 9, 14, 15) that retrievable vena cava filters can be placed perioperatively and removed when the risk of pulmonary embolism is reduced.
Most IVC filters are removed by endovenous method, but hooks in recycling conical filters penetrate the vein wall, resulting in failure of endovenous retrieval of the filter; non-conical filters cause rapid endothelial proliferation and increased difficulty of endovenous retrieval after retention for more than 14 days (16–18), however forced retrieval of the filter may damage the IVC. The filter required been retained for a prolonged period in cases of pulmonary embolism risk, IVC embolism, or floating thrombus in the proximal iliac femoral vein (19). Failure to undergo medical intervention on time or other unknown factors may also increase the filter retention time and increase the risk of filter removal.
IVC filters after failure of removal by endovenous means may be removed by open surgery. This retrospective study aimed to describe the surgical approach, outcome, and experience with the removal of IVC filter by open surgery after failure of removal using the endovenous method.
Methods
General information
We retrospectively analyzed 24 (1.9%) filter retrieval cases by open surgery from July 2019 to June 2021, 21 cases (1.6%) were completed successfully,3 patients were excluded, 2 patients were lost in follow-up after surgery,1 case with high paraplegia from thoracic spine trauma, discontinuation of anticoagulation therapy due to high risk of thrombosis recurrence, all above patients received filter implantation in other medical centers (Table 1 and Figure 1).
Three patients discontinued anticoagulation therapy after 3 months, 8 cases took rivaroxaban 20 mg QD for anticoagulation, and 10 cases took rivaroxaban 10 mg QD for anticoagulation. The study was approved by the Ethics committee of Beijing Jishuitan Hospital (No.JST202201–21).
Removal of filters by open surgery is not a routine procedure and is mostly used in patients with a broken or displaced filter, or with abdominal pain and after the failure of endovenous removal. Selection criteria were as follows: patients aged <70 years, with no contraindications to anticoagulants, and no serious cardiopulmonary disease that would prevent the procedure; IVC is patent at least in unilateral iliac veins, with no thrombus or retaining a small amount of old thrombus in the lower limb veins and IVC, above situations can be considered as low risk of pulmonary embolism after removal of the filter; failure to retrieve the conical filter by endovenous method because of severe tilt or CT scan showing the penetration of filter hook into the IVC wall; patients did not accept permanent placement of a filter or had a strong desire for filter retrieval or accept of filter retrieval by open surgery.
Treatment
Preoperative examinations and symptom observation: Ultrasonography of lower limb veins and IVC was performed to observe the patency of IVC, patency of bilateral iliac veins or at least unilateral iliac veins, absence of thrombus in both lower limb veins or presence of old thrombus, and the risk of thrombus dislodgement. Enhanced CT imaging of the abdomen was performed to observe the patency of IVC, the condition of the filter (broken or not), the penetration of retrievable hook into the vascular wall (21), and the presence of symptoms of pulmonary embolism. The signs of pulmonary embolism were also observed.
Intraoperative manipulation: The surgical operation was performed by a physician with a senior title in vascular surgery. Under general anesthesia, a longitudinal incision was made on the right rectus abdominis; the hepatocolic ligament was severed via the lateral right paracolic sulcus; the right hemi-colon was lifted to the retroperitoneum; the proximal and distal ends of the IVC were freed; the lumbar vein was separated and ligated (special attention was paid to the lumbar vein in the posterior wall of the IVC) to avoid damage to the duodenum, iliac vein, and right ureter; surrounding tissues were protected to minimize damage when separating the retrievable hooks or foot supports of the penetrated filters.
The following two methods were chosen depending on the types of filters: a) Non-conical and Tulip filters: The IVC was blocked after systemic heparinization; the filters were separated by longitudinal dissection of the anterior wall of the IVC; the endothelium of the IVC was repaired and IVC was then sutured (Figures 2, 3A-D). b) For conical filters other than Tulip filters: The penetrated venous wall by the retrievable filter hooks was preplaced with purse-string suture; The filter can be easily removed or with the aid of a 10F arterial sheath tube after incision of the inferior vena cava along the retrieval filter hook, followed by a purse-string ligation to stop bleeding (22) (Figures 3E-F).
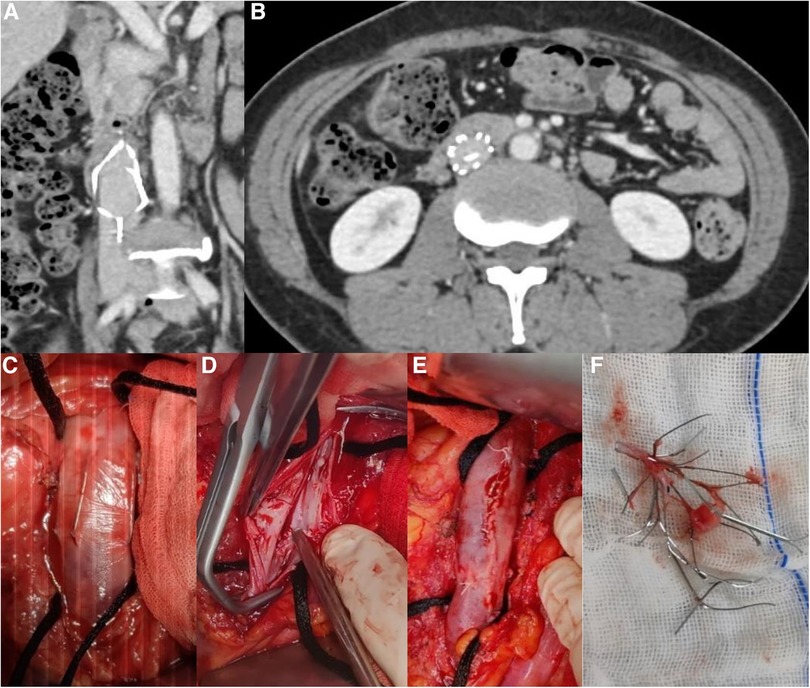
Figure 2. (A) Retention of non-conical filter for 8 years (B) Filter fracture (C) Filter penetrating the IVC (D) Post-repair image of IVC endothelium after filter removal (E) Suture of the IVC (F) Removed filter after disassembly.
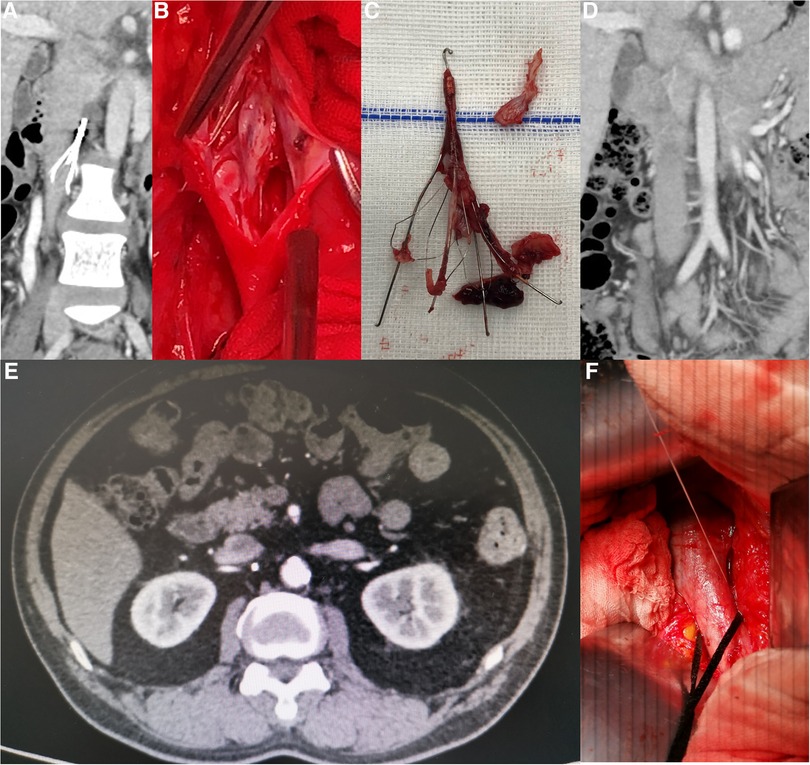
Figure 3. (A) Retention of Tulip filter for 16 months. (B) Tulip filter with obvious endothelial hyperplasia and failed endovenous removal. (C) Complete removal of Tulip filter with severe endothelial hyperplasia. (D) Follow-up of Tulip filter removal at 6 months after surgery with patent IVC. (E) CT image of the Celect filter showing the retrievable hook penetrating the IVC. (F) Intraoperative retrievable hook penetrating the venous wall with a preplaced purse-string suture.
Postoperative treatment: Low molecular weight heparin at the dose of 100 IU/Kg Q12h was administered for anticoagulation. Patients were discharged with the prescription for oral administration of rivaroxaban at a dose of 20 mg QD for anticoagulation (23), with plasma D-dimer monitoring at 1-month intervals.
At 3rd month postoperative follow-up (September 2019 to September 2021), venous ultrasound of both lower limbs was performed to observe the thrombotic changes in the limbs and enhanced CT of the abdomen was performed to observe patency of the IVC. The symptoms of pulmonary embolism were monitored. After discontinuing anticoagulation therapy for 3 months (December 2019 to December 2021), an ultrasound examination of both lower limbs and IVC was performed to observe the patency of IVC and thrombotic changes in the limbs.
Statistical analysis
SPSS version 21.0 software was used for statistical analysis. The measurement data were expressed as mean ± standard deviation, the count data were described as percentages, and the non-normally distributed measurement data were expressed as median (M) (P25, P75); the Wilcoxon rank-sum test was used for comparison between the groups, and the difference was considered statistically significant when P-value was <0.05.
Results
IVC filters
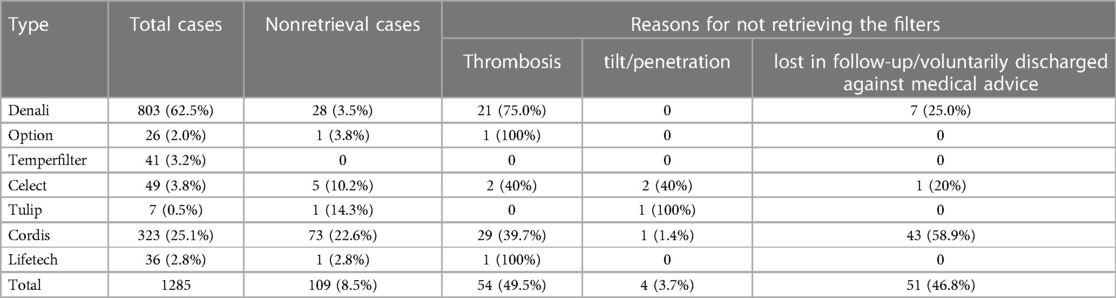
A total of 1,285 patients were admitted for retrieval of retrievable filters, of which 926 (72.1%) patients had conical filters, including 871 (94.1%) cases of endovascular retrieval, and 359 (27.9%) had non-conical filters, including 305 (85.0%) cases of endovascular retrieval. The overall retrieval rate was 91.5% (1,176/1,285) by endovascular method (Table 2).
125 patients (9.7%) were transferred to our hospital after the failure of endovascular retrieval of IVC filters, 24 (1.9%) patients underwent filter retrieval by open surgery, and 21 (1.6%) cases completed the surgery and follow-up. Of the 21 IVC filters left for 26 (10, 37) months (Table 3), 17 (81.0%) were non-conical, 2 (9.5%) of them displayed fractures on CT images (Figures 2C, 4B), did not penetrate the venous wall, and there was no hematoma around the IVC (Figure 2A); of the remaining 16 patients with non-conical filters, 10 had unsuccessful removal by endovenous attempts in other hospitals within two weeks of admission to our hospital and refused further removal by endovenous method, 6 were removed with complications by attempts in our hospital, 3 were removed with abdominal pain, and 3 were removed by double wire lassoing techniques. Four (19.0%) conical filters (Tulip, 2; Celect, 2) did not show a fracture, and removal attempts were made using the loop technique, modified loop technique, and assisted balloon dilation technique, but these techniques were unsuccessful for Celect filters and CT image showed the penetration of retrievable hooks into the IVC (Figures 2A,E). retrievable hooks were captured in Tulip filters, which were not successfully removed due to severe abdominal pain, and removal by endovenous means was abandoned.
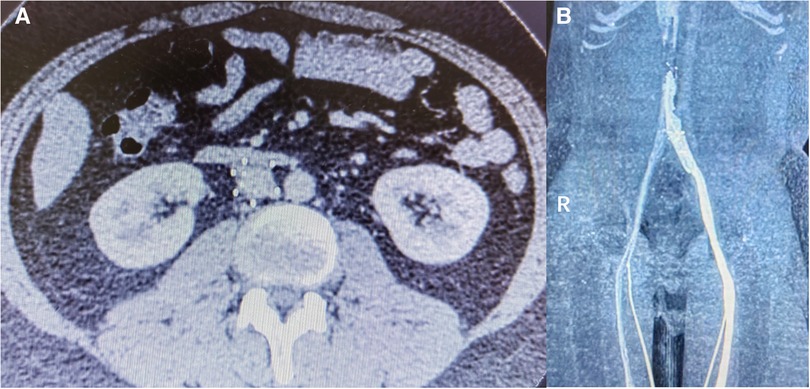
Figure 4. (A) Retention of non-conical filter for 6 years, fractured. (B) IVC occlusion in the follow-up at 3 months after surgery.
Surgical procedure
Open surgery was performed to remove the IVC filters within 1–2 weeks of the failure of removal by the endovenous method. Twenty-one filters were successfully removed with a 100% removal rate (Table 3), no perioperative deaths, and no symptomatic pulmonary embolism. The wound healed well after surgery without serious complications (Table 3). Hemoglobin content comparisons before surgery and 1 day and 7 days after surgery were as follows: 130 (124, 137), 113 (110, 121) and 117 (107, 120) g/l; for the comparison before surgery and 1 day and after surgery, Z = 4.204 and P = 0.0001; for the comparison at 1 day and 7 days after surgery, Z = 1.046 and P = 0.308. Comparison of biochemical indicators before surgery and 3 days after surgery were as follows: glutamic-pyruvic transaminase, 15 (12, 18) and 18 (13, 29) and µmol/l, Z = 1.457, P = 0.153; glutamic oxalocetic transaminase, 16 (14, 17) and 18 (15, 24) µmol/L, Z = 1.681, and P = 0.101; creatinine, 60 (55, 64) and 55 (48, 60) μmoI/L, Z = 1.567, and P = 0.125. This indicated that there was a small amount of bleeding during the filter removal by open surgery technique and after carefully applying hemostasis, no further blood was lost and liver or renal function was not affected after surgery.
Postoperative follow-up
Ultrasonography of the lower limbs and CT imaging of the IVC were performed 3 months after continuous anticoagulation therapy. Twenty-one cases showed no new acute lower limb deep venous thrombosis, 20 cases had patent IVC (Figure 3D) and 1 case (4.8%) had IVC occlusion (Figure 4B).
Anticoagulation therapy was discontinued in 20 cases, except for the case with IVC occlusion. On the reexamination 3 months after discontinuation of anticoagulation treatment, the IVC was patent, there was no new acute lower limb deep venous thrombosis, and no symptomatic pulmonary embolism occurred. Oral administration of rivaroxaban at a dose of 20 mg QD was continued for anticoagulation in the case with IVC occlusion. No complications due to anticoagulation therapy occurred in all patients.
Discussion
Sequelae of permanent filter placement may lead to complications and cause a serious physical and psychological impact on patients and their families (16, 24) who have strong desire to have the filters to be removed, in China. Complications of long-term filter retention are vena cava perforation, movement of filter support adjacent to or penetrating into surrounding organs, and filter fracture with symptoms due to fracture-associated risk (25–28).
Results and implications
Due to the complications associated with long-term retention of filters, our center attaches great importance to the retrieval of filters. The overall filter retrieval rate in our study was 91.5%, and the reasons for failure to retrieve filters were 54 (49.5%) The reasons for failure to retrieve the filter were as follows: inferior vena cava thrombosis or intra-filter thrombosis in 54 (49.5%) cases, missed visits or automatic discharge in 51 (46.8%) cases, and severe tilting of the filter inducing the hook against the wall in 4 (3.7%) cases, mainly due to thrombosis and missed visits.
One of the main risks of filter removal by open surgery is hemorrhage, mainly occurring in lumbar and iliac veins, due to a large number of tributaries from IVC. The lumbar veins at the anterior and lateral walls of the IVC are easy to find, but those at the posterior wall of the IVC are difficult to separate and can be easily damaged. The injury to the lumbar veins may be reduced by ligating the tissue near the posterior wall of the IVC in stages during surgery. Blocking the IVC immediately distal to the filter is the main method of reducing hemorrhage from the iliac vein tributaries, and preoperative CT imaging assessment is important.
The IVC is located posterior to the peritoneum and another risk of open surgery is that it interferes with the intestinal function. The surgery was performed via the lateral right hemi-colon to the retroperitoneum without disrupting the mesenteric and intraperitoneal vessels, thus reducing the impact on the blood supply to the gastrointestinal tract and without causing internal hernia.
Other complications may occur in open surgery to retrieve the filter: ①inferior vena cava thrombosis and pulmonary embolism intraoperative and postoperative. In order to reduce vena cava injury, strict heparinization (100 IU/Kg) before blocking the vena cava is needed. Strict anticoagulation therapy was administered for 3 months following surgery, anticoagulation could be discontinued after a repeat CT scan hinting no stenosis or occlusion in inferior vena cava. In our study, there is no symptomatic pulmonary embolism and no new lower limb deep venous thrombosis. In the follow-up at 3 months after surgery, the IVC was patent in 20 cases and occluded in 1 case. The cause of the occlusion was considered to be related to endothelial hyperplasia and filter fracture after long-term retention of the filter. In the follow-up at 3 months after discontinuation of anticoagulation therapy, the IVC was still patent in 20 cases. Open surgical removal of the IVC filter was associated with a low risk of pulmonary embolism, discontinuation of anticoagulation after repair of the IVC endothelium. ② intraoperative injury to the inferior vena cava, common injury include adhesions between the barb penetrated the vein and the surrounding tissue, and injury due to separation of the filter from the vein wall. The filter can be cut and removed to reduce the damage to the vein intraoperative, and the injure of vena cava can be repaired with sutures. If the defect of vein is too large to be repaired, an autologous vein or an artificial patch, or even reconstruction with an artificial vena cava replacement is preferred. In this study, there was no serious injury to the inferior vena cava occurred in the patients and the injure of vena cava could be repaired by direct suture.
Rigorous preoperative screening and adequate thrombosis management are required. Before surgery, adequate screening should be performed to select patients who have thrombus formation, who have a reduced risk of pulmonary embolism, who have the good inflow and outflow tracts on CT scans, and who are at low risk of developing IVC thrombosis or new acute deep venous thrombosis in the presence of good blood flow. During the surgery, it is important to ligate the lumbar vein on the side of the IVC adjacent to the lumbar spine to significantly reduce hemorrhage. After surgery, anticoagulation therapy may be discontinued after 3–6 months with a patent IVC and no new acute deep venous thrombosis.
Comparison of related filter retrieval techniques
The “Loop snare technique”(29) is often used to correct the tilt of a tapered filter and to retrieve the filter when the retrieval hook is attached to the endothelium. However, the “Loop snare technique” is not successful in retrieving the filter when the retrieval hook is adhered to the inner membrane. In above cases, “the Hangman technique” can be used to retrieve the filter by cutting the adherent endothelium tissues, but it will also be limited by the availability of a localized slit to pass through. “The Loop snare technique” and “the Hangman technique” were used in all four cases of conical filters enrolled in this study and were unsuccessful in retrieving the filters, so the filters were retrieved by open surgery.
The laparoscopic technique of filter removal is more suitable for conical filter adhered to the vein wall with less damage than open surgery, but is limited in two ways: (i) whether the retrieval hook has penetrated the vein wall; if the retrieval hook has not penetrated the vein wall, it is difficult to locate the retrieval hook intraoperatively; and (ii) where the retrieval hook has penetrated the vein wall; when the retrieval hook penetrates the posterior wall of the inferior vena cava, it is more difficult to separate the posterior wall of the inferior vena cava using the laparoscopic technique. The non-conical filter and the vein wall are more heavily lined and the separation process is likely to damage the vein wall, and the non-conical filter has not yet been removed using laparoscopic techniques. In the four cases included in this study, the conical filter was removed by open surgery because the penetration site was in the posterior or lateral posterior wall.
Comparison of relevant studies
Tunner et al. (30) reported 190 IVC filter removals with severe complications in multiple clinical centers, of which 90 were removed using endovenous method and 100 were removed by open surgery. Of the 100 open surgery removals, 45 were performed via thoracotomy approach and 55 were performed via laparotomy approach. Open surgery led to a higher incidence of venous thromboembolism(VTE) complications, whereas no recurrence of IVC and lower limb deep venous thrombosis, and no symptomatic pulmonary embolism were found in the present study. Tunner et al.'s article reported a 5% mortality rate for open surgery, whereas no deaths occurred in the present study, which may have been attributed to the different characteristics of the cases analyzed in the study. Patients in the present study were mainly cases after the failure of removal of the filter by endovenous means, with 2 cases who had fracture complications, whereas cases reported by Tunner et al. were all with complications such as fractures and filter displacements. The cases were recruited in our study were malfunction of the filter and presented with comorbidities including respiratory, gastrointestinal, renal function, infection or thromboembolism. Our study focused on patients with filter rupture, abdominal pain, refusal of permanent anticoagulation or psychological factors, and some patients did not develop filter complications, which may be related to psychological factors in the Chinese population.
Rana (31) reported 6 cases of open surgical filter retrieval, the inferior vena cava was clamped in 2 cases, the inferior vena cava was not clamped in 3 cases, and the broken pedicle was removed successfully in 1 case. The unclamped inferior vena cava surgical approach was mainly applied to tapered filters with the retrieval hook penetrated through the vein wall, and the reserved suture around the retrieval hook could sealed the inferior vena cava after the filter was removed. In our study, the inferior vena cava was clamped intraoperatively in all patients, including 17 cases of non-conical filters and one case of Tulip filter removal using a similar method, but the inferior vena cava was still clamped and no inferior vena cava thrombosis or injury occurred after surgery.
Limitations
CT pulmonary angiogram (CTPA) was not performed before or after open surgery to remove the IVC filter, and no imaging was done to assess the presence of asymptomatic pulmonary embolism before or after surgery. Also, this was a single-center retrospective study with small sample size, and no control group was established.
Summary
In conclusion, open surgery can be used to remove IVC filters in cases after failure of endovenous removal attempts or with complications and as an adjunct intervention for successfully removing filters while avoiding the risk of serious injury to the IVC and relieving the physical and psychological distress in patients without symptomatic pulmonary embolism.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was approved by the Ethics committee of Beijing Jishuitan Hospital (No.JST202201-21). The patients/participants provided their written informed consent to participate in this study.
Author contributions
TX and LJ were responsible for the surgical procedure, article design, and writing; LJ was responsible for data collection, follow-up, and data analysis; JW, JP, CZ, and ZY were responsible for the surgical procedure; LX, MZ and TC were responsible for data collection. All authors contributed to the article and approved the submitted version.
Funding
Capital's Funds for Health Improvement and Research, CFH2022-2-2074 Beijing Municipal Administration of Hospital Incubating Program, Code: PX2022015.
Acknowledgments
The authors would like to thank all the doctors and nurses in the Vascular Surgery Department, Beijing Jishuitan Hospital.
Conflicts of interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Raskob GE, Angchaisuksiri P, Blanco AN, Buller H, Gallus A, Hunt BJ, et al. Thrombosis: a major contributor to global disease burden. Arterioscler Thromb Vasc Biol. (2014) 34(11):2363–71. doi: 10.1161/ATVBAHA.114.304488
2. Qaseem A, Snow V, Barry P, Hornbake ER, Rodnick JE, Tobolic T, et al. Current diagnosis of venous thromboembolism in primary care: a clinical practice guideline from the American academy of family physicians and the American college of physicians. Ann Intern Med. (2007) 146(6):454–8. doi: 10.7326/0003-4819-146-6-200703200-00013
3. Knudson MM, Ikossi DG, Khaw L, Morabito D, Speetzen LS. Thromboembolism after trauma: an analysis of 1602 episodes from the American college of surgeons national trauma data bank. Ann Surg. (2004) 240(3):490–8. doi: 10.1097/01.sla.0000137138.40116.6c
4. Heit JA, Spencer FA, White RH. The epidemiology of venous thromboembolism. J Thromb Thrombolysis. (2016) 41(1):3–14. doi: 10.1007/s11239-015-1311-6
5. Cohen A, Jeyaindran S, Kim JY, Park K, Sompradeekul S, Tambunan KL, et al. Treating pulmonary embolism in pacific Asia with direct oral anticoagulants. Thromb Res. (2015) 136(2):196–207. doi: 10.1016/j.thromres.2015.05.024
6. Pulmonary Embolism and Pulmonary Vascular Disease Group. Chinese Society of respiratory diseases. Guidelines on the prevention, diagnosis and treatment of pulmonary embolism. Nat Med J Chin. (2018) 98(14):1060–87. doi: 10.3760/cma.j.issn.0376-2491.2018.14.007
7. Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du risque d'Embolie pulmonaire par interruption cave study group. N Engl J Med. (1998) 338(7):409–15. doi: 10.1056/NEJM199802123380701
8. Streiff MB, Agnelli G, Connors JM, Crowther M, Eichinger S, Lopes R, et al. Guidance for the treatment of deep vein thrombosis and pulmonary embolism. J Thromb Thrombolysis. (2016) 41(1):32–67. doi: 10.1007/s11239-015-1317-0
9. Charalel RA, Durack JC, Mao J, Ross JS, Meltzer AJ, Sedrakyan A. Statewide Inferior vena Cava filter placement, complications, and retrievals: epidemiology and recent trends. Med Care. (2018) 56(3):260–5. doi: 10.1097/MLR.0000000000000867
10. Expert consensuses on the codes for the insertion and removal of inferior vena cava filters (2nd edition). Interventional physicians branch of Chinese medical doctor association. Nat Med J Chin. (2020) 100(27):2092–101. doi: 10.3760/cma.j.cn112137-20200317-00804
11. Baglin TP, Brush J, Streiff M. British Committee for Standards in Haematology Writing Group, Guidelines on use of vena cava filters. Br J Haematol. (2006) 134(6):590–5. doi: 10.1111/j.1365-2141.2006.06226.x
12. Moriarty JM, Steinberger JD, Bansal AK. Inferior vena Cava filters: when to place and when to remove. Semin Respir Crit Care Med. (2017) 38(1):84–93. doi: 10.1055/s-0036-1597558
13. Sella DM, Oldenburg WA. Complications of inferior vena cava filters. Semin Vasc Surg. (2013) 26(1):23–8. doi: 10.1053/j.semvascsurg.2013.04.005
14. Douketis JD. The 2016 American college of chest physicians treatment guidelines for venous thromboembolism: a review and critical appraisal. Intern Emerg Med. (2016) 11(8):1031–5. doi: 10.1007/s11739-016-1553-0
15. Lee MJ, Valenti D, de Gregorio MA, Minocha J, Rimon U, Pellerin O. The CIRSE retrievable IVC filter registry: retrieval success rates in practice. Cardiovasc Intervent Radiol. (2015) 38(6):1502–7. doi: 10.1007/s00270-015-1112-5
16. Alkhouli M, Morad M, Narins CR, Raza F, Bashir R. Inferior vena Cava thrombosis. JACC Cardiovasc Interv. (2016) 9(7):629–43. doi: 10.1016/j.jcin.2015.12.268
17. Tsui B, Moon E, Zheng J, Kapoor B, Wang W. Outcomes of the TrapEase inferior vena cava filter over 10 years at a single health care system. J Vasc Surg Venous Lymphat Disord. (2018) 6(5):599–605. doi: 10.1016/j.jvsv.2018.03.012
18. Wassef A, Lim W, Wu C. Indications, complications and outcomes of inferior vena cava filters: a retrospective study. Thromb Res. (2017) 153:123–8. doi: 10.1016/j.thromres.2017.02.013
19. Tian X, Liu JL, Jia W, Jiang P, Cheng ZY, Zhang YX, et al. Placing a new filter before removing embolized nonconical filter: a report of 13 cases. Ann Vasc Surg. (2021) 81:249–57. doi: 10.1016/j.avsg.2021.09.036
20. Wang HD, Liu Z, Zhu X, Liu JL, Man LB. Retroperitoneal laparoscopic-assisted retrieval of wall-penetrating Inferior vena Cava filter after endovascular techniques failed: an initial clinical outcome. Vasc Endovascular Surg. (2021) 55(7):706–11. doi: 10.1177/15385744211022517
21. Jeremy C, Antonio C, Stephanie K, Bhanu SB, Avrin DE, Gordon RL, et al. Perforation of the IVC: rule rather than exception after Longer indwelling times for the günther tulip and celect retrievable filters. Cardiovasc Interv Radiol. (2012) 35:299–308. doi: 10.1007/s00270-011-0151-9
22. Peter H, Vinod P, David T, Bush HL Jr. Open surgical inferior vena cava filter retrieval for caval perforation and a novel technique for minimal cavotomy filter extraction. J Vasc Surg. (2012) 56(1):256–9. doi: 10.1016/j.jvs.2011.12.065
23. EINSTEIN Investigators; Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H, Gallus AS, et al. Review of an article: oral rivaroxaban for symptomatic venous thromboembolism. The EINSTEIN investigators et al. N Engl J Med. (2010) 363(26):2499–510. J Vasc Nurs. 2011;29(2):89. doi: 10.1056/NEJMoa1007903
24. Couturaud F, Leroyer C, Tromeur C, Julian JA, Kahn SR, Ginsberg JS, et al. Factors that predict thrombosis in relatives of patients with venous thromboembolism. Blood. (2014) 124(13):2124–30. doi: 10.1182/blood-2014-03-559757
25. Charlton-Ouw KM, Leake SS, Sola CN, Sandhu HK, Albarado R, Holcomb JB, et al. Technical and financial feasibility of an inferior vena cava filter retrieval program at a level one trauma center. Ann Vasc Surg. (2015) 29:84e9. doi: 10.1016/j.avsg.2014.05.018
26. Sarosiek S, Crowther M, Sloan JM. Indications, complications, and management of inferior vena cava filters: the experience in 952 patients at an academic hospital with a level I trauma center. JAMA Intern Med. (2013) 173(7):513–7. doi: 10.1001/jamainternmed.2013.343
27. Grewal S, Chamarthy MR, Kalva SP. Complications of inferior vena cava filters. Cardiovasc Diagn Ther. (2016) 6(6):632–41. doi: 10.21037/cdt.2016.09.08
28. Quencer KB, Smith TA, Deipolyi A, Mojibian H, Ayyagari R, Latich I, et al. Procedural complications of inferior vena cava filter retrieval, an illustrated review. CVIR Endovasc. (2020) 3(1):23. doi: 10.1186/s42155-020-00113-6
29. Tian X, Liu JL, Li JY, Liu X. Case report: endoluminal removal of a retrievable conical inferior vena cava filter with a ruptured retraction hook attached to the wall. Front Surg. (2022) 10(9):985060. doi: 10.3389/fsurg.2022.985060
30. Kim TI, Abougergi MS, Guzman RJ, Ochoa Chaar CI. Costs and complications of hospital admissions for inferior vena cava filter malfunction. J Vasc Surg Venous Lymphat Disord. (2021) 9(2):315–320.e4. doi: 10.1016/j.jvsv.2020.08.002
Keywords: vena cava filter, open surgical filter removal, pulmonary embolism, thrombosis, complication
Citation: Tian X, Liu J, Li J, Jia W, Jiang P, Cheng Z, Zhang Y, Liu X, Zhou MI and Tian C (2023) Removal of inferior vena cava filter by open surgery after failure of endovenous retrieval. Front. Cardiovasc. Med. 10:1127886. doi: 10.3389/fcvm.2023.1127886
Received: 20 December 2022; Accepted: 28 March 2023;
Published: 17 April 2023.
Edited by:
Hua Qu, China Academy of Chinese Medical Sciences, ChinaReviewed by:
Guanhua Xue, Shanghai Jiao Tong University, ChinaYaoguo Yang, Capital Medical University, China
Shaoying Lu, The First Affiliated Hospital of Xi'an Jiaotong University, China
© 2023 Tian, Liu, Li, Jia, Jiang, Cheng, Zhang, Liu, Zhou and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianlong Liu bGpsX2h5ODhAc2luYS5jb20=
Specialty Section: This article was submitted to Thrombosis, a section of the journal Frontiers in Cardiovascular Medicine
 Xuan Tian
Xuan Tian Jianlong Liu
Jianlong Liu Jinyong Li
Jinyong Li Wei Jia
Wei Jia Xiao Liu
Xiao Liu M. I Zhou
M. I Zhou