- Department of Cardiac Surgery, First Affiliated Hospital, China Medical University, Shenyang, China
Background: Total aortic root replacement (TRR) is certainly beneficial for aortic root disease, but does it still have an advantageous prognosis for patients compared to valve-sparing aortic root replacement (VSRR)? An overview of reviews was conducted to assess each of their clinical efficacy/effectiveness.
Review methods: Systematic reviews (SRs)/Meta-analyses comparing the prognosis of TRR and VSRR in aortic root surgery were collected from 4 databases, all searched from the time of database creation to October 2022. Two evaluators independently screened the literature, extracted information and applied the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement, A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR 2) tool, Grading of Recommendations, Assessment, Development and Evaluations (GRADE), and Risk of Bias in Systematic Reviews (ROBIS) to evaluate the quality of reporting, methodological quality, risk of bias, and level of evidence of the included studies.
Main results: A total of 9 SRs/Meta-analyses were ultimately included. In terms of the reporting quality of the included studies, PRISMA scores ranged from 14 to 22.5, with issues mainly in reporting bias assessment, risk of study bias, credibility of evidence, protocol and registration, and funding sources. The methodological quality of the included SRs/Meta-analyses was generally low, with key items 2, 7, and 13 having major flaws and non-key items 10, 12, and 16. In terms of risk of bias assessment, the overall assessment of the included 9 studies was high-risk. The quality of the evidence was rated as low to very low quality for the three outcome indicators selected for the GRADE quality of evidence rating: early (within 30 days postoperatively or during hospitalization) mortality, late mortality, and valve reintervention rate.
Conclusions: VSRR has many benefits including reduced early and late mortality after aortic root surgery and reduced rates of valve-related adverse events, but the methodological quality of the relevant studies is low, and there is a lack of high-quality evidence to support this.
Systematic Review Registration: https://www.PROSPERO, identifier: CRD42022381330.
1. Introduction
TRR using a composite mechanical valve, as proposed by Bentall and De Bono in 1968 (1), has been a boon to many patients requiring surgery for aortic root disease. For more than 50 years, it has long been considered the “gold procedure” for aortic root disease, particularly type A aortic dissection and Marfan syndrome, because of its excellent early and late postoperative results (2, 3). However, the implementation of a mechanical prosthesis exposes patients to a cumulative risk of lifelong anticoagulation, hemodynamic restrictions, and an increased risk of thromboembolism. Even though bio-prosthesis implantation can minimize these risks, re-intervention would be an undesired result of bio-prosthesis degeneration (4–6).
Although TRR is the most common procedure performed during surgery for aortic root disease, the optimal management of the aortic valve at the time of root surgery remains highly controversial. The benefit of preserving the native aortic valve, particularly in some young patients with good aortic valve pathology, has been remarkable. This controversy has become more intense since the introduction of the reimplantation technique by David in 1992 (7) and the remodeling technique by Yacoub in 1983 (8). The superior early outcome, lower late cardiac-related mortality, and valve-related complications of VSRR have led to a strong preference (6, 9, 10). Because VSRR is so challenging, most studies have come from specialist cardiac centers. Some argue that the more technically demanding VSRR has a proportionally increased complication and mortality rate, both intraoperatively and postoperatively. In this way, the prognosis of patients who undergo VSRR is not necessarily better than those who opt for a composite mechanical or biological valve for TRR (11).
A large number of studies exist that have explored the early and late mortality and complications of TRR and VSRR, and several SRs/Meta-analyses have been published based on this. However, there is considerable heterogeneity in the original studies included in the various SRs/Meta-analyses in terms of year of publication, sample size, interventions/controls, and outcome indicators. In particular, the inconsistency of postoperative complication rates across different research has largely limited the application and dissemination of evidence-based evidence in clinical practice. Overview of reviews (Overviews) is a comprehensive approach to collecting systematic reviews on the etiology diagnosis, treatment, and prognosis of the same disease or health problem and conducting a comprehensive study (12). And this article aims to analyze the current published SRs/Meta-analyses on the prognosis of TRR compared to VSRR and provide a basis for clinical selection.
2. Materials and methods
The protocol for this overview was registered on PROSPERO (CRD42022381330) and is accessible on the PROSPERO website (https://www.crd.york.ac.uk/prospero/). The reporting of this overview of reviews adheres to the PRISMA 2020 criteria (13).
2.1. Search and study selection
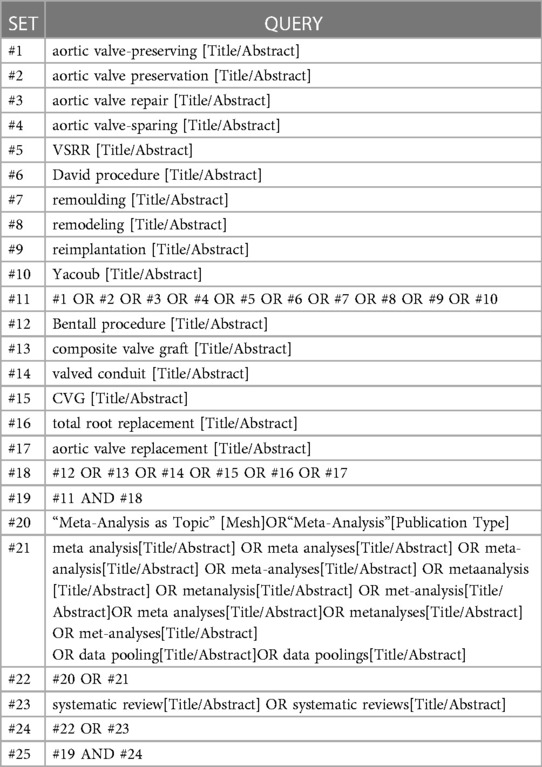
PubMed, Embase, Web of science, and China National Knowledge Infrastructure (CNKI) databases were searched to collect SRs/Meta-analyses comparing survival, mortality, complications, and reoperation rates after VSRR versus TRR, all searched from the time of database creation to October 2022. In addition, references to the included literature were retrospectively included to supplement access to relevant literature. Searches were conducted using a combination of subject terms and free words. Terms include aortic valve-sparing, aortic valve preservation, aortic valve repair, aortic valve-sparing, VSRR, David procedure, remodeling, Yacoub, reimplantation, Bentall procedure, composite valve graft, valved conduit, CVG, total root replacement, aortic valve replacement, systematic review, meta-analysis, etc. The specific search strategy for PubMed, for example, is shown in Table 1.
2.2. Inclusion and exclusion criteria
SRs/Meta-analyses were included if:
(i) Review of studies on the clinical outcomes of TRR and VSRR.
(ii) Research into aortic root diseases, including but not limited to aortic dissection and Marfan syndrome.
(iii) Primary outcome indicators include early mortality (within 30 days of surgery or during hospitalization), mortality during follow-up, reoperation rates, thromboembolic events, endocarditis, and bleeding associated with aortic root and aortic valve lesions.
SRs/Meta-analyses were excluded if:
(i) Reviews, conference abstracts, case reports, and letters.
(ii) Duplicate publications or overlapping studies included.
(iii) Literature for which data could not be extracted or full text was not available.
(iv) Currently incomplete SRs/Meta-analyses.
2.3. Literature screening and data extraction
Two evaluators independently screened the literature, extracted information, and cross-checked it, consulting a third person to assist with any disagreements and contacting the authors to supplement any missing information where possible. The literature was screened by first reading the title and abstract and then, after excluding any irrelevant literature, further reading the full text to determine final inclusion. If multiple SRs/Meta-analyses existed for the same group of researchers, those with a relatively recent year of publication and containing more complete studies were selected for inclusion. Data extraction included the following: first author and year of publication, number of included studies, sample size, interventions, risk of bias assessment tools used, outcome indicators, PRISMA score (14) results, AMSTAR 2 (15) evaluation results and funding sources.
2.4. Assessment of included reviews
All of the evaluation methods were assessed independently by two researchers and then summarized. Any inconsistencies were resolved by consensus or by third-author adjudication.
2.4.1. Reporting quality
The PRISMA Statement (14) evaluates the quality of the reports included in the study using a total of 27 items, with each item being scored 1 for complete reporting, 0.5 for partial reporting, and 0 for no reporting, out of a total of 27 points, with a score of <15 being considered a relatively serious information deficiency in the systematic evaluation report, a score of 15–21 being considered some deficiency in the report, and a score of 21 or more being considered a relatively complete report. The PRISMA statement indicates that a report with a completeness level of <50% for each item is considered to be deficient.
2.4.2. Methodological quality
The AMSTAR 2 (15) scale was used to evaluate the methodological quality of the included studies. The scale contains 16 items, of which items 2, 4, 7, 9, 11, 13, and 15 are key items, and the results are classified into three levels: satisfied, partially satisfied, and not satisfied. AMSTAR 2 scores of satisfied and partially satisfied ≥70% are considered to be a complete report of the items.
2.4.3. Evidence quality
GRADE (16) was used to evaluate the quality of evidence for different outcome indicators of the included studies, with downgrading factors including study limitations, inconsistency of findings, non-directness or indirectness (uncertainty about whether it is direct evidence), imprecision (insufficient precision or wide confidence intervals), and publication bias. The quality of the evidence was graded into four categories: high, moderate, low, and very low.
2.4.4. Risk of bias
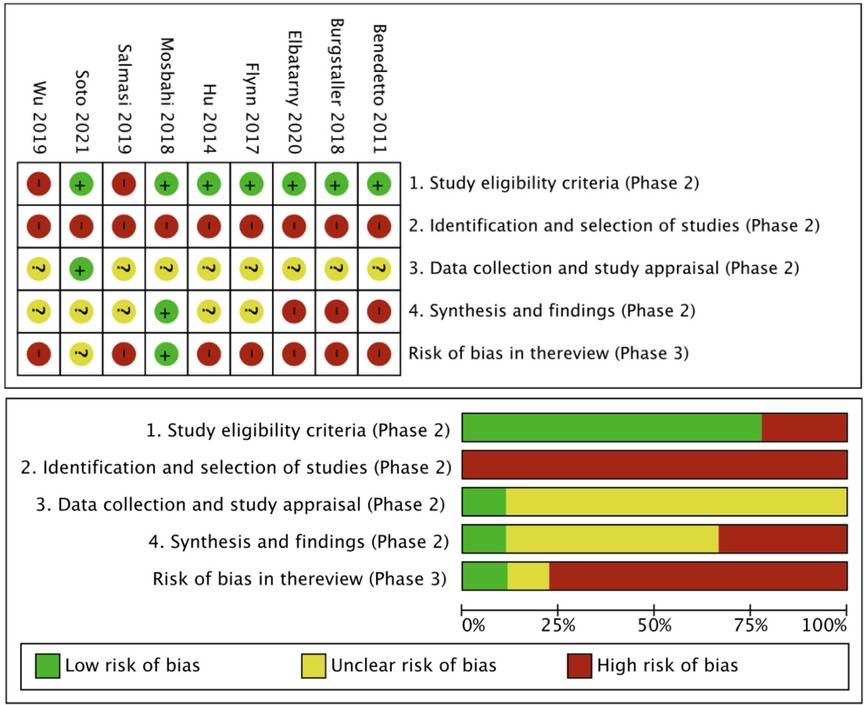
The level of bias in each of the included SRs was assessed using the ROBIS tool (17), which helps to assess the level of bias in four domains: (1) eligibility criteria for each study; (2) study identification and selection; (3) data collection and study evaluation; and (4) overall synthesis and key findings. Within each domain, specific questions were used to determine the risk of bias, with bias rated as “low”, “high” or “uncertain”.
2.5. Data synthesis and application of software
Due to the heterogeneity between SRs, particularly between the TRR and VSRR groups, and the duplication of studies included in the individual RCTs, the selected SRs were analyzed descriptively only, rather than quantitatively synthesized. The data were summarized as percentages and frequencies for each of PRISMA, AMSTAR 2, GRADE, and ROBIS. The characteristics and results of each SR and these tools' results are presented in tables and figures using RStudio and Review Manager (RevMan).
3. Results
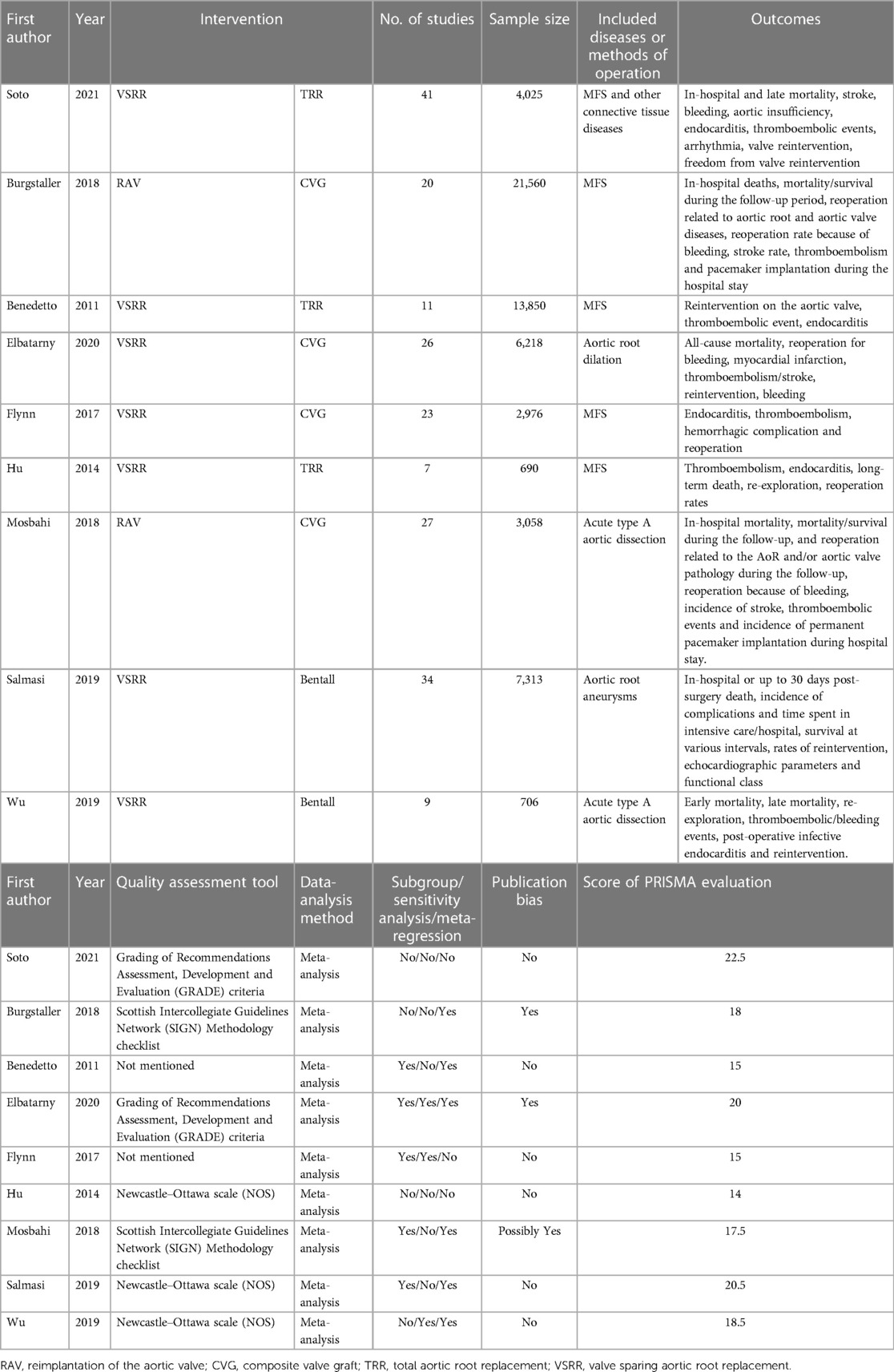
3.1. Literature selection and basic characteristics
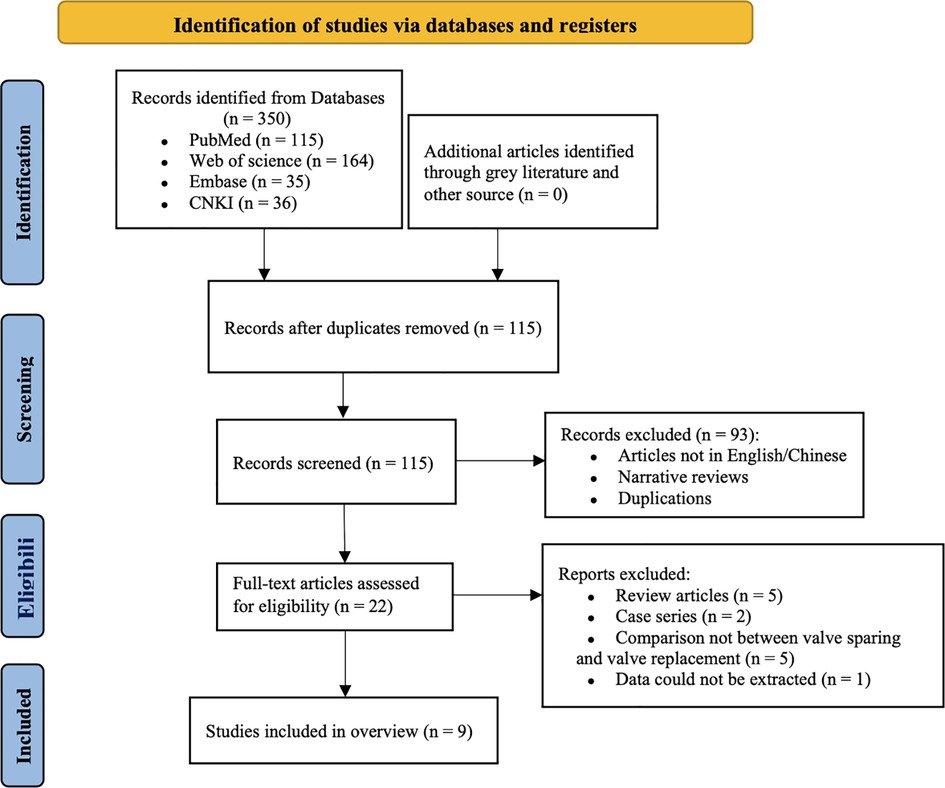
The initial literature search identified 350 potential SRs/Meta-analyses. Duplicate publications were removed by filtering (n = 235). After screening all titles and abstracts, 93 articles were excluded and the remaining 22 articles were retrieved for further review. After screening 22 full-text articles, 13 SRs were excluded and 9 SRs/Meta-analyses (18–26) were ultimately included. The literature screening process and results are shown in Figure 1. The basic characteristics of the included studies are shown in Table 2.
3.2. Quality evaluation of the included studies
3.2.1. Reporting quality
The PRISMA (14) scores for the included studies ranged from 14 to 22.5 (Table 2). Of these, 1 study (23) scored 14 (reported relatively serious information deficiencies) and 7 studies (19–22, 24–26) scored ≤21 (reported some deficiencies). The PRISMA statement (14) items for which more than half of the studies were rated as “not satisfied” included: assessment of reporting bias, risk of study bias, credibility of evidence, protocol and registration, and funding source. PRISMA statement (14) items for which more than half of the studies were evaluated as “partially satisfied” included: a structured summary, inclusion/exclusion criteria, information sources, search strategy, data extraction, data items, synthesis of methods, and synthesis of results.
3.2.2. Methodological quality
The results of the AMSTAR 2 (15) evaluation showed that the methodological quality of all studies was “very low” (Table 3). A total of 5 items with AMSTAR 2 scores of ≥70% satisfied and partially satisfied indicated high quality. Of the 7 critical items in the AMSTAR 2 (15) quality assessment, item 2, item 7, and item 13 had significant deficiencies; the non-critical items with significant deficiencies were item 10, item 12, and item 16. The results for each item in the AMSTAR 2 quality assessment are shown in Figure 2.
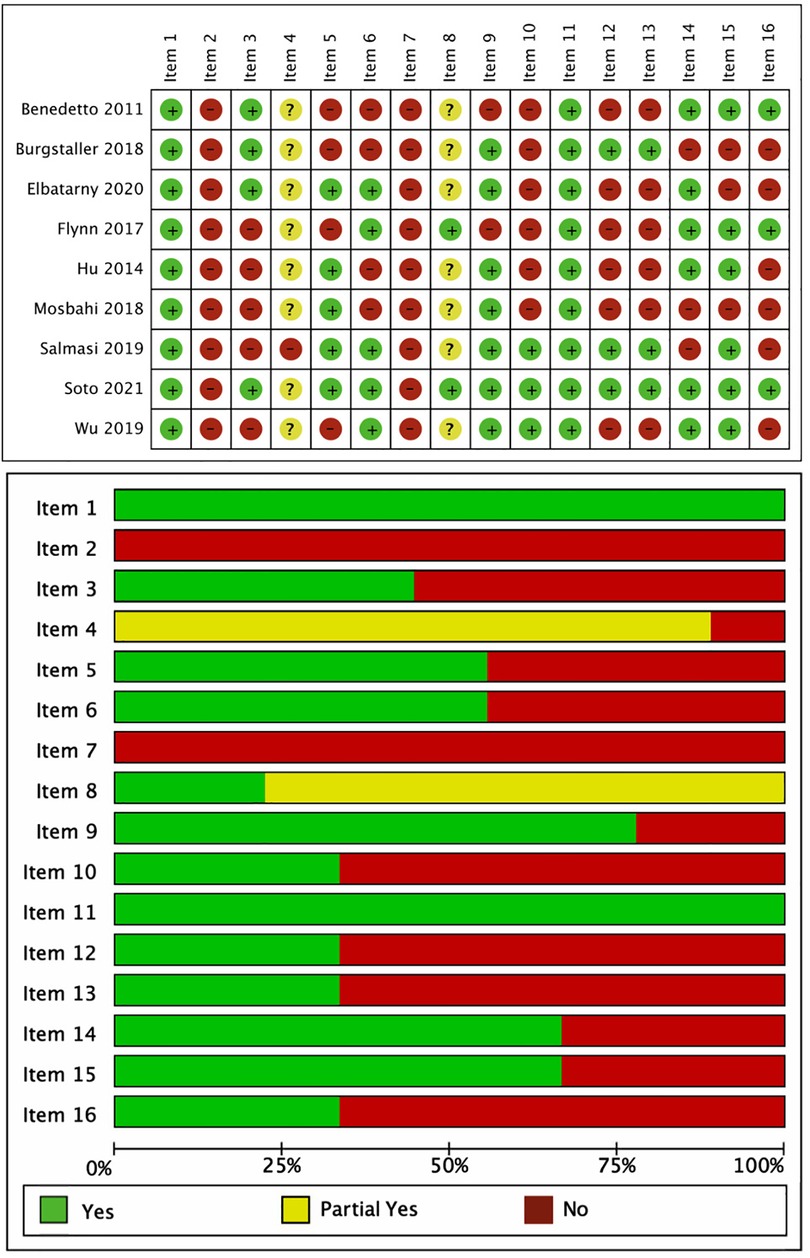
Figure 2. Results of the visualization quality evaluation of A Measurement Tool to Assess Systematic Reviews 2.
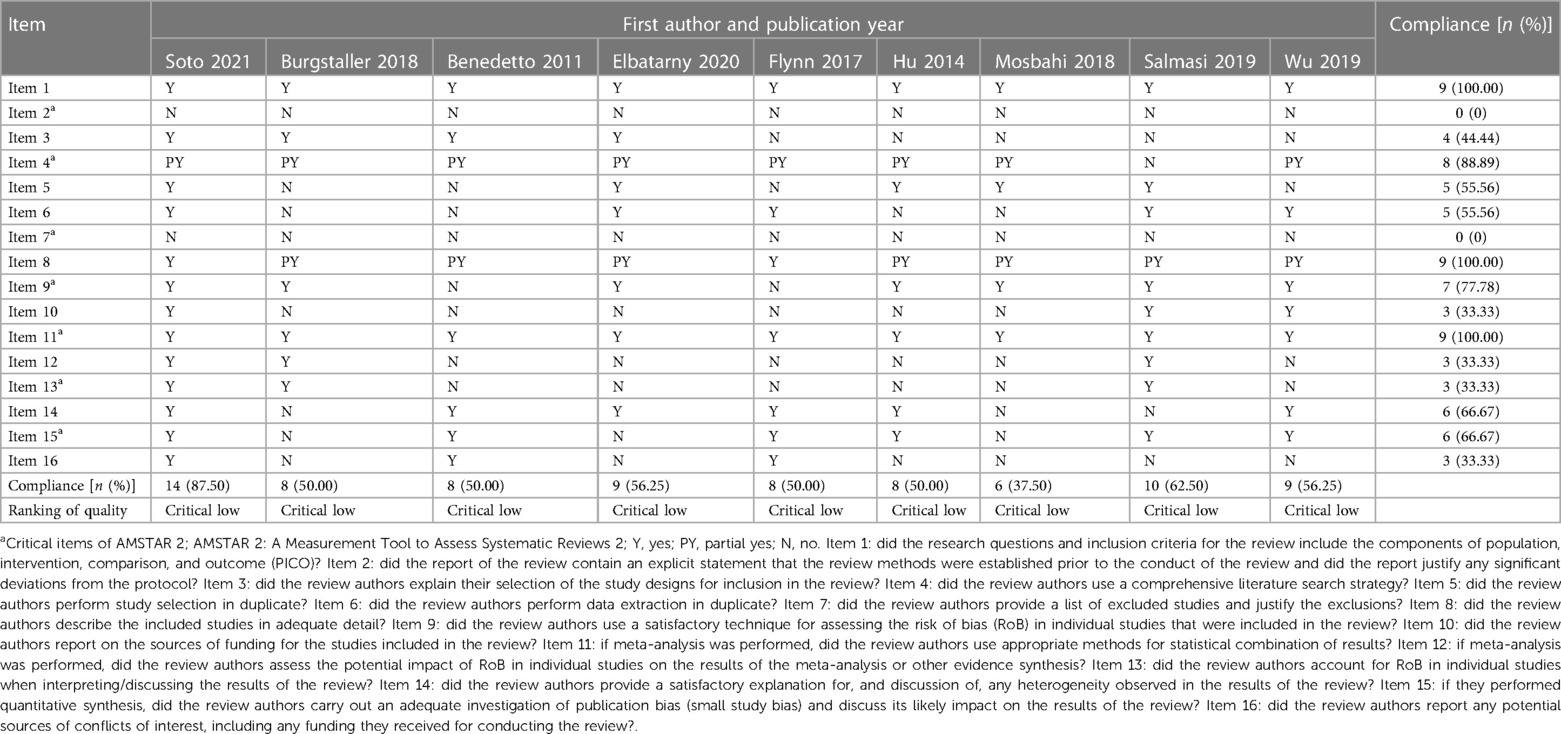
Table 3. Methodological quality assessment of included systematic reviews/meta-analyses by AMSTAR 2.
3.2.3. Evidence quality
7 articles (18, 19, 21, 23–26) reporting early mortality were included, 3 (19, 21, 24) of which showed very low-quality evidence. 6 (18, 21–23, 25, 26) that reported late mortality, 5 (18, 21–23, 26) on valve re-intervention, and 3 (18, 21, 22) on bleeding were included, and they each showed the results of Elbatarny et al. (21) as very low-quality evidence. Except for the very low-quality evidence mentioned above, all were low-quality evidence. The main factors causing the downgrading of the quality of the evidence were Inconsistency, Indirectness, and Imprecision. The results are detailed in Table 4 and Figure 3.
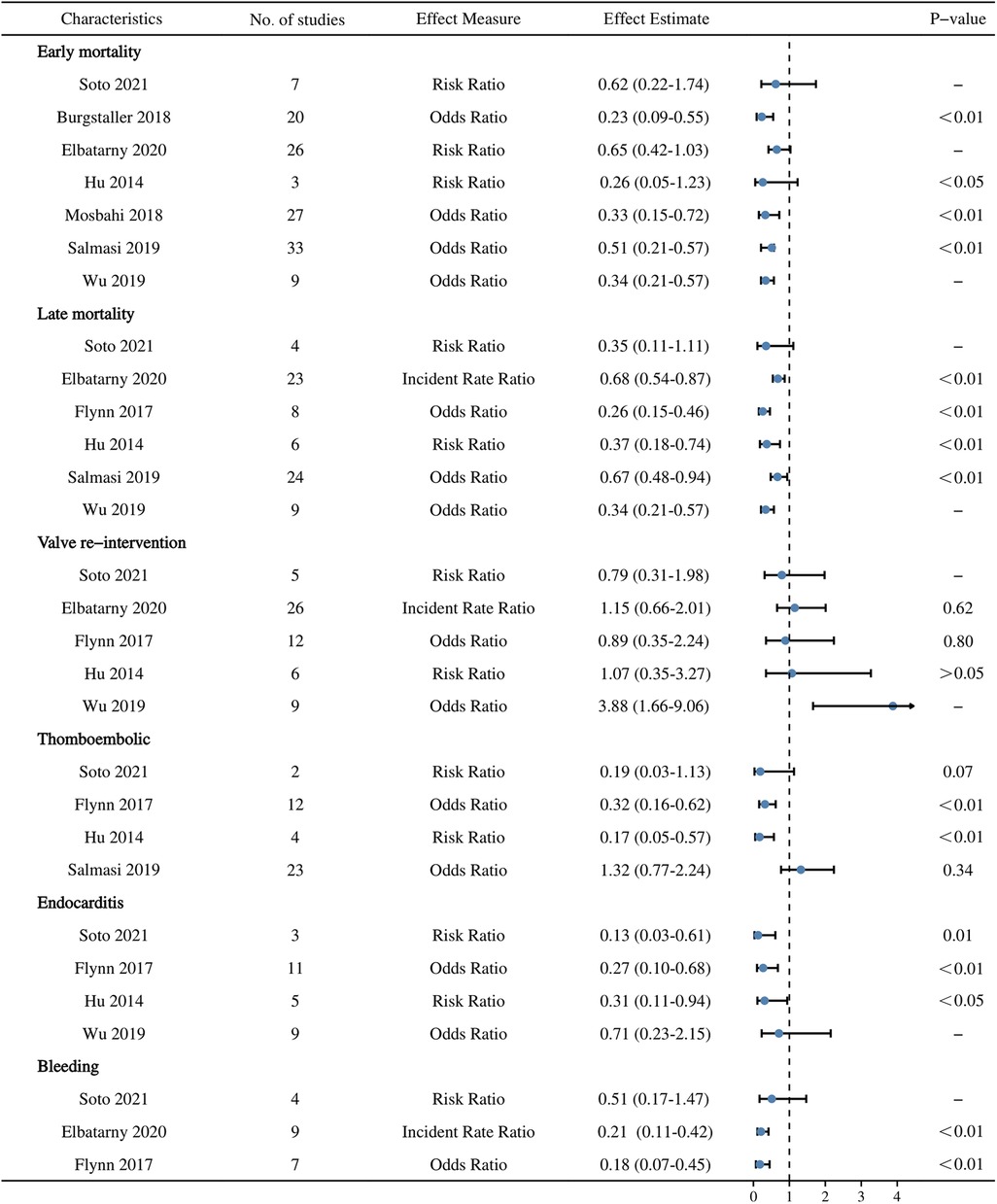
Figure 3. A summary of the 6 postoperative outcomes evaluated using Grading of Recommendations, Assessment, Development and Evaluations.
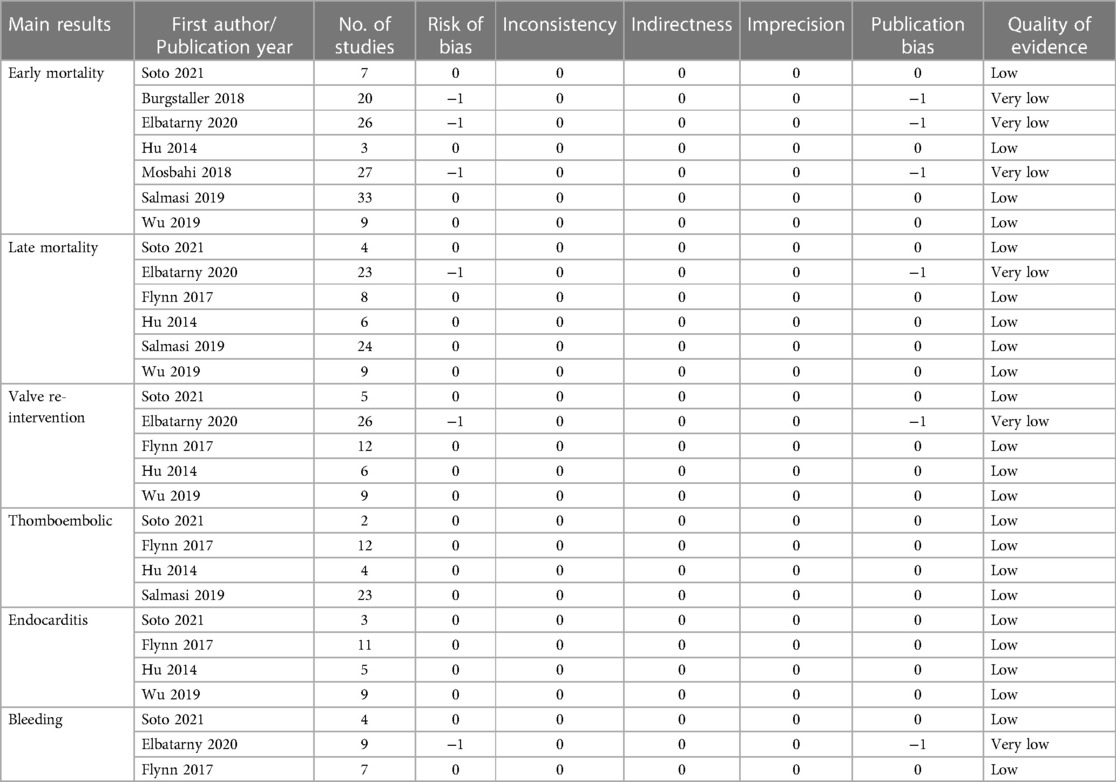
Table 4. Main results assessed by the grading of recommendations, assessment, development and evaluations.
3.2.4. Risk of bias
In this overview, we did not implement the first stage of ROBIS, which was used to determine whether the proposed question and the target question matched. Using Domain-1 to assess the inclusion and exclusion criteria for each study, we found that 77.8% (7/9) of the SRs/Meta-analyses (18–24) had a low risk of bias. Domain-2 examined the process of identifying, retrieving, and selecting literature in each SR and showed that all (18–26) were at high risk of bias. In Domain-3, data extraction and quality evaluation, 1 SR/Meta-analyses (18) with a low risk of bias and 8 SRs/Meta-analyses (19–26) with an uncertain risk of bias were identified. Domain-4 evaluated the overall results and the combined results of each study and showed that 4 studies (19–21, 24) had a high risk of bias and 5 studies (18, 22, 23, 25, 26) had an uncertain risk of bias. Of the 9 SRs/Meta-analyses (18–26) included, all were evaluated as high risk of bias. Table 5 and Figure 4 present the ROBIS results for each SR.
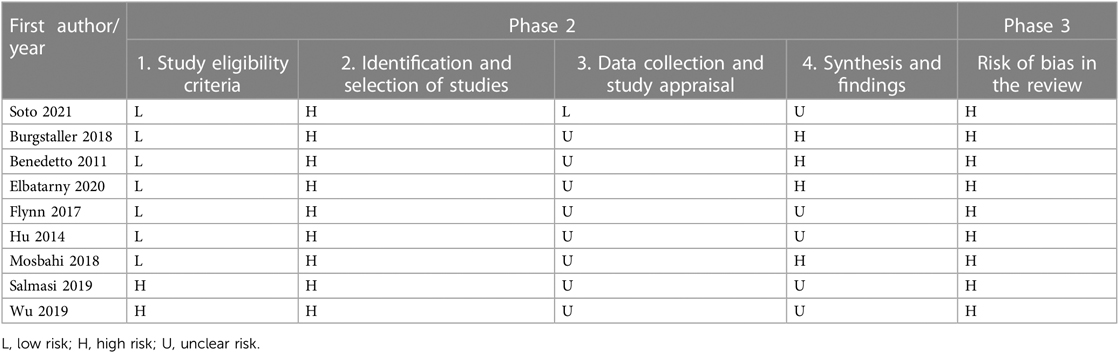
Table 5. Risk of bias of the included systematic reviews assessed by risk of bias in systematic reviews.
4. Discussion
The main objective of this overview is to assess and summarize the available clinical evidence through the currently published SRs/Meta-analyses on VSRR and TRR. However, the currently available SRs/Meta-analyses were of unsatisfactory quality through our series of scale evaluations, suggesting that we need to be more cautious about further interpreting their results.
In terms of reporting quality, 1 (23) study had relatively serious information deficiencies (<15 points) and 7 (19–22, 24–26) had moderate deficiencies (≤21 points), mainly related to the evaluation of reporting bias, risk of study bias, credibility of evidence, protocol and registration, funding source, inclusion/exclusion criteria, search strategy, data extraction, and synthesis of methods and results. Of course, the above-mentioned issues are also common problems with SRs/Meta-analyses at present, especially in terms of scheme and registration, which need our attention. If we make our scheme and register it before the study, it can make us more logical on the one hand, and on the other hand, it can be used by others to search for and find the problems in time, which is a very good pre-communication process. In addition, PICO criteria were not well represented in a significant number of included studies (19, 20, 22–24, 26), and most of the included studies did not provide a complete search formula. This is a reason to suspect that the original literature is missing.
In terms of methodological quality, key items 2 and 7 in all 9 included studies had serious deficiencies. Before the implementation of the systematic review, the authors did not clearly state the study methodology for the systematic review, did not state the existence of a written protocol or guidance document, and all studies did not provide a list of excluded literature. Only three studies (18, 19, 25) considered the risk of bias in the included studies when interpreting and discussing each outcome. These results suggested that the current SR/Meta-analyses of issues related to postoperative VSRR versus TRR were largely able to follow reporting norms, but methodological quality needs to be improved, and investigators still lack attention to protocol registration, provision of search strategies, and the risk of bias in included studies.
In terms of evidence quality, the included SRs/Meta-analyses were of low/very low quality, which may be due to the following reasons. First, the methodological quality of the included cohorts was uneven and subject to large bias. Second, the outcome indicators reported in the cohort studies were not comprehensive, resulting in small sample sizes, wide confidence intervals, and imprecise results in some subgroups. Third, for publication bias reporting, some studies reported only the funnel plot, Egger's test, and Begg's test results for the primary outcome, which may have affected the credibility of other secondary outcomes.
As we know, both VSRR and TRR are different procedures for aortic root disease, and their biggest difference is whether the native aortic valve is preserved or not during the procedure. There is no denying that the VSRR is more difficult than the TRR. As mentioned in the 2022 American College of Cardiology/American Heart Association (ACC/AHA) guidelines (27), valve-preserving aortic root replacement is justified in patients undergoing aortic root replacement if the valve is suitable for repair and performed by an experienced surgeon on a multidisciplinary aortic team. In addition, the evaluation of the patient's aortic valve as well as the overall systemic condition is particularly important when performing VSRR. Through a review of the available literature, as well as our center's experience, VSRR is aggressively performed in patients with the following conditions: (i) good aortic valve pathology with high hope of preservation; (ii) young patients, especially women of reproductive age; and (iii) patients with contraindications to anticoagulation.
It is undeniable that in the secondary studies we included and in some original studies from large centers, patients who underwent VSRR had a longer time to cross-clamping and circulatory arrest than those who underwent TRR, yet the early and late mortality rates were lower in the VSRR group than those in the TRR group (28, 29). There were also very few complications in those receiving VSRR, especially the stroke rate during hospitalization, which was only half that of patients who received TRR (24). Several studies have shown a significant decrease in bleeding/embolic/endocarditis events to varying degrees as well (30–32). Beyond the above problems, the rate of valve re-intervention in patients undergoing VSRR is of real concern to everyone. Among the 5 included studies (18, 21–23, 26), only the re-intervention rate of VSRR was higher in the study by Wu et al. (26) and was approximately 4 times higher than that of patients in the TRR group. The rest of the studies did not differ from the TRR group of patients. However, this is quite acceptable given that the incidence of reintervention was only 3% higher in the VSRR group than in the TRR group in the study [VSRR: 4.9% (95% CI 0.008–0.090), TRR: 1% (95% CI 0.001–0.017)]. Therefore, we said that VSRR should be the first choice for patients if conditions permit.
5. Limitation
Although we have made a more detailed assessment and summary, we still cannot avoid some limitations. Firstly, multiple scales were used in the quality evaluation part of this study, and the subjectivity of the researchers in evaluating the literature could lead to bias and consequently affect the evaluation results. Secondly, SRs/Meta-analyses published more than 5.5 years were generally considered to have reduced timeliness, whereas the cycle of cardiovascular disease-related literature was even shorter (3 years) (33), and some of the studies in this review were published earlier and their contents need to be updated. Finally, there were differences in the level of centers and operators performing the VSRR procedure, and bias in the results was inherently unavoidable.
6. Conclusion
The current SRs/Meta-analyses point to many benefits of VSRR, including reduced early and late mortality after aortic root surgery and reduced incidence of valve-related adverse events, but the methodological quality of the relevant studies was low, and there was a lack of high-quality evidence to support them. Large-sample, multicenter clinical randomized controlled trials are necessary, and we need more rigorous and methodologically sound SRs/Meta-analyses to draw clear conclusions that can guide clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
WW, TG, and ES wrote the main manuscript text. XZ, YS, SX, TS, and XH prepared figures and tables. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bentall H, De Bono A. A technique for complete replacement of the ascending aorta. Thorax. (1968) 23(4):338–9. doi: 10.1136/thx.23.4.338
2. Gott VL, Greene PS, Alejo DE, Cameron DE, Naftel DC, Miller DC, et al. Replacement of the aortic root in patients with Marfan's syndrome. N Engl J Med. (1999) 340(17):1307–13. doi: 10.1056/nejm199904293401702
3. Kouchoukos NT, Marshall WG Jr, Wedige-Stecher TA. Eleven-year experience with composite graft replacement of the ascending aorta and aortic valve. J Thorac Cardiovasc Surg. (1986) 92(4):691–705. doi: 10.1016/S0022-5223(19)35873-8
4. Craver JM, Weintraub WS, Jones EL, Guyton RA, Hatcher CR Jr. Predictors of mortality, complications, and length of stay in aortic valve replacement for aortic stenosis. Circulation. (1988) 78(3 Pt 2):I85–90.3261658
5. Christakis GT, Weisel RD, David TE, Salerno TA, Ivanov J. Predictors of operative survival after valve replacement. Circulation. (1988) 78(3 Pt 2):I25–I34.3409516
6. Ouzounian M, Rao V, Manlhiot C, Abraham N, David C, Feindel CM, et al. Valve-sparing root replacement compared with composite valve graft procedures in patients with aortic root dilation. J Am Coll Cardiol. (2016) 68(17):1838–47. doi: 10.1016/j.jacc.2016.07.767
7. David TE, Feindel CM. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J Thorac Cardiovasc Surg. (1992) 103(4):617–21; discussion 622. doi: 10.1016/S0022-5223(19)34942-6
8. Sarsam MA, Yacoub M. Remodeling of the aortic valve anulus. J Thorac Cardiovasc Surg. (1993) 105(3):435–8. doi: 10.1016/S0022-5223(19)34225-4
9. Coselli JS, Volguina IV, LeMaire SA, Sundt TM, Connolly HM, Stephens EH, et al. Early and 1-year outcomes of aortic root surgery in patients with Marfan syndrome: a prospective, multicenter, comparative study. J Thorac Cardiovasc Surg. (2014) 147(6):1758–66. doi: 10.1016/j.jtcvs.2014.02.021
10. Caceres M, Ma Y, Rankin JS, Saha-Chaudhuri P, Englum BR, Gammie JS, et al. Mortality characteristics of aortic root surgery in North America. Eur J Cardiothorac Surg. (2014) 46(5):887–93. doi: 10.1093/ejcts/ezu083
11. Miller DC. Aortic valve-sparing surgery: yes, but not for every patient and select the center very carefully. J Am Coll Cardiol. (2016) 68(17):1848–50. doi: 10.1016/j.jacc.2016.08.020
12. Becker LA, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.0.2. The cochrane collaboration (2009). Available at: www.cochrane- handbook.org.
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
14. La Moher D, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6(7):e1000097. doi: 10.1371/journal.pmed.1000097
15. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Br Med J. (2017) 358:j4008. doi: 10.1136/bmj.j4008
16. Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence–imprecision. J Clin Epidemiol. (2011) 64(12):1283–93. doi: 10.1016/j.jclinepi.2011.01.012
17. Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. (2016) 69:225–34. doi: 10.1016/j.jclinepi.2015.06.005
18. Soto ME, Ochoa-Hein E, Anaya-Ayala JE, Ayala-Picazo M, Koretzky SG. Systematic review and meta-analysis of aortic valve-sparing surgery versus replacement surgery in ascending aortic aneurysms and dissection in patients with marfan syndrome and other genetic connective tissue disorders. J Thorac Dis. (2021) 13(8):4830–44. doi: 10.21037/jtd-21-789
19. Burgstaller JM, Held U, Mosbahi S, Stak D, Steurer J, Eckstein F, et al. A systemic review and meta-analysis: long-term results of the bentall versus the david procedure in patients with Marfan syndrome. Eur J Cardiothorac Surg. (2018) 54(3):411–9. doi: 10.1093/ejcts/ezy158
20. Benedetto U, Melina G, Takkenberg JJ, Roscitano A, Angeloni E, Sinatra R. Surgical management of aortic root disease in Marfan syndrome: a systematic review and meta-analysis. Heart. (2011) 97(12):955–8. doi: 10.1136/hrt.2010.210286
21. Elbatarny M, Tam DY, Edelman JJ, Rocha RV, Chu MWA, Peterson MD, et al. Valve-sparing root replacement versus composite valve grafting in aortic root dilation: a meta-analysis. Ann Thorac Surg. (2020) 110(1):296–306. doi: 10.1016/j.athoracsur.2019.11.054
22. Flynn CD, Tian DH, Wilson-Smith A, David T, Matalanis G, Misfeld M, et al. Systematic review and meta-analysis of surgical outcomes in Marfan patients undergoing aortic root surgery by composite-valve graft or valve sparing root replacement. Ann Cardiothorac Surg. (2017) 6(6):570–81. doi: 10.21037/acs.2017.11.06
23. Rui H, Zhiwei W, Xiaoping H, Hongbing W, Zhen Z. Effect of native aortic valve sparing aortic root reconstruction surgery on short- and long-term prognosis in Marfan syndrome patients: a meta-analysis. Chin J Cardiol. (2014) 42(5):433–8. 10.3760/cma.j.issn.0253–3758.2014.05.018
24. Mosbahi S, Stak D, Gravestock I, Burgstaller JM, Steurer J, Eckstein F, et al. A systemic review and meta-analysis: bentall versus david procedure in acute type A aortic dissection. Eur J Cardiothorac Surg. (2019) 55(2):201–9. doi: 10.1093/ejcts/ezy266
25. Salmasi MY, Theodoulou I, Iyer P, Al-Zubaidy M, Naqvi D, Snober M, et al. Comparing outcomes between valve-sparing root replacement and the bentall procedure in proximal aortic aneurysms: systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. (2019) 29(6):911–22. doi: 10.1093/icvts/ivz211
26. Wu J, Huang Y, Qiu J, Saeed B, Yu C. Is valve-sparing root replacement a safe option in acute type A aortic dissection? A systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. (2019) 29(5):766–75. doi: 10.1093/icvts/ivz180
27. Isselbacher EM, Preventza O, Hamilton Black Iii J, Augoustides JG, Beck AW, Bolen MA, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American heart association/American college of cardiology joint committee on clinical practice guidelines. J Am Coll Cardiol. (2022) 80(24):e223–e393. doi: 10.1016/j.jacc.2022.08.004
28. Franke UF, Isecke A, Nagib R, Breuer M, Wippermann J, Tigges-Limmer K, et al. Quality of life after aortic root surgery: reimplantation technique versus composite replacement. Ann Thorac Surg. (2010) 90(6):1869–75. doi: 10.1016/j.athoracsur.2010.07.067
29. Lee H, Cho YH, Sung K, Kim WS, Park KH, Jeong DS, et al. Clinical outcomes of root reimplantation and bentall procedure: propensity score matching analysis. Ann Thorac Surg. (2018) 106(2):539–47. doi: 10.1016/j.athoracsur.2018.02.057
30. Halstead JC, Spielvogel D, Meier DM, Rinke S, Bodian C, Malekan R, et al. Composite aortic root replacement in acute type A dissection: time to rethink the indications? Eur J Cardiothorac Surg. (2005) 27(4):626–32; discussion 632–3. doi: 10.1016/j.ejcts.2004.12.059
31. Lewis CT, Cooley DA, Murphy MC, Talledo O, Vega D. Surgical repair of aortic root aneurysms in 280 patients. Ann Thorac Surg. (1992) 53(1):38–45; discussion 45–6. doi: 10.1016/0003-4975(92)90755-s
32. Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The task force for the diagnosis and treatment of aortic diseases of the European society of cardiology (ESC). Eur Heart J. (2014) 35(41):2873–926. doi: 10.1093/eurheartj/ehu281
Keywords: total aortic root replacement, valve-sparing aortic root replacement, aortic surgery, overview of reviews, systematic reviews
Citation: Wang W, Zhang X, Shi Y, Xu S, Shi T, Han X, Gu T and Shi E (2023) Is valve-sparing aortic root replacement better than total aortic root replacement? An overview of reviews. Front. Cardiovasc. Med. 10:1115290. doi: 10.3389/fcvm.2023.1115290
Received: 3 December 2022; Accepted: 3 April 2023;
Published: 18 April 2023.
Edited by:
Xiangjiu Ding, Qilu Hospital, Shandong University, ChinaReviewed by:
Pavel Zacek, University Hospital Hradec Kralove, CzechiaTim Kaufeld, Hannover Medical School, Germany
© 2023 Wang, Zhang, Shi, Xu, Shi, Han, Gu and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Enyi Shi c2hpZW55aTIwMDJAaG90bWFpbC5jb20= Tianxiang Gu c2V5MjAwNEBzaW5hLmNvbQ==
Specialty Section: This article was submitted to Aortic Surgery and Endovascular Repair, a section of the journal Frontiers in Cardiovascular Medicine
 Wei Wang
Wei Wang Xuezhou Zhang
Xuezhou Zhang Enyi Shi
Enyi Shi