- Department of Cardiology, West China Hospital, Sichuan University, Chengdu, China
Background and Objective: The evidence on the risk of mortality after myocardial infarction (MI) among migrants compared with natives is mixed and limited. The aim of this study is to assess the mortality risk after MI in migrants compared to natives.
Methods: This study protocol is registered with PROSPERO, number CRD42022350876. We searched the Medline and Embase databases, without time and language constraints, for cohort studies that reported the risk of mortality after MI in migrants compared to natives. The migration status is confirmed by country of birth, both migrants and natives are general terms and are not restricted to a particular country or area of destination or origin. Two reviewers separately screened searched studies according to selection criteria, extracted data, and assessed data quality using the Newcastle-Ottawa Scale (NOS) and risk of bias of included studies. Pooled estimates of adjusted and unadjusted mortality after MI were calculated separately using a random-effects model, and subgroup analysis was performed by region of origin and follow-up time.
Result: A total of 6 studies were enrolled, including 34,835 migrants and 284,629 natives. The pooled adjusted all-cause mortality of migrants after MI was higher than that of natives (OR, 1.24; 95% CI, 1.10–1.39; I2 = 83.1%), while the the pooled unadjusted mortality of migrants after MI was not significantly different from that of natives (OR, 1.11; 95% CI, 0.69–1.79; I2 = 99.3%). In subgroup analyses, adjusted 5–10 years mortality (3 studies) was higher in the migrant population (OR, 1.27; 95% CI, 1.12–1.45; I2 = 86.8%), while adjusted 30 days (4 studies) and 1–3 years (3 studies) mortality were not significantly different between the two groups. Migrants from Europe (4 studies) (OR, 1.34; 95% CI, 1.16–1.55; I2 = 39%), Africa (3 studies) (OR, 1.50; 95% CI, 01.31–1.72; I2 = 0%), and Latin America (2 studies) (OR, 1.44; 95% CI, 1.30–1.60; I2 = 0%) had significantly higher rates of post-MI mortality than natives, with the exception of migrants of Asian origin (4 studies) (OR, 1.20; 95% CI, 0.99–1.46; I2 = 72.7%).
Conclusions: Migrants tend to have lower socioeconomic status, greater psychological stress, less social support, limited access to health care resources, etc., therefore, face a higher risk of mortality after MI in the long term compared to natives. Further research is needed to confirm our conclusions, and more attention should be paid to the cardiovascular health of migrants.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier: r CRD42022350876.
Introduction
Although the treatment and prognosis of myocardial infarction (MI) have improved greatly in recent decades, ischemic heart disease (IHD) was estimated to be responsible for more than 5 million deaths in 2019 and remains one of the leading causes of mortality in the world, bringing great burdens both to society and individuals (1). It is well known that the morbidity and mortality of cardiovascular diseases between different countries or regions are substantially different, such as the global burden of disease (GBD) study showed the incidence and prevalence of IHD in some high-income countries are higher than those in some low- and middle-income countries, although the disability adjusted life years (DALY) of IHD in some high-income countries are lower than those in some middle-income countries, and the age-standardized DALYs due to IHD were highest in Eastern Europe, Central Asia, Oceania, and the Middle East/North Africa, and relatively low in the rest regions of the world (1–3).
At the same time, with the continuous process of globalization, the number of international migrations has continued to grow in the past few decades. It is estimated that the number of persons living outside of their country of origin reached 281 million in 2020, among them, over 90 percent lived in high-income or upper middle-income countries, and about 76 percent came from a middle-income or low-income country (4). Nearly one in every six persons residing in a high-income country is a migrant, and they have profoundly changed the demographic structure of the destination country (4, 5). Therefore, the health status of the migrant population is of widespread concern.
Most studies have focused on the morbidity or mortality of diseases in the entire population of migrants compared to natives, including cardiovascular diseases, with mixed results (6). Some studies have observed that migrants are generally healthier than the natives, particularly in the early stages of migration, proposing the healthy migration hypothesis, whereby relatively healthier groups are more likely to migrate, and the salmon bias hypothesis, whereby less healthy migrants tend to return to their place of origin (7–9). These hypotheses and supporting observational data contradict the conventional view of migrants' health, as many studies also show that migrants often face many disadvantages, such as low socioeconomic status, language, cultural barriers, psychosocial stress, limited access to health care services, and therefore have poorer health (10, 11). A recent meta-analysis concluded that migrants had an advantage in mortality for most diseases, but no difference in ischemic circulatory disease; however, this study excluded certain patient groups, such as those already in the intensive care unit with MI (12). Despite MI is one of the main diseases that affect the human life span and there are large number of migrants with MI, studies investigating the outcomes of migrants with MI are limited.
The purpose of our study was to conduct a systematic review and meta-analysis to assess the prognostic differences between migrants and natives with MI and to explore the impact of migration on the prognosis of the migrant population with MI. The findings may help improve cardiovascular health in this large population and reduce health disparities while providing a specific perspective to further illustrate the mechanisms by which immigration affects health.
Methods
This is a systematic review and meta-analysis that followed the PRISMA guidelines (13), and the protocol was registered with the prospective register of systematic reviews (PROSPERO; registration number CRD 42022350876). The PRISMA checklist is provided in the Supplementary Appendix S1.
Eligibility criteria
We initially included studies that assessed the prognosis of migrant populations with MI. The study subjects were migrants with MI, whereas the comparison subjects were natives of the destination country with MI, and the main outcome was all-cause mortality after MI. MI are confirmed by ICD codes or clinical definition, and migrants are defined as those born in countries other than the country in which they currently live and the study was conducted. Both migrants and natives are general terms and are not restricted to a particular country or area of destination or origin. Studies were excluded if they met any of the following criteria: an editorial; a conference abstract; studies observing ethnic background only, with no explicit definition of migration; studies focused on subpopulations such as refugees; and a lack of a local resident control group.
Search strategy
We searched MEDLINE via Ovid (from 1946 to November Week 1 2022) and EMBASE via Ovid (from 1974 to 2022 November 15) for published peer-reviewed literature with no restrictions on language and date. Additional records were identified by manual searches for references in the included studies. Using a Boolean search strategy developed by consulting previous literature (14, 15), detailed search terms are listed in Supplementary Appendix S2.
Study selection
All citations in the search were downloaded to Endnote™, and duplicate citations were removed. Two reviewers (LZ and BTH) independently screened the titles and abstracts of all citations in the database, and disagreements were resolved by consensus or by reference to the third reviewer (MC). The full texts of the included articles were assessed for eligibility by two reviewers independently using a checklist of inclusion and exclusion criteria, with reasons for exclusion noted, and disagreements were discussed by all authors to seek consensus.
Data extraction
Two reviewers (LZ and BTH) independently collected data from the included studies: name of first author, year of publication, country, study design, country of origin, year of study, number of participants, age range, sex, number of mortality events, mortality rates, and follow-up time. Duplicate data were removed for studies reporting the same migrant group (by country of destination) for the same mortality outcome and period. Contradictions were resolved by consensus. Microsoft Office Excel was used to manage data extraction.
Quality assessment
We used the Newcastle‒Ottawa Scale (NOS) to assess the risk of bias and methodological quality of the included studies (16). Studies scoring 0 to 3 points, 4 to 6 points, and 7 to 9 points were classified as low-, moderate- and high-quality studies, respectively. All studies were independently evaluated by two authors (LZ and BTH), and discrepancies were resolved by consensus or consultation with the third investigator (MC).
Data analysis
The outcomes were the mortality rate after myocardial infarction, according to the follow-up time, which can be divided into ≤30 days mortality, 1 to 3 years mortality, and 5 to 10 years mortality. There are also several effect sizes with different adjustment factors in the same study, and we chose the one with the most adjustment factors. The heterogeneity among studies was assessed using I2 statistics (17). Effect sizes were aggregated using fixed-effects or random-effects models according to the level of heterogeneity. Pooled estimates of odds ratios (ORs) with 95% confidence intervals were calculated to compare the unadjusted risk of mortality in migrants with natives, while pooled adjusted estimates of hazard ratios (HRs) with 95% confidence intervals were calculated to look at the adjusted risk of mortality in migrants with natives. Subgroup analysis was performed according to the region of the country of origin and the follow-up time, and all included mortality data were adjusted. The p value of statistical significance was set at 0.05. When I2 exceeded 50%, we considered heterogeneity significant, and a sensitivity analysis was performed to explore potential sources of heterogeneity, including country of birth and follow-up time. Publication bias was assessed using the Egger test. All analyses were performed in STATA software 17.0 (Stata Corporation, College Station, TX, USA).
Results
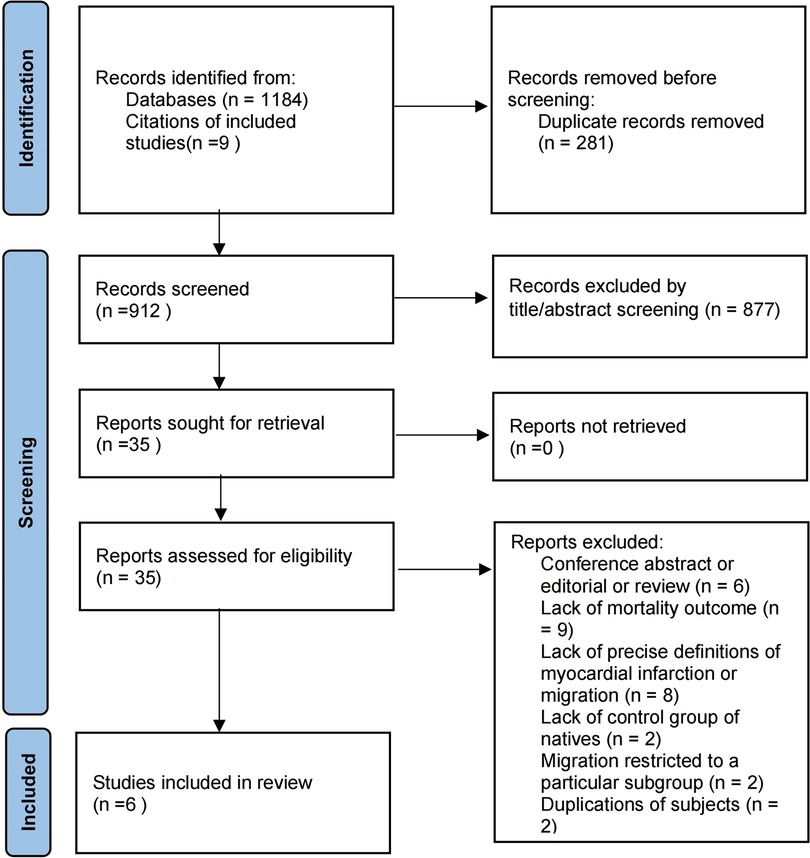
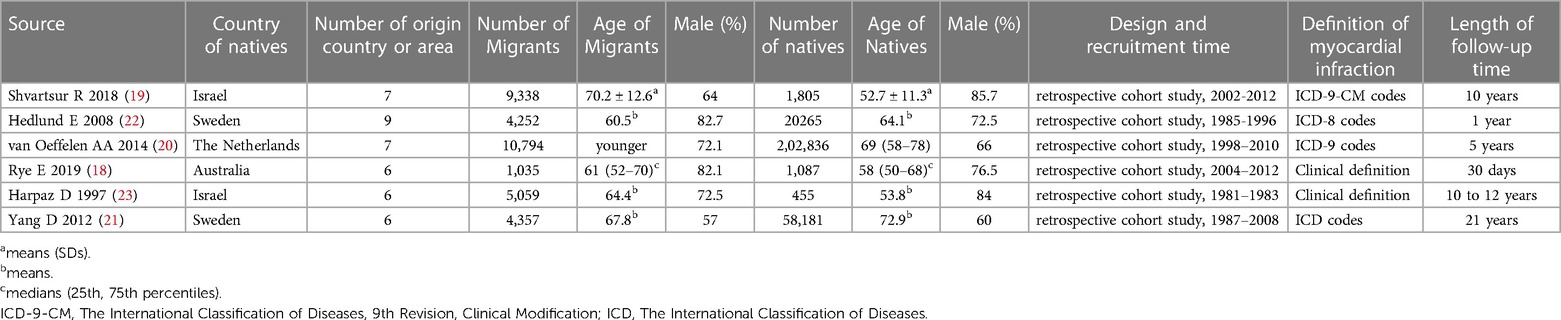
We identified 1,184 publications through the literature search and screened them, 281 of which were duplicates. A total of 903 articles and an additional 9 articles identified by manual searches for references of included studies were screened by title and abstract, of which 35 were included in full-text screening, and 6 studies finally met the inclusion criteria (18–23). The reasons for exclusion are classified and given in Figure 1.
Study characteristics and quality assessment
All included studies were conducted in high-income countries, including Israel (two studies), Sweden (two studies), The Netherlands, and Australia. These studies were published between 5 June 1997 and 22 August 2018, and included a total of 34,835 migrants (weighted average age is about 66.6 years old, and 69.7% male) and 284,629 natives (weighted average age is about 69.1 years old, and 65.4% male) with a recruitment period between 1981 and 2012, and migrants are mainly from Europe and Asia, and the weighted average follow-up time is about 8.1 years. The characteristics of the included studies are shown in Table 1. Using NOS to assess the quality of the 6 included studies, five studies (19–23) received a high-quality rating, and one study (18) received a moderate-quality rating. Overall, the qualities of the included studies were good. The detailed results table can be found in Supplementary Appendix S3.
Main results
Four studies (19, 20, 22, 23) provided an adjusted mortality rate, all including the adjustment factor of age, and the rest were gender, comorbidities, socioeconomic status, onset characteristics, year of event, etc. Mortality endpoint data with the longest follow-up time were selected in each study, and all mortality endpoints used in the adjusted analysis were followed up for more than 1 year. The pooled result showed that migrants had higher mortality after MI than natives (OR, 1.24; 95% CI, 1.10–1.39; I2 = 83.1%), see Figure 2. While unadjusted mortality data were extracted from all the 6 studies, the pooled result showed that there were no statistically significant differences in mortality after MI among migrants compared to natives (OR, 1.11; 95% CI, 0.69–1.79; I2 = 99.3%), see Figure 3.
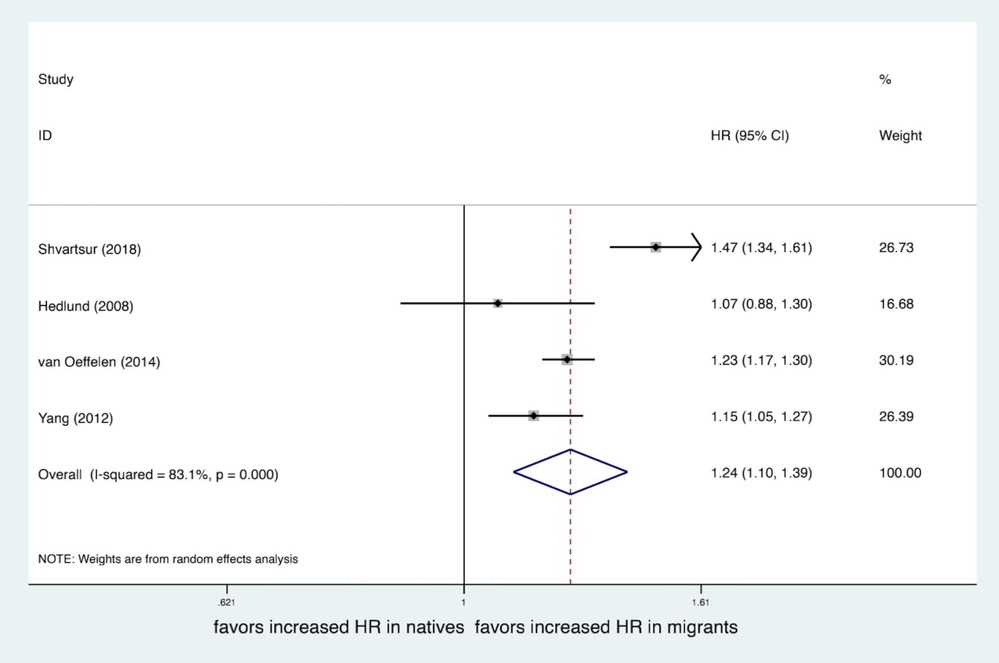
Figure 2. Forest plot of the adjusted hazard ratio (HR) of mortality after MI of migrants compared to natives.
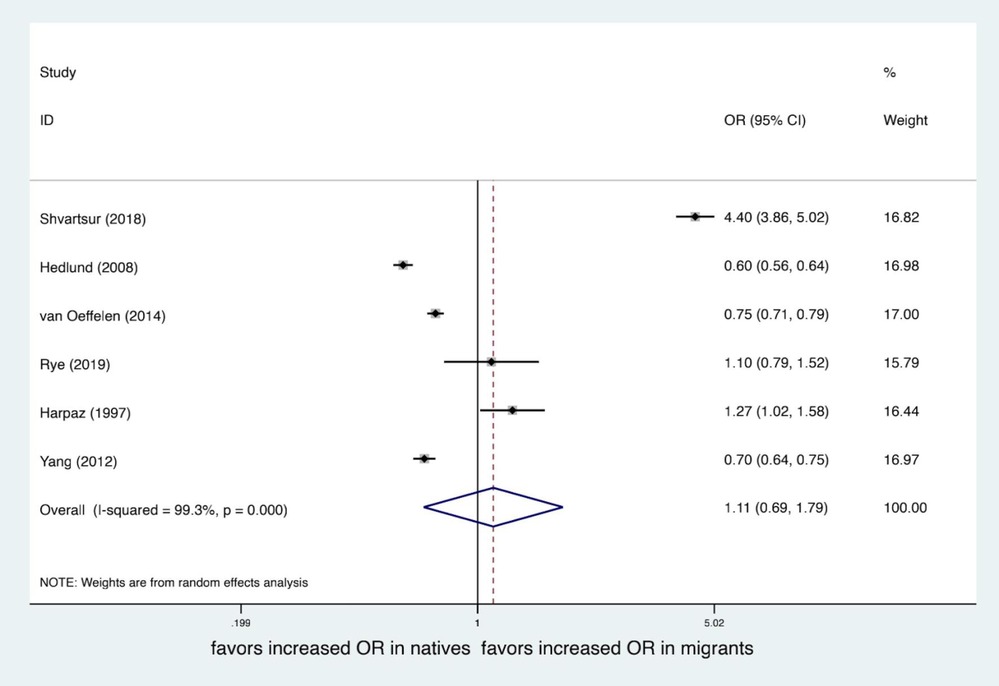
Figure 3. Forest plot of the unadjusted odds ratio (OR) of mortality after MI of migrants compared to natives.
Sensitivity analyses
The heterogeneity between the studies was relatively high, so we used a random effect model and performed a sensitivity analysis. We conducted subgroup analysis by follow-up time and country of birth and found that the area of origin may explain part of the high heterogeneity, and planned subgroup analyses by reason for migration, sex, and education were not practicable due to the lack of relevant data in most studies. For the meta-analysis of adjusted mortality, when the study by Shvartsur et al. was removed (19), heterogeneity was significantly lower (OR, 1.19; 95% CI, 1.11–1.27; I2 = 31.7%), and the complex diversity of the included migrant populations and their origins may also contribute to the high heterogeneity (Supplementary Appendix S4).
Results of the subgroup analysis
We performed a subgroup meta-analysis by the duration of follow-up. Four studies (19, 20, 22, 23) included in-hospital and 30-day mortality, 3 studies (19, 22, 23) included 1–3 years mortality, and 3 studies (19, 20, 23) included 5–10 years mortality. All included mortality data were adjusted. Pooled data showed 5–10 years mortality was significantly worse in migrants (OR, 1.27; 95% CI, 1.12–1.45; I2 = 86.8%), while there is no statistically significant differences in 30 days mortality (OR, 1.05; 95% CI, 0.87–1.27; I2 = 90.5%) and 1–3 years mortality (OR, 1.29; 95% CI, 0.96–1.72; I2 = 85.8%) between migrants and natives. There was high heterogeneity between the groups. See Figure 4.
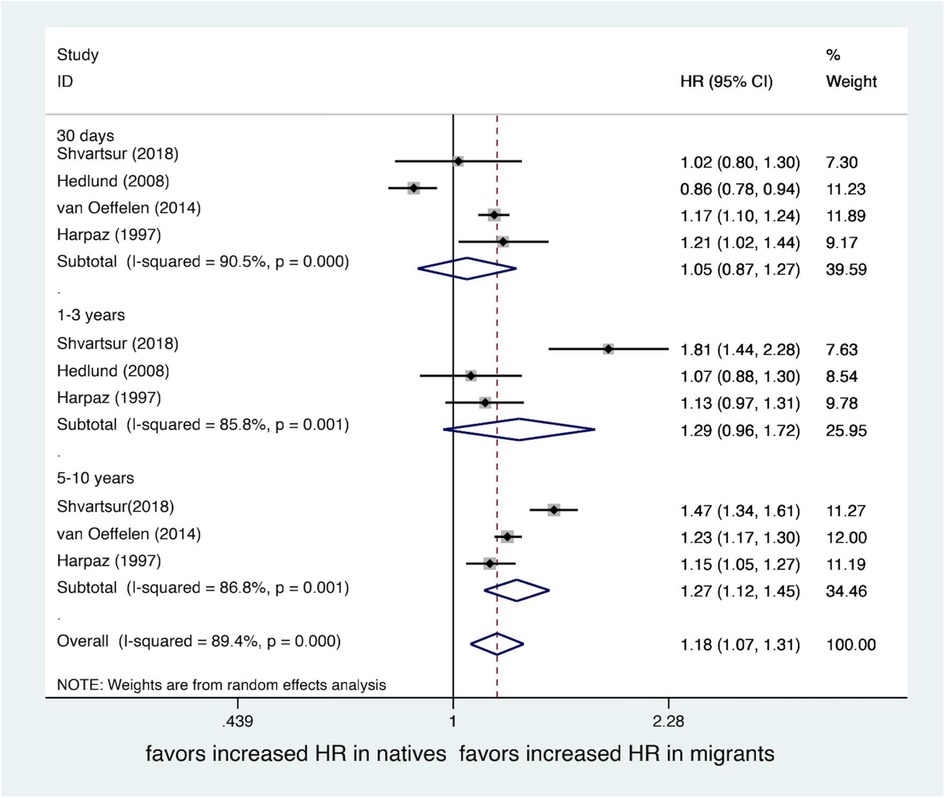
Figure 4. Forest plot of hazard ratio (HR) of mortality after MI of migrants compared with natives by follow-up time.
A subgroup meta-analysis by area of birthplace was also performed. 4 studies (19, 20, 22, 23) included migrants of European and Asian origin, 3 studies (19, 22, 23) included migrants of African origin, and 2 studies (20, 22) included migrants of Latin American origin. All the endpoints of mortality were adjusted, and we also selected the one with the longest follow-up time. Migrants from Europe (OR, 1.34; 95% CI, 1.16–1.55; I2 = 39%), Africa (OR, 1.50; 95% CI, 1.31–1.72; I2 = 0%), and Latin America (OR, 1.44; 95% CI, 1.30–1.60; I2 = 0%) had significantly higher rates of post-MI mortality than natives, with the exception of migrants of Asian origin (OR, 1.20; 95% CI, 0.99–1.46; I2 = 72.7%). The heterogeneity between groups was small, except for the Asian subgroup. See Figure 5.
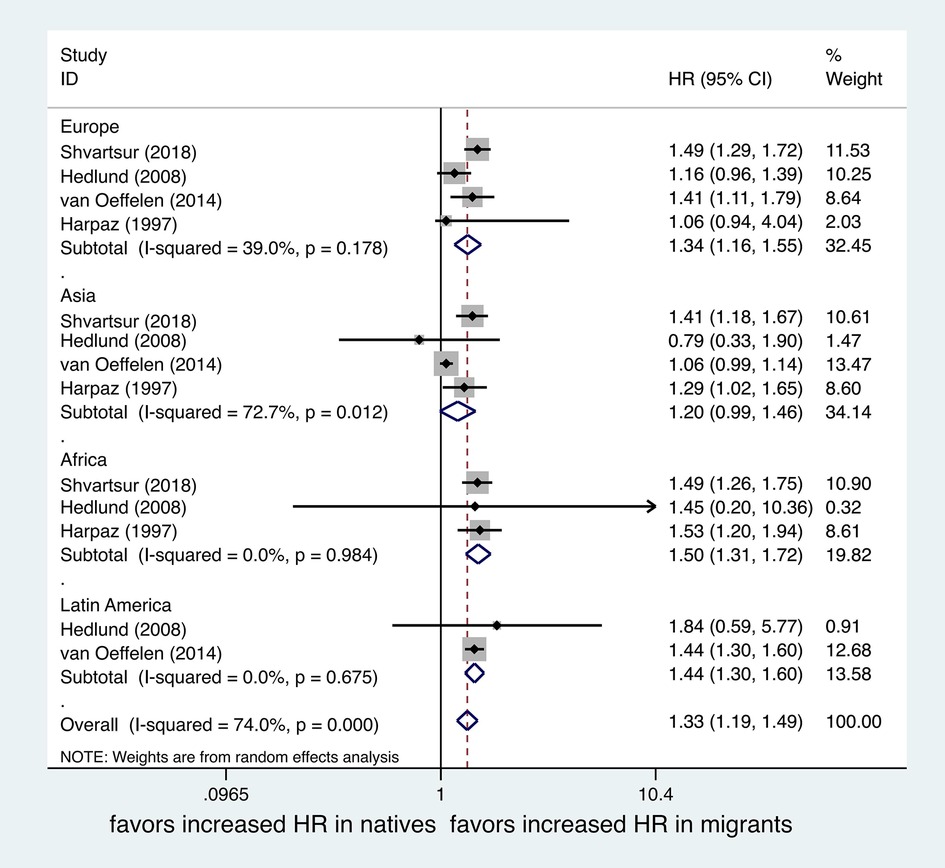
Figure 5. Forest plot of hazard ratio (HR) of mortality after MI of migrants compared with natives by area of birth.
Publication bias
Funnel plots, which are used to evaluate potential publishing biases, are usually displayed when more than ten studies are available and are not appropriate for meta-analysis which has a small number of eligible studies (24). Therefore, Egger's test was used and showed that there was no publication bias for the main unadjusted meta-analysis (Egger's test, p = 0.640 > 0.05) and the adjusted main meta-analysis (Egger's test, p = 0.870 > 0.05).
Discussion
To our knowledge, this systematic review and meta-analysis is the most comprehensive and first to compare outcomes after MI between migrants and natives. The analysis concluded the following main results: compared to natives with MI, the long-term all-cause mortality (1–10 y) after MI of the migrants was higher, possible reason is the social-economic disadvantages migrant faces accumulate overtime; while the short-term all-cause mortality (≤30 d) was not, possibly because the high quality and homogeneous in-hospital treatment and insufficient follow-up time.
Many studies have compared cardiovascular outcomes between migrants and natives, but there is still no consensus. A review showed that cardiovascular outcomes among migrants vary depending on factors such as country of origin, country of destination and duration of migration (25). For example, in Spain, migrants from Asia, the Caribbean and sub-Saharan Africa had higher CVD mortality compared with natives, whereas migrants from North Africa and South America had lower CVD mortality (26). Genetic predisposition, lifestyle, exposure to risk factors, early life factors, socioeconomic factors, etc. that are related to the background of the migrants' country of origin have a major impact on the health status of migrants and are important causes of health disparities between migrants and the native population, as well as between migrants of different origins (11, 25, 26). We therefore conducted a subgroup analysis by migrants' country of origin, which reduces some of the heterogeneity.
There are also many other factors that may affect the cardiovascular health and prognosis of migrants, such as some studies have proposed the health migration effect hypothesis that immigrants tend to be healthier than the general population in their country of origin due to a selection process in which individuals with better health and socioeconomic status are more likely to migrate, and the salmon bias effect that immigrants who experience health problems or illnesses are more likely to return to their home country for medical care or to be with their families, while healthier immigrants tend to stay in the host country, leading to an overestimation of migrant health in the host country (7–9, 27, 28). However, many studies have also found that migrants tend to have a lower socioeconomic status (29–31), greater psychological stress (32, 33), less social support (11), and limited access to health care resources (34, 35), among other disadvantages, and therefore poorer health. For example, some studies have shown a higher prevalence and mortality of cardiovascular disease among migrants (26, 36). As MI is a common and serious cardiovascular disease and a major cause of cardiovascular death, it is important to study its status and prognosis in immigrant populations, and as mentioned above, factors such as socioeconomic status have an important influence on acute MI, but there is insufficient evidence on the prognosis of migrants compared with natives after MI, so we focus on migrant populations in whom MI developed (37, 38).
The pooled adjusted short-term mortality rate did not show significant differences between migrants and natives, and there are several possible reasons for this. The first may be due to the major advances in the treatment of MI, evidence shows that migrants do not differ from natives in terms of key in-hospital treatments, including rates of reperfusion therapy and door-to-balloon time, and no significant differences were observed in length of hospital stay, in-hospital complications, or mortality (18, 39–42). Although migrants are disadvantaged in terms of socioeconomic factors and psychological distress, high quality and homogeneous in-hospital care reduces these disparities, and the short follow-up period may not be sufficient to show a difference in the short-term prognosis of migrants compared to natives. On the other hand, the healthy migration effect observed in many studies from North America to Europe, supported by evidence ranging from physical health to mental health, suggests that the migrant group is a selected healthier group and may contribute positively to the prognosis of migrants, especially at the early stage (43–45). However, only patients who were admitted to the hospital were enrolled, ignoring those who did not present to the hospital after MI, and previous studies suggest that migrants may receive inferior pre-hospital care, which may underestimate short-term mortality of migrants (46, 47).
When the follow-up period was extended, the pooled data showed that the mortality rate of migrants was significantly higher than that of natives. Most migrants move to more developed areas, which also means that they tend to have poorer socioeconomic conditions and health awareness (11, 29–31, 48), and studies have shown that individuals with low socioeconomic status often bear a greater burden of CVD and are more likely to have a higher incidence of MI and poorer outcomes (37, 38). There are large number of studies have also shown that despite migrants receiving similar rates of reperfusion therapy as natives, there is often a delay in the time to treatment, with a study in Singapore showing significantly longer symptom-to-balloon times in migrant patients (40), another study in Australia showing that migrant patients spend longer time in emergency care (49), and several studies in the US showing that migrant patients spend longer in the time from symptom onset to door and door to balloon than natives (50, 51). At the same time, migrating to a new environment introduces barriers such as language and culture, which make migrant groups less likely to seek specialized medical care, less likely to communicate with doctors, and less likely to receive the standard of optimal drug treatment recommended by the guidelines and less likely to adhere to treatment (20, 52, 53). Furthermore, the advantages of the healthy migrant effect in migrants disappear over time, often 5–10 years after immigration, and the health status of migrants is equal to or worse than that of natives (7, 43, 54). For example, cultural adaptation leads to lifestyle changes, including changes in physical activity levels and diet, resulting in increased rates of hypertension, obesity, and diabetes in migrants (55), which are traditional risk factors for MI. Over time, the adverse effects of these disadvantages accumulate, leading to a poorer prognosis for migrants compared to natives.
Strengths and limitations
This study aggregates existing data to complement evidence on the risk of mortality after MI in migrants compared to natives and draws interesting conclusions that inform future research and provide a basis for more targeted health policies. At the same time, the migrant groups included in this study cover a wide range of source regions and are representative to some extent. Furthermore, data from all patients were obtained from medical records, and the follow-up endpoint was all-cause mortality, so there is a high precision of the data.
There are some limitations to consider. First, all included studies were conducted in developed countries, and therefore, the conclusions are not representative of less developed countries and regions. Second, the follow-up endpoint is only death, and while improving precision, it lacks other important indicators, such as the occurrence of MACE (major adverse cardiovascular event) and quality of life; also, it cannot be ruled out that all-cause death may have been disturbed by confounding factors other than MI. Next, all studies included in the analysis were retrospective, and prospective studies in this area are needed in future research. Last, the heterogeneity between studies was very large, although the heterogeneity of subgroup analysis by region of origin was significantly reduced, more detailed data are lacking to further explore the source of heterogeneity. However, these limitations will not affect the need of strengthening our focus on the health of migrants.
Conclusions
In this systematic review and meta-analysis, we summarize the existing research data and conclude that the mortality risk of migrants is higher than that of natives in the long term after MI. Given the large number of migrants and the significant burden of MI, this study is important and highlights the need to improve the cardiovascular health of migrants and reduce health inequities. More researches are needed to explore the differences between migrants and natives in more cardiovascular diseases and the underlying mechanisms, especially among migrants who already develop diseases.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
LZ and BTH conceived the study, designed the study forms and searched the literature. All authors screened the studies for inclusion and extracted data. LZ analyzed the data. All authors drafted and revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Natural Science Foundation of China (82170375).
Acknowledgments
We thank Yuehong Chen (MD, Ph.D., Department of Rheumatology & Immunology, West China Hospital, Sichuan University, Chengdu, PR China) for useful advice on the study concept and analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1101386/full#supplementary-material.
References
1. Collaborators GDaI. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396(10258):1204–22. doi: 10.1016/s0140-6736(20)30925-9
2. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the gbd 2019 study. J Am Coll Cardiol. (2020) 76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010
3. Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. (2014) 371(9):818–27. doi: 10.1056/NEJMoa1311890
4. United Nations Department of Economic and Social Affairs PD. International Migration 2020 Highlights (St/Esa/Ser.A/452). (2020). https://www.un.org/development/desa/pd/news/international-migration-2020 (Accessed November 15, 2022) (2020).
5. Agyemang C, van den Born BJ. Cardiovascular health and disease in migrant populations: a call to action. Nat Rev Cardiol. (2022) 19(1):1–2. doi: 10.1038/s41569-021-00644-y
6. Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. Lancet. (2013) 381(9873):1235–45. doi: 10.1016/s0140-6736(12)62086-8
7. Wallace M, Khlat M, Guillot M. Mortality advantage among migrants according to duration of stay in France, 2004–2014. BMC Public Health. (2019) 19(1):327. doi: 10.1186/s12889-019-6652-1
8. Lu Y, Qin L. Healthy migrant and salmon bias hypotheses: a study of health and internal migration in China. Soc Sci Med. (2014) 102:41–8. doi: 10.1016/j.socscimed.2013.11.040
9. Lu Y. Test of the “healthy migrant hypothesis”: a longitudinal analysis of health selectivity of internal migration in Indonesia. Soc Sci Med. (2008) 67(8):1331–9. doi: 10.1016/j.socscimed.2008.06.017
10. Hargreaves S, Rustage K, Nellums LB, McAlpine A, Pocock N, Devakumar D, et al. Occupational health outcomes among international migrant workers: a systematic review and meta-analysis. Lancet Glob Health. (2019) 7(7):e872–e82. doi: 10.1016/s2214-109x(19)30204-9
11. Sohail QZ, Chu A, Rezai MR, Donovan LR, Ko DT, Tu JV. The risk of ischemic heart disease and stroke among immigrant populations: a systematic review. Can J Cardiol. (2015) 31(9):1160–8. doi: 10.1016/j.cjca.2015.04.027
12. Aldridge RW, Nellums LB, Bartlett S, Barr AL, Patel P, Burns R, et al. Global patterns of mortality in international migrants: a systematic review and meta-analysis. Lancet. (2018) 392(10164):2553–66. doi: 10.1016/s0140-6736(18)32781-8
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The prisma 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
14. Baumeister A, Aldin A, Chakraverty D, Monsef I, Jakob T, Seven US, et al. Interventions for improving health literacy in migrants. Cochrane Database Syst Rev. (2019) 4:CD013303. doi: 10.1002/14651858.CD013303
15. Cabello JB, Burls A, Emparanza JI, Bayliss SE, Quinn T. Oxygen therapy for acute myocardial infarction. Cochrane Database Syst Rev. (2016) 12:CD007160. doi: 10.1002/14651858.CD007160.pub4
16. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (nos) for assessing the quality of nonrandomised studies in meta-analyses. 3rd Symp Syst Rev. (2000):15. Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed April 26 2023).
17. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327(7414):557–60. doi: 10.1136/bmj.327.7414.557
18. Rye E, Lee A, Mukhtar H, Narayan A, Robert Denniss A, Chow C, et al. St-Elevation myocardial infarction in a migrant population: a registry-based study of patient treatment and outcomes. Intern Med J. (2019) 49(4):502–12. doi: 10.1111/imj.14084
19. Shvartsur R, Shiyovich A, Gilutz H, Azab AN, Plakht Y. Short and long-term prognosis following acute myocardial infarction according to the country of origin. Soroka acute myocardial infarction ii (sami ii) project. Int J Cardiol. (2018) 259:227–33. doi: 10.1016/j.ijcard.2018.02.079
20. van Oeffelen AA, Agyemang C, Stronks K, Bots ML, Vaartjes I. Prognosis after a first hospitalisation for acute myocardial infarction and congestive heart failure by country of birth. Heart. (2014) 100(18):1436–43. doi: 10.1136/heartjnl-2013-305444
21. Yang D, Dzayee DA, Beiki O, de Faire U, Alfredsson L, Moradi T. Incidence and case fatality after day 28 of first time myocardial infarction in Sweden 1987–2008. Eur J Prev Cardiol. (2012) 19(6):1304–15. doi: 10.1177/1741826711425340
22. Hedlund E, Pehrsson K, Lange A, Hammar N. Country of birth and survival after a first myocardial infarction in Stockholm, Sweden. Eur J Epidemiol. (2008) 23(5):341–7. doi: 10.1007/s10654-008-9240-8
23. Harpaz D. Ethnic differences in mortality of male and female patients surviving acute myocardial infarction: long-term follow-up of 5,700 patients. The secondary prevention reinfarction Israeli nifedipine trial (sprint) study group. Eur J Epidemiol. (1997) 13(7):745–54. doi: 10.1023/a:1007400419922
24. Page MJ, Higgins JPT, Sterne JAC. Chapter 13: assessing risk of bias due to missing results in a synthesis. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane (2022). Available at: www.training.cochrane.org/handbook.
25. Agyemang C, van den Born BJ. Non-communicable diseases in migrants: an expert review. J Travel Med. (2019) 26(2):tay107. doi: 10.1093/jtm/tay107
26. Dassanayake J, Gurrin L, Payne WR, Sundararajan V, Dharmage SC. Cardiovascular disease risk in immigrants: what is the evidence and where are the gaps? Asia Pac J Public Health. (2011) 23(6):882–95. doi: 10.1177/1010539509360572
27. Ruiz JM, Steffen P, Smith TB. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. Am J Public Health. (2013) 103(3):e52–60. doi: 10.2105/ajph.2012.301103
28. Razum O, Zeeb H, Rohrmann S. The “healthy migrant effect”–not merely a fallacy of inaccurate denominator figures. Int J Epidemiol. (2000) 29(1):191–2. doi: 10.1093/ije/29.1.191
29. Wang Y, Jing Z, Ding L, Tang X, Feng Y, Li J, et al. Socioeconomic inequity in inpatient service utilization based on need among internal migrants: evidence from 2014 national cross-sectional survey in China. BMC Health Serv Res. (2020) 20(1):984. doi: 10.1186/s12913-020-05843-w
30. Li X, Deng L, Yang H, Wang H. Effect of socioeconomic status on the healthcare-seeking behavior of migrant workers in China. PLoS One. (2020) 15(8):e0237867. doi: 10.1371/journal.pone.0237867
31. Shao C, Meng X, Cui S, Wang J, Li C. Income-related health inequality of migrant workers in China and its decomposition: an analysis based on the 2012 China labor-force dynamics survey data. J Chin Med Assoc. (2016) 79(10):531–7. doi: 10.1016/j.jcma.2016.02.009
32. Li Z, Dai J, Wu N, Gao J, Fu H. The mental health and depression of rural-to-urban migrant workers compared to non-migrant workers in Shanghai: a cross-sectional study. Int Health. (2019) 11(S1):S55–s63. doi: 10.1093/inthealth/ihz081
33. Lin D, Li X, Wang B, Hong Y, Fang X, Qin X, et al. Discrimination, perceived social inequity, and mental health among rural-to-urban migrants in China. Community Ment Health J. (2011) 47(2):171–80. doi: 10.1007/s10597-009-9278-4
34. Xi S, Song Y, Li X, Li M, Lu Z, Yang Y, et al. Local-migrant gaps in healthcare utilization between older migrants and local residents in China. J Am Geriatr Soc. (2020) 68(7):1560–7. doi: 10.1111/jgs.16421
35. Zhang J, Lin S, Liang D, Qian Y, Zhang D, Hou Z. Public health services utilization and its determinants among internal migrants in China: evidence from a nationally representative survey. Int J Environ Res Public Health. (2017) 14(9):1002. doi: 10.3390/ijerph14091002
36. Agyemang C, de-Graft Aikins A, Bhopal R. Ethnicity and cardiovascular health research: pushing the boundaries by including comparison populations in the countries of origin. Ethn Health. (2012) 17(6):579–96. doi: 10.1080/13557858.2012.730607
37. Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. (2018) 137(20):2166–78. doi: 10.1161/circulationaha.117.029652
38. Hanley GE, Morgan S, Reid RJ. Income-Related inequity in initiation of evidence-based therapies among patients with acute myocardial infarction. J Gen Intern Med. (2011) 26(11):1329–35. doi: 10.1007/s11606-011-1799-1
39. Bansal E, Ozunaki T, Tun H, Shavelle D. Hispanic patients undergoing primary pci within Los Angeles county stemi receiving system. JACC. (2014) 7:S12–S3. doi: 10.1016/j.jcin.2014.01.014
40. Lee CH, Choo H, Tai BC, Chan MY, Phua QH, Low TT, et al. Immigrant status and disparities in health care delivery in patients with myocardial infarction. Int J Cardiol. (2013) 166(3):696–701. doi: 10.1016/j.ijcard.2011.11.103
41. Abdelnoor M, Eritsland J, Brunborg C, Halvorsen S. Ethnicity and acute myocardial infarction: risk profile at presentation, access to hospital management, and outcome in Norway. Vasc Health Risk Manag. (2012) 8:505–15. doi: 10.2147/vhrm.S33627
42. Jacobi JA, Parikh SV, McGuire DK, Delemos JA, Murphy SA, Keeley EC. Racial disparity in clinical outcomes following primary percutaneous coronary intervention for st elevation myocardial infarction: influence of process of care. J Interv Cardiol. (2007) 20(3):182–7. doi: 10.1111/j.1540-8183.2007.00263.x
43. Helgesson M, Johansson B, Nordquist T, Vingård E, Svartengren M. Healthy migrant effect in the Swedish context: a register-based, longitudinal cohort study. BMJ Open. (2019) 9(3):e026972. doi: 10.1136/bmjopen-2018-026972
44. Salas-Wright CP, Vaughn MG, Goings TC, Miller DP, Schwartz SJ. Immigrants and mental disorders in the United States: new evidence on the healthy migrant hypothesis. Psychiatry Res. (2018) 267:438–45. doi: 10.1016/j.psychres.2018.06.039
45. Blair AH, Schneeberg A. Changes in the “healthy migrant effect” in Canada: are recent immigrants healthier than they were a decade ago? J Immigr Minor Health. (2014) 16(1):136–42. doi: 10.1007/s10903-013-9813-9
46. Wechkunanukul KH, Ullah S, Beilby J. Variation in seeking care for cardiovascular disease and ambulance utilization among migrants in Australia: time, ethnicity, and delay (ted) study iii. Int J Environ Res Public Health. (2022) 19(3):1516. doi: 10.3390/ijerph19031516
47. Mahajan S, Valero-Elizondo J, Khera R, Desai NR, Blankstein R, Blaha MJ, et al. Variation and disparities in awareness of myocardial infarction symptoms among adults in the United States. JAMA Netw Open. (2019) 2(12):e1917885. doi: 10.1001/jamanetworkopen.2019.17885
48. Giannoni M, Franzini L, Masiero G. Migrant integration policies and health inequalities in Europe. BMC Public Health. (2016) 16:463. doi: 10.1186/s12889-016-3095-9
49. Wechkunanukul K, Grantham H, Teubner D, Hyun KK, Clark RA. Presenting characteristics and processing times for culturally and linguistically diverse (cald) patients with chest pain in an emergency department: time, ethnicity, and delay (ted) study ii. Int J Cardiol. (2016) 220:901–8. doi: 10.1016/j.ijcard.2016.06.244
50. Guzman LA, Li S, Wang TY, Daviglus ML, Exaire J, Rodriguez CJ, et al. Differences in treatment patterns and outcomes between hispanics and non-hispanic whites treated for st-segment elevation myocardial infarction: results from the ncdr action registry-gwtg. J Am Coll Cardiol. (2012) 59(6):630–1. doi: 10.1016/j.jacc.2011.10.882
51. Bradley EH, Herrin J, Wang Y, McNamara RL, Webster TR, Magid DJ, et al. Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. Jama. (2004) 292(13):1563–72. doi: 10.1001/jama.292.13.1563
52. Peled Y. Language barriers and epistemic injustice in healthcare settings. Bioethics. (2018) 32(6):360–7. doi: 10.1111/bioe.12435
53. Hempler NF, Diderichsen F, Larsen FB, Ladelund S, Jørgensen T. Do immigrants from Turkey, Pakistan and Yugoslavia receive adequate medical treatment with Beta-blockers and statins after acute myocardial infarction compared with Danish-born residents? A register-based follow-up study. Eur J Clin Pharmacol. (2010) 66(7):735–42. doi: 10.1007/s00228-010-0816-3
54. Fuller-Thomson E, Noack AM, George U. Health decline among recent immigrants to Canada: findings from a nationally-representative longitudinal survey. Can J Public Health. (2011) 102(4):273–80. doi: 10.1007/bf03404048
Keywords: myocardial infraction, migrant, mortality, prognosis, meta analysis
Citation: Zhu L, Huang B-t and Chen M (2023) The mortality risk after myocardial infraction in migrants compared with natives: a systematic review and meta-analysis. Front. Cardiovasc. Med. 10:1101386. doi: 10.3389/fcvm.2023.1101386
Received: 17 November 2022; Accepted: 17 April 2023;
Published: 24 May 2023.
Edited by:
Tiejun Tong, Hong Kong Baptist University, Hong Kong SAR, ChinaReviewed by:
Niya Mileva, Aleksandrovska University Hospital, BulgariaLiam Butler, Wake Forest University, United States
Sivabaskari Pasupathy, University of Adelaide, Australia
© 2023 Zhu, Huang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bao-tao Huang YmFvdGFvLmh1YW5nQGZveG1haWwuY29t Mao Chen aG1hb2NoZW5AdmlwLnNpbmEuY29t
 Lei Zhu
Lei Zhu Bao-tao Huang
Bao-tao Huang Mao Chen
Mao Chen