
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Cardiovasc. Med. , 06 July 2023
Sec. Coronary Artery Disease
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1096265
This article is part of the Research Topic The Clinical Use of Coronary Functional Test in Coronary Artery Disease View all 7 articles
 Nissi Suppogu1,†
Nissi Suppogu1,† Benita Tjoe1,†
Benita Tjoe1,† Janet Wei2
Janet Wei2 Jenna Maughan2
Jenna Maughan2 Sandy Joung2
Sandy Joung2 Odayme Quesada3
Odayme Quesada3 Chrisandra L. Shufelt2
Chrisandra L. Shufelt2 Bruce Samuels2
Bruce Samuels2 Babak Azarbal2
Babak Azarbal2 C. Noel Bairey Merz2*
C. Noel Bairey Merz2*
Women with signs and symptoms of ischemia and no obstructive coronary artery disease (INOCA) often have coronary microvascular dysfunction (CMD). It can be diagnosed by coronary function testing (CFT), which is an invasive coronary angiogram procedure. Frequently, these women have persistent angina despite medical therapy, but it is not clear whether it is due to worsening or persistent CMD or inadequate therapy. In this brief report, we describe findings of repeat CFT in a case series of 12 women undergoing repeat CFT for the assessment of persistent angina in order to better understand the evolving pathology.
More women compared to men have non-obstructive coronary artery disease (CAD); about two-thirds of women with signs and symptoms of ischemia have non-obstructive CAD and often have coronary microvascular dysfunction (CMD) (1). Ischemia with non-obstructive coronary artery disease (INOCA) is not a benign condition as these patients are at increased risk for major adverse cardiovascular events (MACE) including heart failure and myocardial infarction at long-term follow-up (2). CMD can be diagnosed by coronary function testing (CFT), an invasive angiographic procedure using vasoactive substances to assess and delineate pathways of microvascular dysfunction including coronary flow reserve (CFR), a non endothelial dependent pathway, and coronary blood flow (CBF), an endothelial independent microvascular pathway (3). Medical therapy targeted towards abnormal CFT pathways has been shown to improve angina and quality of life at 1-year follow-up (4). We hypothesized that repeat CFT may help better our understanding of pathophysiological progression of abnormal pathways in CMD while the patients are on therapeutics and have ongoing symptoms. This may further help with management options. In this brief retrospective case report, we studied 12 women who were diagnosed initially with invasive CFT and found to have CMD who then underwent clinically ordered repeat testing for further evaluation of persistent angina despite medical management, with subsequent pathway findings and treatment outcomes.
Among 280 women and men at a single tertiary center enrolled in a registry, 12 (4.3%) women underwent repeat CFT per previously published methods in the women's ischemia syndrome evaluation (WISE) studies (3, 5). Long-acting calcium channel blockers (CCB) were held for 48 h while short-acting CCB, angiotensin-converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARBs), beta blockers (1), and long-acting nitrates were held for 24 h and sublingual nitroglycerin for 4 h per-procedurally. Non-obstructive CAD (<50% stenosis) was confirmed and function testing was then performed using a Doppler FloWire (Philips Volcano) in the left anterior descending artery (3). Non-endothelial dependent microvascular dysfunction was defined as a coronary flow reserve (CFR) ≤2.32 to graded doses of 18 mg and 100 mg of intracoronary (IC) adenosine, a threshold associated with elevated risk of MACE as seen in several WISE studies (6, 7). Endothelial dependent microvascular dysfunction was defined as ≤50% increase in coronary blood flow (CBF) to IC acetylcholine (ACH). Both abnormal CFR and abnormal CBF have been shown to have adverse outcomes with elevated risk of MACE (7). Endothelial dependent macrovascular dysfunction was defined as ≤0% increase in coronary artery diameter to 36.4 mcg of IC ACH. Epicardial vasospasm was defined as >75% vasoconstriction to ACH compared to coronary artery diameter post-nitroglycerin, with chest pain and ECG changes. Non-endothelial dependent macrovascular dysfunction was defined as <20% increase in coronary diameter to IC nitroglycerin (3). Angina was assessed using the Seattle Angina Questionnaire (SAQ) following the initial and repeat CFT. Statistical tests were paired t tests. A significance level of 0.05 was used for all tests.
At baseline, mean group age was 52 ± 10.5 years with 75% post-menopausal women, all were nonsmokers, 17% diabetic, 25% hypertension and 25% hyperlipidemia. Median time between initial CFT and follow-up CFT was 8 years (range 2–11). At repeat CFT, all patients remained with non-obstructive atherosclerosis and no new diagnosis of diabetes, hypertension, or smoking. Findings of initial and repeat micro- and macrovascular CMD pathways are shown (Table 1). At baseline CFT, 92% of patients had abnormal CFR ≤ 2.32 compared to 50% at follow-up, with a significant overall improvement (2.27 ± 0.55–2.93 ± 0.72, respectively; p = 0.03) (Figure 1). Increase in CBF was 41.9% ± 44.2% at baseline compared to 64.6% ± 67.2% at repeat testing (p = 0.33). Other pathways did not show a significant improvement (Figure 1). Two patients were found to have epicardial vasospasm on the repeat CFT that was not observed on initial testing. Heart rate and blood pressure readings were not significantly different at the time of initial and repeat CFT as shown (Table 2).
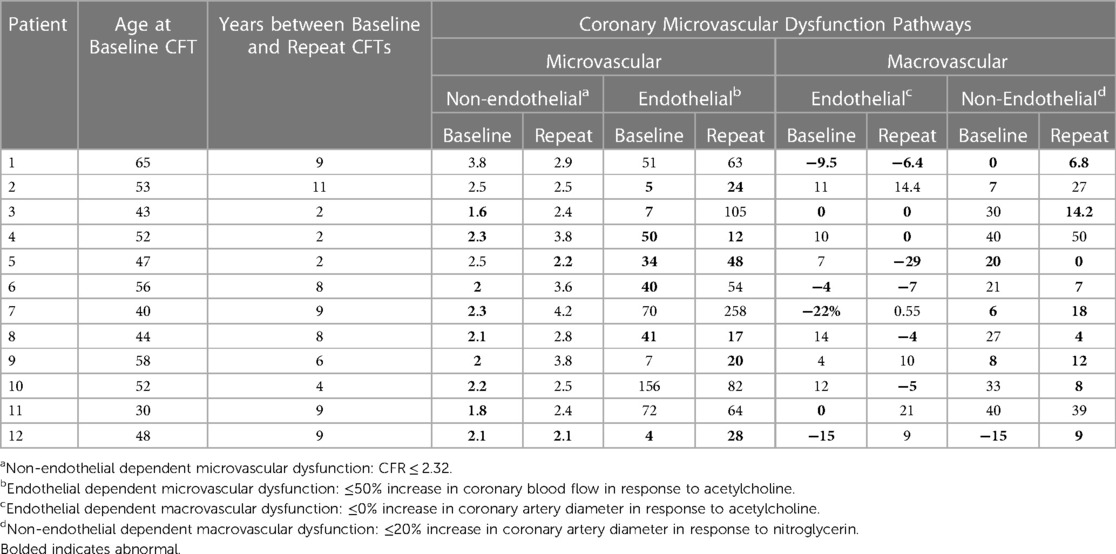
Table 1. Coronary microvascular dysfunction (CMD) pathways at baseline and repeat coronary function testing (CFT).
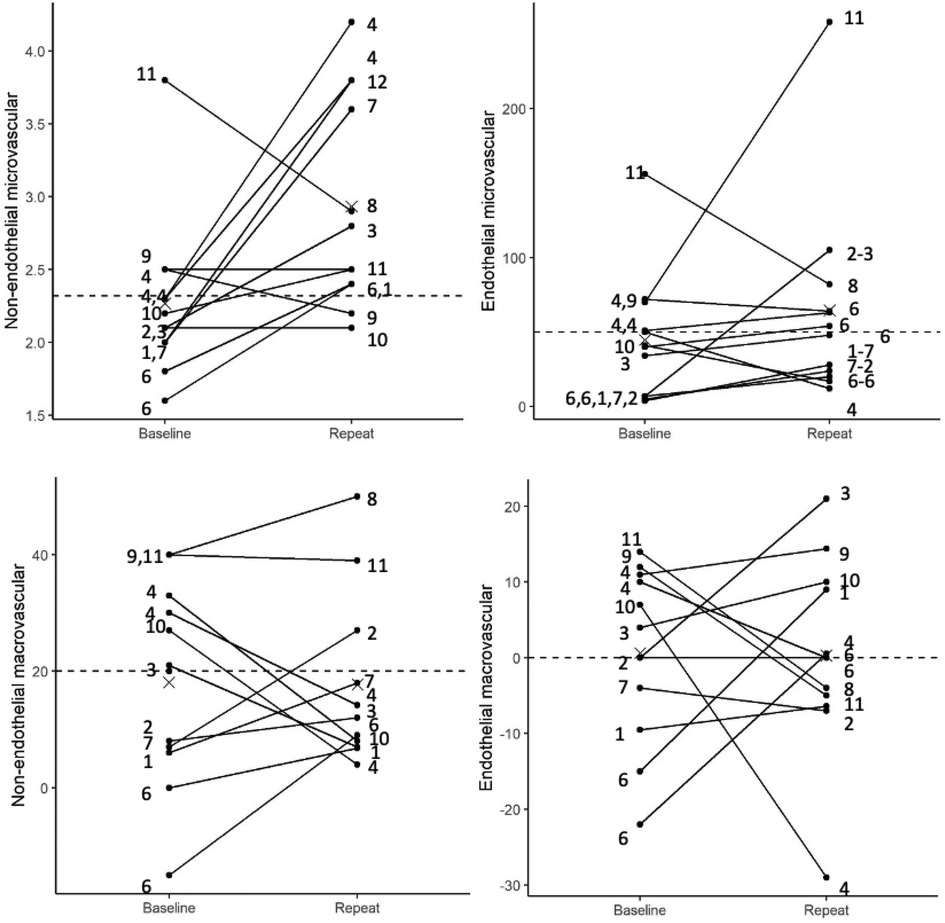
Figure 1. Interaction plot showing baseline CFT pathways and their end points at repeat over a period of time. Numbers on the left of the individual plots indicate combination of medication's patients were on before the initial CFT and numbers on the right of the plot indicate the combination of medication patients were on at the time of the repeat CFT. 1, aspirin and statins; 2, aspirin, statins, calcium channel blockers; 3, aspirin, statins, calcium channel blockers and nitro; 4, aspirin, statin, betablocker, nitro; 5, aspirin, statins, betablockers, nitro, ranexa; 6, statins; 7, statin, betablockers, calcium channel blockers; 8, statins, betablocker, ranexa; 9, statins, betablocker, nitro, ranexa; 10, statin, calcium channel blockers and nitro; 11, betablocker, nitro and ranexa.
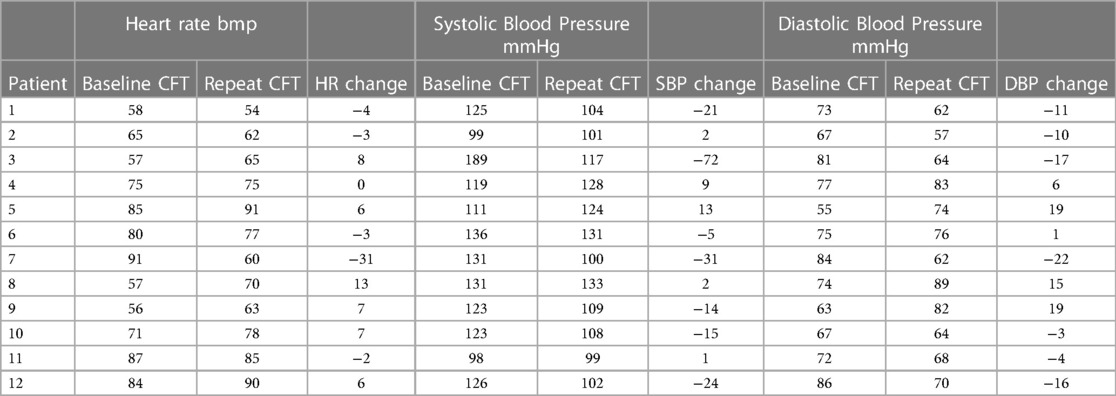
Table 2. Herat rate and blood pressure (systolic and diastolic) at the time of initial and repeat coronary function testing.
Following the initial CFT, 58% of patients were initiated on ACEi/ARBs or BB, while 50% were initiated on nitrates. At the time of repeat CFT, 92% of the twelve patients were being treated with a statin, 92% with an antiplatelet agent, 58% with BB, 58% with nitrates, 50% with ACEi/ARB, 33% with CCB and 25% with ranolazine. All patients with improved CFR were either on statin/BB or ACEi prior to repeat CFT (Table 3) (Figure 2).
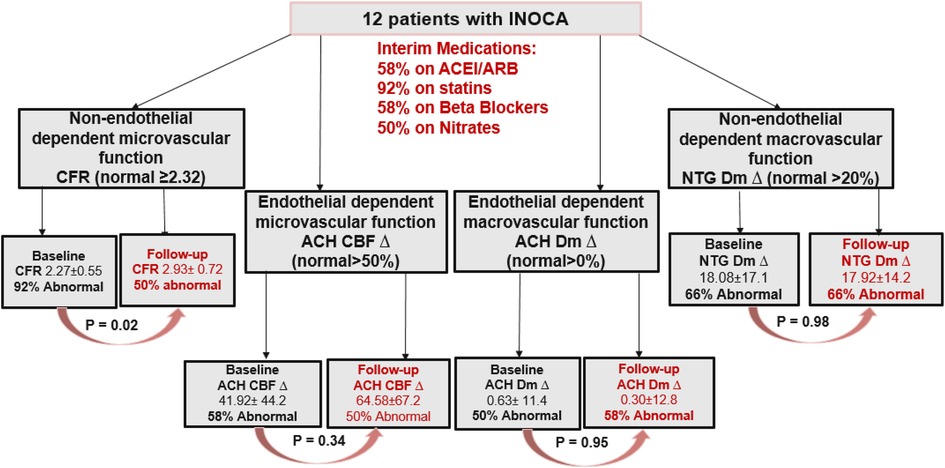
Figure 2. Flow chart of the case series identifying CMD pathway at baseline and at repeat CFT along with the significant changes in percentages in each of the pathways involved. INOCA, ischemia with non-obstructive coronary artery disease; CFR, coronary flow reserve; ACH, acetylcholine; CBF, coronary blood flow; Dm, diameter; NTG, nitroglycerin; ACEi, angiotensin converting enzyme inhibitor; ARB, angiotensin II receptor blocker.
At baseline CFT, the mean SAQ score was 40.1 ± 9.5. It showed a trend towards improvement at repeat to 53.5 ± 3.10 (p = 0.08). Amongst the SAQ domains, there was a trend toward improvement in treatment satisfaction from 69 ± 17.6 to 84 ± 13.5 (p = 0.096). There was also a significant improvement in disease perception from 33 ± 17.8 to 50 ± 24.2 (p = 0.001). There was no significant improvement in angina stability (p = 0.71), angina frequency (p = 0.28), and physical limitation (p = 0.57) scores.
To our knowledge, this is the first case report examining repeat coronary function testing for reassessment of CMD in women with persistent angina. Overall, there was significant improvement in CFR on repeat testing (p = 0.02) that is noteworthy in the context of studies demonstrating a worsening of CFR with age. Notably, this cohort of women reported persistent symptoms (8). In many patients, CFT revealed persistent abnormalities in both macro- and microvascular endothelial function and newly diagnosed epicardial vasospasm spasm in 2 of the 12 cases that may be the culprit of ongoing angina.
Targeted medical management of CMD aims to treat the underlying pathophysiology and pathway of dysfunction (2). Statins have been shown to have both anti-atherosclerotic and anti-inflammatory properties and improve CFR (9). A greater atherosclerotic burden has been observed in patients with CMD, progressing and possibly leading to obstructive CAD over 10 years (10). It can be seen that the majority of our patients (92%) were on statins and had minimal progression of atherosclerosis and also an improvement in CFR.
ACEi therapy for CMD patients is associated with improved symptoms and outcomes, likely driven by improved endothelial function and microvascular tone (11). Only 50% of our patients were on ACEi/ARBs at follow-up, as they had either side effects or low blood pressure limiting therapy, and there was not a significant improvement in CBF at follow-up. CCBs have shown to improve microvascular tone and epicardial vasospasm (11). Ranolazine has been shown to improve angina in women with low CFR (12). For patients with abnormal nociception, TCAs may improve angina likely via visceral analgesic effects (11).
Repeat CFT findings helped guide therapeutic alterations to specified abnormal pathways in a few patients in this small case series. In patients with more observed atherosclerosis, the statin dose was increased. In those with persistent constrictive abnormalities consistent with endothelial dysfunction, ACEi/ARBs were preferentially initiated. In patients with newly observed vasospasm, dual CCB therapy and as needed nitrates were favored for vasodilation. Repeat CFT in our case series also helped in delineation of pathways over a period of time, which is particularly useful in patients with physiological limitations and intolerance to existing therapies. For example, it helped us look further into patients with low blood pressure that may limit anti-hypertensive therapy and help utilize other drug classes. At any given time, the patients with improvement in CFR were either on statins, beta blockers, or ACEi, possibly influencing the improvement in microvascular function in a positive way.
The observed improvement in overall SAQ and significant improvement in treatment satisfaction highlights also that targeted management informed by invasive CFT findings can improve patient reported outcomes. This is consistent with findings from the randomized controlled CorMicA trial which demonstrated that stratified therapy as guided by CFT improves angina and quality of life, compared to standard care following a sham invasive diagnostic procedure (4). It was also evident in our case analyses that many of these patients underwent several non-invasive stress tests both prior to initial CFT and at times between the repeated CFTs. There are different modalities of testing, such as PET, cardiac MRI, and echo doppler, that can diagnose CMD; however, these imaging modalities are surrogates of flow only and need special expertise and equipment as well (13). While these tests can provide useful information regarding ischemia and functional capacity, repeated testing may warrant unnecessary healthcare costs and yield limited findings to guide management.
This is a small retrospective analysis of 12 patients with CMD and further limited to women. Protocol change was seen from initial to repeat testing at times—several women did not participate in vasospasm studies (high dose ACH) during the initial study, and some were not given a higher dose of adenosine per the study design. Limited data are available on the reproducibility of CFR, though randomized trials have demonstrated minimal variability in placebo control groups as compared to ACEi (14). Lastly, there exists intrinsic bias in patient selection, as those undergoing repeat CFT were those in our clinic presenting with persistent angina and lack of improvement or intolerances to medical therapy. It is possible that patients with improvement in symptoms could show improvement in other pathways not observed in this analysis. It is also possible that a placebo effect of guided treatment may affect self-reported outcomes.
This brief report demonstrates that CMD is possibly a persistent condition and that targeted interventions guided by invasive testing may be associated with improvement in CFR and patient-reported treatment satisfaction in follow-up. Clinical trials are underway (15) to better understand the impact of the anti-anginal and anti-ischemic medications on CMD pathways in order to tailor treatment guidelines for CMD in the setting of INOCA.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Cedars Sinai IRB review board. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
All authors contributed to the study, and design of this manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by R01 HL090957, K23 HL105787, K23 HL125941, K23 HL127262, K23HL151867, and GCRC grant MO1-RR00425 from the National Center for Research Resources, the National Center for Advancing Translational Sciences grant UL1TR000124, the Edythe L. Broad and the Constance Austin Women's Heart Research Fellowships, Cedars-Sinai Medical Center, Los Angeles, California, the Barbra Streisand Women's Cardiovascular Research and Education Program, The Linda Joy Pollin Women's Heart Health Program, and the Erika Glazer Women's Heart Health Project, Cedars-Sinai Medical Center, Los Angeles, California. This work is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or National Institutes of Health.
CB, serves as Board of Director for iRhythm, fees paid through CSMC from Abbott Diagnostics and Sanofi. JW served on an advisory board for Abbott Vascular.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL, Camici PG, Chilian WM, et al. Ischemia and no obstructive coronary artery disease (INOCA). Circulation. (2017) 135:1075–92. doi: 10.1161/CIRCULATIONAHA.116.024534
2. Gulati M, Shaw LJ, Bairey Merz CN. Myocardial ischemia in women: lessons from the NHLBI WISE study. Clin Cardiol. (2012) 35:141–8. doi: 10.1002/clc.21966
3. Wei J, Mehta PK, Johnson BD, Samuels B, Kar S, Anderson RD, et al. Safety of coronary reactivity testing in women with no obstructive coronary artery disease: results from the NHLBI-sponsored WISE (women’s ischemia syndrome evaluation) study. JACC Cardiovasc Interv. (2012) 5:646–53. doi: 10.1016/j.jcin.2012.01.023
4. Ford TJ, Stanley B, Sidik N, Good R, Rocchiccioli P, McEntegart M, et al. 1-year outcomes of angina management guided by invasive coronary function testing (CorMicA). JACC Cardiovasc Interv. (2020) 13:33. doi: 10.1016/j.jcin.2019.11.001
5. Sacks D, Baxter B, Campbell BCV, Carpenter JS, Cognard C, Dippel D, et al. Multisociety consensus quality improvement revised consensus statement for endovascular therapy of acute ischemic stroke. Int J Stroke. (2018) 13:612–32. doi: 10.1016/j.jvir.2017.11.026
6. Gulati M, Cooper-DeHoff RM, McClure C, Johnson BD, Shaw LJ, Handberg EM, et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the women’s ischemia syndrome evaluation study and the St James women take heart project. Arch Intern Med. (2009) 169:843–50. doi: 10.1001/archinternmed.2009.50
7. AlBadri A, Bairey Merz CN, Johnson BD, Wei J, Mehta PK, Cook-Wiens G, et al. Impact of abnormal coronary reactivity on long-term clinical outcomes in women. J Am Coll Cardiol. (2019) 73:684–93. doi: 10.1016/j.jacc.2018.11.040
8. Galderisi M, Rigo F, Gheradi S, Cortigiani L, Santoro C, Sicari R, et al. The impact of aging and atherosclerotic risk factors on transthoracic coronary flow reserve in subjects with normal coronary angiography. Cardiovasc Ultrasound. (2012) 10:1–7. doi: 10.1186/1476-7120-10-20
9. Eshtehardi P, McDaniel MC, Dhawan SS, Binongo JNG, Krishnan SK, Golub L, et al. Effect of intensive atorvastatin therapy on coronary atherosclerosis progression, composition, arterial remodeling, and microvascular function. J Invasive Cardiol. (2012) 24:522–9. PMDID: 23043036
10. Bugiardini R, Manfrini O, Pizzi C, Fontana F, Morgagni G. Endothelial function predicts future development of coronary artery disease. Circulation. (2004) 109:2518–23. doi: 10.1161/01.CIR.0000128208.22378.E3
11. Bairey Merz CN, Pepine CJ, Shimokawa H, Berry C. Treatment of coronary microvascular dysfunction. Cardiovasc Res. (2020) 116:856–70. doi: 10.1093/cvr/cvaa006
12. Bairey Merz CN, Handberg EM, Shufelt CL, Mehta PK, Minissian MB, Wei J, et al. A randomized, placebo-controlled trial of late na current inhibition (ranolazine) in coronary microvascular dysfunction (CMD): impact on angina and myocardial perfusion reserve. Eur Heart J. (2016) 37:1504–13. doi: 10.1093/eurheartj/ehv647
13. Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. (2019) 2020(41):407–77. doi: 10.1093/eurheartj/ehz425
14. Pauly DF, Johnson BD, Anderson RD, Handberg E, Smith KM, Cooper-DeHoff RM, et al. In women with symptoms of cardiac ischemia, non-obstructive coronary arteries, and microvascular dysfunction, ACE inhibition is associated with improved microvascular function: a double-blind randomized study from the NHLBI women’s ischemia syndrome evaluation (WISE). Am Heart J. (2011) 162:678–84. doi: 10.1016/j.ahj.2011.07.011
Keywords: INOCA, women, ischemia, coronary function test (CFT), coronary microvascular dysfunction (CMD)
Citation: Suppogu N, Tjoe B, Wei J, Maughan J, Joung S, Quesada O, Shufelt CL, Samuels B, Azarbal B and Bairey Merz CN (2023) Case report: Repeat coronary function testing in women with ischemia and no obstructive coronary artery disease. Front. Cardiovasc. Med. 10:1096265. doi: 10.3389/fcvm.2023.1096265
Received: 12 June 2023; Accepted: 20 June 2023;
Published: 6 July 2023.
Edited by:
Branko Dusan Beleslin, Clinical Center of Serbia, SerbiaReviewed by:
Caitlin E.M. Vink, Amsterdam Cardiovascular Sciences (ACS), Netherlands© 2023 Suppogu, Tjoe, Wei, Maughan, Joung, Quesada, Shufelt, Samuels, Azarbal and Bairey Merz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: C. Noel Bairey Merz bWVyekBjc2hzLm9yZw==
†These authors share first authorship
Abbreviations CFT, coronary function testing; INOCA, ischemia with non-obstructive coronary artery disease; CAD, coronary artery disease; CMD, coronary microvascular dysfunction; MACE, major adverse cardiovascular event; CFR, coronary flow reserve; CBF, coronary blood flow; IC, intracoronary; ACH, acetylcholine; ACEi, angiotensin converting enzyme inhibitor; ARB, angiotensin II receptor blocker; BB, beta blocker.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.