- 1Center for Health Management and Policy Research, School of Public Health, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, China
- 2NHC Key Lab of Health Economics and Policy Research (Shandong University), Jinan, Shandong, China
- 3Center for Health Preference Research, Shandong University, Jinan, Shandong, China
- 4Department of Cardiovascular Surgery, General Hospital of Tianjin Medical University, Tianjin, China
Background: Although the five-level version of the EuroQol five-dimensional questionnaire (EQ-5D-5L) has been validated in various diseases, no empirical study has evaluated the responsiveness and minimal clinically important difference (MCID) of the instrument in patients with coronary heart disease (CHD), which limits the interpretability and clinical application of EQ-5D-5L. Therefore, this study aimed to determine the responsiveness and MCID of EQ-5D-5L in patients with CHD who underwent percutaneous coronary intervention (PCI) and identify the relationship between the MCID values and minimal detectable change (MDC).
Methods: Patients with CHD were recruited for this longitudinal study at the Tianjin Medical University’s General Hospital in China. At baseline and 4 weeks after PCI, participants completed the EQ-5D-5L and Seattle Angina Questionnaire (SAQ). Additionally, we used the effect size (ES) to assess the responsiveness of EQ-5D-5L. The anchor-based, distribution-based, and instrument-based methods were used in this study to calculate the MCID estimates. The MCID estimates to MDC ratios were computed at the individual and group levels at a 95% CI.
Results: Seventy-five patients with CHD completed the survey at both baseline and follow-up. The EQ-5D-5L health state utility (HSU) improved by 0.125 at follow-up compared with baseline. The ES of EQ-5D HSU was 0.850 in all patients and 1.152 in those who improved, indicating large responsiveness. The average (range) MCID value of the EQ-5D-5L HSU was 0.071 (0.052–0.098). These values can only be used to determine whether the change in scores were clinically meaningful at the group level.
Conclusion: EQ-5D-5L has large responsiveness among CHD patients after undergoing PCI surgery. Future studies should focus on calculating the responsiveness and MCID for deterioration and examining the health changes at the individual level in CHD patients.
1. Introduction
Coronary heart disease (CHD) is one of the most common cardiovascular diseases worldwide. Despite tremendous efforts in the prevention, treatment, and rehabilitation of CHD, which has led to a decline in mortality over the last few decades, CHD remains the leading cause of death and disability in adults worldwide, including in China (1, 2). It is expected to account for 30.5% of all deaths worldwide by 2030 (2). In China, it is estimated that approximately 11 million people have CHD, and the morbidity and mortality of CHD are still increasing annually (3).
Several factors are thought to increase the likelihood of CHD development. The main traditional risk factors are hypertension, smoking, hyperlipidemia, diabetes, old age, gender, obesity, lack of exercise, and family history of CHD (4). Often, these risk factors do not exist in isolation. Therefore, CHD patients commonly present with multiple comorbidities and are often accompanied by psychological problems such as anxiety and depression (5). Percutaneous coronary intervention (PCI) guided by coronary physiology can relieve patients’ clinical symptoms and has been regarded as a standard and effective treatment for CHD (6, 7). Previous studies have found that PCI can improve the health-related quality of life (HRQoL) of patients with CHD, but the effects do not last (8).
HRQoL refers to different health domains, including physiological, psychological, and social components (9). It is increasingly accepted as an important outcome, especially for chronic conditions, including CHD (8, 10). HRQoL in patients with CHD can be quantified using generic or disease-specific instruments (11). CHD-specific HRQoL instruments, such as the Seattle Angina Questionnaire (SAQ) and the Minnesota Living with Heart Failure Questionnaire (MLHF), can examine the specific impact of CHD (11). Generic instruments, such as SF-36 and EQ-5D, enable the comparison of HRQoL between CHD and other conditions (11).
The EuroQoL five-dimensional questionnaire (EQ-5D) is a generic preference-based HRQoL instrument developed by the EuroQoL group that has been widely used and validated in populations with various diseases (12). The original version of EQ-5D has three response levels (13). However, studies have found that the three-level version has an obvious ceiling effect and cannot capture small changes sufficiently (14, 15). Therefore, a five-level version of EQ-5D was developed (16). Furthermore, health state utility (HSU) generated by the EQ-5D can support the calculation of quality-adjusted life years (QALYs), which will allow for pharmacoeconomic evaluation (17).
However, the interpretation of HRQoL instrument scores faces enormous challenges, particularly in defining what constitutes a trivial or an important change in patients’ quality of life (18–20). The results of HRQoL scores are usually analyzed and interpreted using statistical tests in clinical research. Although statistical tests can reflect statistical changes in the measured outcomes, they do not always indicate that the changes are clinically relevant (18, 21). Therefore, to explain the clinical relevance of score changes, the concept of minimal clinically important difference (MCID) was developed (19). Calculating the MCID values of HRQoL instruments can not only assess clinically meaningful score changes for patients in clinical trials but also supports the interpretability of the measuring instrument (22).
The minimal detectable change (MDC) is the smallest change in scores that can be detected after considering the measurement error (21). For a reliable instrument, the MCID should be greater than MDC (23, 24). Therefore, we can use the ratio between the MCID and MDC to judge whether the calculated MCID is a real change or just a meaningless measurement error, which can support the application of MCID in clinical research. Furthermore, MCID and MDC are related to responsiveness. The former two indicators are more clinically oriented, and the responsiveness is regarded as an indicator reflecting the ability of the instrument to detect changes over time (25, 26).
Previous studies have shown that the responsiveness and MCID are affected by clinical setting, and their use requires calculations in specific disease contexts (27, 28). Therefore, although the responsiveness and MCID of the EQ-5D-5L HSU have been calculated in patients with various diseases, the results vary. For example, previous studies have found small-to-moderate responsiveness in patients with stroke (29) and large responsiveness in venous leg ulcers (30). The MCID of the EQ-5D-5L HSU in patients with cervical intraepithelial neoplasia (CIN) was 0.039 (31), while in patients with COPD was 0.051 (32). Furthermore, a study evaluating the relationship between MCID and MDC in patients with CIN showed that when the MCID of the EQ-5D HSU was 0.039, it could not be distinguished from measurement error at the individual level (31). Another study in patients after hip or knee replacement found that when the MCID of EQ-5D HSU was 0.32, it could be distinguished from measurement error at both individual and group levels (33). All of these studies support the interpretability and applicability of EQ-5D in different clinical settings. Nevertheless, according to our knowledge, no empirical study has evaluated the responsiveness and MCID of EQ-5D-5L in CHD patients after PCI, and none has analyzed the relationship between MCID and MDC in CHD patients.
Therefore, our study aimed to (1) evaluate the responsiveness of EQ-5D-5L in CHD patients who underwent PCI, (2) calculate the MCID estimates of EQ-5D-5L HSU, and (3) identify the validity of MCID by using the ratios between MCID and MDC.
2. Materials and methods
2.1. Study design and population
This prospective cohort study was conducted at the General Hospital of Tianjin Medical University, China, between April and September 2019. Inclusion criteria were (1) recruited from the cardiology inpatients, (2) one or more lesions with ≥50% stenosis as shown by coronary angiography and met the requirements of the “Chinese Guidelines for Percutaneous Coronary Intervention” (34), (3) aged 18 years or older, and (4) will undergo PCI within 1 or 2 days. The exclusion criteria were (1) unwillingness to provide informed consent, (2) inability to understand the questionnaire, (3) serious comorbidities (such as severe liver and kidney insufficiency or cirrhosis, malignant tumor), (4) a history of mental illness, and (5) hearing or vision impairment.
The sample size was considered sufficient if the number of patients was at least 5–10 times the number of items in the main outcome (EQ-5D-5L in this study). Depending on the questionnaire used in the study, the estimated sample size was at least 25–50 cases. We anticipated a potential 20% loss to follow-up, so at least 60 patients were required. All patients who completed the questionnaire and provided informed consent were enrolled in this study. Ethical approval was obtained from the Ethics Review Board of the School of Health Care Management, Shandong University (No. ECSHCMSDU20191002). The study was carried out in accordance with the Declaration of Helsinki.
2.2. Study procedure and quality control
Before the survey, we provided homogeneous training to all investigators, addressing the survey process and questionnaires, the significance of questionnaire items, and points for attention during the survey. During the survey process, uniform terminology was adopted to explain the research purpose and questionnaire requirements to all participants in detail. Participants filled out the questionnaire anonymously after they provided their informed consent.
All eligible participants completed the questionnaires at baseline (before PCI surgery) and a follow-up point (4-week after PCI). At baseline, socio-demographic characteristics, including age, gender, marital status, education level, and occupation, were collected through face-to-face interviews with eligible patients on-site. Additionally, clinical data, including CHD types, duration time, disease status, and comorbidities, were collected from their clinicians. Well-trained investigators conducted a follow-up survey over the telephone. The participants’ phone numbers were randomly and anonymously assigned to different investigators. After confirming the free time of each participant, the investigator conducted a one-to-one telephone follow-up. At both time points, the participants were asked to complete the SAQ and EQ-5D-5L to evaluate their health status. The questionnaire was completed within 10–20 min. The data were entered uniformly. After the original data were entered, another member checked them to ensure the correctness of the data entry.
2.3. Instruments
EQ-5D-5L includes a multi-attribute health description system based on five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression (16). Each dimension has a five-point response option: no problems, slight problems, moderate problems, severe problems, and extreme problems (35). The Chinese version of the EQ-5D-5L has been verified, and the Chinese-specific tariff was used in this study (35, 36). EQ-5D-5L HSU calculated by Chinese-specific tariff ranges from −0.391 to 1.000, where 1 indicates “full health” and 0 means “dead.” A negative HSU represents a certain health status that is worse than death.
Seattle Angina Questionnaire is a disease-specific instrument used to measure the health status of CHD patients. It consists of 19 items divided into five domains: physical limitation, angina stability, angina frequency, treatment satisfaction, and disease perception (37). The SAQ was scored by assigning each response an ordinal value, with 1 being the option with the lowest level of health and 5 being the option with the best level of health. All domain scores can be calculated by summing the scores of items in each domain and can be transformed to 0–100 points. Higher scores indicated a better quality of life (38). The Chinese version of the SAQ has been proven to be a valid and reliable instrument (39).
2.4. Statistical analysis
Descriptive statistics were used to describe the socio-demographic characteristics, clinical characteristics, and distribution of EQ-5D-5L HSU and SAQ scores. Characteristics were presented as means and standard deviations (SD) for continuous variables and numbers and percentages (%) for categorical variables. For comparing scores between two-time points, the paired t-test was used for parametric data, and the Wilcoxon signed-rank test was used for nonparametric data. Statistical analysis was conducted using the SPSS software (IBM SPSS Statistics 25.0). All statistical tests were two-tailed, with a significance level of 0.05.
2.5. Responsiveness
Researchers have no consensus regarding the best method for calculating responsiveness (40, 41). Therefore, we used effect size (ES) to examine the responsiveness in this study. ES was defined as the difference in scores between baseline and follow-up divided by the SD of the baseline scores (21, 29, 42). According to Cohen’s d criteria, ES can be categorized as small (<0.5), moderate (0.5 ~ 0.8), or large (>0.8) (43).
2.6. Minimal clinically important difference
Anchor-based method: The anchor-based approach uses external criteria to anchor minimal but important change scores for participants (44). Correlation ≥|0.3| can be used as a threshold to assess the usefulness of the anchor (44). Therefore, Spearman’s correlation coefficient was used to quantify the association between changes in EQ-5D-5L HSU and SAQ scores. We used half the SD of anchor scores at baseline as the lower cut-off of minimal change and twice the lower cut-off as the upper cut-off (45, 46). Specifically, participants were categorized into three groups according to the change scores of the anchor: no change (<0.5 baseline SD), minimal change (≥0.5 baseline SD and ≤1 baseline SD), and large change (>1 baseline SD). To obtain the MCID for improvement, the mean change score for the “minimal improvement” group was subtracted from the average change score for the “no change” group (47). Likewise, the deteriorative MCID was the difference between the mean change score for the “minimal deterioration” group and the “no change” group (47).
A receiver operating characteristic (ROC) curve was constructed to estimate the MCID in this study, and the area under the curve (AUC) was used to represent the ability of the instrument to distinguish patients who underwent a clinically meaningful change. The Youden index was calculated to determine MCID estimates with the highest sensitivity and specificity using the following formula: The cut-off point corresponding to the maximum Youden index was the optimal cut-off value of the ROC curve and was the MCID (48, 49).
Instrument-based method: Instrument-based method is based on the average difference in the EQ-5D HSU between the baseline health states and single-level transitions to other health states (50). According to the direction of single-level transitions, MCID can be categorized into three groups: only transitions to better health states, only transitions to worse states and all transitions to other health states (46). In this study, we only focused on the better transitions. In addition, because the conversion parameter between Lever 3 (moderate problem) and Level 4 (severe problem) exceeds other adjacent levers at least 1.4 times in all dimensions according to the Chinese scoring algorithm, we excluded the interconversion between these two levels to avoid overestimating MCID (31, 46). Finally, when calculating the improved MCID, we excluded the baseline health state “11,111” because it could no longer be improved.
Distribution-based method: Based on previous studies, half the SD of baseline scores and one-SEM were considered to approximate values of MCID (45, 51, 52). Therefore, we calculated half the SD of the EQ-5D-5L HSU at baseline as the MCID. Additionally, the standard error measurement (SEM) was calculated using the following formula: , where r is the test–retest reliability or Cronbach’s α coefficient (51). The Cronbach’s α coefficient of the EQ-5D-5L was calculated at baseline and follow-up in this study. The SEM was computed for the baseline and follow-up scores, and the mean was calculated to provide an MCID estimate.
2.7. Minimal detectable change
The MDC is derived from SEM and is calculated using the formula: (33). In this study, a 95% confidence level was established, corresponding to a Z-score of 1.96. This MDC was considered MDC95%(ind), representing the smallest detectable change after considering the measurement error at the individual level. According to Boer, MDC95%(group) is equal to MDC95%(ind) divided by , where n represents the sample size (53). Finally, we used the ratio of MCID to MDC for comparisons at the individual and group levels. If the ratio of MCID to MDC > 1, the calculated MCID can be used to reflect the real minimal important change. Otherwise, the calculated MCID represents the measurement error of the questionnaire and is not a valid value (54).
3. Results
3.1. Descriptive analysis
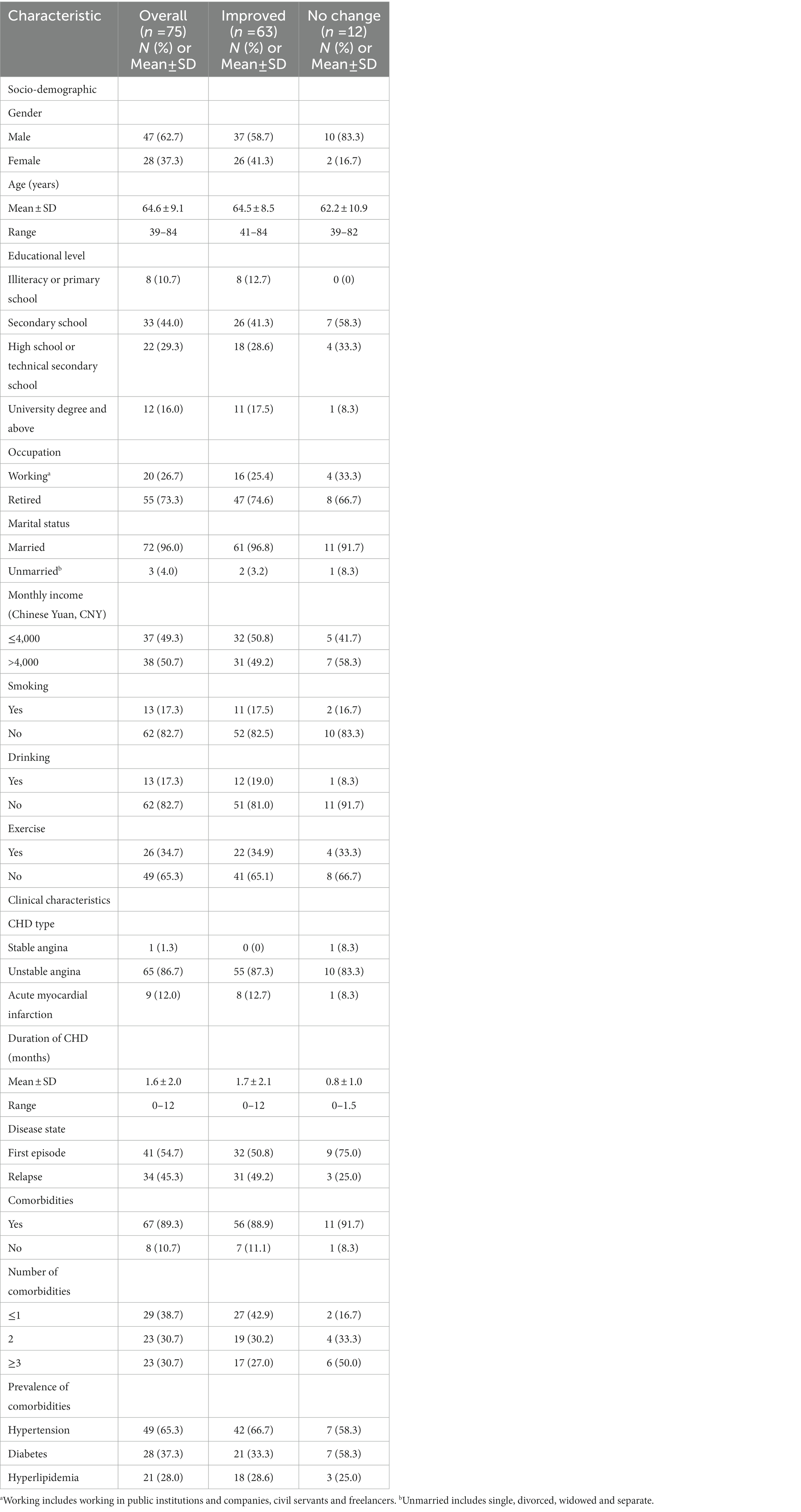
Seventy-nine patients were included at baseline. Three patients were lost to follow-up during the study period, and one died. The socio-demographic and clinical characteristics of the 75 patients who completed the questionnaire at both time points are presented in Table 1. The mean age of the patients was 64.6 ± 9.1 years. Most of them were male (62.7%), retired (73.3%), and married (96.0%). More than four-fifths (86.7%) of them were diagnosed with unstable angina, and the mean duration of the disease was 1.6 ± 2.0 months. The proportion of participants with hypertension, diabetes, and hyperlipidemia was 65.3, 37.3, and 28.0%, respectively. Most patients (61.3%) had at least two comorbidities. Additionally, 84% of patients reported an improved health status after PCI, and their mean age was 64.5 ± 8.5 years. Most were male (58.7%), retired (74.6%) and married (96.8%). Furthermore, 16% of patients reported no change in their health status, and their mean age was 62.2 ± 10.9 years, and they were mostly male (83.3%), retired (66.7%), and married (91.7%).
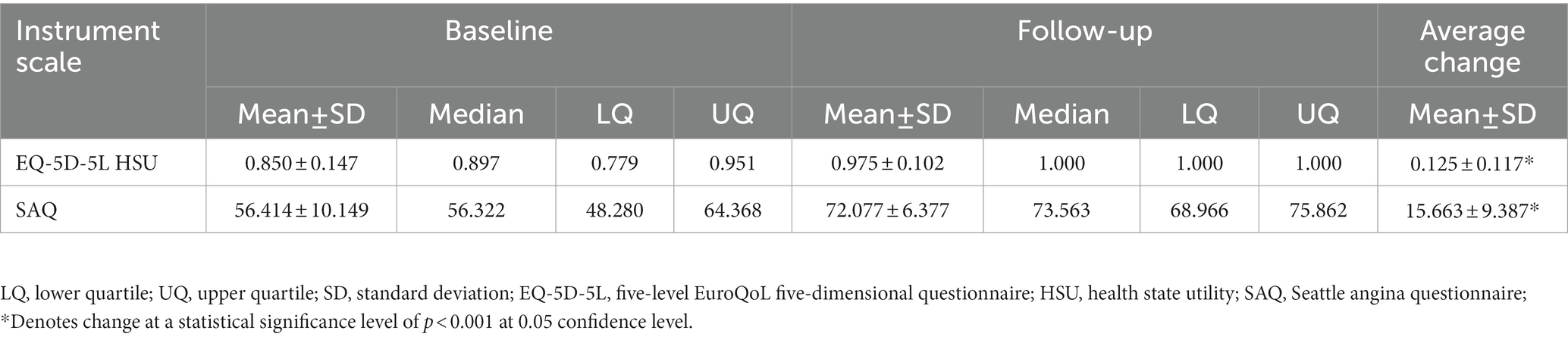
Table 2 describes the score distribution of the EQ-5D-5L HSU and SAQ at both time points. The mean EQ-5D-5L HSU scores at baseline and follow-up were 0.850 and 0.975, respectively, with an average change of 0.125 (p < 0.001). For the SAQ, the mean scores were 56.414 and 72.077 at the two time points, respectively, with an average change score of 15.663 (p < 0.001).
3.2. Responsiveness
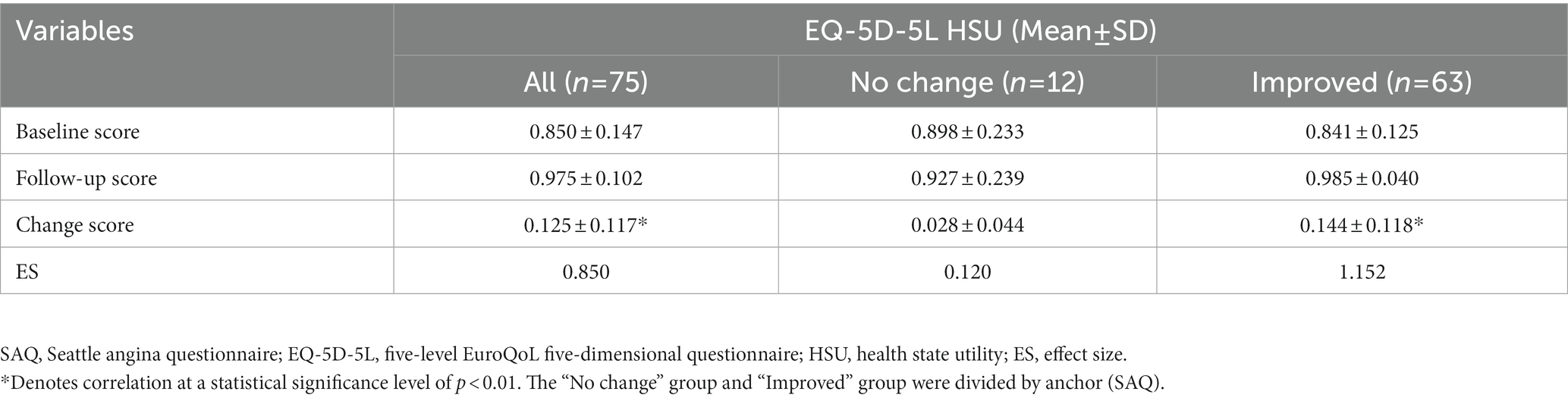
Table 3 reports the responsiveness results of the EQ-5D-5L. Among all patients, the EQ-5D HSU increased by 0.125 (p < 0.001) after PCI. The ES of EQ-5D-5L HSU was 0.850, indicating large responsiveness in all patients. Among patients who responded to the anchor transition as “improvement” (including minimal improvement and much improvement), the ES was 1.152, suggesting a large effect size. Additionally, for the patients who were “no change,” the change of HSU was 0.028 (p > 0.05). ES showed no responsiveness among the “no change” group.
3.3. Minimal clinically important difference
3.3.1. Anchor-based analysis
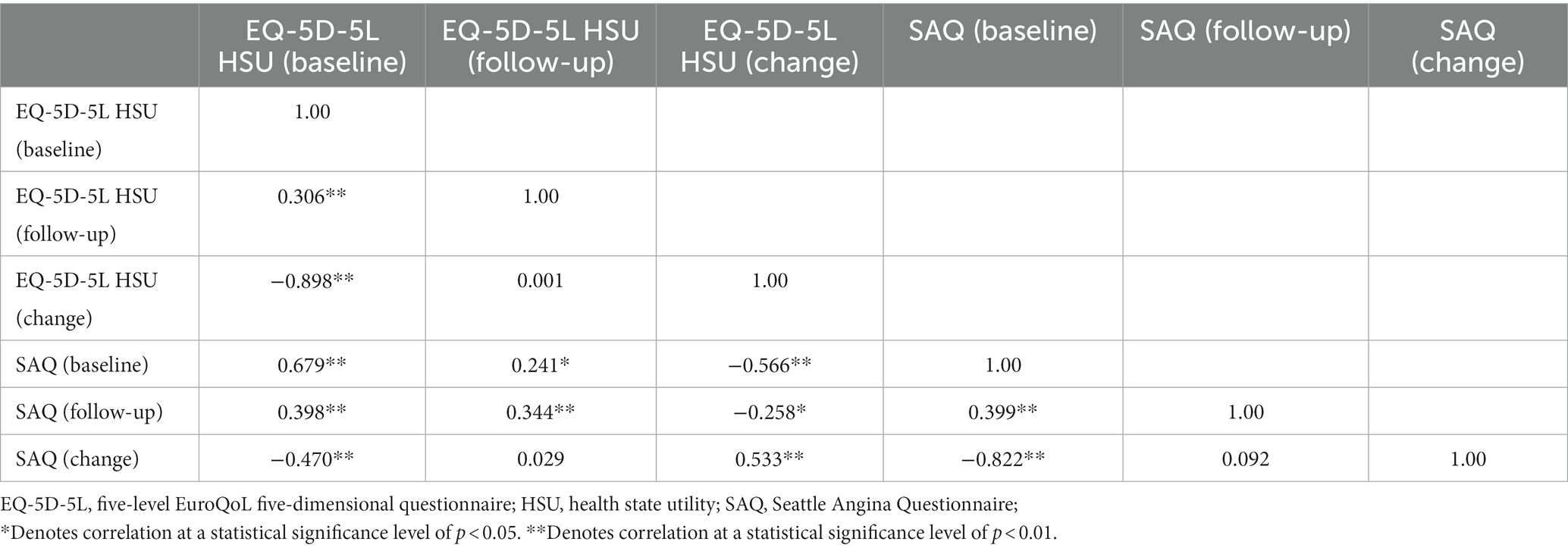
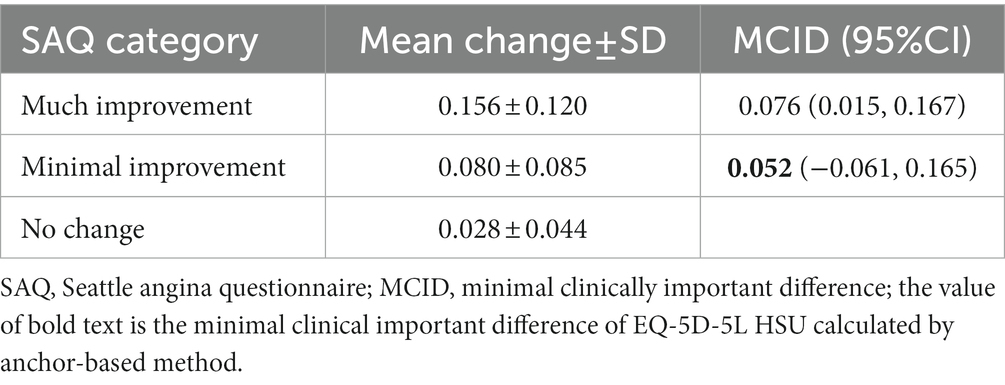
There was a moderate correlation between the change scores of the EQ-5D HSU and SAQ, with a correlation coefficient of 0.533 (Table 4). The MCID estimates of the EQ-5D HSU based on the SAQ-anchored method are listed in Table 5. Based on the SAQ scores, no participant reported a worsening health state from baseline to four-week after PCI; therefore, in this study, we only focused on the improved MCID. As shown in Table 5, an increase of 0.052 points (95% CI: −0.061, 0.165) in the EQ-5D HSU corresponded to a minimally important change for patients anchored by the SAQ.
Receiver operating characteristic analysis was also performed to identify improved MCID only (Figure 1). The MCID estimate derived from the ROC curve was 0.098, corresponding to a sensitivity of 69.8% and a specificity of 91.7%. The AUC anchored by the SAQ was 0.845 (95% CI: 0.753, 0.936), suggesting that EQ-5D can excellently distinguish patients whose health states improved and those whose health states did not change.
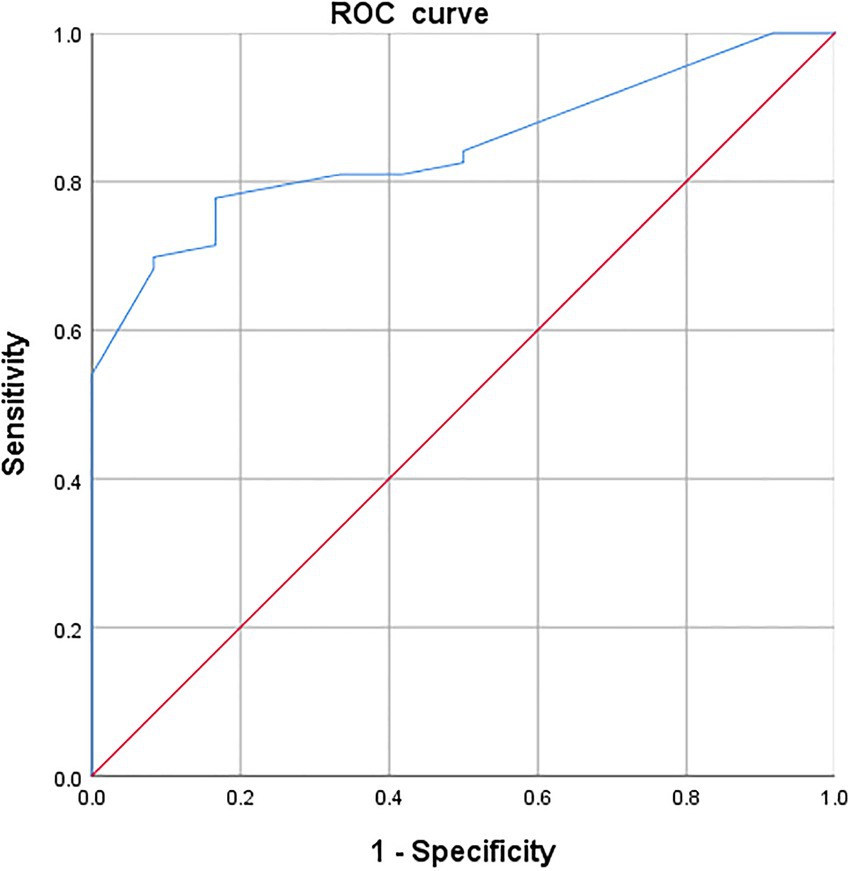
Figure 1. Receiver-operating characteristic (ROC) curve of EQ-5D-5L HSU change score in patients whose health states improved.
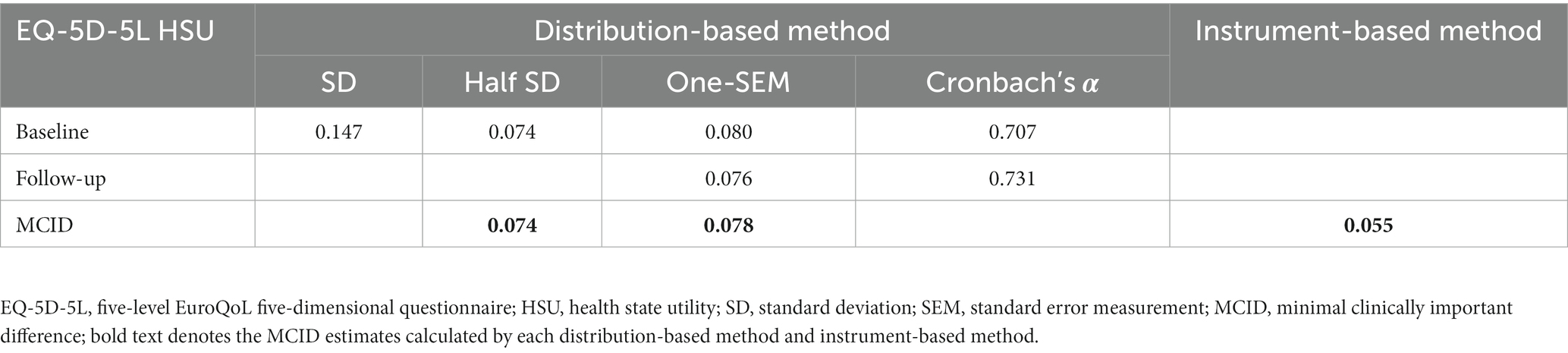
3.3.2. Instrument- and distribution-based analysis
Based on the instrument-defined method, the MCID of EQ-5D HSU was 0.055 (95% CI: 0.054, 0.58). An MCID estimate of 0.074 was produced using half the SD of HSU at baseline. The MCID derived from the SEM value was 0.078 (Table 6).
3.4. Validity of the MCID estimates
Table 7 shows ratios of MCID estimates calculated by all methods to MDC95%(ind) and MDC95%(group). The ratios of MCIDs computed by all methods to MDC95%(ind) were all less than 1, indicating that on individual levels, the MCIDs cannot be discriminated from measurement error to reflect a real meaningful change. However, the ratios of MCIDs to MDC95%(group) all exceeded 1, which means that the MCID can detect the smallest important improvement in the group of 75 CHD patients with 95% confidence.
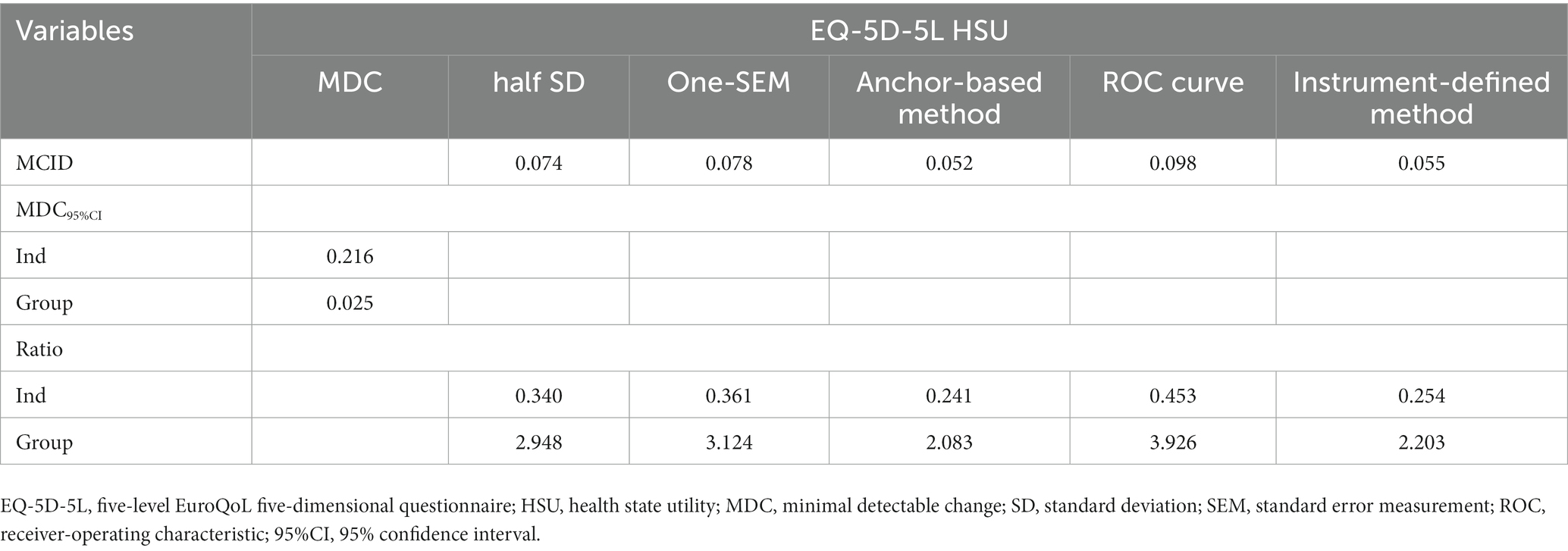
Table 7. Minimal clinically important difference (MCIDs) of the EQ-5D-5L HSU through different methods and the relation to the MDC at individual and group levels.
4. Discussion
This study estimated the responsiveness and MCID of the instrument in CHD patients after PCI surgery to support score interpretation and clinical application of the EQ-5D-5L. This study showed that the EQ-5D-5L was largely responsive to changes and provided evidence that the MCID of the EQ-5D-5L HSU in patients with CHD ranged from 0.052 to 0.098. The MCID calculated in this study can distinguish significant changes in the HSU at the group level but not at the individual level.
Responsiveness has been suggested as an additional criterion for evaluating HRQoL instruments, which can reflect the ability of an instrument to respond to changes and is essential for longitudinal validity (55). Various methods can be used to assess responsiveness, such as ES, SRM, relative efficiency (RE), and regression models. However, there is no consensus on the preferred method, and different methods provide different results (40, 41). According to Husted et al. (42) ES is one of the most frequently used approaches for assessing responsiveness. Therefore, this method was used in this study, and a large responsiveness of the EQ-5D-5L was found in all participants and improved participants.
The responsiveness of EQ-5D-5L HSU has been explored in several diseases. In patients with acute asthma who self-reported improvement, researchers found that the EQ-5D-5L had moderate to large responsiveness (56). Chen et al. (29) found that the EQ-5D-5L had small-to-moderate responsiveness in subacute and chronic stroke patients. Golicki et al. (57) found moderate to large responsiveness of the EQ-5D-5L in acute stroke patients whose health status improved from baseline. Although the above studies all found that EQ-5D-5L is responsive, this is quite different from our finding of large responsiveness. The source of inconsistency may be attributed to differences in patients’ disease stage or severity at baseline. In this study, 98.7% of patients had unstable angina or acute myocardial infarction, and 61.4% had at least two comorbidities, making patients have a stronger perception of the change in their health status compared with patients with chronic or stable disease stages, leading to large responsiveness. Furthermore, EQ-5D is more responsive to large treatment effects (28). Compared with other treatments, PCI surgery can greatly improve patients’ perceived HRQoL in the short term (58).
There is no “one-size-fits-all” method and no consensus on the best method to calculate the MCID of HRQoL instruments (59). Anchor-based and distribution-based methods are the main methods for evaluating the MCID (60). The anchor-based approaches use an external and independent indicator to calculate the MCID by comparing the scores in anchor-based groups, including the change difference method, ROC curve, regression model, etc. (44). In contrast, the distribution-based methods rely on measures of outcome variability, using the statistical property of the data set to identify the MCID (61), including the SD, SEM, and ES methods. Usually, these two methods are used together to ensure the accuracy of MCID estimates because each has its advantages and disadvantages (47). In this study, we chose the most commonly used anchor-based methods (i.e., the change difference method and ROC curve) and distribution-based methods (i.e., 0.5 SD and SEM) to calculate the MCID of the EQ-5D-5L (27, 62). In addition to these two methods, Luo et al. (50) first used an instrument-based method to evaluate MCID for the EQ-5D-3L, and the results showed that it is feasible to use this method to evaluate the MCID of preference-based HRQoL instruments. Subsequently, the instrument-based method has been widely used for calculating the MCID of the EQ-5D (46, 63, 64). Therefore, we used the above three methods simultaneously to ensure the accuracy of the MCID and found that the average MCID was 0.071, with a range from 0.052 to 0.098.
The ratios of MCIDs to MDC95%(group) were all greater than 1, indicating that the MCIDs were valid at the group level and could be distinguished from measurement errors. However, the ratios of MCIDs to MDC95%(ind) were all less than 1, which means that the calculated MCIDs would not be useful at the individual level. One possible explanation may be that most patients had longer CHD duration, and nearly half of them were not first-episode CHD, which made them adapt to this disease and improved baseline scores. Another explanation may be that most patients have at least two comorbidities, resulting in lower psychological expectations of health changes.
Previous studies commonly used the Global Rating of Change Questionnaire (GRCQ) as an anchor. However, the GRCQ contains only one question, which makes it difficult or impossible to capture changes in participants’ HRQoL (49). Moreover, its validity and reliability are uncertain (18). Studies have shown that disease-specific questions have higher construct validity than global transition questions as anchors for determining MCID (65). The GRCQ was not used or adopted in this study because of these limitations. In contrary, we used a valid, reliable, multi-attribute, and disease-specific instrument to anchor the EQ-5D-5L HSU as in previous studies (32, 66). Furthermore, it has been illustrated that responsiveness and MCID may be affected by the direction of changes (60, 67–69). However, no patients in this study reported that they experienced health deterioration after PCI anchored by SAQ change scores. The outcome of clinical interest lies in surgery-associated health improvement and the resulting effect on CHD patients’ quality of life rather than exacerbation. Therefore, deteriorative responsiveness and MCID were not evaluated in this study.
The MCID values may vary according to disease, interventions, and baseline characteristics, including socio-demographic and clinical characteristics; therefore, MCID may vary by gender, education level, type of CHD, and different comorbidities in this study (47, 70). In particular, studies found that the prognosis of male patients with CHD after PCI was better than that of female patients; the mortality, incidence of major adverse cardiovascular events, and bleeding events after PCI in female patients were higher than those in male patients; and the health status (such as HRQoL, mental health) of female patients after PCI was worse than that of male patients (71–73). Therefore, these differences in prognosis between genders may affect their perception of health and cause the MCID to vary among genders. However, due to the limited sample size within anchor-defined categories for the different stratified subgroups, it was impossible to explore whether the resultant MCID estimates based on these clinical/demographic factors in patients with CHD were different. We suggest exploring this issue using a larger sample size in the future.
This is the first study to evaluate the responsiveness and MCID of the EQ-5D-5L HSU in CHD patients after PCI. This study has several advantages. First, in addition to commonly used anchor-based and distribution-based methods, we adopted the instrument-based method to ensure the accuracy of the MCID estimates. Second, we used a multidimensional disease-specific scale as an anchor, which can reflect the changes in patients’ HRQoL from multiple dimensions. Third, we analyzed whether the MCID calculated by each method could reflect meaningful changes at both the individual and group levels, which allowed us to avoid false interpretations of the MCID.
This study also has few limitations. First, the patients were recruited from one Tianjin city hospital, which may not represent all the CHD patients across China. Second, the small sample size of our study may have affected the accuracy of the results, although it met the basic requirements for calculating the MCID (26). Third, the responsiveness and MCID may differ depending on the research setting, including interventions and patients’ characteristics. Therefore, the results of this study may not be applicable under other conditions. Fourth, this was a longitudinal real-world study, and randomized controlled trials are needed to verify the MCID among CHD patients after PCI in the future.
5. Conclusion
The EQ-5D-5L was largely responsive to patients with CHD undergoing PCI surgery. The MCID of EQ-5D-5L was 0.071, with a range between 0.052 and 0.098 in this study, and the calculated MCIDs could only determine whether patients experienced meaningful changes at the group level. Future studies should focus on the calculation of deteriorative responsiveness and MCID and examine the validity of MCID in CHD patients at individual levels.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Review Board of the School of Health Care Management, Shandong University (Reference No. ECSHCMSDU20191002). The patients/participants provided their written informed consent to participate in this study.
Author contributions
LD and SL designed the study. QF performed the data collection. LD and YZ performed the data analyses, and all authors contributed to interpreting the data. YZ drafted the manuscript, which was critically revised by all others. All authors read and approved the final manuscript.
Funding
Financial support for this project was provided by NHC Key Lab of Health Economics and Policy Research (Shandong University; no. NHC-HEPR2018003) and National Natural Science Foundation of China (no. 71403056).
Acknowledgments
The authors gratefully thank the investigators of the Department of Cardiovascular surgery, General Hospital of Tianjin Medical University for helping to collect the questionnaires. Thanks to all the participants for their time and effort to this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tušek-Bunc, K, and Petek, D. Comorbidities and characteristics of coronary heart disease patients: their impact on health-related quality of life. Health Qual Life Outcomes. (2016) 14:159. doi: 10.1186/s12955-016-0560-1
2. Wang, W, Lau, Y, Chow, A, Thompson, DR, and He, HG. Health-related quality of life and social support among Chinese patients with coronary heart disease in mainland China. Eur J Cardiovasc Nurs. (2014) 13:48–54. doi: 10.1177/1474515113476995
3. Dou, L, Mao, Z, Fu, Q, Chen, G, and Li, S. Health-related quality of life and its influencing factors in patients with coronary heart disease in China. Patient Prefer Adherence. (2022) 16:781–95. doi: 10.2147/PPA.S347681
4. Yusuf, S, Hawken, S, Ounpuu, S, Dans, T, Avezum, A, Lanas, F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the Interheart study): case-control study. Lancet. (2004) 364:937–52. doi: 10.1016/S0140-6736(04)17018-9
5. Dickens, C, Cherrington, A, and McGowan, L. Depression and health-related quality of life in people with coronary heart disease: a systematic review. Eur J Cardiovasc Nurs. (2012) 11:265–75. doi: 10.1177/1474515111430928
6. Mao, C, Fu, XH, Yuan, JQ, Yang, ZY, Chung, VC, Qin, Y, et al. Tong-Xin-Luo capsule for patients with coronary heart disease after percutaneous coronary intervention. Cochrane Database Syst Rev. (2015):Cd010237. doi: 10.1002/14651858.CD010237.pub2
7. Ding, D, Huang, J, Westra, J, Cohen, DJ, Chen, Y, Andersen, BK, et al. Immediate post-procedural functional assessment of percutaneous coronary intervention: current evidence and future directions. Eur Heart J. (2021) 42:2695–707. doi: 10.1093/eurheartj/ehab186
8. Wong, MS, and Chair, SY. Changes in health-related quality of life following percutaneous coronary intervention: a longitudinal study. Int J Nurs Stud. (2007) 44:1334–42. doi: 10.1016/j.ijnurstu.2006.07.011
9. Karimi, M, and Brazier, J. Health, health-related quality of life, and quality of life: what is the difference? PharmacoEconomics. (2016) 34:645–9. doi: 10.1007/s40273-016-0389-9
10. Muhammad, I, He, HG, Kowitlawakul, Y, and Wang, W. Narrative review of health-related quality of life and its predictors among patients with coronary heart disease. Int J Nurs Pract. (2016) 22:4–14. doi: 10.1111/ijn.12356
11. Thompson, DR, and Yu, CM. Quality of life in patients with coronary heart disease-I: assessment tools. Health Qual Life Outcomes. (2003):42. doi: 10.1186/1477-7525-1-42
12. Zhou, T, Guan, H, Wang, L, Zhang, Y, Rui, M, and Ma, A. Health-related quality of life in patients with different diseases measured with the Eq-5D-5L: a systematic review. Front Public Health. (2021):675523. doi: 10.3389/fpubh.2021.675523
13. EuroQol Group. EuroQol--a new Facility for the Measurement of health-related quality of life. Health Policy. (1990) 16:199–208. doi: 10.1016/0168-8510(90)90421-9
14. Jia, YX, Cui, FQ, Li, L, Zhang, DL, Zhang, GM, Wang, FZ, et al. Comparison between the EQ-5D-5L and the EQ-5D-3L in patients with hepatitis B. Qual Life Res. (2014) 23:2355–63. doi: 10.1007/s11136-014-0670-3
15. Tordrup, D, Mossman, J, and Kanavos, P. Responsiveness of the EQ-5D to clinical change: is the patient experience adequately represented? Int J Technol Assess Health Care. (2014) 30:10–9. doi: 10.1017/S0266462313000640
16. Herdman, M, Gudex, C, Lloyd, A, Janssen, M, Kind, P, Parkin, D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. (2011) 20:1727–36. doi: 10.1007/s11136-011-9903-x
17. Devlin, NJ, and Brooks, R. EQ-5D and the Euroqol group: past, present and future. Appl Health Econ Health Policy. (2017) 15:127–37. doi: 10.1007/s40258-017-0310-5
18. Copay, AG, Subach, BR, Glassman, SD, Polly, DW Jr, and Schuler, TC. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J. (2007) 7:541–6. doi: 10.1016/j.spinee.2007.01.008
19. Jaeschke, R, Singer, J, and Guyatt, GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. (1989) 10:407–15. doi: 10.1016/0197-2456(89)90005-6
20. Juniper, EF, Guyatt, GH, Willan, A, and Griffith, LE. Determining a minimal important change in a disease-specific quality of life questionnaire. J Clin Epidemiol. (1994) 47:81–7. doi: 10.1016/0895-4356(94)90036-1
21. Fayers, P, and Machin, D. Quality of life: the assessment, analysis and interpretation ofpatient-reported outcomes. 2nd ed Wiley Blackwell (2014).
22. Tsiplova, K, Pullenayegum, E, Cooke, T, and Xie, F. EQ-5D-derived health utilities and minimally important differences for chronic health conditions: 2011 Commonwealth Fund survey of sicker adults in Canada. Qual Life Res. (2016) 25:3009–16. doi: 10.1007/s11136-016-1336-0
23. Beaton, DE. Understanding the relevance of measured change through studies of responsiveness. Spine (Phila Pa 1976). (2000) 25:3192–9. doi: 10.1097/00007632-200012150-00015
24. Hägg, O, Fritzell, P, and Nordwall, A. The clinical importance of changes in outcome scores after treatment for chronic low Back pain. Eur Spine J. (2003) 12:12–20. doi: 10.1007/s00586-002-0464-0
25. Bilbao, A, García-Pérez, L, Arenaza, JC, García, I, Ariza-Cardiel, G, Trujillo-Martín, E, et al. Psychometric properties of the EQ-5D-5L in patients with hip or knee osteoarthritis: reliability validity and responsiveness. Qual Life Res. (2018) 27:2897–908. doi: 10.1007/s11136-018-1929-x
26. Terwee, CB, Bot, SD, de Boer, MR, van der Windt, DA, Knol, DL, Dekker, J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. (2007) 60:34–42. doi: 10.1016/j.jclinepi.2006.03.012
27. Coretti, S, Ruggeri, M, and McNamee, P. The minimum clinically important difference for EQ-5D index: a critical review. Expert Rev Pharmacoecon Outcomes Res. (2014) 14:221–33. doi: 10.1586/14737167.2014.894462
28. Payakachat, N, Ali, MM, and Tilford, JM. Can the EQ-5D detect meaningful change? A systematic review. PharmacoEconomics. (2015) 33:1137–54. doi: 10.1007/s40273-015-0295-6
29. Chen, P, Lin, KC, Liing, RJ, Wu, CY, Chen, CL, and Chang, KC. Validity, responsiveness, and minimal clinically important difference of EQ-5D-5l in stroke patients undergoing rehabilitation. Qual Life Res. (2016) 25:1585–96. doi: 10.1007/s11136-015-1196-z
30. Cheng, Q, Kularatna, S, Lee, XJ, Graves, N, and Pacella, RE. Comparison of EQ-5D-5L and SPVU-5D for measuring quality of life in patients with venous leg ulcers in an Australian setting. Qual Life Res. (2019) 28:1903–11. doi: 10.1007/s11136-019-02128-6
31. Hu, X, Jing, M, Zhang, M, Yang, P, and Yan, X. Responsiveness and minimal clinically important difference of the EQ-5D-5L in cervical intraepithelial neoplasia: a longitudinal study. Health Qual Life Outcomes. (2020):324. doi: 10.1186/s12955-020-01578-8
32. Nolan, CM, Longworth, L, Lord, J, Canavan, JL, Jones, SE, Kon, SS, et al. The EQ-5D-5l health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax. (2016) 71:493–500. doi: 10.1136/thoraxjnl-2015-207782
33. Bilbao, A, García-Pérez, L, Arenaza, JC, García, I, and Martín-Fernández, J. Psychometric properties of the Eq-5d-5l in patients with hip or knee osteoarthritis: reliability, validity and responsiveness. Qual Life Res. (2018):1–12.
34. Yang, LX, and Guo, RW. The 《Chinese guidelines for percutaneous coronary intervention (2016)》 guide the clinical practice of acute coronary syndrome (in Chinese). Chin J Interv Cardiol. (2016) 24:714–17. doi: 10.3969/j.issn.1004-8812.2016.12.013
35. Luo, N, Li, M, Liu, GG, Lloyd, A, de Charro, F, and Herdman, M. Developing the Chinese version of the new 5-level EQ-5D descriptive system: the response scaling approach. Qual Life Res. (2013) 22:885–90. doi: 10.1007/s11136-012-0200-0
36. Luo, N, Liu, G, Li, M, Guan, H, Jin, X, and Rand-Hendriksen, K. Estimating an EQ-5D-5L value set for China. Value Health. (2017) 20:662–9. doi: 10.1016/j.jval.2016.11.016
37. Spertus, JA, Winder, JA, Dewhurst, TA, Deyo, RA, Prodzinski, J, McDonell, M, et al. Development and evaluation of the Seattle angina questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. (1995) 25:333–41. doi: 10.1016/0735-1097(94)00397-9
38. Garratt, AM, Hutchinson, A, and Russell, I. The UK version of the Seattle angina questionnaire (SAQ-UK): reliability, validity and responsiveness. J Clin Epidemiol. (2001) 54:907–15. doi: 10.1016/s0895-4356(01)00352-3
39. Liu, XT, Kong, SP, Liao, ZY, and Lu, SK. Assessment study on physical Function and the quality of life for CHD patients with SAQ. Chin J Behav Med. (1997) 6:49–51.
40. Wright, JG, and Young, NL. A comparison of different indices of responsiveness. J Clin Epidemiol. (1997) 50:239–46. doi: 10.1016/S0895-4356(96)00373-3
41. Murawski, MM, and Miederhoff, PA. On the generalizability of statistical expressions of health related quality of life instrument responsiveness: a data synthesis. Qual Life Res. (1998) 7:11–22. doi: 10.1023/a:1008828720272
42. Husted, JA, Cook, RJ, Farewell, VT, and Gladman, DD. Methods for assessing responsiveness: a critical review and recommendations. J Clin Epidemiol. (2000) 53:459–68. doi: 10.1016/S0895-4356(99)00206-1
43. Muller, K. Statistical power analysis for the behavioral sciences. Technometrics. (1988) 31:499–500. doi: 10.1080/00401706.1989.10488618
44. Revicki, D, Hays, RD, Cella, D, and Sloan, J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol. (2008) 61:102–9. doi: 10.1016/j.jclinepi.2007.03.012
45. Norman, GR, Sloan, JA, and Wyrwich, KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. (2003) 41:582–92. doi: 10.1097/01.MLR.0000062554.74615.4C
46. McClure, NS, Sayah, FA, Ohinmaa, A, and Johnson, JA. Minimally important difference of the Eq-5d-5l index score in adults with type 2 diabetes. Value Health. (2018) 21:1090–7. doi: 10.1016/j.jval.2018.02.007
47. Cheung, YT, Foo, YL, Shwe, M, Tan, YP, Fan, G, Yong, WS, et al. Minimal clinically important difference (MCID) for the functional assessment of cancer therapy: cognitive function (FACT-Cog) in breast cancer patients. J Clin Epidemiol. (2014) 67:811–20. doi: 10.1016/j.jclinepi.2013.12.011
48. Youden, WJ. Index for rating diagnostic tests. Cancer. (1950) 3:32–5. doi: 10.1002/1097-0142(1950)3:1<32::AID-CNCR2820030106>3.0.CO;2-3
49. Sedaghat, AR. Understanding the minimal clinically important difference (MCID) of patient-reported outcome measures. Otolaryngol Head Neck Surg. (2019) 161:551–60. doi: 10.1177/0194599819852604
50. Luo, N, Johnson, J, and Coons, SJ. Using instrument-defined health state transitions to estimate minimally important differences for four preference-based health-related quality of life instruments. Med Care. (2010) 48:365–71. doi: 10.1097/MLR.0b013e3181c162a2
51. Wyrwich, KW, Tierney, WM, and Wolinsky, FD. Further evidence supporting an SEM-based criterion for identifying meaningful intra-individual changes in health-related quality of life. J Clin Epidemiol. (1999) 52:861–73. doi: 10.1016/S0895-4356(99)00071-2
52. Wyrwich, KW, Nienaber, NA, Tierney, WM, and Wolinsky, FD. Linking clinical relevance and statistical significance in evaluating intra-individual changes in health-related quality of life. Med Care. (1999) 37:469–78. doi: 10.1097/00005650-199905000-00006
53. de Boer, MR, de Vet, HC, Terwee, CB, Moll, AC, Völker-Dieben, HJ, and van Rens, GH. Changes to the subscales of two vision-related quality of life questionnaires are proposed. J Clin Epidemiol. (2005) 58:1260–8. doi: 10.1016/j.jclinepi.2005.04.007
54. Lyman, S, Lee, YY, McLawhorn, AS, Islam, W, and MacLean, CH. What are the minimal and substantial improvements in the Hoos and Koos and Jr versions after Total joint replacement? Clin Orthop Relat Res. (2018) 476:2432–41. doi: 10.1097/CORR.0000000000000456
55. Guyatt, G, Walter, S, and Norman, G. Measuring change over time: assessing the usefulness of evaluative instruments. J Chronic Dis. (1987) 40:171–8. doi: 10.1016/0021-9681(87)90069-5
56. Crossman-Barnes, CJ, Sach, T, Wilson, A, and Barton, G. The construct validity and responsiveness of the EQ-5D-5L, AQL-5D and a bespoke TTO in acute asthmatics. Qual Life Res. (2020) 29:619–27. doi: 10.1007/s11136-019-02345-z
57. Golicki, D, Niewada, M, Karlińska, A, Buczek, J, Kobayashi, A, Janssen, MF, et al. Comparing responsiveness of the EQ-5D-5L, EQ-5D-3L, and EQ VAS in stroke patients. Qual Life Res. (2015) 24:1555–63. doi: 10.1007/s11136-014-0873-7
58. Yazdani-Bakhsh, R, Javanbakht, M, Sadeghi, M, Mashayekhi, A, Ghaderi, H, and Rabiei, K. Comparison of health-related quality of life after percutaneous coronary intervention and coronary artery bypass surgery. ARYA Atheroscler. (2016) 12:124–31.
59. Wyrwich, KW, Bullinger, M, Aaronson, N, Hays, RD, Patrick, DL, and Symonds, T. Estimating clinically significant differences in quality of life outcomes. Qual Life Res. (2005) 14:285–95. doi: 10.1007/s11136-004-0705-2
60. Crosby, RD, Kolotkin, RL, and Williams, GR. Defining clinically meaningful change in health-related quality of life. J Clin Epidemiol. (2003) 56:395–407. doi: 10.1016/S0895-4356(03)00044-1
61. Guyatt, GH, Osoba, D, Wu, AW, Wyrwich, KW, and Norman, GR. Methods to explain the clinical significance of health status measures. Mayo Clin Proc. (2002) 77:371–83. doi: 10.4065/77.4.371
62. Mouelhi, Y, Jouve, E, Castelli, C, and Gentile, S. How is the minimal clinically important difference established in health-related quality of life instruments? Review of anchors and methods. Health Qual Life Outcomes. (2020) 18:136. doi: 10.1186/s12955-020-01344-w
63. Henry, EB, Barry, LE, Hobbins, AP, McClure, NS, and O'Neill, C. Estimation of an instrument-defined minimally important difference in EQ-5D-5L index scores based on scoring algorithms derived using the EQ-VT version 2 valuation protocols. Value Health. (2020) 23:936–44. doi: 10.1016/j.jval.2020.03.003
64. McClure, NS, Sayah, FA, Xie, F, Luo, N, and Johnson, JA. Instrument-defined estimates of the minimally important difference for EQ-5D-5L index scores. Value Health. (2017) 20:644–50. doi: 10.1016/j.jval.2016.11.015
65. Su, F, Allahabadi, S, Bongbong, DN, Feeley, BT, and Lansdown, DA. Minimal clinically important difference, substantial clinical benefit, and patient acceptable symptom state of outcome measures relating to shoulder pathology and surgery: a systematic review. Curr Rev Musculoskelet Med. (2021) 14:27–46. doi: 10.1007/s12178-020-09684-2
66. Hoehle, LP, Phillips, KM, Speth, MM, Caradonna, DS, Gray, ST, and Sedaghat, AR. Responsiveness and minimal clinically important difference for the EQ-5D in chronic rhinosinusitis. Rhinology. (2019) 57:110–6. doi: 10.4193/Rhin18.122
67. Cella, D, Hahn, EA, and Dineen, K. Meaningful change in cancer-specific quality of life scores: differences between improvement and worsening. Qual Life Res. (2002) 11:207–21. doi: 10.1023/a:1015276414526
68. Kvam, AK, Fayers, P, and Wisloff, F. What changes in health-related quality of life matter to multiple myeloma patients? A prospective study. Eur J Haematol. (2010) 84:345–53. doi: 10.1111/j.1600-0609.2009.01404.x
69. Beaton, DE, Boers, M, and Wells, GA. Many faces of the minimal clinically important difference (MCID): a literature review and directions for future research. Curr Opin Rheumatol. (2002) 14:109–14. doi: 10.1097/00002281-200203000-00006
70. Kolin, DA, Moverman, MA, Pagani, NR, Puzzitiello, RN, Dubin, J, Menendez, ME, et al. Substantial inconsistency and variability exists among minimum clinically important differences for shoulder arthroplasty outcomes: a systematic review. Clin Orthop Relat Res. (2022) 480:1371–83. Epub 2022/03/19. doi: 10.1097/CORR.0000000000002164
71. Koh, Y, Stehli, J, Martin, C, Brennan, A, Dinh, DT, Lefkovits, J, et al. Does sex predict quality of life after acute coronary syndromes: an Australian, state-wide multicentre prospective cohort study. BMJ Open. (2019) 9:e034034. doi: 10.1136/bmjopen-2019-034034
72. Biering, K, Frydenberg, M, and Hjollund, NH. Self-reported health following percutaneous coronary intervention: results from a cohort followed for 3 years with multiple measurements. Clin Epidemiol. (2014) 6:441–9. doi: 10.2147/CLEP.S65476
Keywords: responsiveness, minimal clinically important difference, minimal detectable change, EQ-5D-5L, coronary heart disease, percutaneous coronary intervention
Citation: Zheng Y, Dou L, Fu Q and Li S (2023) Responsiveness and minimal clinically important difference of EQ-5D-5L in patients with coronary heart disease after percutaneous coronary intervention: A longitudinal study. Front. Cardiovasc. Med. 10:1074969. doi: 10.3389/fcvm.2023.1074969
Edited by:
Tommaso Gori, Johannes Gutenberg University Mainz, GermanyReviewed by:
Rongjing Ding, Peking University, ChinaAkhmetzhan Galimzhanov, Semey State Medical University, Kazakhstan
Copyright © 2023 Zheng, Dou, Fu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Dou, ZG91bGVpQHNkdS5lZHUuY24=
 Yu Zheng1,2,3
Yu Zheng1,2,3 Lei Dou
Lei Dou Shunping Li
Shunping Li