
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 25 November 2022
Sec. General Cardiovascular Medicine
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.991479
This article is part of the Research Topic The Role of Stem Cells, RNA Binding Proteins and Non-Coding RNAs in Diabetes and Vascular Diseases View all 8 articles
Background: Patients with ST-segment elevation myocardial infarction (STEMI) with diabetes mellitus (DM) had higher mortality and poorer prognosis than those without DM. Previous studies had demonstrated the effectiveness of regional network systems (RNS) for reperfusion therapy in patients with STEMI. However, the differences in nursing care with RNS in subgroups of patients with DM with STEMI were unclear. Our study aimed to evaluate the validity of RNS in reperfusion therapy in patients with STEMI with or without DM.
Methods: We retrospectively enrolled patients with STEMI who received reperfusion therapy at the chest pain center of the 920th Hospital in Kunming City, Yunnan Province from 2019 to 2021. Personal information and hospitalization information for patients with STEMI were collected through the chest pain center registration system. Univariate and multivariate logistic regression were used to analyze factors associated with outcomes in patients with STEMI who received RNS. Wilcoxon rank-sum test and chi-squared test were used to analyze the differences in reperfusion therapy times and clinical outcomes between RNS and non-RNS in patients with STEMI with or without DM.
Results: This study enrolled 1,054 patients with STEMI, including 148 patients with DM and 906 patients without DM. Logistic regression analysis indicated that DM was associated with patients with STEMI who received RNS [OR 1.590 95% CI (1.034–2.446), P = 0.035]. RNS may decrease the reperfusion therapy time in patients with STEMI and patients without DM with STEMI, including the first medical contact (FMC) to door, FMC to wire and FMC to catheterization laboratory activity (all P < 0.05). However, we found no significant difference in reperfusion therapy times with and without RNS in patients with DM (all P > 0.05).
Conclusion: Regional network systems may decrease the reperfusion therapy time in patients without DM with STEMI, but no decrease was found in patients with DM with STEMI.
Diabetes mellitus (DM) was an important and common chronic disease, which can cause metabolic disorders in patients, thus resulting in vascular inflammation, endothelial dysfunction and thrombosis (1). These mechanisms may be closely associated with an elevated risk of coronary heart disease and poor prognosis. Acute heart failure or cardiogenic shock accounted for more than 80% of the mortality in hospitalize patients with DM (2). Previous studies had reported that hospital mortality rates among patients with DM with ST-segment elevation myocardial infarction (STEMI) were more than twice those of patients without DM in men and were even higher in women (2–4). Compared with patients without DM, patients with DM had higher short-term and long-term mortality rates after heart attack (5). Therefore, these patients required better medical treatment to improve their condition.
A regional network system (RNS) in the United States, involving regional collaborative treatment programs based in hospitals able to provide percutaneous coronary intervention (PCI), as implemented by state or interstate units, had been independently associated with shorter admission times (6). Previous studies had found that RNS use can decrease the reperfusion therapy time in patients with STEMI (7–9). However, patients with STEMI and DM had poorer prognosis than those without DM, and the extent to which RNS might decrease the time of reperfusion therapy in patients with DM with STEMI was unclear.
The purposes of our study were (1) to retrospectively analyze whether RNS might improve the reperfusion therapy time for patients with STEMI with or without DM, and (2) to analyze factors associated with STEMI in patients with DM to understand and improve the treatment plans for these patients.
The 920th Hospital is located in Kunming, an important central city in western China. Since its cardiology department first opened a rapid diagnosis and treatment channel for interventional diagnosis and treatment of AMI in Yunnan Province in 2003, the chest pain center (CPC) has been staffed by cardiology, emergency and ambulance pre-hospital first aid personnel in the core, joint radiology, laboratory and other related departments, and currently comprises 24 non-PCI network hospitals at the grass-roots level. A set of effective clinical pathways and a diagnostic operation flow were established; for example, a WeChat group between ambulances and network hospitals has been used to achieve timely transmission of pre-hospital electrocardiography (ECG) results and patient information to the center, thus providing a seamless connection between the green channel in the hospital and the pre-hospital first aid system. The preoperative preparation and catheterization can thus be completed before patients with STEMI and high-risk non-STEMI arrive at the hospital with emergency PCI indications. Patients can arrive directly at the catheter room, bypassing the emergency department and coronary care unit, thus greatly shortening the time before reperfusion treatment.
We retrospectively enrolled patients with STEMI who received reperfusion therapy at the CPC in the 920 Hospital in Kunming city between 2019 and 2021. Personal information and hospitalization information for patients with STEMI were collected through the CPC registration system, including age, sex, smoking history, DM history, admission status, cardiac function grade, complications (hypertension, hyperlipidemia, obesity, and family history of CVD, or coronary heart disease), remote ECG, thrombolytic therapy, clinical outcomes (hospitalization cost and time and discharge status) and reperfusion therapy time, including the first medical contact (FMC) to door (10), FMC to wire (11) and FMC to catheterization laboratory activity (CLA).
Patients with the following conditions were excluded: (1) AMI occurring in our hospital; (2) chest pain without symptoms or hemodynamic disorder lasting more than 12 h; (3) contraindications for antiplatelet or anticoagulation, such as active peptic ulcer, thrombocytopenia, severe coagulation dysfunction or hemorrhagic disease; (4) severe valvular heart disease, cardiomyopathy, severe infection or severe hepatorenal insufficiency; (5) allergy to contrast agents or stent materials; (6) refusal (of patients or family members) to accept emergency interventional examination; (7) missing information and data on diagnosis and treatment records. (8) Patients in the present study had a first STEMI and admitted within 12 h after symptom onset (FMC-door ≤ 12 h) (12, 13). The diagnostic criteria for type 2 DM were typical diabetes symptoms (polydipsia, polyuria, polyphagia or unexplained weight loss) and random venous plasma glucose ≥ 11.1 mmol/L, fasting venous plasma glucose ≥ 7.0 mmol/L or plasma glucose ≥ 11.1 mmol/L 2 h after an oral glucose tolerance test (14). AMI should be used when evidence of myocardial injury (defined as an elevation of cardiac troponin values with at least one value above the 99th percentile upper reference limit) is observed with necrosis in a clinical setting, findings are consistent with myocardial ischemia, or persistent chest discomfort or other symptoms indicating ischemia and ST segment elevation are observed in at least two adjacent leads—findings usually resulting in STEMI diagnosis (15, 16). We further divided the DM group and the non-DM group into an RNS group and No RNS group.
All patients provided informed consent for study participation, and the research study was approved by the Medical Ethics Committee of the 920 Hospital of Kunming Medical University (2015067).
Statistical analysis was performed in SPSS statistics version 26.0 (IBM Corp. Armonk, NY, USA). Continuous variables showing a normal distribution are presented as mean ± standard deviation, and continuous variables without a normal distribution are presented as median [interquartile range (IQR)]. We compared baseline characteristics between the RNS group and non-RNS group with Student’s t-test, Wilcoxon rank-sum test or chi-squared test. Univariate and multivariate logistic regression was used to analyze factors associated with outcomes in patients with STEMI who received RNS treatment. Wilcoxon rank-sum test and chi-squared test were used to analyze the differences in reperfusion therapy times and clinical outcomes in patients with STEMI with or without DM with RNS. All reported P-values were two-sided. We assumed significance at the 5% level (P < 0.05).
A flow chart of the selection process and dropouts in the present study was showed in Figure 1. A total of 1,054 patients with STEMI were enrolled, including 148 (14.0%) patients with diabetes and 906 (86.0%) patients without diabetes. Table 1 shows the baseline characteristics of patients with and without DM. Compared with patients without DM, the patients with DM included more women (36.5 vs. 23.3%, P = 0.001), and had greater hypertension (58.8 vs. 39.7%, P < 0.001) and less hyperlipidemia (35.8 vs. 45.8%, P = 0.023). A total of 114 (77.0%) patients with DM received RNS treatment, whereas 34 (23.0%) patients with DM did not. No significant differences were observed in most variables between the RNS and No RNS groups in both patients with and without DM. The RNS group, compared with the No RNS group, had less hypertension (38.3 vs. 47.3%, P = 0.042), and more patients received remote ECG (98.7 vs. 93.2%, P < 0.001) among patients with DM.
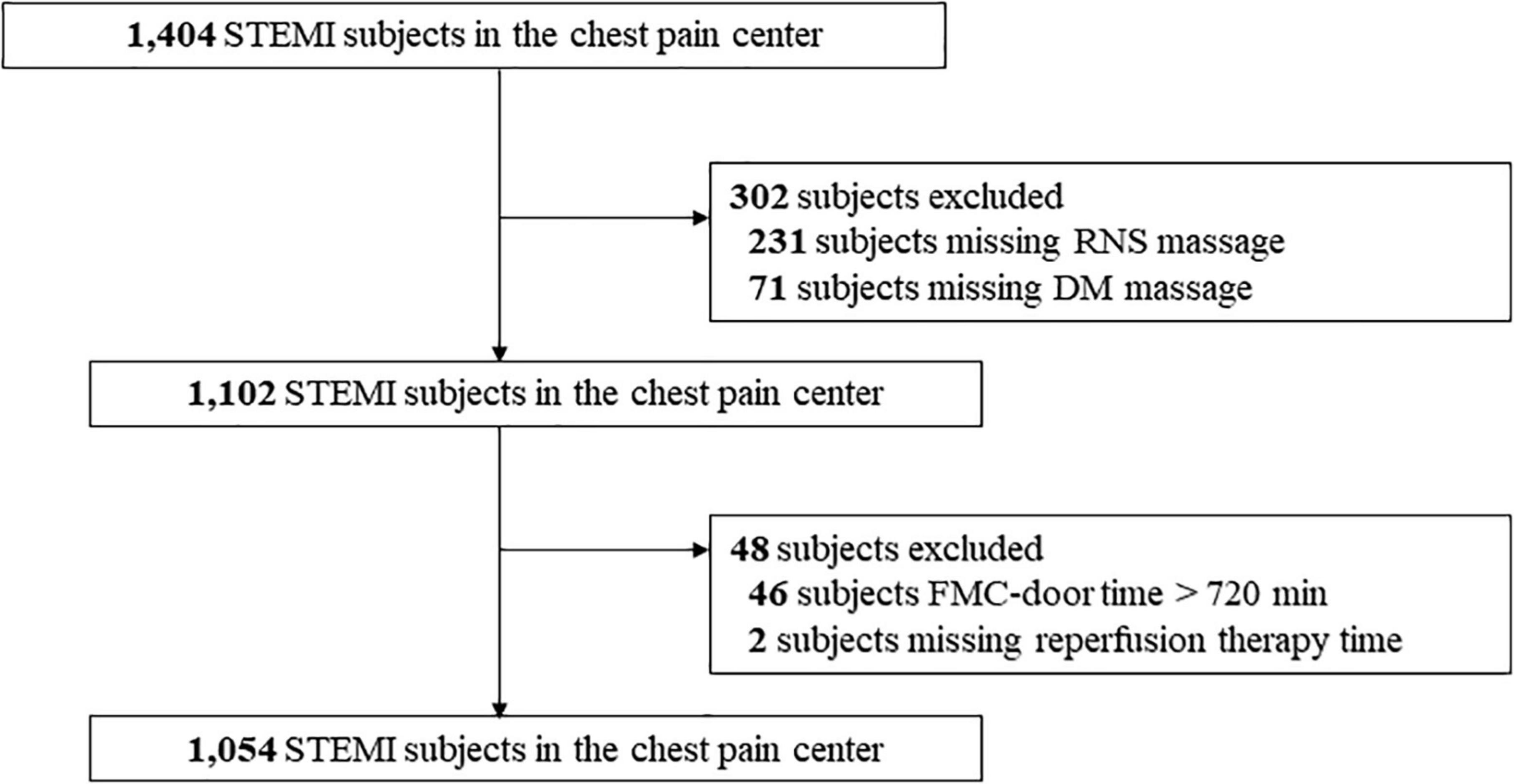
Figure 1. Flow chart of selection process and dropouts of the present study. FMC-door, the first medical contact to door. RNS, regional network systems; DM, diabetes mellitus; STEMI, ST-segment elevation myocardial infarction.
Table 2 showed serological examination results for patients with STEMI with or without DM. Compared with patients without DM, patients with DM had higher triglyceride (TG) [1.30 (0.88–2.53) vs. 1.00 (0.69–1.49), P < 0.001]and lower high-density lipoprotein cholesterol (HDL-C) [1.15 (0.99–1.42) vs. 1.25 (1.05–1.50), P = 0.042]. Patients with STEMI who received RNS had lower troponin than those who did not and this result was observed in patients with or without DM. Meanwhile, we found that patients with STEMI who received RNS had lower TG [0.97 (0.66–1.42) vs. 1.20 (0.83–1.60), P = 0.024] in no-DM patients but no found in DM patients [1.36 (0.86–2.52) vs. 1.20 (1.07–3.00), P = 0.657].
Table 3 showed the clinical outcomes of patients with STEMI with or without DM. Compared with patients without DM, patients with DM had worse adverse outcomes (death or transfer) (12.2 vs. 5.6%, P = 0.003). However, no significant difference was observed between patients with or without DM in hospitalization time [10.00 (8.00–12.00) vs. 10.00 (8.00–13.00), P = 0.171] and hospitalization costs [35.00 (27.27–46.40) vs. 35.00 (28.32–43.69), P = 0.846]. We found no statistically significant differences in hospitalization time, hospitalization costs and adverse outcomes between the RNS and No RNS groups in both patients with and without DM (all P > 0.05).
Univariate logistic regression analysis indicated that hospital state [0.525, 95%CI (0.320–0.860), P = 0.011], Killip classification [1.476, 95%CI (1.123–1.940), P = 0.005] and DM [1.553, 95%CI (1.018–2.367), P = 0.041] were associated with receiving RNS. Multivariate logistic regression analysis indicated that hospital state [0.515, 95%CI (0.311–0.853), P = 0.010], Killip classification [1.425, 95%CI (1.072–1.893), P = 0.015] and DM [1.590, 95%CI (1.034–2.446), P = 0.035] were still associated with receiving RNS (Table 4).
In the total population, RNS decreased the reperfusion therapy time in all patients with STEMI, including FMC-door [186 (140–282) vs. 220 (154–316), P = 0.002], FMC-wire [220 (169–314) vs. 247 (187–352), P = 0.005] and FMC-CLA [160 (114–257) vs. 197 (129–295), P = 0.003] (Figure 2). RNS also decreased the findings for patients without DM, including FMC-door [188 (140–284) vs. 229 (155–322), P = 0.001], FMC-wire [221 (169–315) vs. 255 (188–356), P = 0.004] and FMC-CLA [160 (114–257) vs. 201 (133–299), P = 0.003] (Figure 3). However, no statistically significant difference in reperfusion therapy time was observed between the No RNS group and RNS group in patients with DM (Figure 4).
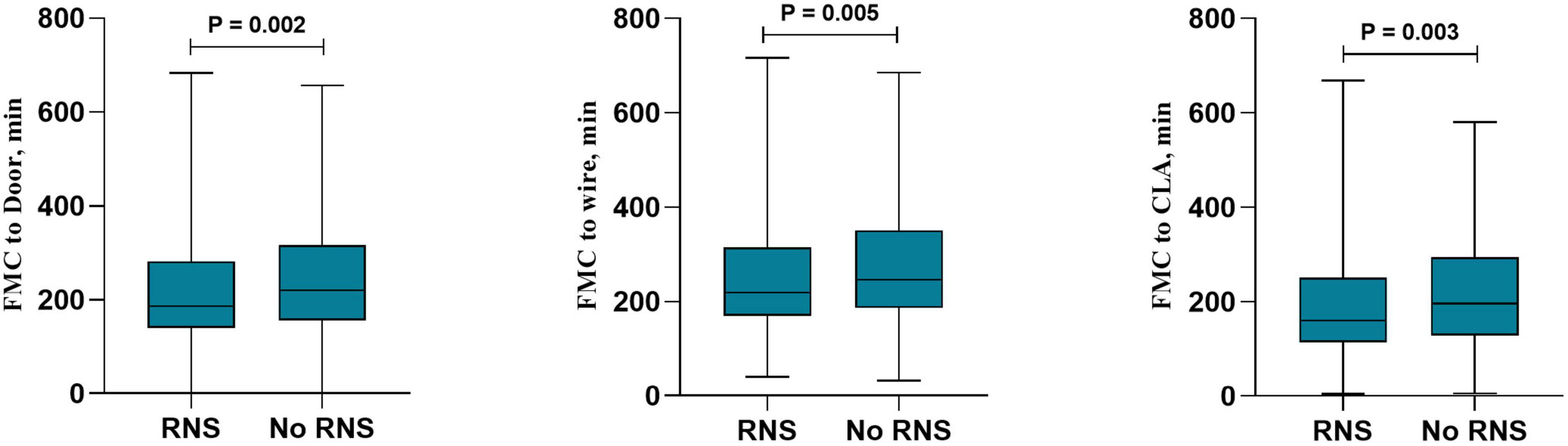
Figure 2. Reperfusion therapy time between RNS and non-RNS in all patients with STEMI. RNS, receive regional network system; NO-RNS, no receive regional network system; FMC-door, the first medical contact to door; FMC-CLA, FMC to catheterization laboratory activity.
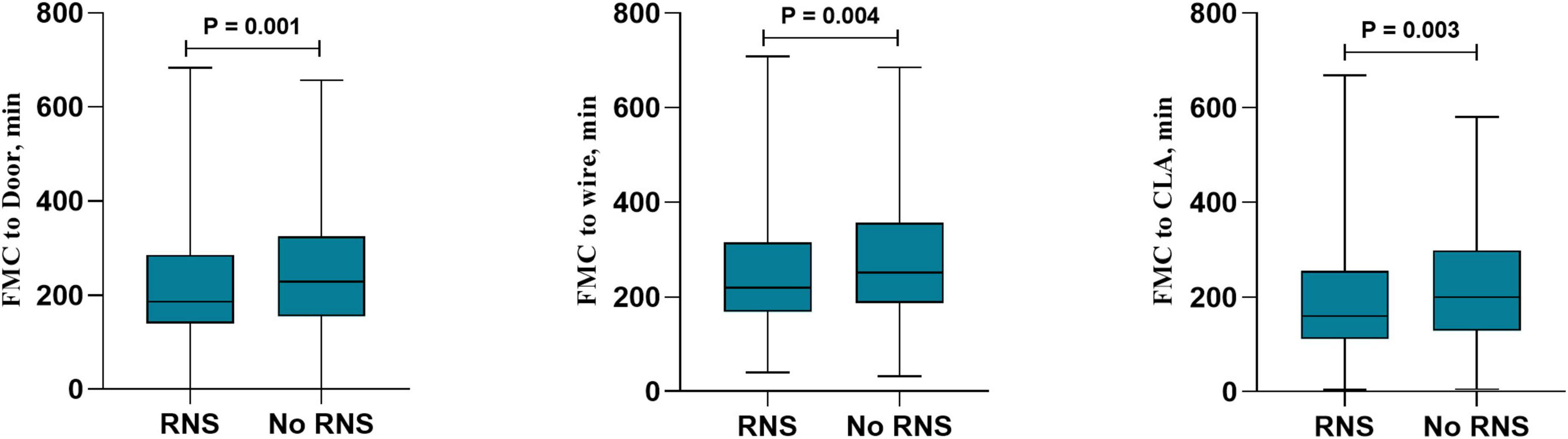
Figure 3. Reperfusion therapy time between RNS and non-RNS in patients without DM and with STEMI. RNS, receive regional network system; NO-RNS, no receive regional network system; FMC-door, the first medical contact to door; FMC-CLA, FMC to catheterization laboratory activity.
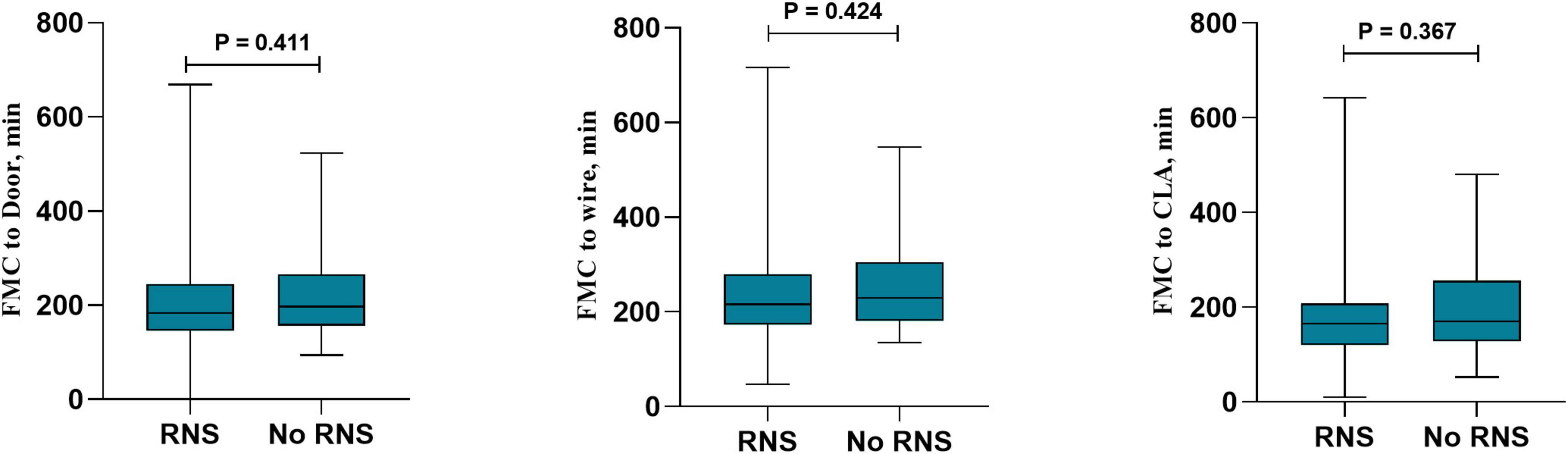
Figure 4. Reperfusion therapy time between RNS and non-RNS in patients with DM and STEMI. RNS, receive regional network system; NO-RNS, no receive regional network system; FMC-door, the first medical contact to door; FMC-CLA, FMC to catheterization laboratory activity.
We explored the RNS-associated differences in clinical characteristics, clinical outcomes and reperfusion therapy time among patients with STEMI with or without DM. This retrospective study indicated that RNS may decrease reperfusion therapy time in all patients with STEMI and in patients without DM with STEMI; however, no decrease was found in patients with DM with STEMI.
Diabetes mellitus was a major risk factor for cardiovascular disease that may nearly double the risk of AMI (17). DM and impaired glucose tolerance were common in patients with AMI. We identified 148 patients with DM and STEMI, accounting for 14%, a finding approximately consistent with the results of previous studies (18–21). Our study found that patients with DM had more hypertension, higher TG and lower HDL-C than those without DM. These cardiovascular factors may lead to poorer prognosis in patients with DM (22).
Over the past decade, advances in PCI and surgical techniques had greatly improved the treatment of patients with STEMI. The RNS had been demonstrated to effectively decrease reperfusion therapy time in STEMI patients, but the emergence of diabetes may lead to poor prognosis in patients with STEMI. However, it was unclear whether RNS might improve the management and prognosis of patients with DM and STEMI. Our study conducted the first exploration of the differences in reperfusion therapy time in patients with STEMI with or without DM according to the presence or absence of RNS. Logistic regression indicated that DM was associated with receipt of RNS. This indicated that patients with DM were more willing to accept RNS. It was not surprising. DM patients had worse prognosis and complications than no DM and better nursing strategies may be needed in DM patients. Physicians in RNS were familiar with STEMI nursing procedures, and can identify patients’ conditions and provide diagnosis and treatment in time. Our hypothesis was confirmed by serological examination results that patients with STEMI who received RNS had lower troponin, an important risk factor for the prognosis of AMI (23), than those who did not, and this result was observed in both DM and no DM patient. It suggested that RNS may timely diagnose and treat patients with DM, and effectively decrease the risk of poor prognosis to some extent.
Our study found that RNS may decrease reperfusion therapy time in STEMI patients without DM. It was not difficult to explain. Among patients without DM, a higher proportion of remote electrocardiograms were performed in patients with RNS compared with No RNS. Some studies showed that remote ECG can effectively predict the adverse outcome in patients with myocardial infarction and decrease reperfusion therapy time (24–26). RNS was therefore beneficial for the management of patients with STEMI without DM.
However, we found that RNS may not decrease reperfusion therapy time. Possible explanations based on the analyzed results for this finding may be that: (1) In DM patients, there was no difference in remote ECG between RNS group and No RNS group. Remote ECG was a crucial examination to identifying patients with STEMI and DM. One study showed that the incidence of first asymptomatic myocardial infarction and asymptomatic myocardial infarction accounted for 25% of all myocardial infarction in DM patients with no history of atherosclerotic events (27). A study reported that ECG changes in patients with myocardial infarction with DM were not typical, which also caused delays in treatment (28). It suggested that the condition of patients with DM has been suggested to require special management in many aspects beyond ECG. (2) We believe that triglyceride (TG) was also one of the factors. One study found that TG may be an independent risk factor and predictor of DM (29), and another study reported that increasing TG levels within the normal range also led to a sustained increase in the incidence of DM in healthy individuals without metabolic syndrome. These findings indicated that almost everyone may benefit from lower TG. We found that there was no significant difference in TG between RNS and No RNS patients in DM patients. However, RNS group had lower TG in patients without DM, indicating that it was insufficient for RNS in the treatment of blood lipids in DM patients. (3) When patients with DM presented with symptoms of myocardial infarction, their symptoms were often atypical or unusual (30, 31), and their chest pain might not have corresponded to that typical of a heart attack. And it was associated with cardiac autonomic neuropathy, a complication of diabetes, may lead to changes in pain perception (32).
This study had some limitations. First, these data represented relatively small hospital samples and may partially explain the effects of RNS on reperfusion therapy in patients with STEMI with or without DM, but our result found that there was no significant decreasing trend in reperfusion therapy time in patients with DM. A further increase in sample size is necessary for analysis. Second, we might not have considered all relevant confounding factors, and we could not rule out the possibility of reverse causality. Finally, some patients with DM had type 1 DM, but we were unable to perform subgroup analysis to analyze the effects of RNS on the reperfusion therapy time between the two types of diabetes.
RNS may decrease the reperfusion therapy time in patients with STEMI and without DM. However, we observed no decrease in patients with STEMI and DM, who required enhanced diagnostic procedures and aggressive treatment strategies, including ECG detection and treatment of dyslipidemia. Clinicians must pay attention to prevention strategies, particularly to eliminate modifiable risk factors in patients with AMI and DM. Careful assessment of patients with diabetes and adequate education for the target population are necessary to improve overall survival (33, 34).
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of the 920 Hospital of Kunming Medical University (2015067). The patients/participants provided their written informed consent to participate in this study.
RG was the study guarantor, designed the project, and planned the statistical analysis. XL and LL drafted and revised the manuscript. XL, QY, LY, and LD collected and monitored the data collection. All authors approved the final draft of the manuscript for publication.
This study was supported by the Science and Technology Department of Yunnan Province (202101AY070001-030) and the 920th Hospital of Joint Logistics Support Force, PLA (2020YGD11).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
DM, Diabetes mellitus; STEMI, ST-segment elevation myocardial infarction; RNS, regional network systems; CPC, chest pain Center; FMC, first medical contact; CLA, catheterization laboratory activity; AMI, acute myocardial infarction; ECG, electrocardiography; OGTT, oral glucose tolerance test.
1. Creager MA, Lüscher TF, Cosentino F, Beckman JA. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Circulation. (2003) 108:1527–32.
2. Savage MP, Krolewski AS, Kenien GG, Lebeis MP, Christlieb AR, Lewis SM. Acute myocardial infarction in diabetes mellitus and significance of congestive heart failure as a prognostic factor. Am J Cardiol. (1988) 62(10 Pt. 1):665–9. doi: 10.1016/0002-9149(88)91199-x
3. Bradley R, Bryfogle J. Survival of diabetic patients after myocardial infarction. Am J Med. (1956) 20:207–16.
4. Soler N, Bennett M, Lamb P, Pentecost B, Fitzgerald M, Malins J. Coronary care for myocardial infarction in diabetics. Lancet. (1974) 303:475–7.
5. Milazzo V, Cosentino N, Genovese S, Campodonico J, Mazza M, De Metrio M, et al. Diabetes mellitus and acute myocardial infarction: impact on short and long-term mortality. Diabetes. (2020) 1307:153–69.
6. Glickman SW, Lytle BL, Ou F-S, Mears G, O’Brien S, Cairns CB, et al. Care processes associated with quicker door-in–door-out times for patients with St-elevation–myocardial infarction requiring transfer: results from a statewide regionalization program. Circ Cardiovasc Qual Outcomes. (2011) 4:382–8. doi: 10.1161/CIRCOUTCOMES.110.959643
7. Yan J, Wang Z, Xu LJ, Liang Y. Effects of new regional cooperative rescue model on patients with St-elevation myocardial infarction. Int J Cardiol. (2014) 177:494–6.
8. Glickman SW, Granger CB, Ou F-S, O’Brien S, Lytle BL, Cairns CB, et al. Impact of a statewide St-segment–elevation myocardial infarction regionalization program on treatment times for women, minorities, and the elderly. Circ Cardiovasc Qual Outcomes. (2010) 3:514–21. doi: 10.1161/CIRCOUTCOMES.109.917112
9. Niles NW, Conley SM, Yang RC, Vanichakarn P, Anderson TA, Butterly JR, et al. Primary percutaneous coronary intervention for patients presenting with st-segment elevation myocardial infarction: process improvement in a rural St-segment elevation myocardial infarction receiving center. Progr Cardiovasc Dis. (2010) 53:202–9. doi: 10.1016/j.pcad.2010.08.004
10. Maor E, Abend Y, Ganem D, Kusniec F, Grosman-Rimon L, Elbaz-Greener G, et al. Sex disparities in first medical contact of patients with suspected acute coronary syndrome using telemedicine technology. Telemed J E Health. (2020) 26:411–8. doi: 10.1089/tmj.2019.0036
11. Gopar-Nieto R, Araiza-Garaygordobil D, Raymundo-Martínez GI, Martínez-Amezcua P, Cabello-López A, Manzur-Sandoval D, et al. Demographic description and outcomes of a metropolitan network for myocardial infarction treatment. Arch Cardiol México. (2021) 91:167–77. doi: 10.24875/ACM.20000133
12. Zhang Y, Wang S, Cheng Q, Zhang J, Qi D, Wang X, et al. Reperfusion strategy and in-hospital outcomes for St elevation myocardial infarction in secondary and tertiary hospitals in predominantly Rural Central China: a multicentre, prospective and observational study. BMJ Open. (2021) 11:e053510. doi: 10.1136/bmjopen-2021-053510
13. Lønborg J, Schoos MM, Kelbæk H, Holmvang L, Steinmetz J, Vejlstrup N, et al. Impact of system delay on infarct size, myocardial salvage index, and left ventricular function in patients with St-segment elevation myocardial infarction. Am Heart J. (2012) 164:538–46. doi: 10.1016/j.ahj.2012.07.021
14. Association AD. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2019. Diabetes Care. (2019) 42(Suppl_1):S13–28. doi: 10.2337/dc19-S002
15. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. (2012) 60:1581–98. doi: 10.1016/j.jacc.2012.08.001
16. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with St-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with St-segment elevation of the European society of cardiology (ESC). Eur Heart J. (2018) 39:119–77.
17. Members ATF, Rydén L, Grant PJ, Anker SD, Berne C, Cosentino F, et al. ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the Easd: the task force on diabetes, pre-diabetes, and cardiovascular diseases of the European society of cardiology (ESC) and developed in collaboration with the European association for the study of diabetes (EASD). Eur Heart J. (2013) 34:3035–87. doi: 10.1093/eurheartj/eht108
18. Han Z, Yan-min Y, Jun Z, Li-sheng L, Hui-qiong T, Yao L. Prognostic value of admission heart rate in patients with St-Segment elevation myocardial infarction: role of type 2 diabetes mellitus. BMC Cardiovasc Disord. (2012) 12:104. doi: 10.1186/1471-2261-12-104
19. Madsen JK, Thomsen BL, Sorensen JN, Kjeldgaard KM, Kromann-Andersen B. Risk factors and prognosis after discharge for patients admitted because of suspected acute myocardial infarction with and without confirmed diagnosis. Am J Cardiol. (1987) 59:1064–70.
20. Mak K-H, Moliterno DJ, Granger CB, Miller DP, White HD, Wilcox RG, et al. Influence of diabetes mellitus on clinical outcome in the thrombolytic era of acute myocardial infarction. J Am Coll Cardiol. (1997) 30:171–9.
21. Barbash GI, White HD, Modan M, Van de Werf F. Trial†IotITPASM. Significance of diabetes mellitus in patients with acute myocardial infraction receiving thrombolytic theraphy. J Am Coll Cardiol. (1993) 22:707–13.
22. Kip KE, Faxon DP, Detre KM, Yeh W, Kelsey SF, Currier JW. Coronary angioplasty in diabetic patients: the national heart, lung, and blood institute percutaneous transluminal coronary angioplasty registry. Circulation. (1996) 94:1818–25. doi: 10.1161/01.cir.94.8.1818
23. Tang O, Matsushita K, Coresh J, Ndumele C, McEvoy JW, Sharrett AR, et al. High-sensitivity cardiac troponin I and T for cardiovascular risk stratification in adults with diabetes. Diabetes Care. (2020) 43:e144–6. doi: 10.2337/dc20-1312
24. Zègre Hemsey JK, Dracup K, Fleischmann KE, Sommargren CE, Paul SM, Drew BJ. Prehospital electrocardiographic manifestations of acute myocardial ischemia independently predict adverse hospital outcomes. J Emerg Med. (2013) 44:955–61. doi: 10.1016/j.jemermed.2012.07.089
25. Kerem Y, Eastvold JS, Faragoi D, Strasburger D, Motzny SE, Kulstad EB. The role of prehospital electrocardiograms in the recognition of st-segment elevation myocardial infarctions and reperfusion times. J Emerg Med. (2014) 46:202–7. doi: 10.1016/j.jemermed.2013.08.084
26. Brunetti ND, Dell’Anno A, Martone A, Natale E, Rizzon B, Di Cillo O, et al. Prehospital Ecg transmission results in shorter door-to-wire time for stemi patients in a remote mountainous region. Am J Emerg Med. (2020) 38:252–7. doi: 10.1016/j.ajem.2019.04.046
27. Soejima H, Ogawa H, Morimoto T, Okada S, Sakuma M, Nakayama M, et al. One quarter of total myocardial infarctions are silent manifestation in patients with type 2 diabetes mellitus. J Cardiol. (2019) 73:33–7. doi: 10.1016/j.jjcc.2018.05.017
28. Schmitz T, Thilo C, Linseisen J, Heier M, Peters A, Kuch B, et al. Admission Ecg changes predict short term-mortality after acute myocardial infarction less reliable in patients with diabetes. Sci Rep. (2021) 11:6307. doi: 10.1038/s41598-021-85674-9
29. Wang L, Cong HL, Zhang JX, Hu YC, Wei A, Zhang YY, et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with diabetes and acute coronary syndrome. Cardiovasc Diabetol. (2020) 19:80. doi: 10.1186/s12933-020-01054-z
30. Berman N, Jones MM, De Coster DA. ‘Just like a normal pain’, what do people with diabetes mellitus experience when having a myocardial infarction: a qualitative study recruited from Uk hospitals. BMJ Open. (2017) 7:e015736. doi: 10.1136/bmjopen-2016-015736
31. Funk M, Naum JB, Milner KA, Chyun D. Presentation and symptom predictors of coronary heart disease in patients with and without diabetes. Am J Emerg Med. (2001) 19:482–7.
32. Vinik AI, Ziegler D. Diabetic cardiovascular autonomic neuropathy. Circulation. (2007) 115:387–97. doi: 10.1161/circulationaha.106.634949
33. Gradišer M, Dilber D, Cmrečnjak J, Ostrički B, Bilić-Ćurčić I. Comparison of the hospital arrival time and differences in pain quality between diabetic and non-diabetic stemi patients. Int J Environ Res Public Health. (2015) 12:1387–96. doi: 10.3390/ijerph120201387
Keywords: ST-segment elevation myocardial infarction, reperfusion therapy, regional network systems, diabetes mellitus, FMC to wire
Citation: Li X, Lu L, Yuan Q, Yang L, Du L and Guo R (2022) Validity of regional network systems on reperfusion therapy in diabetes mellitus and non-diabetes mellitus patients with ST-segment elevation myocardial infarction. Front. Cardiovasc. Med. 9:991479. doi: 10.3389/fcvm.2022.991479
Received: 11 July 2022; Accepted: 11 November 2022;
Published: 25 November 2022.
Edited by:
Gian Marco Rosa, San Martino Hospital (IRCCS), ItalyReviewed by:
Rocco Edoardo Stio, San Camillo-Forlanini Hospital, ItalyCopyright © 2022 Li, Lu, Yuan, Yang, Du and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ruiwei Guo, Z3J3NzcxMjEwQDE2My5jb20=, orcid.org/0000-0002-3617-6169
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.