
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 11 October 2022
Sec. Atherosclerosis and Vascular Medicine
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.973530
 Qianhao Zhao1,2†
Qianhao Zhao1,2† Kun Yin1,2†
Kun Yin1,2† Nan Zhou1,2†
Nan Zhou1,2† Qiuping Wu3†
Qiuping Wu3† Yuxi Xiao1,2
Yuxi Xiao1,2 Jinxiang Zheng4,5
Jinxiang Zheng4,5 Da Zheng1,2
Da Zheng1,2 Qiming Bi1,2
Qiming Bi1,2 Li Quan1,2
Li Quan1,2 Bingjie Hu3*
Bingjie Hu3* Jianding Cheng1,2*
Jianding Cheng1,2*Thoracic aortic dissection (TAD) is the most common cause of sudden cardiac death associated with aortic diseases. The age of TAD victims in forensic studies is significantly younger than hospitalized patients with TAD, while only a few studies have been conducted on autopsy-diagnosed TAD deceased. A retrospective study was conducted at the Medicolegal Center of Sun Yat-sen University from 1999 to 2019 to address the characteristics of TAD victims. A total of 200 deceased from spontaneous rupture of TAD were assessed, with 165 (82.5%) males and 175 (87.5%) Stanford type A deceased. Our main results showed that compared with patients with TAD diagnosed during their lifetime, individuals diagnosed with TAD until an autopsy showed an earlier onset (43.80 years old) and less accompanied hypertension (<50%). Sudden death was the initial symptom of 32 decedents. Instead of chest/back pain (40 decedents), abdominal pain (59 decedents) was the most common initial symptom, and 42 decedents presented with no accompanying pain. A higher proportion of abdominal pain and the painless symptom was associated with a higher risk of misdiagnosis. Women showed a more atypical clinical presentation and rapid progression than men. Younger decedents showed more pronounced left heart changes. The present study implicated the TAD individuals diagnosed until an autopsy as a particular entity, indicating the urgent need for further investigation on early diagnosis and pathogenesis of patients with TAD with atypical pain and painless or with younger age to reduce the burden of TAD-related sudden death.
Thoracic aortic dissection (TAD) is an emergent and life-threatening cardiovascular disease resulting in sudden cardiac death (SCD). Hospital studies have ascertained the annual incidence of acute aortic dissection (AAD) of about three cases per 100,000 (1), which may underestimate the incidence of aortic dissection as hospital-based reports do not account for preadmission deaths (2–5). Thus, these deaths are not accounted for unless an autopsy is performed. Systematic and standardized autopsy investigation is crucial for forensic pathologists to determine the cause of death of SCD victims (6). Our previous study reported that rupture of aortic dissection accounts for 5.2% of SCD victims (7). Prakash et al. (8) found that the age of TAD decedents was significantly younger than hospitalized patients with TAD, which indicated that autopsy-diagnosed TAD decedents might be a particular entity in TAD cases. However, only a few studies have been conducted on TAD deceased, and the sample size was too small to further investigate. Large sample size study of TAD deceased who were diagnosed until an autopsy could help us to uncover the nature of the particular TAD entity.
Our study recruiting 200 autopsy cases of TAD showed the characteristics of TAD deceased and identified that forensic autopsy is essential for determining the cause of death in sudden death cases and provides valuable additional information for physicians to further understand TAD. The prompt investigation of forensic autopsy data is indispensable to revealing pivotal information about TAD.
A retrospective study of forensic autopsy cases at the Medicolegal Center of Sun Yat-sen University was conducted. Autopsy reports that listed the primary cause of death as spontaneous rupture of TAD from 1999 to 2019 were reviewed. Decedents who died due to traumatic, iatrogenic TAD, or for who without a complete autopsy were excluded. Thus, 200 adult cases (≥18 years old) who met the study inclusion criteria formed the TAD group. As for control cases, each decedent from the TAD group was sex- and age-matched (same sex, with an age difference of no more than 3 years, with a death time difference of no more than 2 years) with three separate cases and decedents with aorta-related disease (intramural hematoma, penetrating aortic ulcer, aortic pseudoaneurysm, thoracic aortic aneurysms, abdominal aortic aneurysm/dissection, and aortic tumors) were excluded. All the control cases, aggregate up to 600, were classified into the control group. All the procedures followed were in accordance with the ethical standards of Sun Yat-sen University (approval no. 2019-004).
We retrospectively collected the index event's circumstances, including demographic data and medical history. Pathological data, including the location and extent of TAD, myocardial characteristics and dimensions, aortic and epicardial atherosclerotic diseases, and other congenital disabilities, was obtained from autopsy reports.
Continuous variables were presented as mean ± SEM or median (interquartile range) and analyzed using the unpaired Student's t-test or Mann–Whitney U-test. Categorical variables were expressed as the count (percent) and analyzed using the Pearson's chi-squared test and Fisher's exact test. A measure probability value of P <.05 was considered significant. Statistical evaluation was performed using SPSS Statistics version 22.0 (IBM Incorporation, Chicago, Illinois, USA).
Overall, 200 deaths from spontaneous rupture of TAD were identified in a population aged from 19 to 73 years old, and the average age was 43.80 ± 0.75 years old; a total of 165 cases (82.5%) were male (Table 1). The TAD decedents in this study spanned more than 20 years, with significantly more decedents in the latter decade (149 decedents, 2010–2009) than in the first decade (51 decedents, 1999–2009). Still, there were no significant differences in the mean age at death, age distribution, and sex distribution between the two decades.
The TAD decedent number during the warmer period (85 decedents, May to October) in Southern China was less than that during the colder period (115 decedents, November to April) in our study. However, 60% (21 decedents) of female TAD died during the warm period, compared with only 38.32% (64 decedents, P = 0.0211) of the total male TAD deaths during the same period.
Unfortunately, thirty-two victims (16%) have not been able to get to the hospital, and sudden death was their initial symptom (female: 8 in 35, 22.86%; male: 24 in 165, 14.55%). Meanwhile, the rest victims died very soon after admission to the emergency room. A total of 168 (84%) intervals from hospital admission to clinical death of TAD deaths were recorded. Seventy-one decedents (42.26%) died within 12 h, and 102 decedents (60.71%) died within 24 h. The interval from hospitalization to clinical death (IHD), with 17.5 (5.84, 41.21) h in men and 10.17 (3.33, 32) h in women, revealed a trend (P = 0.1966) in favor of men, and the median absolute difference of 7.33 h was likely to reveal the more urgent situation for women.
Excluding the TAD cases with sudden death as the initial symptom, abdominal pain was the most common symptom [59 decedents, 35.12% (Table 2)]. Rightfully, the most common misdiagnosis was acute abdomen. The acute onset of severe chest/back pain was the second most common initial complaint (40 decedents, 23.81%). In addition, the TAD deceased with headache or low back pain as their initial symptom showed a lower TAD suspected diagnosis ratio and a shorter IHD than those initially with chest/back pain or abdominal pain (Table 2). Meanwhile, 42 decedents (25%) presented with no accompanying pain in the present study. Syncope, chest distress, distention, and hemiplegia or paresis were the primary manifestations among these painless TAD deceased (Table 2). Painless TAD deceased showed a lower TAD suspected diagnosis ratio [4.76 vs. 12.70% (Table 2)] and a shorter IHD [10.98 (3.20, 30.00) vs. 18.67 (6, 42.09) (Table 2)] than the painful TAD deceased. Surprisingly, the proportion of painless victims was slightly higher among females than males (40.74 vs. 21.99%, P = 0.0519).
The clinical characteristics and outcomes in deceased with TAD vary with age. Compared with the older TAD deceased [>35 years old, 157 decedents, 47 (41, 52) years old], the incidence of sudden death as the initial symptom in youngers [≤35 years old, 43 decedents, 30 (26, 33) years old] was significantly higher (27.91 vs. 12.74%, P = 0.0319), while the incidence of painless TAD deceased was significantly lower among younger victims than older victims (6.45 vs. 29.20%, P = 0.0061).
Hypertension is an independent risk factor for TAD. In the present study, only 55.17% (32 in 58 available cases) of TAD deceased had a history of hypertension, and 48.74% (58 in 119 available cases) of TAD deceased with systolic blood pressure (SBP) ≥140 mm Hg.
Autopsy findings are shown in Table 3. According to Stanford classification, Stanford type A (175 cases, 87.5%) deceased was much more common than Stanford type B (25 cases, 12.5%). Dissection extended to the abdominal aorta in 41 victims (type A: 35). The intimal tear was most often single. Only in 8 cases, there were two tears, and in 1 case, there were three tears. The intimal tear was mainly found at ascending aorta in type A decedents, while at descending aorta in type B decedents, which was the same with the adventitial tear. Therefore, cardiac tamponade due to a rupture of the dissected channel into the pericardial sac was the most common cause of death for type A TAD decedents (167 of 175, 95.43%).
Pathological examination of the hearts from most TAD autopsy cases showed severe ventricular hypertrophy with an average cardiac mass of 450 (400, 500) g [control: 360 (300, 410) g, P < 0.0001 (Table 4)] and an average left ventricular-free wall thickness of 1.4 (1.2, 1.5) cm [control: 1.2 (1.1, 1.4) cm, P < 0.0001 (Table 4)]. As for the circumference of the cardiac valve annulus, except for the tricuspid annulus, the circumferences of the mitral/aortic/pulmonary annulus in the TAD group were significantly longer than those in the control group. Furthermore, we found that younger TAD decedents showed more pronounced changes in the left heart than their control counterparts. Compared with their control counterparts, younger TAD decedents not only had thicker left ventricular free wall [1.4 (1.2, 1.5) vs. 1.2 (1.0, 1.3) cm, P < 0.0001 (Table 5)] and longer circumference of the aortic annulus (CAA) [7.8 (7, 8.5) vs. 6.5 (6, 7) cm, P < 0.0001 (Table 5)], but also had a longer circumference of the mitral annulus (CMA) [9.7 (9, 10.5) vs. 9 (8.5, 9.5) cm, P = 0.0007 (Table 5)]. In addition, the differences in heart weight, CMA, and CAA between younger TAD and their control counterparts were more significant than those between older TAD and their control counterparts [heart weight: 90 vs. 70 g, CMA: 0.7 vs. 0 cm, and CAA: 1.3 vs. 0.5 cm (Table 5)].
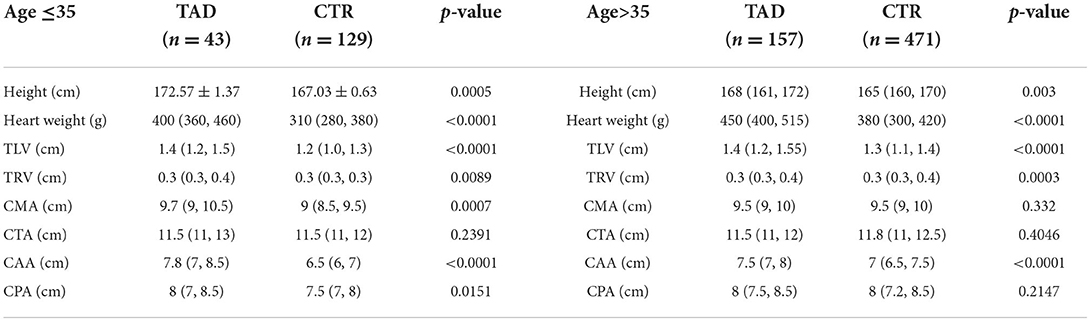
Table 5. Differences of postmortem findings between different age groups and their control counterparts.
The most common congenital disorder found in this study was bicuspid aortic valves (BAV) [eight cases, 4%, all Stanford A (Table 3, Figure 1)], classified by autopsy. Only one deceased was found with Marfan syndrome (MFS). The prevalence of coronary atherosclerosis in the TAD group was slightly higher than in controls (22.5 vs. 16.5%, P = 0.0703), but generally, there is no association of coronary atherosclerosis with TAD. Patients with TAD were reported to have a greater prevalence of renal cysts on CT than healthy controls. Our findings regarding the detection rate of renal cysts in TAD deceased were consistent with this [8 vs. 3.67%, P = 0.0197 (Table 3)]. As to microscopic examination of medial alteration, the mucoid extracellular matrix accumulation (MEMA) was confirmed in all the available cases to varying grades (Figure 2).
In addition to clinical data, a forensic pathological autopsy could also find some anatomical features that might be related to hypertension, such as the thickness of the compact myocardium of the left ventricular >1.5 cm, heart weight >500 g, hyalinosis of the central splenic artery, and renal arteriosclerosis. However, none of the above indicators had a positive rate of more than 50% alone (Table 6).
Thoracic aortic dissection still represented one of the most catastrophic cardiovascular diseases. Hitherto, many series of clinical studies have been conducted on hospitalized patients with TAD. Only reporting the incidence of hospitalized patients would introduce a serious underestimation of the incidence. A large number of patients with TAD remained undiagnosed until postmortem forensic autopsy and were not included in routine clinical studies of TAD (9–11). TAD decedents diagnosed until autopsy generally experienced fewer medical interventions and had a more natural course and a more severe outcome than hospitalized patients with TAD. However, studies on the deceased with TAD are limited. Our study recruited 200 autopsy-diagnosed TAD decedents and found that the characteristics of TAD among individuals diagnosed until autopsy were significantly different among hospitalized patients with TAD.
It has been shown in several studies that Chinese patients with AD are approximately 10 years younger than patients from western countries (12, 13). Similarly, compared to the TAD victims in the west, the age of TAD victims in our study was significantly younger (8, 14, 15), which may be related to the inadequate control of hypertension in China. Furthermore, compared with the age of onset of clinical patients with TAD, the age of TAD victims in forensic TAD studies was significantly younger (12, 13, 15, 16). Similar findings have been found in studies abroad between forensic and clinical TAD cases (8, 17). One possible reason was that the older patients were more likely to seek medical care after the onset of symptoms and be admitted with higher blood pressure. However, advanced age was associated with less administration of forensic autopsy. Earlier onset of TAD deceased in our study brings up a lower incidence of comorbid hypertension. In addition to those well-known possible causes such as incomplete clinical data, poor health awareness, and fewer routine physical examinations, the high proportion of Stanford type A cases may be another reason for the low prevalence of hypertension in our study, for the reason that hypertension was more prevalent in those with type B AD than in those with type A AD (13, 18, 19).
Aortic dissection has a myriad of clinical presentations and is for certain a diagnostic challenge. The symptoms of patients with TAD can vary and sometimes be very minimal. Symptoms of chest pain, abdominal pain, low back pain, limb ischemia, neurological dysfunction, and syncope have all been reported as potentially the sole presentation of TAD (20–23). In common sense, the most common symptom of TAD is chest pain, which is usually sharp and sometimes reported as tearing or ripping, while often radiating to the back or the abdomen (18, 24). Acute aortic chest pain can mimic pain from other more common acute conditions such as angina and acute coronary syndrome (ACS), which is more common than TAD and is, therefore, preferentially suspected by clinicians (20). The proportion of patients eventually diagnosed with TAD who receive a prior emergency diagnosis and management plan for ACS can be as high as 80% (25).
While the most common symptom in the present study was the sudden onset of abdominal pain rather than chest pain, regardless of Stanford type, which was different from that reported by the International Registry of Acute Aortic Dissection (IRAD) (chest pain) (24) and Sino-RAD (back pain) (13). Owe to lesion location, it is easy to understand that most Stanford type B patients with TAD presented with pain in the abdomen or low back. However, abdominal pain was also the initial symptom in Stanford type A deceased in the present study. Upchurch et al. found that patients who presented primarily with acute abdominal pain alone (4.6%) tended to have a delayed diagnosis and had higher mortality than those with more typical symptoms (26). In addition, our study found that TAD deceased present primarily with headache or low back pain showed a lower rate of suspected TAD diagnosis and a shorter IHD than those present with chest/back pain (Table 2). Atypical pain symptoms make correct diagnosis difficult.
Sudden onset of severe chest, back, or abdominal pain represents the most frequent symptom (13, 24). However, atypical presentation is seen in ~5% of AAD and is characterized by painless aortic dissection associated with higher mortality (27–29). In our study, the figure was 25%, far more than that in other studies. The trend of lower TAD suspected diagnosis ratio and shorter IHD in painless TAD decedents implicated that TAD decedents with painless symptoms propagated more rapidly and were more vitally. The higher risk of misdiagnosis secondary to atypical manifestations might be a crucial cause of the death of patients with TAD.
Women were reported to be about 5 years older than men at presentation in hospitalized patients with TAD (10, 30–32). In the present autopsy-based study, women were of comparable age to men and did not show longer event-free survival (Table 1). Interestingly, we found that women were more frequently affected during the warmer period, which was not the higher risk season for TAD (33, 34). Besides, women also showed a higher proportion of painless symptoms. These atypical features of TAD in women could mislead clinicians about the diagnosis. Further, our study found that women showed a higher proportion of sudden death as an initial symptom and shorter IHD. These results indicated that women die faster once the onset. Atypical clinical presentation and rapid progression made women with dissection die more often than men. Similar findings have been suggested in other hospitalized patient-based studies (10, 31) and speculated that sex differences in aortic morphology and hidden coronary heart disease (CHD) in women were possible reasons (35). In our study, female and male TAD decedents showed a comparable proportion of CHD. Compared to their control counterparts, women were more frequently affected by CHD (women, TAD vs. control: 22.86 vs. 5.71%; men, TAD vs. control: 22.42 vs. 18.79%), which may provide a clue for the early diagnosis of TAD in women.
Left ventricular hypertrophy (LVH) was previously identified in AAD using echocardiography (36–38), and LVH was also present in the youngest subjects with AAD and did not increase in relationship to age (8). Interestingly, in our study, younger TAD decedents with a higher prevalence of normotension showed more pronounced morphological changes in the left heart (Table 5). This result suggested that monitoring of cardiac volumes by echocardiography may be helpful in the early screening of TAD, especially in young patients. Further, familial TAD caused by several genetic mutations was also reported to be associated with disproportionate LVH in normotensive individuals (39), raising the possibility that some LVH (especially in youngers) may result from a genetic predisposition for both TAD and cardiac disease. In addition, our previous study found that the more genetic variants an individual carries, the earlier the onset of dissection (16). Genetic screening would help to anticipate prognosis and establish accurate risk stratification of any family member at risk of developing the same disease, especially for those of young TAD deceased.
Due to the retrospective nature of the present autopsy study, the body mass index (BMI) data in some autopsies was inadequate, which is associated with mortality in patients with cardiovascular diseases (CVDs) (40, 41) and is very important to evaluate the risks of CVD. Besides, as we do not routinely conduct toxicological analysis in decedents with a clear cause of death, cocaine use is not available in this study, which is associated with numerous CVDs and SCD (42, 43). Furthermore, there was no adequate correlation between postmortem values and values obtained from living patients by imaging techniques. Last, our results relied on data from a single center that may not reflect nationwide trends.
In summary, a significant number of patients remained undiagnosed until postmortem autopsy and were rarely reported compared to hospitalized patients. We conducted an autopsy-based study of TAD to detect the characteristics of the TAD deceased. Our results implicated the TAD individuals diagnosed until an autopsy was a particular entity. It showed an earlier onset and a low incidence of hypertension, a high incidence of painless and abdominal pain, more atypical and critical situation for women, and more pronounced left heart changes for young decedents. Our findings indicate the urgent need for studies on forensic TAD deaths to explore the early diagnosis of atypical TAD, as well as the pathogenesis and prevention of young patients with TAD to minimize the burden of TAD-related sudden death.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author/s.
This project was approved by the Ethics Committee of Sun Yat-sen University (Approval No. 2019-004), and it was carried out in strict accordance with the ethical research principle of Sun Yat-sen University.
JC, BH, and QZ designed the project. QZ, NZ, QW, YX, and JZ collected all the data. DZ and QB managed the documents and tissue slides. KY managed the histopathological data. QZ, NZ, and QW analyzed the data. QZ, LQ, BH, and JC discussed the data. QZ, BH, and JC wrote the manuscript. All the authors have approved the final version of the manuscript.
This study was supported by the National Natural Science Foundation of China (grant nos. 81920108021 and 81901919), the Guangzhou Municipal Science and Technology Project (grant no. 202102080092), and the Natural Science Foundation of Guangdong Province (grant no. 2020A1515010078).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Nienaber CA, Clough RE. Management of acute aortic dissection. Lancet. (2015) 385:800–11. doi: 10.1016/S0140-6736(14)61005-9
2. Nienaber CA, Clough RE, Sakalihasan N, Suzuki T, Gibbs R, Mussa F, et al. Aortic Dissection. Nature Reviews Disease Primers. (2016) 2:16053. doi: 10.1038/nrdp.2016.53
3. Mehta RH, Manfredini R, Hassan F, Sechtem U, Bossone E, Oh JK, et al. Chronobiological Patterns of Acute Aortic Dissection. Circulation. (2002) 106:1110–5. doi: 10.1161/01.cir.0000027568.39540.4b
4. Ramanath VS, Oh JK, Sundt TM. 3rd, Eagle KA. Acute Aortic Syndromes and Thoracic Aortic Aneurysm Mayo Clin Proc. (2009) 84:465–81. doi: 10.4065/84.5.465
5. Thrumurthy SG, Karthikesalingam A, Patterson BO, Holt PJ, Thompson MM. The diagnosis and management of aortic dissection. Bmj. (2011) 344:d8290. doi: 10.1136/bmj.d8290
6. Sessa F, Esposito M, Messina G, Di Mizio G, Di Nunno N, Salerno M. Sudden death in adults: a practical flow chart for pathologist guidance. Healthcare. (2021) 9(7). Epub 2021/08/07. doi: 10.3390/healthcare9070870
7. Wu Q, Zhang L, Zheng J, Zhao Q, Wu Y, Yin K, et al. Forensic pathological study of 1,656 cases of sudden cardiac death in Southern China. Medicine (Baltimore). (2016) 95:e2707. doi: 10.1097/MD.0000000000002707
8. Prakash SK, Haden-Pinneri K, Milewicz DM. Susceptibility to acute thoracic aortic dissections in patients dying outside the hospital: an autopsy study. Am Heart J. (2011) 162:474–9. doi: 10.1016/j.ahj.2011.06.020
9. Olsson C, Thelin S, Stahle E, Ekbom A, Granath F. Thoracic aortic aneurysm and dissection: increasing prevalence and improved outcomes reported in a nationwide population-based study of more than 14,000 cases from 1987 to 2002. Circulation. (2006) 114:2611–8. doi: 10.1161/CIRCULATIONAHA.106.630400
10. Smedberg C, Steuer J, Leander K, Hultgren R. Sex differences and temporal trends in aortic dissection: a population-based study of incidence, treatment strategies, and outcome in swedish patients during 15 years. Eur Heart J. (2020) 41:2430–8. doi: 10.1093/eurheartj/ehaa446
11. Mahase E. Half of patients with acute aortic dissection in england die before reaching a specialist centre. Bmj. (2020) 368:m304. doi: 10.1136/bmj.m304
12. Huang B, Chen Z, Lu H, Zhao Z, Hui R, Yang Y, et al. Influence of age on clinical presentation, therapeutic options, and outcome in chinese patients with acute aortic dissection. Int Heart J. (2019) 60:1373–80. doi: 10.1536/ihj.18-532
13. Wang W, Duan W, Xue Y, Wang L, Liu J, Yu S, et al. Clinical features of acute aortic dissection from the registry of aortic dissection in China. J Thorac Cardiovasc Surg. (2014) 148:2995–3000. doi: 10.1016/j.jtcvs.2014.07.068
14. Huynh N, Thordsen S, Thomas T, Mackey-Bojack SM, Duncanson ER, Nwuado D, et al. Clinical and pathologic findings of aortic dissection at autopsy: review of 336 cases over nearly 6 decades. Am Heart J. (2019) 209:108–15. doi: 10.1016/j.ahj.2018.11.006
15. Li Y, Li L, Mu HS, Fan SL, He FG, Wang ZY. Aortic dissection and sudden unexpected deaths: a retrospective study of 31 forensic autopsy cases. J Forensic Sci. (2015) 60:1206–11. doi: 10.1111/1556-4029.12768
16. Zheng J, Guo J, Huang L, Wu Q, Yin K, Wang L, et al. Genetic diagnosis of acute aortic dissection in south china han population using next-generation sequencing. Int J Legal Med. (2018) 132:1273–80. doi: 10.1007/s00414-018-1890-9
17. de Boer HH, Dedouit F, Chappex N, van der Wal AC, Michaud K. Sudden aortic death-proposal for a comprehensive diagnostic approach in forensic and in clinical pathology practice. Int J Legal Med. (2017) 131:1565–72. doi: 10.1007/s00414-017-1560-3
18. Evangelista A, Isselbacher EM, Bossone E, Gleason TG, Eusanio MD, Sechtem U, et al. Insights from the international registry of acute aortic dissection: a 20-year experience of collaborative clinical research. Circulation. (2018) 137:1846–60. doi: 10.1161/CIRCULATIONAHA.117.031264
19. Pape LA, Awais M, Woznicki EM, Suzuki T, Trimarchi S, Evangelista A, et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the international registry of acute aortic dissection. J Am Coll Cardiol. (2015) 66:350–8.
20. Salmasi MY, Al-Saadi N, Hartley P, Jarral OA, Raja S, Hussein M, et al. The risk of misdiagnosis in acute thoracic aortic dissection: a review of current guidelines. Heart. (2020) 106:885–91. doi: 10.1136/heartjnl-2019-316322
21. Manea MM, Dragos D, Antonescu F, Sirbu AG, Tiron AT, Dobri AM, et al. Aortic dissection: an easily missed diagnosis when pain doesn't hold the stage. Am J Case Rep. (2019) 20:1788–92. doi: 10.12659/AJCR.917179
22. Matsumoto H, Yoshida Y, Hirata Y. Usefulness of cervical magnetic resonance imaging for detecting type a acute aortic dissection with acute stroke symptoms. Magn Reson Imaging. (2016) 34:902–7. doi: 10.1016/j.mri.2016.04.021
23. Besli GE, Durakbasa CU, Yildirim S, Acar M, Cakir B. Acute aortic dissection mimicking acute abdomen in a 14-year-old boy. Pediat Int J Japan Pediatric Soc. (2015) 57:1169–71. doi: 10.1111/ped.12709
24. Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The international registry of acute aortic dissection (Irad): new insights into an old disease. JAMA. (2000) 283:897–903. doi: 10.1001/jama.283.7.897
25. Asouhidou I, Asteri T. Acute aortic dissection: be aware of misdiagnosis. BMC Res Notes. (2009) 2:25. doi: 10.1186/1756-0500-2-25
26. Upchurch GR. Jr., Nienaber C, Fattori R, Evangelista A, Oh J, Cooper JV, et al. Acute aortic dissection presenting with primarily abdominal pain: a rare manifestation of a deadly disease. Ann Vasc Surg. (2005) 19:367–73. doi: 10.1007/s10016-004-0171-x
27. Imamura H, Sekiguchi Y, Iwashita T, Dohgomori H, Mochizuki K, Aizawa K, et al. Painless acute aortic dissection. - diagnostic, prognostic and clinical implications. Circ J Jap Circ Soc. (2011) 75:59–66. doi: 10.1253/circj.CJ-10-0183
28. Ayrik C, Cece H, Aslan O, Karcioglu O, Yilmaz E. Seeing the invisible: painless aortic dissection in the emergency setting. Emerg Med J. (2006) 23:e24. doi: 10.1136/emj.2004.021790
29. Park SW, Hutchison S, Mehta RH, Isselbacher EM, Cooper JV, Fang J, et al. Association of painless acute aortic dissection with increased mortality. Mayo Clin Proc. (2004) 79:1252–7. doi: 10.4065/79.10.1252
30. Howard DP, Banerjee A, Fairhead JF, Perkins J, Silver LE, Rothwell PM. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the oxford vascular study. Circulation. (2013) 127:2031–7. doi: 10.1161/CIRCULATIONAHA.112.000483
31. Nienaber CA, Fattori R, Mehta RH, Richartz BM, Evangelista A, Petzsch M, et al. Gender-related differences in acute aortic dissection. Circulation. (2004) 109:3014–21. doi: 10.1161/01.CIR.0000130644.78677.2C
32. Maitusong B, Sun HP, Xielifu D, Mahemuti M, Ma X, Liu F, et al. Sex-related differences between patients with symptomatic acute aortic dissection. Medicine. (2016) 95:e3100. doi: 10.1097/MD.0000000000003100
33. Ballaro A, Cortina-Borja M, Collin J. A seasonal variation in the incidence of ruptured abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. (1998) 15:429–31. doi: 10.1016/S1078-5884(98)80205-0
34. Vitale J, Manfredini R, Gallerani M, Mumoli N, Eagle KA, Ageno W, et al. Chronobiology of acute aortic rupture or dissection: a systematic review and a meta-analysis of the literature. Chronobiol Int. (2015) 32:385–94. doi: 10.3109/07420528.2014.983604
35. Ulug P, Powell JT, Warschkow R, von Allmen RS. Editor's choice - sex specific differences in the management of descending thoracic aortic aneurysms: systematic review with meta-analysis. Eur J Vasc Endovasc Surg. (2019) 58:503–11. doi: 10.1016/j.ejvs.2019.04.022
36. Iarussi D, Caruso A, Galderisi M, Covino FE, Dialetto G, Bossone E, et al. Association of left ventricular hypertrophy and aortic dilation in patients with acute thoracic aortic dissection. Angiology. (2001) 52:447–55. doi: 10.1177/000331970105200702
37. Kim SJ, Park TH, Cho YR, Park K, Park JS, Kim MH, et al. Left Ventricular geometric patterns in patients with type a aortic dissection. Cardiovasc Ultrasound. (2019) 17:2. doi: 10.1186/s12947-019-0152-4
38. Taylor AP, Freeman RV, Bartek MA, Shalhub S. Left Ventricular hypertrophy is a possible biomarker for early mortality after type B aortic dissection. J Vasc Surg. (2019) 69:1710–8. doi: 10.1016/j.jvs.2018.09.050
39. van de Laar IM, Oldenburg RA, Pals G, Roos-Hesselink JW, de Graaf BM, Verhagen JM, et al. Mutations in Smad3 cause a syndromic form of aortic aneurysms and dissections with early-onset osteoarthritis. Nat Genet. (2011) 43:121–6. doi: 10.1038/ng.744
40. Xia JY, Lloyd-Jones DM, Khan SS. Association of body mass index with mortality in cardiovascular disease: new insights into the obesity paradox from multiple perspectives. Trends Cardiovasc Med. (2019) 29:220–5. doi: 10.1016/j.tcm.2018.08.006
41. Abou Ghayda R, Duck-Young Park D, Lee JY, Kim JY, Lee KH, Hong SH, et al. Body mass index and mortality in patients with cardiovascular disease: an umbrella review of meta-analyses. Eur Rev Med Pharmacol Sci. (2021) 25:273–86.
42. Turillazzi E, Bello S, Neri M, Pomara C, Riezzo I, Fineschi V. Cardiovascular effects of cocaine: cellular, ionic, and molecular mechanisms. Curr Med Chem. (2012) 19:5664–76. doi: 10.2174/092986712803988848
Keywords: thoracic aortic dissection, sudden death, forensic autopsy, epidemiology, retrospective study
Citation: Zhao Q, Yin K, Zhou N, Wu Q, Xiao Y, Zheng J, Zheng D, Bi Q, Quan L, Hu B and Cheng J (2022) The characteristics of thoracic aortic dissection in autopsy-diagnosed individuals: An autopsy study. Front. Cardiovasc. Med. 9:973530. doi: 10.3389/fcvm.2022.973530
Received: 20 June 2022; Accepted: 20 September 2022;
Published: 11 October 2022.
Edited by:
Pasqualino Sirignano, Sapienza University of Rome, ItalyCopyright © 2022 Zhao, Yin, Zhou, Wu, Xiao, Zheng, Zheng, Bi, Quan, Hu and Cheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bingjie Hu, aHViaW5namllQDEyNi5jb20=; Jianding Cheng, Y2hlbmdqZEBtYWlsLnN5c3UuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.