
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 24 August 2022
Sec. Cardiovascular Therapeutics
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.958895
This article is part of the Research Topic Novel and Emerging Therapies in Acute and Chronic Heart Failure View all 12 articles
Purpose: The purpose of the study was to access the impact of phase 1 cardiac rehabilitation (CR) on cardiac function and hemodynamic changes in patients with coronary heart disease (CHD) and acute heart failure (AHF).
Materials and methods: A total of 98 patients with CHD and AHF were recruited and randomized into two groups. Control group received standard pharmacotherapy and CR group received standard pharmacotherapy combined phase 1 CR. NT-proBNP and hemodynamic parameters measured by impedance cardiography (ICG) were estimated at baseline and at the end of treatment period.
Results: Phase 1 CR combined routine medical treatment could lower NT-proBNP levels. The percentage of high-risk patients was significantly decreased in CR group, although the post-treatment NT-proBNP level between control group and CR group showed no significant differences. Similarly, most hemodynamic parameters improved in the CR group, but not in the control group, suggesting that phase 1 CR in combination with the standard pharmacotherapy improved hemodynamic characteristics by elevating cardiac output, ameliorating preload, improving systolic and diastolic function, and relieving afterload, although the post-treatment hemodynamic parameters showed no statistically significant differences between the control group and the CR group.
Conclusion: Phase 1 CR combined routine medication can improve cardiac function and hemodynamic characteristics in patients with CHD and AHF. Thus, recommendation of phase 1 CR to stable patients is necessary.
Coronary heart disease (CHD) is one of the most common causes of heart failure (HF). Despite the improvement in long-term prognosis of patients with HF due to the development of pharmacotherapy, intervention, implantable cardioverter defibrillator, and cardiac resynchronization therapy, the mortality and re-admission rate of patients with HF, however, remain high. Thus, improving prognosis and outcomes of patients with HF is of high priority.
Cardiac rehabilitation (CR), an accessible and economical therapy, has attracted progressive attention in the recent years. European Society Of Cardiology (ESC) and American Heart Association/American College of Cardiology (AHA/ACC) have recognized CR as a class I recommendation for patients with HF (1). CR includes three phases: inpatient CR (phase 1 CR), early stage of outpatient CR (phase 2 CR), and long-term community-based CR (phase 3 CR). Phase 1 CR (or inpatient CR) provides hospitalized patients with cardiac rehabilitation and preventive measures including exercise training, patient education, and behavior interventions. Several guidelines and expert consensus recommend phase 1 CR to hemodynamical stable patients with acute heart failure (AHF) and patients with HF recurrence (2–5).
It has been demonstrated that phase 1 CR contributed to alleviate symptoms (6), improve functional capacity and activity of daily living (7–9), shorten hospital stay length (10, 11), and reduce re-admission rate (11, 12) and all-cause mortality (11, 13). Specifically, patients receiving phase 1 CR had a 26% increase in 6-min walk test (6MWT) compared with controls (14), suggesting an enhancement in cardiopulmonary function and exercise capacity. Consistently, early movement within 48 h improved oxygen uptake efficiency slope in patients with acute myocardial infarction (AMI) (15). Besides, early movement training also ameliorated the inflammatory level in patients with AMI (16).
However, the prevalence of phase 1 CR remains low. A cross-sectional investigation including 454 hospitals revealed that only 24% hospitals provide phase 1 CR program (17). Meanwhile, the awareness of phase 1 CR in patients remains relatively insufficient (18). Therefore, there is a need to promote phase 1 CR.
The continuous monitoring and evaluation of patients with HF in phase 1 CR is critical, but an accurate and efficient method lacks. Impedance cardiography (ICG), a non-invasive approach of constant monitoring instantaneous changes in thoracic electrical impedance based on the Ohm’s law, can provide reliable hemodynamic values and has been used to estimate cardiac function in patients with HF (19). Previous studies have confirmed the accuracy of ICG by comparing it to echocardiography (20). Meanwhile, as the change of hemodynamics status happens prior to occurrence of symptoms, the feature that ICG can capture small hemodynamic changes and thus can identify asymptomatic abnormalities makes ICG a more sensitive method than echocardiography. Most importantly, the intensity and duration of phase 1 CR can be adjusted promptly based on patients’ condition reflected by ICG-measured hemodynamic changes. Furthermore, the prospective evaluation and identification of cardiac decompensation by ICG test (PREDICT) study finds that the combination of parameters measured by ICG can predict the short-term mortality and re-admission rate of patients with HF (21). Thus, ICG can be applicated as a useful approach in evaluating the effectiveness of phase 1 CR.
However, the effects of phase 1 CR on hemodynamic changes in patients with AHF remain unknown. In this study, we attempt to explore the impact of phase 1 CR on cardiac function and hemodynamics in patients with CHD and AHF through the pre- and post-treatment hemodynamic changes detected by ICG.
This study was approved by the Clinical Research Ethics Committee, the Second Xiangya Hospital of Central South University, China. All participants provided informed consent.
This study was a randomized controlled trial. A total of 106 patients with CHD and AHF who were admitted for treatment in cardiac care units from 2019 to 2020 were recruited and randomly assigned to one of two treatment groups, the control group or the CR group.
Randomization and allocation sequence was based on a block size fixed to 2 and generated through a computerized random number generator by a staff not involved in the trial. The patients in control group were treated with ordinary standard medical treatment. The patients in CR group received medical treatment plus 1-week phase 1 CR program during hospitalization.
The inclusion criteria were as follows: (1) age > 18 years; (2) the percutaneous transluminal coronary intervention revealed > 75% narrowing of the proximal anterior descending artery or three main coronary arteries; (3) the echocardiography showed enlarged heart with the diagnosis meets the criteria of left ventricular end diastolic diameter (LVEDd) > 5 cm; (4) the left ventricular ejection faction (LVEF) between 30 and 50%; (5) apparent clinical signs and symptoms of AHF appeared; and (6) laboratory test showed elevated NT-proBNP level.
The exclusion criteria were as follows: (1) any life-threatening comorbidities, (2) patients with unstable hemodynamics; (3) acute phase of pulmonary diseases, including asthma attacks, pulmonary embolism, pneumothorax, and impaired cognition, (4) severe infections, such as infectious endocarditis and septicemia; (5) uncontrolled arrhythmia; (6) severe valvular disease; (7) trauma or surgical history in the past 6 months; (8) aortic dissection; (9) cancer; (10) cognitive limitation; and (11) refuse to provide consent. Patients with the main diagnosis other than CHD and AHF were also excluded.
Phase 1 CR was performed under the instruction and observation of experienced physicians and adjusted according to the patients’ conditions. The specific procedure was followed by the fourth edition of guidelines for CR and secondary prevention program (22).
Phase 1 CR began when patients fitted those following conditions: (1) no chest pain in the past 8 h; (2) no evident symptoms or signs of decompensated heart failures; (3) no new onset arrhythmia nor changes on electrocardiograph (ECG); and (4) no elevation of NT-proBNP.
The phase 1 CR program lasted for 7 days. On each day, the duration is 30 min, including 10-min warm-up activity, 10-min aerobic exercise, and 10-min Meridians patting or flexibility training according to the patients’ conditions.
The evaluation of the phase 1 CR program is the combination of targeted heart rate, which is to raise heart rate to 20 ± 5 beat per minute above the rest heart rate, and Borg scale, a rating of perceived exertion scale.
The criteria of termination of phase 1 CR were as follows: (1) chest pain, palpitations, dyspnea, sweating, and other obvious discomfort symptoms; (2) ECG showed frequent ventricular tachycardia, atrial tachycardia, atrial fibrillation, and other malignant arrhythmias; (3) systolic blood pressure did not increase but decreased by 10 mmHg or more, or systolic blood pressure elevated by 180 mmHg; and (4) the patient requested to stop.
The echocardiography was performed by experienced physician within 24 h of admission.
The hemodynamic parameters were detected by experienced staff using ICG (CSM3000, the Cheer Sails Medical). ICG was performed after 5 min of rest in the supine position. The electrodes were placed following the instructions. The hemodynamic variables included cardiac output (CO), cardiac index (CI), stroke volume (SV), stroke index (SI), thoracic fluid content (TFC), pre-ejection period (PEP), left ventricular ejection time (LVET), systolic time ratio (STR), systemic vascular resistance (SVR), stroke systemic vascular resistance (SSVR), and stroke systemic vascular resistance index (SSVRI). The venous blood was obtained for detection of NT-proBNP followed by ICG measurements.
The data were analyzed by SPSS version 20.0. Measurement data followed normal distribution were expressed as mean ± standard deviation, whereas non-normal distributional data were expressed as median (interquartile range). Enumeration data were expressed as proportion and evaluated by Chi-square test. Paired t-test was used to compare the changes in normal distributional parameters, and Kruskal–Wallis test was used to compare the changes in non-normal distributional parameters. A repeated measures ANOVA was used to compare the pre- and post-treatment changes in control and CR group. Spearman’s correlation analysis was used to evaluate the correlation between the parameters determined by ICG and blood NT-proBNP. A value of p < 0.05 was considered statistically significant.
The study included 106 patients (average age 66.96 ± 2.76 years old, 72.4% male). The control group contained 53 patients, 52 of whom finished the treatment. The CR group contained 53 patients, 46 of whom were analyzed (Figure 1). The fundamental data are shown in Table 1. There were no differences in height, weight, body mass index (BMI), blood pressure and rest heart rate, companion diseases, and medical history between control and CR group before treatment. The echocardiography showed comparable in cardiac structure and cardiac function between two groups (Table 2).
As shown in Table 3, there were no differences in NT-proBNP level between control and CR group before treatment.
In control group, the NT-proBNP level decreased from 1913.62 (926.33; 4,378.22) pg/ml to 1,439.61 (283.7275; 2,594.87) pg/ml after the treatment (p < 0.05). In CR group, the NT-proBNP level decreased from 2,643.00 (1,527.59; 4,360.00) pg/ml to 1,889.00 (704.85; 3,315.00) pg/ml after the treatment (p < 0.05).
After treatment, the NT-proBNP level in CR group was non-significantly lower than that of control group.
The level of NT-proBNP was found to correlated with the short-term prognosis of patients with AHF and that patients with NT-proBNP higher than 5,180 pg/ml had higher risk of sudden death (23). Thus, the subgroup analyses defined patients with NT-proBNP > 5,180 pg/ml as high NT-proBNP group, whereas NT-proBNP ≤ 5,180 pg/ml as low NT-proBNP group. Before the treatment, 22.4% of patients (control group 19.2%, CR group 26.1%) were divided into high NT-proBNP group, while after the treatment, 8.2% of patients (control group 13.5%, CR group 2.2%) have NT-proBNP higher than 5,180 pg/ml. In control group, the patients with high NT-proBNP group decreased by 5.7%, whereas in CR group, that percentage decreased by 23.4%. In addition, the number and the percentages of patients with NT-proBNP higher than 5,180 pg/ml in the CR group significantly decreased (p < 0.05), which suggested that phase 1 CR could further lower plasma NT-proBNP level and improve short-term prognosis of patients with CHD and AHF based on the routine medicine.
Table 4 showed the following cardiac output parameters: cardiac output (CO), cardiac output index (CI), stroke volume (SV), and stroke volume index (SI) of control group and CR group. As it showed, there were no differences between two groups before treatment. After the treatment, no significant changes were found between two groups.
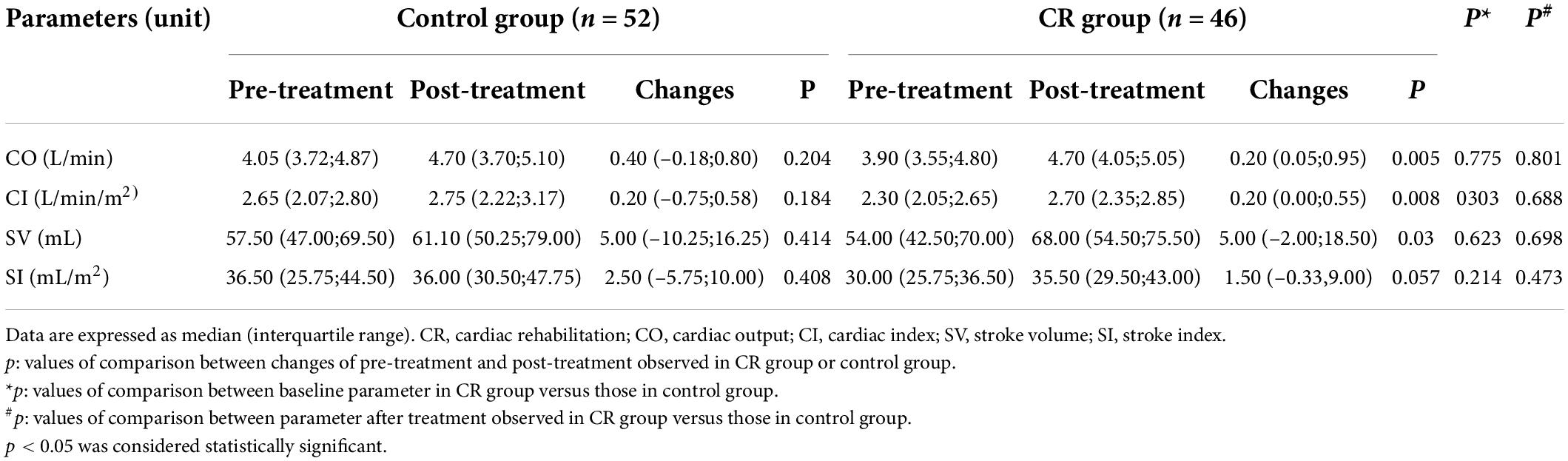
Table 4. Comparisons of parameters of cardiac output measured by impedance cardiography of patients with CHD and AHF before and after the treatment.
In control group, the cardiac output parameters showed no changes before and after the treatment, whereas in CR group, CO, CI, and SV increased after the treatment (p < 0.05). It indicated that routine treatment had limitations in improving cardiac output in short term, while medical treatment combined phase 1 CR could improve cardiac output in patients with CHD and AHF.
As Table 5 showed, there were no differences in TFC between two groups before and after the treatment. After the treatment, the TFC of control group decreased from 0.034 (0.029; 0.036)/Ω to 0.030 (0.025; 0.035)/Ω (p > 0.05), at the same time, the TFC of CR group decreased from 0.035 (0.029;0.041)/Ω to 0.031 (0.029;0.035)/Ω (p > 0.05). However, the statistics showed no significant changes in TFC before and after treatment in both groups.
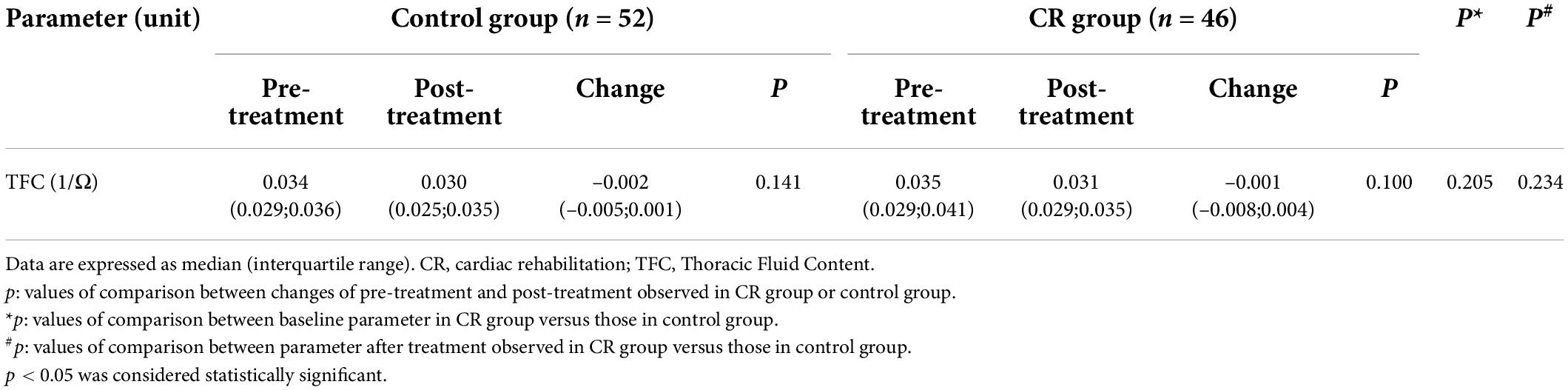
Table 5. Comparison of preload parameter measured by impedance cardiography of patients with CHD and AHF before and after the treatment.
To further determine whether phase 1 CR has influence on TFC level, we divided patients into two subgroups: patients with TFC ≥ 0.035/Ω were defined as high-preload group, whereas patients with TFC < 0.035/Ω were defined as low-preload group. Before the treatment, 50.0% of patients (50.0% in control group, 50.0% in CR group) were in high-preload subgroup. After the treatment, 29.6% of patients (30.8% in control group, 28.3% in CR group) had TFC higher than 0.035/Ω. The percentage of patients with high preload was decreased in both control group and CR group.
To further identify the effects of phase 1 CR under same preload situation, we compared TFC changes of high- or low-preload settings in control group and CR group. The results are shown in Table 6. In control group, TFC changes were not statistically significant in either high- or low-preload settings. In CR group, though no significant change was found in low-preload subgroup, the TFC level decreased from 0.0395 (0.0365; 0.0427)/Ω to 0.0315 (0.0290; 0.0350)/Ω (p < 0.05) in high-preload setting. Taken together, these findings indicated that phase 1 CR plus routine treatment decrease TFC in high-preload patients.
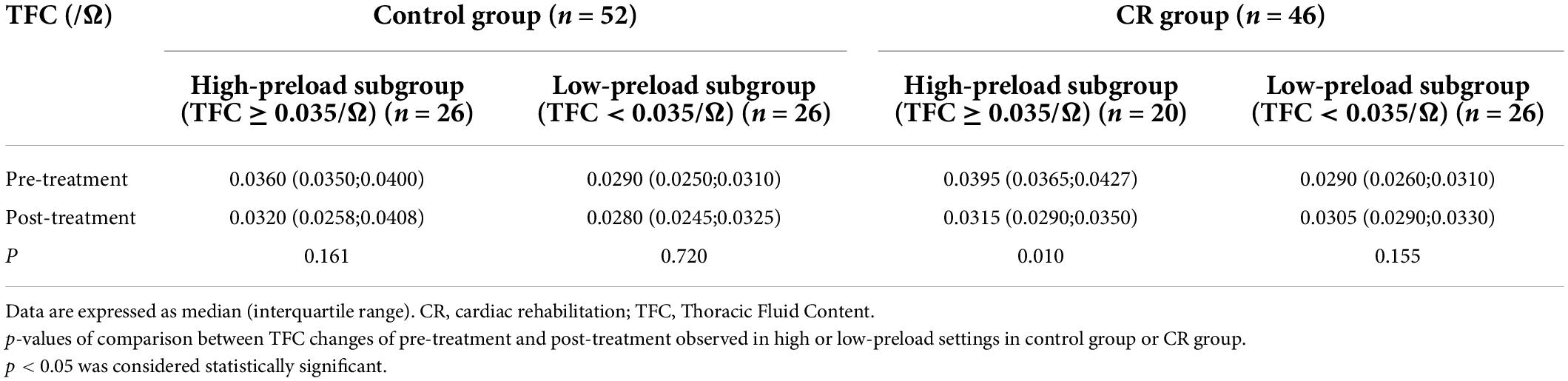
Table 6. Comparison of preload of patients with CHD and AHF before and after the treatment under same preload setting.
As Table 7 showed, there were no differences in PEP, LVET, and STR between two groups before and after the treatment.
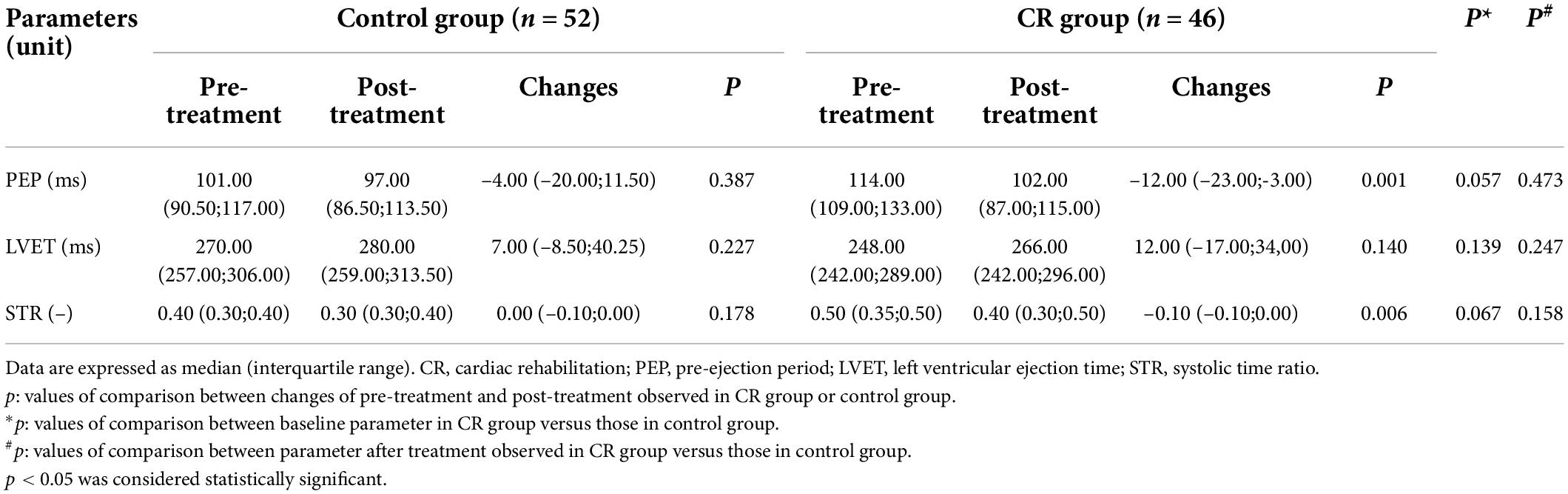
Table 7. Comparisons of cardiac function of contraction measured by impedance cardiography of patients with CHD and AHF before and after the treatment.
Medical treatment decreased the PEP in control group from 101.00 (90.50; 117.00) to 97.00 (86.50; 113.50) ms (p > 0.05), whereas phase 1 CR plus medication shorter PEP from 114.00 (109.00; 133.00) to 102.00 (87.00;115.00) ms (p < 0.05).
Pre- and post-treatment LVET showed no differences in both control and CR groups.
The STR in control group was shorter from 0.40 (0.30; 0.40) to 0.30 (0.30; 0.40) (p > 0.05), whereas in CR group, the STR was changed from 0.50 (0.35; 0.50) to 0.40 (0.30; 0.50) (p < 0.05). The results suggested that routine treatment plus phase 1 CR shorter PEP and STR, thus improving constriction function of left ventricular.
Moreover, to identify the effects of phase 1 CR in improving left ventricular constriction, subgroup analysis was made. STR > 0.4 was defined as dysfunctional constriction. Before the treatment, 39.8% of patients (control group 21.2%, CR group 60.8%) were defined as dysfunctional constriction, while after the treatment, 16.3% of patients (control group 5.8%, CR group 28.3%) had dysfunctional constriction. The standardized percentage of patients with constriction problem decreased 15.1 and 32.0%, respectively, in control group and CR group, which implied that phase 1 CR can improve constriction function of left ventricular.
As Table 8 showed, there were no differences in SVR, SSVR, and SSVRI between two groups before and after the treatment.
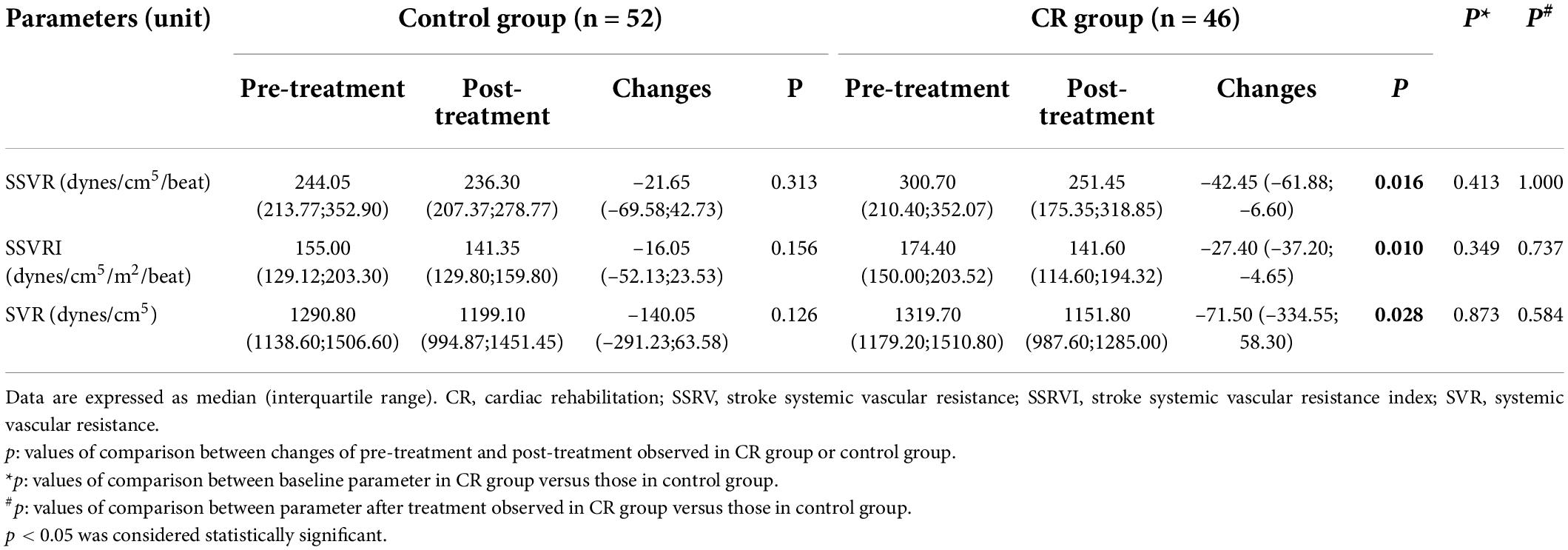
Table 8. Comparison of afterload parameters measured by impedance cardiography of patients with CHD and AHF before and after the treatment.
In control group, the SVR, SSVR, and SSVRI showed no differences before and after the treatment. In CR group, the SSVR decreased from 300.70 (210.40; 352.07) dynes/cm5/beat to 251.45 (175.35; 318.85) dynes/cm5/beat (p < 0.05), SSVRI decreased from 174.40 (150.00;203.52) dynes/cm5/m2/beat to 141.60 (114.60;194.32) dynes/cm5/m2/beat (p < 0.05), and SVR decreased from 1,319.70 (1,179.20; 1,510.80) dynes/cm5 to 1,151.80 (987.60; 1,285.00) dynes/cm5 (p < 0.05). The results above suggested that phase 1 CR plus routine treatment could decrease system resistance to lower pressure load.
Spearman’s correlation analysis was used to identify the correlation between the changes in ICG parameters and NT-proBNP (Table 9); however, no correlation was observed between these two items.
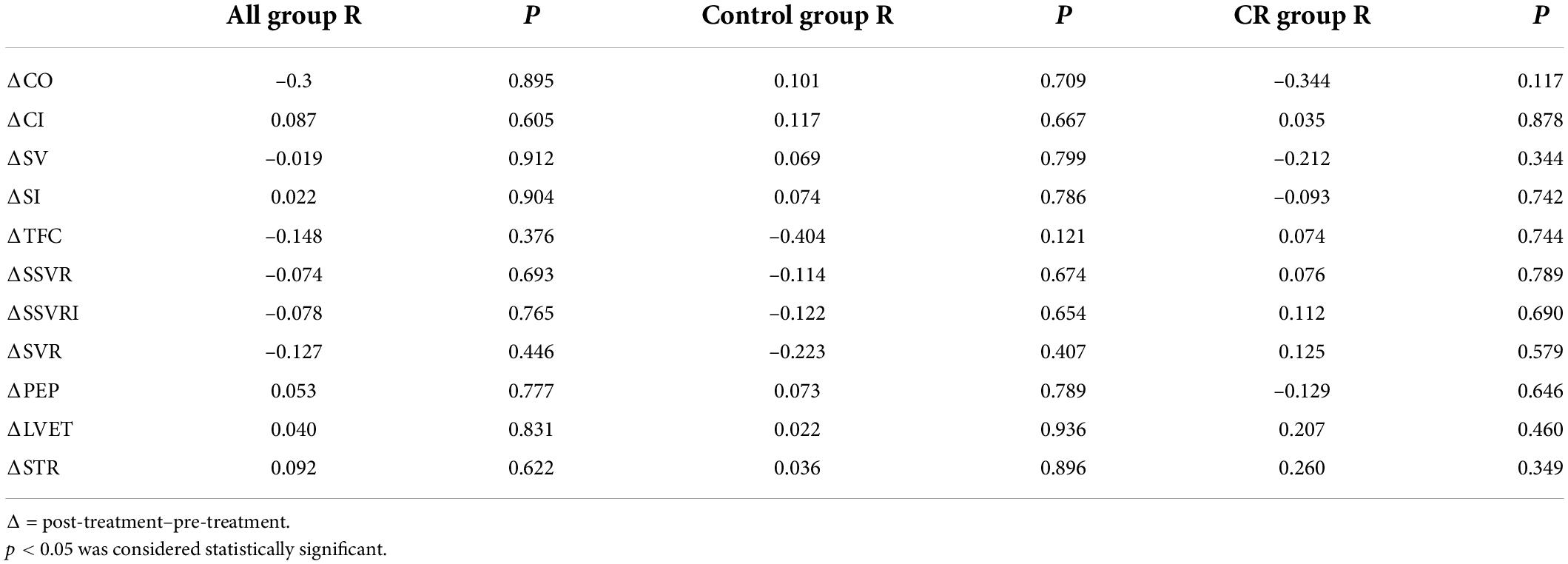
Table 9. Correlation between change of hemodynamic parameters measured by impedance cardiology and change of NT-proBNP in patients with CHD and AHF.
Previous studies have demonstrated that hemodynamic parameters measured by ICG can reflect the hemodynamic characteristics of patients with HF. In this study, we found that both standard pharmacotherapy and phase 1 CR combined routine medical treatment could lower NT-proBNP levels in patients with CHD and AHF. However, the number and the percentages of high-risk patients in CR group significantly decreased after the treatment. Meanwhile, most hemodynamic parameters improved after the treatment in CR group, but not in control group, suggesting that phase 1 CR plus standard pharmacotherapy improved hemodynamic characteristics by elevating SV, CO, and CI, decreasing TFC in high-preload patients, shortening PEP and STR, and lowering SVR, SSVR, and SSVRI, although the post-treatment hemodynamic parameters showed no statistically significant differences between control group and CR group. Most importantly, the decrease of standardized percentage of patients with dysfunctional problem in CR group was higher than that in control group, indicating an improvement in systolic and diastolic function of left ventricular.
Large amounts of studies have demonstrated that the level of NT-proBNP is a predictor of outcome of patients with HF (24, 25). Normally, the higher level of NT-proBNP, the higher of New York Heart Association (NYHA) functional classes, the worse of prognosis of patients with HF (26). Meanwhile, in this study, both routine treatment and routine treatment combined phase 1 CR could decrease the level of NT-proBNP effectively in patients with CDH and AHF. Subgroup analysis demonstrated that the number and the percentages of patients with higher level of NT-proBNP in the CR group significantly decreased (p < 0.05), suggesting that phase 1 CR plus medication can further lower the levels of NT-proBNP in patients with CHD and AHF, which implies that phase 1 CR may improve the outcome in patients with HF. Previous studies have found that phase 1 CR could improve the symptoms of patients with HF. A perspective study showed that phase 1 CR improved the percentage of patients in NYHA class I and class II from 19.6 and 35.2% in the admission to 24.8 and 54.1% in the dismission, respectively, and the percentage of patients with NYHA class III decreased from 44.2 to 19.6% (6). Similarly, Taya et al. found that the high-intense intermittent training decreased the serum level of BNP in patients with HF from 432 (812) pg/ml to 254 (400) pg/ml (p < 0.001) (27). Those results imply that early movement can improve the symptoms of patients with HF. Moreover, Motoki et al. demonstrated that phase 1 CR improved the daily activity function in patients with acute decompensated HF (7).
Several reports have demonstrated the accuracy of SV and CO detected by ICG (28, 29). We found that patients in CR group had a significant improvement in SV, CO, and CI and a non-significant improvement in SI. However, no significant differences were observed after the treatment in all parameters above mentioned between control group and CR group. The improvement of post- and pre- treatment SV in the CR group, not in control group, implied that early movement may improve pump function of heart. Consistent with our finding, Chursina et al. reported that free-load bicycle exercise improved LVEF in patients with ischemic cardiomyopathy (30, 31).
Thoracic fluid content is used to reflect the preload or volume load in ICG. Previous studies have found that TFC is negatively correlated with pulmonary capillary wedge pressure (32). The patients with severer symptoms and higher NYHA levels had higher TFC level in AHF (33). Moreover, TFC in patients with HF had a significant positive correlation with re-admission rate and risk of death in 2 months (34). However, there is no research deciphering the effect of phase 1 CR on TFC. In this study, phase 1 CR plus routine medical treatment only showed a decrease tendency in TFC. Interestingly, in patients with TFC ≥ 0.035/Ω, phase 1 CR plus medical treatment significantly decreased TFC. However, such improvement was not discovered in patients with TFC < 0.035/Ω. Taken together, our findings suggested that phase 1 CR decreased preload of heart in patients with high preload. Consistently, Gielerak et al. found that 8-week CR could decrease TFC, elevate the maximum oxygen uptake, and improve exercise tolerance in patients with HF (35). Moreover, the decrease in TFC had positive correlation with the improvement in 6-min walk test (36). All the results above suggest that CR can improve cardiac function by decreasing TFC level.
Pre-ejection period refers to the time period of isovolumic contraction and LVET refers to time period of left ventricular isometric contraction. The decreased contraction would result in prolonging PEP and shortening LVET. STR is the ratio of PEP and LVET. Thus, STR can reflect the efficiency of ventricular contraction and left ventricular function.
In this study, the significant decrease of PEP and STR in CR group, not in control group, implied that phase 1 CR combined medical treatment improved left ventricular contraction in patients with CHD and AHF, although no significant differences have been found between control group and CR group. Emerging studies have demonstrated the correlation of STR and risk of death in patients with HF. Sadauskas et al. reported that STR ≥ 0.55 is an indicator of higher risk to death in 6 months in patients with recurrent HF (OR = 0.29) (37). Moreover, in PREDICT trial, a multicenter trial including 2,316 patients, the hemodynamic parameters including STR were identified as a predictor of short-term clinical events, such as HF recurrent decompensation (21). The findings above suggest that STR could be used to warn the risk of adverse cardiovascular events.
Furthermore, STR is related to short-term outcome of patients with HF (21). Thompson reported the negative correlation between STR and LVEF (r = –0.54; p < 0.001) (38). Vijayaraghavan et al. analyzed ICG parameters and quality of life in 64 patients with chronic HF and pointed out that shorter PEP was associated with the improvement in NYHA level (39), suggesting that PEP could be a reflection of symptoms in patients with HF.
In addition, STR can imply diastole function. In IMPEDDANS study, ICG was used to evaluate diastolic dysfunction in patients with arterial hypertension. Nazario Leao et al. found that PEP, LVET, and STR had good discriminative ability in discovering left ventricular diastole dysfunction. Amid them, the sensibility of STR was 99% and the specificity was 90%. The threshold of diastole dysfunction is PEP ≤ 104 ms, LVET ≥ 320 ms, and STR ≤ 0.31 (40). Although we did not focus on diastolic improvement, the results of our study implicated that phase 1 CR combined medical treatment could shorten PEP and STR, which suggests the improvement of phase 1 CR on diastole function in patients with CHD and AHF worthy further investigation.
Systemic vascular resistance, SSVR, and SSVRI are the parameters that reflect pressure load in ICG. Cotter et al. found an elevation in SVRI in patients with AHF (41), which was due to the activation of neuroendocrine. The elevation of SVRI contributed to the persistence of blood pressure and perfusion of important organs under the circumstance of decreased contractility. Overload SVRI may cause elevated afterload, decreased CI, increased left ventricular end-diastolic pressure and pulmonary capillary wedge pressure, and eventually leading to pulmonary edema. While decreasing SVR properly can increase SV, which could improve pulmonary congestion, however, there is no research indicating the effects of phase 1 CR on cardiac afterload. In this research, the significant decrease of SVR, SSVR, and SSVRI in CR group, but not in control group, suggested that phase 1 CR combined medical treatment could reduce afterload, at least to some extent, in patients with CHD and AHF, although no significant differences of post-treatment SVR, SSVR, and SSVRI have been found between control group and CR group.
Previous studies identified some correlations between BNP and ICG parameters. As Pomenta et al. reported, the TFC measured by ICG is an independent predictor of BNP in patients with AHF, despite the severe contraction dysfunction and NYHA levels (34). However, in this study, we did not determine the correlation between NT-proBNP and ICG parameters.
Despite that 1-week period of phase 1 CR improved cardiac function and hemodynamic characteristics in patients with CHD and AHF, whether the short-term benefits remain in the long run still needs to be further studied. Of note, though emerging studies have suggested that long-term exercise can improve the outcomes in patients with HF, the participation of long-term exercise is relatively low. Whether patients completed phase 1 CR would choose to continue phase 2 and phase 3 CR depends on the willing of patients, the recommendation of physicians, and the convenience, that is, whether there are facilities near the their communities (5). Thus, facilities need to be built and physicians should take the responsibility to recommend patients to further exercise movements.
This study has several limitations. Frist, the sample amount was relatively small due to the limitation of collection time and one-center study. Second, this study did not compare the effects of phase 1 CR in population with HF with preserved EF, HF with might reversed EF, and HF with reserved EF. Therefore, more studies with larger population and multicenters were needed to confirm the effects of phase 1 CR on cardiac function and hemodynamics in patients with CHD and AHF.
In this study, we find that phase 1 CR plus routine medication can improve cardiac function and hemodynamic parameters in patients with CHD and AHF in short term. Thus, it is important to recommend phase 1 CR to patients once they are stable.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Clinical Research Ethics Committee, the Second Xiangya Hospital of Central South University. The patients/participants provided their written informed consent to participate in this study.
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
This work was supported by the National Nature Scientific Funding of China (no. 82072555), Chinese Cardiovascular Association- Access fund (2019-CCA-ACCESS-023), and the National Nature Scientific Funding of Hunan Province and Changsha (2021JJ30948 and 202203013201).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Anderson L, Thompson DR, Oldridge N, Zwisler A-D, Rees K, Martin N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. (2016) 2016:CD001800. doi: 10.1002/14651858.CD001800
2. Commitee of Cardiac Rehabilitation and Prevention of Chinese Association of Rehabilitation Medicine. Guidelines for cardiovascular rehabilitation and secondary prevention in China 2018 simplified edition. Zhonghua Nei Ke Za Zhi. (2018) 57:802–10. doi: 10.3760/cma.j.issn.0578-1426.2018.11.003
3. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 esc guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (Esc). Developed with the special contribution of the Heart Failure Association (Hfa) of the Esc. Eur J Heart Fail. (2016) 18:891–975. doi: 10.1002/ejhf.592
4. Moe GW, Ezekowitz JA, O’Meara E, Howlett JG, Fremes SE, Al-Hesayen A, et al. The 2013 Canadian cardiovascular society heart failure management guidelines update: focus on rehabilitation and exercise and surgical coronary revascularization. Can J Cardiol. (2014) 30:249–63. doi: 10.1016/j.cjca.2013.10.010
5. Thomas RJ, Balady G, Banka G, Beckie TM, Chiu J, Gokak S, et al. 2018 Acc/Aha clinical performance and quality measures for cardiac rehabilitation: a report of the american college of cardiology/american heart association task force on performance measures. J Am Coll Cardiol. (2018) 71:1814–37. doi: 10.1016/j.jacc.2018.01.004
6. Schürmann J, Noack F, Bethge S, Heinze V, Schlitt A. Patients with heart failure during and after inpatient cardiac rehabilitation. Vasc Health Risk Manag. (2021) 17:49–58. doi: 10.2147/VHRM.S276465
7. Motoki H, Nishimura M, Kanai M, Kimura K, Minamisawa M, Yamamoto S, et al. Impact of inpatient cardiac rehabilitation on barthel index score and prognosis in patients with acute decompensated heart failure. Int J Cardiol. (2019) 293:125–30. doi: 10.1016/j.ijcard.2019.06.071
8. Suzuki S, Momosaki R, Watanabe T, Abo M. Effectiveness of early rehabilitation for acute heart failure: a retrospective cohort study. J Cardiopulm Rehabil Prev. (2019) 39:E23–5. doi: 10.1097/HCR.0000000000000422
9. Takada S, Kondo T, Yasunaga M, Watanabe S, Kinoshita H, Fukuhara S, et al. Early rehabilitation in older patients hospitalized with acute decompensated heart failure: a retrospective cohort study. Am Heart J. (2020) 230:44–53. doi: 10.1016/j.ahj.2020.09.009
10. Nakamura K, Ohbe H, Uda K, Fushimi K, Yasunaga H. Early rehabilitation after acute myocardial infarction: a nationwide inpatient database study. J Cardiol. (2021) 78:456–62. doi: 10.1016/j.jjcc.2021.06.004
11. Kaneko H, Itoh H, Kamiya K, Morita K, Sugimoto T, Konishi M, et al. Acute-phase initiation of cardiac rehabilitation and clinical outcomes in hospitalized patients for acute heart failure. Int J Cardiol. (2021) 340:36–41. doi: 10.1016/j.ijcard.2021.08.041
12. Reeves GR, Whellan DJ, O’Connor CM, Duncan P, Eggebeen JD, Morgan TM, et al. A novel rehabilitation intervention for older patients with acute decompensated heart failure: the rehab-Hf pilot study. JACC Heart Fail. (2017) 5:359–66. doi: 10.1016/j.jchf.2016.12.019
13. Scalvini S, Grossetti F, Paganoni AM, La Rovere MT, Pedretti RF, Frigerio M. Impact of in-hospital cardiac rehabilitation on mortality and readmissions in heart failure: a population study in Lombardy, Italy, from 2005 to 2012. Eur J Prev Cardiol. (2019) 26:808–17. doi: 10.1177/2047487319833512
14. Scrutinio D, Passantino A, Catanzaro R, Farinola G, Lagioia R, Mastropasqua F, et al. Inpatient cardiac rehabilitation soon after hospitalization for acute decompensated heart failure: a propensity score study. J Cardiopulm Rehabil Prev. (2012) 32:71–7. doi: 10.1097/HCR.0b013e31823be124
15. Tsai Y-J, Li M-H, Chen C-H, Tuan S-H, Chen Y-J, Lin K-L. Improved oxygen uptake efficiency slope in acute myocardial infarction patients after early phase I cardiac rehabilitation. Int J Rehabil Res. (2017) 40:215–9. doi: 10.1097/MRR.0000000000000229
16. Balen S, Vukelić-Damijani N, Persić V, Ruzić A, Miletić B, Samardiija M, et al. Anti-inflammatory effects of exercise training in the early period after myocardial infarction. Coll Antropol. (2008) 32:285–91.
17. Zhang Z, Pack Q, Squires RW, Lopez-Jimenez F, Yu L, Thomas RJ. Availability and characteristics of cardiac rehabilitation programmes in China. Heart Asia. (2016) 8:9–12. doi: 10.1136/heartasia-2016-010758
18. Zhou Y, Li J, Du S, Du X, Fu C, Cao C, et al. Cardiac rehabilitation knowledge in patients with coronary heart disease in baoding city of china: a cross-sectional study. Int J Nurs Sci. (2017) 4:24–8. doi: 10.1016/j.ijnss.2016.12.011
19. Yancy C, Abraham WT. Noninvasive hemodynamic monitoring in heart failure: utilization of impedance cardiography. Congest Heart Fail. (2003) 9:241–50. doi: 10.1111/j.1751-7133.2003.tb00021.x
20. Nazário Leão R, Silva PMD, Pocinho RM, Alves M, Virella D, Palma Reis R. Good agreement between echocardiography and impedance cardiography in the assessment of left ventricular performance in hypertensive patients. Clin Exp Hypertens. (2018) 40:461–7. doi: 10.1080/10641963.2017.1392558
21. Packer M, Abraham WT, Mehra MR, Yancy CW, Lawless CE, Mitchell JE, et al. Utility of impedance cardiography for the identification of short-term risk of clinical decompensation in stable patients with chronic heart failure. J Am Coll Cardiol. (2006) 47:2245–52. doi: 10.1016/j.jacc.2005.12.071
22. National Center for Cardiovascular Diseases Expert Committee on Expert Consensus on Phase I Cardiac Rehabilitation of Integrated Traditional Chinese and Western Medicine. Consensus on phase I cardiac rehabilitation of integrated traditional Chinese and western medicine. Chin. J. Hypertens. (2017) 25:1140–8.
23. Januzzi JL, van Kimmenade R, Lainchbury J, Bayes-Genis A, Ordonez-Llanos J, Santalo-Bel M, et al. Nt-Probnp testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the international collaborative of Nt-Probnp study. Eur Heart J. (2006) 27:330–7. doi: 10.1093/eurheartj/ehi631
24. Santaguida PL, Don-Wauchope AC, Oremus M, McKelvie R, Ali U, Hill SA, et al. Bnp and Nt-probnp as prognostic markers in persons with acute decompensated heart failure: a systematic review. Heart Fail Rev. (2014) 19:453–70. doi: 10.1007/s10741-014-9442-y
25. Kang S-H, Park JJ, Choi D-J, Yoon C-H, Oh I-Y, Kang S-M, et al. Prognostic value of Nt-Probnp in heart failure with preserved versus reduced Ef. Heart. (2015) 101:1881–8. doi: 10.1136/heartjnl-2015-307782
26. Seino Y, Ogawa A, Yamashita T, Fukushima M, Ogata K-I, Fukumoto H, et al. Application of Nt-Probnp and Bnp measurements in cardiac care: a more discerning marker for the detection and evaluation of heart failure. Eur J Heart Fail. (2004) 6:295–300. doi: 10.1016/j.ejheart.2003.12.009
27. Taya M, Amiya E, Hatano M, Maki H, Nitta D, Saito A, et al. High-intensity aerobic interval training can lead to improvement in skeletal muscle power among in-hospital patients with advanced heart failure. Heart Vessels. (2018) 33:752–9. doi: 10.1007/s00380-018-1120-x
28. Summers RL, Shoemaker WC, Peacock WF, Ander DS, Coleman TG. Bench to bedside: electrophysiologic and clinical principles of noninvasive hemodynamic monitoring using impedance cardiography. Acad Emerg Med. (2003) 10:669–80. doi: 10.1111/j.1553-2712.2003.tb00054.x
29. Parashar R, Bajpai M, Goyal M, Singh S, Tiwari S, Narayan VS. Impedance cardiography for monitoring changes in cardiac output. Indian J Physiol Pharmacol. (2012) 56:117–24.
30. Chursina TV, Shcherbatykh SI, Tarasov KM, Molchanov AV. [Physical rehabilitation of inpatients with ischemic heart disease]. Klin Med. (2008) 86:31–5.
31. Chursina TV, Molchanov AV. [Physical exercises in rehabilitation of patients with coronary heart disease at in-patient stage]. Vopr Kurortol Fizioter Lech Fiz Kult. (2008) 9–12.
32. Yu C-M, Wang L, Chau E, Chan RH-W, Kong S-L, Tang M-O, et al. Intrathoracic impedance monitoring in patients with heart failure: correlation with fluid status and feasibility of early warning preceding hospitalization. Circulation. (2005) 112:841–8.
33. Galas A, Krzesiński P, Gielerak G, Piechota W, Uziębło-Życzkowska B, Stańczyk A, et al. Complex assessment of patients with decompensated heart failure: the clinical value of impedance cardiography and N-terminal pro-brain natriuretic peptide. Heart Lung. (2019) 48:294–301. doi: 10.1016/j.hrtlng.2018.10.004
34. Pimenta J, Paulo C, Mascarenhas J, Gomes A, Azevedo A, Rocha-Gonçalves F, et al. Bnp at discharge in acute heart failure patients: is it all about volemia? A study using impedance cardiography to assess fluid and hemodynamic status. Int J Cardiol. (2010) 145:209–14. doi: 10.1016/j.ijcard.2009.08.001
35. Gielerak G, Krzesiński P, Piotrowicz E, Piotrowicz R. The usefulness of impedance cardiography for predicting beneficial effects of cardiac rehabilitation in patients with heart failure. Biomed Res Int. (2013) 2013:595369. doi: 10.1155/2013/595369
36. Gielerak G, Piotrowicz E, Krzesiński P, Kowal J, Grzȩda M, Piotrowicz R. The effects of cardiac rehabilitation on haemodynamic parameters measured by impedance cardiography in patients with heart failure. Kardiol Pol. (2011) 69:309–17.
37. Sadauskas S, Naudžiūnas A, Unikauskas A, Mašanauskienė E, Ališauskas A, Bakšytė G, et al. Diagnostic and outcome prediction value of transthoracic impedance cardiography in heart failure patients during heart failure flare-Ups. Med Sci Monit. (2018) 24:6573–8. doi: 10.12659/MSM.910754
38. Thompson B, Drazner MH, Dries DL, Yancy CW. Systolic time ratio by impedance cardiography to distinguish preserved Vs impaired left ventricular systolic function in heart failure. Congest Heart Fail. (2008) 14:261–5. doi: 10.1111/j.1751-7133.2008.00001.x
39. Vijayaraghavan K, Crum S, Cherukuri S, Barnett-Avery L. Association of impedance cardiography parameters with changes in functional and quality-of-life measures in patients with chronic heart failure. Congest Heart Fail. (2004) 10(2 Suppl 2):22–7.
40. Nazário Leáo R, Marques Silva P, Branco L, Fonseca H, Bento B, Alves M, et al. Systolic time ratio measured by impedance cardiography accurately screens left ventricular diastolic dysfunction in patients with arterial hypertension. Clin Hypertens. (2017) 23:28. doi: 10.1186/s40885-017-0084-y
Keywords: phase 1 cardiac rehabilitation, impedance cardiography, acute heart failure, cardiac function, hemodynamics
Citation: Wang Y, Xiao Y, Tang J, Liu Y, Li H, Peng Z, Xu D and Shen L (2022) Effects of early phase 1 cardiac rehabilitation on cardiac function evaluated by impedance cardiography in patients with coronary heart disease and acute heart failure. Front. Cardiovasc. Med. 9:958895. doi: 10.3389/fcvm.2022.958895
Received: 01 June 2022; Accepted: 01 August 2022;
Published: 24 August 2022.
Edited by:
Grigorios Giamouzis, University Hospital of Larissa, GreeceReviewed by:
Emmanouil S. Kallistratos, Asklepeion General Hospital, GreeceCopyright © 2022 Wang, Xiao, Tang, Liu, Li, Peng, Xu and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Shen, c2hlbmxpMTk4NjEyMjJAY3N1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share second authorship
§These authors have contributed equally to this work and share third authorship
||These authors have contributed equally to this work and share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.