- 1Centro Cardiologico Monzino IRCCS, Milan, Italy
- 2Department of Electronics, Information and Biomedical Engineering, Politecnico di Milano, Milan, Italy
Aims: COVID-19 has dramatically impacted the healthcare system. Evidence from previous studies suggests a decline in in-hospital admissions for acute myocardial infarction (AMI) during the pandemic. However, the effect of the pandemic on mechanical complications (MC) in acute ST-segment elevation myocardial infarction (STEMI) has not been comprehensively investigated. Therefore, we evaluated the impact of the pandemic on MC and in-hospital outcomes in STEMI during the second wave, in which there was a huge SARS-CoV-2 diffusion in Italy.
Methods and results: Based on a single center cohort of AMI patients admitted with STEMI between February 1, 2019, and February 28, 2021, we compared the characteristics and outcomes of STEMI patients treated during the pandemic vs. those treated before the pandemic. In total, 479 STEMI patients were included, of which 64.5% were during the pandemic. Relative to before the pandemic, primary percutaneous coronary intervention (PCI) declined (87.7 vs. 94.7%, p = 0.014) during the pandemic. Compared to those admitted before the pandemic (10/2019 to 2/2020), STEMI patients admitted during the second wave (10/2020 to 2/2021) presented with a symptom onset-to-door time greater than 24 h (26.1 vs. 10.3%, p = 0.009) and a reduction of primary PCI (85.2 vs. 97.1%, p = 0.009). MC occurred more often in patients admitted during the second wave of the pandemic than in those admitted before the pandemic (7.0 vs. 0.0%, p = 0.032). In-hospital mortality increased during the second wave (10.6 vs. 2.9%, p = 0.058).
Conclusion: Although the experience gained during the first wave and a more advanced hub-and-spoke system for cardiovascular emergencies persists, late hospitalizations and a high incidence of mechanical complications in STEMI were observed even in the second wave.
Introduction
The global outbreak of coronavirus disease 2019 (COVID-19) has led to not only a significant number of deaths and morbidities but has also impacted other non-COVID-19 conditions, including cardiovascular ones (1). Indeed, a growing amount of data suggests a dramatic decline in hospital admissions for acute myocardial infarction (AMI) worldwide during the COVID-19 pandemic, mostly because patients did not activate emergency medical systems because hospitals were perceived as dangerous places due to the infection risk (2–6). Moreover, several hospitals were dedicated to COVID-19 emergencies. Most intensive therapy beds, including those in intensive cardiac care units, have been dedicated to treating patients with pneumonia and severe acute respiratory syndrome. For this reason, the government of Lombardy (Italy), one of the first countries hit by the pandemic outside China, and local health authorities decided to centralize the treatment of cardiovascular emergencies in a limited number of centers. In particular, a big hub-and-spoke model for cardiovascular, either cardiological or cardiac surgical emergencies, was built up soon after the COVID-19 outbreak to converge treatment of acute coronary syndrome (ACS) in dedicated centers active 24/7 in the region, implementing availability of intensive care unit beds in general hospitals converted to COVID-19 treatment. Therefore, our cardiology institute (Centro Cardiologico Monzino, Milan) became one of the four referral centers for cardiovascular emergencies in this regional hub-and-spoke system, and we, therefore, admitted and treated an increased number of AMI patients, compared with the decline in hospitalizations for AMI observed overall in our region and other countries.
It is also well-known that, during the COVID-19 pandemic, patients with AMI had a significantly higher in-hospital mortality than those admitted before COVID-19, potentially due to their late arrival at the hospital. In this critical clinical setting, mechanical complications (MC) and cardiogenic shock are rare but disastrous complications with a poor prognosis (7). Data on MC rates during the COVID-19 pandemic are scarce. However, delays and lack of prompt pharmacologic or invasive reperfusion therapies during the COVID-19 pandemic might have been linked to increased AMI complications.
In this study, we aimed to compare in-hospital outcomes of AMI patients admitted before (October 2019–February 2020) and during the pandemic (March 2020–February 2021), with a special focus on the incidence of MC between the two study periods. Moreover, we believe that the second pandemic wave, mainly thanks to knowledge and experience gained during the first wave and a more advanced hub-and-spoke system, may be more representative of the impact of COVID-19 on acute cardiovascular disease; we compared the hospital outcomes, and MC rates of AMI patients hospitalized only during the second wave (October 2020–February 2021) with those admitted before the pandemic.
Materials and methods
Study population
This retrospective study was carried out on a consecutive cohort of AMI patients admitted to Cardiac Center Monzino IRCCS (Milan, Italy) with acute ST-segment elevation myocardial infarction (STEMI) between February 1, 2019, and February 28, 2021. Patients underwent primary PCI if they had typical chest pain within 12 h (24 h for those with cardiogenic shock) and ST-segment elevation of at least 1 mm in two or more contiguous leads or a new left bundle branch block. The exclusion criteria were non-evidence of atherothrombotic coronary artery disease at angiography (e.g., vasospastic angina or coronary dissection). The history of each patient was recorded at the time of hospital admission in a single electronic database, and the identification of STEMI was based on data generated at hospital discharge. In order to compare the clinical characteristics, management, and outcomes of STEMI patients before and during the COVID-19 period, we decided to consider the cut-off date for the introduction of the state of sanitary emergency for the COVID-19 pandemic in Italy (March 1, 2020). Therefore, the study population was categorized into two periods: from March 2020 to February 2021 (during the pandemic) and from February 2019 to February 2020 (before the pandemic). To outline the characteristics of STEMI patients admitted during the second COVID-19 wave period (Figure 1), patients admitted for STEMI from October 2020 to February 2021 were identified and compared with those admitted before the COVID-19 pandemic (from October 2019 to February 2020). The study complied with the Declaration of Helsinki. The ethics committee approved the research, and informed consent was obtained from each subject.
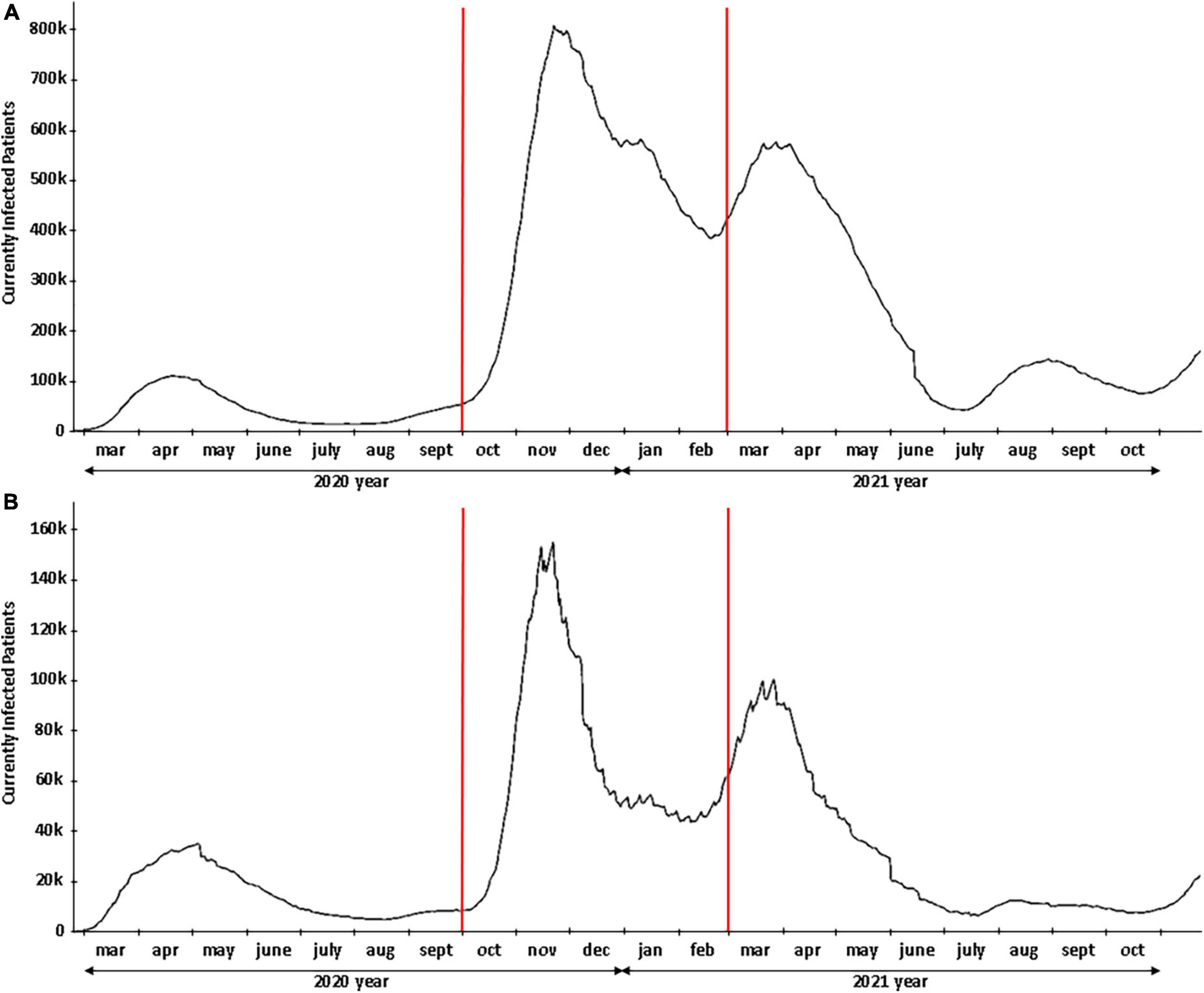
Figure 1. COVID-19 pandemic profile. (A) Cases in Italy. (B) Cases in the Lombardy region. The red lines delineate the second wave of COVID-19.
Clinical variables and definitions
Evaluation of patients included medical history, electrocardiography (ECG), blood examination, transthoracic echocardiography (TTE), and coronary angiography. In addition to demographic characteristics (age, sex, body mass index [BMI]), and cardiovascular risk factors (including arterial hypertension, current smoking, dyslipidemia, diabetes mellitus, prior cardiovascular events, etc.), the following variables were collected: medical therapy before admission and during hospitalization; Killip class; ischemic time (time from symptoms’ onset to hospital admission); Thrombolysis In Myocardial Infarction (TIMI) flow grade before and after PCI; left ventricular (LV) ejection fraction (LVEF); intensive coronary care unit length of stay; MC; concomitant SARS-CoV-19 infection. SARS-CoV-19 infection was defined by molecular testing on nasopharyngeal swabs or bronchoalveolar lavage fluid at presentation. The decision to perform PCI or surgical approach for MC was decided by the heart team according to guidelines (8, 9). MCs included: rupture of the LV free wall defined as an abrupt tear in the infarcted myocardium causing hemopericardium and cardiac tamponade; rupture of the papillary muscle defined as a tear in the infarcted mitral subvalvular apparatus causing acute mitral regurgitation; and ventricular septal rupture defined as a tear in the infarcted interventricular septum with evidence of a shunt between the left and right ventricle (Figure 2). TTE was performed in all patients soon after hospital admission and then repeated during hospitalization, using commercially available ultrasound systems (Vivid E9 and E95; GE Medical Systems, Horten, Norway; and iE33 and Epiq; Philips Medical Systems, Andover, Massachusetts) in the parasternal (long- and short-axis) and apical (2-, 3-, and 4-chamber) views. Echocardiographic measurements were made in accordance with guidelines (10). Transesophageal echocardiography (TEE) was also performed when TTE was suboptimal to confirm and complete TTE evaluation, particularly in ventilated patients and all cases undergoing surgery.
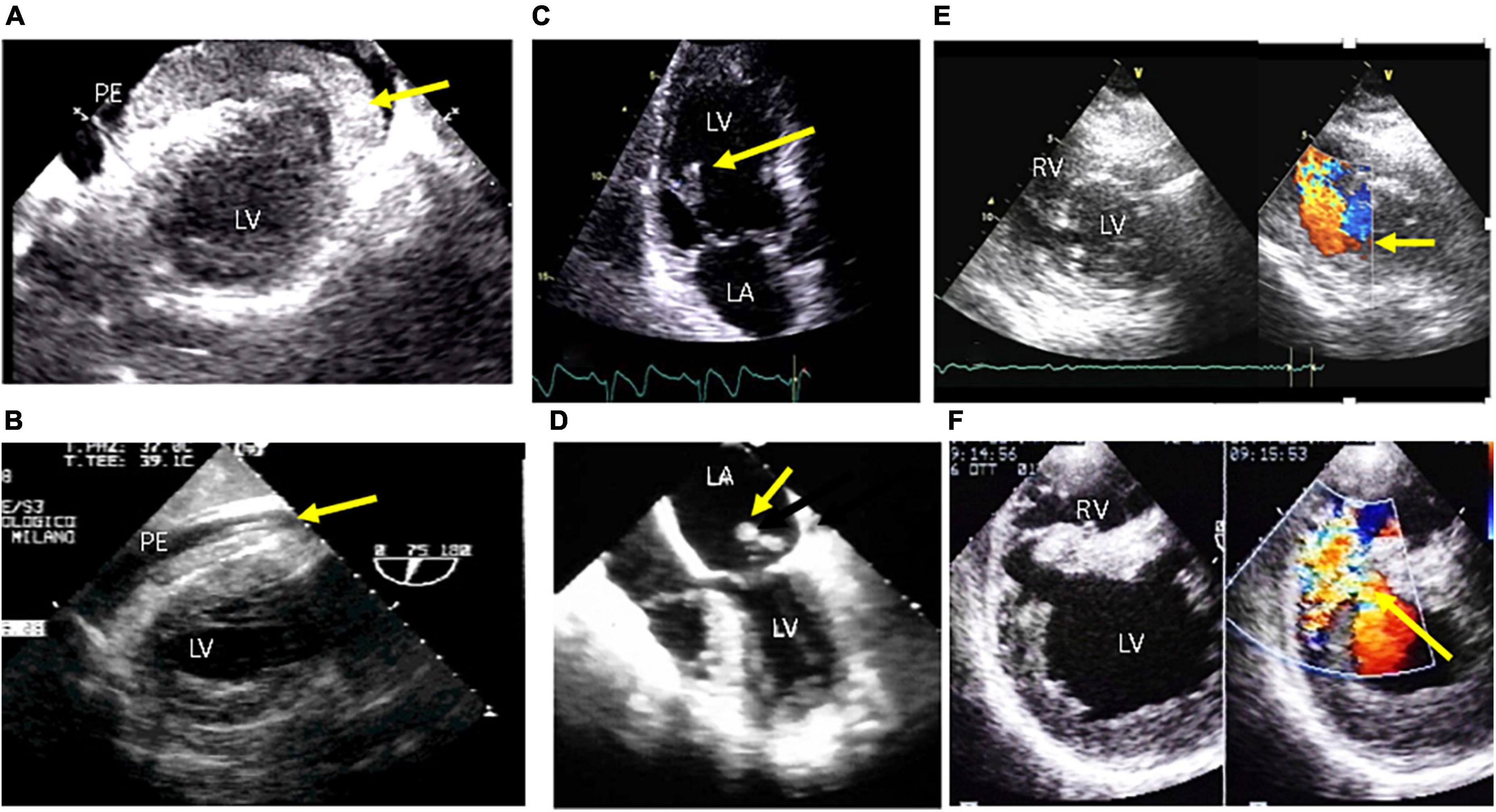
Figure 2. Echocardiographic aspects of mechanical complications of acute myocardial infarction. Upper panel: transthoracic echo. Lower panel: transesophageal echo. LV, left ventricle; RV, right ventricle. (A,B) Free wall rupture with pericardial effusion (PE) and thrombosis intrapericardial hematoma in the pericardial space (yellow arrows); (C) partial papillary muscle rupture (yellow arrow); (D) Complete papillary muscle rupture (yellow arrow) with eversion in the left atrium (LA); (E,F) ventricular septal defect with left-to-right shunt across the septum (yellow arrows).
Statistical analysis
Statistical analysis was performed with SPSS, version 27 software (SPSS, Inc., Chicago, IL, USA). Continuous variables were expressed as mean ± standard deviation (SD) or median (25th–75th percentile) as appropriate, and discrete variables as absolute numbers and percentages. Student-independent t- or Mann–Whitney U tests were used as appropriate to compare continuous variables between patients during and before the pandemic. Comparisons between groups of discrete variables were performed by χ2 or Fisher exact test if the expected cell count was < 5. Logistic regression analysis was used to assess independent predictors of MCs (results presented as odds ratio and 95% confidence interval). Variables with a P < 0.05 in univariate analysis were included in a multivariate logistic regression analysis with a stepwise selection procedure for identifying independent variables predicting MCs. All tests were two-tailed, and a P-value < 0.05 was considered statistically significant.
Results
A total of 479 STEMI patients were included in the analysis from February 2019 to February 2021. Of them, 170 (35.5%) were admitted before the pandemic, whereas 309 (64.5%) were admitted during the pandemic. The study population comprised 367 men and 112 women (mean age, 67 ± 12 years). The number of STEMI patients positive for SARS-CoV-2 infection was 7 (2.3%). Patients’ characteristics before and during the COVID-19 period are listed in Table 1. Cardiovascular risk factors (arterial hypertension, diabetes mellitus, dyslipidemia), LVEF at presentation, and arrhythmic complications (atrial fibrillation and/or ventricular arrhythmias) were similar in the study groups, regardless of the temporal window considered. Patients undergoing primary PCI within 24 h of the onset of symptoms had significantly fewer symptoms during the pandemic than those before the pandemic (87.7 vs. 94.7%, p = 0.014). During the pandemic, a higher incidence of intraventricular thrombosis (6.1 vs. 1.2%, p = 0.01) was observed compared to the previous no-pandemic year. There was no significant difference in MC rate between the two study periods, despite a clear trend toward more MC in the pandemic period (13 cases vs. 3 cases, respectively). Furthermore, in-hospital deaths (18.1 vs. 14.7%, p = 0.218) were higher during the pandemic, but the difference was insignificant.
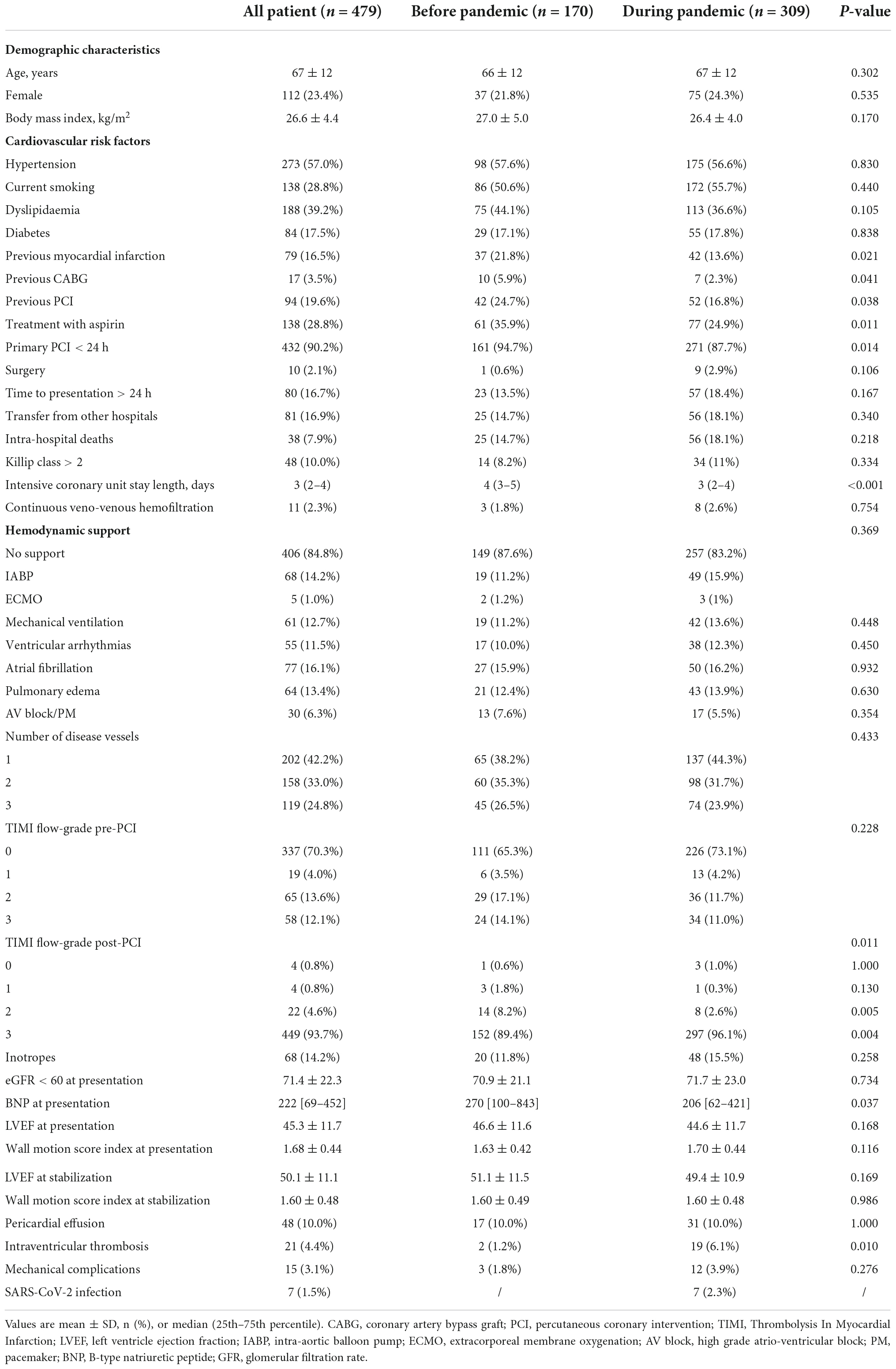
Table 1. Baseline and clinical characteristics of the study population before and during the pandemic.
Regarding the second wave of the COVID-19 pandemic in Italy, from October 1, 2020, to February 28, 2021 (Figure 1), in which there was a huge SARS-CoV-2 diffusion, 142 STEMI patients were admitted to our center. During the second wave of the pandemic, two STEMI patients (1.7%) had a concomitant infection with SARS-CoV-2. Compared to the same non-COVID-19 temporal window (from October 1, 2019, to February 28, 2020), patients admitted during the second wave presented more frequently with symptoms of onset-to-door time longer than 24 h (26.1 vs. 10.3%, p = 0.009). The rate of reperfusion by primary PCI within 24 h of the onset of symptoms was lower during the second wave of the pandemic than in the same pre-pandemic time window (85.2 vs. 97.1%, p = 0.009). Inotropic drugs were significantly more frequent during the second wave than during the pre-pandemic period (19.0 vs. 7.4%, p = 0.028). Pericardial effusion and LV thrombosis were higher in STEMI patients admitted during the second-wave period than in those admitted before COVID-19 (14.1 vs. 7.4%, p = 0.159; 7.7% vs. 1.5%, p = 0.108, respectively), although these differences were not significant (Table 2).
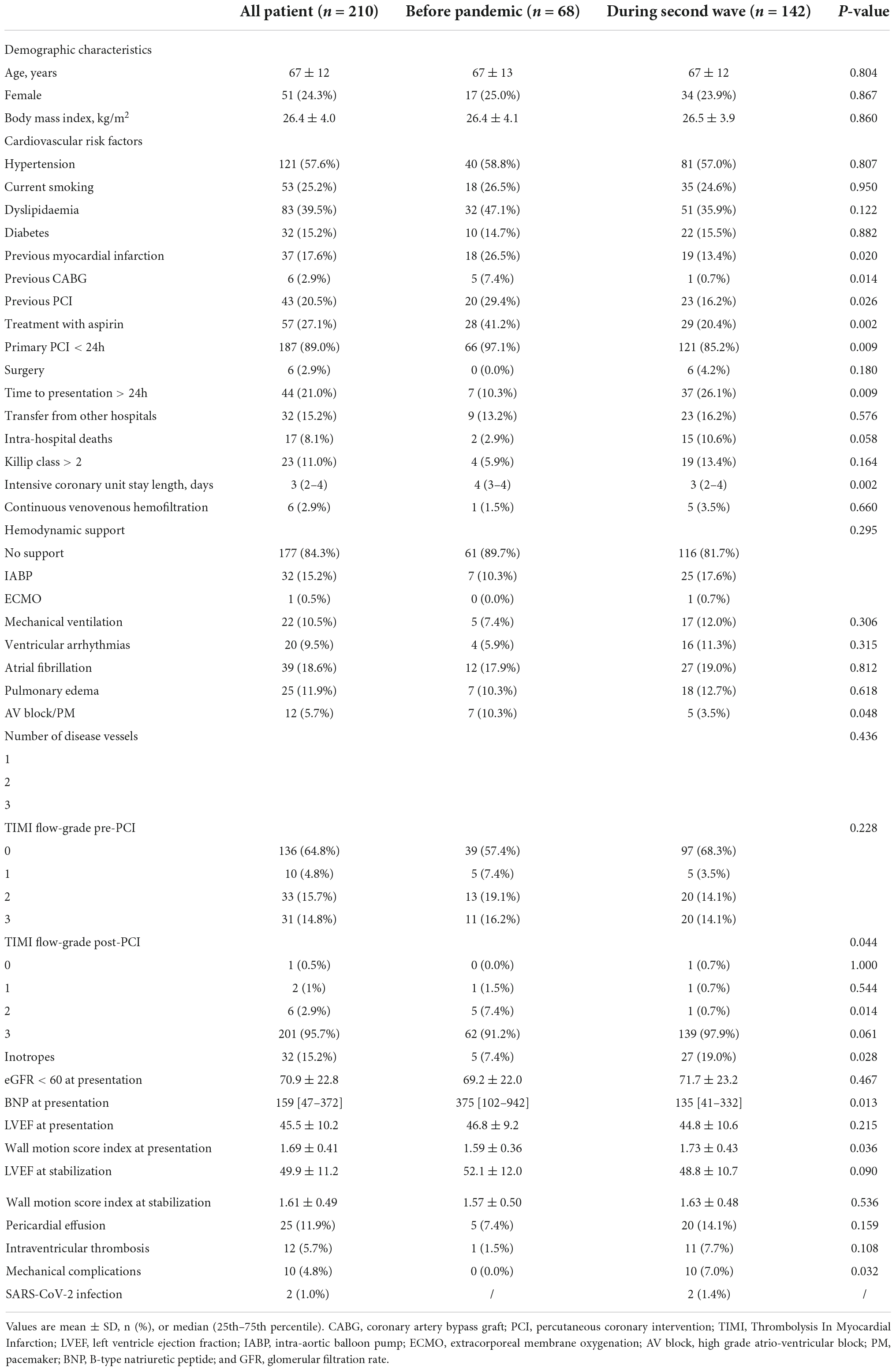
Table 2. Patient’s baseline and clinical characteristics before the pandemic and during the second COVID-19 wave.
Moreover, MC occurred more often in patients admitted during the second wave of the COVID-19 pandemic than in those admitted before the pandemic (7.0 vs. 0.0%, p = 0.032) (Table 2). Finally, in-hospital deaths (10.6 vs. 2.9%, p = 0.058) tended to be higher during the second wave than in the pre-pandemic period (Table 2). Additionally, the wall motion score index at presentation was significantly higher in STEMI patients admitted during the second wave of the pandemic than before the pandemic period (1.73 ± 0.43 vs. 1.59 ± 0.36, p = 0.036) (Table 2).
Looking at the 10 STEMI patients with MC during the second wave of the pandemic, we observed that acute free wall rupture, ventricular septal rupture, and papillary muscle rupture occurred in two (1.4%), four (2.8%), and four (2.8%) patients, respectively (Supplementary Table 1). Seven cases underwent surgery; three survived, while three others were not operated on and died. The baseline characteristics of patients with MC are reported in Table 3. Overall, 50% were men, and the mean age was 77 ± 5 years; 40.0% had pericardial effusion, 30.0% had an apical aneurism, 20.0% reported an apical thrombosis, 70.0% died during the hospital stay, and 80.0% had a symptom onset to hospital arrival time ≥ 24 h (Figure 3). Due to late arrival and/or no indications for other clinical and angiographic reasons, eight out of these ten cases did not undergo PCI. None were confirmed positive for SARS-CoV-2 infection.
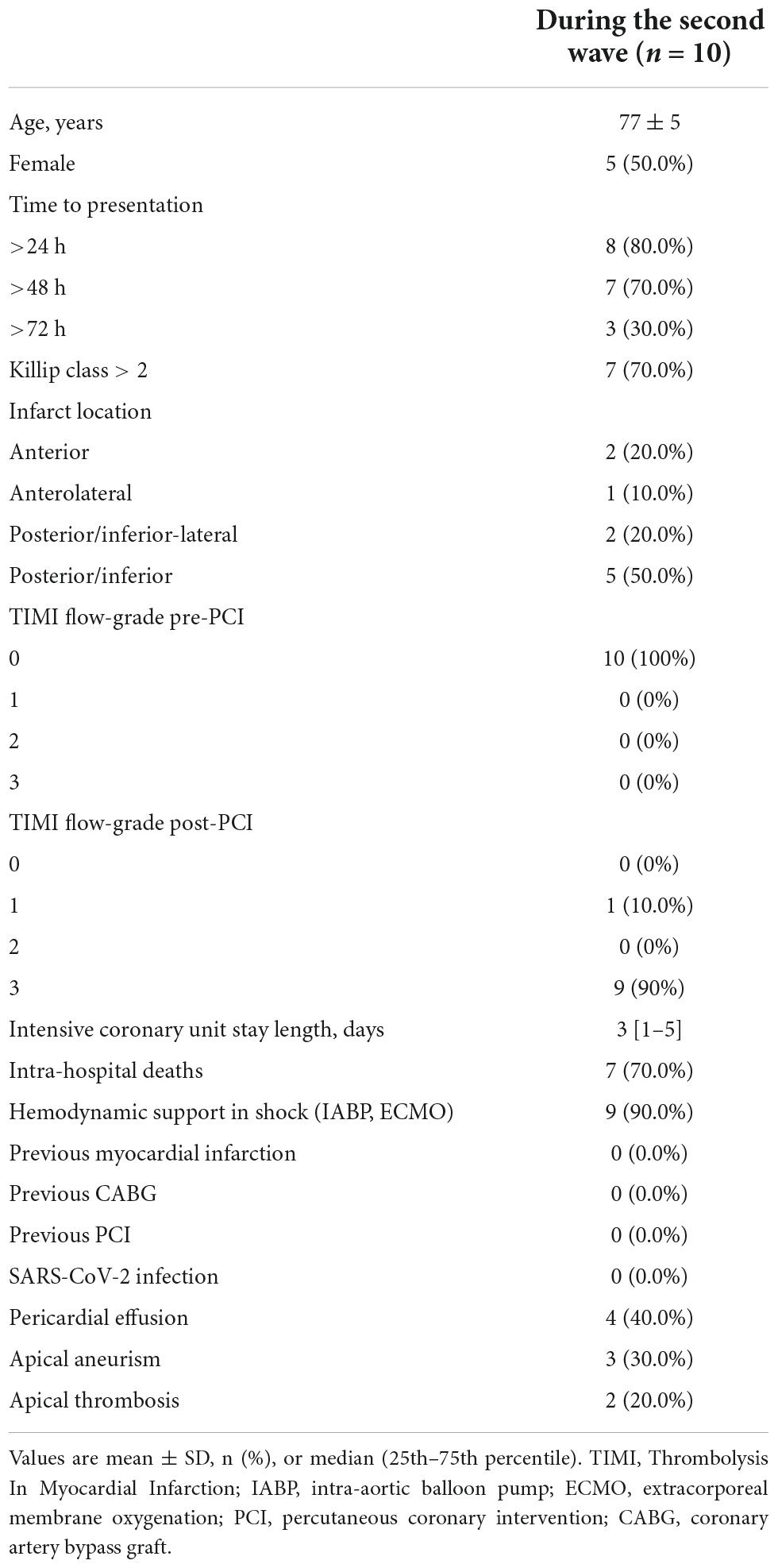
Table 3. Patient characteristics of STEMI patients with mechanical complications admitted during the second COVID-19 wave.
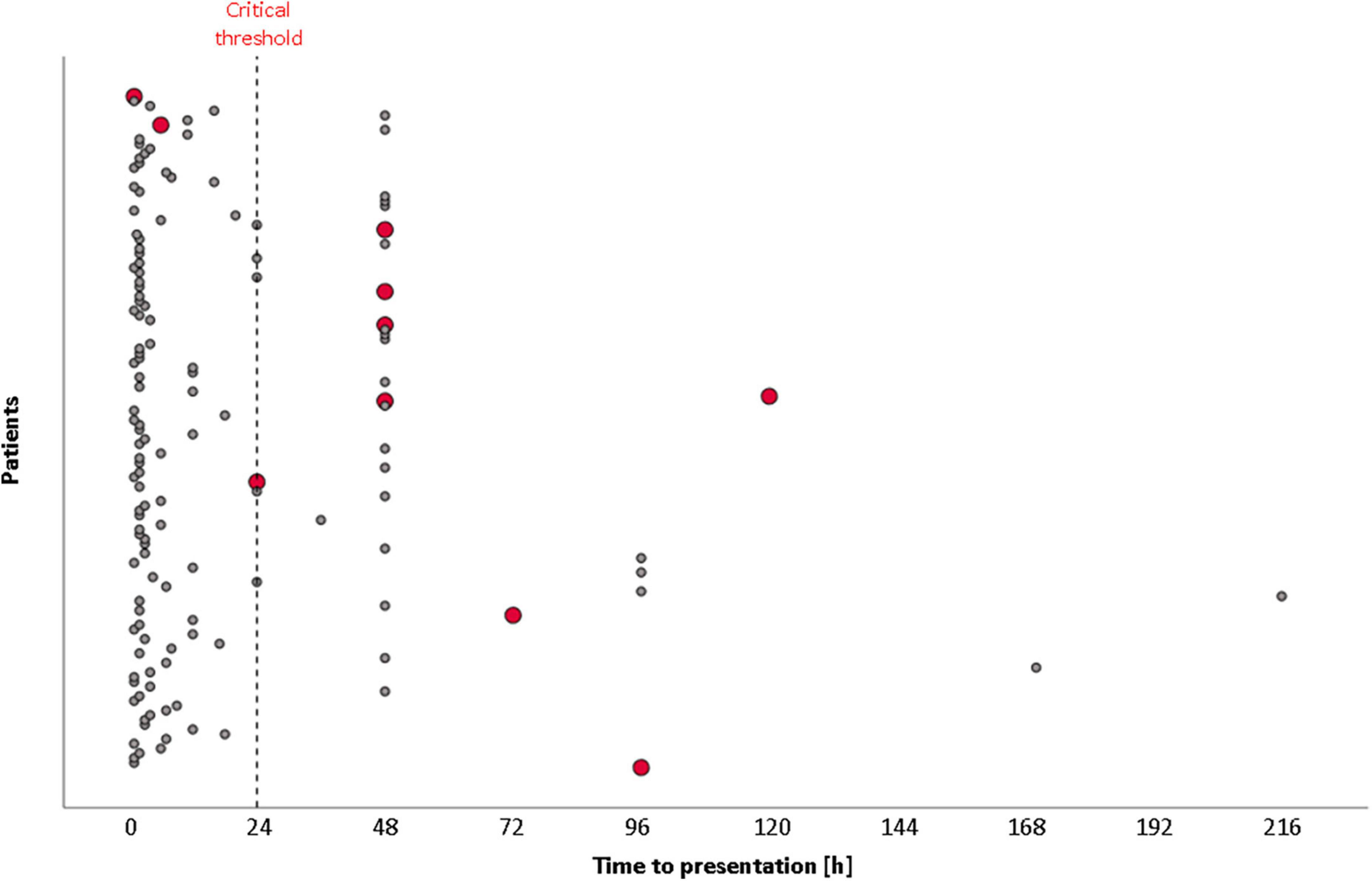
Figure 3. Time from symptoms’ onset to hospital presentation in STEMI patients during the second wave of COVID-19. Red points represent STEMI patients with mechanical complications.
In an analysis limited to STEMI patients admitted during the second wave of the pandemic, including all variables that clustered patients with MCs with a p < 0.05, the multivariable analysis demonstrated that transfer from other hospitals (OR: 5.53 [95% CI: 1.03–29.77]) and cardiogenic shock (OR: 18.92 [95% CI: 1.68–212.56]) were independent predictors of MCs (Table 4).

Table 4. Univariable and multivariable predictors of risk of mechanical complications were observed during the second COVID-19 wave.
Discussion
This study aimed to investigate the impact of the COVID-19 pandemic on AMI patients, specifically on clinical and echocardiographic complications, including MCs rate, admitted to a macro-hub center during the COVID-19 pandemic, with a special focus on the second wave of COVID-19.
Indeed, the Lombardy Region government built up a big hub-and-spoke model to converge treatment of ACS in 13 dedicated centers active 24/7 in the region, implementing the availability of intensive care unit beds in general hospitals converted to COVID-19 treatment. Our institute was one of the four selected macro-hub centers in Milan (Lombardy, Italy) for cardiological or cardiac surgical emergencies (four in the entire Lombardy Region). Due to this specific hub-and-spoke organization, we admitted and treated more AMI patients during the COVID-19 pandemic, compared to the decrease in PCI procedures and AMI admissions in our region and other countries. Therefore, we had the unique opportunity to investigate the time trends of admissions for AMI, rate of major complications, and in-hospital mortality, as well as detailed clinical and echocardiographic data before and during the pandemic and according to the first or second COVID-19 wave. By focusing our analysis on the second wave of the pandemic, we observed that the main finding of this study is the clear demonstration that the incidence of MC significantly increased with the delay between symptoms onset and hospital admission. In particular, 10 AMI patients had an MC in the second wave (7%) vs. 0 in the pre-pandemic matched period. Of the 10 cases with MC (Figure 3), 1 had a delay of >24 h and 7 > 48 h. In-hospital mortality in the second wave of the COVID-19 period was 10.6 vs. 2.9% of the pre-pandemic period, and a time to presentation > 24 h was observed in 26.1 vs. 10.3% of the second-wave and pre-pandemic periods, respectively, thereby markedly reducing the rate of PCI < 24 h.
All clinical and echocardiographic findings showed a trend toward higher severity of the myocardial injury and related hemodynamic consequences in patients admitted during the COVID-19 pandemic and, in particular, in those admitted during the second wave, as reported in Table 2. Indeed, Killip class, B-type natriuretic peptide at presentation, inotropes therapy, LV wall motion score, pericardial effusion, and LV thrombus formation confirmed the late arrival to the hospital and no/or late reperfusion dramatically affected hemodynamic status and significantly increased the rates of major AMI complications.
Mechanical complications in the PCI era has a low incidence (0.3–1%) (7, 11). Bouisset et al. (12) recently showed an increased MC in STEMI patients admitted during the pandemic, related to pre-hospital delay in the last 6 months in France (1.3%). The delay between symptoms onset and first medical contact was significantly longer among patients with MC: 801 [210–3406] vs. 135 [60–369] min. Similar to our data, they also observed that LV aneurysm and LV thrombus were more frequent among patients with MC: 4.8 vs. 0.4% and 3.6 vs. 1.3%, respectively. The main difference between that study and ours is that it was a national cohort (65 centers), and half of their cohort was recruited during the first wave of the COVID-19 pandemic in France. Moreover, that period was associated with a strong decrease in hospitalizations in France for ACS. As in our data, very few cases had COVID-19 infection. Thus, MC seems not to be directly related to virus infection and inflammation.
Previous reports described an increasing trend in the cases of MC during the COVID-19 pandemic compared to a parallel time frame before the pandemic. Bryndza et al. (13) observed a decrease among patients presenting with STEMI during the case period (18.6%), with a trend toward a more frequent incidence of MC, correlated to a longer delay between symptoms onset and hospital admission. Compared with the corresponding period before pandemic, Kitahara et al. (14) detected an increase in STEMI late admission during the COVID-19 outbreak (25.4 vs. 14.2%). Patient delay translated into a higher proportion of patients presenting MC upon hospital arrival (14.3 vs. 3.6%). Similarly, Lin et al. (15) showed that although there was no reduction in AMI hospital admissions during the COVID-19 pandemic, a longer onset-to-hospital time may increase MC incidence.
Our data reinforce the well-known relationship between myocardial damage and late or lack of myocardial reperfusion. Studies in the pre-thrombolytic era showed rates of MC as high as 6% with transmural MI, while the incidence in the reperfusion PCI era was as low as < 1%. Elbadawi et al. (7), in a 13-year observational analysis of about 9 million hospitalizations with AMI, showed that the rate of MC was 0.27% in the STEMI cohort and 0.06% in the NSTEMI cohort, with no significant changes over time. The overall in-hospital mortality rate among patients who developed MCs was 42.4% among patients with STEMI and 18.0% among those with NSTEMI, with no changes over time. In our study, the finding of 7% of MC is similar to the pre-PCI era. Moreover, in-hospital mortality (10.6%) was similar to pre-PCI (9–10% with fibrinolytic therapy and 11.5% among patients without therapy). Interestingly, our institute’s in-hospital mortality before the pandemic was 2.9%.
Damluji et al. (16), in a scientific statement from the American Heart Association on MC of Acute Myocardial Infarction, reported that advances in primary prevention resulted in a significant decline in the age- and sex-adjusted incidence of AMI during the past decades. However, despite such improvements, large infarcts, late hospital presentation, and a lack of tissue-level reperfusion attributable to no-reflow or poor coronary flow after PCI remain risk factors for MC, hemodynamic instability, and pump failure. The mortality rate for the 3 MC was very high, even in the PCI era. Although a modern pharmacological and non-pharmacological approach to cardiogenic shock includes papillary muscle rupture (10–40%), ventricular septal defect (30–40%), and rupture of the free LV wall (50%). These data refer to the “ideal” medical and surgical approach in the pre-COVID-19 period with early recognition due to diagnosis, multidisciplinary stakeholder involvement in medical resuscitation, stabilization, and patient-centered planning and timing of appropriate surgical intervention, percutaneous technologies, and mechanical circulatory support. Despite having all these potentialities and approaches in our institute during the second pandemic period, the overall mortality in MC was very high, thus further underlining the severity of the clinical and hemodynamic status in our cases and the differences related to very late arrival at the hospital.
Hub-and-spoke model and impact on MI treatment
Italy was the first western country to be hit by the pandemic. From February 2020, the COVID-19 infection rate rose significantly within a few weeks, prompting a lockdown from March to May (69 consecutive days overall). Therefore, a regional law redesigned the hub-and-spoke system for time-dependent diseases to better allocate resources for COVID-19 patients. The model adopted by Lombardy, the most densely populated region in Italy (approximately 10 million inhabitants with 20 different cardiac surgical units and 55 catheterization laboratories, of which most perform 24/7 PCI), was to concentrate cardiac emergencies in four vascular surgery hubs.
Lombardy was the first European region to reorganize its cardiovascular emergency system in reaction to the spread of the COVID-19 infection. This well-defined pathway for cardiovascular emergencies was efficient in allowing surgical and percutaneous procedures in cases with ACS and rapidly reacting to the first wave of the pandemic. Similarly, when the second wave occurred, the same model was maintained, and our study documented that we admitted 309 patients with AMI in 4 months. Despite this organization, as already demonstrated in the first wave (17), the hub-and-spoke model should be associated with a strong media campaign on the importance of early hospital admission for suspected ACS in a COVID-19-free hospital environment. However, independent of patients’ consideration of the hospital as a possible contagion area, which triggered many patients’ fear of going to the emergency rooms, our data also showed the critical role of transfer from other hospitals. On multivariate analysis, this variable impacted MC, which should stimulate a more rapid transfer to hub hospitals based on symptoms and/or triage, including ECG in the organization of transport in emergency suspected MI.
Several countries organized specific systems to react to this emergency (18–20). As a concern in our region, Bonalumi et al. (21) reported that the proposed hub-and-spoke organization system efficiently safeguarded access to heart and vascular surgery.
In conclusion, despite an efficient hub-and-spoke model for cardiovascular emergencies in our region (Lombardy, Italy), even in the second wave of the COVID-19 pandemic, persistent late admission to the hospital resulted in high STEMI mortality and a high incidence of MC. In parallel with reorganization and optimal resource allocation in a pandemic, health authorities should provide effective programs to increase awareness of the symptoms and timely and standard-of-care treatment of AMI to the general public.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Centro Cardiologico Monzino IRCCS. The patients/participants provided their written informed consent to participate in this study.
Author contributions
MarP, AF, NC, GT, FC, PR, ST, GM, and MauP contributed to the conception and design of the study. AF, NC, MI, PR, ST, and GM organized the database. MarP performed the statistical analysis. MarP and MauP wrote the first draft of the manuscript. GT and AF wrote sections of the manuscript. All authors contributed to the manuscript revision, read, and approved the submitted version.
Funding
This research was supported by the Italian Ministry of Health-Ricerca Corrente to Centro Cardiologico Monzino IRCCS.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.950952/full#supplementary-material
References
1. Thakkar S, Arora S, Kumar A, Jaswaney R, Faisaluddin M, Ammad Ud Din M, et al. A systematic review of the cardiovascular manifestations and outcomes in the setting of Coronavirus-19 disease. Clin Med Insights Cardiol. (2020) 14:1179546820977196. doi: 10.1177/1179546820977196
2. Pessoa-Amorim G, Camm CF, Gajendragadkar P, De Maria GL, Arsac C, Laroche C, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European society of cardiology. Eur Heart J Qual Care Clin Outcomes. (2020) 6:210–6. doi: 10.1093/ehjqcco/qcaa046
3. Xiang D, Xiang X, Zhang W, Yi S, Zhang J, Gu X, et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. (2020) 76:1318–24.
4. Katz JN, Sinha SS, Alviar CL, Dudzinski DM, Gage A, Brusca SB, et al. COVID-19 and disruptive modifications to cardiac critical care delivery: JACC review topic of the week. J Am Coll Cardiol. (2020) 76:72–84. doi: 10.1016/j.jacc.2020.04.029
5. De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, et al. Società Italiana di Cardiologia and the CCU academy investigators group. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. (2020) 41:2083–8.
6. Mesnier J, Cottin Y, Coste P, Ferrari E, Schiele F, Lemesle G, et al. Hospital admissions for acute myocardial infarction before and after lockdown according to the regional prevalence of COVID-19 and patient profile in France: a registry study. Lancet Public Health. (2020) 5:e536–42. doi: 10.1016/S2468-2667(20)30188-2
7. Elbadawi A, Elgendy IY, Mahmoud K, Barakat AF, Mentias A, Mohamed AH, et al. Temporal trends and outcomes of mechanical complications in patients with acute myocardial infarction. JACC Cardiovasc Interv. (2019) 12:1825–36.
8. Kimura K, Kimura T, Ishihara M, Nakagawa Y, Nakao K, Miyauchi K, et al. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ J. (2019) 83:1085–196. doi: 10.1253/circj.CJ-19-0133
9. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. (2018) 39:119–77.
10. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. (2005) 18:1440–63. doi: 10.1016/j.echo.2005.10.005
11. Puerto E, Viana-Tejedor A, Martínez-Sellés M, Domínguez-Pérez L, Moreno G, Martín-Asenjo R, et al. Temporal trends in mechanical complications of acute myocardial infarction in the elderly. J Am Coll Cardiol. (2018) 72:959–66.
12. Bouisset F, Deney A, Ferrières J, Panagides V, Becker M, Riviere N, et al. Mechanical complications in ST-elevation myocardial infarction: the impact of pre-hospital delay. Int J Cardiol. (2021) 345:14–9. doi: 10.1016/j.ijcard.2021.10.020
13. Bryndza MA, Litwinowicz R, Bartuś S, Nosal M, Godlewski J, Orzechowska A, et al. Incidence of mechanical complications following myocardial infarction during the first two months of the COVID-19 pandemic in the Southern Poland region: a multicenter study. Kardiol Pol. (2021) 79:66–8. doi: 10.33963/KP.15653
14. Kitahara S, Fujino M, Honda S, Asaumi Y, Kataoka Y, Otsuka F, et al. COVID-19 pandemic is associated with mechanical complications in patients with ST-elevation myocardial infarction. Open Heart. (2021) 8:e001497.
15. Lin TW, Tsai MT, Wu HY, Roan JN, Luo CY. Mechanical complications of acute myocardial infarction during the COVID-19 pandemic. Acta Cardiol Sin. (2021) 37:114–6.
16. Damluji AA, van Diepen S, Katz JN, Menon V, Tamis-Holland JE, Bakitas M, et al. Mechanical complications of acute myocardial infarction: a scientific statement from the American heart association. Circulation. (2021) 144:e16–35.
17. Trabattoni D, Montorsi P, Merlino L. Late STEMI and NSTEMI patients’ emergency calling in COVID-19 outbreak. Can J Cardiol. (2020) 36:1161.e7–8. doi: 10.1016/j.cjca.2020.05.003
18. Wojakowski W, Bartuś S, Grygier M. Challenging clinical and organizational scenarios in cardiovascular diseases during the SARS-CoV-2 pandemic in Poland. Can we do better? Postepy Kardiol Interwencyjnej. (2020) 16:121–2. doi: 10.5114/aic.2020.95734
19. Scholz KH, Lengenfelder B, Thilo C, Jeron A, Stefanow S, Janssens U, et al. Impact of COVID-19 outbreak on regional STEMI care in Germany. Clin Res Cardiol. (2020) 109:1511–21.
20. Wang J, Ullah I, Dong Z, Ye Z, Gu Q, Tan C, et al. Efficacy of an adjusted treatment strategy on the management and in-hospital outcome of patients with STEMI during the COVID-19 pandemic. J Biomed Res. (2022) 36:70–2. doi: 10.7555/JBR.35.20210173
Keywords: STEMI, COVID-19, coronavirus disease, mechanical complications, acute myocardial infarction
Citation: Penso M, Frappampina A, Cosentino N, Tamborini G, Celeste F, Ianniruberto M, Ravagnani P, Troiano S, Marenzi G and Pepi M (2022) Outcomes and mechanical complications of acute myocardial infarction during the second wave pandemic in a Milan HUB center for cardiac emergencies. Front. Cardiovasc. Med. 9:950952. doi: 10.3389/fcvm.2022.950952
Received: 23 May 2022; Accepted: 15 September 2022;
Published: 03 October 2022.
Edited by:
Fatih Kahraman, Kutahya Health Sciences University, TurkeyReviewed by:
İbrahim Ersoy, Afyonkarahisar Health Sciences University, TurkeyArtur Dziewierz, Jagiellonian University Medical College, Poland
Copyright © 2022 Penso, Frappampina, Cosentino, Tamborini, Celeste, Ianniruberto, Ravagnani, Troiano, Marenzi and Pepi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marco Penso, bWFyY28xLnBlbnNvQG1haWwucG9saW1pLml0
 Marco Penso
Marco Penso Antonio Frappampina1
Antonio Frappampina1 Monica Ianniruberto
Monica Ianniruberto Sarah Troiano
Sarah Troiano Mauro Pepi
Mauro Pepi