- 1School of Physiotherapy, Delhi Pharmaceutical Sciences and Research University, New Delhi, India
- 2Department of Physiotherapy and Health Rehabilitation, College of Applied Medical Sciences, Majmaah University, Al Majmaah, Saudi Arabia
- 3School of Allied Health Sciences, Delhi Pharmaceutical Sciences and Research University, New Delhi, India
- 4Department of Community Medicine/Public Health, College of Medicine, Majmaah University, Al Majmaah, Saudi Arabia
- 5Department of Nursing, College of Applied Medical Sciences, Majmaah University, Al Majmaah, Saudi Arabia
- 6Department of Physical Therapy, Buraydah Private Colleges, Buraydah, Saudi Arabia
- 7Department of Internal Medicine, Security Forces Hospital, Riyadh, Saudi Arabia
- 8College of Applied Medical Sciences, Al Maarefa University, Riyadh, Saudi Arabia
- 9Department of Orthopedic Surgery, College of Medicine, King Khalid University, Abha, Saudi Arabia
- 10Department of Public Health, College of Health Science, Saudi Electronic University, Riyadh, Saudi Arabia
- 11Faculty of Physiotherapy, SGT University, Gurugram, India
- 12Mewat Engineering College, Nuh, India
Objective: Presently, evidence-based research studies on the efficacy of complimentary therapies like yoga for patients with different cardiac diseases are limited and conflicting. The objective of this study is to conduct a systematic review and meta-analysis of randomized controlled trials (RCTs) on yogic interventions compared with usual care or non-pharmacological treatment in patients diagnosed with cardiac diseases.
Methods: We conducted an electronic search of literature published from 2006 to May 2021 through five databases. PRISMA statement was used to develop and report a systematic review and meta-analysis protocol. Sixteen RCTs were included in the systematic review and 11 RCTs were used for meta-analysis. Outcome measures were blood pressure, lipid profile, and psychosocial measures. The Cochrane collaboration tool was used to assess bias risk.
Results: The results show that yogic interventions resulted in significant reduction in systolic (d = 046; 95% CI.08–0.84; I2 = 81.86%) and diastolic blood pressures (d = 0.56; 95% CI.13–0.99, I2 = 84.84%). A medium statistically significant increase in HDL (d =0.67; 95% CI 0 to 1.33; I2 79.7%) and a low but significant effect on LDL (d = 0.23; 95% CI −0.08–0.54; I2 32.61%), total cholesterol (d =0.28; 95% CI −0.14–0.7; I2 63.72%), and triglycerides (d = 0.43; 95% CI −0.1–0.97; I2 76.64%) were observed. Pooled effect sizes showed a medium to low statistically significant effect on psychosocial indicators viz., QoL, stress, anxiety, and depression.
Conclusion: The meta-analysis found strong evidence of effectiveness of yogic interventions on lipid profile, blood pressure, and psychosocial outcomes in patients with diagnosed cardiac diseases.
Introduction
Cardiac diseases constitute a global public health challenge and a substantial cause of morbidity and mortality (1). Around 17.8 million people died of cardiac diseases across the world in 2017 that corresponds to 35.6 million years lived with disability and 330 million years of life lost (2, 3). Economic loss resulting from debilitating and mortal outcomes of various cardiac diseases has resulted into billions of dollars spent for healthcare and reduced work productivity (4). Although the progress in medical treatment has resulted into a reduction in the rate of mortality resulting from different cardiac diseases, these are still the most important cause of death worldwide (5).
The United Nations in 2011 set out an aspiring plan to conclusively reduce the effect of non-communicable diseases. In addition to pharmacological treatment, investigations exploring the effects of complimentary therapies on overall management of cardiac diseases are getting equal importance. There is a growing body of evidence that supports that teams associated with rehabilitation of patients with cardiac diseases are exploring more and more non-traditional methods of interventions like mind-body interventions, dance and hydrotherapy, and music (6–8). Yoga can be defined as a holistic approach to mind body interaction and is an amalgamation of various physical postures, respiratory training, and meditation practices. The word “yoga” is derived from a Sanskrit word that is metaphorically described as the association of inner self with the universe with a main purpose to achieve consonance between the mind, body, and soul. Its eventual aim is to achieve salvation of the soul (9). Yoga also incorporates modifications in lifestyle habits such as diet control and abstention from smoking and alcohol (10). Various research studies in recent past have supported the fact that yogic interventions have numerous physical and psychological health benefits by downregulating the hypothalamus-pituitary-adrenal axis and the sympathetic component of the autonomic nervous system. Various reported benefits of yoga include reduction in blood pressure, enhanced dominance of the parasympathetic nervous system over the sympathetic nervous system, normalization of endocrinal function and gastrointestinal function, improved musculoskeletal fitness and posture, enhanced energy levels, normalization of body weight, better sleep and immunity, reduced pain, and better quality of life, whereas psychological benefits associated with yoga include enhanced mood, feeling of subjective well-being and self-acceptance, and reduced anxiety and depression (11, 12). The literature also reports improved biochemical profile in terms of antioxidant effects of yoga like reduced cholesterol, triglycerides, and glucose levels, increased lymphocyte count, and many more (13, 14).
Rationale
The last few years have seen increased attention being paid to yogic interventions by the medical community for management of various medical conditions. This has happened because of increased acknowledgment and comprehension related to yoga. Effects of yogic intervention on modifying risk factors related to cardiac diseases and rehabilitation are continuously gaining significant importance (15). Moreover there is enough evidence to prove that yogic interventions are safe, effective, and can be used as compliment to pharmacological management and have also been found successful for treating various conditions such as sleep disorders, chronic pain syndrome, hypertension, post-menopausal syndrome, and diseases related to the cardiovascular system (5, 16). Evidence also supports the role of yoga in modifying various risk factors associated with cardiovascular diseases (CVDs) such as diabetes, obesity, psychological stress, and hypertension (17–21). The positive results underpin the inclusion of mind-body interventions in management of patients with cardiac diseases.
At present, evidence-based research studies on the efficacy of mind-body interventions like yoga therapy in patients with different cardiac diseases are limited and conflicting. Most of the research studies have focused on comparative studies on different types of training. Reviews on articles conducted previously have found yogic interventions feasible in patients with various diagnosed cardiovascular diseases. Previous reviews and meta-analysis have recommended a requirement of high-quality studies related to yogic interventions for patients with various cardiac diseases. This study extends a previously conducted study with focus on randomized controlled trials incorporating the impact of yoga interventions on anthropometric dimensions and different physiological parameters like mental health and cardiovascular variables, and psychosocial parameters like quality of life, stress, anxiety, and depression in patients diagnosed with cardiac diseases.
Objective
The objective of this study is to conduct a systematic review and meta-analysis of the effects of yogic interventions on patients diagnosed with cardiac diseases focusing on physical and psychosocial outcomes.
Methods
Eligibility Criteria
Studies fulfilling the following eligibility criteria were included:
(a) Randomized control trial as the study design. (b) Full-text articles written in English, diagnosed cardiac condition, yogic intervention compared to or in addition to standard treatment (routine pharmacological treatment/cardiac rehabilitation/educational sessions/physiotherapy based lifestyle modifications) or no treatment at all in adult patients with cardiac diseases. (c) Full-text studies that examined physical outcomes including cardiovascular-related health parameters, anthropometric measurements, inflammatory markers, antioxidant status, and hemodynamic parameters, and psychosocial outcomes like anxiety, stress, and depression.
Studies that were excluded were those that included yoga as part of a mind-body intervention program, review articles, or meta-analysis, abstracts, opinion articles or letter to editors, and interventions other than randomized control trials.
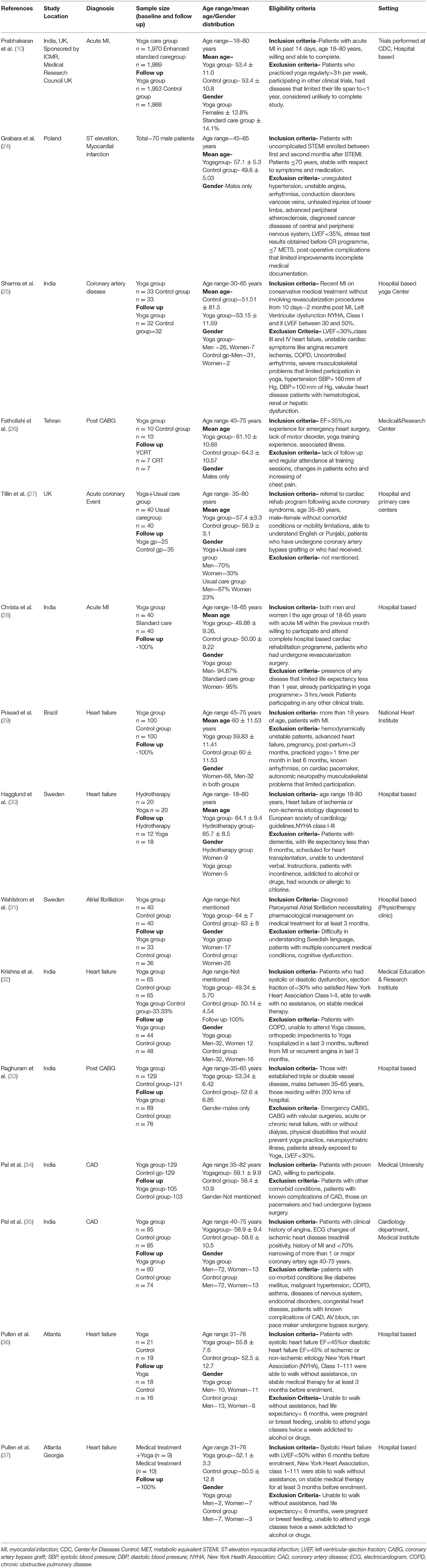
The PRISMA flow diagram of study is presented in Figure 1.
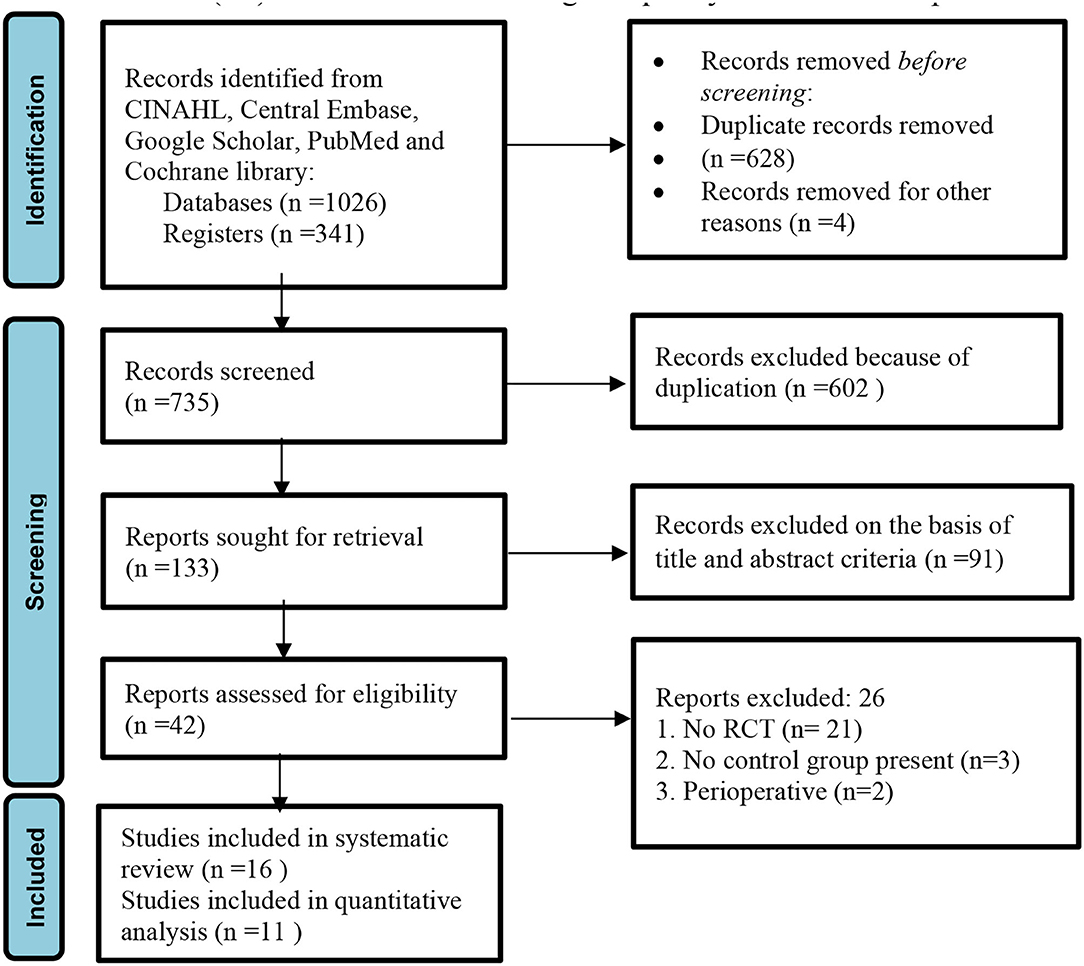
Figure 1. PRISMA flow diagram of the study (22).
Information Sources
We conducted an electronic search of literature published in last the 15 years, i.e., from 2006 to May 2021 through five databases, viz., CINAHL, Central Embase, Google Scholar, PubMed, and Cochrane Library. Randomized controlled trials (RCTs) on yogic interventions compared with usual care or non-pharmacological treatment in patients diagnosed with cardiovascular diseases were included.
Strategy for Literature Search
To optimize the search strategy and to make the search more precise, MeSH terms and Boolean operators were used in library databases. The search strategy used was: [“yoga OR yog OR yogic practices OR yogic interventions] AND [cardiac diseases OR cardiovascular diseases OR cardiac failure OR heart failure OR heart attack OR hypertensive heart disease OR atrial fibrillation OR ischemic heart disease OR valvular heart disease OR cardiomyopathy”]. Potential randomized controlled trials that met the inclusion criteria of the study were also screened by searching references of selected articles. The preferred reporting items for systematic review and meta-analysis protocols (PRISMA) statement was used to develop and report systematic a review and meta-analysis protocol (23).
Data Extraction and Management
Data were independently extracted by two reviewers, SK and PA, on characteristics of study location, year of study, participants, study duration, sample size, male-female ratio, inclusion and exclusion criteria, details of intervention given to experimental groups and control groups, duration of study, outcome measures, and results of study. The data were rechecked by a third reviewer, SP, and all disagreements and discrepancies were resolved by consensus.
Effect Measures
Outcome measures were blood pressure, lipid profile, and psychosocial measures. The Cochrane collaboration tool was used to assess bias risk. For analyzing maximum treatment effect, post-intervention mean scores and standard deviations related to pre-defined outcome measures were used in order to pool the data. In studies where different scales were used to measure the outcome, effect size (standardized mean difference, d) was calculated.
Risk of Bias in Individual Studies
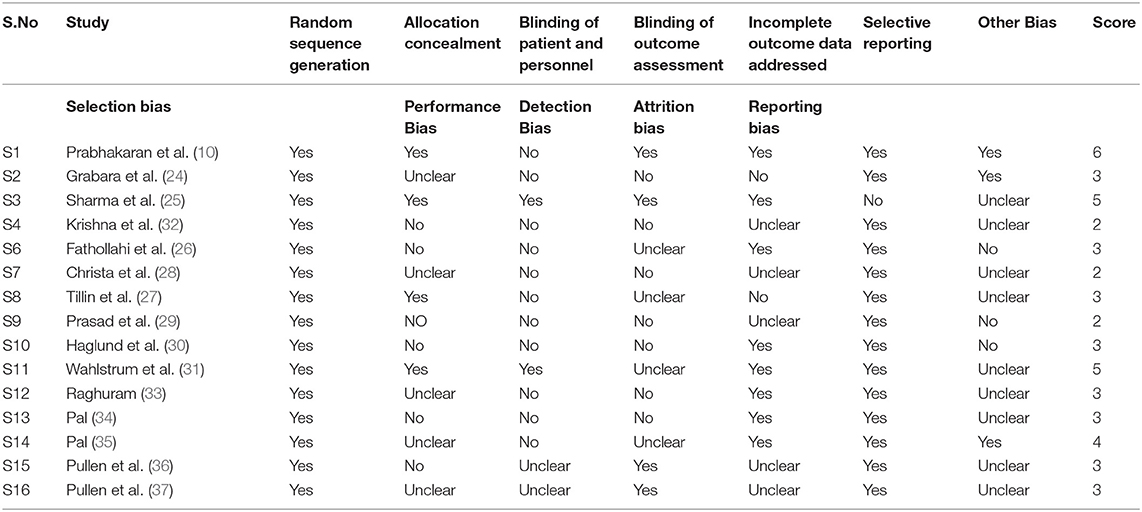
Risk of bias in individual studies and methodological quality assessment was performed by the 2 independent reviewers, SK and PA, with more than 15 years of experience in empirical research. The Cochrane collaboration tool was used to assess bias risk in randomized control trials in selected articles. The tool assesses bias risk on the basis of 7 domains. Judgment regarding bias was categorized into 3: (a) low risk, (b) high risk, and (c) unclear risk. PRISMA guidelines were used for reporting the results of systematic reviews and meta-analysis. Any disagreement between the 2 reviewers regarding appraisal recommendation was resolved by another reviewer (VJ). The results of methodological quality assessment are presented in Table 2.
Data Synthesis and Meta-Analysis
Post intervention mean score and standard deviation of outcome measures were used for pooling the data. Effect size (standardized mean difference, d), whenever required, was calculated by subtracting the mean of post intervention score of the control groups from that of the yoga group. The result was divided by pooled standard deviations of both groups. An effect size of.2–0.5, 0.5–0.8 and more than 0.8 is considered small, moderate, and large, respectively (Cohen). A positive value of SMD indicates beneficial effects of yoga in comparison to control and vice versa. Also, in three studies, median and range were reported instead of post intervention mean score/standard deviation and mean differences. Hogg's formula was used in these cases to calculate post intervention mean scores and standard deviation (38, 39).
The Meta-Essentials software was used for summarization of data for all the outcome measures provided that at least two studies were available on a particular outcome. Random-effects models were used to calculate summary estimate with 95% confidence interval. A random-effects model is based on the assumption that selected studies were drawn from a population of studies that are systematically different from each other. Forest plots were constructed to graphically display the results. Zero specifies no heterogeneity, 25% is low, 50% is moderate, and 75% is high heterogeneity. A value of more than 0.05 in Q statistic indicated variance in studies and not between studies. An analysis was conducted on all the studies with exclusion of outliers.
Results
Study Selection Search Results
In the initial literature search, 1,367 titles emerged as relevant studies. After removal of duplicates and studies not the fulfilling eligibility criteria, a total of 42 unique full-text records were identified. A total of 15 RCTs were included in the qualitative analysis. Four RCTs reported different outcome measures and were excluded from the quantitative analysis (meta-analysis). Eleven RCTs with sufficient data were included for the meta-analysis (Figure 1).
Study Characteristics
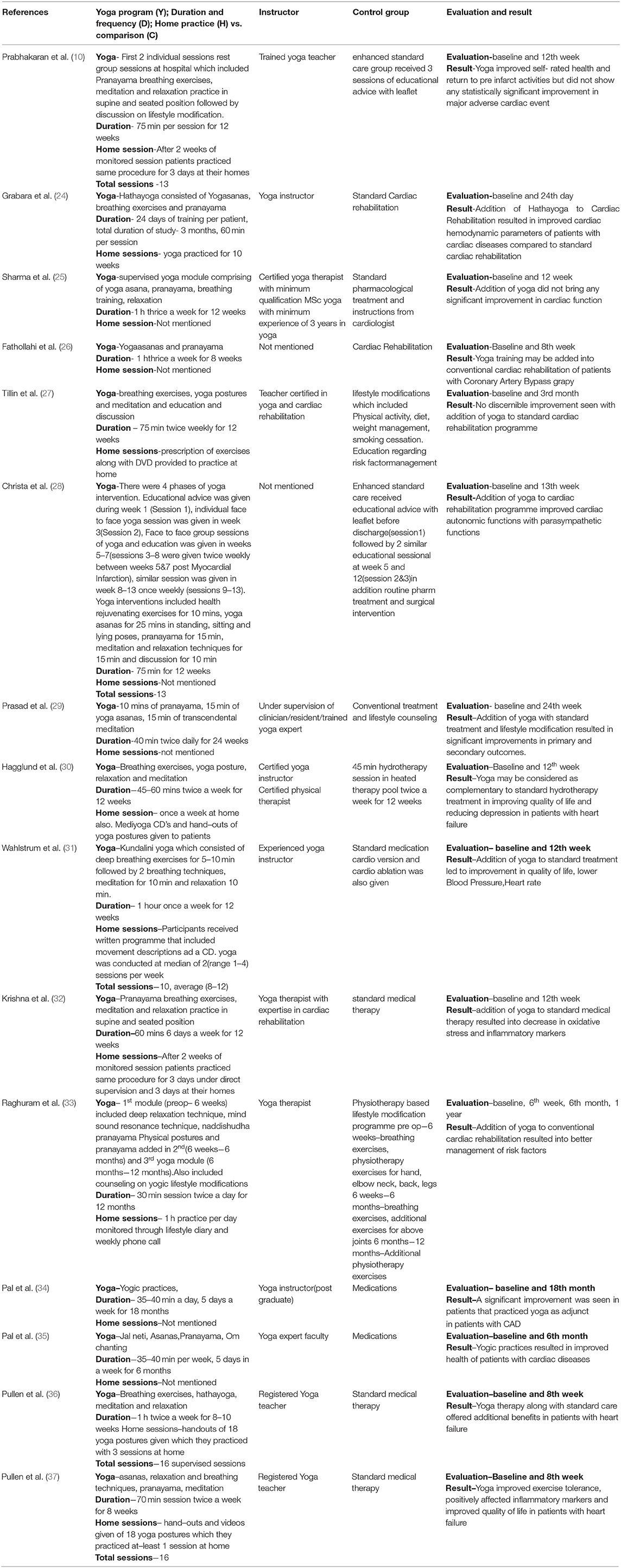
Out of the total 15 randomized controlled trials included in this review, six were conducted in India, places of 16 RCT are mentioned, two in Atlanta, two in Sweden, one each in Brazil, the United Kingdom, Tehran, and Poland; one was a collaboration between India and the United Kingdom. Five RCTs included patients with heart failure, four with coronary artery disease, three with acute myocardial infarction, and one with atrial fibrillation. Two RCTs were performed on post CABG (coronary artery bypass graft) patients. The study by Fathollahi, Raghuram, and Grabara had male participants only (24, 26, 33), while the study by Pal (34) did not mention about gender. Tillin et al. did not mention about the exclusion criteria of the study (27). Most of the studies mentioned intervention provided to a yoga group by a certified yoga therapist/experienced yoga instructor. The study by Christa et al. and Fathollahi et al. did not mention about the instructor (26, 28). All the trials were conducted either in the hospital (yoga clinic, physiotherapy department) or in a medical institute/university. Details of study population are presented in Table 1. All yoga trials were composed of yogic postures and breathing, training, and relaxation exercises. Duration, frequency of yoga sessions, and length of entire study varied among the trials. Yoga session duration ranged from 30 to75 min, with 16 as maximum total sessions. Yoga length, frequency, and duration varied between the trials. Treatments extended to control groups included standard care in the form of cardiac rehabilitation, pharmacotherapy, educational advice, or lifestyle modification. Baseline measurements were provided in all the RCTs. The time of assessment of outcome measures varied from 24 days, 12 weeks, 13 weeks, 24 weeks, 1 year, to 5years. Studies by Pal et al. did not describe about home sessions to the patients (34, 35).
Table 2 presents a description of interventions provided to both groups, time of evaluation, and results obtained.
The number of dropouts varied in all the studies. The highest number of dropouts was reported in the study of Raghuram (40 from the intervention group and 45 from the control group) followed by the study of Prabhakaran (29 from the intervention group and 19 from the control group), Pal (34) (24 from the intervention group and 26 from the control group), Krishna (21 from the intervention group and 17 from the control group), Tillin (11 from the intervention group and five from the control group), Wahlstrum (seven from the intervention group and four from the control group), Hagglund (two from the intervention group and 8 from the control group), Prasad (two from the intervention group and six from the control group) Fathollahi (two from the intervention group and three from the control group), Pullen (three from the intervention group and 8 from the control group), and Sharma (one from the intervention group and 1 from the control group).
The main barriers for not completing the study include unwillingness to continue with yoga classes, participants frequently citing ill health as a reason, return to work, family issues, long travel distance to the hospital, muscular skeletal symptoms, cognitive decline, and constraints in time to come for follow-up.
Risk of Bias Assessment
Random sequence generation was conducted on all the 15 trials. Only four trials reported allocation concealment, while it was unclear in five trials reporting unclear risk of selection bias. Eleven trials did not report on blinding of patient and personnel and were therefore rated as high risk of performance bias. Seven trials did not report on blinding of outcome assessors, and four trials reported unclear risk of detection bias. Seven trials reported loss to follow-up, and four trials that were unclear about loss to follow-up were rated as unclear risk of attrition bias. The 15 trials reported all the outcomes and were assessed as low risk of selective reporting bias. A detailed description of the risk of bias assessment is presented in Table 3.
Results of Syntheses and Intervention Outcomes
Physiological Outcomes
Resting Blood Pressure
Eight trials comprising 1,035 participants reported resting blood pressure. The results show that yogic interventions resulted in significant reduction in systolic blood pressure and diastolic blood pressure. Effect sizes for SBP and DBP depicted a similar heterogeneity pattern. The pooled results depict a low but statistically significant effect on SBP (Cohen d = 0.46; 95% CI.08–0.84; I2 = 81.86%) and a medium effect on DBP (Cohen d = 0.56; 95% CI.13–0.99; I2 = 84.84%) (Figure 2).
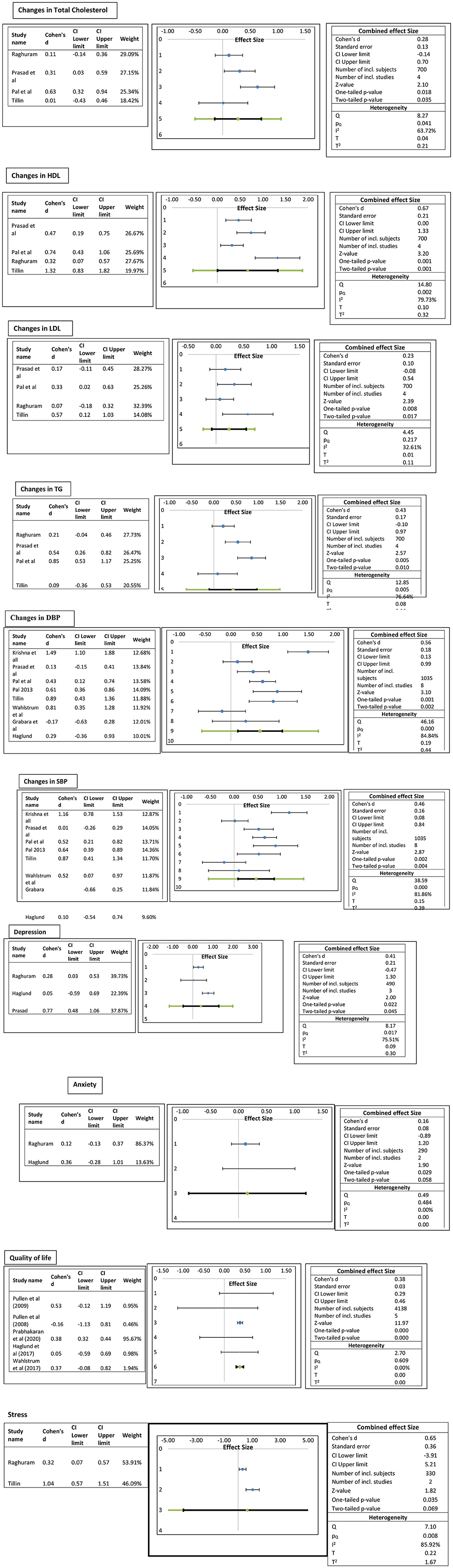
Figure 2. Forest plots of the effect of yogic interventions on physiological and psychosocial parameters.
Lipid Profile
Four trials comprising 700 participants reported lipid profiles. The pooled results depict a medium statistically significant increase in HDL in the yoga group compared to the control group (Cohen d = 0.67; 95% CI to 1.33; I2 79.7%) and a low effect on LDL (Cohen d = 0.23; 95% CI −0.08–0.54; I232.61%). Similarly, a low effect on total cholesterol (Cohen d = 0.28; 95% CI.14–0.7; I2 63.72%) and triglycerides (Cohen d = 0.43; 95% CI −0.10 to.97; I2 76.64%) was observed (Figure 2).
Psychosocial Outcomes
It was observed that overall yoga had statistically significant promising results in psychosocial outcomes. Quality of life was assessed among 4,138 participants in five trials with three different questionnaires [Minnesota Living with Heart Failure Questionnaire, MLWHFQ], The Kansas City Cardiomyopathy Questionnaire (KCCQ), and EuroQol-5 Dimension (EQ-5D)]. The pooled effect sizes show medium statistically significant (Cohen d = 0.38; 95% CI 0.29 −0.46 to 0; I2 0%) QoL score. It was observed that the results of the study by Prabhakaran et al. (10) were influenced by large sample size. Stress was measured in two studies with the same instrument, Perceived Stress Scale. The pooled results depict a medium statistically significant effect on stress scores (Cohen d = 0.65; 95% CI −3.91 to 5.21; I2 85.92%). Anxiety was assessed with “The Hospital Anxiety and Depression Scale (HADS)” in two studies and depression in three studies with two scales, HADS and “Beck's Depression Inventory.” The pooled results showed a low statistically significant effect size of d = 0.16 (95% CI −0.89 to 1.2, I2 0%) on stress and a medium statistically significant effect size of d =0.41 (95% CI −0.47–1.3, I2 75.5%) (Figure 2). Description of physical and psychological outcomes of selected studies are shown in Table 4.
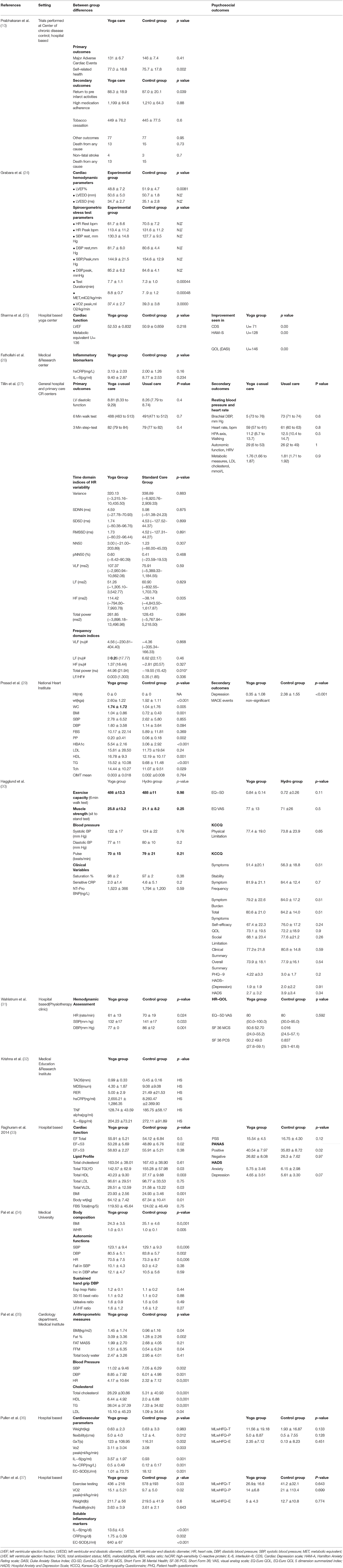
Table 4. Description of physical and psychosocial outcomes and between group differences (yoga vs. control).
Discussion
This systematic review and meta-analysis enrolled15 RCTs examining the role of yogic interventions in managing physiological and psychosocial parameters in patients diagnosed with cardiac diseases. The heterogenous but promising results indicate significant improvements in several psychosocial outcomes including quality of life, stress and depression, and low to moderate effects on physiological parameters. The analysis reported evidence of reduction in systolic and diastolic blood pressures along with reduction in total cholesterol, low-density lipoproteins, and triglyceride levels, and increase in high-density lipoproteins levels. The results of this systematic review are in line with studies and previous reviews reporting the role of yoga in improving psychosocial and physiological outcomes in cardiac patients (5, 40). The literature reveals positive physiological effects on cardiac parameters like heart rate, lipid profile, blood pressure, respiration rate, and oxygen consumption with yogic interventions (21, 32, 41–44). Sivasankaran et al. discussed about favorable changes in endothelial-dependent vasodilatation in cardiac patients brought about by yoga and meditation (45). Yoga is known to lower heart rate and blood pressure under cardiac conditions by modulating the autonomic nervous system. Yoga and meditation have also been shown to raise melatonin, aminobutyric acid, and a variety of other neurotransmitters. Importantly, a drop in stress markers like 8-hydroxydeoxyguanosine and an increase in endorphin levels with yoga clearly imply that it can help people cope with stress (44, 45).
Many studies have evidenced the relationship between psychosocial factors and vascular functions (46, 47). Psychosocial variables like stress, depression, and anxiety are associated with cardiovascular diseases in different stages, i.e., causing arteriosclerosis and severe cardiac symptoms that may lead to development of chronic diseases (20, 48, 49). All the research studies showed that cardiac patients engage in yoga practices because of several reasons. First, the interventions are easier to learn and motivate patients to play a more active role in their own treatment. Second, after proper learning sessions, most of the exercises can be performed at home without any external assistance. Furthermore, the exercises are relatively cost-effective and involve minimal physical and emotional risks (50, 51). Despite requiring commitment and time adherence, yogic interventions are progressively gaining popularity (52).
Yoga programs have also been demonstrated to enhance physical function measures like balance, strength, and endurance, as well as symptoms in cardiac patients. Therefore, a growing body of research supports yoga's beneficial neurohumoral benefits such as lower serum cortisol, catecholamine, and aldosterone levels.
Strengths and Limitations
The large-scale search conducted on different databases, inclusion of exclusive randomized controlled trials, and methodological quality assessment conducted the meta-analysis are the strong points of the study. Studies that had only yogic interventions were included, thus making comparison of studies feasible. Studies that included yoga as part of mind-body practices that could have brought variability between the results obtained were not included.
This meta-analysis generates evidence for the effectiveness of yoga intervention on lipid profile, blood pressure, and psychosocial outcomes in patients diagnosed with cardiac diseases. Sixteen RCTs examining the role of yogic interventions in managing physiological and psychosocial parameters in patients diagnosed with cardiac diseases were enrolled. Heterogeneity was high for most of the variables. Second, variations in types of yoga in the included articles and differences between yoga interventions, outcomes measured (physical and psychological), and variations in control groups, again possibly resulting in different effects on physiological and psychological parameters in patients with cardiac diseases, also led to heterogeneity. Therefore, high heterogeneity brought the need for more large scale high-quality RCTs to affirm the findings. Third, the included articles were limited to those published in the English language only. Some articles published in other languages might have been missed. Finally, more articles with high-level evidence such as randomized controlled trials using a consistent control group should be further conducted to assess the efficacy of yoga in patients with cardiac diseases. Therefore, in this study, publication bias cannot be ruled out because of assessment of heterogeneity and small number of studies.
Conclusion
This systematic review and meta-analysis showed strong evidence of the effectiveness of yogic interventions in the lipid profile, blood pressure, depression, stress, anxiety, and quality of life of patients diagnosed with cardiac diseases. However, because of relatively small sample sizes of some of the trials, the results of the current review must be interpreted with caution. Randomized controlled trials with large sample sizes and rigorous study designs are required to improve our understanding of the physiological and psychosocial effects of yogic interventions on cardiac parameters. Furthermore, in the future, RCTs should address the optimal duration and frequency of yogic interventions in specific cardiac diseases so that their generalizability can be enhanced.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
Conception and design of the work and drafting the work: SK, MM, PA, and RS. Substantial contributions to the acquisition of data for the work: MAlq, SP, VJ, FA, MS, and AS. Substantial contributions to the analysis of data for the work: MS, EM, MAlz, and AA. Substantial contributions to the interpretation of data for the work, final approval of the version to be published, and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: SK, MM, GS, PA, SA, HA, and SS. Revising the draft of the work critically for important intellectual content: ML, SK, AS, GS, and SA. All authors contributed to the article and approved the submitted version.
Funding
The authors are grateful to the Deanship of Scientific Research, Majmaah University, for funding through Deanship of Scientific Research vide Project No. RGP-2019-35. The authors are also thankful to AlMareefa and Saudi Electronic University, Riyadh, Saudi Arabia, for providing support to do this research.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bovet P, Paccaud P. Cardiovascular disease and the changing face of global public health: a focus on low and middle income countries. Public Health Rev. (2011) 33:397–415. doi: 10.1007/BF03391643
2. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. (2017) 70:1–25. doi: 10.1016/j.jacc.2017.04.052
3. Ali S, Destaw Z, Misganaw A, Worku A, Negash L, Bekele A, et al. The burden of injuries in Ethiopia from 1990-2017: evidence from the global burden of disease study. Injury epidemiology. (2020) 7:1–11. doi: 10.1186/s40621-020-00292-9
4. Gaziano TA. Economic burden and the cost-effectiveness of treatment of cardiovascular diseases in Africa. Heart. (2008) 94:140–4. doi: 10.1136/hrt.2007.128785
5. Younge JO, Gotink RA, Baena CP, Roos-Hesselink JW, Hunink MM. Mind–body practices for patients with cardiac disease: a systematic review and meta-analysis. Eur J Prev Cardiol. (2015) 22:1385–98. doi: 10.1177/2047487314549927
6. Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, Woo P. Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis. Health Technol Assess Rep. (2005) 9:iii-v. doi: 10.3310/hta9390
7. Gomes Neto M, Menezes MA, Carvalho VO. Dance therapy in patients with chronic heart failure: a systematic review and a meta-analysis. Clin Rehabil. (2014) 28:1172–9. doi: 10.1177/0269215514534089
8. Kaltsatou AC, Kouidi EI, Anifanti MA, Douka SI, Deligiannis AP. Functional and psychosocial effects of either a traditional dancing or a formal exercising training program in patients with chronic heart failure: a comparative randomized controlled study, Clin. Rehabil. (2014) 28:128–38. doi: 10.1177/0269215513492988
9. Guidetti S, Nielsen KT, Von Bülow C, Pilegaard MS, Klokker L, Wæhrens EE. Evaluation of an intervention programme addressing ability to perform activities of daily living among persons with chronic conditions: study protocol for a feasibility trial (ABLE). BMJ open. 2018 8:e020812. doi: 10.1136/bmjopen-2017-020812
10. Prabhakaran D, Chandrasekaran AM, Singh K, Mohan B, Chattopadhyay K, Chadha DS, et al. Yoga-based cardiac rehabilitation after acute myocardial infarction: a randomized trial. J Am Coll Cardiol. (2020) 75:1551–61. doi: 10.1016/j.jacc.2020.01.050
11. Ross ST. The health benefits of yoga and exercise: a review of comparison studies. JACM. (2010) 16:3–12. doi: 10.1089/acm.2009.0044
12. Riley KE, Park CL. How does yoga reduce stress? A systematic review of mechanisms of change and guide to future inquiry. Health Psychol Rev. (2015) 9:379–96. doi: 10.1080/17437199.2014.981778
13. Gokal R, Shillito L, Maharaj SR. Positive impact of yoga and pranayam on obesity, hypertension, blood sugar, and cholesterol: a pilot assessment, JACM.13 (2007) 1056-8. doi: 10.1089/acm.2007.0679
14. Raju MVR. Sahay B, Murthy K. Impact of pranayama and yoga on lipid profile in normal healthy volunteers. J Exerc Physiol. (2006) 9. doi: 10.5455/njppp.2022.12.11413202126112021
15. Jayasinghe SR. Yoga in cardiac health (a review). Eur J Cardiovasc Prev Rehabil. (2004) 11:369–75. doi: 10.1097/00149831-200410000-00002
16. Chiesa A, Serretti A, A systematic review of neurobiological and clinical features of mindfulness meditations. Psychol Med. (2010) 40:1239. doi: 10.1017/S0033291709991747
17. Chimkode SM, Kumaran SD, Kanhere V, Shivanna R. Effect of yoga on blood glucose levels in patients with type 2 diabetes mellitus. JCDR. (2015) 9:CC01. doi: 10.7860/JCDR/2015/12666.5744
18. Sreedevi A, Gopalakrishnan UA, Ramaiyer SK, Kamalamma L, A. randomized controlled trial of the effect of yoga and peer support on glycaemic outcomes in women with type 2 diabetes mellitus: a feasibility study. BMC Complement Altern Med. (2017) 17:1–8. doi: 10.1186/s12906-017-1574-x
19. Gadham J, Sajja S, Rooha V. Effect of yoga on obesity, hypertension and lipid profile. Int J Res Med Sci. (2015) 3:1061–5. doi: 10.5455/2320-6012.ijrms20150506
20. Lakkireddy D, Atkins D, Pillarisetti J, Ryschon K, Bommana S, Drisko J, et al. Effect of yoga on arrhythmia burden, anxiety, depression, and quality of life in paroxysmal atrial fibrillation: the YOGA My Heart Study. J Am Coll Cardiol. (2013) 61:1177–82. doi: 10.1016/j.jacc.2012.11.060
21. Guddeti RR, Dang G, Williams MA, Alla VM. Role of yoga in cardiac disease and rehabilitation. J Cardiopulm Rehabil Prev. (2019) 39:146–52. doi: 10.1097/HCR.0000000000000372
22. Akl SEB. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372. doi: 10.1136/bmj.n71
23. Shekelle LAS. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350. (2016) 354:i4086. doi: 10.1136/bmj.i4086
24. Grabara M, Nowak Z, Nowak A. Effects of Hatha Yoga on cardiac hemodynamic parameters and physical capacity in cardiac rehabilitation patients. J Cardiopulm Rehabil Prev. (2020) 40:263–7. doi: 10.1097/HCR.0000000000000503
25. Sharma KS, Pailoor S, Choudhary NR, Bhat P, Shrestha S. Integrated yoga practice in cardiac rehabilitation program: a randomized control trial. JACM. (2020) 26:918–27. doi: 10.1089/acm.2019.0250
26. Fathollahi FG. H. Nikbakht, S Lotfian, A Nikpajouh, The effects of 8 weeks yoga and cardiac rehabilitation training on interlukin-6 and high sensitivity C-reaction proteins after coronary artery bypass surgery: a randomized controlled Trial. JCRPS. (2020) 9:0. doi: 10.5812/jcrps.98289
27. Tillin T, Tuson C, Sowa B, Chattopadhyay K, Sattar N, Welsh P, et al. Yoga and Cardiovascular Health Trial (YACHT): a UK-based randomised mechanistic study of a yoga intervention plus usual care versus usual care alone following an acute coronary event. BMJ Open. (2019) 9:e030119. doi: 10.1136/bmjopen-2019-030119
28. Christa E, Srivastava P, Chandran DS, Jaryal AK, Yadav RK, Roy A, et al. Effect of Yoga-based cardiac rehabilitation on heart rate variability: randomized controlled trial in patients post-MI. Int J Yoga Therap. (2019) 29:43–50. doi: 10.17761/2019-00019
29. Prasad A, Bhardwaj S, Dwivedi S, Arora Y, Sharma V. Effect of Yoga in post-myocardial infarction cases. JSIR. (2020) 9:63–8. doi: 10.31254/jsir.2020.9205
30. Hägglund E, Hagerman I, Dencker K, Strömberg A. Effects of yoga versus hydrotherapy training on health-related quality of life and exercise capacity in patients with heart failure: a randomized controlled study, Eur. J Cardiovasc Nurs. (2017) 16:381–9. doi: 10.1177/1474515117690297
31. Wahlstrom M, Rydell Karlsson M, Medin J, Frykman V. Effects of yoga in patients with paroxysmal atrial fibrillation–a randomized controlled study. Eur J Cardiovasc Nurs. (2017) 16:57–63. doi: 10.1177/1474515116637734
32. Krishna BH, Pal P, Pal G, Balachander J, Jayasettiaseelon E, Sreekanth Y, et al. Effect of yoga therapy on heart rate, blood pressure and cardiac autonomic function in heart failure. JCDR. (2014) 8:14. doi: 10.7860/JCDR/2014/7844.3983
33. Raghuram N, Parachuri VR, Swarnagowri M, Babu S, Chaku R, Kulkarni R, et al. Yoga based cardiac rehabilitation after coronary artery bypass surgery: One-year results on LVEF, lipid profile and psychological states–a randomized controlled study. Indian Heart J. (2014) 66:490–502. doi: 10.1016/j.ihj.2014.08.007
34. Pal A, Srivastava N, Narain VS, Agrawal GG, Rani M. Effect of yogic intervention on the autonomic nervous system in the patients with coronary artery disease: a randomized controlled trial. EMHJ-Eastern Mediterranean Health Journal. (2013) 19 452-8. doi: 10.26719/2013.19.5.452
35. Pal A, Srivastava N, Tiwari S, Verma N, Narain V, Agrawal G, et al. Effect of yogic practices on lipid profile and body fat composition in patients of coronary artery disease, Complement. Ther Med. (2011) 19:122–7. doi: 10.1016/j.ctim.2011.05.001
36. Pullen PR, Thompson WR, Benardot D, Brandon LJ, Mehta PK, Rifai L, et al. Benefits of yoga for African American heart failure patients. Med Sci Sports Exerc. (2010) 42:651–7. doi: 10.1249/MSS.0b013e3181bf24c4
37. Pullen PR, Nagamia SH, Mehta PK, Thompson WR, Benardot D, Hammoud R, et al. Effects of yoga on inflammation and exercise capacity in patients with chronic heart failure, J. Card Fail. (2008) 14:407–13. doi: 10.1016/j.cardfail.2007.12.007
38. Hogg RV, McKean JW, Craig AT. Introduction to mathematical statistics, Pearson Education. Upper Saddle River, NJ. (2005), p. 407–13. Available online at: https://faculty.ksu.edu.sa/sites/default/files/hogg_craig_-_introduction_to_mathematical_statistics_4th_edition1.pdf
39. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. (2005) 5:1–10. doi: 10.1186/1471-2288-5-13
40. Li J, Gao X, Hao X, Kantas D, Mohamed EA, Zheng X, et al. Yoga for secondary prevention of coronary heart disease: A systematic review and meta-analysis. Complement Ther Med. (2021) 57:102643. doi: 10.1016/j.ctim.2020.102643
41. Wolff M, Sundquist K, Lönn SL, Midlöv P. Impact of yoga on blood pressure and quality of life in patients with hypertension–a controlled trial in primary care, matched for systolic blood pressure. BMC Cardiovasc Disord. (2013) 13:1–9. doi: 10.1186/1471-2261-13-111
42. Wolff M, Rogers K, Erdal B, Chalmers J, Sundquist K, Midlöv P. Impact of a short home-based yoga programme on blood pressure in patients with hypertension: a randomized controlled trial in primary care. J Hum Hypertens. (2016) 30:599–605. doi: 10.1038/jhh.2015.123
43. Vinay A, Venkatesh D, Ambarish V. Impact of short-term practice of yoga on heart rate variability. Int J Yoga. (2016) 9:62. doi: 10.4103/0973-6131.171714
44. Yeh GY, Davis RB, Phillips RS. Use of complementary therapies in patients with cardiovascular disease. AJC. (2006) 98:673–80. doi: 10.1016/j.amjcard.2006.03.051
45. Sivasankaran S, Pollard-Quintner S, Sachdeva R, J. Pugeda, SM Hoq, SW Zarich. The effect of a six-week program of yoga and meditation on brachial artery reactivity: do psychosocial interventions affect vascular tone? Clin Cardiol. (2006) 29:393–8. doi: 10.1002/clc.4960290905
46. Kop WJ, Krantz DS, Howell RH, Ferguson MA, Papademetriou V, Lu D, et al. Effects of mental stress on coronary epicardial vasomotion and flow velocity in coronary artery disease: relationship with hemodynamic stress responses. J Am Coll Cardiol. (2001) 37:1359–66. doi: 10.1016/S0735-1097(01)01136-6
47. R. von Kanel. Mills PJ, Fainman C Dimsdale JE. Effects of psychological stress and psychiatric disorders on blood coagulation and fibrinolysis: a biobehavioral pathway to coronary artery disease. Psychosom Med. (2001) 63:531–44. doi: 10.1097/00006842-200107000-00003
48. Thurston RC, Rewak M, Kubzansky LD. An anxious heart: anxiety and the onset of cardiovascular diseases. Prog Cardiovasc Dis. (2013) 55:524–37. doi: 10.1016/j.pcad.2013.03.007
49. Ghiadoni L, Donald AE, Cropley M, Mullen MJ, Oakley G, Taylor M, et al. Mental stress induces transient endothelial dysfunction in humans. Circulation. (2000) 102:2473–8. doi: 10.1161/01.CIR.102.20.2473
50. D.S. Sobel. Mind matters, money matters: the cost-effectiveness of mind/body medicine. JAMA. (2000) 284:1705–1705. doi: 10.1001/jama.284.13.1705-JMS1004-3-1
51. Friedman R, Sobel D, Myers P, Caudill M, Benson H. Behavioral medicine, clinical health psychology, and cost offset. Health Psychol. (1995) 14:509. doi: 10.1037/0278-6133.14.6.509
Keywords: cardiac diseases, yoga, cardiovascular outcomes, psychosocial outcomes, review, meta-analysis
Citation: Kalra S, Miraj M, Ajmera P, Shaik RA, Seyam MK, Shawky GM, Alasiry SM, Mohamed EH, Alasiri HM, Alzhrani M, Alanazi A, Alqahtani M, Shaikh AR, Al-Otaibi ML, Saleem S, Pal S, Jain V and Ahmad F (2022) Effects of Yogic Interventions on Patients Diagnosed With Cardiac Diseases. A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 9:942740. doi: 10.3389/fcvm.2022.942740
Received: 12 May 2022; Accepted: 20 June 2022;
Published: 04 August 2022.
Edited by:
Jinfeng Xu, The University of Hong Kong, Hong Kong SAR, ChinaReviewed by:
Surabhi Gautam, All India Institute of Medical Sciences, IndiaBidita Khandelwal, Sikkim Manipal University, India
Raj Kumar Yadav, All India Institute of Medical Sciences, India
Chandra Nanthakumar, HELP University, Malaysia
Vijay Singh, Manipal Academy of Higher Education, India
Copyright © 2022 Kalra, Miraj, Ajmera, Shaik, Seyam, Shawky, Alasiry, Mohamed, Alasiri, Alzhrani, Alanazi, Alqahtani, Shaikh, Al-Otaibi, Saleem, Pal, Jain and Ahmad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammad Miraj, bS5tb2xsYSYjeDAwMDQwO211LmVkdS5zYQ==
 Sheetal Kalra
Sheetal Kalra Mohammad Miraj2*
Mohammad Miraj2* Puneeta Ajmera
Puneeta Ajmera Vineet Jain
Vineet Jain Fuzail Ahmad
Fuzail Ahmad