- College of Medicine and Health, University College Cork, Cork, Ireland
Introduction: Transcatheter aortic valve replacement (TAVR) is a minimally invasive procedure to replace a diseased and faulty aortic valve in patients with severe aortic stenosis. As TAVR gains popularity among lower-risk younger patients with a longer life expectancy; there is a need to investigate the long-term shortcomings and limitations of the procedure for this patient group. One such shortcoming is that commissural alignment of transcatheter heart valves (THV) appears to be random; meaning that the THV neo-commissures can misalign with the native commissures of the aortic valve during deployment or self-expansion.
Objectives: Identify techniques and procedures used to obtain commissural alignment in TAVR. Evaluate the effectiveness of these procedures in terms of the degree of commissural alignment. Analyse the impact of commissural alignment on coronary filling and re-access.
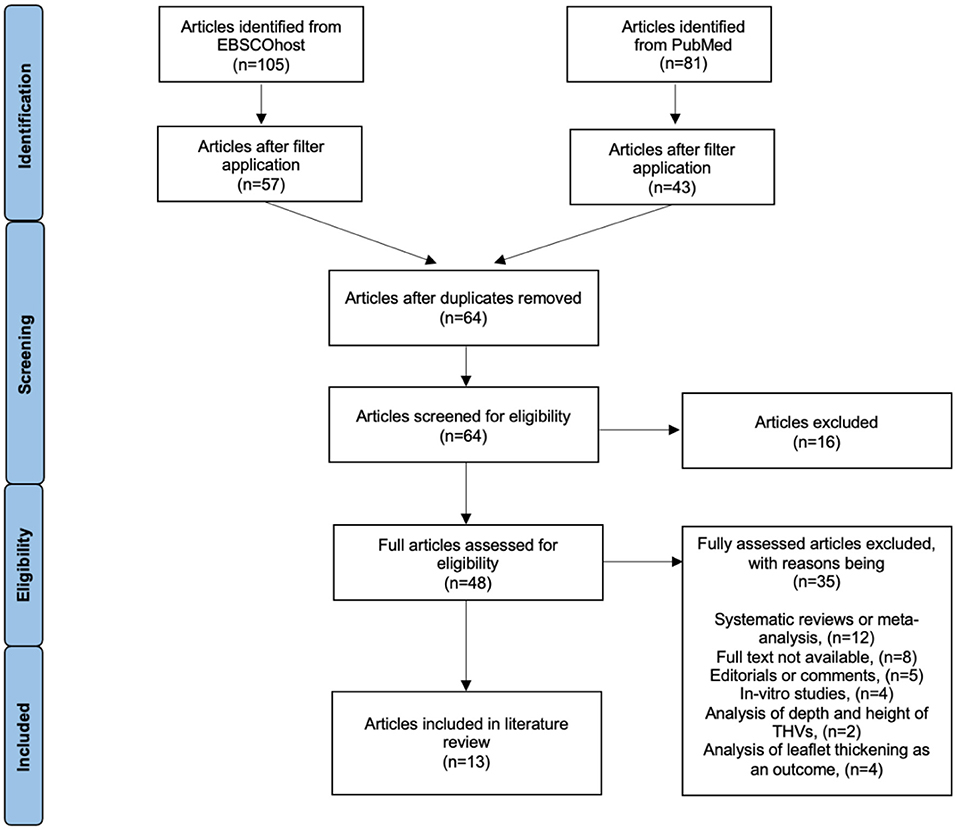
Methods: Two electronic online databases were searched to identify existing literature relevant to the aim and objectives of this review: EBSCOhost and PubMed. After search filters were applied and duplicates removed; a total of 64 articles from both databases were screened against the inclusion/exclusion criteria. This resulted in a total of thirteen articles which met the objectives of this review and thus; were included.
Results: All studies focused on a patient centered approach involving pre-TAVR computed tomography to obtain commissural alignment. Other studies modified this approach and combined techniques. All studies that implemented a technique to reduce commissural misalignment were significantly successful in obtaining commissural alignment when compared to a study in which alignment was random when no technique was implemented. Severe coronary overlapping in commissural aligned heart valves was relatively low compared to severe coronary overlapping when no technique was implemented.
Conclusions: An increase in optimal commissural alignment via introduction of an alignment technique may seem attractive; however; the categorization of commissural alignment is arbitrary and does not accurately reflect real life clinical implications. Further research is needed to determine whether a routine procedure to achieve commissural alignment is necessary in low-risk younger patients undergoing TAVR.
Introduction
Transcatheter aortic valve replacement (TAVR) is a minimally invasive procedure to replace a diseased and faulty aortic valve in patients with severe aortic stenosis (1). Previously; the standard for treatment of aortic stenosis was surgical (open heart) aortic valve replacement (SAVR); and unfortunately patients deemed as high-risk for surgery had limited options for treatment; such as diuretics; which only served as palliative care (2). TAVR was approved by the US Food and Drug Administration for high-risk surgical patients in 2012; allowing such patients an option for long term treatment. More recently; in 2019 it was approved for low-risk patients (2). In a randomized trial; TAVR was concluded to be superior to SAVR at 1 year in terms of deaths related to stroke or rehospitalization at an occurrence of 8.5% for TAVR and 15.1% for SAVR (3, 4). Other randomized trial studies either showed non-inferiority or superiority of TAVR over SAVR (4). The positive response from these trials combined with the fact that as many as 50% of patients with severe aortic stenosis are low risk for surgery has resulted in TAVR becoming the dominant treatment for aortic stenosis (3, 4). As TAVR becomes more popular for lower-risk younger patients with a longer life expectancy; there is a need to investigate the long-term shortcomings and limitations of the procedure for this patient group (3, 5).
One such shortcoming is that commissural alignment of transcatheter heart valves (THV) appears to be random; meaning that the THV neo-commissures can misalign with the native commissures of the aortic valve during deployment or self-expansion (5, 6). In contrast; bioprosthetic valves used in SAVR can be reliably aligned correctly; commissure-to-commissure with the native valve (7). In TAVR; the misalignment may result in the THV neo-commissures partially or fully overlapping the coronary artery ostia (5, 6). As a result; complications can arise if a younger patient needs a percutaneous coronary intervention or redo-TAVR especially since some of them will present with ischemic heart disease later in life (5, 7). With commissural misalignment there is also an increased risk of a leak during diastole because of the unnatural orientation of the THV; this may add undue stress to the THV leaflets (7). Improving commissural alignment in TAVR could possibly make subsequent coronary access and re-do TAVR easier; improve valve durability and enhance coronary blood flow (5, 7). The challenge lies in the fact that aortic anatomy as well as native orientation of the aortic valve differs in every patient; thus a universal approach would not suffice (5). Little attention has been paid to commissural alignment in clinical practice and no official instructions from THV manufacturers exist to achieve commissural alignment (5). Major randomized trials comparing SAVR and TAVR have not considered this limitation either (5).
Aim
The aim of this study is to review published literature on procedures used to obtain commissural alignment in TAVR.
Objectives
1. Identify techniques and procedures used to obtain commissural alignment in TAVR.
2. Evaluate the effectiveness of these procedures in terms of the degree of commissural alignment.
3. Analyse the impact of commissural alignment on coronary filling and re-access.
Methods
Two online databases were searched; including PubMed and EBSCOhost (all databases within EBSCOhost were selected); with a publication date range of 2014 to February 2022. The search terms “Transcatheter Aortic Valve Replacement” [Mesh] and “commissural alignment” were utilized in the search strategy. Search filters were applied to reflect the following: articles published in English available in full text with the subjects as adult humans. One reviewer independently identified articles investigating techniques to achieve commissural alignment in TAVR and screened them against the inclusion/exclusion criteria (see appendix A). A summary of the article selection process is given in Figure 1 according to the PRISMA statement. Reference lists of articles were searched to identify any missed studies and relevant articles were included. The quality of individual studies was assessed using the EBL critical appraisal checklist for quantitative studies and the CASP critical appraisal tool for qualitative studies (see appendix B and C). Each study was approved by its local medical ethics committee.
Results
The data extracted from the articles reviewed are detailed in the summary Table 1 below.
Objective 1: Techniques and procedures used to obtain commissural alignment in TAVR
All studies focused on a patient centered approach to obtain commissural alignment. The most common technique to obtain commissural alignment was a patient-centered approach involving pre-TAVR multidetector or multislice CT to create or calculate a projection of the THV on the native aortic valve which may predict the final valve orientation. This was the core methodology used in nine studies (5–11, 14, 15). A subgroup of these studies modified this technique further and combined the CT imaging with fluoroscopic imaging to identify “markers” on the frame of the THV platforms which could be used to align THV and native commissures (5–8). A few studies modified the approach and used computer simulations using a specialized software (3mensio) to create projections onto CT images in order to minimize coronary artery overlap by predicting the optimal orientation for commissural alignment (6, 7, 14, 15). Another technique used was crimping of the THV on to the delivery catheter suited to the aortic anatomy of the patients based on pre-calculated commissural alignment (6, 13).
Objective 2: The effectiveness of these procedures in terms of the degree of commissural alignment
Many studies used a consistent method of assessing the extent of commissural misalignment (CMA) which involved categorizing the alignment into angle deviations (5–9). The categories were: aligned (angle deviation of <15°); mild CMA (15° to 30°) moderate CMA (30° to 45°) and severe CMA (>45°). Within the low to high quality studies that assessed this aspect after implementation of alignment techniques; very few patients had severe CMA after TAVR; ranging from 0% to 3.3% of their respective populations (5, 7, 9). However; the occurrence of mild and moderate CMA was more variable between the studies (5, 7, 9). The occurrence of correct alignment was high and occurred in more than half the population in all three studies assessing this aspect; ranging from 60% to 75.5% of their respective populations (5, 7, 9) Comparatively; the study by Fuchs et al. in which techniques to achieve commissural alignment were not implemented; the distributions of occurrences of the alignment categories were found to be random in TAVR (8).
Objective 3: Impact of commissural alignment on coronary filling and re-access
Five studies addressed the impact of commissural alignment on coronary blood flow and subsequent intervention in the form of coronary angiography or PCI. In these studies; severe overlap of either the RCA or LCA with the THV commissures was classified if a THV commissure and coronary ostium were 0° to 20° apart (6, 8, 10, 12, 13). The results were variable as severe overlapping occurred in a range of 9% to 16% of the patients in their respective populations within the various studies (8, 10, 12–14). This was still relatively low compared to severe coronary overlapping when no technique to align commissures was implemented; as in the case of the study by Fuchs et al. in which 50% of cases had severe coronary overlapping. One study found that severe CMA did not result in significant pressure drop within coronary arteries when compared to aligned THVs (8). The success rates for CAG or PCI post-TAVR were significantly lower in patients deemed as unfavorable for coronary access (10). When commissural alignment was achieved successfully; coronary intervention was possible in all cases (14).
Discussion
All studies that implemented a technique to reduce commissural misalignment were significantly successful in obtaining commissural alignment when compared to the study by Fuchs et al. in which alignment was random when no technique was implemented. An increase in optimal commissural alignment of 22% (8) to 75.5% (10) via introduction of an alignment technique may seem attractive; however; one major shortcoming of these results was that classification of commissural alignment was artificial and did not reflect the clinical implications of even mild CMA. There was no method to measure differences in clinical implications of CMA in slight adjustments of THV orientation by 1° angle deviation in either direction. Thus; the categorization of commissural alignment was arbitrary and does not accurately reflect real life clinical implications.
Another major shortcoming of the results was that an angle deviation of <15° was considered as commissural alignment; whereas severe coronary artery overlap was defined if a THV commissure and coronary ostium were 0° to 20° apart. This means that if the THV was aligned with the native commissures of the aortic valve at 15°; a slight overlap of even one of the commissures with either coronary artery could be deemed as severe coronary overlap and thus coronary intervention unfeasible. These contradictory classifications between studies open the question for validity and the clinical implications of these studies. Post-TAVR intervention feasibility was hypothetical in most studies and was only carried out in a clinical scenario within a subset of the sample population treated. Thus; the validity and application to real world scenarios on a larger scale is questionable.
Comparisons between commissural alignment achieved in the different THV platforms were drawn in a few studies and the results from Ochiai et al. (10) and Tarantini et al. (17) may indicate that the SAPIEN 3 platform is favorable to commissural alignment and subsequent coronary access as patients receiving this platform had considerably lower percentages of unfavorable coronary access. For example; when compared to the Evolut and Acurate Neo platforms; coronary access was higher in SAPIEN 3 than both Evolut and Neo THVs regardless of whether they were aligned or misaligned (95% vs. 71% and 46%; respectively). This is however contradictory to the findings of the study by Bieliauskas et al. (5) in which the Acurate Neo platform had the highest rate of achieving mild CMA compared to others. It is too early to determine which platform is best suited for commissural alignment as they require different techniques to achieve commissural alignment and each patient is individual in the selection of the THV platform based on their clinical situation; comorbidities; anatomy of the aortic root and the potential access route (18).
Due to the recency of commissural alignment in TAVR; a clear gap can be identified in the research area; which is that the long-term implications of commissural alignment have not been studied. From the lack of long-term studies; cardiologists around the world are not sure if commissural alignment is if even worth adopting as a routine procedure for low-risk younger patients with aortic stenosis as the long-term benefits or complications are not known. A cohort study design where low risk patients who have undergone TAVR using a commissural alignment technique are observed for a minimum of 10 years is needed to justify the adoption of commissural alignment as a routine procedure.
The limitations of this review include the relative recency of commissural alignment in TAVR as a topic; thus the articles reviewed had very similar study designs and lacked control groups to compare outcomes such as coronary filling and intervention. This also means that the data extracted from the articles was very similar and could easily be interpreted as a continuous study. On the other hand; the relative recency of this topic also creates the strengths of this literature view as since the studies available are limited; a comprehensive review was able to be carried out covering most of the literature available for the topic at hand.
Author contributions
AK is the primary author and CO'S is the project supervisor. Both authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations; or those of the publisher; the editors and the reviewers. Any product that may be evaluated in this article; or claim that may be made by its manufacturer; is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.938653/full#supplementary-material
Abbreviations
TAVR, Transcatheter Aortic Valve Replacement; SAVR, Surgical Aortic Valve Replacement; SAS, Severe Aortic Stenosis; THV, Transcatheter Heart Valve; SHV, Surgical Heart Valve; LCC/RCC, Left Coronary Cusp/Right Coronary Cusp; CT, Computed Tomography; CMA, Commissural Misalignment; RCA/LCA, Right Coronary Artery/Left Coronary Artery; Percutaneous Coronary Intervention, PCI; CAG, Coronary Angiography.
References
1. Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O'Hair D, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. (2019) 380:1706–15. doi: 10.1056/NEJMoa1816885
2. Mahmaljy H, Tawney A, Young M. Transcatheter aortic valve replacement. In: StatPearls. Treasure Island (FL): StatPearls Publishing (2021).
3. Hanzel GS, Gersh BJ. Transcatheter aortic valve replacement in low-risk, young patients. Circulation. (2020) 142:1317–9. doi: 10.1161/CIRCULATIONAHA.120.047874
4. Kumbhani D. TAVR is not the ‘beginning of the end’ for Aortic Stenosis Open Heart Surgery. Heart UT Southwestern Medical Center. Available online at: http://utswmed.org/medblog/tavr-not-beginning-end-aortic-stenosis-open-heart-surgery/ (accessed November 13, 2021).
5. Bieliauskas G, Wong I, Bajoras V, Wang X, Kofoed KF, De Backer O, et al. Patient-Specific implantation technique to obtain neo-commissural alignment with self-expanding transcatheter aortic valves. JACC Cardiovasc Interv. (2021) 14:2097–108. doi: 10.1016/j.jcin.2021.06.033
6. Tang GHL, Zaid S, Fuchs A, Yamabe T, Yazdchi F, Gupta E, et al. Alignment of Transcatheter Aortic-Valve Neo-Commissures (ALIGN TAVR): impact on final valve orientation and coronary artery overlap. JACC Cardiovasc Interv. (2020) 13:1030–42. doi: 10.1016/j.jcin.2020.02.005
7. Redondo A, Valencia-Serrano F, Santos-Martínez S, Delgado-Arana JR, Barrero A, Serrador A, et al. Accurate commissural alignment during ACURATE neo TAVI procedure. Proof of concept. Rev Esp Cardiol (Engl Ed). (2021) 75:203–12. doi: 10.1016/j.rec.2021.02.004
8. Fuchs A, Kofoed KF, Yoon S-H, Schaffner Y, Bieliauskas G, Thyregod HG, et al. Commissural alignment of bioprosthetic aortic valve and native aortic valve following surgical and transcatheter aortic valve replacement and its impact on valvular function and coronary filling. JACC Cardiovasc Interv. (2018) 11:1733–43. doi: 10.1016/j.jcin.2018.05.043
9. De Marco F, Casenghi M, Spagnolo P, Popolo Rubbio A, Brambilla N, Testa L, et al. A patient-specific algorithm to achieve commissural alignment with Acurate Neo: the sextant technique. Catheter Cardiovasc Interv. (2021) 98:E847–54. doi: 10.1002/ccd.29737
10. Ochiai T, Chakravarty T, Yoon S-H, Kaewkes D, Flint N, Patel V, et al. Coronary access after TAVR. JACC Cardiovasc Interv. (2020) 13:693–705. doi: 10.1016/j.jcin.2020.01.216
11. Holzamer A, Sitka E, Hengstenberg C, Schmid C, Debl K, Maier L, et al. Multislice computed tomography-based prediction of the implantation plane in transcatheter aortic valve implantation: determination of the line of perpendicularity and the implanter's views. Eur J Cardiothorac Surg. (2015) 48:879–85. doi: 10.1093/ejcts/ezv095
12. Abdelghani M, Landt M, Traboulsi H, Becker B, Richardt G. Coronary access after TAVR with a self-expanding bioprosthesis: insights from computed tomography. JACC Cardiovasc Interv. (2020) 13:709–22. doi: 10.1016/j.jcin.2020.01.229
13. Rogers T, Greenspun BC, Weissman G, Torguson R, Craig P, Shults C, et al. Feasibility of coronary access and aortic valve reintervention in low-risk TAVR patients. JACC Cardiovasc Interv. (2020) 13:726–35. doi: 10.1016/j.jcin.2020.01.202
14. Buono A, Morello A, Pero G, Corcione N, Bettari L, Saccocci M, et al. Commissural alignment with new-generation self-expanding transcatheter heart valves during aortic replacement. Cardiovasc Revasc Med. (2021). doi: 10.1016/j.carrev.2021.07.027. [Epub ahead of print].
15. Redondo A, Baladr ón ZC, Tch étché D, Santos -Martinez Sandra, Delgado -Arana Jose Raúl, Barrero A, et al. Commissural versus coronary optimized alignment during transcatheter aortic valve replacement JACC Cardiovas Interv. (2022) 15:135–46. doi: 10.1016/j.jcin.2021.10.005
16. Tang GHL, Sengupta A, Alexis SL, Zaid S, Leipsic JA, Blanke P, et al. Conventional versus modified delivery system technique in commissural alignment from the evolut low-risk CT substudy. Catheter Cardiovasc Interv. (2022) 99:924–31. doi: 10.1002/ccd.29973
17. Tarantini G, Nai Fovino L, Scotti A, Massussi M, Cardaioli F, Rodinò G, et al. Coronary access after transcatheter aortic valve replacement with commissural alignment: the ALIGN-ACCESS study. Circ Cardiovasc Interv. (2022) 15:e011045. doi: 10.1161/CIRCINTERVENTIONS.121.011045
Keywords: TAVR, commissures, transcatheter and surgical aortic valve replacement, SAVR-surgical aortic valve replacement, alignment, THV, transcatheter heart valve
Citation: Khalid AM and O'Sullivan CJ (2022) Commissural alignment in transcatheter aortic valve replacement: A literature review. Front. Cardiovasc. Med. 9:938653. doi: 10.3389/fcvm.2022.938653
Received: 07 May 2022; Accepted: 18 July 2022;
Published: 09 August 2022.
Edited by:
Giuseppe Tarantini, University of Padua, ItalyReviewed by:
Mevlut Celik, Erasmus Medical Center, NetherlandsPaul Schoenhagen, Case Western Reserve University, United States
Copyright © 2022 Khalid and O'Sullivan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdul Muiz Khalid, YWJkdWxtdWl6a0Bob3RtYWlsLmNvbQ==; Crochan J. O'Sullivan, Y3Jvc3VsbGl2YW5AaG90bWFpbC5jb20=
 Abdul Muiz Khalid
Abdul Muiz Khalid Crochan J. O'Sullivan
Crochan J. O'Sullivan