- 1Clinical Epidemiology and Biostatistics Department, Children's Hospital of Chongqing Medical University, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, Key Laboratory of Pediatrics in Chongqing, China International Science and Technology Cooperation Center of Child Development and Critical Disorders, Chongqing, China
- 2Shimian People's Hospital, Ya'an, China
- 3Chongqing Medical and Pharmaceutical College, Chongqing, China
- 4Department of Public Health and Preventive Medicine, School of Medicine, Jinan University, Guangzhou, China
Background: Previous studies found that remnant cholesterol (RC) is a risk factor for cardiovascular diseases and childhood obesity is associated with cardiometabolic diseases. This study aimed to explore the relationship between RC and abdominal obesity in children.
Methods: A total of 5,959 children, aged 6−12 years old, were selected from a cross-sectional study in urban-rural areas of Chongqing, China. RC was calculated by total cholesterol (TC)—high-density lipoprotein (HDL-C) cholesterol—low-density lipoprotein (LDL-C) cholesterol and was divided into four groups by quartiles (Q1–Q4).
Results: Compared to children with the lowest RC (Q1), children with higher RC had significantly higher odds of abdominal obesity (Q2: OR = 1.450, 95% CI: 1.131−1.859, p < 0.05; Q3: OR = 2.127, 95% CI: 1.632−2.772, p < 0.001; Q4: OR = 2.386, 95% CI: 1.819−3.130, p < 0.001). In the stratified analyses by urban-rural areas, the odds ratios were greater in rural areas (Q2: OR = 2.228, 95% CI: 1.572−3.160, p < 0.001; Q3: OR = 3.668, 95% CI: 2.191−6.140, p < 0.001; Q4: OR = 6.490, 95% CI: 2.271−18.551, p < 0.001) than in urban areas (Q2: OR = 1.644, 95% CI: 1.192−2.266, p < 0.05; Q3: OR = 2.266, 95% CI: 1.667−3.082, p < 0.001; Q4: OR = 2.711, 95% CI: 2.005−3.665, p < 0.001).
Conclusions: Our study found that RC was positively correlated with abdominal obesity in children, and this association was higher for children living in rural areas.
Introduction
Remnant cholesterol (RC) is the amount of cholesterol in triglyceride (TC)-rich lipoproteins produced by the liver and the intestine. It can also be considered as the sum of all non-low-density lipoprotein (LDL) and non-high-density lipoprotein (HDL) cholesterol levels (1). RC is associated with higher cardiometabolic risk and contributes to the residual risk after controlling LDL cholesterol (2, 3). In recent years, the prevalence of childhood obesity, especially abdominal obesity, has increased dramatically worldwide (4–7). Childhood obesity is a primary contributor to the development of cardiometabolic diseases, including dyslipidemia (8, 9). Therefore, it is particularly important to identify biochemical markers in children to help identify high-risk children early and conduct interventions in advance. While traditional lipid markers are not usually elevated in children with obesity (10), RC is predictive of coronary artery stenosis in patients with normal serum TC levels (11). Previous studies also showed that RC is associated with obesity, triglycerides, and systolic blood pressure (BP) and could mediate the transition from obesity to ischemic cardiomyopathy (12, 13). Further, apolipoprotein B48 (specific to RC) is more strongly associated with central adiposity in obese prepubertal children, compared to classical lipid marker LDL-C or total cholesterol (TC) (14). Therefore, RC may be more representative of early cardiovascular risk compared to LDL. However, there are limited data on children and adolescents, but there are no studies on Asian children.
This study hypothesized that RC is correlated with abdominal obesity in children and an urban-rural difference may exist. A large cohort from Chongqing, China was used to test the hypothesis. The results could provide a basis for the prevention of early dyslipidemia in children with obesity and to reduce the cardiovascular risk in adulthood.
Methods
Subjects
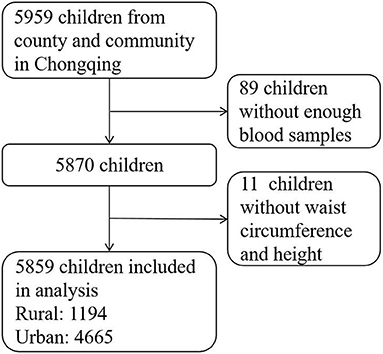
The Chongqing Children's Health Cohort was selected through a two-stage stratified (county and community) sampling. Details of participant recruitment and questionnaire collection were described in a previously published article (15). The baseline data collected in 2014 was used to assess the relationship between RC and abdominal obesity. Participants who met the following inclusion criteria were included in this study: (1) aged 6–12 years old, (2) living in the target area for more than 6 months, (3) free of serious diseases, such as cardiovascular diseases, nephropathy, and cancer, and, (4) both participants and their parents/guardians gave informed consent, and (5) gave permission to collect blood samples. Finally, 5,859 samples were analyzed after excluding participants without enough blood samples to check serum lipid levels (n = 89) or without data on waist circumference and height (n = 11) (shown in Figure 1). The Medical Research Ethics Committee of the Research Division of the Children's Hospital of Chongqing Medical University gave its approval for the study, approval number (No. 2019-86).
Demographic variables and dietary intake
Demographic data included age, gender, and residing in rural/urban areas. Socioeconomic status (SES) including parents' occupation, fathers' education level, household income, living situation, people living with a child, and medical insurance were collected. Parental education level was represented by a 4-point scale (≤ 9, 10–12, 13–15, and >15 years) (16, 17). Data on birth weight, breastfeeding, and family history of obesity were also collected. Dietary intakes were collected using a quantitative food frequency questionnaire, as previously described in detail (18).
Physical examination
Physical examination was conducted by trained pediatric nurses, as previously described (19). In brief, height and weight were measured using a mobile medical ultrasonic machine (model WS-H300D). Body mass index (BMI) was calculated by weight/height2 (kg/m2). Waist circumference was measured two times at the center of the umbilicus, and the average value was taken to calculate the waist-to-height ratio (WHtR) as a measure of abdominal obesity.
Blood pressure (BP) and heart rate were measured on three different occasions using an OMRON arm-mounted electronic sphygmomanometer (HEM7051). Children were diagnosed with hypertension if all three BP measurements met the criteria for hypertension according to the diagnostic criteria for Chinese children (20).
Biochemical indexes
Blood samples were taken after at least 12 h of fasting for the measurement of biochemical indexes, including fasting blood glucose (FBG), TC, TG, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C). TC was measured by the Cholesterol Determination - Peroxidase and 4-Aminoantipyrine substrate method. The mixture of cholesteryl esters and free cholesterol was reacted with cholesteryl esterase and cholesterol oxidase to produce hydrogen peroxide, which reacted with 4-aminoantipyrine and produced quinone imine compounds. HDL cholesterol was measured by the direct peroxidase clearance method in two steps. In the first step, reagent one (buffer 2-ethanesulfonic acid and surfactant 1) and serum lipid compositions (celiac particles, very-low-density lipoproteins (VLDL), and LDL) were reacted to expose the cholesterol in the serum. After cholesterol esterase and cholesterol oxidase catalyzed the cholesterol, hydrogen peroxide was produced. In the second step, similarly, another surfactant was used to expose the cholesterol in HDL, which would react with cholesterol enzymes for chromogenic reaction, and the shade of color was proportional to the amount of HDL cholesterol. LDL cholesterol was measured by the direct surfactant removal method. Except for LDL, surfactant 1 was used to alter the structure of lipoproteins (chylomicron, VLDL, HDL, etc.), and the metabolite would react with cholesterol esterases and cholesterol oxidases. As a result, all lipoproteins, except LDL, were eliminated. Then, a chromogenic reaction of LDL occurred with surfactant 2. The shade of color was proportional to the amount of LDL cholesterol. The details were described in a previous study (15), and RC was calculated by TC—HDL-C—LDL-C and was divided into four groups by quartiles (Q1–Q4).
Diagnostic criteria
A threshold of WHtR ≥0.480 for boys and WHtR ≥ 0.456 for girls were identified for abdominal obesity in childhood (21).
Statistical analyses
Normally distributed continuous variables were expressed as mean ± standard deviation, and the differences between rural and urban areas were assessed with Student's t-test. Skewed distribution continuous variables (e.g., diet) were reported as medians (interquartile range), and the Mann–Whitney U test was used for comparison between the two groups. The Chi-square test was used to compare categorical variables. A linear regression model was used to evaluate the association between RC and WHtR, and a logistic regression model was used to assess the relationship between abdominal obesity and quartile range increase of RC.
Statistical analysis was performed using SAS 9.4 software (Copyright© 2016 SAS Institute Inc., Cary, NC, USA). A p-value <0.05 was considered statistically significant.
Results
General characteristics
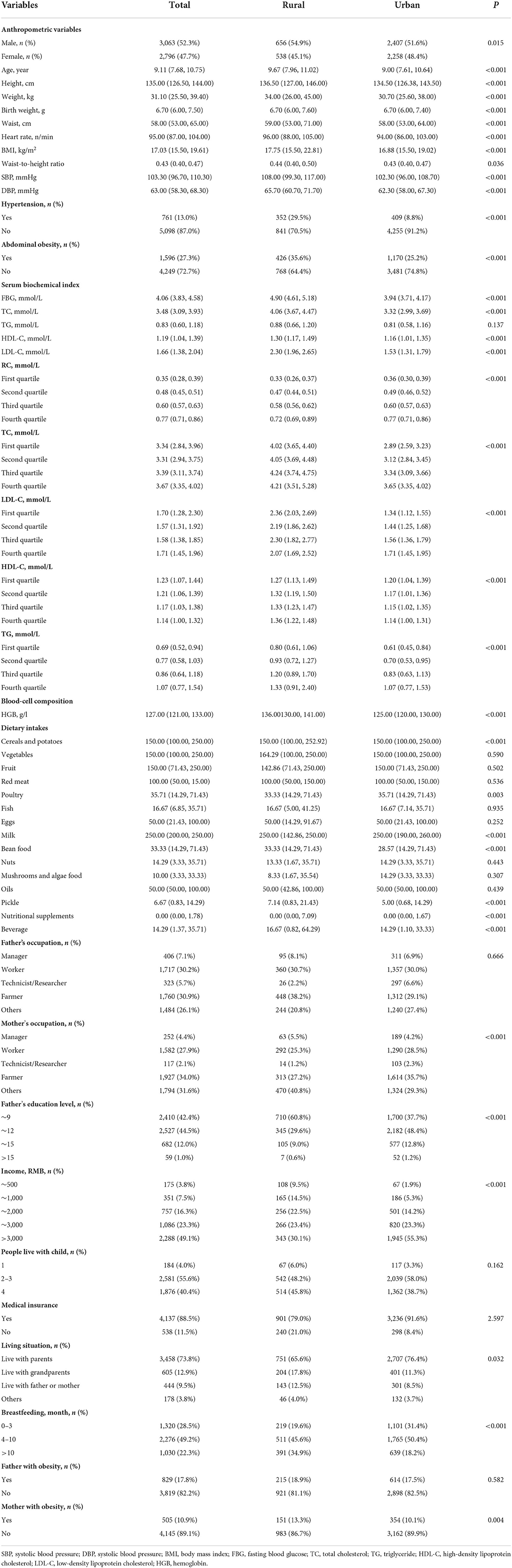
The demographic characteristics of the participants are presented in Table 1. The mean age was 9.14 ± 1.76 years, and 52.3% (3063/5859) were boys. There are differences in the characteristics of children living in urban and rural areas (Table 1). Therefore, subgroup analyses of the urban-rural areas were performed in this study.
Prevalence of abdominal obesity
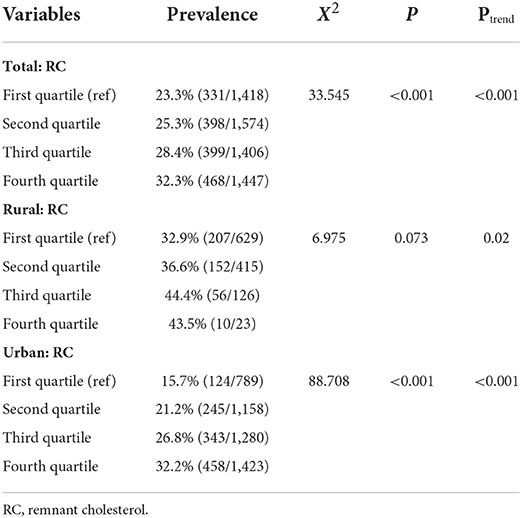
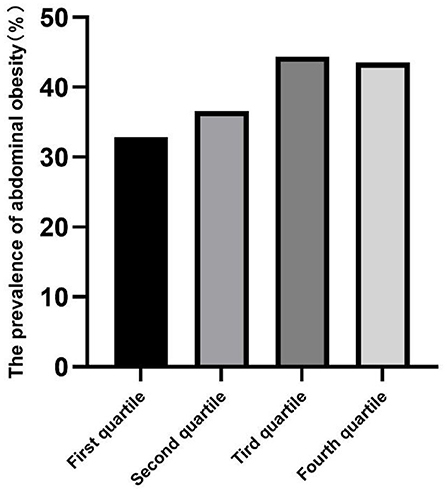
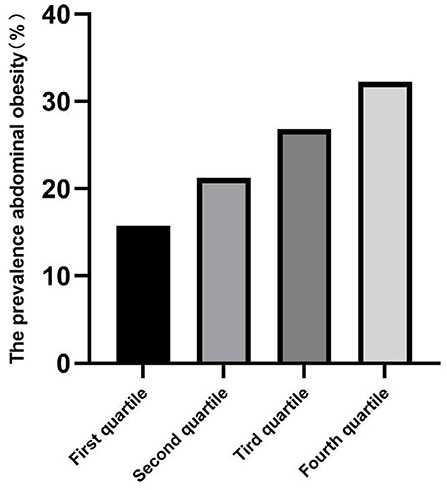
The prevalence of abdominal obesity was higher in children with increased total RC, and the RC of children living in urban areas was higher than those living in rural areas (all p < 0.05) (Table 2). The prevalence of abdominal obesity increased with increasing RC quartiles in the total, urban, and rural areas (Figures 2–4). Additionally, the children with the highest RC had the highest prevalence of abdominal obesity (p for trend <0.05), which was found in both urban and rural areas.
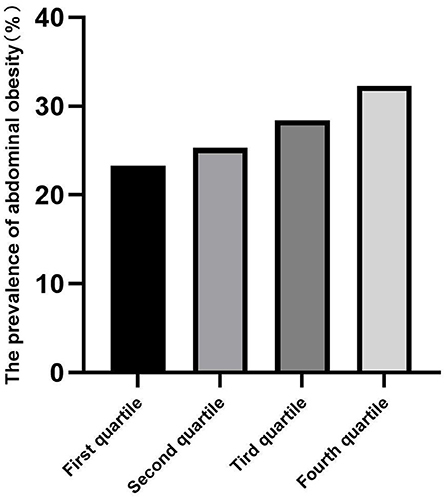
Figure 2. The prevalence of abdominal obesity among remnant cholesterol (RC) quartiles in total participants.
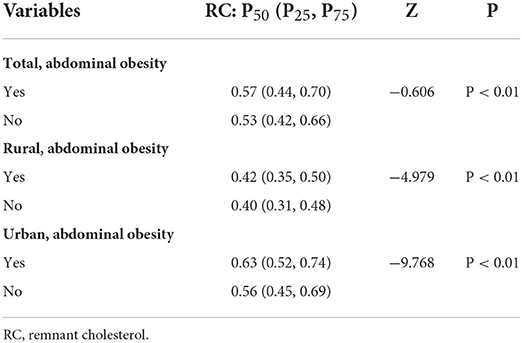
The univariate analysis of RC
Compared to the normal-weight children, the RC levels were higher in children with abdominal obesity, and the difference was significant both in urban and rural areas (all p < 0.001, in Table 3).
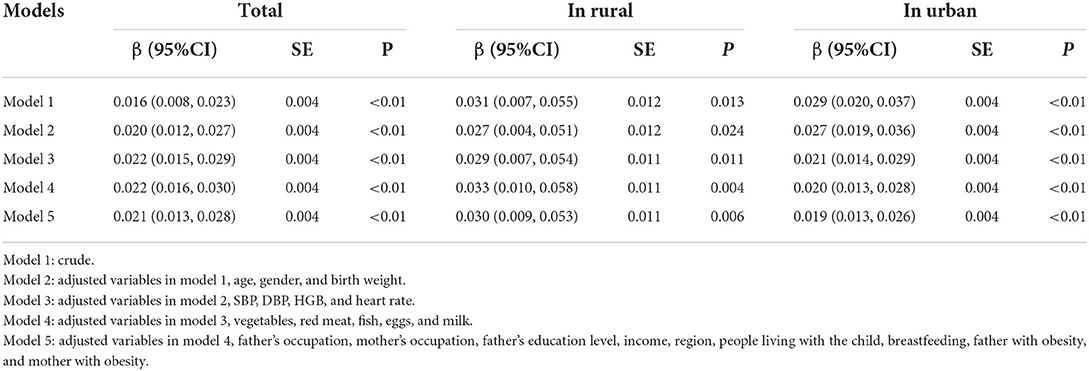
The association between RC and WHtR
A linear regression model was used to examine the relationship between RC and WHtR in Table 4. After adjusting for other covariates in model 5, RC was significantly positively associated with WHtR (β = 0.021, 95% CI: 0.013−0.028, p < 0.05). In the subgroup analyses, the RC level was significantly positively associated with WHtR in children living in both urban (β = 0.019, 95% CI: 0.013−0.026, p < 0.05) and rural (β = 0.030, 95% CI: 0.009−0.053, p < 0.05) areas.
The association between quartile range increase of RC and abdominal obesity
A logistic regression model was used to investigate the relationship between RC by quartiles and abdominal obesity in Table 5. After controlling for other covariates in model 5, compared to children with the lowest RC (Q1), children with higher RC had significantly higher odds of abdominal obesity (Q2: OR = 1.450, 95% CI: 1.131−1.859, p < 0.05; Q3: OR = 2.127, 95% CI: 1.632−2.772, p < 0.001; Q4: OR = 2.386, 95% CI: 1.819−3.130, p < 0.001). In the stratified analyses by urban-rural areas, the odds ratios were greater in rural areas (Q2: OR = 2.228, 95% CI: 1.572−3.160, p < 0.001; Q3: OR = 3.668, 95% CI: 2.191−6.140, p < 0.001; Q4: OR = 6.490, 95% CI: 2.271−18.551, p < 0.001) than in urban areas (Q2: OR =1.644, 95% CI: 1.192−2.266, p < 0.05; Q3: OR = 2.266, 95% CI: 1.667−3.082, p < 0.001; Q4: OR = 2.711, 95% CI: 2.005−3.665, p < 0.001).
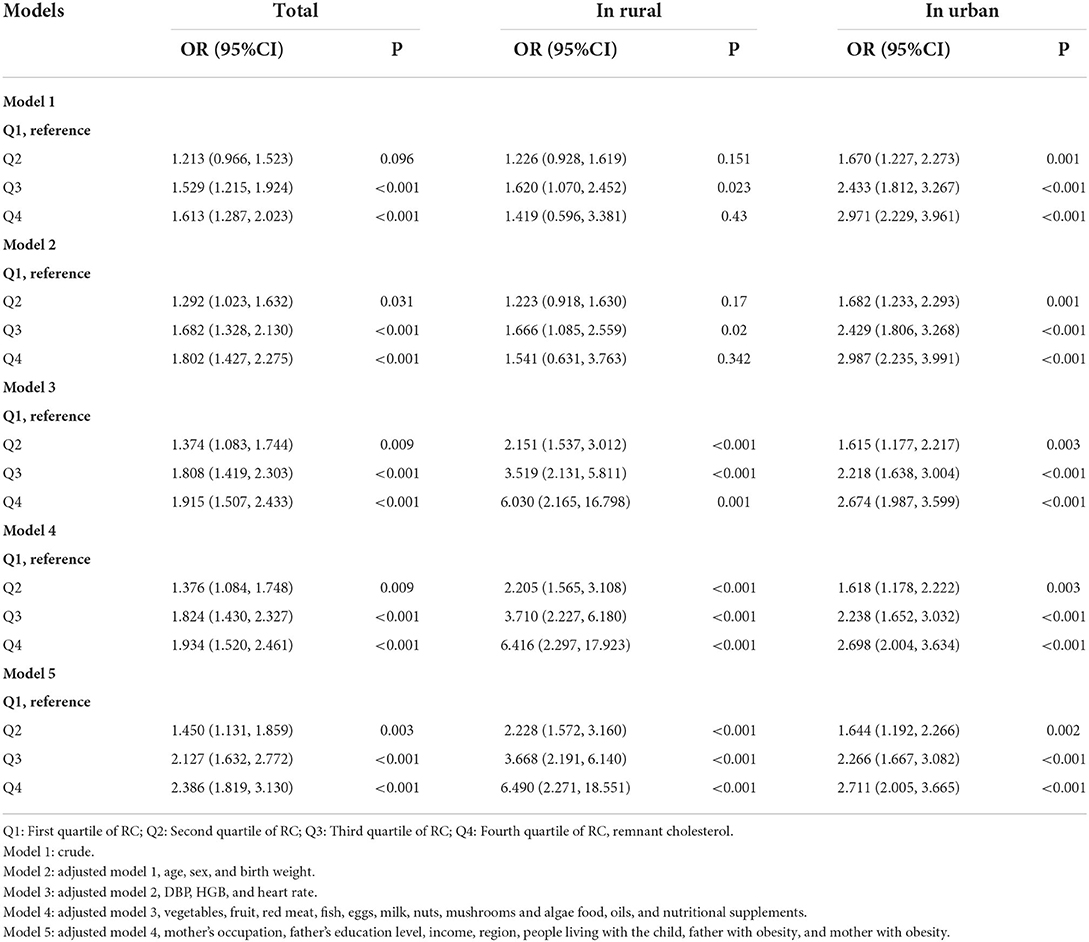
Table 5. The logistic regression analysis of quartile range increase of the RC level with abdominal obesity.
Discussion
Our study showed a significant positive association between RC and abdominal obesity in children. Children living in urban areas had a higher level of RC than children living in rural areas. However, the prevalence of abdominal obesity among children in rural areas was higher than that in urban areas. The association between RC and abdominal obesity was higher for children living in rural areas.
Similarly, previous studies found that, both in children and adults, RC was positively correlated with waist circumference and BMI (2, 13, 22). In our study, the prevalence of abdominal obesity in children increased with the increase in the RC quartile range, which was consistent with previous studies. In a Danish study in adults, BMI increased with progressively higher RC concentrations in four subgroups. The median RC level in this study was higher than that observed in a previous study. This may be due to the differences in lipid levels between adults and children, and RC concentrations in this study were both calculated and measured (22). In addition, evidence from Di Costanzo et al. proved that the prevalence of overweight/obesity and BMI were gradually increased by the RC tertiles, and the RC level was significantly and positively correlated with BMI and waist circumference (23); besides, Varbo et al. found that BMI also increased with nonfasting RC tertile range increase (24). Moreover, our study and previous studies confirmed that the obese group had higher levels of RC than the normal weight group, both in adults and children (13, 25, 26). However, this study added new reliable evidence from a large sample size of urban-rural childhood participants. Since most of the fat in children is deposited in the abdomen, children who were not obese/overweight according to BMI may be abdominally obese, which was more common than generalized obesity (27). Interestingly, our study found that the association between RC and abdominal obesity was higher for children living in rural areas. This may be explained by the different lifestyle and dietary intake patterns.
The dietary structure of children had changed greatly during the past decades, and accompanying it, the incidence of childhood obesity had increased dramatically (7, 28, 29). Hepatic absorption and metabolism of cholesterol in celiac residues was influenced by the type of fat in the diet and the composition of fatty acid. A saturated fat-rich diet reduces the excretion of residual cholesterol from celiac disease (30). Nutritional excess and central obesity exacerbated dietary lipid intolerance and impaired metabolism of celiac residues, resulting in elevated plasma concentrations of TC-rich lipoprotein residues (31–33).
Remnant cholesterol (RC) had been found as an independent risk factor for cardiovascular disease, similar to LDL, and the RC in the bloodstream passed through the endothelium and collected within the arterial wall, where it was absorbed by macrophages and smooth muscle cells, forming foam cells that eventually became part of the atherosclerotic plaque (34). Atherosclerosis due to RC was primarily driven by RC concentrations in the bloodstream, independent of the cause of increased residual cholesterol, such as due to overweight and obesity (22). Individuals with obesity have higher RC concentrations. However, the etiological mechanism of increased RC was not clearly explained, such as whether and how overweight and obesity increased RC (22). Importantly, due to the complexity of lipid metabolism and the mechanisms of gene-environment interactions in metabolic diseases, previous studies found that the genetic variants with the greatest impact on RC concentrations were found at a key point of lipoprotein metabolisms, such as apolipoprotein E (APOE), apolipoprotein C3 (APOC3), and apolipoprotein C2 (APOC2) genes encoding apolipoproteins and genes encoding enzymes involved in residue degradation, such as lipoprotein lipase (LPL) (1).
Fasting RC was not only a risk factor for cardiovascular diseases such as atherosclerosis and myocardial infarction but was also associated with diabetes, kidney disease, and carotid artery intima-media thickness in adolescents (22, 23, 35–37). Moreover, it was a useful predictor of postprandial hyperlipidemia (38, 39). On the one hand, our results added evidence that fasting RC was positively correlated with obesity. On the other hand, postprandial RC was also found to be associated with waist-to-hip ratio (WHR) in adults, independent of BMI, and the increased risk of IHD due to obesity was mediated in part by non-fasting RC (12, 26). Therefore, the study of non-fasting RC will also be an important focus for us in the future. Further, studies showed that elevated non-fasting RC was causally associated with mild inflammation and IHD and that recent epidemiological data strongly supported RC in the non-fasting state as a contributor to residual risk (3, 24). More studies are required to investigate the roles of fasting and non-fasting RC in cardiovascular outcomes.
Strengths and limitation
Obesity in children is mainly subcutaneous fat, so the use of abdominal obesity indicators is more appropriate than using general obesity diagnosed by BMI (40). Our study was the first study to examine the relationship between RC and abdominal obesity in a large Chinese cohort.
There are several limitations to this study. First, the RC calculated from the standard lipid profile as TC minus LDL-C minus HDL-C is different from the RC measured by nuclear magnetic resonance (41), as there was no uniform clinical method for measuring RC. Second, the causal relationship cannot be explained by a cross-sectional study. Third, the study did not exclude children with fatty liver disease and/or atherosclerosis and did not collect information on background therapy in this study. Therefore, future studies are needed to investigate the causal association between RC and abdominal obesity and potential etiological mechanisms.
Conclusion
In our study, RC was positively associated with childhood abdominal obesity both in urban and rural areas. Moreover, the association was higher for children living in rural areas. Our findings provided a theoretical basis for cardiovascular prevention in children with abdominal obesity. Further cohort studies are needed to confirm the causal relationship between RC and abdominal obesity in children.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by the Medical Research Ethics Committee of the Research Division of the Children's Hospital of Chongqing Medical University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
XiaohL: conceptualization, planning the methodology, and writing—review and editing. SL, DH, and LZ: investigation and supervision. FT, YF, YR, and XP: validation and obtaining resources. JT, XiaoyL, XinggL, and GH: writing—original draft and writing—review and editing. All authors critically reviewed and approved the final draft of the manuscript.
Funding
This work was supported by the Basic Research Project of Key Laboratory of the Ministry of Education of China in 2021 (GBRP-202106), the Major Health Project of Chongqing Science and Technology Bureau (CSTC2021jscx-gksb-N0001), the Research and Innovation Team of Chongqing Medical University (W0088), the Joint Medical Research Project of Chongqing Municipal Health Commission and Chongqing Science and Technology Bureau (2020MSXM062), the National Key Research and Development Project (2017YFC0211705), the Education Commission of Chongqing Municipality (KJQN201900443), and the National Natural Science Foundation of China (82003521). The funders had no role in the study design, data collection and analysis, the decision to publish, or the preparation of the manuscript.
Acknowledgments
The authors would like to acknowledge the laboratory support of the Ministry of Education Key Laboratory of Child Development and Disorders and all the staff members of the 6 elementary schools in the two regions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Varbo A, Nordestgaard BG. Remnant lipoproteins. Curr Opin Lipidol. (2017) 28:300–7. doi: 10.1097/MOL.0000000000000429
2. Krysa JA, Vine DF, Beilin LJ, Burrows S, Huang RC, Mori TA, et al. Apob48-remnant lipoproteins are associated with increased cardiometabolic risk in adolescents. Atherosclerosis. (2020) 302:20–6. doi: 10.1016/j.atherosclerosis.2020.04.021
3. Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. (2014) 384:626–35. doi: 10.1016/S0140-6736(14)61177-6
4. McPhee PG, Singh S, Morrison KM. Childhood obesity and cardiovascular disease risk: working toward solutions. Can J Cardiol. (2020) 36:1352–61. doi: 10.1016/j.cjca.2020.06.020
5. Daley MF, Barrow JC, Tabano DC, Reifler LM, Kraus EM, Davies SD, et al. Estimating childhood obesity prevalence in communities through multi-institutional data sharing. J Public Health Manag Pract. (2020) 26:1–E10. doi: 10.1097/PHH.0000000000000942
6. Beynon C, Bailey L. Prevalence of severe childhood obesity in wales UK. J Public Health. (2020) 42:e435–e9. doi: 10.1093/pubmed/fdz137
7. Rito AI, Buoncristiano M, Spinelli A, Salanave B, Kunesova M, Hejgaard T, et al. Association between characteristics at birth, breastfeeding and obesity in 22 countries: the who European childhood obesity surveillance initiative - Cosi 2015/2017. Obes Facts. (2019) 12:226–43. doi: 10.1159/000500425
8. Ayer J, Charakida M, Deanfield JE, Celermajer DS. Lifetime risk: childhood obesity and cardiovascular risk. Eur Heart J. (2015) 36:1371–6. doi: 10.1093/eurheartj/ehv089
9. Weihrauch-Bluher S, Schwarz P, Klusmann JH. Childhood obesity: increased risk for cardiometabolic disease and cancer in adulthood. Metabolism. (2019) 92:147–52. doi: 10.1016/j.metabol.2018.12.001
10. Expert Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents National Heart Lung Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. (2011) 128(Suppl. 5):S213–56. doi: 10.1542/peds.2009-2107C
11. Masuoka H, Kamei S, Ozaki M, Kawasaki A, Shintani U, Ito M, et al. Predictive value of remnant-like particle cholesterol as an indicator of coronary artery stenosis in patients with normal serum triglyceride levels. Intern Med. (2000) 39:540–6. doi: 10.2169/internalmedicine.39.540
12. Varbo A, Benn M, Smith GD, Timpson NJ, Tybjaerg-Hansen A, Nordestgaard BG. Remnant cholesterol, low-density lipoprotein cholesterol, and blood pressure as mediators from obesity to ischemic heart disease. Circ Res. (2015) 116:665–73. doi: 10.1161/CIRCRESAHA.116.304846
13. Choi YJ, Jo YE, Kim YK, Ahn SM, Jung SH, Kim HJ, et al. High plasma concentration of remnant lipoprotein cholesterol in obese children and adolescents. Diabetes Care. (2006) 29:2305–10. doi: 10.2337/dc06-0938
14. Wilke MS, Maximova K, Henderson M, Levy E, Paradis G, O'Loughlin J, et al. Adiposity in children and Cvd risk: Apob48 has a stronger association with central fat than classic lipid markers. J Clin Endocrinol Metab. (2016) 101:2915–22. doi: 10.1210/jc.2016-1171
15. Liang X, Xiao L, Luo Y, Xu J. Prevalence and risk factors of childhood hypertension from birth through childhood: a retrospective cohort study. J Hum Hypertens. (2020) 34:151–64. doi: 10.1038/s41371-019-0282-z
16. Liang X, Su S, Hao G, Snieder H, Treiber F, Kapuku G, et al. Determinants of pulse wave velocity trajectories from youth to young adulthood: the georgia stress and heart study. J Hypertens. (2019) 37:563–71. doi: 10.1097/HJH.0000000000001933
17. Chen J, Luo S, Liang X, Luo Y, Li R. The relationship between socioeconomic status and childhood overweight/obesity is linked through paternal obesity and dietary intake: a cross-sectional study in Chongqing, China. Environ Health Prev Med. (2021) 26:56. doi: 10.1186/s12199-021-00973-x
18. Liang X, Chen M, Qu P, Hao G, Huang Y, Chen J, et al. The association of vitamin A and vitamin D with hypertension in children: a case-control study. Int J Hypertens. (2018) 2018:9295147. doi: 10.1155/2018/9295147
19. Liang X, He Y, Chen M, Ping Q, Chen J. The association of lecithin retinol acyltransferase and the 25(Oh)D receptor with pediatric overweight and obesity. Eur J Clin Nutr. (2019) 73:1626–9. doi: 10.1038/s41430-019-0422-0
20. Fan Hui Y-kM. Updating blood pressure references for Chinese children aged 3–17 years. Chin J Hypertens. (2017) 5:428–35. doi: 10.16439/j.cnki.1673-7245.2017.05.009
21. Dou Y, Jiang Y, Yan Y, Chen H, Zhang Y, Chen X, et al. Waist-to-height ratio as a screening tool for cardiometabolic risk in children and adolescents: a nationwide cross-sectional study in China. BMJ Open. (2020) 10:e037040. doi: 10.1136/bmjopen-2020-037040
22. Varbo A, Freiberg JJ, Nordestgaard BG. Remnant cholesterol and myocardial infarction in normal weight, overweight, and obese individuals from the copenhagen general population study. Clin Chem. (2018) 64:219–30. doi: 10.1373/clinchem.2017.279463
23. Di Costanzo A, Perla FM, D'Erasmo L, Arca M, Chiesa C, Pacifico L. Elevated serum concentrations of remnant cholesterol associate with increased carotid intima-media thickness in children and adolescents. J Pediatr. (2021) 232:133–9 e1. doi: 10.1016/j.jpeds.2021.01.019
24. Varbo A, Benn M, Tybjaerg-Hansen A, Nordestgaard BG. Elevated remnant cholesterol causes both low-grade inflammation and ischemic heart disease, whereas elevated low-density lipoprotein cholesterol causes ischemic heart disease without inflammation. Circulation. (2013) 128:1298–309. doi: 10.1161/CIRCULATIONAHA.113.003008
25. Wang Y, Pendlebury C, Dodd MM, Maximova K, Vine DF, Jetha MM, et al. Elevated remnant lipoproteins may increase subclinical Cvd risk in pre-pubertal children with obesity: a case-control study. Pediatr Obes. (2013) 8:376–84. doi: 10.1111/j.2047-6310.2012.00116.x
26. van Hees AM, Saris WH, Dallinga-Thie GM, Hul GB, Martinez JA, Oppert JM, et al. Fasting and postprandial remnant-like particle cholesterol concentrations in obese participants are associated with plasma triglycerides, insulin resistance, and body fat distribution. J Nutr. (2008) 138:2399–405. doi: 10.3945/jn.108.094516
27. Solanki DK, Walia R, Gautam A, Misra A, Aggarwal AK, Bhansali A. Prevalence of abdominal obesity in non-obese adolescents: a North Indian adolescent study. J Pediatr Endocrinol Metab. (2020) 33:853–8. doi: 10.1515/jpem-2019-0026
28. Huang JY, Qi SJ. Childhood obesity and food intake. World J Pediatr. (2015) 11:101–7. doi: 10.1007/s12519-015-0018-2
29. An R. Diet quality and physical activity in relation to childhood obesity. Int J Adolesc Med Health. (2017) 29:2015-0045. doi: 10.1515/ijamh-2015-0045
30. Lambert MS, Avella MA, Botham KM, Mayes PA. The type of dietary fat alters the hepatic uptake and biliary excretion of cholesterol from chylomicron remnants. Br J Nutr. (2000) 83:431–8. doi: 10.1017/S0007114500000532
31. Krysa JA, Ball GDC, Vine DF, Jetha M, Proctor SD. Apob-lipoprotein remnant dyslipidemia and high-fat meal intolerance is associated with markers of cardiometabolic risk in youth with obesity. Pediatr Obes. (2021) 16:e12745. doi: 10.1111/ijpo.12745
32. Klop B, Elte JW, Cabezas MC. Dyslipidemia in obesity: mechanisms and potential targets. Nutrients. (2013) 5:1218–40. doi: 10.3390/nu5041218
33. Sabaka P, Kruzliak P, Gaspar L, Caprnda M, Bendzala M, Balaz D, et al. Postprandial changes of lipoprotein profile: effect of abdominal obesity. Lipids Health Dis. (2013) 12:179. doi: 10.1186/1476-511X-12-179
34. Nordestgaard BG. Triglyceride-Rich lipoproteins and atherosclerotic cardiovascular disease: new insights from epidemiology, genetics, and biology. Circ Res. (2016) 118:547–63. doi: 10.1161/CIRCRESAHA.115.306249
35. Carvalho LSF, Bensenor IM, Nogueira ACC, Duncan BB, Schmidt MI, Blaha MJ, et al. Increased particle size of triacylglycerol-enriched remnant lipoproteins, but not their plasma concentration or lipid content, augments risk prediction of incident type 2 diabetes. Diabetologia. (2021) 64:385–96. doi: 10.1007/s00125-020-05322-1
36. Yan P, Xu Y, Miao Y, Bai X, Wu Y, Tang Q, et al. Association of remnant cholesterol with chronic kidney disease in middle-aged and elderly Chinese: a population-based study. Acta Diabetol. (2021) 58:1615–25. doi: 10.1007/s00592-021-01765-z
37. Quispe R, Martin SS, Michos ED, Lamba I, Blumenthal RS, Saeed A, et al. Remnant cholesterol predicts cardiovascular disease beyond Ldl and Apob: a primary prevention study. Eur Heart J. (2021) 42:4324–32. doi: 10.1093/eurheartj/ehab432
38. Nagata T, Sugiyama D, Kise T, Tsuji S, Ohira H, Sato I, et al. Fasting remnant lipoproteins can predict postprandial hyperlipidemia. Lipids Health Dis. (2012) 11:146. doi: 10.1186/1476-511X-11-146
39. Masuda D, Yamashita S. Postprandial hyperlipidemia and remnant lipoproteins. J Atheroscler Thromb. (2017) 24:95–109. doi: 10.5551/jat.RV16003
40. Staiano AE, Katzmarzyk PT. Ethnic and sex differences in body fat and visceral and subcutaneous adiposity in children and adolescents. Int J Obes. (2012) 36:1261–9. doi: 10.1038/ijo.2012.95
Keywords: abdominal obesity, children, remnant cholesterol, urban-rural area, waist-to-height ratio
Citation: Tong J, Li X, Liang X, Tang F, Ren Y, Hao G, Peng X, Luo S, Feng Y, Huang D, Zhao L and Liang X (2022) The relationship of remnant cholesterol and abdominal obesity in children: A cross-sectional study. Front. Cardiovasc. Med. 9:929560. doi: 10.3389/fcvm.2022.929560
Received: 27 April 2022; Accepted: 30 June 2022;
Published: 27 July 2022.
Edited by:
Ruan Kruger, North-West University, South AfricaReviewed by:
Aldo Grefhorst, Amsterdam University Medical Center, NetherlandsAntonina Giammanco, University of Palermo, Italy
Copyright © 2022 Tong, Li, Liang, Tang, Ren, Hao, Peng, Luo, Feng, Huang, Zhao and Liang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaohua Liang, bGlhbmd4aWFvaHVhNjY2QHNpbmEuY29t, eGlhb2h1YWxpYW5nQGhvc3BpdGFsLmNxbXUuZWR1LmNu
†These authors have contributed equally to this work
 Jishuang Tong1,2†
Jishuang Tong1,2† Daochao Huang
Daochao Huang Xiaohua Liang
Xiaohua Liang