- 1Division of Cardiology, Department of Medical Biotechnologies, University of Siena, Siena, Italy
- 2Division of Cardiology, Department of Cardiovascular Diseases -AUSL Romagna, Ospedale S. Maria delle Croci, Ravenna, Italy
- 3Department of Cardiac Surgery, Cardiac Surgery, St. Michael Hospital, Toronto, ON, Canada
- 4Department of Cardiac Surgery, Azienda Ospedaliera Universitaria Senese, Siena, Italy
The use of a left ventricular assist device (LVAD) as a bridge-to-transplantation or destination therapy to support cardiac function in patients with end-stage heart failure (HF) is increasing in all developed countries. However, the expertise needed to implant and manage patients referred for LVAD treatment is limited to a few reference centers, which are often located far from the patient's home. Although patients undergoing LVAD implantation should be permanently referred to the LVAD center for the management and follow-up of the device also after implantation, they would refer to the local healthcare service for routine assistance and urgent health issues related to the device or generic devices. Therefore, every clinician, from a bigger to a smaller center, should be prepared to manage LVAD carriers and the possible risks associated with LVAD management. Particularly, emergency treatment of patients with LVAD differs slightly from conventional emergency protocols and requires specific knowledge and a multidisciplinary approach to avoid ineffective treatment or dangerous consequences. This review aims to provide a standard protocol for managing emergency and urgency in patients with LVAD, elucidating the role of each healthcare professional and emphasizing the importance of collaboration between the emergency department, in-hospital ward, and LVAD reference center, as well as algorithms designed to ensure timely, adequate, and effective treatment to patients with LVAD.
Introduction
A left ventricular assist device (LVAD) is implanted to support cardiac function in patients with end-stage heart failure (HF), when the myocardium is no more capable of ensuring the necessary hemodynamic conditions to maintain normal vital functions. The device implantation stage is strictly a matter of cardiac surgeons and should take place only in designated centers under the coordination of the National Heart Transplantation Center.
Thanks to rapid improvements in technology using more reliable and durable devices and an increasing incidence of advanced HF, the use of LVAD is widespread in almost all developed countries (1–3); however, few centers have the required expertise and supplies. This entails the referral of many patients coming from the whole country to a reference LVAD center, even many miles away from the local center. After implantation, these patients will have to be permanently referred to the LVAD center for device management and follow-up; however, routine assistance will be demanded by their trusted cardiologists and family doctors. Moreover, in case of urgent health issues, whether device-related or generic, they would refer to the local healthcare service. The concept of “shared-care” was born to optimize the management of severe patients and patients with chronic diseases through improved communication between primary and specialty centers and knowledge sharing. The result is an improvement in the quality of care by primary care hospitals alongside a reduction in the workload for tertiary center and, therefore, the overall cost. It has also proven to be a feasible and effective strategy for patients with LVAD (4).
Therefore, as the number of patients treated with LVAD is increasing, many clinicians, from bigger to smaller centers and from cardiologists to all healthcare professionals, will have to deal with LVAD carriers in the near future, so they should be prepared for the possible risks associated with LVAD management. In fact, emergency treatment of patients with LVAD differs slightly from the conventional emergency protocols and requires specific knowledge to properly manage, avoid ineffective treatment, or provide dangerous consequences (5, 6).
Several authors have already addressed this concern, and a recent expert consensus has been published on this topic (7, 8) However, the importance of a multidisciplinary approach for these patients and cooperation between the emergency department (ED) and in-hospital ward, within the LVAD center or, for local centers, with the LVAD center, and the role of each healthcare professional in the critical management of these sensitive patients has not been fully elucidated.
The main purpose of this paper is to present a standard protocol addressed to all healthcare professionals, based on the available evidence and authors experience, focused on the role of multiple clinical parts for the care and management of patients with LVAD. This would provide algorithms designed to ensure an adequate and timely response of all clinicians involved in the emergency care areas and clear indications for the interaction between dedicated and non-dedicated professionals.
LVAD-associated complications
Left ventricular assist device-associated complications may be classified into LVAD-specific and LVAD-related complications (9). LVAD-specific complications are those directly involving structural or functional properties of the device and include suction event, pump thrombosis, pump failure, pump stoppage, and driveline damage. Besides, complications referred to as “related” are those not directly affecting the device but due to its presence and associated treatment. LVAD-related complications are, therefore, bleeding, hemorrhagic or ischemic stroke, infections, right ventricular failure, dysrhythmia, and aortic regurgitation (10).
In most of the cases, LVAD-related complications present themselves as emergencies, requiring the patient to be admitted to the nearest ED. As reported by the Heart Failure Society of America (HFSA), the Society for Academic Emergency Medicine (SAEM), and the International Society for Heart and Lung Transplantation (ISHLT) in the 2019 consensus for managing emergencies in patients with ventricular assist devices (VAD) (1), among the most worrisome medical emergencies commonly reported in individuals with VADs are cardiac arrest, unstable arrhythmias, myocardial infarction, and unexplained hypotension.
The nearest healthcare center plays a crucial role in readily evaluating patients who arrive in an unstable condition and stabilizing their vital parameters before sending them to a center with appropriate expertise. Situations that typically require immediate transfer to a primary VAD center are
• cardiac tamponade,
• mechanical VAD failure,
• pump thrombosis,
• emergency non-cardiac surgery, and
• neurological events.
Many concerns about the management of such patients arise from their intrinsic precarious coagulation balance. In fact, LVAD carriers are both at high thrombotic and high bleeding risk. On one hand, the risk of thrombosis is mainly determined by the presence of a foreign body, a severely reduced ejection fraction, and possibly atrial fibrillation. On the other hand, bleeding risk is due to the assumption of vitamin K antagonists along with aspirin, the possibility of hepatic congestion consequent to right heart dysfunction, and von Willebrand acquired disease.
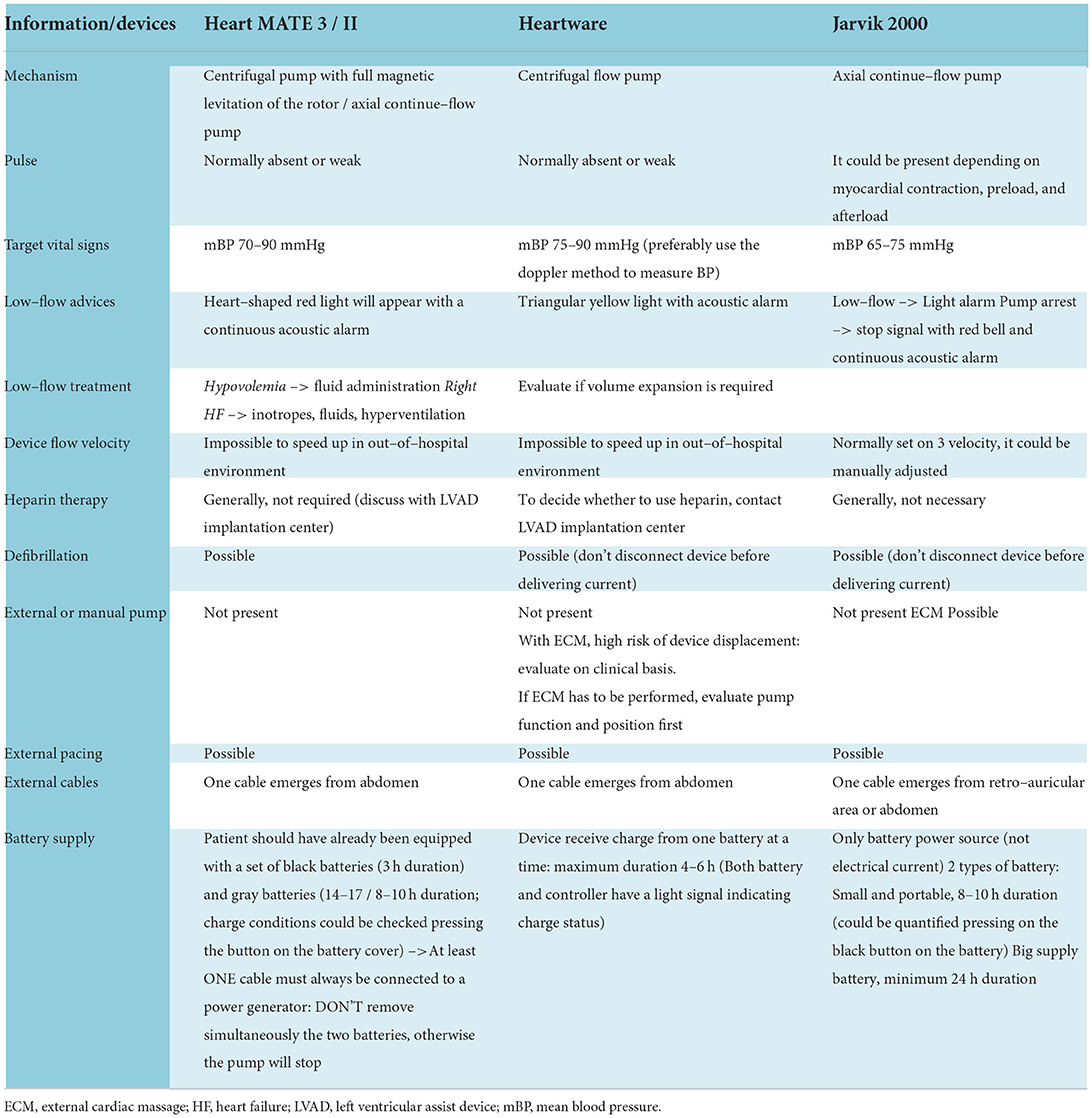
Table 1 lists specific recommendations for the primary assistance of the most common LVAD-specific and LVAD-related emergencies.
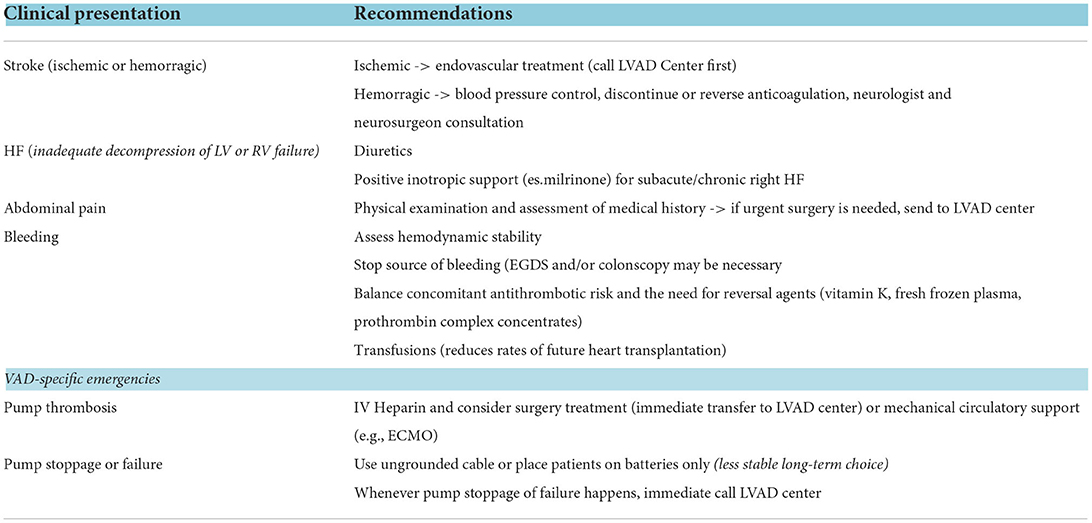
Table 1. Management of the main emergency conditions of patients with LVAD according to the Heart Failure Society of America (HFSA), the Society for Academic Emergency Medicine (SAEM), and the International Society for Heart and Lung Transplantation (ISHLT) consensus document (1).
Emergency care
Patient's approach
There are some pivotal indications that each healthcare worker should respect when dealing with LVAD carriers (Table 2).
- Undress the patient delicately and do not use sharp tools to remove clothes.
- Pay attention to device cables and batteries, and do not use potentially damaging tools (e.g., scissors and scalpel).
- Check that batteries are connected to cables and are correctly working.
- The cardiologist in charge of the coronary care unit (CCU) must be immediately notified of the patient's admission and should take charge of the patient.
- Contact the LVAD reference regional center (telephone number list in the CCU).
- Invite the parent with LVAD to participate (if they are absent, call them quickly).
- Make sure that the patient is provided with an extra battery.
Almost all patients with LVADs have a small tag on their controllers that indicate specific devices, the center of implantation, and an emergency phone number. It is paramount in an emergency to focus on the color of the tag, which could rapidly lead to recognize the type of device, since each color is paired with a specific device following the emergency medical services (EMS) guide (10). Currently, the most widely used devices are HeartMate III, Jarvik 2000, and Heartware. Even if different devices share some characteristics and possible management, there are significant differences from technical to practical aspects, which are fully presented in Table 3.
Clinical evaluation and advanced cardiovascular life support algorithm
Figure 1 shows a practical algorithm to be followed in case of emergency in patients with LVAD (11).
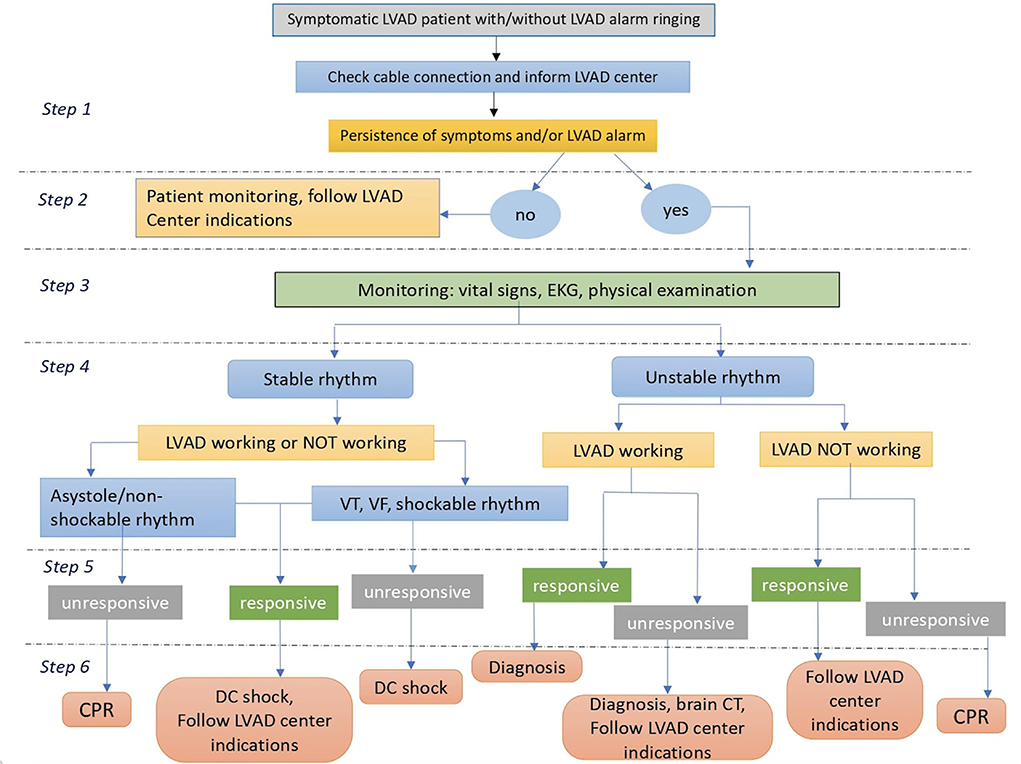
Figure 1. An algorithm for emergency management of patients with LVAD. CPR, cardiopulmonary resuscitation; DC, direct current; LVAD, left ventricular assist device; VF, ventricular fibrillation; VT, ventricular tachycardia; ED, emergency department.
The healthcare worker conducting the clinical evaluation must remember that:
- The patient could have no pulse (LVAD flow could continue, therefore not pulsatile).
- Heart rate at electrocardiogram (ECG) could differ from those evaluated with a pulse if the device has a continuous flow and is not synchronized with the heart rate.
- Blood pressure (BP) assessment could be challenging in the absence of pulsatile blood flow. Arterial BP could be measured manually using the sphygmomanometer (also with Doppler assistance) with the first audible Korotkoff tone corresponding to the medium BP or using an invasive system of BP monitoring. A medium BP value between 70 and 90 mmHg is indicated.
- Pulse oximeter could be less accurate for estimating oxygen blood saturation.
- Heart auscultation is anomalous; heart sounds are partially concealed by continuous LVAD noise. The absence of continuous LVAD noise could indicate a device dysfunction.
Just after the clinical evaluation, the CCU nurse should be informed to check the availability of beds in the CCU. Remember not to stop anticoagulation therapy unless indicated by the CCU cardiologist. The patient should be transferred to the CCU as soon as possible, unless clinical conditions require immediate treatment or urgent transfer to an LVAD center.
If required, resuscitation maneuvers start immediately following the advanced cardiovascular life support (ACLS) LVAD algorithm. Remember that resuscitation maneuvers can provoke LVAD cannula displacement (particularly cannulas positioned at the apex of the left ventricle and in the aorta), leading to sudden death. Therefore, the use of these maneuvers is permitted only in extreme situations as a last chance after excluding other resolvable causes of circulatory arrest. Electrical cardioversion and defibrillation are possible with any device. When performing electrical cardioversion or defibrillation, care should be taken not to place metal plates in a position corresponding to the device. However, aggressive treatment of arrhythmias in asymptomatic patients should be avoided. All drugs listed in ACLS could be administered.
Further assessments
Additional assessments may be required to get to the root of the problem. These include:
a) Laboratory data: A complete blood count should be routinely performed, along with other assessments such as lactate dehydrogenase (LDH), haptoglobin, plasma free hemoglobin, troponin, and brain natriuretic peptide (BNP/N-terminal-pro-BNP) coagulation panel. Anemia may be indicative of ongoing bleeding or hemolysis if accompanied by an increase in LDH and free hemoglobin and a decrease in haptoglobin levels. Of note, hemolysis is often due to pump thrombosis in LVAD carriers, so it should be carefully excluded (12–15). On the other hand, abnormalities in the coagulation panel may support a diagnosis of pump thrombosis, if clinically suspected. Also, BNP/NT-pro-BNP could be elevated in this case, as well as in case of device malfunction or a new onset right HF (16–20). Troponin elevation can be found in multiple scenarios and should be specifically requested in case of new onset angor, dyspnea, or new alterations on the ECG.
b) Arterial blood gas analysis: To assess the presence of acidemia. Please consider that arterial puncture will not be easy as usual because the pulse is often diminished and the patients are always on anticoagulation therapy.
c) Imaging:
▪ Chest X-Ray: Easily available and helpful to evaluate pump and inflow–outflow cannula position (11).
▪ Echocardiography: Important to analyze pump flow, possible thrombosis, mechanical complications, LV hemodynamic conditions and filling, and valvular regurgitation [aortic regurgitation can frequently occur in patients with continuous LVAD flow due to multiple factors such as LV unloading (9)]. If available, it is important to perform bedside echocardiography to help focus the diagnosis. Figure 2 shows an algorithm to speed up diagnosis and treatment of the emergence of LVAD starting from echocardiographic findings (15, 16, 21).
▪ Computed tomography (CT): It could help evaluate areas not visible by echocardiography, such as outflow pump cannula position, and the lack of information due to the poor acoustic window in these patients (22, 23). Moreover, cranial acquisition is crucial in case of suspected stroke, to differentiate hemorrhagic from ischemic ones.

Figure 2. An algorithm for the differential diagnosis and treatment of LVAD emergencies that represent an important added value of performing bedside echocardiography. JVP, jugular venous pressure; LV, left ventricle; LVAD, left ventricle assist device; OTI, intubation orotracheal; PDE, phosphodiesterase; PE, pulmonary embolism; PH, pulmonary hypertension; RV right ventricle.
Remember that magnetic resonance imaging (MRI) is contraindicated in patients with LVAD.
Roles and responsibilities
Each healthcare worker plays a specific role in emergency care as described above.
Role of the medical director
a) To ensure the distribution of this document and the comprehension of its content with reference to all possible participants in the management of patients with LVAD.
b) To organize a systematic pathway between LVAD centers and the local hospital to identify all patients with old and new LVAD implantations possibly pertaining to that area.
A list of LVAD carriers should be placed in a dedicate folder and stored in the ED or CCU.
Role of the HF and LVAD multidisciplinary team
A) To ensure continuous update of this document based on the newest evidence.
B) To supervise compliance and correct application of the following procedure when a patient with LVAD is referred to the local hospital.
C) To verify that each patients with LVAD has been correctly identified in the medical records and marked as an “LVAD carrier.”
D) To provide a promptly available list of all national LVAD reference centers (to be stored in the CCU).
Role of the physician who is in charge of a patient with LVAD
A) Inform the CCU referral cardiologist of the admission of a patient with LVAD.
B) To ensure that the HF and LVAD multidisciplinary team has been informed of the admission of a patient with LVAD.
C) To apply the management algorithm reported in Figure 1.
D) To ensure that a phone contact of the closest LVAD reference center is present and that all information about emergency phone numbers, emergency instructions, and battery supply of the device is available to healthcare workers.
E) To ensure systematic follow-up of the patient after discharge [following existing models in other clinical settings (24, 25)] following the Hub–Spoke model in collaboration with the LVAD reference center.
Role of the CCU team
A) If required, to draw up an appropriate treatment plan that integrates clinical and nursing roles for the care of patients with LVAD.
B) To facilitate a timely transfer and admission of the patient with LVAD from the ED to the CCU.
C) To ensure that this protocol is followed specifically in case of the admission of a patient with LVAD.
D) To inform the LVAD implantation center of the patient's hospitalization as soon as possible (using the phone contacts on the list stored in the CCU-point D in paragraph 2.2).
Role of biomedical engineer
A) Be available for any technical consultation in case of a device malfunction that is not clearly identifiable.
B) Provide technical indications for solving the problem.
Role of nurse care manager
A) Build up and lead the development of a comprehensive, individualized care plan for each hospitalized patient.
B) Contribute to the education of patients and their families by having them fully understand their clinical condition, manage the symptoms associated with their condition, and understand treatment alternatives.
C) Address nonclinical issues that impact quality of life and outcome.
Role of clinicians and nurses in the other departments in which patients with LVAD could be admitted (e.g., surgical department, neurologic department, and so on)
A) Inform the CCU referral cardiologist immediately (if not already done).
B) To ensure that each healthcare operator of the ward is aware of this document.
C) To monitor strict compliance with the advice contained in this document.
Role of each healthcare professional
A) To be aware of the procedures explained in this document.
B) To perform them correctly in case of the admission of the patient with LVAD.
Conclusions
The growing use of LVAD implantation as destination therapy worldwide has resulted in the need of specific training for clinicians of all specialties to manage patients with LVAD. Particularly, in the emergency setting, a standardized multidisciplinary approach and collaboration between small and VAD centers are essential to ensure the best treatment for patients. This document offers an easy consultation and practical guide for the appropriate management of emergencies in patients with LVAD.
Author contributions
MC, MP, and SV had the idea for this paper. MC, MP, GM, and FL performed the literature search and analysis and drafted the manuscript. ML, LC, CT, MM, SB, FD'A, MF, and SV critically revised the work. All authors contributed to this review conception. All authors have read and approved the final manuscript.
Acknowledgments
The Authors thank the University of Siena for the contribution to open access publishment.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Potapov EV, Antonides C, Crespo-Leiro MG, Combes A, Färber G, Hannan MM, et al. 2019 EACTS expert consensus on long-term mechanical circulatory support. Eur J Cardiothorac Surg. (2019) 56:230–70. doi: 10.1093/ejcts/ezz098
2. Crespo-Leiro MG, Metra M, Lund LH, Milicic D, Costanzo MR, Filippatos G, et al. Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. (2018) 20:1505–35. doi: 10.1002/ejhf.1236
3. Mehra MR, Uriel N, Naka Y, Cleveland JC Jr, Yuzefpolskaya M, Salerno CT, et al. MOMENTUM 3 Investigators. A fully magnetically levitated left ventricular assist device - final report. N Engl J Med. (2019) 380:1618–27. doi: 10.1056/NEJMoa1900486
4. Yin MY, Strege J, Gilbert EM, Stehlik J, McKellar SH, Elmer A, et al. Impact of shared care in remote areas for patients with left ventricular assist devices. JACC. (2020):302–12. doi: 10.1016/j.jchf.2020.01.004
5. Tainter CR, Braun OÖ, Teran F, Nguyen AP, Robbins K, O'Brien EO, et al. Emergency department visits among patients with left ventricular assist devices. Intern Emerg Med. (2018) 13:907–13. doi: 10.1007/s11739-017-1776-8
6. Long B, Robertson J, Koyfman A, Brady W, et al. Left ventricular assist devices and their complications: a review for emergency clinicians. Am J Emerg Med. (2019) 37:1562–70. doi: 10.1016/j.ajem.2019.04.050
7. Givertz MM, DeFilippis EM, Colvin M, Darling CE, Elliott T, Hamad E, et al. HFSA/SAEM/ISHLT clinical expert consensus document on the emergency management of patients with ventricular assist devices. J Heart Lung Transplant. (2019) 38:677–98. doi: 10.1016/j.healun.2019.05.004
8. Ben Gal T, Ben Avraham B, Milicic D, Crespo-Leiro MG, Coats AJS, Rosano G, et al. Guidance on the management of left ventricular assist device (LVAD) supported patients for the non-LVAD specialist healthcare provider: executive summary. Eur J Heart Fail. (2021) 23:1597–609. doi: 10.1002/ejhf.2327
9. Teuteberg JJ, Cleveland JC Jr, Cowger J, Higgins RS, Goldstein DJ, Keebler M, et al. The society of thoracic surgeons intermacs 2019 annual report: the changing landscape of devices and indications. Ann Thorac Surg. (2020) 109:649–60. doi: 10.1016/j.athoracsur.2019.12.005
10. Bouabdallaoui N, El-Hamamsy I, Pham M, Giraldeau G, Parent MC, Carrier M, et al. Aortic regurgitation in patients with a left ventricular assist device: a contemporary review. J Heart Lung Transplant. (2018) 37:1289–97. doi: 10.1016/j.healun.2018.07.002
11. International Consortium of Circulatory Assist Clinicians. EMS Guide 2016. Available online at: https://www.mylvad.com/sites/default/files/MCSO%20EMS%20GUIDE%20New%20Cover.pdf
12. Bowles CT, Hards R, Wrightson N, Lincoln P, Kore S, Marley L, et al. Algorithms to guide ambulance clinicians in the management of emergencies in patients with implanted rotary left ventricular assist devices. Emerg Med J. (2017) 34:842–50. doi: 10.1136/emermed-2016-206172
13. Shah P, Mehta VM, Cowger JA, Aaronson KD, Pagani FD, et al. Diagnosis of hemolysis and device thrombosis with lactate dehydrogenase during left ventricular assist device support. J Heart Lung Transplant. (2014) 33:102–4. doi: 10.1016/j.healun.2013.07.013
14. Goldstein DJ, Ranjit J, Salerno C, Silvestry S, Moazami N, Horstmanshof D, et al. Algorithm for the diagnosis and management of suspected pump thrombus. J Heart Lung Transplant. (2013) 32:667–70. doi: 10.1016/j.healun.2013.05.002
15. Tchantchaleishvili V, Sagebin F, Ross RE, Hallinan W, Schwarz KQ, Massey HT, et al. Evaluation and treatment of pump thrombosis and hemolysis. Ann Cardiothorac Surg. (2014) 3:490–5. doi: 10.3978/j.issn.2225-319X.2014.09.01
16. Robertson J, Long B, Koyfman A. The emergency management of ventricular assist devices. Am J Emerg Med. (2016) 34:1294–301. doi: 10.1016/j.ajem.2016.04.033
17. Trinquero P, Pirotte A, Gallagher LP, Iwaki KM, Beach C, Wilcox JE. Left ventricular assist device management in the emergency department. West J Emerg Med. (2018) 19:834–41. doi: 10.5811/westjem.2018.5.37023
18. Brady W, Weigand S, Bergin J. Ventricular assist device in the emergency department: evaluation and management considerations. AJEM. (2018) 36:1295–9. doi: 10.1016/j.ajem.2018.04.047
19. Greenwood JC, Herr DL. Mechanical circulatory support. Emerg Med Clin North Am. (2014) 32:851–69. doi: 10.1016/j.emc.2014.07.009
20. Klein T, Jacob MS. Management of implantable assisted circulation devices: emergency issues. Cardiol Clin. (2012) 30:673–82. doi: 10.1016/j.ccl.2012.07.003
21. Stainback RF, Estep JD, Agler DA, Birks EJ, Bremer M, Hung J, et al. Echocardiography in the management of patients with left ventricular assist devices: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. (2015) 28:853–091. doi: 10.1016/j.echo.2015.05.008
22. Gill GS, Weissman G, Meirovich YF, Medvedofsky D, Mohammed SF, Waksman R, et al. Reproducibility of semi-automated three-dimensional volumetric analysis using cardiac computed tomography in patients with left ventricular assist device. Cardiovasc Revasc Med. (2019) 20:381–6. doi: 10.1016/j.carrev.2019.01.024
23. Weigold WG, Verdun V. Left ventricular assist device evaluation using cardiac CT: initial experience at a high volume center. J Am Coll Cardiol. (2017) 69:1438. doi: 10.1016/S0735-1097(17)34827-1
24. Locuratolo N, Scicchitano P, Antoncecchi E, Basso P, Bonfantino VM, Brescia F, et al. Follow-up del paziente dopo sindrome coronarica acuta: il progetto PONTE-SCA Puglia [Follow-up of patients after an acute coronary event: the Apulia PONTE-SCA program]. G Ital Cardiol (Rome). (2022) 23:63–74. doi: 10.1714/3715.37064
Keywords: emergency, heart failure, urgency, LVAD (left ventricular assist device), mechanical circulatory support (MCS)
Citation: Cameli M, Pastore MC, Mandoli GE, Landra F, Lisi M, Cavigli L, D'Ascenzi F, Focardi M, Carrucola C, Dokollari A, Bisleri G, Tsioulpas C, Bernazzali S, Maccherini M and Valente S (2022) A multidisciplinary approach for the emergency care of patients with left ventricular assist devices: A practical guide. Front. Cardiovasc. Med. 9:923544. doi: 10.3389/fcvm.2022.923544
Received: 19 April 2022; Accepted: 21 June 2022;
Published: 22 August 2022.
Edited by:
Laurens F. Tops, Leiden University Medical Center, NetherlandsReviewed by:
Marco Matteo Ciccone, University of Bari Aldo Moro, ItalyAlan Gallingani, University Hospital of Parma, Italy
Copyright © 2022 Cameli, Pastore, Mandoli, Landra, Lisi, Cavigli, D'Ascenzi, Focardi, Carrucola, Dokollari, Bisleri, Tsioulpas, Bernazzali, Maccherini and Valente. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Concetta Pastore, cGFzdG9yZTI0MTFAZ21haWwuY29t
†These authors have contributed equally to this work and share first authorship
 Matteo Cameli
Matteo Cameli Maria Concetta Pastore
Maria Concetta Pastore Giulia Elena Mandoli
Giulia Elena Mandoli Federico Landra1
Federico Landra1