- 1Division of Cardiology, Pederzoli Hospital-Peschiera del Garda, Verona, Italy
- 2Division of Cardiology, Nanjing First Hospital, Nanjing Medical University, Nanjing, China
- 3Division of Cardiology, Medistra Hospital, University of Indonesia Medical School, Jakarta, Indonesia
- 4Division of Cardiology, Binawaluya Cardiac Center, Jakarta, Indonesia
Background: Provisional stenting (PS) is the main treatment for a majority of coronary bifurcation lesion and includes PS with 1-stent and PS with 2-stent. However, the treatment difference between PS with 1-stent and with 2-stent remains unclear in patients with the acute coronary syndrome (ACS) and coronary bifurcation lesions.
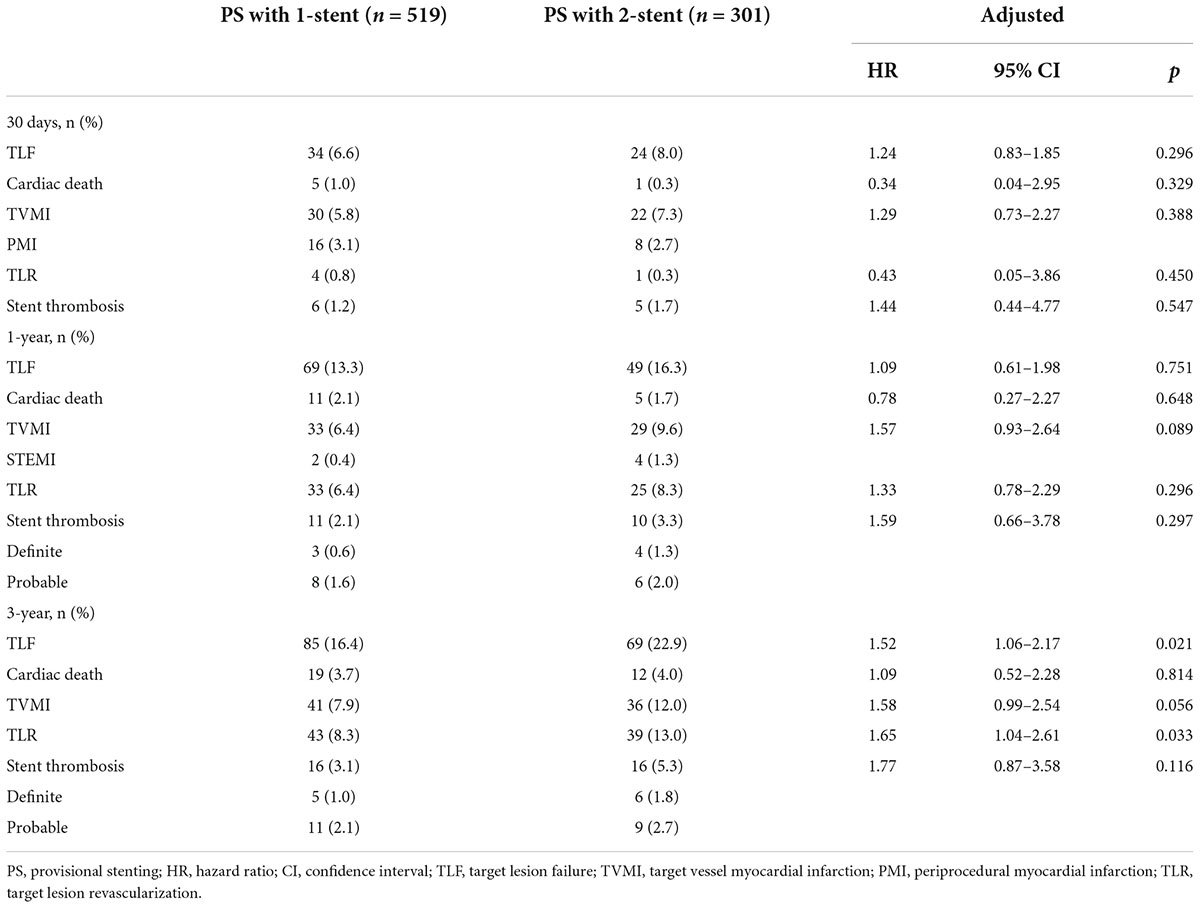
Materials and methods: Overall, 820 ACS patients with Medina 1,1,1 or 0,1,1 coronary bifurcation lesion who had completed 3-year follow-up were included and assigned to the PS with 1-stent (n = 519) or the PS with 2-stent (n = 301) according to the use of final stenting technique. The primary endpoint was the target lesion failure (TLF) at 3 years since stenting procedures.
Results: At 3-year follow-up, TLF occurred in 85 (16.4%) patients in the PS with 1-stent group and 69 (22.9%) in the PS with 2-stent group (hazard ratio [HR] 1.52, 95% confidence interval [CI] 1.06–2.17, p = 0.021), mainly driven by a higher rate of target lesion revascularization (TLR) in the PS with 2-stent group (13.0% vs. 8.3%, HR 1.65, 95% CI 1.04–2.61, p = 0.033). Complex bifurcations, side branch (SB) pretreatment, intravascular imaging guidance, and hyperlipidemia were the four predictors for 3-year TLF. SB pretreatment was associated with increased 3-year TLR, leading to an extremely higher 3-year TLF.
Conclusion: Provisional with 2-stent for patients with ACS is associated with a higher rate of 3-year TLF, mainly due to increased requirement of revascularization. SB pretreatment should be avoided for simple bifurcation lesion.
Introduction
Coronary artery bifurcation lesions involve three vessel segments (proximal main vessel [MV], distal MV, and side branch [SB]), leading to technical challenging of bifurcation stenting and suboptimal clinical outcomes (1, 2). While upfront two-stent approach (like DK crush stenting) has been demonstrated to be associated with less rate of target lesion failure (TLF) for the treatment of patients with bifurcation lesions localizing at distal left main (LM) or having higher complexity (3, 4), provisional stenting (PS) is still accepted to be a major technique for simple bifurcation lesions (2, 5–7). PS requires a jailed wire or balloon in the SB, which could rescue an SB at risk of occlusion after stenting MV. Thus, PS could be shifted to PS with 1-stent or PS with 2-stent, with a rate of crossover to 2-stent varying from 2 to 40% (2, 4–9), depending on the performance of SB pretreatment and final kissing balloon inflation (KBI), lesions’ complexity, flow-limiting dissection, severely compromised ostial SB induced by plaque or carina shifting, and criteria for treating SB in clinical trials. As a result, PS with SB rescue stenting is unavoidable for complex bifurcations (4, 9). However, there is a paucity of data showing the difference in clinical outcomes between PS with 1-stent and PS with 2-stent among patients with acute coronary syndrome (ACS) and bifurcation lesions. Accordingly, this study includes all ACS patients with bifurcations who underwent the PS approach and had completed 3-year clinical follow-up from previous four trials (4, 9–11) with a view to identify the rate of crossover to 2-stent, the difference in 3-year TLF between PS with 1-stent and with 2-stent, and the independent factors of 3-year TLF.
Materials and methods
Study design
We included data of the following clinical trials with only Medina 1,1,1 and 0,1,1 bifurcation lesions in patients with ACS: DKCRUSH II (10), DKCRUSH V (9), DKCRUSH VI (11), and DEFINITION II (4; Figure 1). All patients were prospectively followed up till January 1, 2022. The study protocol was approved by the ethics committee at each participating center and complied with the Declaration of Helsinki. All patients provided written informed consent for participation in the respective trials. All authors had free access to the database.
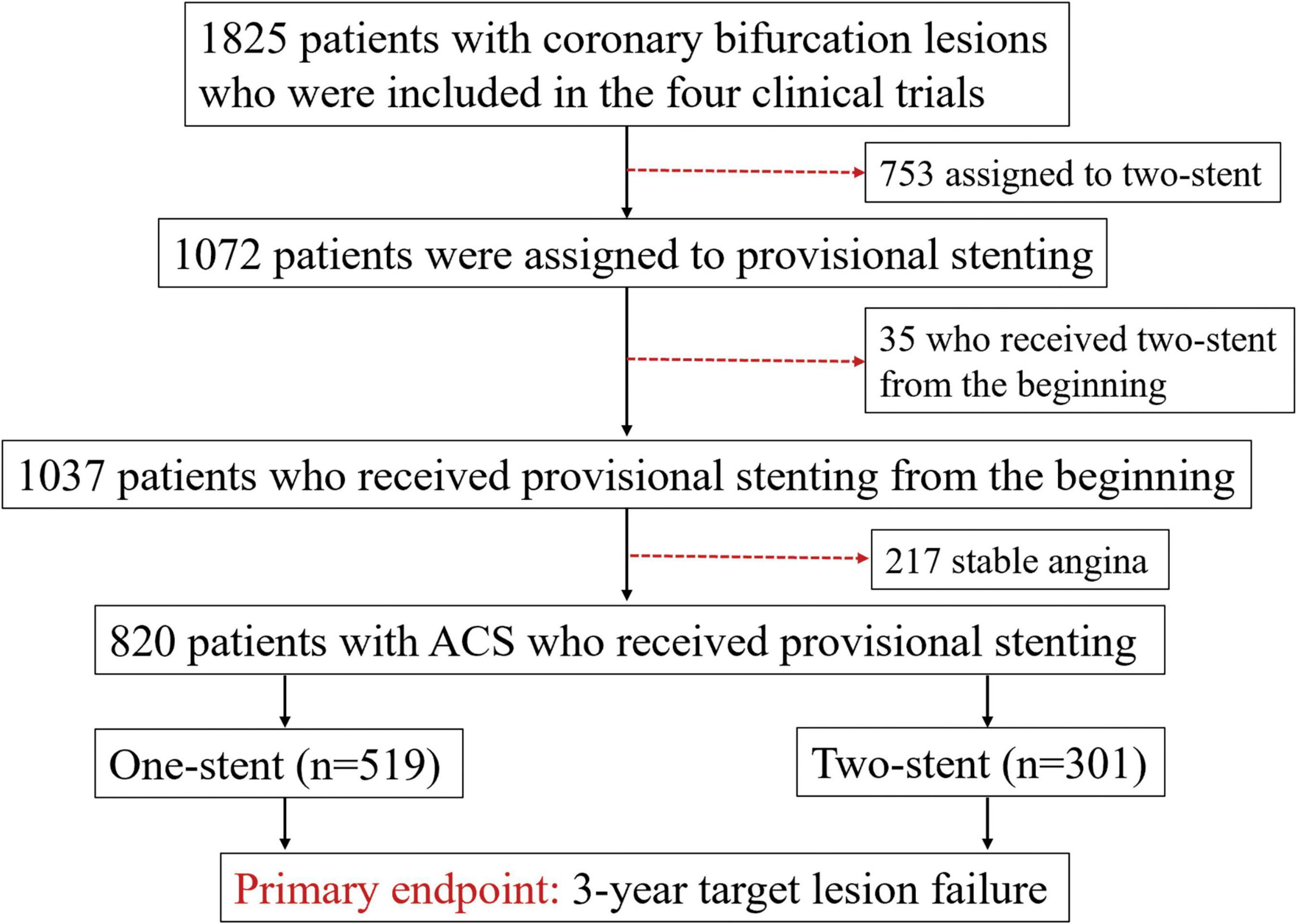
Figure 1. Study flowchart. Description: 820 patients with acute coronary syndrome (ACS) were assigned to the provisional stenting (PS) with 1-stent and the PS with 2-stent groups.
Patient population
Overall, 1,825 patients with coronary bifurcation lesions from the four clinical trials were screened. We excluded 1,005 patients because of upfront 2-stent (n = 753) at randomization, SB pretreatment leading to the urgent requirement of stenting SB before stenting the MV (n = 35), and stable angina patients (n = 217). Finally, 820 patients with ACS who underwent PS were included (Figure 1), with 519 patients assigned to the PS with 1-stent group and 301 patients assigned to the PS with 2-stent group.
Provisional stenting procedures
The PS approach has been previously described (4, 9–11). In brief, the MV and SB are wired. Predilation was left to the operator’s discretion, although predilating the SB is discouraged. A new-generation drug-eluting stent was used in the bifurcation lesions. A stent with a stent/artery ratio of 1.1:1 was implanted in the MV, and then the proximal optimization technique (POT) using non-compliant balloons (balloon/stent ratio of 1:1, > 18 atm) was performed. Ballooning or stenting the SB after MV stenting is performed only if the SB ostium is severely compromised or has a Type B/C dissection or thrombolysis in myocardial infarction (TIMI) flow < 3. If SB dilatation or stenting is required, the SB is rewired through a distal cell of the MV stent, followed by re-POT, KBI, and final POT using non-compliant balloons with a suggested inflation pressure of >18 atm.
Medications and follow-up
All patients were treated with aspirin preprocedure and 300 mg loading dose of clopidogrel or 180 mg ticagrelor if they were not under chronic dual antiplatelet therapy (DAPT). After the intervention, they received 100 mg/day aspirin indefinitely and 75 mg/day clopidogrel or 180 mg (90 mg, bid) ticagrelor for at least 12 months. A clinical follow-up was performed at 1 and 12 months and annually subsequently through 3 years.
Follow-up coronary angiography was scheduled at 13 months (after ascertainment of the primary clinical endpoint) unless performed earlier for clinical indications. Quantitative coronary analysis (QCA) was analyzed at a central core laboratory using the Cardiovascular Angiographic Analysis System (CAAS) II software (Pie Medical Imaging, The Netherlands), as previously described (4). Restenosis was defined as a QCA DS > 50% at follow-up.
Endpoints and definitions
The primary endpoint was TLF at 3 years, defined as the composite of cardiac death, target vessel MI (TVMI), or clinically driven TLR. Death from cardiac causes was defined as any death without a clear non-cardiac cause. Protocol-defined periprocedural MI (within 48 h) was defined as a creatine kinase-MB (CK-MB) > 10 × upper reference limit (URL) of the assay or > 5 × URL plus either (1) new pathological Q waves in ≥ 2 contiguous leads or new left bundle branch block (LBBB); (2) angiographically documented graft or coronary artery occlusion or new severe stenosis with thrombosis; (3) imaging evidence of new loss of viable myocardium; or (4) new regional wall motion abnormality. Spontaneous MI (after 48 h) was defined as a clinical syndrome consistent with MI with a CK-MB or troponin > 1 × URL and new ST-segment elevation or depression or other findings as above. All MIs were considered TVMI unless there was clear evidence that they were attributable to a non-target vessel (4, 12). Clinically driven TLR was defined as angina or ischemia referable to the target lesion requiring repeat PCI or coronary artery bypass graft. Secondary endpoints included cardiac death, TVMI, clinically driven TLR, and stent thrombus (ST). Definite or probable ST according to the Academic Research Consortium (13) was the major safety endpoint. All events were adjudicated by a central committee using original source documents blinded to the treatment.
Statistical analysis
Baseline characteristics are reported as counts and percentages or mean ± standard deviation (SD). The chi-squared or Fisher’s exact test was used to compare categorical variables. Student’s t-test or Wilcoxon rank-sum scores for non-normally distributed data were used to compare continuous variables. Time-to-first event curves were generated using Kaplan–Meier analysis and compared using the log-rank test. Cox regression was also used to compare the differences in both primary and secondary endpoints, with outputs of hazard ratio (HR), 95% confidence interval (CI), and p-value. Multivariate analysis was performed to identify the independent factors of 3-year TLF. All statistical tests were two-sided, and a p-value of <0.05 was considered statistically significant. All analyses were performed using SPSS version 26.0 (SPSS Institute Inc., Chicago, Illinois, USA).
Results
Baseline clinical characteristics
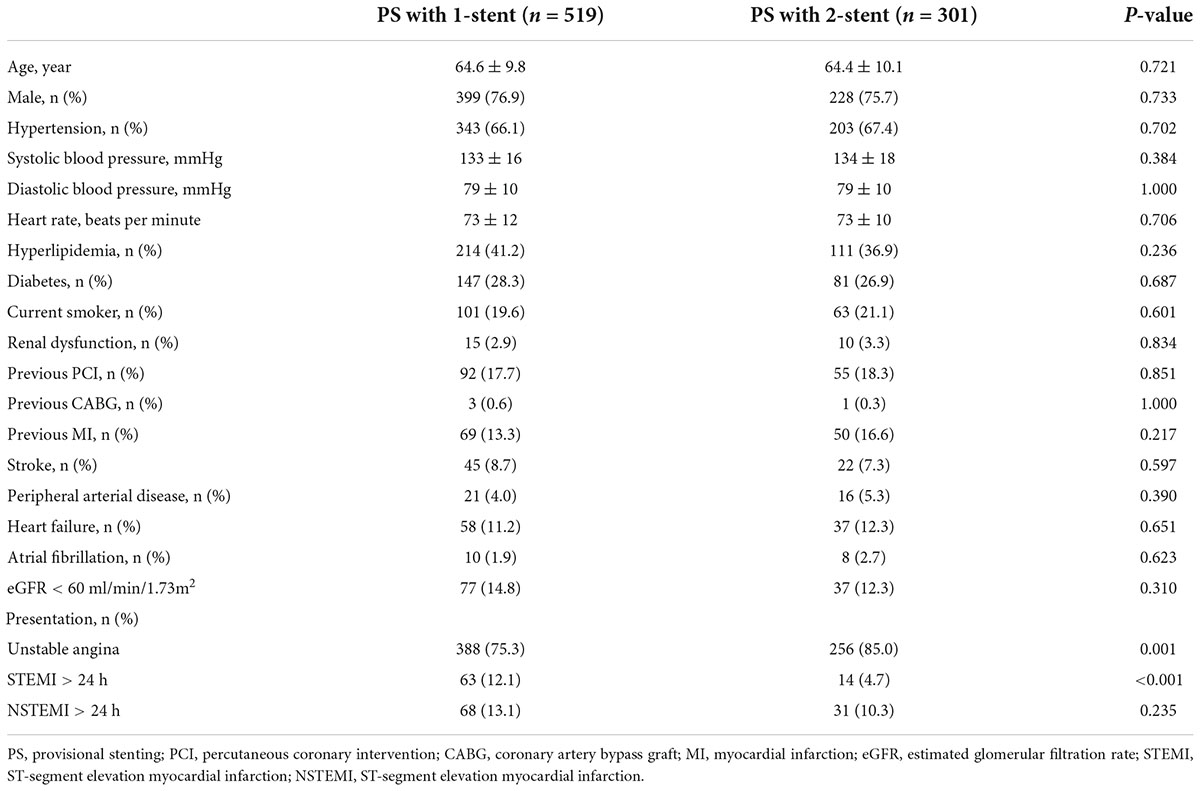
Baseline clinical characteristics were well comparable between the groups (Table 1), except for unstable angina (85.0% in the 2-stent group vs. 75.3% in the 1-stent group, p = 0.001) and ST-segment elevation MI (4.7% in the 2-stent group vs. 12.1% in the 1-stent group, p < 0.001). Diabetes was present in 27.6% of patients.
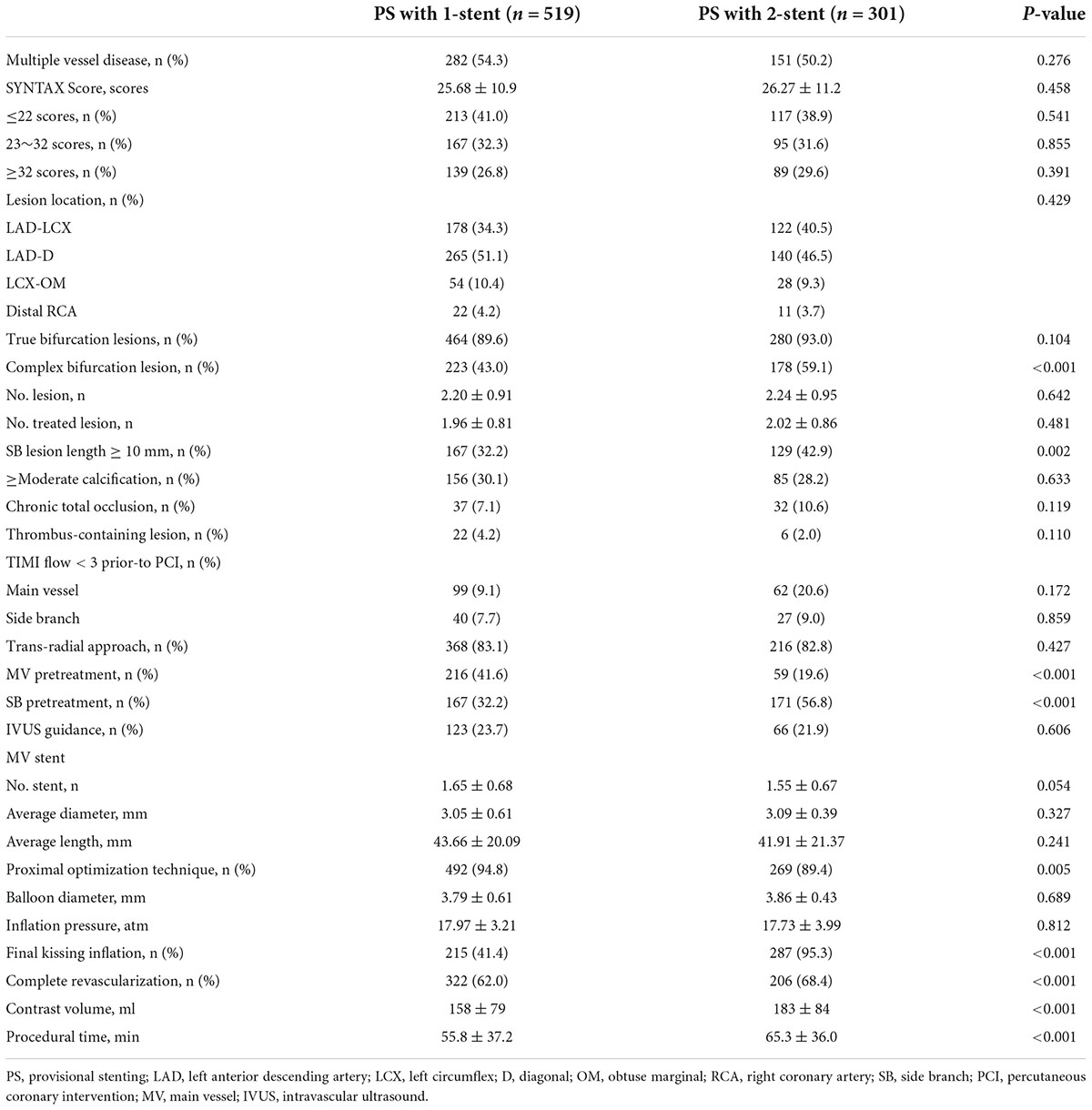
Lesion characteristics and procedures
Multivessel disease was present in 52.2% of patients, and the mean SYNTAX score was 26 (Table 2). Notably, 37.4% of the lesions were localized in the distal LM. Complex bifurcation lesions were seen in 59.1% of patients in the 2-stent group, compared to 43.0% in the 1-stent group (p < 0.001), with an extremely higher rate of SB lesion length ≥ 10 mm in the 2-stent group (42.9% vs. 32.2%, p = 0.002), as confirmed by the QCA analysis (Table 3).
The trans-radial approach was predominantly used (82%, Table 2). In the 2-stent group, SB pretreatment was used in 56.8%, significantly different from 32.2% in the 1-stent group (p < 0.001), resulting in more frequent use of KBI in the 2-stent group (95.3 vs. 41.4%, p < 0.001). Final POT was only used in 89.4% of patients in the 2-stent group, lower than 94.8% in the 1-stent group (p < 0.001). Complete revascularization was achieved in 68.4% of patients in the 2-stent group, compared to 62.0% in the 1-stent group (p < 0.001). IVUS guidance was only used in <30.0% of patients, without a significant difference between the groups. The two-stent strategy was associated with longer procedural time and more contrast volume compared with the PS with 1-stent approach.
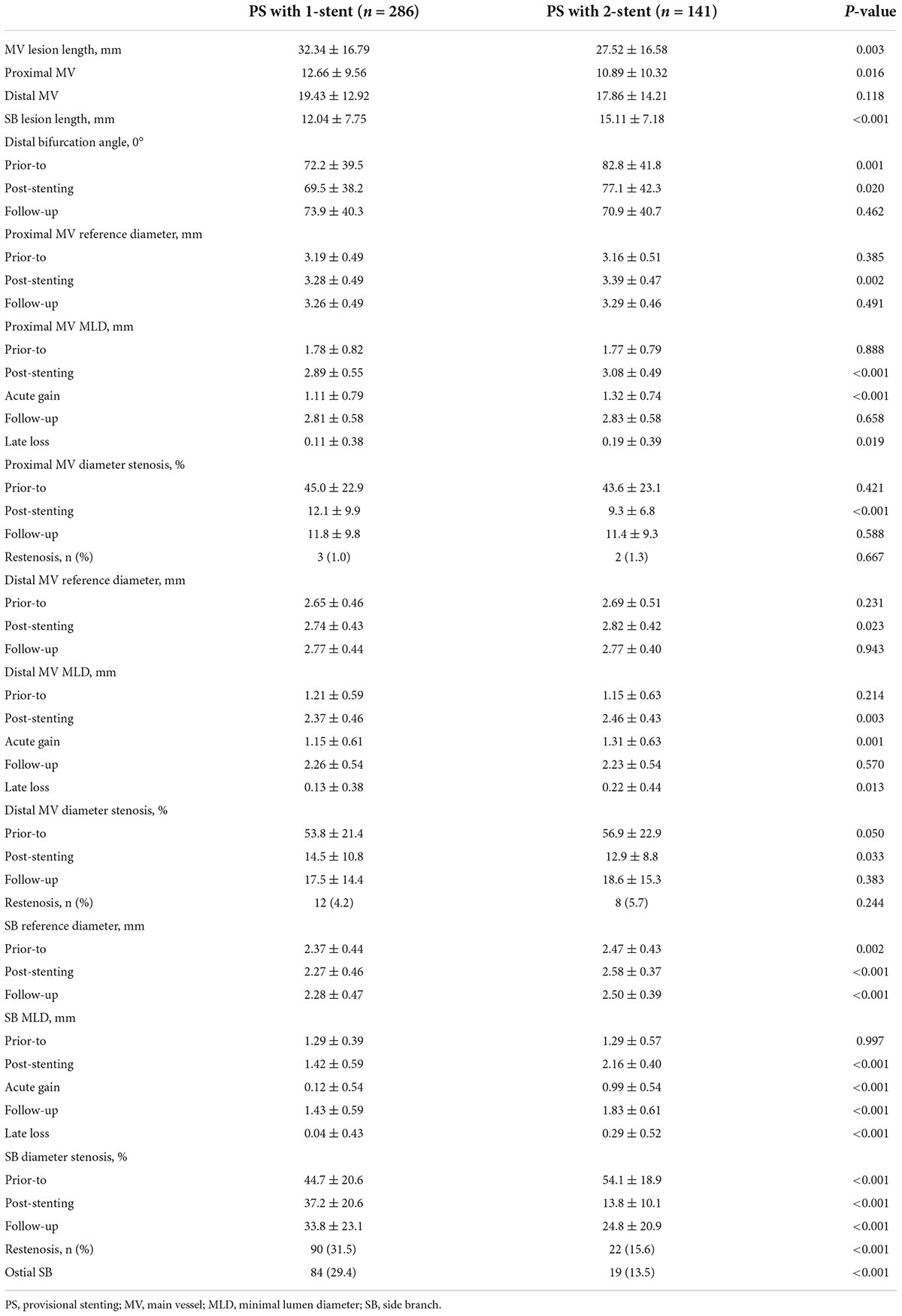
Quantitative coronary analysis
Except for longer SB lesion length, the 2-stent group also had a more severe SB diameter stenosis (54.1 vs. 44.7%, p < 0.001) at baseline. At 3 years since procedures, a total of 427 (52.1%) patients underwent repeat angiography, with 246 (30.0%) at 13 months and 181 (22.1%) after 13 months. The in-stent restenosis (ISR) rate in the MV was non-significantly different between the 2 groups (Table 3). In the 2-stent group, the rate of ISR at the ostial SB was 13.3%, compared to 29.4% in the 1-stent group (p < 0.001).
Clinical outcomes
At 3 years, DAPT was prescribed to 203 (39.1%) patients in the PS with 1-stent and 198 (65.8%) in the PS with 2-stent (p < 0.001). Ticagrelor (90 mg; twice a day) was administered in 58.6% of patients in the PS with 2-stent group and 38.2% in the PS with 1-stent group (p < 0.001).
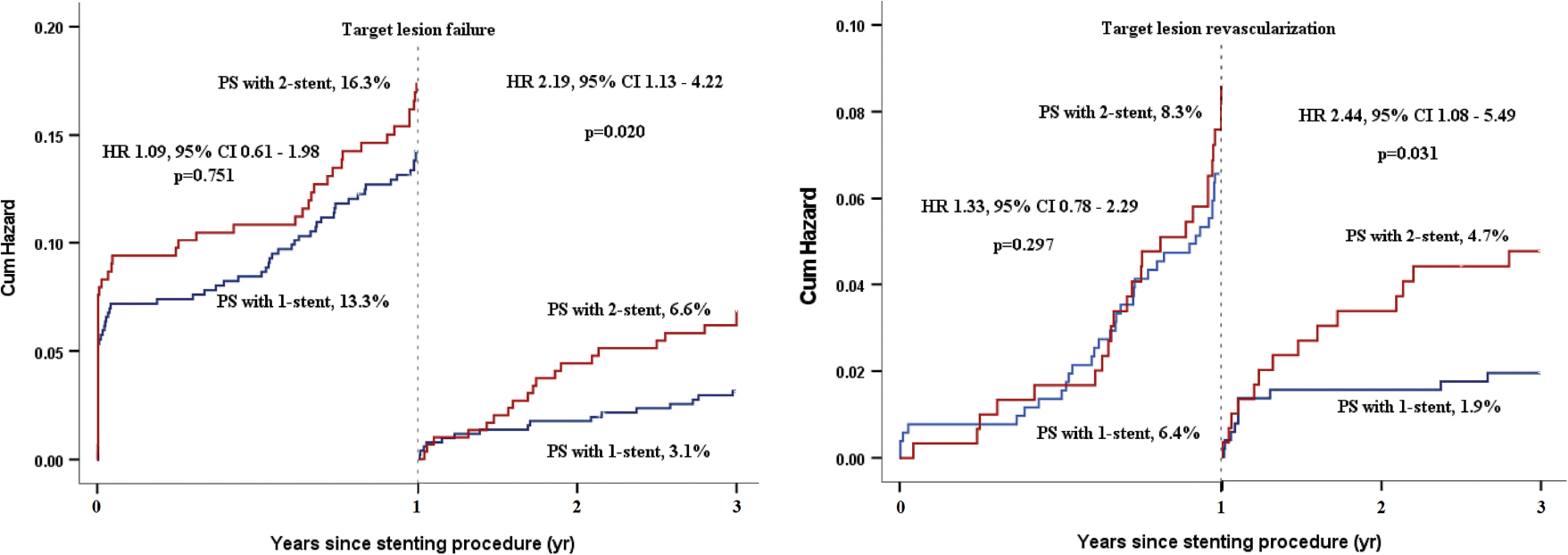
A 1-year clinical follow-up was completed in all patients. The primary endpoint of TLF at 1 year occurred in 69 (13.3%) patients in the PS with 1-stent group and 49 (16.3%) patients in the PS with 2-stent group (HR 1.09, 95% CI 0.61–1.98, p = 0.751) (Table 4). The rates of TVMI, cardiac death, TLR, and ST at 1 year were also non-significantly different between the two groups.
At 3 years, 12 (1.6%) patients were lost to the follow-up, with 7 (2.3%) in the PS with 2-stent group and 5 (0.9%) in the PS with 1-stent group. TLF at 3 years occurred in 85 (16.4%) patients in the PS with 1-stent group and 69 (22.9%) in the PS with 2-stent group (HR 1.52, 95% CI 1.06–2.17, p = 0.021, Table 4 and Figure 2A), mainly driven by increased TLR (8.3% vs. 13.0%, HR 1.65, 95% CI 1.04–2.61, p = 0.033, Table 4 and Figure 2B), without statistical differences in cardiac death, TVMI, and ST. By landmark analysis (Graphic Abstract), the rates of TLF and TLR at 1 year were comparable between PS with 1-stent and PS with 2-stent; however, the increased rate of TLR from year 1 to year 3 was 3.5% in the PS with 2-stent group (4.7 vs. 1.9%, HR 2.44, 95% CI 1.08–5.49, p = 0.031, Graphic Abstract), resulted in a significant difference in TLF after 1 year between the PS with 2-stent (6.6%) and the PS with 1-stent (3.1%, HR 2.19, 95% CI 1.13–4.22, p = 0.020).
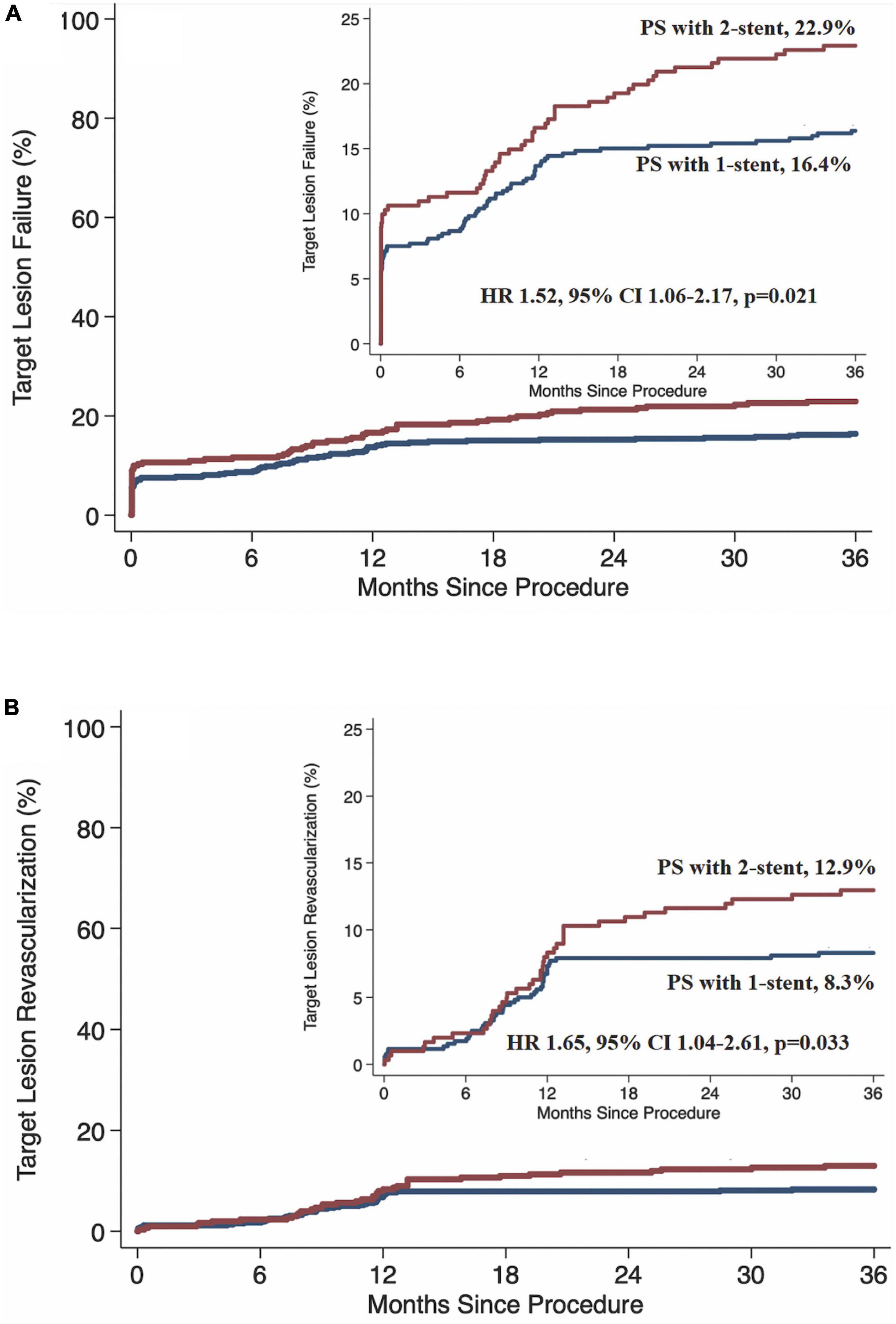
Figure 2. Kaplan–Meier survival rate. PS, provisional stenting; HR, hazard ratio; CI, confidence interval. (A) Target lesion failure. (B) Target lesion revascularization.
By multivariate analysis, SB pretreatment (HR 1.66, 95% CI 1.19–2.31, p = 0.003), complex bifurcation lesions (HR 2.76, 95% CI 1.42–5.38, p = 0.003), without intravascular imaging (HR 1.51, 95% CI 1.07–2.14, p = 0.020), and hyperlipidemia (HR 1.15, 95% CI 1.04–1.88, p = 0.006) were the four independent factors of 3-year TLF. SB pretreatment was performed because operators were worried about the abrupt closure of an SB after ballooning or stenting MV. Supplementary Table 1 shows that the SB pretreatment subgroup had a longer lesion length (mean length of 14.47 vs. 12.25 mm, p = 0.001) and more severe disease (mean diameter stenosis of 51.99 vs. 42.96%) in the SB compared to those in the non-pretreatment subgroup. Subsequent clinical follow-up demonstrated a higher rate of 30-day PMI (8.6%) in the SB pretreatment subgroup, compared to 4.8% (p = 0.036) in the non-pretreatment subgroup. At 1- and 3-year follow-up, the increased rates of TVMI and TLR in the PS with 2-stent group led to significantly different TLF rates in the pretreatment subgroup (18.9 and 24.6%) when compared with 11.2% (p = 0.002) and 14.7% (p = 0.001) in the non-pretreatment subgroup, respectively (Supplementary Figure 1).
Discussion
This analysis for the first time compared the difference in clinical outcome between the PS with 1-stent and the PS with 2-stent for patients with ACS. The major findings are (1) PS with 2-stent is associated with a higher rate of TLF at 3-year follow-up, largely driven by an increased 3-year rate of TLR, compared to those in the PS with 1-stent group; (2) by multivariate analysis, SB pretreatment, complex bifurcation lesions, without intravascular imaging, and hyperlipidemia were the four independent factors of 3-year TLF; and (3) the rate of TLF at 3-year follow-up in the SB pretreatment subgroup is significantly higher than that in the no pretreatment subgroup, mainly induced by the extreme increments in TVMI and TLR.
The PS with 2-stent is a rescue strategy for SB and reduces the incidence of SB occlusion and PMI and is required in 2–40% of bifurcation lesion treated by provisional approach (2, 4–9). This wide discrepancy in the rate of cross-over to two stents is due to the different criteria for treating SB from previous trials (4–9). For example, SB TIMI flow < 3 was the only criterion for stenting SB in the BBC ONE trial (6), and composite criteria of TIMI flow < 3, Type B or C dissection, and severely compromised in the SB after stenting MV were more commonly used in others (2–5, 7, 9–11). While a few risk stratifications have been proposed to predict the occurrence of clinical events after the PS or upfront two-stent techniques (3, 14–16), the difference in treatment effect between the PS with 1-stent and the PS with 2-stent remained understudied. To echo this issue, Song et al. (17, 18) for the first time randomized 258 patients with a coronary bifurcation lesion to the conservative and aggressive groups according to the criteria for SB intervention after MV stenting (for non-LM bifurcations, the criterion for SB treatment was TIMI < 3 [conservative] or diameter stenosis > 75% [aggressive]; for LM bifurcation lesions, the criterion for SB treatment was diameter stenosis > 75% [conservative] or > 50% [aggressive]). The study reported that at a 3-year follow-up, the primary endpoint (target vessel failure [TVF]) occurred in 11.7% of the conservative group vs. 20.8% of the aggressive group (p = 0.049). Although no significant differences were observed in the incidence of TVF between groups at 1 year, landmark analysis between 1 and 3 years showed significantly less TVF in patients assigned to the conservative strategy (2.6 vs. 12.7%; p = 0.004). Conservative treatment for SB obviously had a less requirement of additional SB stent. However, the real difference in TVF between the PS with 1-stent and 2-stent could not be directly derived from that study with a small sample size. In this study, we found that a higher rate of 3-year TLF in the PS with 2-stent group was predominantly induced by the increased requirement of TLR after 1-year follow-up, which indicated the reduction in the durability of the second stent in the SB. While the crossover to the 2-stent technique was an independent predictor of TVF (4, 17, 18), we further found that complex bifurcation lesions, SB pretreatment, IVUS use, and hyperlipidemia were the four predictors of 3-year TLF. In this study, IVUS was only used in less than 30% of procedures; although it was equally used in the two groups, the results still recommended the importance of routine use of IVUS in improving the clinical outcome after the PS approach (19–21). In contrast, complex bifurcation defined by DEFINITION criteria (3, 4, 8) was associated with a higher rate of crossover to two stents and a subsequent increased rate of MI and TLR. As a result, an upfront two-stent approach may be an appropriate option for real complex bifurcation lesions.
Side branch pretreatment mirrors the complexity of a given bifurcation lesion, particularly in the SBs having a higher grade of diameter stenosis, as shown by our data. To answer the correlation of the SB pretreatment with increased TVF, Song et al. (22) reported that an additional SB stent was frequently required in the SB pretreatment group and that SB pretreatment increased the rate of TLR and TVF at 24-month follow-up, similar to our results. Recently, a meta-analysis (23) including the four studies demonstrated that bifurcation lesions stented without SB predilation demonstrated lower OR of requiring further SB intervention compared with lesions receiving upfront SB predilation. In fact, our result showed a prediction of SB pretreatment for PMI. More recently, Sheiban et al. (12) reported that PMI was positively correlated with TLF at 1-year follow-up after stenting bifurcation lesions. Conclusively, the routine performance of SB pretreatment before the PS procedures was not recommended by the current consortium (24) and previous clinical trials (4–9). SB pretreatment should be avoided for simple bifurcation lesions (short lesion length and less severe disease in the SB).
Acute coronary syndrome is a stage where coronary plaques become unstable (25). The COBIS Registry showed a lower rate of 3-year TLF after the PS approach for patients with ACS but no difference between the PS and upfront 2-stent for patients without ACS (26), confirmed by another study of Korean team which further found that SB lesion length was an independent factor of TLF (27). The underlying mechanisms for a higher rate of TLF in patients with ACS were multifactorial, of them DAPT might be one major reason (25). However, this study reported more frequent prescription of DAPT in the PS with 2-stent group and DAPT was not the factor for predicting TLF. This may again address the critical importance of intravascular imaging in guiding SB treatment.
Limitations
This study has some limitations. First, the non-randomized feature raised concerns about the exact different treatment effects between the PS with 1-stent and the PS with 2-stent as SB rescue stenting was performed in the scenario that SB was severely compromised or had complications induced by pretreatment. Thus, a randomized study using physiological assessment as the sole criterion for treating SB after stenting MV is crucial. Second, we did not compare the difference in clinical outcome between the PS with T and the PS with T-and-Protrusion (TAP) (4, 9, 10, 24) when a second stent was required in the SB. When an SB needed to be dilated after MV stenting, rewire was recommended across the distal cell of the MV stent (24). However, a very narrow space at the ostial SB after stenting MV did not allow precisely rewiring (from proximal or distal cell) so long as successfully crosses the struts to restore the SB flow, particularly for complex bifurcations (4). Finally, intravascular imaging was not routinely used because imaging guidance was not recommended in the studies (4, 9–11). Therefore, an intravascular imaging-guided stenting bifurcation is highly recommended. For this issue, two ongoing studies (28, 29) would launch their results, demonstrating the advantage of intravascular imaging guidance in treating a bifurcation lesion.
Conclusion
Provisional stenting with 2-stent is associated with a higher rate of 3-year TLF, mainly due to increased requirement of revascularization. A further study identifying the underlying mechanisms correlated with stent failure is warranted.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Nanjing First Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
S-LC and IS made substantial contributions to the initial conception and design of the whole study and to the revision of the manuscript. IS and ZG wrote the first draft. JK contributed to data management and statistical expertise. J-JZ, TS, MM, FY, and NT provided comments and suggestions in critical revision of the manuscript. All authors approved the final version of the article.
Funding
This study was funded by grants from the National Science Foundation of China (Grant numbers: NSFC 91639303 and NSFC 81770441) and jointly supported by the Jiangsu Provincial Special Program of Medical Science (BE2019615) and Microport (Shanghai, China).
Acknowledgments
We thank Professor Feng Chen for his thorough statistical analysis. We also acknowledge Dr. Spencer B. King (Director of Clinical Event Committee), Dr. Tanveer S. Rab, and Dr. Tak W. Kwan for their meticulous work assessing all events. S-LC is a Fellow at the Collaborative Innovation Center for Cardiovascular Disease Translational Medicine, Nanjing Medical University, Nanjing, China.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.910313/full#supplementary-material
Abbreviations
PS, provisional stenting; ACS, acute coronary syndrome; TLF, target lesion failure; TVF, target vessel failure; TLR, target lesion revascularization; SB, side branch; MV, main vessel; DK crush, double kissing crush; KBI, kissing balloon inflation; TIMI, thrombolysis in myocardial infarction; POT, proximal optimization technique; QCA, quantitative coronary analysis; TVMI, target vessel myocardial infarction; ST, stent thrombus; DAPT, dual antiplatelet therapy; PMI, periprocedural myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft.
References
1. Fihn SD, Blankenship JC, Alexander KP, Bittl JA, Byrne JG, Fletcher BJ, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused on update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. (2014) 64:1929–49. doi: 10.1161/CIR.0000000000000095
2. Steigen TK, Maeng M, Wiseth R, Erglis A, Kumsars I, Narbute I, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. (2006) 114:1955–61. doi: 10.1161/CIRCULATIONAHA.106.664920
3. Chen SL, Sheiban I, Xu B, Jepson N, Paiboon C, Zhang JJ, et al. Impact of the complexity of bifurcation lesions treated with drug-eluting stents: the DEFINITION study (Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts). JACC Cardiovasc Interv. (2014) 7:1266–76. doi: 10.1016/j.jcin.2014.04.026
4. Zhang JJ, Ye F, Xu K, Kan J, Tao L, Santoso T, et al. Multicentre, randomized comparison of two-stent and provisional stenting techniques in patients with complex coronary bifurcation lesions: the DEFINITION II trial. Eur Heart J. (2020) 41:2523–36.
5. Colombo A, Bramucci E, Saccà S, Violini R, Lettieri C, Zanini R, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary bifurcations: application of the crushing technique using sirolimus-eluting stents) study. Circulation. (2009) 119:71–8. doi: 10.1161/CIRCULATIONAHA.108.808402
6. Hildick-Smith D, de Belder AJ, Cooter N, Curzen NP, Clayton TC, Oldroyd KG, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. (2010) 121:1235–43. doi: 10.1161/CIRCULATIONAHA.109.888297
7. Hildick-Smith D, Egred M, Banning A, Brunel P, Ferenc M, Hovasse T, et al. The European bifurcation club Left Main Coronary Stent study: a randomized comparison of stepwise provisional vs. systematic dual stenting strategies (EBC MAIN). Eur Heart J. (2021) 42:3829–39. doi: 10.1093/eurheartj/ehab283
8. Di Gioia G, Sonck J, Ferenc M, Chen SL, Colaiori I, Gallinoro E, et al. Clinical outcomes following coronary bifurcation PCI techniques: a systematic review and network meta-analysis comprising 5,711 patients. JACC Cardiovasc Interv. (2020) 13:1432–44. doi: 10.1016/j.jcin.2020.03.054
9. Chen X, Li X, Zhang JJ, Han Y, Kan J, Chen L, et al. 3-year outcomes of the DKCRUSH-V Trial comparing DK crush with provisional stenting for left main bifurcation lesions. JACC Cardiovasc Interv. (2019) 12:1927–37. doi: 10.1016/j.jcin.2019.04.056
10. Chen SL, Santoso T, Zhang JJ, Ye F, Xu YW, Fu Q, et al. A randomized clinical study comparing double kissing crush with provisional stenting for treatment of coronary bifurcation lesions: results from the DKCRUSH-II (Double kissing crush versus provisional stenting technique for treatment of coronary bifurcation lesions) trial. J Am Coll Cardiol. (2011) 57:914–20. doi: 10.1016/j.jacc.2010.10.023
11. Chen SL, Ye F, Zhang JJ, Ye F, Xu YW, Fu Q, et al. Randomized comparison of FFR-guided and angiography-guided provisional stenting of true coronary bifurcation lesions: the DKCRUSH-VI trial (Double kissing crush versus provisional stenting technique for treatment of coronary bifurcation lesions VI). JACC Cardiovasc Interv. (2015) 8:536–46.
12. Sheiban I, Ge Z, Kan J, Nie S, Zhang JJ, Santoso T, et al. Association of peri-procedural myocardial infarction with mortality after stenting true coronary bifurcation lesions: a pooled individual participant data analysis from four randomized controlled trials. Catheter Cardiovasc Interv. (2022) 99:617–26. doi: 10.1002/ccd.29946
13. Mauri L, Hsieh WH, Massaro JM, Ho KK, D’Agostino R, Cutlip DE. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med. (2007) 356:1020–9. doi: 10.1056/NEJMoa067731
14. Vassilev D, Mileva N, Collet C, Nikolov P, Sokolova K, Karamfiloff K, et al. Bifurcation functional significance score as predictor of mortality: a validating study. Sci Rep. (2021) 11:24308. doi: 10.1038/s41598-021-03815-6
15. Chen SL, Chen JP, Mintz G, Xu B, Kan J, Ye F, et al. Comparison between the NERS (new risk stratification) score and the SYNTAX (Synergy between percutaneous coronary intervention with taxus and cardiac surgery) score in outcome prediction for unprotected left main stenting. JACC Cardiovasc Interv. (2010) 3:632–41. doi: 10.1016/j.jcin.2010.04.006
16. Chen SL, Han YL, Zhang YJ, Ye F, Liu HW, Zhang JJ, et al. The anatomic- and clinical-based NERS (new risk stratification) score II to predict clinical outcomes after stenting unprotected left main coronary artery disease: results from a multicenter, prospective, registry study. JACC Cardiovasc Interv. (2013) 6:1233–41. doi: 10.1016/j.jcin.2013.08.006
17. Song YB, Hahn JY, Song PS, Yang JH, Choi JH, Choi SH, et al. Randomized comparison of conservative versus aggressive strategy for provisional side branch intervention in coronary bifurcation lesions: results from the SMART-STRATEGY (Smart angioplasty research team-optimal strategy for side branch intervention in coronary bifurcation lesions) randomized trial. JACC Cardiovasc Interv. (2012) 5:1133–40. doi: 10.1016/j.jcin.2012.07.010
18. Song YB, Park TK, Hahn JY, Yang JH, Choi JH, Choi SH, et al. Optimal strategy for provisional side branch intervention in coronary bifurcation lesions: 3-year outcomes of the SMART-STRATEGY randomized trial. JACC Cardiovasc Interv. (2016) 9:517–26. doi: 10.1016/j.jcin.2015.11.037
19. Zhang J, Gao X, Kan J, Ge Z, Han L, Lu S, et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: the ULTIMATE trial. J Am Coll Cardiol. (2018) 72:3126–37. doi: 10.1016/j.jacc.2018.09.013
20. Hong SJ, Kim BK, Shin DH, Nam CM, Kim JS, Ko YG, et al. Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: the IVUS-XPL randomized clinical trial. JAMA. (2015) 314:2155–63. doi: 10.1001/jama.2015.15454
21. Hong SJ, Zhang JJ, Mintz GS, Ahn CM, Kim JS, Kim BK, et al. Improved 3-year cardiac survival after IVUS-guided long DES implantation: a patient-level analysis from 2 randomized trials. JACC Cardiovasc Interv. (2022) 15:208–16. doi: 10.1016/j.jcin.2021.10.020
22. Song PS, Song YB, Yang JH, Hahn JY, Choi SH, Choi JH, et al. The impact of side branch predilatation on procedural and long-term clinical outcomes in coronary bifurcation lesions treated by the provisional approach. Rev Esp Cardiol (Engl Ed). (2014) 67:804–12. doi: 10.1016/j.rec.2014.01.032
23. Mirzaee S, Isa M, Thakur U, Cameron JD, Nicholls SJ, Dundon BK. Impact of side-branch predilation on angiographic outcomes in non-left main coronary bifurcation lesions. J Invasive Cardiol. (2020) 32:42–8.
24. Burzotta F, Lassen JF, Lefèvre T, Banning AP, Chatzizisis YS, Johnson TW, et al. Percutaneous coronary intervention for bifurcation coronary lesions: the 15th consensus document from the European Bifurcation Club. EuroIntervention. (2021) 16:1307–17. doi: 10.4244/EIJ-D-20-00169
25. Tomaniak M, Katagiri Y, Modolo R, de Silva R, Khamis RY, Bourantas CV, et al. Vulnerable plaques and patients: state-of-the-art. Eur Heart J. (2020) 41:2997–3004. doi: 10.1093/eurheartj/ehaa227
26. Kim MC, Ahn Y, Sun Sim D, Joon Hong Y, Han Kim J, Ho Jeong M, et al. Comparison of the planned one- and elective two-stent techniques in patients with coronary bifurcation lesions with or without acute coronary syndrome from the COBIS II Registry. Catheter Cardiovasc Interv. (2018) 92:1050–60. doi: 10.1002/ccd.27551
27. Sang Song P, Ryeol Ryu D, Choi SH, Yang JH, Song YB, Hahn JY, et al. Impact of acute coronary syndrome classification and procedural technique on clinical outcomes in patients with coronary bifurcation lesions treated with drug-eluting stents. Clin Cardiol. (2012) 35:610–8. doi: 10.1002/clc.22020
28. Holm NR, Andreasen LN, Walsh S, Kajander OA, Witt N, Eek C, et al. Rational and design of the European randomized optical coherence tomography optimized bifurcation event reduction trial (OCTOBER). Am Heart J. (2018) 205:97–109. doi: 10.1016/j.ahj.2018.08.003
29. Ge Z, Kan J, Gao XF, Kong XQ, Zuo GF, Ye F, et al. Comparison of intravascular ultrasound-guided with angiography-guided double kissing crush stenting for patients with complex coronary bifurcation lesions: rationale and design of a prospective, randomized, and multicenter DKCRUSH VIII trial. Am Heart J. (2021) 234:101–10.
Keywords: acute coronary syndrome (ACS), coronary artery bifurcation lesions, provisional stenting, drug-eluting stent, target lesion failure
Citation: Sheiban I, Ge Z, Kan J, Zhang J-J, Santoso T, Munawar M, Ye F, Tian N and Chen S-L (2022) Provisional stenting with side branch rescue stenting is associated with increased 3-year target lesion failure in patients with acute coronary syndrome and coronary bifurcation lesions. Front. Cardiovasc. Med. 9:910313. doi: 10.3389/fcvm.2022.910313
Received: 01 April 2022; Accepted: 15 August 2022;
Published: 11 October 2022.
Edited by:
Dobrin Vassilev, University of Ruse, BulgariaReviewed by:
Plinio Cirillo, University of Naples Federico II, ItalyGianluca Rigatelli, Hospital Santa Maria della Misericordia of Rovigo, Italy
Copyright © 2022 Sheiban, Ge, Kan, Zhang, Santoso, Munawar, Ye, Tian and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shao-Liang Chen, Y2htZW5neEAxMjYuY29t
†These authors have contributed equally to this work
 Imad Sheiban
Imad Sheiban Zhen Ge
Zhen Ge Jing Kan
Jing Kan Jun-Jie Zhang
Jun-Jie Zhang Teguh Santoso3
Teguh Santoso3 Muhammad Munawar
Muhammad Munawar Shao-Liang Chen
Shao-Liang Chen