- State Key Laboratory of Organ Failure Research, Department of Cardiology, Nanfang Hospital, Southern Medical University, Guangzhou, China
Objective: To explore the association between dietary fiber and heart failure (HF).
Methods: Data were collected from the 2009–2018 National Health and Nutrition Examination Survey. Dietary fiber intake data were obtained from two 24-h dietary recall interviews. Logistic regression and restricted cubic spline models were used to explore the association of dietary intakes of total, cereal, fruit, and vegetable fiber with HF prevalence.
Results: A total of 21869 adults were included in this study. After adjusting for multiple confounding factors, the odds ratios (OR) and 95% confidence intervals (CI) for HF was 0.49 (0.28 to 0.87, P for trend = 0.016) for the highest tertile versus lowest tertile of total fiber intake. Similar results were observed for cereal but not fruit and vegetable fiber intake. Dose-response analysis indicated that dietary intake of total and cereal fiber were inversely associated with HF in a linear manner.
Conclusion: Intakes of total and cereal fiber were inversely associated with HF in adults.
Introduction
Heart failure (HF) is a growing global public health burden, with more than 37.7 million individuals estimated to be affected worldwide (1), and the prevalence of HF is increasing as populations age, and poor lifestyle determinants rise (2). Although advances in treatments and devices for HF have substantially improved the survival and quality of life in patients, the mortality rates remain high, with the 10-year survival rate at only 25% (3). Therefore, it is of great importance to identify modifiable factors for the prevention or delay of HF and its complications.
Dietary fiber, which comprises many different, mainly plant-based, that are not completely digested in the human gut, has become increasingly popular in recent years due to its health benefits. Although nutrition guidelines encourage increased consumption of dietary fiber and a consensus statement from the Heart Failure Society of America recommended plant-based diets for patients with HF (4, 5), most individuals in the United States consume less than half of the recommended levels of daily dietary fiber. Notwithstanding the increase in the daily recommended amount to 30 g, just 13% of men and 4% of women adhere to this recommendation (6). The apparent benefits of dietary fiber intake vary substantially from large relative risk reduction to no benefit depending on the outcome or the geographical region (Europe, the United States, Japan, or China). Emerging evidence from randomized trials and observational studies has shown the potential role of dietary fiber intake in reducing coronary heart disease (7, 8), stroke (8), peripheral vascular disease (9), mortality (10), and cancer (11).
However, previous studies were centered just on the association between dietary fiber and many cardiovascular diseases with no scrutiny of its involvement in HF. Several studies have reported that dietary fiber can improve intestinal flora and risk factors for heart failure (e.g., insulin resistance, inflammation, and metabolic disorders) (12–14), suggesting a potential association between dietary fiber and heart failure. We thus examined the relation between HF prevalence and dietary fiber intake.
Materials and Methods
Study Population
The National Health and Nutrition Examination Survey (NHANES) is a nationally representative study to assess the health and nutritional status of the non-institutionalized civilian population in the United States. This survey combines several interviews which were initially executed in participants’ homes, and subsequent health examinations were completed in a mobile examination center (MEC). This database is global and public with data released every 2 years and accessed from their website. The sampling method and data collection details have been published elsewhere (15).
This study is based on an analysis of data from NHANES cycles between 2009 and 2018. As shown in Figure 1, participants who were pregnant or lactating women (n = 576) were excluded. Participants with missing self-reported HF history (n = 20,358) or incomplete dietary recall (n = 6,797), those documenting extreme total energy intakes, i.e., in women: <500 or >5,000 kcal/day and in men: <500 or >8,000 kcal/day (n = 98) were also excluded. Our study included a final total of 21,869 adult participants. As NHANES is a publicly available dataset, this study was exempt from approval by an institutional review board. Informed consent was sourced from the participants prior to the interview and examination steps.
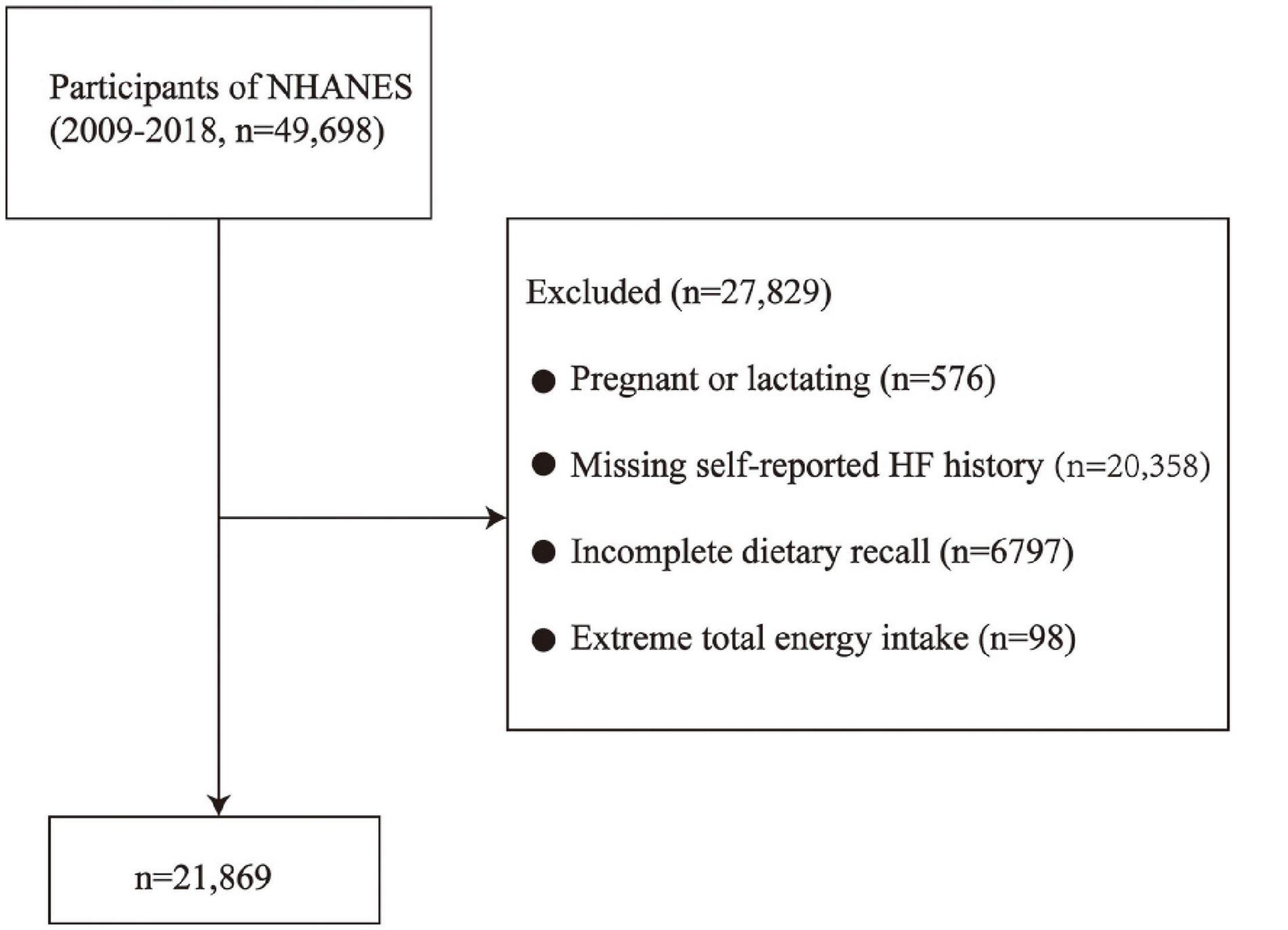
Figure 1. Flow chart of the screening process for the selection of eligible participants. NHANES, National Health and Nutrition Examination Survey.
Dietary Fiber Intake
Dietary fiber intake was assessed by two 24-h dietary recall interviews collected by skilled dietitians. While the MEC was the site of the initial dietary interview, the second interview was collected by telephone after 3 to 10 days. The U.S. Department of Agriculture’s Dietary Research Food and Nutrition Database for Dietary Studies scrutinized the nutrient intakes. Cereal, vegetable, and fruit dietary fiber are calculated by the sum of the corresponding food code in the Individual Foods files. The average 2-day fiber amount was employed to compute the dietary fiber intakes from the two aforementioned interviews and was adjusted to the body weight. In this study, dietary fiber intake was categorized into tertiles.
Heart Failure
Similar to a prior NHANES study (16), HF was defined as participants who have conducted the audiometric assessment and had a self-reported HF history. The latter entailed an affirmative answer to, “Has a doctor ever diagnosed you with heart failure?”
Covariates
Data of age, sex, race, education level, family income, and smoking status were collected from household interviews with standardized questionnaires. Bodyweight, height, and blood pressure were obtained when people participated in the physical examinations at a MEC. Plasma glucose and total cholesterol were measured at baseline when the participants provided their blood samples. Body mass index (BMI) was calculated as weight in kilograms (kg) divided by height in meters squared (m2). Race classification was Mexican American, other Hispanic, non-Hispanic White, non-Hispanic Black, and other races. Education level was categorized as less than high school, high school or equivalent, or college and above. Family income was classified as <$20,000, $20,000–$55,000, $55,000–$75,000, and ≥$75,000. Smoking status was grouped into “never” (never smoked or less than a hundred cigarettes in life), “current” (more than a hundred cigarettes in life and is also ongoing currently), or “former” (more than a hundred cigarettes in life but currently not smoking). Diabetes was defined as a fasting blood glucose level of ≥7.0 mmol/l, 2-h plasma glucose level of ≥11.1 mmol/l, use of diabetes medications, or self-reported diabetes diagnosis. For hypertension, systolic blood pressure and diastolic blood pressure of ≥130 and ≥80 mmHg, respectively, hypertension medication consumption or self-reported hypertension diagnosis were taken into account. The aggregate daily energy, protein, fat, vitamin A, and vitamin B6 from the diet and supplement usage was employed to compute the total energy intake, total protein intake, total fat intake, total vitamin A intake, and total vitamin B6 intake, respectively.
Statistical Analysis
While continuous data were reported as mean and SD, or median with interquartile range, numbers and percentages were employed to express categorical data. Intergroup variation in the former entailed one-way ANOVA and χ2 tests for the latter. Logistic regression models were employed to assess the association between dietary fiber intake and HF prevalence. While Model 1 was unadjusted, model 2 was inclusive of the adjustment for age, sex, and race and model 3 was inclusive of model 2 variables with total energy intake, total protein intake, total fat intake, total vitamin A intake, total vitamin B6 intake, BMI, education, annual household income, smoking category, hypertension, diabetes, and total cholesterol (TC) levels. As mentioned above, subsequent to the categorization of the dietary fiber intake as tertiles, the lowest tertile was then employed as the reference group. The odds ratios (ORs) and 95% CIs were calculated. Subgroup analyses ensued for dietary fiber intake and the prevalence of HF by sex, race, hypertension, diabetes, and obesity status. To assess the dose-response association between dietary fiber intake and the prevalence of HF, we fitted a cubic spline regression using the same covariates adjusted in model 3 and located three knots at the 5th, 50th, and 95th. The probabilities here were all two-sided with significance at P < 0.05. All analyses were conducted using R version 3.3.3.
Results
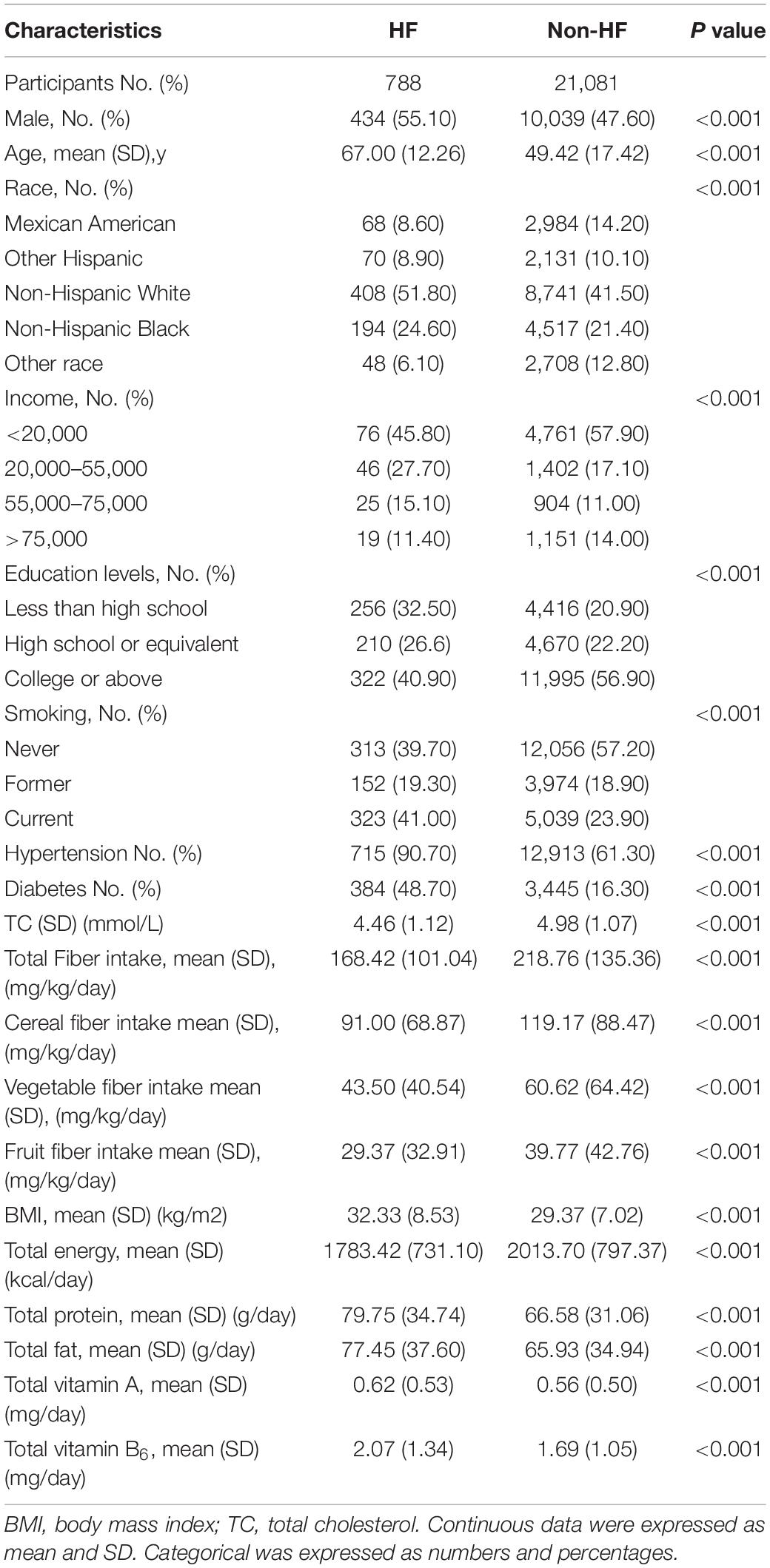
A total of eligible 21,869 participants were included in our study. Mean (SD) age was 50.1 (17.6) years: 10,473 (47.9%) were men, and 9,149 (41.8%) were non-Hispanic White. Population characteristics are presented in Table 1. The HF prevalence is 3.6%. As opposed to non-HF participants, patients with HF were more likely to be older, male, white, highly educated, a current smoker, and were less likely to earn a substantial income and consume high dietary nutrition (such as fiber, protein, fat, vitamin A, and vitamin B6) and total energy. They also tended to have lower total cholesterol but higher BMI and higher hypertension and diabetes prevalence.
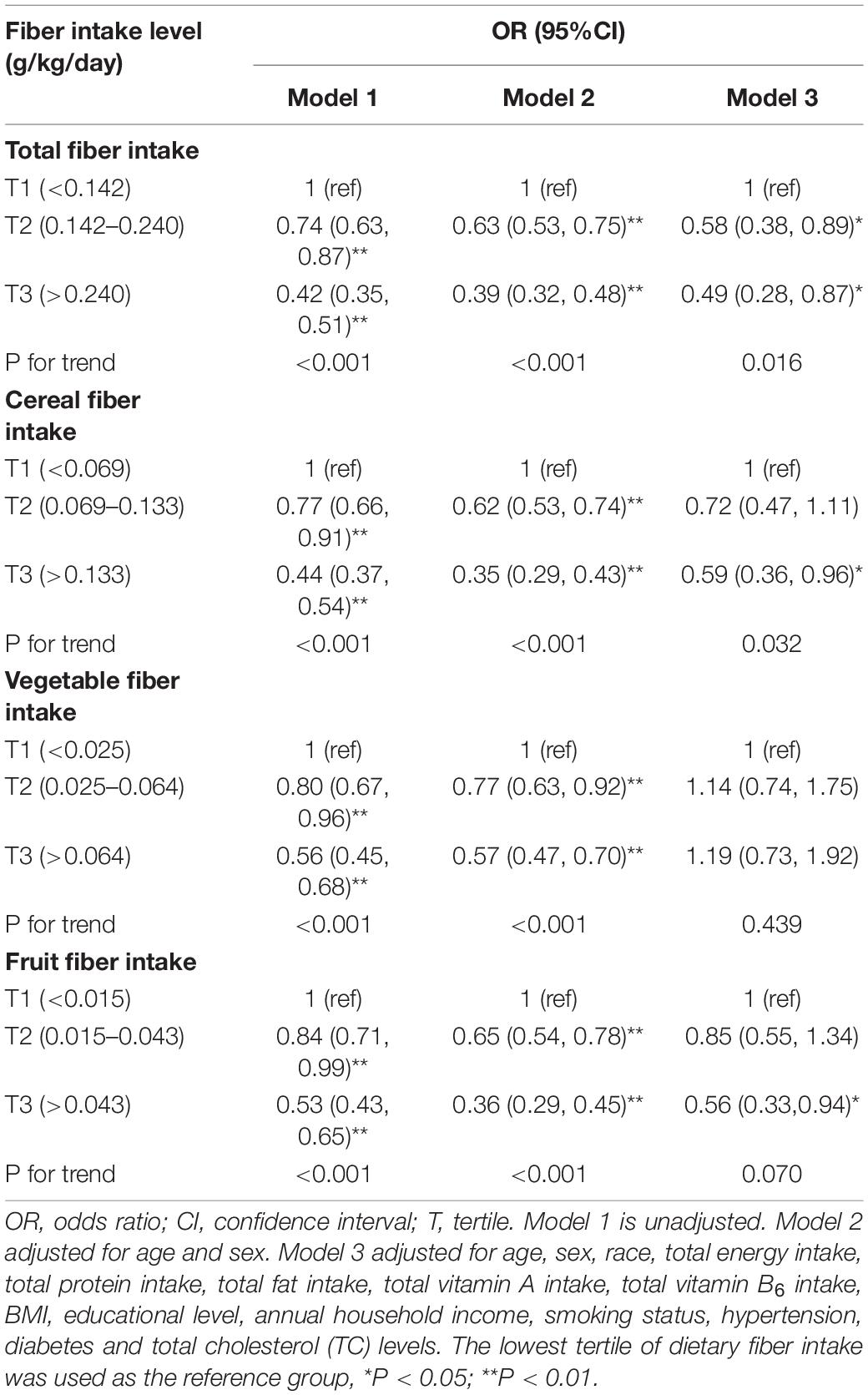
In univariate logistic regression (Table 2), a consistent association was observed between higher fiber intake (total, cereal, vegetable, and fruit) and lower HF prevalence. These associations remained significant following age, sex, and race adjustments (model 2). After further adjustment for total energy intake, total protein intake, total fat intake, total vitamin A intake, total vitamin B6 intake educational level, annual household income, smoking status, hypertension, diabetes, TC, and body mass index (model 3), the ORs of HF were 0.49 (95% CI 0.28–0.87, Pfor trend = 0.016), 0.59 (95% CI 0.36–0.96, Pfor trend = 0.032), 1.19 (95% CI 0.73–1.92, Pfor trend = 0.439), and 0.56 (95% CI 0.33–0.94, Pfor trend = 0.070) for the highest tertile of the total, cereal, vegetable, and fruit fiber, respectively, as opposed to the lowest tertile. An association remained for the highest tertile of total and cereal fiber with a lowered HF prevalence, while the association between vegetable and fruit fiber with HF was no longer significant.
The dose-response relationship analysis between total, cereal fiber intake, and HF is shown in Figure 2. A linear relationship was observed between total dietary fiber intake and HF (P for non-linearity = 0.14). HF prevalence significantly decreased with the increase in total fiber intake. This linear inverse association was also observed for the cereal fiber intakes and HF prevalence (P for non-linearity = 0.27). The dose-response relationship analysis between vegetable and fruit fiber with HF was not performed as no significant association was observed in the multivariable logistic regression analysis (model 3).
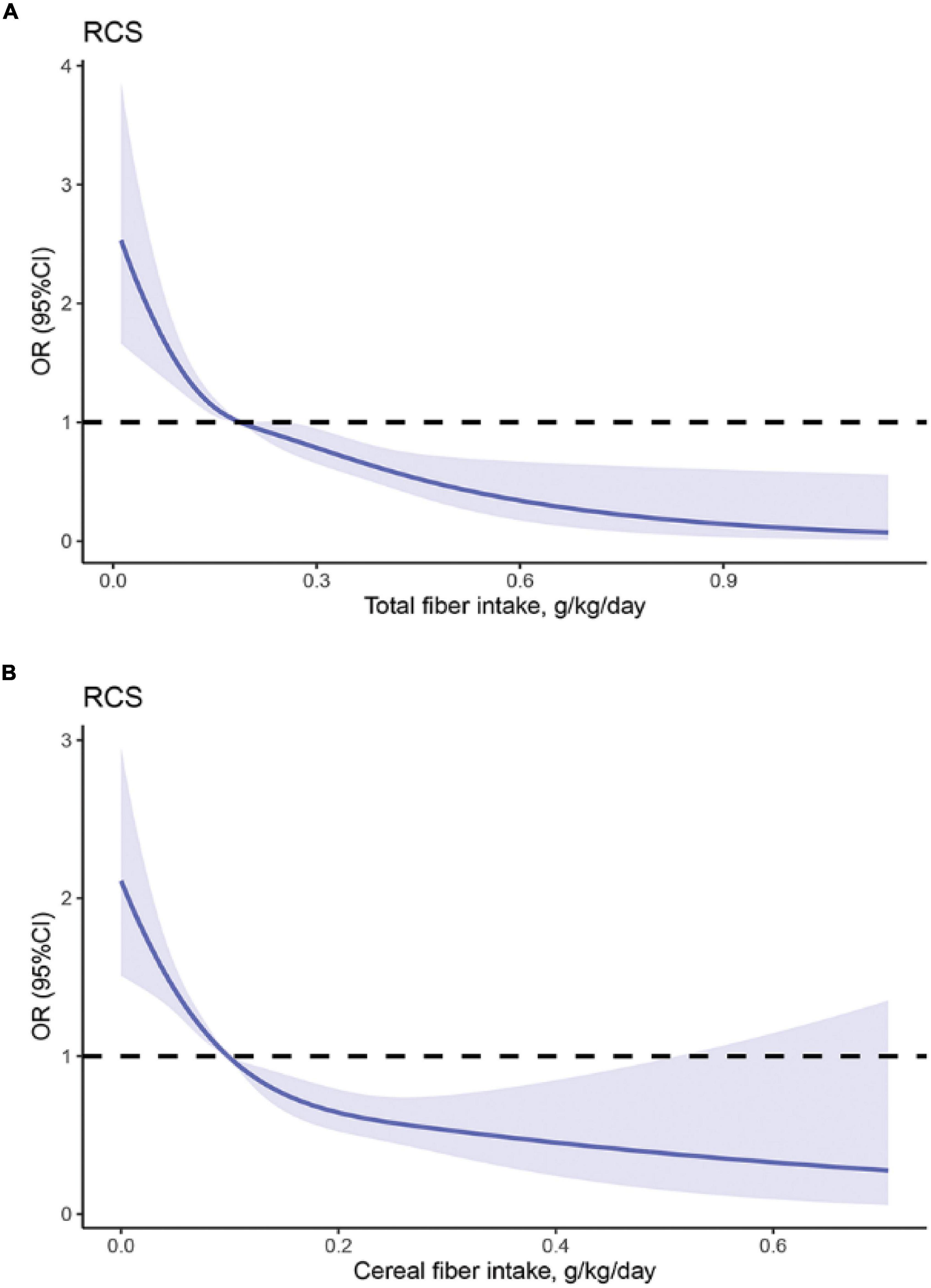
Figure 2. The restricted cubic spline model showed a dose-response relationship between total, cereal fiber intake and HF. (A) = Total fiber, P for non-linearity = 0.14; (B) Cereal fiber, Pfor non-linearity = 0.27; The restricted cubic splines model adjusted for age, sex, race, total energy intake, total protein intake, total fat intake, total vitamin A intake, total vitamin B6 intake, BMI, educational level, annual household income, smoking status, hypertension, diabetes and total cholesterol (TC) levels. The solid line and dashed line represent the estimated ORs and the corresponding 95% confidence intervals, respectively. OR, odds ratio.
The association between dietary fiber intake and HF in subgroup analyses was displayed in Table 3. Subsequent to adjustment for the same covariates in model 3, the subgroup analysis shows that the intake of total and cereal fiber has no significant interaction with sex, race, hypertension, diabetes, and obesity status.
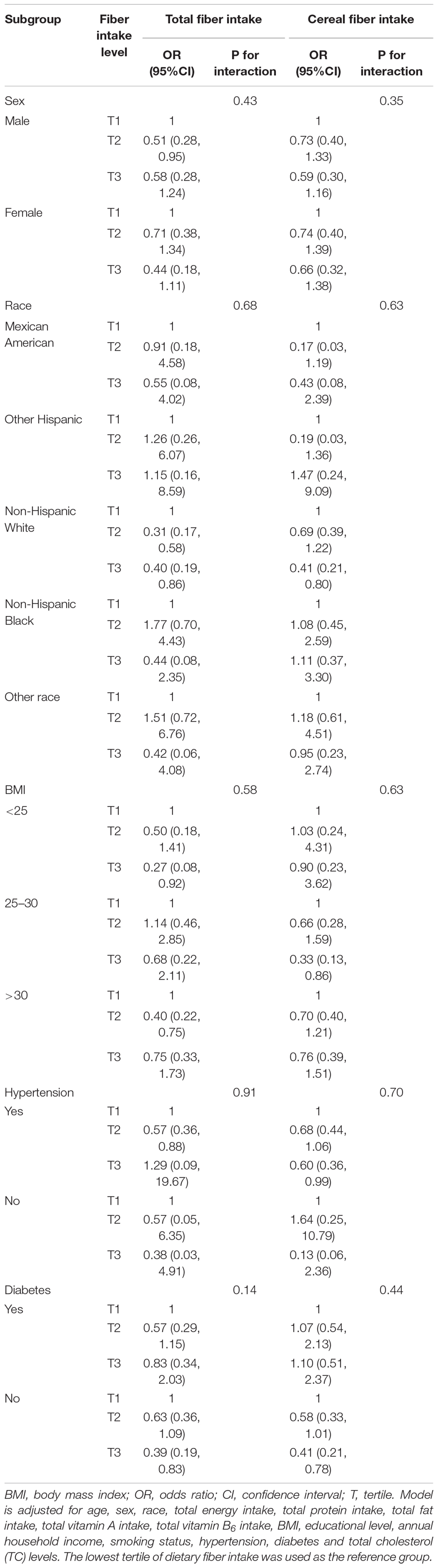
Table 3. ORs and 95% CIs for HF according to tertiles of total fiber intake, stratified by sex, race, hypertension, diabetes, and obese status, NHANES 2009–2018.
Discussion
This study found an association between higher total and cereal fiber intake and lower HF prevalence in adults. Dose-response analysis showed a linear relationship between total and cereal fiber intake with HF prevalence.
Dietary fiber, common nutrition, has a variety of benefits for several diseases (6). A randomized, crossover study documented lowered hyperinsulinemia and plasma lipid concentrations with a high intake of dietary fiber (mainly the soluble type) to improve glycemic control in patients with type 2 diabetes (17). A meta-analysis encompassing 18 studies and 672,408 participants was indicative of an inverse association between dietary fiber consumption and coronary heart disease risk (18). The risk of stroke was lowered by 60% in an 8-year follow-up study with Japanese patients with type 2 diabetes who were in the fourth quartile of total dietary fiber as opposed to those in the first quartile (19). In a large prospective study with a long follow-up period (16.8 years), an inverse association emerged between all-cause mortality and dietary fiber (20). However, the association between HF and dietary fiber intake was not probed in any such work. Our study investigated this association to reveal a lower HF prevalence with higher total and cereal fiber intakes in a dose-responsive manner.
This study found a linear relationship between total fiber intake and HF. HF risk decreased with the increase in total fiber intake, and the rate reduction slightly plateaued at a consumption of 0.3 g/kg/day of total fiber. Similarly, we found a similar dose-response pattern for cereal fiber intake, the rate reduction plateaued at about 0.2 g/kg/day. This observation is consistent with a previous study demonstrating that the risk of hypertension gradually decreased as total dietary fiber intake increased to 0.35 g/kg/day (21). The dose-response relationship in our study suggests the protective role of dietary fiber intake in reducing HF risk, especially for those who do not meet the recommended intake.
The mechanism by which dietary fiber intake might impact HF remains to be elucidated in detail. Several potential pathophysiological mechanisms may contribute to the association between dietary fiber and HF. First, reductions in blood cholesterol and glucose might be involved in the inverse association between dietary fiber intake and HF (22). A study showed that the β-glucans, derived from dietary fiber, lower bile acid reabsorption which in turn reduces the levels of circulating cholesterol (23). The entrapment of sugar by soluble fiber in the small intestine to form a barrier inhibiting amylase and slower glucose absorption is known to diminish blood glucose and improve insulin sensitivity (24). Second, dietary fiber has been shown to improve intestinal flora and increase colonic fermentation (production of SCFA) in the large bowel (25, 26). Animal models have documented that high dietary fiber can improve intestinal flora and reduce blood pressure, cardiac fibrosis, left ventricular hypertrophy, and delay the process of HF in hypertensive mice (26, 27). In addition, other studies reported that high consumption of dietary fiber increased the abundance of SCFA, which might decrease risk factors for HF, such as insulin resistance (28), chronic inflammation, and metabolic disorders (29). The amalgamation of epidemiological and experimental analyses on dietary fiber facilitates us to propose that increasing the dietary fiber intake can cause betterment in HF.
Our study has important clinical implications. Given the increasing prevalence and disease burden of HF along with the lack of approved pharmacological treatment, it is important to scour for modifiable risk factors and to develop preventive strategies. Previous studies have found significant relationships between dietary nutrients and HF (30, 31). Our findings support a potentially adverse association between total, cereal dietary fiber and HF prevalence. The drafting of questionnaires on dietary fiber intake can help to identify individuals at high risk for HF. These observations emerge to reinforce the current recommendations of increasing dietary fiber consumption as part of a healthy diet to prevent HF.
Our study has several advantages. Our study included a large population of different races, social backgrounds, and geographical areas to assess the association between dietary fiber intake and the prevalence of HF. This allowed us to investigate the relationship between dietary fiber and HF for people from different demographics and social backgrounds. However, a few limitations are also put forth here. First, drawing inferences for causal interpretations is challenged towing to the cross-sectional model of our work. Second, despite controlling several potential confounding factors, the possibility of unmeasured confounding factors causing residual confusion remains. Third, the association between specific fiber types (i.e., soluble and insoluble fiber) and HF was not probed which may impact the HF risk.
Conclusion
A higher intake of total and cereal dietary fiber was associated with a lower prevalence of heart failure in adults, in a dose-response manner. These findings provide further support for the current recommendations that promote increased consumption of dietary fiber to prevent HF.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics Statement
This study was reviewed and approved by the National Center for Health Statistics Research Ethics Review Board, and written informed consent was obtained from all NHANES participants.
Author Contributions
HZha and ZL contributed to conception and design of the study. DG, HZho, and ZM acquired the data. XZ, YX, and XW performed the statistical analysis. JC and QZh wrote the first draft of the manuscript. QZe and DX critically revised the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor YH declared a shared affiliation with the authors at the time of review.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the investigators, the staff, and the participants of the NHANES study for their dedication and highly valued contributions.
References
1. Cai X, Liu X, Sun L, He Y, Zheng S, Zhang Y, et al. Prediabetes and the risk of heart failure: a meta-analysis. Diabetes Obes Metab. (2021) 23:1746–53. doi: 10.1111/dom.14388
2. Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet. (2018) 391:572–80. doi: 10.1016/S0140-6736(17)32520-5
3. Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. (2020) 22:1342–56.
4. Lichtenstein AH, Appel LJ, Vadiveloo M, Hu FB, Kris-Etherton PM, Rebholz CM, et al. 2021 Dietary guidance to improve cardiovascular health: a scientific statement from the American heart association. Circulation. (2021) 144:e472–87. doi: 10.1161/CIR.0000000000001031
5. Vest AR, Chan M, Deswal A, Givertz MM, Lekavich C, Lennie T, et al. Nutrition, obesity, and cachexia in patients with heart failure: a consensus statement from the heart failure society of America Scientific Statements Committee. J Card Fail. (2019) 25:380–400. doi: 10.1016/j.cardfail.2019.03.007
6. Evans C. Dietary fibre and cardiovascular health: a review of current evidence and policy. Proc Nutr Soc. (2020) 79:61–7. doi: 10.1017/S0029665119000673
7. Lillioja S, Neal AL, Tapsell L, Jacobs DJ. Whole grains, type 2 diabetes, coronary heart disease, and hypertension: links to the aleurone preferred over indigestible fiber. Biofactors. (2013) 39:242–58. doi: 10.1002/biof.1077
8. Bechthold A, Boeing H, Schwedhelm C, Hoffmann G, Knuppel S, Iqbal K, et al. Food groups and risk of coronary heart disease, stroke and heart failure: a systematic review and dose-response meta-analysis of prospective studies. Crit Rev Food Sci Nutr. (2019) 59:1071–90. doi: 10.1080/10408398.2017.1392288
9. Kulezic A, Bergwall S, Fatemi S, Sonestedt E, Zarrouk M, Gottsater A, et al. Healthy diet and fiber intake are associated with decreased risk of incident symptomatic peripheral artery disease - A prospective cohort study. Vasc Med. (2019) 24:511–8. doi: 10.1177/1358863X19867393
10. Man SF, Connett JE, Anthonisen NR, Wise RA, Tashkin DP, Sin DD. C-reactive protein and mortality in mild to moderate chronic obstructive pulmonary disease. Thorax. (2006) 61:849–53. doi: 10.1136/thx.2006.059808
11. Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. (2008) 454:436–44.
12. Reynolds AN, Akerman AP, Mann J. Dietary fibre and whole grains in diabetes management: systematic review and meta-analyses. PLoS Med. (2020) 17:e1003053. doi: 10.1371/journal.pmed.1003053
13. Myhrstad M, Tunsjo H, Charnock C, Telle-Hansen VH. Dietary Fiber, Gut Microbiota, and Metabolic Regulation-Current Status in Human Randomized Trials. Nutrients. (2020) 12:859. doi: 10.3390/nu12030859
14. Li W, Huang A, Zhu H, Liu X, Huang X, Huang Y, et al. Gut microbiota-derived trimethylamine N-oxide is associated with poor prognosis in patients with heart failure. Med J Aust. (2020) 213:374–9. doi: 10.5694/mja2.50781
15. Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, et al. National health and nutrition examination survey: analytic guidelines, 1999-2010. Vital Health Stat 2. (2013) 161:1–24.
16. Glynn PA, Ning H, Bavishi A, Freaney PM, Shah S, Yancy CW, et al. Heart failure risk distribution and trends in the United States Population, NHANES 1999-2016. Am J Med. (2021) 134:e153–64. doi: 10.1016/j.amjmed.2020.07.025
17. Chandalia M, Garg A, Lutjohann D, von Bergmann K, Grundy SM, Brinkley LJ. Beneficial effects of high dietary fiber intake in patients with type 2 diabetes mellitus. N Engl J Med. (2000) 342:1392–8. doi: 10.1056/NEJM200005113421903
18. Wu Y, Qian Y, Pan Y, Li P, Yang J, Ye X, et al. Association between dietary fiber intake and risk of coronary heart disease: a meta-analysis. Clin Nutr. (2015) 34:603–11. doi: 10.1016/j.clnu.2014.05.009
19. Tanaka S, Yoshimura Y, Kamada C, Tanaka S, Horikawa C, Okumura R, et al. Intakes of dietary fiber, vegetables, and fruits and incidence of cardiovascular disease in Japanese patients with type 2 diabetes. Diabetes Care. (2013) 36:3916–22. doi: 10.2337/dc13-0654
20. Katagiri R, Goto A, Sawada N, Yamaji T, Iwasaki M, Noda M, et al. Dietary fiber intake and total and cause-specific mortality: the Japan Public Health Center-based prospective study. Am J Clin Nutr. (2020) 111:1027–35. doi: 10.1093/ajcn/nqaa002
21. Sun B, Shi X, Wang T, Zhang D. Exploration of the association between dietary fiber intake and hypertension among U.S. adults using 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines: NHANES 2007(-)2014. Nutrients. (2018) 10:1091. doi: 10.3390/nu10081091
22. Stephen AM, Champ MM, Cloran SJ, Fleith M, van Lieshout L, Mejborn H, et al. Dietary fibre in Europe: current state of knowledge on definitions, sources, recommendations, intakes and relationships to health. Nutr Res Rev. (2017) 30:149–90. doi: 10.1017/S095442241700004X
23. Fuller S, Beck E, Salman H, Tapsell L. New horizons for the study of dietary fiber and health: a review. Plant Foods Hum Nutr. (2016) 71:1–12. doi: 10.1007/s11130-016-0529-6
24. Khan K, Jovanovski E, Ho H, Marques A, Zurbau A, Mejia SB, et al. The effect of viscous soluble fiber on blood pressure: a systematic review and meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis. (2018) 28:3–13. doi: 10.1016/j.numecd.2017.09.007
25. Nogal A, Valdes AM, Menni C. The role of short-chain fatty acids in the interplay between gut microbiota and diet in cardio-metabolic health. Gut Microbes. (2021) 13:1–24. doi: 10.1080/19490976.2021.1897212
26. Pakhomov N, Baugh JA. The role of diet-derived short-chain fatty acids in regulating cardiac pressure overload. Am J Physiol Heart Circ Physiol. (2021) 320:H475–86. doi: 10.1152/ajpheart.00573.2020
27. Marques FZ, Nelson E, Chu PY, Horlock D, Fiedler A, Ziemann M, et al. High-fiber diet and acetate supplementation change the gut microbiota and prevent the development of hypertension and heart failure in hypertensive mice. Circulation. (2017) 135:964–77. doi: 10.1161/CIRCULATIONAHA.116.024545
28. Evans CE, Greenwood DC, Threapleton DE, Cleghorn CL, Nykjaer C, Woodhead CE, et al. Effects of dietary fibre type on blood pressure: a systematic review and meta-analysis of randomized controlled trials of healthy individuals. J Hypertens. (2015) 33:897–911. doi: 10.1097/HJH.0000000000000515
29. Salamone D, Rivellese AA, Vetrani C. The relationship between gut microbiota, short-chain fatty acids and type 2 diabetes mellitus: the possible role of dietary fibre. Acta Diabetol. (2021) 58:1131–8. doi: 10.1007/s00592-021-01727-5
30. Zheng S, Qiu M, Wu J, Pan XF, Liu X, Sun L, et al.. Long-chain omega-3 polyunsaturated fatty acids and the risk of heart failure. Ther Adv Chronic Dis. (2022) 13:374130192. doi: 10.1177/20406223221081616
Keywords: heart failure (HF), dietary fiber intake, dose-response, National Health and Nutrition Examination Survey (NHANES), nutrition
Citation: Zhang H, Lin Z, Chen J, Gan D, Zhou H, Ma Z, Zeng X, Xue Y, Wang X, Zhan Q, Zeng Q and Xu D (2022) Association Between Dietary Fiber Intake and Heart Failure Among Adults: National Health and Nutrition Examination Survey 2009–2018. Front. Cardiovasc. Med. 9:893436. doi: 10.3389/fcvm.2022.893436
Received: 10 March 2022; Accepted: 30 March 2022;
Published: 17 May 2022.
Edited by:
Yuli Huang, Southern Medical University, ChinaReviewed by:
Dachun Xu, Tongji University, ChinaHongbin Qiu, Jiamusi University, China
Lingjun Jie, Xiamen University, China
Copyright © 2022 Zhang, Lin, Chen, Gan, Zhou, Ma, Zeng, Xue, Wang, Zhan, Zeng and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingchun Zeng, cWluZ2NodW56ZW5nQHNtdS5lZHUuY24=; Dingli Xu, ZGluZ2xpeHVAc211LmVkdS5jbg==
 Hao Zhang
Hao Zhang Zhibin Lin
Zhibin Lin Zhuang Ma
Zhuang Ma Qingchun Zeng
Qingchun Zeng