- 1Laboratory of Experimental Cardiology, University Medical Center Utrecht, Utrecht, Netherlands
- 2Department of Physiology, Faculty of Medicine, University of Iceland, Reykjavík, Iceland
Introduction
The steroid hormone 17β-estradiol (E2), together with its receptors (ER), is thought to play a major role in the modulation of cardiovascular physiology and pathology (1–6). E2 signals through the classical nuclear ERα and ERβ, as well as the membrane G protein-coupled receptor GPR30 (also referred to as GPER), via the genomic or non-genomic pathway. The E2/ER axis has been shown to exert vast effects in the cardiovascular system, regulating contractile function, (micro)vascular function, metabolic processes, calcium signaling, gene expression and protein abundance (7–22), among others, which can be sex-dependent (3, 23–28).
From a clinical perspective, the decline in E2 at menopause may contribute to the onset of cardiovascular disorders, such as atherosclerosis, heart failure with preserved ejection fraction (HFpEF) and other conditions that involve the microvasculature (9, 29, 30). Along this line, a consensus article was published recently by Maas et al. (31), which we found very informative and clear, and the authors are to be commended. The authors discuss several biological processes and pathways, which may eventually impact cardiovascular health and risk factors. These include altered vascular function, enhanced inflammation and up-regulation of other hormonal systems, such as the renin-angiotensin-aldosterone system, the sympathetic nervous system, and reduced nitric oxide-dependent vasodilation, as well as vascular and myocardial stiffness. Some additional key mechanisms require consideration and are briefly highlighted in this article (Figure 1).
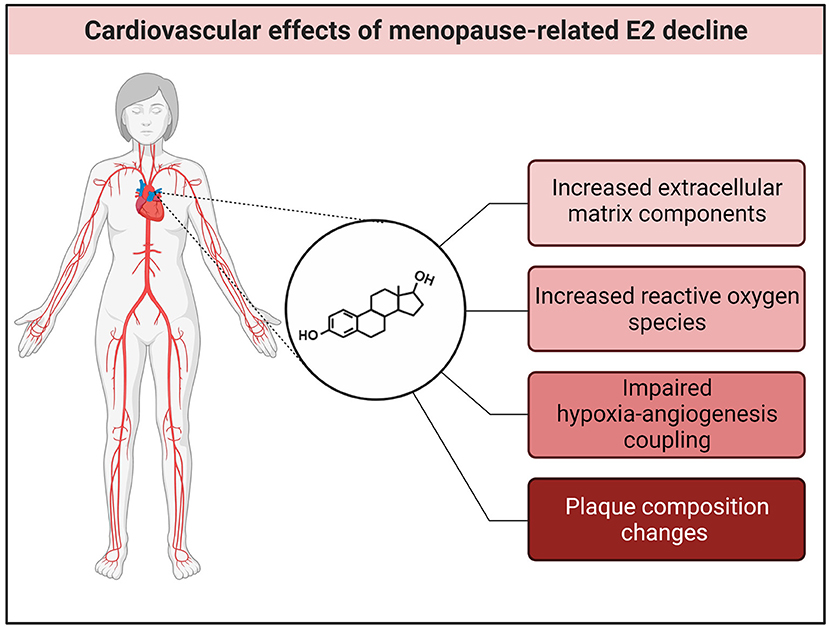
Figure 1. E2 effects in the cardiovascular system. The decline of E2 at menopause may lead to an increase in extracellular matrix (ECM) components and reactive oxygen species (ROS), impaired hypoxia-angiogenesis coupling and increased atherosclerotic plaque formation. Created with BioRender.com.
E2 Mechanisms in the Cardiovascular System
Cardiovascular remodeling and dysfunction are associated with alterations and disruptions of homeostasis of the extracellular matrix. Vascular and myocardial stiffness has been widely associated with fibrillar collagen and cross-linking. Given that E2 is involved in the regulation of collagens (32), decreased E2 levels might eventually contribute to increases in cardiac extracellular matrix components in postmenopausal women (33).
Endothelial dysfunction is associated with increased systemic oxidative stress and vascular inflammation, characterized by reduced vasodilators, such as nitric oxide. Antioxidant properties of E2 have been previously reported, scavenging free radicals, as well as inhibiting the formation of mitochondrial reactive oxygen species, thereby leading to lower levels of oxidative stress (34, 35). Reduced E2 levels in postmenopausal women may also contribute to an impaired hypoxia-angiogenesis coupling, thereby limiting the recovery from ischemia.
Interestingly, recent work on human atherosclerotic plaques suggests that E2 may also regulate gene expression of multiple downstream targets and thereby influence the activity of molecular networks, even years after menopause (36). In postmenopausal women undergoing coronary artery bypass grafting, atherosclerotic plaques showed enrichment of the gene set E2 responses in molecular networks important for smooth muscle cells of the plaque (36).
E2 in Transgender Women
In the article by Maas et al., we were also very interested to see the discussion on cardiovascular disease risks for cross-sex therapy in transgender women (31). The authors point to the fact that only venous thromboembolism risk has been evaluated in transgender women undergoing estrogen treatment. This clearly highlights an important gap in the field. They further note that transgender women have an increased risk for various cardiovascular disorders. This is not surprising. E2 is primarily synthesized in the gonads, particularly in the ovaries. However, there are extra-ovarian sources of E2 production. These include the adipose, breast and adrenal tissues, bone, heart, brain and skin, where aromatase can be produced (28). In addition, the testes and prostate are production sites of E2 through the local conversion of androgenic precursors by the aromatase enzyme, which may lead to significant levels of E2. In this context, there may be a marked increase of E2 production in individuals with obesity (37), as the adipose tissue is a major contributor of E2 synthesis, and in elderly individuals, men may have higher concentrations of E2 compared with age-matched women (38). Notably, elevated E2 levels have been associated with an increased risk and incidence of cardiovascular disease in cisgender men (39–41). Although explanations for causal pathways and putative mechanisms for this association are incompletely understood, E2 appears to influence the contractile machinery, modulating regulatory proteins (24).
Conclusions
Collectively, we greatly appreciate the focus of the article by Maas et al. The elucidation of underlying mechanisms is essential to the identification of potential therapeutic targets with the ultimate goal of improving medical care. Clearly, further research into the effects of menopause-related decreases in E2 on cardiovascular (patho)physiology is warranted.
Author Contributions
All authors have read and agreed to the published version of the manuscript.
Funding
GK acknowledges lab support provided by grants from the Icelandic Research Fund (217946-051), Icelandic Cancer Society Research Fund and University of Iceland Research Fund.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ. (2017) 8:33. doi: 10.1186/s13293-017-0152-8
2. Murphy E. Estrogen signaling and cardiovascular disease. Circ Res. (2011) 109:687–96. doi: 10.1161/CIRCRESAHA.110.236687
3. Murphy E, Steenbergen C. Estrogen regulation of protein expression and signaling pathways in the heart. Biol Sex Differ. (2014) 5:6. doi: 10.1186/2042-6410-5-6
4. Menazza S, Murphy E. The expanding complexity of estrogen receptor signaling in the cardiovascular system. Circ Res. (2016) 118:994–1007. doi: 10.1161/CIRCRESAHA.115.305376
5. Puglisi R, Mattia G, Care A, Marano G, Malorni W, Matarrese P. Non-genomic effects of estrogen on cell homeostasis and remodeling with special focus on cardiac ischemia/reperfusion injury. Front Endocrinol. (2019) 10:733. doi: 10.3389/fendo.2019.00733
6. Lowe DA, Kararigas G. Editorial: new insights into estrogen/estrogen receptor effects in the cardiac and skeletal muscle. Front Endocrinol. (2020) 11:141. doi: 10.3389/fendo.2020.00141
7. Schubert C, Raparelli V, Westphal C, Dworatzek E, Petrov G, Kararigas G, et al. Reduction of apoptosis and preservation of mitochondrial integrity under ischemia/reperfusion injury is mediated by estrogen receptor beta. Biol Sex Differ. (2016) 7:53. doi: 10.1186/s13293-016-0104-8
8. Mahmoodzadeh S, Dworatzek E. The role of 17β-estradiol and estrogen receptors in regulation of Ca(2+) channels and mitochondrial function in cardiomyocytes. Front Endocrinol. (2019) 10:310. doi: 10.3389/fendo.2019.00310
9. Sickinghe AA, Korporaal SJA, den Ruijter HM, Kessler EL. Estrogen contributions to microvascular dysfunction evolving to heart failure with preserved ejection fraction. Front Endocrinol. (2019) 10:442. doi: 10.3389/fendo.2019.00442
10. Ventura-Clapier R, Piquereau J, Veksler V, Garnier A. Estrogens, estrogen receptors effects on cardiac and skeletal muscle mitochondria. Front Endocrinol. (2019) 10:557. doi: 10.3389/fendo.2019.00557
11. Zhang B, Miller VM, Miller JD. Influences of sex and estrogen in arterial and valvular calcification. Front Endocrinol. (2019) 10:622. doi: 10.3389/fendo.2019.00622
12. Kararigas G, Fliegner D, Forler S, Klein O, Schubert C, Gustafsson JA, et al. Comparative proteomic analysis reveals sex and estrogen receptor beta effects in the pressure overloaded heart. J Proteome Res. (2014) 13:5829–36. doi: 10.1021/pr500749j
13. Kararigas G, Fliegner D, Gustafsson JA, Regitz-Zagrosek V. Role of the estrogen/estrogen-receptor-beta axis in the genomic response to pressure overload-induced hypertrophy. Physiol Genomics. (2011) 43:438–46. doi: 10.1152/physiolgenomics.00199.2010
14. Kararigas G, Nguyen BT, Jarry H. Estrogen modulates cardiac growth through an estrogen receptor alpha-dependent mechanism in healthy ovariectomized mice. Mol Cell Endocrinol. (2014) 382:909–14. doi: 10.1016/j.mce.2013.11.011
15. Kararigas G, Nguyen BT, Zelarayan LC, Hassenpflug M, Toischer K, Sanchez-Ruderisch H, et al. Genetic background defines the regulation of postnatal cardiac growth by 17β-estradiol through a beta-catenin mechanism. Endocrinology. (2014) 155:2667–76. doi: 10.1210/en.2013-2180
16. Sanchez-Ruderisch H, Queiros AM, Fliegner D, Eschen C, Kararigas G, Regitz-Zagrosek V. Sex-specific regulation of cardiac microRNAs targeting mitochondrial proteins in pressure overload. Biol Sex Differ. (2019) 10:8. doi: 10.1186/s13293-019-0222-1
17. Duft K, Schanz M, Pham H, Abdelwahab A, Schriever C, Kararigas G, et al. 17β-estradiol-induced interaction of estrogen receptor alpha and human atrial essential myosin light chain modulates cardiac contractile function. Basic Res Cardiol. (2017) 112:1. doi: 10.1007/s00395-016-0590-1
18. Lai S, Collins BC, Colson BA, Kararigas G, Lowe DA. Estradiol modulates myosin regulatory light chain phosphorylation and contractility in skeletal muscle of female mice. Am J Physiol Endocrinol Metab. (2016) 310:E724–33. doi: 10.1152/ajpendo.00439.2015
19. Mahmoodzadeh S, Pham TH, Kuehne A, Fielitz B, Dworatzek E, Kararigas G, et al. 17beta-Estradiol-induced interaction of ERalpha with NPPA regulates gene expression in cardiomyocytes. Cardiovasc Res. (2012) 96:411–21. doi: 10.1093/cvr/cvs281
20. Nguyen BT, Kararigas G, Jarry H. Dose-dependent effects of a genistein-enriched diet in the heart of ovariectomized mice. Genes Nutr. (2012) 8:383–90. doi: 10.1007/s12263-012-0323-5
21. Nguyen BT, Kararigas G, Wuttke W, Jarry H. Long-term treatment of ovariectomized mice with estradiol or phytoestrogens as a new model to study the role of estrogenic substances in the heart. Planta Med. (2012) 78:6–11. doi: 10.1055/s-0031-1280228
22. Beikoghli Kalkhoran S, Kararigas G. Oestrogenic Regulation of Mitochondrial Dynamics. Int J Mol Sci. (2022) 23:1118. doi: 10.3390/ijms23031118
23. Kararigas G, Becher E, Mahmoodzadeh S, Knosalla C, Hetzer R, Regitz-Zagrosek V. Sex-specific modification of progesterone receptor expression by 17β-oestradiol in human cardiac tissues. Biol Sex Differ. (2010) 1:2. doi: 10.1186/2042-6410-1-2
24. Kararigas G, Bito V, Tinel H, Becher E, Baczko I, Knosalla C, et al. Transcriptome characterization of estrogen-treated human myocardium identifies Myosin regulatory light chain interacting protein as a sex-specific element influencing contractile function. J Am Coll Cardiol. (2012) 59:410–7. doi: 10.1016/j.jacc.2011.09.054
25. Hein S, Hassel D, Kararigas G. The zebrafish (Danio rerio) is a relevant model for studying sex-specific effects of 17β-estradiol in the adult heart. Int J Mol Sci. (2019) 20:6287. doi: 10.3390/ijms20246287
26. Fliegner D, Schubert C, Penkalla A, Witt H, Kararigas G, Dworatzek E, et al. Female sex and estrogen receptor-beta attenuate cardiac remodeling and apoptosis in pressure overload. Am J Physiol Regul Integr Comp Physiol. (2010) 298:R1597–606. doi: 10.1152/ajpregu.00825.2009
27. Queiros AM, Eschen C, Fliegner D, Kararigas G, Dworatzek E, Westphal C, et al. Sex- and estrogen-dependent regulation of a miRNA network in the healthy and hypertrophied heart. Int J Cardiol. (2013) 169:331–8. doi: 10.1016/j.ijcard.2013.09.002
28. Kararigas G. Oestrogenic contribution to sex-biased left ventricular remodelling: the male implication. Int J Cardiol. (2021) 343:83–4. doi: 10.1016/j.ijcard.2021.09.020
29. Sabbatini AR, Kararigas G. Estrogen-related mechanisms in sex differences of hypertension and target organ damage. Biol Sex Differ. (2020) 11:31. doi: 10.1186/s13293-020-00306-7
30. Sabbatini AR, Kararigas G. Menopause-related estrogen decrease and the pathogenesis of HFpEF: JACC review topic of the week. J Am Coll Cardiol. (2020) 75:1074–82. doi: 10.1016/j.jacc.2019.12.049
31. Maas A, Rosano G, Cifkova R, Chieffo A, van Dijken D, Hamoda H, et al. Cardiovascular health after menopause transition, pregnancy disorders, and other gynaecologic conditions: a consensus document from European cardiologists, gynaecologists, and endocrinologists. Eur Heart J. (2021) 42:967–84. doi: 10.1093/eurheartj/ehaa1044
32. Dworatzek E, Mahmoodzadeh S, Schriever C, Kusumoto K, Kramer L, Santos G, et al. Sex-specific regulation of collagen I and III expression by 17β-estradiol in cardiac fibroblasts: role of estrogen receptors. Cardiovasc Res. (2019) 115:315–27. doi: 10.1093/cvr/cvy185
33. Dworatzek E, Baczko I, Kararigas G. Effects of aging on cardiac extracellular matrix in men and women. Proteomics Clin Appl. (2016) 10:84–91. doi: 10.1002/prca.201500031
34. Kim JK, Pedram A, Razandi M, Levin ER. Estrogen prevents cardiomyocyte apoptosis through inhibition of reactive oxygen species and differential regulation of p38 kinase isoforms. J Biol Chem. (2006) 281:6760–7. doi: 10.1074/jbc.M511024200
35. Ruiz-Larrea MB, Martin C, Martinez R, Navarro R, Lacort M, Miller NJ. Antioxidant activities of estrogens against aqueous and lipophilic radicals; differences between phenol and catechol estrogens. Chem Phys Lipids. (2000) 105:179–88. doi: 10.1016/S0009-3084(00)00120-1
36. Hartman RJG, Owsiany K, Ma L, Koplev S, Hao K, Slenders L, et al. Sex-stratified gene regulatory networks reveal female key driver genes of atherosclerosis involved in smooth muscle cell phenotype switching. Circulation. (2021) 143:713–26. doi: 10.1161/CIRCULATIONAHA.120.051231
37. Ferrini RL, Barrett-Connor E. Sex hormones and age: a cross-sectional study of testosterone and estradiol and their bioavailable fractions in community-dwelling men. Am J Epidemiol. (1998) 147:750–4. doi: 10.1093/oxfordjournals.aje.a009519
38. Carlson LE, Sherwin BB. Higher levels of plasma estradiol and testosterone in healthy elderly men compared with age-matched women may protect aspects of explicit memory. Menopause. (2000) 7:168–77. doi: 10.1097/00042192-200007030-00007
39. Abbott RD, Launer LJ, Rodriguez BL, Ross GW, Wilson PW, Masaki KH, et al. Serum estradiol and risk of stroke in elderly men. Neurology. (2007) 68:563–8. doi: 10.1212/01.wnl.0000254473.88647.ca
40. Jankowska EA, Rozentryt P, Ponikowska B, Hartmann O, Kustrzycka-Kratochwil D, Reczuch K, et al. Circulating estradiol and mortality in men with systolic chronic heart failure. JAMA. (2009) 301:1892–901. doi: 10.1001/jama.2009.639
Keywords: cardiac, heart failure, steroid hormone, vasculature, transgender
Citation: den Ruijter HM and Kararigas G (2022) Estrogen and Cardiovascular Health. Front. Cardiovasc. Med. 9:886592. doi: 10.3389/fcvm.2022.886592
Received: 28 February 2022; Accepted: 14 March 2022;
Published: 30 March 2022.
Edited by:
Emma Louise Robinson, University of Colorado, United StatesReviewed by:
Susana Novella, University of Valencia, SpainCopyright © 2022 den Ruijter and Kararigas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Georgios Kararigas, Z2Vvcmdla2FyYXJpZ2FzQGdtYWlsLmNvbQ==
 Hester M. den Ruijter
Hester M. den Ruijter Georgios Kararigas
Georgios Kararigas