
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Cardiovasc. Med. , 19 May 2022
Sec. Thrombosis and Haemostasis
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.874795
This article is part of the Research Topic Anticoagulation in Cardiovascular Diseases: Evolving role, unmet needs and grey areas View all 26 articles
Background: The use of anticoagulants is an established strategy to prevent stroke, embolism, and cardiovascular mortality in patients with atrial fibrillation (AF), but its role in the prevention of incident diabetes is unclear. We aimed to investigate this question by using participant data from cohort studies.
Methods: We conducted a meta-analysis of participants to investigate the impact of direct oral anticoagulants (DOACs) on the risk of new-onset diabetes in AF patients. The collection of related data was performed in the PubMed and EMBASE databases until December 2021, including studies associated with evaluating the correlation between DOACs and incident diabetes. The hazard ratios (HRs) and 95% confidence intervals (CIs) were adjusted by the random-effects model with an inverse variance method.
Results: Two cohort studies with a total of 24,434 patients were included in this study (warfarin: n = 6,906; DOACs: n = 17,528). Compared with warfarin, the use of DOACs could reduce the incident diabetic risk in AF patients (HR = 0.75, 95%CI: 0.68–0.82). Investigations about the effects of three major classes of DOACs showed that the individual use of dabigatran (HR = 0.76, 95%CI: 0.64–0.90), rivaroxaban (HR = 0.74, 95%CI: 0.64–0.87), apixaban (HR = 0.74, 95%CI: 0.60–0.92) and the combined use of rivaroxaban and apixaban (HR = 0.74, 95%CI: 0.66–0.84) could reduce the risk of new-onset diabetes compared with warfarin. This risk reduction effect could be observed in both male and female groups (HR = 0.73, 95%CI: 0.64–0.84, P < 0.00001; HR = 0.82, 95%CI: 0.82–0.99, P = 0.04).
Conclusions: Treatment with DOACs compared with warfarin reduced the risk of new-onset diabetes in both male and female patients with AF.
Atrial fibrillation (AF) is the most common cardiac arrhythmia in the clinic, characterized by high rates of thromboembolic complications and related mortality.
An integrated approach of AF care mainly contains rhythm and rate control therapy, anticoagulation therapy (OAC), and comprehensive upstream therapy (1). Among them, OAC is of vital importance in AF-related stroke prevention. As a traditional oral anticoagulant, vitamin K antagonists such as warfarin plays their role by antagonizing vitamin K epoxide reductase complex. Warfarin has a narrow therapeutic range, multiple drug and food interactions, and requires frequent blood monitoring of the international normalized ratio (INR) (2). Therefore, direct oral anticoagulants (DOACs, sometimes referred to as non-vitamin K antagonist anticoagulants) have been introduced in the clinic, reducing the risk of stroke or systemic embolism and bleeding compared with warfarin among patients with AF (3–5).
Patients with comorbid AF and DM have a higher risk of stroke, thromboembolism, and cardiovascular mortality (3, 6–9). Vitamin K has been suggested to regulate the activity of vitamin K-dependent proteins (VKDP) such as osteocalcin, which effectively improve β cell proliferation and insulin secretion to reduce the risk of new-onset DM (9–14). Due to the different effects of warfarin and DOACs on vitamin K, the use of DOACs was considered with the potential of reducing DM risk in AF patients. Two cohort studies have been conducted to compare the risk of DM induction in AF patients treated by warfarin and DOACs (9, 15). The study of Cheung et al. included the data of 13,688 DOACs new users from the Clinical Data Analysis and Reporting System (CDARS) managed by the Hong Kong Hospital Authority (HA). Their results showed that dabigatran was significantly related to incident diabetes risk reduction, and for Xa inhibitor anticoagulants, only the combination use of rivaroxaban and apixaban rather than individual drugs could decrease this risk. In this study, males were the only gender with a diabetic risk-reduction effect. While in a cohort analysis performed by Huang et al., a total of 10,746 AF patients from Taiwan’s National Health Insurance Research Database (NHIRD) were fitted into the study. All of the three different DOACs (dabigatran, rivaroxaban, apixaban) were reported with the incident diabetic reduction effect compared with warfarin. In this study, a similar trend of lowering new-onset DM risk was observed in both male and female groups treated with DOAC vs. warfarin. We used individual participants’ data from the two cohort studies to assess the impact of DOACs on new-onset diabetes risk in AF patients.
The preferred reporting items for systematic review and meta-analysis (PRISMA) 2020 guidelines were used to conduct our present meta-analysis. Only published publications were included in our meta-analysis, so we did not need ethical permission. Readers can contact the corresponding authors for data, techniques, and materials to recreate the results or the program.
Two databases PubMed and Embase were used for systemic search in this study, retrieval keywords included (1) atrial fibrillation OR AF AND (2) incident diabetes OR new-onset diabetes AND (3) Direct oral anticoagulants OR DOAC OR DOAC OR oral anticoagulants OR dabigatran OR rivaroxaban OR apixaban AND (4) vitamin K antagonists OR warfarin OR VKA.
The literature inclusion criteria of this study include (1) randomized controlled trials or observational cohort studies focusing on the risk of developing DM in AF patients treated by warfarin vs. DOACs (Apixaban, dabigatran, rivaroxaban or edoxaban), (2) The outcomes of studies include the appearance of new-onset diabetes, which meets the International Classification of Diseases, the use of anti-diabetic medication, or death occurred during the investigation period. (3) All of the patients included in the cohort study were treated with at least one type of anticoagulant after AF diagnosis. The clinical follow-up time was unlimited. Specific literature forms including reviews, case reports, case series, editorials, meeting abstracts, and insufficient clinical data were excluded.
Two independent researchers extracted data independently through screening the titles and abstracts to select potential studies for meta-analysis. Then full-text screening was carried out subsequently. Controversies were resolved by discussing with the third researcher. If multiple screened studies suitable for meta-analysis were from the same data source, the study that was more in line with predefined criteria was included. Studies with later publication years and longer follow-up times were preferentially included. The relevant information of each available study included the first author, publication year, study design, outcomes, types of DOACs, follow-up period, the sample size and the number of events in the warfarin or DOACs groups, hazard ratio (HR) and 95% confidence intervals (CI) were collected independently by the fourth author.
Newcastle-Ottawa Scale (NOS) was used by authors to assess the quality of included studies. A total of nine points were divided into three domains, including the cohort selection (0–4 points), cohort comparability (0–2 points), and the outcomes evaluation (0–3 points) were assessed by the NOS tool. Studies with the NOS results < 6 points were considered as low quality.
We chose the Cochrane Q-test and I2 statistic to assess the consistency of the included studies. A P < 0.1 for the Q-test or I2 ≥ 50% result was considered as the existence of substantial heterogeneity. The Review Manager Version 5.3 (The Nordic Cochrane Center, The Cochrane Collaboration, 2014, Copenhagen, Denmark1) was used for all statistical analyses; P < 0.05 was considered statistically significant. First, we collected the sample size and number of events in the warfarin or DOACs groups, then the crude events rates of DM induction risk were carried out and expressed by HRs and 95% CIs. Second, the HR of DM induction was calculated in both the warfarin group and DOACs group with respect to gender differences. The adjusted HRs were converted to the natural logarithms and standard errors. The inverse variance method was used to incorporate random effect models.
The retrieval flow chart of this meta-analysis is shown in Figure 1. A total of 205 studies were acquired through online searching in the PubMed and Embase databases. After removing repeated investigations, 25 studies were chosen to develop title/abstract screening. Then 10 studies were evaluated in detail. On the basis of predefined criteria, finally, two eligible cohort studies were included in our meta-analysis (9, 15). Exhibited in Table 1 was the baseline information of patients in the included studies. A total of 24,434 individual participants (warfarin: n = 6,906; DOACs: n = 17,528) from two cohort studies were included in our meta-analysis. The data of included cohort studies were from Taiwan’s National Health Insurance Research Database (NHIRD) and Clinical Data Analysis and Reporting System (CDARS) managed by the Hong Kong Hospital Authority (HA). Their study periods were not less than 5 years and the medical use conditions that may influence patients’ DM risk were recorded in the baseline characteristic table. Both of these two studies could meet our screening criteria. For the quality assessment, the NOS scores of both included studies were ≥ 6 points. The number of included studies was less than 10. Thus, there was no need for publication bias assessment.
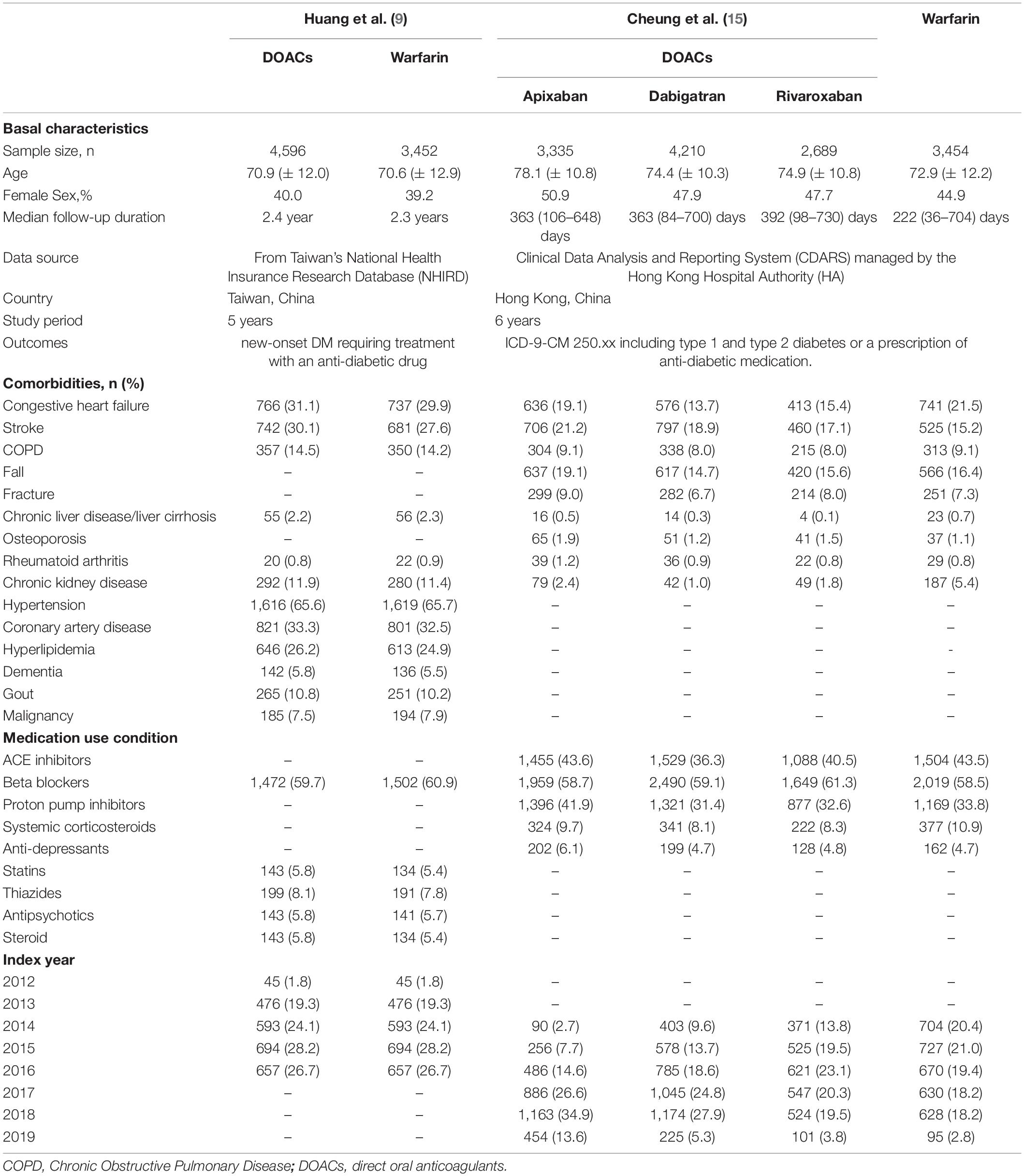
Table 1. Main baseline characteristics of DOACs and warfarin treated patients in the included cohort studies.
The crude rates of the occurrence of the incident DM in AF patients treated by warfarin or DOACs were reported in both cohort studies, shown in Table 2. Compared with warfarin, the incidence of new-onset diabetes was relatively lower in DOACs treated group (6.78% vs 7.68%). Both coagulation factor Xa inhibitors apixaban (5.38% vs 6.14%), rivaroxaban (8.03% vs 8.05%) and thrombin inhibitor dabigatran (6.73% vs 8.49%) show the effectiveness in reducing the incidence of new-onset diabetes in AF patients, and this effect in coagulation factor Xa inhibitors combination group also exist (6.82% vs 7.23%).
Both included studies have reported the adjusted data of new-onset DM in AF patients treated by DOACs vs warfarin (9, 15). The outcomes displayed in Figure 2 were able to confirm that compared with warfarin, DOACs can reduce the risk of diabetes in AF patients (HR = 0.75, 95%CI: 0.68–0.82). Moreover, the outcomes of the gender subgroup according to the included studies are shown in Supplementary Figure 1. Compared with warfarin, the tendency of DOACs to reduce the incidence of new-onset diabetes can be observed in both male and female groups (male: HR = 0.73, 95%CI: 0.24–0.84; female: HR = 0.82, 95%CI: 0.68–0.99).
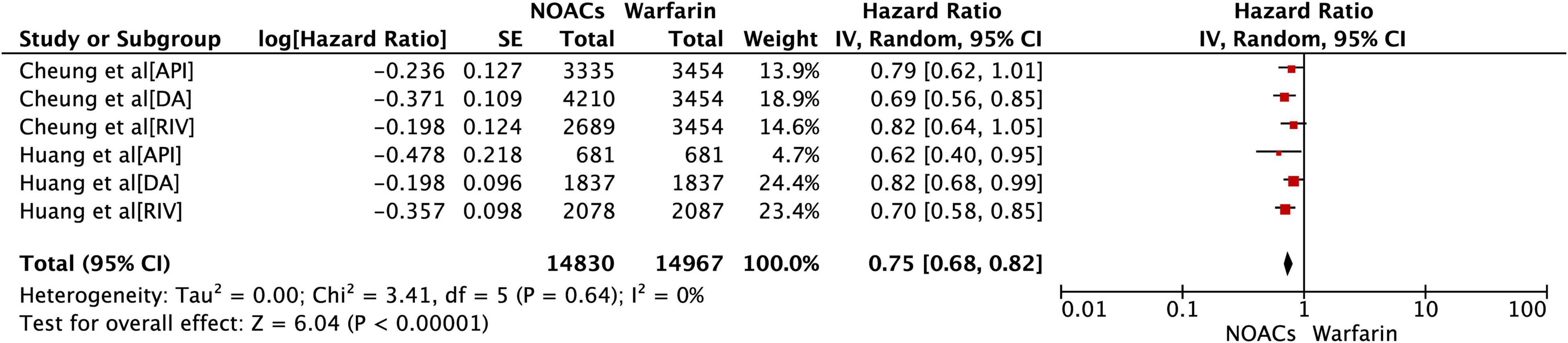
Figure 2. Comparing the primary outcomes of incident diabetes in DOACs vs. warfarin. DOACs, direct oral anticoagulants; HR, hazard ratio; CI, confidence interval; SE, standard error; IV, inverse of the variance.
As shown in Table 2, the subgroup analysis of different types of DOAC were also analyzed in our study. All of the three evaluated DOACs associated with the decreased risk of inducing incident diabetes (Apixaban: HR = 0.74, 95% CI: 0.60–0.92; Dabigatran: HR = 0.76, 95% CI: 0.66–0.88; Rivaroxaban: HR = 0.74, 95% CI: 0.64–0.86). After pooling the data of rivaroxaban and apixaban, a similar effect could also be detected (HR = 0.74, 95% CI: 0.66–0.84), which confirms the reducing-effect of coagulation factor Xa inhibitors on the risk of new onset diabetes.
The primary findings of this study included (1) Compared with warfarin, DOACs including thrombin inhibitor dabigatran, coagulation factor Xa inhibitor rivaroxaban and apixaban could reduce the risk of new-onset diabetes in AF patients. (2) The DM-reduced effect of DOACs vs. warfarin can be observed in both male and female groups.
Compared with DOACs, warfarin has various limitations in the process of anticoagulant treatment. The changing international standardized ratio (INR) control and dose adjustment, various dietary or drug interactions (16, 17), narrow therapeutic window (17) result in the restrictions of warfarin in clinical use. Several meta-analyses and randomized controlled trials have reported the contrasts with the effectiveness and safety between DOACs and warfarin (18–20). The role of reducing AF and diabetes-associated risk factors including major bleeding, renal decline and cardiac valve calcification can be observed in the use of DOACs rather than warfarin (21–25).
Warfarin plays its role by antagonizing vitamin K, which is an important influence factor of glucose homeostasis and insulin sensitivity. In animal tissues, vitamin K homolog menaquinone-4 (MK-4) might act as an incretin-like nutrient and a cofactor of microsomal γ-glutamyl carboxylase (14, 26, 27). It contributes to the post-translational carboxylation process of transferring glutamate to γ-carboxyglutamate (Gla) residues of VKDP. Insulin production could be promoted by VKDP–osteoblast-specific secreted osteocalcin in a bone-pancreas endocrine loop to regulate glucose metabolism (14). The insulin resistance ameliorating effect of vitamin K was suggested through the inactivation of the NF-κβ signaling pathway to inhibit inflammatory responses and lipid-decreasing effect (11, 12). Considering the vitamin K antagonizing function of warfarin, it can influence the incidence of diabetes. However, the anticoagulation process of DOACs does not influence the vitamin K concentration in the circulatory system. Therefore, using DOACs compared with warfarin could reduce the risk of new-onset diabetes in AF patients.
In 2017, a novel drug betrixaban was approved by FDA as the fifth DOAC that can be used in clinic. With low renal clearance and minimal hepatic metabolism, betrixaban was considered particularly beneficial for patients with renal or hepatic dysfunction (28). However, the lack of an effective reversal agent makes betrixaban has a longer terminal half-life compared with other approved DOACs (28, 29). The impact of betrixaban on the risk of new-onset diabetes has not been evaluated in current studies, and the relevant results are expected to be supplemented in the future.
Our study was based on two cohort studies with a total sample size of 24,434, which is the most comprehensive and latest study according to the risk of DOACs vs. warfarin in inducing new-onset diabetes in AF patients. The result in the cohort study from Cheung et al. (15) proposed that only dabigatran was significantly associated with incident diabetes risk reduction, our results support that three of existing approved DOAC dabigatran, apixaban, and rivaroxaban with the function of reducing incident diabetic risk. At the same time, this effect in factor Xa inhibitors rivaroxaban and apixaban were not obvious, and our findings confirmed that all of these three drugs with the risk reduction ability. Also, in the outcomes of Cheung et al., only a specific gender of AF patients with the advantage of incident diabetic risk reduction in DOACs treatment, whereas the result of our investigation suggested that this effect could be observed in both male and female groups. In addition, the estimated crude events rates of new-onset diabetes were evaluated during our investigation process. Although available data is insufficient to support the effect of vitamin K in ameliorating prediabetes (the impaired glucose tolerance, fasting blood sugar, fasting serum insulin level would not be restored), the glucose and insulin levels of 2-h post-oral glucose tolerance test could be reduced by stable vitamin K support (10, 30, 31), which indicate that DOACs may not induce the rapid deterioration of prediabetes compared with warfarin. Also, the clinical trials have demonstrated that the new anti-diabetic drug sodium-glucose linked transporter inhibitors (SGLTi) with a beneficial effect on cardiovascular disease (32–34), regardless if diabetes exists or not (34). In the aspect of AF, SGLTi can counteract the production of cellular ROS in cardiomyocytes, which may change atrial remodeling and reduce the burden of AF (34). This suggests that the new anti-diabetic drug SGLTi and new oral anticoagulants DOAC may have similar effects on the prevention of new-onset diabetes during AF treatment.
The results of our study suggested that DOACs could reduce the risk of incident diabetes, which is probably more suitable for AF patients with a higher risk of new-onset diabetes. More prospective clinical data about the risk of incident DM in AF patients treated by DOACs and warfarin could prove our point.
This meta-analysis still had several limitations: (1) Only two cohort studies were included in our study, and the data were relatively limited, therefore the evaluation of the effect of edoxaban and betrixaban on incident diabetes was not supported. (2) The included population in our study only contain AF patients from Hong Kong and Taiwan, thus the evaluation of new-onset diabetes risk just considered Asian AF patients. (3) The subtypes of DM were not be distinguished in this study, whether DOACs have the same effect in reducing the risk of type 1 and type 2 diabetes in AF patients is still not clear. (4) The confounding factors cannot be completely excluded in observational studies. According to clinical guidelines, patients with rheumatic heart disease, congenital heart disease, or valve replacement surgery are more likely to be treated with warfarin rather than DOAC (9). This group that may induce selection bias was not completely excluded in our study. Future research could carry out propensity score matching on the basis of incorporating more data to minimize the impact of confounding factors.
Our findings of current analysis suggested that treatment with DOACs compared with warfarin reduced the risk of new-onset diabetes in both male and female patients with AF.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
This study was funded by the National Natural Science Foundation of China (82100273).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.874795/full#supplementary-material
1. Lip GYH. The ABC pathway: an integrated approach to improve AF management. Nat Rev Cardiol. (2017) 14:627–8. doi: 10.1038/nrcardio.2017.153
3. Itzhaki Ben Zadok O, Eisen A. Use of non-vitamin K oral anticoagulants in people with atrial fibrillation and diabetes mellitus. Diabet Med. (2018) 35:548–56. doi: 10.1111/dme.13600
4. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update: a report from the American heart association. Circulation. (2016) 133:e38–360.
5. Grymonprez M, Simoens C, Steurbaut S, De Backer TL, Lahousse L. Worldwide trends in oral anticoagulant use in patients with atrial fibrillation from 2010 to 2018: a systematic review and meta-analysis. Europace. (2021). doi: 10.1093/europace/euab303 [Epub ahead of print].
6. Plitt A, Zelniker TA, Park JG, McGuire DK, Ruff CT, Antman EM, et al. Patients with diabetes mellitus and atrial fibrillation treated with non-vitamin K antagonist oral anticoagulants: meta-analysis of eight outcomes in 58 634 patients across four randomized controlled trials. Eur Heart J Cardiovasc Pharmacother. (2021) 7:f40–9. doi: 10.1093/ehjcvp/pvaa120
7. Korgaonkar S, Yang Y, Banahan B, Bentley JP. Comparative effectiveness and safety of non-vitamin-K antagonist oral anticoagulants and warfarin in older adults with atrial fibrillation and diabetes. Curr Med Res Opin. (2021) 37:343–56. doi: 10.1080/03007995.2020.1865748
8. Wang A, Green JB, Halperin JL, Piccini JP.Sr Atrial fibrillation and diabetes mellitus: JACC review topic of the week. J Am Coll Cardiol. (2019) 74:1107–15. doi: 10.1016/j.jacc.2019.07.020
9. Huang HK, Liu PP, Lin SM, Hsu JY, Peng CC, Munir KM, et al. Risk of developing diabetes in patients with atrial fibrillation taking non-vitamin K antagonist oral anticoagulants or warfarin: a nationwide cohort study. Diabetes Obes Metab. (2021) 23:499–507. doi: 10.1111/dom.14243
10. Karamzad N, Maleki V, Carson-Chahhoud K, Azizi S, Sahebkar A, Gargari BP. A systematic review on the mechanisms of vitamin K effects on the complications of diabetes and pre-diabetes. Biofactors. (2020) 46:21–37. doi: 10.1002/biof.1569
11. Manna P, Kalita J. Beneficial role of vitamin K supplementation on insulin sensitivity, glucose metabolism, and the reduced risk of type 2 diabetes: a review. Nutrition. (2016) 32:732–9. doi: 10.1016/j.nut.2016.01.011
12. Li Y, Chen JP, Duan L, Li S. Effect of vitamin K2 on type 2 diabetes mellitus: a review. Diabetes Res Clin Pract. (2018) 136:39–51. doi: 10.1016/j.diabres.2017.11.020
13. Rahimi Sakak F, Moslehi N, Niroomand M, Mirmiran P. Glycemic control improvement in individuals with type 2 diabetes with vitamin K2 supplementation: a randomized controlled trial. Eur J Nutr. (2021) 60:2495–506. doi: 10.1007/s00394-020-02419-6
14. Ho HJ, Komai M, Shirakawa H. Beneficial effects of vitamin K status on glycemic regulation and diabetes mellitus: a mini-review. Nutrients. (2020) 12:2485. doi: 10.3390/nu12082485
15. Cheung CL, Sing CW, Lau WCY, Li GHY, Lip GYH, Tan KCB, et al. Treatment with direct oral anticoagulants or warfarin and the risk for incident diabetes among patients with atrial fibrillation: a population-based cohort study. Cardiovasc Diabetol. (2021) 20:71. doi: 10.1186/s12933-021-01263-0
16. Liu F, Xu Z, Luo J, Yu P, Ma J, Yuan P, et al. Effectiveness and safety of DOACs vs. VKAs in AF patients with cancer: evidence from randomized clinical trials and observational studies. Front Cardiovasc Med. (2021) 8:766377. doi: 10.3389/fcvm.2021.766377
17. Vranckx P, Valgimigli M, Heidbuchel H. The significance of drug-drug and drug-food interactions of oral anticoagulation. Arrhythm Electrophysiol Rev. (2018) 7:55–61. doi: 10.15420/aer.2017.50.1
18. Bang OY, On YK, Lee MY, Jang SW, Han S, Han S, et al. The risk of stroke/systemic embolism and major bleeding in Asian patients with non-valvular atrial fibrillation treated with non-vitamin K oral anticoagulants compared to warfarin: results from a real-world data analysis. PLoS One. (2020) 15:e0242922. doi: 10.1371/journal.pone.0242922
19. Balsam P, Ozieranski K, Tyminska A, Zukowska K, Zaleska M, Szepietowska K, et al. Comparison of clinical characteristics of real-life atrial fibrillation patients treated with vitamin K antagonists, dabigatran, and rivaroxaban: results from the CRAFT study. Kardiol Pol. (2018) 76:889–98. doi: 10.5603/KP.a2018.0027
20. Cha MJ, Choi EK, Han KD, Lee SR, Lim WH, Oh S, et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in Asian patients with atrial fibrillation. Stroke. (2017) 48:3040–8. doi: 10.1161/strokeaha.117.018773
21. Yu YB, Liu J, Fu GH, Fang RY, Gao F, Chu HM. Comparison of dabigatran and warfarin used in patients with non-valvular atrial fibrillation: meta-analysis of random control trial. Medicine (Baltimore). (2018) 97:e12841. doi: 10.1097/MD.0000000000012841
22. Shahzada TS, Guo CL, Lee APW. Renal outcomes in Asian patients receiving oral anticoagulants for non-valvular atrial fibrillation. Hong Kong Med J. (2021) 28:24–32. doi: 10.12809/hkmj209201
23. Liu F, Yang Y, Cheng W, Ma J, Zhu W. Reappraisal of non-vitamin K antagonist oral anticoagulants in atrial fibrillation patients: a systematic review and meta-analysis. Front Cardiovasc Med. (2021) 8:757188. doi: 10.3389/fcvm.2021.757188
24. Di Lullo L, Lavalle C, Magnocavallo M, Mariani MV, Della Rocca DG, Severino P, et al. New evidence of direct oral anticoagulation therapy on cardiac valve calcifications, renal preservation and inflammatory modulation. Int J Cardiol. (2021) 345:90–7. doi: 10.1016/j.ijcard.2021.10.025
25. Alappan HR, Kaur G, Manzoor S, Navarrete J, O’Neill WC. Warfarin accelerates medial arterial calcification in humans. Arterioscler Thromb Vasc Biol. (2020) 40:1413–9. doi: 10.1161/ATVBAHA.119.313879
26. Pittas AG, Harris SS, Eliades M, Stark P, Dawson-Hughes B. Association between serum osteocalcin and markers of metabolic phenotype. J Clin Endocrinol Metab. (2009) 94:827–32. doi: 10.1210/jc.2008-1422
27. Mokgalaboni K, Nkambule BB, Ntamo Y, Ziqubu K, Nyambuya TM, Mazibuko-Mbeje SE, et al. Vitamin K: a vital micronutrient with the cardioprotective potential against diabetes-associated complications. Life Sci. (2021) 286:120068. doi: 10.1016/j.lfs.2021.120068
28. Thoenes M, Minguet J, Bramlage K, Bramlage P, Ferrero C. Betrixaban - the next direct factor Xa inhibitor? Expert Rev Hematol. (2016) 9:1111–7. doi: 10.1080/17474086.2016.1256194
29. Lee K, Cham S, Lam S. Betrixaban: a novel factor Xa inhibitor for the prevention of venous thromboembolism in acutely Ill medical patients. Cardiol Rev. (2018) 26:331–8. doi: 10.1097/CRD.0000000000000227
30. Rasekhi H, Karandish M, Jalali MT, Mohammadshahi M, Zarei M, Saki A, et al. Phylloquinone supplementation improves glycemic status independent of the effects of adiponectin levels in premonopause women with prediabetes: a double-blind randomized controlled clinical trial. J Diabetes Metab Disord. (2015) 14:1. doi: 10.1186/s40200-014-0127-9
31. Rasekhi H, Karandish M, Jalali MT, Mohammad-Shahi M, Zarei M, Saki A, et al. The effect of vitamin K1 supplementation on sensitivity and insulin resistance via osteocalcin in prediabetic women: a double-blind randomized controlled clinical trial. Eur J Clin Nutr. (2015) 69:891–5. doi: 10.1038/ejcn.2015.17
32. Chaurasia PP, Dholariya S, Kotadiya F, Bhavsar M. A new hope in type 2 diabetes mellitus management: sodium-glucose cotransporter 2 inhibitors. Cureus. (2021) 13:e18300. doi: 10.7759/cureus.18300
33. Ferreira JP, Oliveira AC, Saraiva FA, Vasques-Novoa F, Leite-Moreira A. Sodium-glucose co-transporter inhibitors in insulin-treated diabetes: a meta-analysis. Eur J Endocrinol. (2021) 184:783–90. doi: 10.1530/EJE-20-1484
Keywords: atrial fibrillation, non-vitamin K antagonist oral anticoagulants, diabetes mellitus, warfarin, meta-analysis
Citation: Liu X, Feng S, Chen Z, Zhou Y, Yin K, Xue Z and Zhu W (2022) Is the Risk of Diabetes Lower in Patients With Atrial Fibrillation Treated With Direct Oral Anticoagulant Compared to Warfarin? Front. Cardiovasc. Med. 9:874795. doi: 10.3389/fcvm.2022.874795
Received: 13 February 2022; Accepted: 25 April 2022;
Published: 19 May 2022.
Edited by:
Antonino Tuttolomondo, University of Palermo, ItalyCopyright © 2022 Liu, Feng, Chen, Zhou, Yin, Xue and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kang Yin, NDc0NjE0OTA5QHFxLmNvbQ==; Zhengbiao Xue, NTc0Mzg0NDBAcXEuY29t; Wengen Zhu, NjAyNzAxOTcwQHFxLmNvbQ==; emh1d2c2QG1haWwuc3lzdS5lZHUuY24=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.