- 1CIRI – Centre International de Recherche en Infectiologie, Team GIMAP, Université de Lyon, Université Jean Monnet, Université Claude Bernard Lyon 1, Inserm, U1111, CNRS, UMR530, Saint-Étienne, France
- 2Internal Medicine Department, Saint-Etienne University Hospital, Saint-Étienne, France
- 3Amsterdam UMC, Department of Vascular Medicine, Amsterdam Cardiovascular Sciences, Amsterdam Reproduction and Development, University of Amsterdam, Amsterdam, Netherlands
The antiphospholipid syndrome is an autoimmune disease characterized by thrombosis and pregnancy morbidity. The manifestations are caused by antibodies targeting cell membrane phospholipids and/or associated proteins. The triggers leading to these antibodies' production are unknown but recent work suggests cross-reactivity between the autoantigens and peptides produced by the intestinal microbiome. Work on how the autoantibodies could cause clinical manifestations implicates different mechanisms. Binding to surface proteins of different cell types can induce intracellular signaling leading to cell activation and tissue factor expression. Complement activation and neutrophil extracellular-traps are also involved, and recent evidence implicates endothelial protein C receptor-lysobisphosphatidic acid complex. Pregnancy is a high-risk situation for antiphospholipid syndrome patients due to the increased risk of thrombosis and obstetric complications. Epidemiological and clinical research on APS is hampered by heterogeneity in populations, testing and treatment strategies. About one in 10 to one in fifty APS pregnancies is complicated by thrombosis, despite treatment. Pregnant patients with prior thrombosis are prescribed therapeutic dose heparins and low dose aspirin. Without prior thrombosis a prophylactic dose is used. The most frequent obstetrical manifestation is recurrent early pregnancy loss. The association of APS antibodies with late pregnancy loss is stronger, however. Prevention of recurrence is achieved with aspirin and prophylactic dose heparin, although the evidence is of low certainty. The third obstetrical classifying manifestation comprises preterm delivery due to placenta-mediated complications and is treated in subsequent pregnancies with aspirin with or without prophylactic dose heparin, again based on low quality evidence. New therapies are under investigation.
Introduction
Antiphospholipid syndrome (APS) is a rare autoimmune disease, whose key features are recurrent vascular thrombosis and obstetrical complications, but can also be responsible for thrombocytopenia, haemolytic anemia, cardiac valvular disease, renal thrombotic microangiopathy, neurological symptoms, cognitive impairment or pulmonary hypertension (1). It is also frequently associated with systemic lupus erythematosus, and its approximate prevalence is 40 per 100 000 individuals (2, 3).
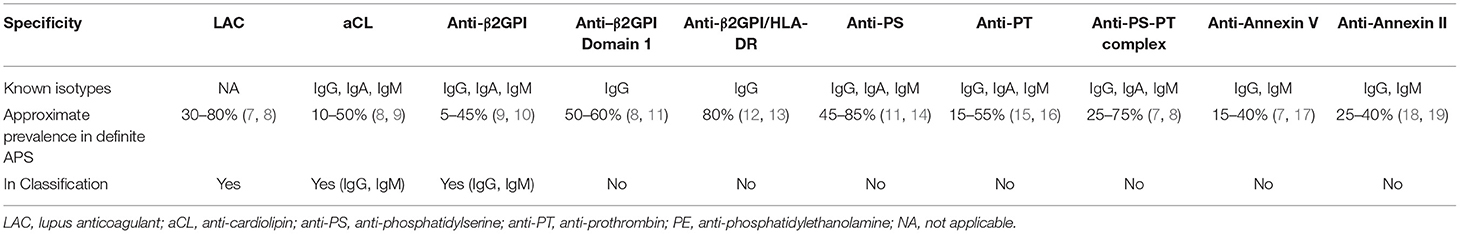
APS-specific autoimmune response is targeting components of the cell membrane i.e., phospholipids (e.g., cardiolipin) and/or their associated proteins (mainly β2-glycoprotein-I [β2GPI]) in its phospholipid-bound “activated” open conformation which is exposing cryptic epitopes in its first domain (4–6). Antiphospholipid antibodies (aPL; see Table 1), have historically been described in 1983, in Syphilis, as well as in multiple infectious diseases since (20). In such infectious setting, aPL are usually thought of as transient and non-thrombogenic, however thombotic complications have been reported in a small number of aPL-positive infection cases, possibly in autoimmunity-prone individuals (21, 22). Interestingly, aPL have recently been reported in a significant proportion (up to 30–50%) of acute COVID patients, especially in severe cases, but it is still debated whether they could be contributing to the disease prothrombotic state independently of the several potentially confounding factors (23). Of note, the aPL epitope specificity is different in COVID (i.e., rarely targeting β2GPI domain I) (24), and the autoantibody persistence over time (≥ 2 positive testing, 12 weeks apart) seems to be absent in most COVID cases (23, 25), in line with what has been described in infection-related cases (26).
Detecting aPL is primordial for diagnosing APS, but determining if these autoantibodies are culprits (aPL positivity with an APS-compatible clinical setting) or innocent bystanders (aPL positivity alone) can be complicated (23, 27). Classification criteria have been formulated during International Congresses on APS in Sapporo and Sydney, and subsequently published as consensus statements in 1999 (28) and 2006 (29), respectively. The 2006 revised classification criteria for definite APS are met when at least one clinical criterion (vascular thrombosis or pregnancy morbidity), and one biological criterion (Lupus Anticoagulant [LAC], IgM/IgG anti-cardiolipin [aCL], and/or IgM/IgG anti-2GPI positivity) are present. These criteria, which were never intended for diagnostic use, have significant drawbacks: non-inclusion of the less frequent but well-identified APS manifestations (30) or non-inclusion of “non-criteria” autoantibodies (e.g., anti-prothrombin, anti-annexin V, anti-phosphatidylserine…) (31, 32).
The objective of this mini review article is to provide a clear but concise summary regarding pregnancy-related complications in APS, particularly focusing on recent insights, research gaps and future concepts in the pathogenesis, epidemiology, prevention, and treatment of thrombotic and non-thrombotic manifestations.
Origin of APS Autoantibodies
APS pathogenesis is thought to rely upon both genetic and environmental factors, which would explain why several microorganisms can trigger transient aPL, whereas only few predisposed individuals will develop definite APS (33). Like other autoimmune diseases, the exact trigger for autoantibodies is unknown. Several theories exist however, including recent work identifying an intestinal microbe as a source of cross-reactive antigens thought to trigger APS autoimmunity (34, 35). A comparison of known APS epitopes within β2GPI with intestinal microbiome metagenomic data, identified Roseburia Intestinalis as a gut microbe with “mimotope” peptides for both B and T-cells, and cross-reactivity was experimentally confirmed in humans and mice. Moreover, a Roseburia Intestinalis-induced APS phenotype was reported in APS-prone mice.
On another note, some non-β2GPI-specific aPL could be natural antibodies (i.e., polyreactive, non-immunization induced and B1 cell-secreted) (36), whose pathogenicity could be secondarily induced or enhanced by antigen-driven mutation (37).
Regarding the genetic background, different human leukocyte antigen (HLA) gene polymorphisms have been associated with the occurrence of certain types of aPL: HLA-DR5 and HLA-DRw53 with aCL and LAC; HLA-DPB1*0301 and HLA-DPB1*1901 with anti-β2GPI; HLA-DQB1*0301, HLA-DQA1*03, and HLA-DRB1*04 with anti-prothrombin; HLA-DRB1*08 with anti-annexin V, and HLA-DQB1*0301 with anti-phosphatidylserine (38). These findings suggest that the way these autoantigens—or microbial antigens, through molecular mimicry (21, 34)—are presented to the immune system, is important for the generation of the corresponding autoantibodies. Interestingly, another potential autoantibody-generating mechanism has been described for HLA class II molecules and their ability to aberrantly present cellular misfolded proteins [i.e., exposing cryptic epitopes (5) or creating neoantigens (12)] to the cell surface without processing to peptide (39). In line with this, anti-β2GPI/HLA-DR complex antibodies were recently reported in 83% cases of APS (12), and 20% cases of unexplained recurrent pregnancy loss (13).
Pathophysiology of Thrombotic Manifestations
According to the 2006 revised classification criteria for APS, the “vascular thrombosis” criterion is met with the occurrence of ≥1 episode(s) of objectively (i.e., via appropriate imaging or histopathology) confirmed arterial, venous, or small vessel thrombosis, in any tissue or organ, excluding superficial venous thrombosis (29).
The exact underlying pathogenic mechanisms behind APS have not yet been fully elucidated (40), but multiple leads linking coagulation and autoimmunity have been described:
- aPL direct interference with the endogenous anticoagulant systems e.g., decrease in protein C/S and thrombin plasma levels (41).
- inhibition of β2GPI-stimulated fibrinolysis by anti-β2GPI autoantibodies (42).
- anti-β2GPI antibody-dependent activation of the classical complement pathway in the “standard” thrombotic manifestations of APS (43, 44), but also of the alternative pathways in its catastrophic form due to additional germline mutations in complement regulatory genes (45).
- autoantibody-mediated activation (including C5a and C5b9-related mechanisms) of endothelial cells (46– 48), platelets (48–52) and monocytes (53, 54), particularly leading to tissue factor pathway-dependent procoagulant activity via various [and sometimes paradoxical (55)] mechanisms (56).
- release of neutrophil extracellular traps (NETs) by activated neutrophils (57).
- endothelial protein C receptor (EPCR)-lysobisphosphatidic acid (LBPA) engagement by aPL, leading to thrombosis and driving dendritic cell interferon-α production for the expansion of aPL-secreting B1 cells (56).
These autoantibodies' pathogenic effects are frequently referred to as the “first hit,” inducing a persistent thrombophilic state, which requires a “second hit,” usually an inflammatory and/or a prothrombotic condition, to elicit the clinical manifestations (40). Pregnancy can be viewed as such, because of its well-described associated hypercoagulable state, including overlapping mechanisms such as acquired activated protein C resistance or increased tissue factor expression and activation (58).
Pathophysiology of Pregnancy Manifestations
According to the 2006 revised classification criteria for APS, the “pregnancy morbidity” criterion is met with the occurrence of at least one of these events (without any alternative cause): (1) ≥1 unexplained death(s) of a morphologically normal fetus (≥10th week of gestation). (2) ≥1 premature births of a morphologically normal neonate (<34th week of gestation) because of eclampsia, severe pre-eclampsia or placental insufficiency. (3) ≥3 unexplained consecutive spontaneous abortions (<10th week of gestation) (29).
Interestingly, whereas high titres and multiple aPL positivity are usually associated with thrombotic manifestations in APS, low titres aPL have been frequently reported in obstetric APS (59, 60). The fact that high levels of β2GPI can be found in the placenta is a possible explanation for this, moreover direct effects (notably through complement, Toll Like Receptors and inflammasome pathways) on trophoblast cell and endometrium differentiation have been reported for aPL (61–65). The recently described anti-β2GPI/HLA-DR antibodies may have a pathogenic role in obstetric APS by inducing complement-dependent cytotoxicity-mediated damaging in vascular endothelial cells of the placental decidua (12). Similarly, the EPCR/LBPA complex is involved in aPL signaling in embryonic trophoblast cells, and using an anti-EPCR/LBPA-blocking antibody was protective from fetal loss in a relevant mouse model (56). Other non-criteria aPL have been reported in obstetric APS, including anti-Annexin antibodies (66) or aPL of the IgA isotype (67).
Clinical Implications of Pregnancy in APS
A current or planned pregnancy demands careful counseling and therapeutic decision making in APS patients. Unfortunately, clinical research on APS is hampered by equivocal data from both epidemiological studies and clinical trials. General reasons for this include heterogeneity in APS testing, cut-off values, patient selection, and treatment protocols. The mainstay of treatment for pregnant APS patients—despite the evidence for a coexisting role of non-thrombotic processes in the pathogenesis—is anticoagulant therapy. This applies to both thrombotic and obstetric APS. Bleeding complications are the main drawback. Bleeding risk was investigated in a post-hoc analysis of one retrospective and one prospective cohort of pregnant APS patients receiving low dose aspirin (LDA) and/or low molecular weight heparin (LMWH) (68). The incidence of bleeding events was 25% in the retrospective cohort, with major bleedings, all early post-partum, occurring in 3% of pregnancies. In the prospective cohort only a single bleeding event (1.2%) was recorded. Major bleeding was defined as requiring intervention for hemostasis or blood transfusion, or during the peripartum period >500 mL. A control group was not included in this study, but the rates do not clearly exceed those in untreated pregnant women. Heparin-induced thrombocytopenia and allergic reactions also seem rare (69).
Pregnancy-Related Venous Thrombosis
Epidemiology
Pregnancy is a prothrombotic state, due to physiological changes in anatomy and circulating hormones and coagulation proteases (70). Hence, pregnancy forms an additional risk factor for thrombosis in APS patients. An estimated one in four thrombotic events in APS are pregnancy related (71). The absolute risk for thrombosis during pregnancy and the postpartum period is variously reported from 1 to 12% (72–74). Not all patients in these studies had APS according to the currently accepted criteria. The reported thrombotic events, mostly venous thrombosis, occurred under different treatment regimens including with and without heparins. Despite these limitations, pregnancy carries a high risk for thrombosis in APS. The risk is further determined by the patients' antibody profile. A high-risk profile comprises persistent positivity for LAC or a combination of at least two of the three aPL, with the general concept of higher titers conferring a higher risk (75). Another major risk factor is a previous thrombosis, and traditional venous thromboembolism (VTE) risk factors likewise apply to the pregnant APS patient.
Patients with purely obstetric APS also have an increased risk for future thrombotic events. Patients with recurrent miscarriage had a thrombotic event rate of 19.3% after a mean follow-up of 7.3 years in one study, with no thrombosis in the group with idiopathic recurrent miscarriage (76). Another case control study in obstetric APS patients reported a approximatively doubled VTE risk when compared to idiopathic controls (77).
Pregnancy can also trigger the most severe form of the syndrome, called catastrophic APS. This rare manifestation is characterized by multiorgan thrombosis, often in the microvasculature, occurring within a single week. Pregnancy is the precipitating factor in an estimated eight percent of cases, half of which occur during the pregnancy and half after (78, 79). Both maternal and perinatal mortality were high in one case-series, around fifty percent.
Interestingly, aPL do cross the placenta and newborns from APS mothers can test postive for these antibodies. Fortunately, this does not appear to cause thrombosis in the infants. Neurodevelopmental disorders have been observed but it is unclear whether there is an increased risk, let alone a causal relation (78, 80).
Prevention and Treatment of Venous Thrombosis
The risk for pregnancy-related thrombosis necessitates prevention using anticoagulants. No trials have assessed different strategies for secondary thrombosis prophylaxis specifically in pregnant APS patients. But even under dual anticoagulant therapy with LDA and LMWH, pregnancy carries a high risk for thrombosis recurrence (81). Experts agree on treating all APS patients with previous thrombosis with therapeutic dose LMWH and LDA during pregnancy (75, 82). Women with obstetric APS are treated with a prophylactic dose during pregnancy and the puerperium. Vitamin K antagonists cross the placenta and can be teratogenic and cause fetal hemorrhage (83). They should therefore be replaced with LMWH as soon as pregnancy is confirmed. Based on data from animal studies, direct oral anticoagulants are also deemed unsafe during pregnancy and lactation (84). Moreover, data from clinical trials outside of pregnancy suggests these anticoagulants have inferior effectiveness compared to vitamin K antagonists, and at least for high-risk patients with arterial thrombosis they are not recommended (85, 86). Direct oral anticoagulants, if prescribed to APS patients, are ideally replaced by LMWH preconceptionally. This recommendation is largely based on the uncertainty about the teratogenicity of these agents (84), which may leave room for an alternative approach in patients with regular menses. If there is a strong preference to avoid long duration LWMH treatment (from the undefined preconceptional period until postpartum), frequent pregnancy testing in case of delayed menses and direct switching to LWMH upon a positive test may be preferred by a well-counseled patient.
New thrombosis occurring during pregnancy in an obstetric APS patient is also treated with LWMH. Catastrophic APS triggered by pregnancy is treated with a combination of intravenous heparin, glucocorticoids and either intravenous immunoglobulins or plasma exchange. Due to the nature of this manifestation, no trials are available, and treatment is based on expert opinion (87). Delivery should be considered, although it is not known whether this improves outcomes (88).
APS patients undergoing assisted reproductive technology procedures are also at high-risk for thrombosis (89). LMWH is recommended, at the same dose as what would be prescribed during a pregnancy in that individual patient (75, 82). The thrombotic risk is thought to be caused by the high estrogen levels. For this same reason, estrogen containing contraception is discouraged in women with APS (75, 82).
Pregnancy Morbidity
Epidemiology
The other clinical hallmark of APS aside from thrombosis, is obstetrical morbidity. A systematic review of the literature on APS antibody frequencies has shown that 6% of patients with APS related pregnancy morbidity are antibody positive (90). When restricting the analysis to studies that confirmed the diagnosis according to current criteria, the frequency ranged from 0 to 29%. The strength of the association seems to differ between the different obstetrical manifestations. In a European registry study of aPL-positive women, most of whom had APS according to the classification criteria, 54% had a history of recurrent miscarriage (91). However, the baseline risk of a single recognized pregnancy ending in miscarriage is already as high as 13% (92). Although recurrent miscarriage is a part of the classification criteria, the association with aPL is a matter of debate (93). Comparisons of observational studies on the topic are hampered by variation in the number and timing of pregnancy losses, aPL testing, and whether other causes for miscarriage were excluded. An extensive systematic review of these studies does suggest that the risk of early pregnancy losses is tripled in the presence of LAC and/or aCL (94). The same study reported risk increases with LAC for second trimester [OR 14.3 (95% CI 4.7–43.2)] and third trimester [OR 2.4 (95% CI 0.81–7.0)] pregnancy loss, and with aCL for third trimester loss [OR 3.3 (95% CI 1.6–6.7)]. A recent systematic review found odds ratios for late pregnancy loss ranging from 4.3 to 23, depending on the type of antibody (95). The third obstetric classifying manifestation of APS are placenta-mediated complications leading to premature birth, specifically pre-eclampsia, eclampsia and placental insufficiency. The frequency of pre-eclampsia in APS pregnancies is reported from 10 to 48% (96). Conversely, about 1 in 7 cases of pre-eclampsia may be APS-associated. The frequency of placental insufficiency is about 30%.
Prevention of Pregnancy Morbidity
One question related to therapy for obstetric APS is whether a single treatment strategy is optimal for all the different manifestations. The 2020 American College of Rheumatology (ACR) Guidelines on the topic strongly recommends treating pregnant women with APS without prior thrombosis, with prophylactic heparin or LMWH, together with LDA (82). No distinction is made between prior APS manifestations. For patients with ≥ 2 prior early losses the evidence is summarized by a Cochrane Review (69). Meta-analysis of five trials produced a relative risk of live birth of 1.3 (95% CI 1.1–1.5) for heparin plus aspirin vs. aspirin alone. The certainty of evidence was judged low. Aspirin is started preconceptionally and heparin as soon as pregnancy is confirmed. LMWH are usually prescribed instead of unfractionated heparin because of convenience. A direct comparison in two small trials showed no difference (97, 98).
The European Alliance of Associations for Rheumatology does differentiate in its recommendations between women with late or recurrent early losses and women with preterm delivery due to placenta mediated complications (75). For the former, the recommendation parallels the recommendations made by the ACR. For the latter, it recommends either aspirin alone or in combination with prophylactic dose heparin. For this patient subgroup, one trial randomized between the two treatment strategies. It was unfortunately underpowered due to recruitment issues and did not show a difference in efficacy. There were no events in the LMWH plus aspirin group and two in the aspirin only group (99).
In analogy to systemic lupus erythematosus and based on a retrospective observational study, the ACR also recommends treating pregnant APS patients with hydroxychloroquine. This strategy is being evaluated in ongoing trials (100). Interestingly LMWH and LDA are also thought to act through non-antithrombotic (i.e., immunomodulatory) functions (101, 102), as hydroxychloroquine (103), but evidence is not conclusive to date (104). Another immunomodulatory therapeutic strategy under investigation is TNF-alpha inhibition by certolizumab pegol (NCT03152058).
Discussion
Despite clear classification criteria, APS remains a complex disease, as highlighted by the large body of work implicating a wide range of cell types, signaling pathways and plasma proteases in its pathophysiology. A single key event within the pathophysiological pathway has however not yet been undisputedly pinpointed, although recent work does identify a new cell membrane lipid complex which links the antibody formation with induction of thrombosis and pregnancy morbidity.
Likewise, the exact origin of aPL remains an open question. Molecular mimicry has been suspected for a long time, but robust evidence linking the targeted autoantigens with intestinal microbe-expressed proteins were only recently reported and deserve further investigation.
Pregnancy is an important second hit in APS. It frequently provokes thrombosis, requiring secondary and sometimes primary thromboprophylaxis. A careful risk assessment is required. Similarly, in women in whom APS previously presented with pregnancy morbidity, secondary thromboprophylaxis is essential.
Trials have been performed to determine the optimal treatment strategy, but overall did not produce unequivocal results. Variations in patient populations, aPL testing and treatment are part of the explanation. Given the suboptimal efficacy and safety of anticoagulants and the non-coagulation-related mechanisms also involved in the pathophysiology, new non-anticoagulant based treatments are under investigation.
Author Contributions
MK and TM wrote sections of the manuscript. Both authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ruiz-Irastorza G, Crowther M, Branch W, Khamashta MA. Antiphospholipid syndrome. Lancet. (2010) 376:1498–509. doi: 10.1016/S0140-6736(10)60709-X
2. Nalli C, Andreoli L, Pascariello G, Zentilin A, Raffetti E, Martini G, et al. AB1287 A population-based study on the prevalence and incidence of vascular primary antiphospholipid syndrome: a new rare disease. Ann Rheum Dis. (2018) 77:1736. doi: 10.1136/annrheumdis-2018-eular.5676
3. Duarte-García A, Pham MM, Crowson CS, Amin S, Moder KG, Pruthi RK, et al. The epidemiology of antiphospholipid syndrome: a population-based study. Arthritis Rheumatol. (2019) 71:1545–52. doi: 10.1002/art.40901
4. de Laat B, Derksen RHWM, van Lummel M, Pennings MTT, de Groot PG. Pathogenic anti-beta2-glycoprotein I antibodies recognize domain I of beta2-glycoprotein I only after a conformational change. Blood. (2006) 107:1916–24. doi: 10.1182/blood-2005-05-1943
5. Agar Ç, van Os GMA, Mörgelin M, Sprenger RR, Marquart JA, Urbanus RT, et al. β2-Glycoprotein I can exist in 2 conformations: implications for our understanding of the antiphospholipid syndrome. Blood. (2010) 116:1336–43. doi: 10.1182/blood-2009-12-260976
6. de Groot PG, Urbanus RT. The significance of autoantibodies against β2-glycoprotein I. Blood. (2012) 120:266–74. doi: 10.1182/blood-2012-03-378646
7. Hu C, Li S, Xie Z, You H, Jiang H, Shi Y, et al. Evaluation of the diagnostic value of non-criteria antibodies for antiphospholipid syndrome patients in a chinese cohort. Front Immunol. (2021) 12:741369. doi: 10.3389/fimmu.2021.741369
8. Bradacova P, Slavik L, Ulehlova J, Skoumalova A, Ullrychova J, Prochazkova J, et al. Current promising biomarkers and methods in the diagnostics of antiphospholipid syndrome: a review. Biomedicines. (2021) 9:166. doi: 10.3390/biomedicines9020166
9. Garcia D, Erkan D. Diagnosis and management of the antiphospholipid syndrome. N Engl J Med. (2018) 378:2010–21. doi: 10.1056/NEJMra1705454
10. Fierro JJ, Velasquez M, Cadavid AP, de Leeuw K. Effects of anti-beta 2-glycoprotein 1 antibodies and its association with pregnancy-related morbidity in antiphospholipid syndrome. Am J Reprod Immunol. (2022) 87:e13509. doi: 10.1111/aji.13509
11. McDonnell T, Wincup C, Buchholz I, Pericleous C, Giles I, Ripoll V, et al. The role of beta-2-glycoprotein I in health and disease associating structure with function: more than just APS. Blood Rev. (2020) 39:100610. doi: 10.1016/j.blre.2019.100610
12. Tanimura K, Jin H, Suenaga T, Morikami S, Arase N, Kishida K, et al. β2-Glycoprotein I/HLA class II complexes are novel autoantigens in antiphospholipid syndrome. Blood. (2015) 125:2835–44. doi: 10.1182/blood-2014-08-593624
13. Tanimura K, Saito S, Nakatsuka M, Nagamatsu T, Fujii T, Fukui A, et al. The β 2 -glycoprotein I/HLA-DR complex as a major autoantibody target in obstetric antiphospholipid syndrome. Arthritis Rheumatol. (2020) 72:1882–91. doi: 10.1002/art.41410
14. Khogeer H, Alfattani A, Al Kaff M, Al Shehri T, Khojah O, Owaidah T. Antiphosphatidylserine antibodies as diagnostic indicators of antiphospholipid syndrome. Lupus. (2015) 24:186–90. doi: 10.1177/0961203314552462
15. Pengo V, Denas G, Bison E, Banzato A, Padayattil Jose S, Gresele P, et al. Prevalence and significance of anti-prothrombin (aPT) antibodies in patients with Lupus Anticoagulant (LA). Thromb Res. (2010) 126:150–53. doi: 10.1016/j.thromres.2010.05.018
16. Sciascia S, Sanna G, Murru V, Roccatello D, Khamashta MA, Bertolaccini ML. Anti-prothrombin (aPT) and anti-phosphatidylserine/prothrombin (aPS/PT) antibodies and the risk of thrombosis in the antiphospholipid syndrome. A systematic review. Thromb Haemost. (2014) 111:354–64. doi: 10.1160/TH13-06-0509
17. de Laat B, Derksen RHWM, Mackie IJ, Roest M, Schoormans S, Woodhams BJ, et al. Annexin A5 polymorphism (−1C → T) and the presence of anti-annexin A5 antibodies in the antiphospholipid syndrome. Ann Rheum Dis. (2006) 65:1468–72. doi: 10.1136/ard.2005.045237
18. Cañas F, Simonin L, Couturaud F, Renaudineau Y. Annexin A2 autoantibodies in thrombosis and autoimmune diseases. Thromb Res. (2015) 135:226–30. doi: 10.1016/j.thromres.2014.11.034
19. Cesarman-Maus G, Ríos-Luna NP, Deora AB, Huang B, Villa R, Cravioto M del C, et al. Autoantibodies against the fibrinolytic receptor, annexin 2, in antiphospholipid syndrome. Blood. (2006) 107:4375–82. doi: 10.1182/blood-2005-07-2636
20. Asherson RA, Cervera R. Antiphospholipid antibodies and infections. Ann Rheum Dis. (2003) 62:388–93. doi: 10.1136/ard.62.5.388
21. Shoenfeld Y, Blank M, Cervera R, Font J, Raschi E, Meroni P. Infectious origin of the antiphospholipid syndrome. Ann Rheum Dis. (2006) 65:2–6. doi: 10.1136/ard.2005.045443
22. Cervera R, Asherson RA, Acevedo ML, Gómez-Puerta JA, Espinosa G, De La Red G, et al. Antiphospholipid syndrome associated with infections: clinical and microbiological characteristics of 100 patients. Ann Rheum Dis. (2004) 63:1312–7. doi: 10.1136/ard.2003.014175
23. Foret T, Dufrost V, du Mont LS, Costa P, Lefevre B, Lacolley P, et al. Systematic review of antiphospholipid antibodies in covid-19 patients: culprits or bystanders? Curr Rheumatol Rep. (2021) 23:65. doi: 10.1007/s11926-021-01029-3
24. Borghi MO, Beltagy A, Garrafa E, Curreli D, Cecchini G, Bodio C, et al. Anti-phospholipid antibodies in COVID-19 are different from those detectable in the anti-phospholipid syndrome. Front Immunol. (2020) 11:584241. doi: 10.3389/fimmu.2020.584241
25. Vollmer O, Tacquard C, Dieudonné Y, Nespola B, Sattler L, Grunebaum L, et al. Follow-up of COVID-19 patients: LA is transient but other aPLs are persistent. Autoimmun Rev. (2021) 20:102822. doi: 10.1016/j.autrev.2021.102822
26. Von LANDENBERG P, Döring Y, Modrow S, Lackner KJ. Are antiphospholipid antibodies an essential requirement for an effective immune response to infections? Ann N Y Acad Sci. (2007) 1108:578–583. doi: 10.1196/annals.1422.060
27. Gardiner C, Hills J, Machin S, Cohen H. Diagnosis of antiphospholipid syndrome in routine clinical practice. Lupus. (2013) 22:18–25. doi: 10.1177/0961203312460722
28. Wilson WA, Gharavi AE, Koike T, Lockshin MD, Branch DW, Piette JC, et al. International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome: report of an international workshop. Arthritis Rheum. (1999) 42:1309–11.
29. Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. (2006) 4:295–306. doi: 10.1111/j.1538-7836.2006.01753.x
30. Abreu MM, Danowski A, Wahl DG, Amigo M-C, Tektonidou M, Pacheco MS, et al. The relevance of “non-criteria” clinical manifestations of antiphospholipid syndrome: 14th International Congress on Antiphospholipid Antibodies Technical Task Force Report on Antiphospholipid Syndrome Clinical Features. Autoimmun Rev. (2015) 14:401–14. doi: 10.1016/j.autrev.2015.01.002
31. Naranjo L, Ostos F, Gil-Etayo FJ, Hernández-Gallego J, Cabrera-Marante Ó, Pleguezuelo DE, et al. Presence of extra-criteria antiphospholipid antibodies is an independent risk factor for ischemic stroke. Front Cardiovasc Med. (2021) 8:665741. doi: 10.3389/fcvm.2021.665741
32. Pignatelli P, Ettorre E, Menichelli D, Pani A, Violi F, Pastori D. Seronegative antiphospholipid syndrome: refining the value of “non-criteria” antibodies for diagnosis and clinical management. Haematologica. (2020) 105:562–72. doi: 10.3324/haematol.2019.221945
33. García-Carrasco M, Galarza-Maldonado C, Mendoza-Pinto C, Escarcega RO, Cervera R. Infections and the antiphospholipid syndrome. Clin Rev Allergy Immunol. (2009) 36:104–8. doi: 10.1007/s12016-008-8103-0
34. Ost KS, Round JL. Communication between the microbiota and mammalian immunity. Annu Rev Microbiol. (2018) 72:399–422. doi: 10.1146/annurev-micro-090817-062307
35. Ruff WE, Dehner C, Kim WJ, Pagovich O, Aguiar CL, Yu AT, et al. Pathogenic autoreactive T and B cells cross-react with mimotopes expressed by a common human gut commensal to trigger autoimmunity. Cell Host Microbe. (2019) 26:100–13.e8. doi: 10.1016/j.chom.2019.05.003
36. Panda S, Ding JL. Natural antibodies bridge innate and adaptive immunity. J Immunol. (2015) 194:13–20. doi: 10.4049/jimmunol.1400844
37. Lackner KJ, Müller-Calleja N. Antiphospholipid antibodies: their origin and development. Antibodies. (2016) 5:E15. doi: 10.3390/antib5020015
38. Noureldine MHA, Nour-Eldine W, Khamashta MA, Uthman I. Insights into the diagnosis and pathogenesis of the antiphospholipid syndrome. Semin Arthritis Rheum. (2019) 48:860–66. doi: 10.1016/j.semarthrit.2018.08.004
39. Jin H, Arase N, Hirayasu K, Kohyama M, Suenaga T, Saito F, et al. Autoantibodies to IgG/HLA class II complexes are associated with rheumatoid arthritis susceptibility. Proc Natl Acad Sci USA. (2014) 111:3787–92. doi: 10.1073/pnas.1401105111
40. Meroni PL, Borghi MO, Raschi E, Tedesco F. Pathogenesis of antiphospholipid syndrome: understanding the antibodies. Nat Rev Rheumatol. (2011) 7:330–9. doi: 10.1038/nrrheum.2011.52
41. Urbanus R, de Laat B. Antiphospholipid antibodies and the protein C pathway. Lupus. (2010) 19:394–9. doi: 10.1177/0961203309360841
42. Bu C, Gao L, Xie W, Zhang J, He Y, Cai G, et al. β2-Glycoprotein I is a cofactor for t-PA–mediated plasminogen activation. Arthritis Rheum. (2009) 60:559–68. doi: 10.1002/art.24262
43. Chaturvedi S, Brodsky RA, McCrae KR. Complement in the pathophysiology of the antiphospholipid syndrome. Front Immunol. (2019) 10:449. doi: 10.3389/fimmu.2019.00449
44. Müller-Calleja N, Ritter S, Hollerbach A, Falter T, Lackner KJ, Ruf W. Complement C5 but not C3 is expendable for tissue factor activation by cofactor-independent antiphospholipid antibodies. Blood Adv. (2018) 2:979–86. doi: 10.1182/bloodadvances.2018017095
45. Chaturvedi S, Braunstein EM, Yuan X, Yu J, Alexander A, Chen H, et al. Complement activity and complement regulatory gene mutations are associated with thrombosis in APS and CAPS. Blood. (2020) 135:239–51. doi: 10.1182/blood.2019003863
46. Saadi S, Holzknecht RA, Patte CP, Stern DM, Platt JL. Complement-mediated regulation of tissue factor activity in endothelium. J Exp Med. (1995) 182:1807–14. doi: 10.1084/jem.182.6.1807
47. Allen KL, Fonseca FV, Betapudi V, Willard B, Zhang J, McCrae KR. A novel pathway for human endothelial cell activation by antiphospholipid/anti-β2 glycoprotein I antibodies. Blood. (2012) 119:884–93. doi: 10.1182/blood-2011-03-344671
48. Capozzi A, Riitano G, Recalchi S, Manganelli V, Costi R, Saccoliti F, et al. Effect of heparanase inhibitor on tissue factor overexpression in platelets and endothelial cells induced by anti-β2-GPI antibodies. J Thromb Haemost. (2021) 19:2302–13. doi: 10.1111/jth.15417
49. Shi T, Giannakopoulos B, Yan X, Yu P, Berndt MC, Andrews RK, et al. Anti-beta2-glycoprotein I antibodies in complex with beta2-glycoprotein I can activate platelets in a dysregulated manner via glycoprotein Ib-IX-V. Arthritis Rheum. (2006) 54:2558–67. doi: 10.1002/art.21968
50. Zhang W, Gao F, Lu D, Sun N, Yin X, Jin M, et al. Anti-β2 glycoprotein I antibodies in complex with β2 glycoprotein I induce platelet activation via two receptors: apolipoprotein E receptor 2' and glycoprotein I bα. Front Med. (2016) 10:76–84. doi: 10.1007/s11684-015-0426-7
51. Chayoua W, Nicolson PLR, Meijers JCM, Kardeby C, Garcia-Quintanilla L, Devreese KMJ, et al. Antiprothrombin antibodies induce platelet activation: a possible explanation for anti-FXa therapy failure in patients with antiphospholipid syndrome? J Thromb Haemost. (2021) 19:1776–82. doi: 10.1111/jth.15320
52. Capozzi A, Manganelli V, Riitano G, Recalchi S, Truglia S, Alessandri C, et al. Tissue factor over-expression in platelets of patients with anti-phospholipid syndrome: induction role of anti-β2-GPI antibodies. Clin Exp Immunol. (2019) 196:59–66. doi: 10.1111/cei.13248
53. Sorice M, Longo A, Capozzi A, Garofalo T, Misasi R, Alessandri C, et al. Anti–β2-glycoprotein I antibodies induce monocyte release of tumor necrosis factor α and tissue factor by signal transduction pathways involving lipid rafts. Arthritis Rheum. (2007) 56:2687–97. doi: 10.1002/art.22802
54. Virachith S, Saito M, Watanabe Y, Inoue K, Hoshi O, Kubota T. Anti-β2 -glycoprotein I antibody with DNA binding activity enters living monocytes via cell surface DNA and induces tissue factor expression. Clin Exp Immunol. (2019) 195:167–78. doi: 10.1111/cei.13229
55. Müller-Calleja N, Hollerbach A, Ritter S, Pedrosa DG, Strand D, Graf C, et al. Tissue factor pathway inhibitor primes monocytes for antiphospholipid antibody-induced thrombosis. Blood. (2019) 134:1119–31. doi: 10.1182/blood.2019001530
56. Müller-Calleja N, Hollerbach A, Royce J, Ritter S, Pedrosa D, Madhusudhan T, et al. Lipid presentation by the protein C receptor links coagulation with autoimmunity. Science. (2021) 371:eabc0956. doi: 10.1126/science.abc0956
57. Wirestam L, Arve S, Linge P, Bengtsson AA. Neutrophils-important communicators in systemic lupus erythematosus and antiphospholipid syndrome. Front Immunol. (2019) 10:2734. doi: 10.3389/fimmu.2019.02734
58. Brenner B. Haemostatic changes in pregnancy. Thromb Res. (2004) 114:409–14. doi: 10.1016/j.thromres.2004.08.004
59. Pregnolato F, Gerosa M, Raimondo MG, Comerio C, Bartoli F, Lonati PA, et al. EUREKA algorithm predicts obstetric risk and response to treatment in women with different subsets of anti-phospholipid antibodies. Rheumatology. (2021) 60:1114–24. doi: 10.1093/rheumatology/keaa203
60. Levy RA, dos Santos FC, de Jesús GR, de Jesús NR. Antiphospholipid antibodies and antiphospholipid syndrome during pregnancy: diagnostic concepts. Front Immunol. (2015) 6:205. doi: 10.3389/fimmu.2015.00205
61. Quenby S, Mountfield S, Cartwright JE, Whitley GS, Chamley L, Vince G. Antiphospholipid antibodies prevent extravillous trophoblast differentiation. Fertil Steril. (2005) 83:691–8. doi: 10.1016/j.fertnstert.2004.07.978
62. Francis J, Rai R, Sebire NJ, El-Gaddal S, Fernandes MS, Jindal P, et al. Impaired expression of endometrial differentiation markers and complement regulatory proteins in patients with recurrent pregnancy loss associated with antiphospholipid syndrome. Mol Hum Reprod. (2006) 12:435–42. doi: 10.1093/molehr/gal048
63. Mulla MJ, Brosens JJ, Chamley LW, Giles I, Pericleous C, Rahman A, et al. Antiphospholipid antibodies induce a pro-inflammatory response in first trimester trophoblast via the TLR4/MyD88 pathway. Am J Reprod Immunol. (2009) 62:96–111. doi: 10.1111/j.1600-0897.2009.00717.x
64. Mulla MJ, Weel IC, Potter JA, Gysler SM, Salmon JE, Peraçoli MTS, et al. Antiphospholipid antibodies inhibit trophoblast toll-like receptor and inflammasome negative regulators. Arthritis Rheumatol. (2018) 70:891–902. doi: 10.1002/art.40416
65. Gysler SM, Mulla MJ, Guerra M, Brosens JJ, Salmon JE, Chamley LW, et al. Antiphospholipid antibody-induced miR-146a-3p drives trophoblast interleukin-8 secretion through activation of Toll-like receptor 8. Mol Hum Reprod. (2016) 22:465–74. doi: 10.1093/molehr/gaw027
66. Misasi R, Longo A, Recalchi S, Caissutti D, Riitano G, Manganelli V, et al. Molecular mechanisms of “antiphospholipid antibodies” and their paradoxical role in the pathogenesis of “seronegative APS.” Int J Mol Sci. (2020) 21:E8411. doi: 10.3390/ijms21218411
67. Cabrera-Marante O, Rodríguez de Frías E, Serrano M, Lozano Morillo F, Naranjo L, Gil-Etayo FJ, et al. The weight of IgA anti-β2glycoprotein I in the antiphospholipid syndrome pathogenesis: closing the gap of seronegative antiphospholipid syndrome. Int J Mol Sci. (2020) 21:E8972. doi: 10.3390/ijms21238972
68. Yelnik CM, Lambert M, Drumez E, Le Guern V, Bacri J-L, Guerra MM, et al. Bleeding complications and antithrombotic treatment in 264 pregnancies in antiphospholipid syndrome. Lupus. (2018) 27:1679–86. doi: 10.1177/0961203318787032
69. Hamulyák EN, Scheres LJ, Marijnen MC, Goddijn M, Middeldorp S. Aspirin or heparin or both for improving pregnancy outcomes in women with persistent antiphospholipid antibodies and recurrent pregnancy loss. Cochrane Database Syst Rev. (2020) 5:CD012852. doi: 10.1002/14651858.CD012852.pub2
70. Barco S, Nijkeuter M, Middeldorp S. Pregnancy and venous thromboembolism. Semin Thromb Hemost. (2013) 39:549–58. doi: 10.1055/s-0033-1343893
71. Silver RM, Draper ML, Scott JR, Lyon JL, Reading J, Branch DW. Clinical consequences of antiphospholipid antibodies: an historic cohort study. Obstet Gynecol. (1994) 83:372–7.
72. Lima F, Khamashta MA, Buchanan NM, Kerslake S, Hunt BJ, Hughes GR. A study of sixty pregnancies in patients with the antiphospholipid syndrome. Clin Exp Rheumatol. (1996) 14:131–6.
73. Branch DW, Silver RM, Blackwell JL, Reading JC, Scott JR. Outcome of treated pregnancies in women with antiphospholipid syndrome: an update of the Utah experience. Obstet Gynecol. (1992) 80:614–20.
74. Clark CA, Spitzer KA, Crowther MA, Nadler JN, Laskin MD, Waks JA, et al. Incidence of postpartum thrombosis and preterm delivery in women with antiphospholipid antibodies and recurrent pregnancy loss. J Rheumatol. (2007) 34:992–6.
75. Tektonidou MG, Andreoli L, Limper M, Tincani A, Ward MM. Management of thrombotic and obstetric antiphospholipid syndrome: a systematic literature review informing the EULAR recommendations for the management of antiphospholipid syndrome in adults. RMD Open. (2019) 5:e000924. doi: 10.1136/rmdopen-2019-000924
76. Martinez-Zamora MA, Peralta S, Creus M, Tassies D, Reverter JC, Espinosa G, et al. Risk of thromboembolic events after recurrent spontaneous abortion in antiphospholipid syndrome: a case-control study. Ann Rheum Dis. (2012) 71:61–6. doi: 10.1136/ard.2011.153817
77. Gris J-C, Bouvier S, Molinari N, Galanaud J-P, Cochery-Nouvellon E, Mercier E, et al. Comparative incidence of a first thrombotic event in purely obstetric antiphospholipid syndrome with pregnancy loss: the NOH-APS observational study. Blood. (2012) 119:2624–32. doi: 10.1182/blood-2011-09-381913
78. Rodríguez-Pintó I, Moitinho M, Santacreu I, Shoenfeld Y, Erkan D, Espinosa G, et al. Catastrophic antiphospholipid syndrome (CAPS): descriptive analysis of 500 patients from the International CAPS Registry. Autoimmun Rev. (2016) 15:1120–4. doi: 10.1016/j.autrev.2016.09.010
79. Gómez-Puerta JA, Cervera R, Espinosa G, Asherson RA, García-Carrasco M, da Costa IP, et al. Catastrophic antiphospholipid syndrome during pregnancy and puerperium: maternal and fetal characteristics of 15 cases. Ann Rheum Dis. (2007) 66:740–6. doi: 10.1136/ard.2006.061671
80. Soybilgic A, Avcin T. Pediatric APS: state of the art. Curr Rheumatol Rep. (2020) 22:9. doi: 10.1007/s11926-020-0887-9
81. Fischer-Betz R, Specker C, Brinks R, Schneider M. Pregnancy outcome in patients with antiphospholipid syndrome after cerebral ischaemic events: an observational study. Lupus. (2012) 21:1183–9. doi: 10.1177/0961203312451335
82. Sammaritano LR, Bermas BL, Chakravarty EE, Chambers C, Clowse MEB, Lockshin MD, et al. 2020 American College of Rheumatology Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases. Arthritis Rheumatol. (2020) 72:529–56. doi: 10.1002/art.41191
83. Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos A-M, Vandvik PO. VTE, thrombophilia, antithrombotic therapy, and pregnancy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. (2012) 141:e691S−736S. doi: 10.1378/chest.11-2300
84. Cohen H, Arachchillage DR, Middeldorp S, Beyer-Westendorf J, Abdul-Kadir R. Management of direct oral anticoagulants in women of childbearing potential: guidance from the SSC of the ISTH. J Thromb Haemost. (2016) 14:1673–6. doi: 10.1111/jth.13366
85. Ordi-Ros J, Sáez-Comet L, Pérez-Conesa M, Vidal X, Riera-Mestre A, Castro-Salomó A, et al. Rivaroxaban versus vitamin K antagonist in antiphospholipid syndrome: a randomized noninferiority trial. Ann Intern Med. (2019) 171:685–94. doi: 10.7326/M19-0291
86. Woller SC, Stevens SM, Kaplan D, Wang T-F, Branch DW, Groat D, et al. Apixaban compared with warfarin to prevent thrombosis in thrombotic antiphospholipid syndrome: a randomized trial. Blood Adv. (2021) doi: 10.1182/bloodadvances.2021005808 [Epub ahead of print].
87. Legault K, Schunemann H, Hillis C, Yeung C, Akl EA, Carrier M, et al. McMaster RARE-Bestpractices clinical practice guideline on diagnosis and management of the catastrophic antiphospholipid syndrome. J Thromb Haemost. (2018) 16:1656–64. doi: 10.1111/jth.14192
88. Silver RM. Catastrophic antiphospholipid syndrome and pregnancy. Semin Perinatol. (2018) 42:26–32. doi: 10.1053/j.semperi.2017.11.006
89. Orquevaux P, Masseau A, Le Guern V, Gayet V, Vauthier D, Guettrot-Imbert G, et al. In vitro fertilization in 37 women with systemic lupus erythematosus or antiphospholipid syndrome: a series of 97 procedures. J Rheumatol. (2017) 44:613–8. doi: 10.3899/jrheum.160462
90. Andreoli L, Chighizola CB, Banzato A, Pons-Estel GJ, Ramire de Jesus G, Erkan D. Estimated frequency of antiphospholipid antibodies in patients with pregnancy morbidity, stroke, myocardial infarction, and deep vein thrombosis: a critical review of the literature. Arthritis Care Res. (2013) 65:1869–73. doi: 10.1002/acr.22066
91. Alijotas-Reig J, Ferrer-Oliveras R, Ruffatti A, Tincani A, Lefkou E, Bertero MT, et al. The European Registry on Obstetric Antiphospholipid Syndrome (EUROAPS): a survey of 247 consecutive cases. Autoimmun Rev. (2015) 14:387–95. doi: 10.1016/j.autrev.2014.12.010
92. Magnus MC, Wilcox AJ, Morken N-H, Weinberg CR, Håberg SE. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. (2019) 364:l869. doi: 10.1136/bmj.l869
93. Clark CA, Laskin CA, Spitzer KA. Anticardiolipin antibodies and recurrent early pregnancy loss: a century of equivocal evidence. Hum Reprod Update. (2012) 18:474–484. doi: 10.1093/humupd/dms020
94. Robertson L, Wu O, Langhorne P, Twaddle S, Clark P, Lowe GDO, et al. Thrombophilia in pregnancy: a systematic review. Br J Haematol. (2006) 132:171–96. doi: 10.1111/j.1365-2141.2005.05847.x
95. Abou-Nassar K, Carrier M, Ramsay T, Rodger MA. The association between antiphospholipid antibodies and placenta mediated complications: a systematic review and meta-analysis. Thromb Res. (2011) 128:77–85. doi: 10.1016/j.thromres.2011.02.006
96. Geis W, Branch DW. Obstetric implications of antiphospholipid antibodies: pregnancy loss and other complications. Clin Obstet Gynecol. (2001) 44:2–10. doi: 10.1097/00003081-200103000-00002
97. Fouda UM, Sayed AM, Abdou A-MA, Ramadan DI, Fouda IM, Zaki MM. Enoxaparin versus unfractionated heparin in the management of recurrent abortion secondary to antiphospholipid syndrome. Int J Gynaecol Obstet. (2011) 112:211–5. doi: 10.1016/j.ijgo.2010.09.010
98. Noble LS, Kutteh WH, Lashey N, Franklin RD, Herrada J. Antiphospholipid antibodies associated with recurrent pregnancy loss: prospective, multicenter, controlled pilot study comparing treatment with low-molecular-weight heparin versus unfractionated heparin. Fertil Steril. (2005) 83:684–90. doi: 10.1016/j.fertnstert.2004.11.002
99. van Hoorn ME, Hague WM, van Pampus MG, Bezemer D, de Vries JIP, FRUIT Investigators. Low-molecular-weight heparin aspirin in the prevention of recurrent early-onset pre-eclampsia in women with antiphospholipid antibodies: the FRUIT-RCT. Eur J Obstet Gynecol Reprod Biol. (2016) 197:168–73. doi: 10.1016/j.ejogrb.2015.12.011
100. Schreiber K, Breen K, Cohen H, Jacobsen S, Middeldorp S, Pavord S, et al. HYdroxychloroquine to Improve Pregnancy Outcome in Women with AnTIphospholipid Antibodies (HYPATIA) protocol: a multinational randomized controlled trial of hydroxychloroquine versus placebo in addition to standard treatment in pregnant women with antiphospholipid syndrome or antibodies. Semin Thromb Hemost. (2017) 43:562–71. doi: 10.1055/s-0037-1603359
101. Di Simone N, Meroni PL, D'Asta M, Di Nicuolo F, D'Alessio MC, Caruso A. Pathogenic role of anti-beta2-glycoprotein I antibodies on human placenta: functional effects related to implantation and roles of heparin. Hum Reprod Update. (2007) 13:189–96. doi: 10.1093/humupd/dml051
102. Walsh SW, Strauss JF. The road to low-dose aspirin therapy for the prevention of preeclampsia began with the placenta. Int J Mol Sci. (2021) 22:6985. doi: 10.3390/ijms22136985
103. Mekinian A, Costedoat-Chalumeau N, Masseau A, Tincani A, De Caroli S, Alijotas-Reig J, et al. Obstetrical APS: is there a place for hydroxychloroquine to improve the pregnancy outcome? Autoimmun Rev. (2015) 14:23–9. doi: 10.1016/j.autrev.2014.08.040
Keywords: pregnancy morbidity, obstetric antiphospholipid, antiphospholipid syndrome, venous thromboembolism (VTE), antiphospholipid antibodies
Citation: Killian M and van Mens TE (2022) Risk of Thrombosis, Pregnancy Morbidity or Death in Antiphospholipid Syndrome. Front. Cardiovasc. Med. 9:852777. doi: 10.3389/fcvm.2022.852777
Received: 11 January 2022; Accepted: 07 February 2022;
Published: 01 March 2022.
Edited by:
Avi Leader, Rabin Medical Center, IsraelReviewed by:
Fionnuala Ni Ainle, University College Dublin, IrelandQuitterie Reynaud, Hospices Civils de Lyon, France
Copyright © 2022 Killian and van Mens. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thijs E. van Mens, dC5lLnZhbm1lbnNAYW1zdGVyZGFtdW1jLm5s
 Martin Killian
Martin Killian Thijs E. van Mens
Thijs E. van Mens