
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med., 11 March 2022
Sec. Atherosclerosis and Vascular Medicine
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.819274
This article is part of the Research TopicCerebrovasculature in Health and DiseasesView all 13 articles
 Lai Wei1†
Lai Wei1† Junxiang Sun2†
Junxiang Sun2† Hankun Xie1†
Hankun Xie1† Qian Zhuang2
Qian Zhuang2 Pengfei Wei2
Pengfei Wei2 Xianghai Zhao2
Xianghai Zhao2 Yanchun Chen2
Yanchun Chen2 Jiayi Dong1
Jiayi Dong1 Mengxia Li1
Mengxia Li1 Changying Chen1
Changying Chen1 Song Yang2*
Song Yang2* Chong Shen1*
Chong Shen1*Background: Dyslipidemia and hypertension are two important independent risk factors for ischemic stroke (IS); however, their combined effect on IS remains uncertain.
Objectives: This present study aimed to evaluate the interaction effect of hypertension and abnormal lipid indices on IS in a 10-year prospective cohort in Chinese adults.
Methods: The cohort study of 4,128 participants was conducted in May 2009 and was followed up to July 2020. All qualified participants received a questionnaire survey, physical examination, and blood sample detection. Cox regression was used to evaluate the association of dyslipidemia and hypertension with IS, and calculate the hazard ratio (HR) and 95% confidence interval (CI). The relative excess risk of interaction (RERI) and the HR (95%CI) of interaction terms were used to examine additive and multiplicative interactions.
Results: In the hypertensive population, Non-HDL-C ≥190 mg/dl, LDL-C/HDL-C ≥2 and HDL-C ≥60 mg/dl were statistically associated with IS, and after adjusting for covariates, HRs (95%CIs) were 1.565 (1.007–2.429), 1.414 (1.034–1.933) and 0.665 (0.450–0.983), respectively. While in the non-hypertension population, no significant association of Non-HDL-C ≥190 mg/dl, LDL-C/HDL-C ≥2, and HDL-C ≥60 was detected with IS (P > 0.05). There was a significant association between TC/HDL-C ≥ 3.6 and the decreased risk of IS in the non-hypertension population, and the HR (95%CI) was 0.479 (0.307–0.750). Whereas, a similar association was not observed in the hypertensive population. HDL-C ≥ 60 mg/dl, Non-HDL-C ≥ 190 mg/dl, TC/HDL-C ≥ 3.6, and TG/HDL-C ≥ 1 have additive and multiplicative interactions with hypertension (P < 0.05). The RERIs (95% CIs) of the additive interaction are −0.93 (−1.882–0.044), 1.394 (0.38–2.407), 0.752 (0.354–1.151) and 0.575 (0.086–1.065), respectively. The HRs (95% CIs) of the multiplicative interaction terms were 0.498 (0.272–0.911), 4.218 (1.230–14.464), 2.423 (1.437–4.086) and 1.701 (1.016–2.848), respectively.
Conclusion: High concentration of HDL-C reduces the impact of hypertension on IS, while the high concentration of Non-HDL-C, TC/HDL-C, and TG/HDL-C positively interact with hypertension affecting the incidence of IS. This study provides useful evidence for the combined effects of dyslipidemia and hypertension in predicting IS.
Stroke is a major public health issue worldwide, with a high incidence rate, recurrence rate, disability rate, and mortality rate in the population (1). The global lifetime stroke risk from 25 years onward was estimated to be 24.9%, with China having the highest risk of stroke (39.3%), in 2016 (2). In China, stroke has also caused the highest number of disability-adjusted life years of all diseases and has been ranked third among the leading causes of death after malignant tumors and heart disease (3, 4). Moreover, due to changes in lifestyle and population structure and insufficient control over major risk factors, the burden it has brought to public health will be worsened in the future (5). Ischemic stroke (IS), the main subtype of stroke, accounts for almost 78% of stroke cases in China and takes up most of the health burden that stroke caused (6). IS usually occurs suddenly with acute signs and symptoms, which calls for emergency treatment. If emergency care is not provided timely, it will cause severe damage to blood vessels and nerves in the brain, resulting in irreversible complications, lifelong disabilities, or even death. However, the existing treatment for IS requires a strict time window, and the effect of its treatments is not satisfactory. The function damage to the brain will basically not recover fully after the stroke. Consequent side effects and a high risk of recurrence will continuously impact the prognosis and survivors' quality of life. Thus, it is key to focus on the management of risk factors to prevent IS.
IS is a multi-factorial disorder (7) of which prevention may require an improved understanding of modifiable risk factors. Several risk factors increase the IS incidence, such as hypertension, diabetes mellitus, hyperlipidemia, obesity, smoking, drinking, physical inactivity, and a family history of stroke (8, 9). Although each risk factor may contribute significantly to the development of IS, its occurrence is the result of a combination of multiple risk factors (10). According to GBD, over 90% of the global stroke burden is caused by the combined impact of modifiable risk factors (11).
Numerous studies have demonstrated that hypertension and dyslipidemia are two important independent risk factors that can be controlled and modified to prevent IS (12–15). Dyslipidemia is generally believed to play a critical role in the pathogenesis of IS, which can be represented by abnormal changes of traditional and non-traditional lipid indices. Traditional lipid indices, usually referring to total cholesterol (TC), triglycerides (TGs), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C), were identified to have predictive effects on the risk of cardiovascular disease and stroke (16–18). While compared with the traditional lipid indices, non-traditional lipid indices (non-HDL-C, TG/HDL-C, TC/HDL-C, and LDL-C/HDL-C) could serve as a more powerful predictor for vascular risk in stroke and CVD (19). Hypertension has a high co-occurrence rate with dyslipidemia, especially in the middle-aged and elderly population (20). A large cohort study in a French population showed a significantly higher risk of CVD in people under 55 years of age who suffered from comorbid hypertension and dyslipidemia (21). Therefore, exploring the possible interaction effect between hypertension and dyslipidemia on IS is of great significance for preventing and treating IS. However, few studies have examined the interaction of these two risk factors regarding IS. This present study aimed to evaluate the interaction effect of hypertension and abnormal lipid indices on IS in a 10-year prospective cohort in Chinese adults.
This study adopted a prospective cohort design and a total of 4,128 individuals over 18 years old were recruited by a cluster sampling approach from 6 villages for baseline investigation in Guanlin Town and Xushe Town, Yixing City, Jiangsu Province from May to October 2009. The first field follow-up survey proceeded from May to October in 2014. After excluding 30 baseline stroke patients, the remaining 4,098 patients were followed up to July 27th, 2020 for stroke onset. For more information of this cohort, please refer to our previous published literature (22).
The Ethics Committee approved this study of Nanjing Medical University (#200803307). All participants or their caregivers provided signed informed consent before being included in this study.
Population baseline investigation included questionnaire survey, physical examination, blood sample collection, etc. All the personnel involved in on-site investigations have received standardized training, and only after passing the assessment could they start their investigation.
Participants' demographic characteristics, smoking status, drinking status, and disease history were obtained from a validated questionnaire at the time of enrollment. Height, weight, and blood pressure were measured by standardized instruments, which were performed in duplicates to reduce random errors. Smoking was defined as cigarettes consumption greater than ≥ cigarettes per week, lasting at least 3 months a year. Drinking was defined as alcohol consumption ≥2 times per week, lasting at least 6 months per year. Body mass index (BMI) was obtained by dividing weight (kg) by the square of height (m2). Hypertension was defined as average systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg, or currently receiving antihypertensive medication to lower blood pressure. The blood pressure of all subjects was measured 3 times with an interval of 30 s. If the difference between any two systolic or diastolic blood pressures is more than 8 mmHg, the fourth measurement is performed. Diabetes was defined as fasting plasma glucose (FPG) ≥7.0 mmol/l or a self-reported diabetes history. Received lipid-lowering treatment was defined as patients self-reported taking lipid-lowering medications or other lipid-lowering treatment measures.
All participants underwent 8-h overnight fasting and blood sampling to detect FPG and lipid indices, including total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C). Non-HDL-C, TC/HDL-C, TG/HDL-C, LDL-C/HDL-C, and remnant-cholesterol (RC) were derived from detected lipids. The non-HDL-C value was calculated as the difference value of TC minus HDL-C. RC was calculated by TC minus LDL-C minus HDL-C. Baseline dyslipidemia was defined by meeting any of the following conditions: (1) TC ≥ 6.2 mmol/l (240 mg/dl), TG ≥ 2.3 mmol/l (200 mg/dl), LDL-C ≥ 4.1 mmol/l (160 mg/dl), HDL-C < 1.04 mmol/l (40 mg/dl) or HDL-C ≥ 1.55 mmol/l (60 mg/dl); (2) Self-reported diagnosis of dyslipidemia; (3) Currently taking lipid-lowering drugs. As per Chinese Guidelines for the Management of Dyslipidemia in Adults (2016), the cut-off points of TC, TG, LDL-C, HDL-C, and non-HDL-C were 240 mg/dl, 200 mg/dl, 160 mg/dl, 40–60 mg/dl, and 190 mg/dl, respectively. While for indices like RC, TC/HDL-C, TG/HDL-C, and LDL-C/HDL-C, there are no definite clinical diagnostic criteria, so the median of these indicators, which were 30 mg/dl, 3.6, 1, and 2, were defined as the cut-off point value in this study.
Outcome events of stroke in this cohort were collected through the local register system of disease and death of the Center for Disease Control and Prevention (CDC). International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) was used to identify for stroke (I60~I64), IS (I63), and hemorrhagic stroke (I60, I61, I62, and I64). All the monitored stroke onset events were further inspected by certified neurologists and cardiologists through reviewing the medical records system and relevant files of Yixing People's Hospital.
Mann-Whitney U test was used to examine the differences of all the quantitative variables among groups of dyslipidemia presented as median (interquartile range). Chi-square (χ2) test was performed to compare the frequency distributions of qualitative variables. Cox proportional hazards regression models were used to estimate the HRs and 95% confidence intervals (CIs) of IS after adjustment for age, gender, smoking, drinking, BMI, hypertension, diabetes, and received lipid-lowering treatment. Heterogeneity was tested for inter-subgroup associations using Cochran's Q test. The interaction effect was evaluated using the relative excess risk of interaction (RERI) for additive interactions and the HR (95% CI) of multi-factor interaction terms for multiplicative interactions. All statistical analyses were conducted using SAS software version 9.4 (SAS Institute, Inc, Cary, NC), and test results were considered significant at the two-sided 0.05 level.
Descriptive characteristics of the 4,098 participants at baseline are presented in Table 1. The participants were followed up for a median duration of 10.76 years, with 272 participants who developed IS. All participants were categorized into four groups according to the presence of dyslipidemia and hypertension at baseline. The proportion of people with only dyslipidemia, hypertension, and co-morbidity were 26.2, 20.8, and 27.6%, respectively. The median age is 59.20 years, with females accounting for 59.5% of the total population. Smokers and drinkers accounted for 24.3 and 21.5%, respectively. The prevalence of dyslipidemia, hypertension, and diabetes in the population was 53.9, 48.4, and 11.2%, respectively, at baseline. Participants with dyslipidemia or hypertension were more likely to have higher levels of BMI and higher proportions of drinkers and diabetes than their counterparts without dyslipidemia and hypertension (P < 0.05). The sex ratio and the proportion of smokers were approximately the same among four groups (Table 1).
As of July 27th, 2020, the median follow-up time was 10.76 years. There were 272 new IS with a prevalence density of 65.41 per 10,000 person-years during the follow-up period. The incidence density was higher among hypertensive patients, those with dyslipidemia, and both together, at 43.48 per 10,000 person-years, 91.52 per 10,000 person-years, and 92.28 per 10,000 person-years, respectively, compared to those with normal lipids and no hypertension. The corresponding HRs (95%) CIs are 1.603 (1.097–2.343), 1.025 (0.677–1.553) and 1.627 (1.129–2.343), respectively (Table 2).
Non-HDL-C ≥ 190 mg/dl was associated with an increased risk of IS in the whole population, but the correlation was not statistically significant after adjusting the covariates (Supplementary Table S1). The HR (95%CI) before and after adjustment were 1.529 (1.028–2.275) and 1.128 (0.751–1.694), respectively. The remaining lipid indices showed no statistically significant association with IS among the total population (Supplementary Table S1).
In the hypertensive population, Non-HDL-C ≥ 190 mg/dl and LDL-C/HDL-C ≥ 2 were significantly associated with increased risk of IS, after adjusting for covariates, HRs (95%CIs) were 1.565 (1.007–2.429) and 1.414 (1.034–1.933), respectively. HDL-C ≥ 60 mg/dl was significantly associated with reduced risk of IS with adjusted HR (95%CI) of 0.665 (0.450–0.983). While in the non-hypertension population, no significant association of Non-HDL-C ≥ 190 mg/dl, LDL-C/HDL-C ≥ 2, and HDL-C ≥ 60 was detected with IS (P > 0.05).
Additionally, there was a significant association between TC/HDL-C ≥ 3.6 and the decreased risk of IS in the non-hypertension population, and the HR (95%CI) was 0.479 (0.307–0.750). However, a similar association was not observed in the hypertensive population.
Further analysis of heterogeneity test results indicated that the association of HDL-C ≥ 60 mg/dl, Non-HDL-C ≥ 190 mg/dl, TC/HDL-C ≥ 3.6, and TG/HDL-C ≥ 1 and IS are heterogeneous between hypertension and non-hypertension groups (Pheterogeneity < 0.05). See Table 3 for details.
We further analyzed the interaction between those indices which had heterogeneous associations with IS among different blood pressure statuses and hypertension. The results showed that HDL-C ≥ 60 mg/dl (vs HDL-C < 60 mg/dl), Non-HDL-C ≥ 190 mg/dl (vs. Non-HDL-C < 190 mg/dl), TC/HDL-C ≥ 3.6 (vs TC/HDL-C < 3.6), and TG/HDL-C ≥ 1 (vs. TG/HDL-C < 1) have additive and multiplicative interactions with hypertension. The RERIs (95% CIs) of the additive interaction are −0.93 (−1.882–0.044), 1.394 (0.38–2.407), 0.752 (0.354–1.151) and 0.575 (0.086–1.065), respectively. The HRs (95% CIs) of the multiplicative interaction terms were 0.498 (0.272–0.911), 4.218 (1.230–14.464), 2.423 (1.437–4.086) and 1.701 (1.016–2.848), respectively. In the analysis of the interaction between total dyslipidemia and hypertension, the association was not statistically significant. The RERI (95% CI) of the additive interaction was −0.002 (−0.635–0.632), while the HR (95% CI) of the multiplicative interaction term was 0.990 (0.595–1.645). See Table 4 for details.
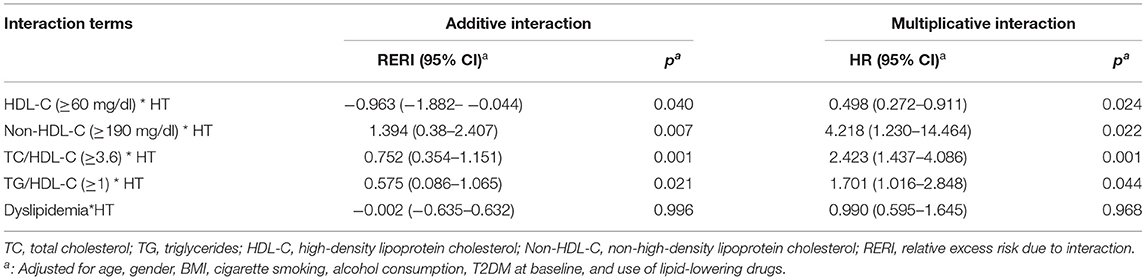
Table 4. Analysis of the additive and multiplicative interaction of abnormal blood lipids and hypertension on IS.
This study indicated that higher HDL-C levels will reduce the impact of hypertension on the risk of developing IS, while higher levels of Non-HDL-C, TC/HDL-C, and TG/HDL-C have a positive interaction effect with hypertension on the incidence of IS in Chinese adults.
Dyslipidemia is one of the major and modifiable risk factors for IS (23, 24). In China, the prevalence of adult dyslipidemia has increased significantly, from 18.6 in 2002 to 40.4% in 2012. Yet the awareness, treatment, and control rates of dyslipidemia are still low, at 31.0, 19.5, and 8.9%, respectively (12, 25, 26). Several studies have reported the association between cardiovascular disease and dyslipidemia, involving the conventional lipid indices such as TC, TG, LDL-C, HDL-C, and the lipid ratios such as TC/HDL-C, TG/HDL-C, and LDL-C/HDL-C. Two large prospective cohort studies both confirmed that high TC, TG, and LDL-C levels or low HDL-C levels increase the risk of CVD (27, 28). However, recent studies have also found a “U” or “J” shaped association between cholesterol levels (including TC, LDL-C, HDL-C) and CVD, with both high and low TC, LDL-C, and HDL-C levels contributing to adverse cardiovascular events (29–34). To comprehensively consider the effects of different lipid components on CVD risk, non-HDL-C, TC/HDL-C, TG/HDL-C, and LDL-C/HDL-C were proposed. Due to the ease of calculation of non-HDL-C and its strong predictive power for CVD, non-HDL-C was recommended as an independent risk factor for CVD (35, 36). Previous epidemiological studies have also demonstrated that higher levels of TC/HDL-C, TG/HDL-C, and LDL-C/HDL-C are associated with an increased risk of developing CVD.
In this study, stratification analysis showed that Non-HDL-C, LDL-C/HDL-C, and HDL-C were associated with IS in the hypertensive population and TC/HDL-C in the non-hypertensive population. These statistically significant indices are derived indices of HDL-C, which may indicate the important influence of HDL-C in the occurrence and development of IS. Besides, analyses of the association of dyslipidemia with IS demonstrated that, compared to LDL-C, non-HDL-C had a stronger relationship with IS risk in the hypertension stratified analysis. This finding may provide more evidence for non-HDL-C as a better predictor for atherogenesis risk than LDL-C in the hypertensive population. However, in the whole population analysis, none of the lipid indices showed a statistical association with IS. There are two main reasons. First, the cohort population and the number of patients with IS are relatively small, especially in performing subgroup analysis. So, it may be difficult to observe a statistically significant association, but the association trend can still be observed. Second, hypertension has a greater effect on the onset of IS, and the etiologic effect of dyslipidemia is relatively small. In the present study population, the prevalence of hypertension was as high as ~50%, so the effect of dyslipidemia may be masked.
Hypertension is another critical and controllable risk factor for IS. It can occur simultaneously with dyslipidemia and act synergistically to affect the risk of CVD according to previous research (21, 37). So, in this study, we analyze different results of the additive model and multiplicative models to evaluate the interaction between blood lipid indices and hypertension comprehensively. Our results suggested that HDL-C ≥ 60 mg/dl negatively affected IS in the hypertension group, from which we could infer that higher HDL-C levels may help reduce the impact of hypertension on IS risk. The underlying mechanism of this finding could be related to endothelial dysfunction in cerebral blood vessels. Atherosclerosis involving impairment of endothelial function and vascular contractility is an essential pathological basis for the development of IS (38). Hypertension-induced abnormalities in the cerebrovascular structure are known to play an important part in the pathogenesis of IS (39). Previous studies have shown that endothelium-mediated vasodilation is undermined in patients with essential hypertension (40–42). This abnormality is associated with attenuated endothelial Nitric Oxide (NO) activity and may be caused by selective abnormalities in NO synthesis (43). However, HDL particles could increase NO production by stimulating endothelial nitric oxide synthase (eNOS) activity and enhance endothelium- and NO-dependent relaxation in wild-type mice (44), which may help to explain, to some extent, the atheroprotective role of HDL-C in reducing the effect of hypertension on IS.
Non-HDL-C, TC/HDL-C, and TG/HDL-C, closely related to HDL-C, are all lipid indices derived from HDL-C but measure other lipids in the blood as well. Thus, these non-traditional lipid parameters may depict a more accurate and more comprehensive lipid profile than traditional ones. In the present study, non-HDL-C, TC/HDL-C, and TG/HDL-C had a positive interaction with hypertension for IS, implying that the abnormal imbalance of circulating lipids may amplify the effect of hypertension on IS. The pathophysiological mechanisms that could possibly explain the interaction between dyslipidemia and hypertension can be summarized as follows. First, LDL-C and hypercholesterolemia have been shown to make a difference in the interference for NO signaling activities resulting in the decrease of NO production and bioavailability, which consequently reduce endothelial vasolidaiton and enhance vasoconstructive activation. Therefore, dyslipidemia exacerbates the development of hypertensive status (45, 46). Moreover, subsequent vascular changes in function and structure caused by hypertension, such as altered hemodynamics at arterial bifurcations, as well as proinflammatory activities and oxidative stress, may worsen the harm produced by dyslipidemia (47). These can be supported by an animal study, which suggests that hypertension and hypercholesterolemia synergistically reduce endothelial function and increase oxidative stress in blood vessels in pigs, possibly exacerbating atherosclerosis due to dyslipidemia (48). In addition, previous research also indicated that the elevated LDL-C level indirectly increased the calcium influx into cells and stimulated vascular smooth muscle cell contraction (47).
With a follow-up of up to 10.75 years, this study systematically and prospectively investigated the interaction between lipid indices and hypertension on IS development. However, the following limitations exist. First, the sample size of this study was relatively small, which may reduce the efficacy of the test. Second, the study did not collect information on physical activity, whereas previous studies have shown that active physical activity reduces the risk of CVD morbidity and mortality by improving CVD risk factors. In addition, because the lipid data in this analysis were collected only at baseline, it was impossible to assess the effect of changes in lipid levels on CVD morbidity and mortality during follow-up. Therefore, a prospective cohort study with larger sample size, more comprehensive baseline information, and repeated lipid measurements during follow-up is urgently needed to validate the results of this study.
This large prospective cohort study is the first for all we know to evaluate the combined effects of abnormal lipid parameters and hypertension on IS. The current results demonstrate that higher HDL-C levels may help reduce the impact of hypertension on IS risk and higher levels of non-HDL-C, TC/HDL-C, and TG/HDL-C, additively interacting with hypertension, increase the risk for developing IS. This study provides useful evidence for the combined effects of dyslipidemia and hypertension in predicting IS in Chinese adults. Therefore, the combination of non-traditional lipid indices and hypertension could aid in the screening process to identify high-risk populations before IS and may lead to more effective prevention of IS in clinical practice. Furthermore, because of the high comorbidity of dyslipidemia and hypertension and the interaction effect on IS, it is essential to implement lipids-control measures to prevent and treat IS in patients with hypertension in China. Targeting both dyslipidemia and hypertension in the clinical context could help build optimal therapeutic interventions for the prevention and management of IS.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Nanjing Medical University. The patients/participants provided their written informed consent to participate in this study.
LW: data analysis and manuscript preparation. JS and QZ: data acquisition and sorting. HX and CC: manuscript preparation. PW, XZ, YC, and ML: data acquisition. JD: data analysis. SY: study design and manuscript preparation. CS: study design, data interpretation, and manuscript preparation. All authors have read and approved the final manuscript.
This work was supported by the National Natural Science Foundation of China (Grant No. 81872686, No.82173611, and No. 81573232), the Priority Academic Program for the Development of Jiangsu Higher Education Institutions (Public Health and Preventive Medicine), and the Flagship Major Development of Jiangsu Higher Education Institutions. The Funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank Solim Essomandan Clemence Bafei for helping to edit the English language. We sincerely thank all patients and healthy volunteers who participated in this study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.819274/full#supplementary-material
1. Al Kasab S, Lynn MJ, Turan TN, Derdeyn CP, Fiorella D, Lane BF, et al. Impact of the new American heart association/American stroke association definition of stroke on the results of the stenting and aggressive medical management for preventing recurrent stroke in intracranial stenosis trial. J Stroke Cerebrovasc Dis. (2017) 26:108–15. doi: 10.1016/j.jstrokecerebrovasdis.2016.08.038
2. Feigin VL, Nguyen G, Cercy K, Johnson CO, Alam T, Parmar PG, et al. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. (2018) 379:2429–37. doi: 10.1056/NEJMoa1804492
3. Wang YJ, Li ZX, Gu HQ, Zhai Y, Jiang Y, Zhao XQ, et al. China stroke statistics 2019: a report from the national center for healthcare quality management in neurological diseases, China national clinical research center for neurological diseases, the Chinese stroke association, national center for chronic and non-communicable disease control and prevention, chinese center for disease control and prevention and institute for global neuroscience and stroke collaborations. Stroke Vasc Neurol. (2020) 5:211–39. doi: 10.1136/svn-2020-000457
4. Wu S, Wu B, Liu M, Chen Z, Wang W, Anderson CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. (2019) 18:394–405. doi: 10.1016/S1474-4422(18)30500-3
5. Lou H, Dong Z, Zhang P, Shao X, Li T, Zhao C, et al. Interaction of diabetes and smoking on stroke: a population-based cross-sectional survey in China. BMJ Open. (2018) 8:e017706. doi: 10.1136/bmjopen-2017-017706
6. Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. (2017) 135:759–71. doi: 10.1161/CIRCULATIONAHA.116.025250
7. Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, et al. Primary prevention of ischemic stroke: a guideline from the American heart association/American stroke association stroke council: cosponsored by the atherosclerotic peripheral vascular disease interdisciplinary working group; cardiovascular nursing council; clinical cardiology council; nutrition, physical activity, and metabolism council; and the quality of care and outcomes research interdisciplinary working group: the American academy of neurology affirms the value of this guideline. Stroke. (2006) 37:1583–633. doi: 10.1161/01.STR.0000223048.70103.F1
8. Cui Q, Naikoo NA. Modifiable and non-modifiable risk factors in ischemic stroke: a meta-analysis. Afr Health Sci. (2019) 19:2121–9. doi: 10.4314/ahs.v19i2.36
9. O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. (2010) 376:112–23. doi: 10.1016/S0140-6736(10)60834-3
10. Wang J, Wen X, Li W, Li X, Wang Y, Lu W. Risk factors for stroke in the Chinese population: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. (2017) 26:509–17. doi: 10.1016/j.jstrokecerebrovasdis.2016.12.002
11. Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, et al. Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. (2016) 15:913–24. doi: 10.1016/S1474-4422(16)30073-4
12. Sun L, Clarke R, Bennett D, Guo Y, Walters RG, Hill M, et al. Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adults. Nat Med. (2019) 25:569–74. doi: 10.1038/s41591-019-0366-x
13. Gorgui J, Gorshkov M, Khan N, Daskalopoulou SS. Hypertension as a risk factor for ischemic stroke in women. Can J Cardiol. (2014) 30:774–82. doi: 10.1016/j.cjca.2014.01.007
14. Hindy G, Engström G, Larsson SC, Traylor M, Markus HS, Melander O, et al. Role of blood lipids in the development of ischemic stroke and its subtypes: a mendelian randomization study. Stroke. (2018) 49:820–7. doi: 10.1161/STROKEAHA.117.019653
15. Cipolla MJ, Liebeskind DS, Chan SL. The importance of comorbidities in ischemic stroke: impact of hypertension on the cerebral circulation. J Cereb Blood Flow Metab. (2018) 38:2129–49. doi: 10.1177/0271678X18800589
16. Jain M, Jain A, Yerragondu N, Brown RD, Rabinstein A, Jahromi BS, et al. The triglyceride paradox in stroke survivors: a prospective study. Neurosci J. (2013) 2013:870608. doi: 10.1155/2013/870608
17. Tirschwell DL, Smith NL, Heckbert SR, Lemaitre RN, Longstreth WT Jr, et al. Association of cholesterol with stroke risk varies in stroke subtypes and patient subgroups. Neurology. (2004) 63:1868–75. doi: 10.1212/01.WNL.0000144282.42222.DA
18. Gorelick PB, Mazzone T. Plasma lipids and stroke. J Cardiovasc Risk. (1999) 6:217–21. doi: 10.1177/204748739900600405
19. Park JH, Lee J, Ovbiagele B. Nontraditional serum lipid variables and recurrent stroke risk. Stroke. (2014) 45:3269–74. doi: 10.1161/STROKEAHA.114.006827
20. Lu S, Bao MY, Miao SM, Zhang X, Jia QQ, Jing SQ, et al. Prevalence of hypertension, diabetes, and dyslipidemia, and their additive effects on myocardial infarction and stroke: a cross-sectional study in Nanjing, China. Ann Transl Med. (2019) 7:436. doi: 10.21037/atm.2019.09.04
21. Thomas F, Bean K, Guize L, Quentzel S, Argyriadis P, Benetos A. Combined effects of systolic blood pressure and serum cholesterol on cardiovascular mortality in young (<55 years) men and women. Eur Heart J. (2002) 23:528–35. doi: 10.1053/euhj.2001.2888
22. Dong J, Yang S, Zhuang Q, Sun J, Wei P, Zhao X, et al. The associations of lipid profiles with cardiovascular diseases and death in a 10-year prospective cohort study. Front Cardiovasc Med. (2021) 8:745539. doi: 10.3389/fcvm.2021.745539
23. Kostis JB. The importance of managing hypertension and dyslipidemia to decrease cardiovascular disease. Cardiovasc Drugs Ther. (2007) 21:297–309. doi: 10.1007/s10557-007-6032-4
24. Turer CB, Brady TM, de Ferranti SD. Obesity, hypertension, and dyslipidemia in childhood are key modifiable antecedents of adult cardiovascular disease: a call to action. Circulation. (2018) 137:1256–9. doi: 10.1161/CIRCULATIONAHA.118.032531
25. Song PK, Man QQ, Li H, Pang SJ, Jia SS, Li YQ, et al. Trends in lipids level and dyslipidemia among chinese adults, 2002-2015. Biomed Environ Sci. (2019) 32:559–70. doi: 10.3967/bes2019.074
26. Zhang M, Deng Q, Wang L, Huang Z, Zhou M, Li Y, et al. Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: a nationally representative survey of 163,641 adults. Int J Cardiol. (2018) 260:196–203. doi: 10.1016/j.ijcard.2017.12.069
27. Bowe B, Xie Y, Xian H, Balasubramanian S, Zayed MA, Al-Aly Z. High density lipoprotein cholesterol and the risk of all-cause mortality among U.S. Veterans. Clin J Am Soc Nephrol. (2016) 11:1784–93. doi: 10.2215/CJN.00730116
28. Gu X, Li Y, Chen S, Yang X, Liu F, Li Y, et al. Association of lipids with ischemic and hemorrhagic stroke: a prospective cohort study among 267 500 Chinese. Stroke. (2019) 50:3376–84. doi: 10.1161/STROKEAHA.119.026402
29. Castañer O, Pintó X, Subirana I, Amor AJ, Ros E, Hernáez Á, et al. Remnant cholesterol, Not LDL cholesterol, is associated with incident cardiovascular disease. J Am Coll Cardiol. (2020) 76:2712–24. doi: 10.1016/j.jacc.2020.10.008
30. Yokokawa H, Yasumura S, Tanno K, Ohsawa M, Onoda T, Itai K, et al. Serum low-density lipoprotein to high-density lipoprotein ratio as a predictor of future acute myocardial infarction among men in a 2.7-year cohort study of a Japanese northern rural population. J Atheroscler Thromb. (2011) 18:89–98. doi: 10.5551/jat.5215
31. Ingelsson E, Schaefer EJ, Contois JH, McNamara JR, Sullivan L, Keyes MJ, et al. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA. (2007) 298:776–85. doi: 10.1001/jama.298.7.776
32. Sung KC, Ryu S, Wild SH, Byrne CD. An increased high-density lipoprotein cholesterol/apolipoprotein A-I ratio is associated with increased cardiovascular and all-cause mortality. Heart. (2015) 101:553–8. doi: 10.1136/heartjnl-2014-306784
33. Ding D, Li X, Qiu J, Li R, Zhang Y, Su D, et al. Serum lipids, apolipoproteins, and mortality among coronary artery disease patients. Biomed Res Int. (2014) 2014:709756. doi: 10.1155/2014/709756
34. Zhong GC, Huang SQ, Peng Y, Wan L, Wu YQ, Hu TY, et al. HDL-C is associated with mortality from all causes, cardiovascular disease and cancer in a J-shaped dose-response fashion: a pooled analysis of 37 prospective cohort studies. Eur J Prev Cardiol. (2020) 27:1187–203. doi: 10.1177/2047487320914756
35. Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. (2016) 37:2999–3058. doi: 10.1093/eurheartj/ehw272
36. Averna M, Stroes E. How to assess and manage cardiovascular risk associated with lipid alterations beyond LDL. Atheroscler Suppl. (2017) 26:16–24. doi: 10.1016/S1567-5688(17)30021-1
37. Agbor-Etang BB, Setaro JF. Management of hypertension in patients with ischemic heart disease. Curr Cardiol Rep. (2015) 17:119. doi: 10.1007/s11886-015-0662-0
38. Rajendran P, Rengarajan T, Thangavel J, Nishigaki Y, Sakthisekaran D, Sethi G, et al. The vascular endothelium and human diseases. Int J Biol Sci. (2013) 9:1057–69. doi: 10.7150/ijbs.7502
39. Yu JG, Zhou RR, Cai GJ. From hypertension to stroke: mechanisms and potential prevention strategies. CNS Neurosci Ther. (2011) 17:577–84. doi: 10.1111/j.1755-5949.2011.00264.x
40. Hirooka Y, Imaizumi T, Masaki H, Ando S, Harada S, Momohara M, et al. Captopril improves impaired endothelium-dependent vasodilation in hypertensive patients. Hypertension. (1992) 20:175–80. doi: 10.1161/01.HYP.20.2.175
41. Linder L, Kiowski W, Bühler FR, Lüscher TF. Indirect evidence for release of endothelium-derived relaxing factor in human forearm circulation in vivo. Blunted response in essential hypertension. Circulation. (1990) 81:1762–7. doi: 10.1161/01.CIR.81.6.1762
42. Panza JA, Quyyumi AA, Brush JE Jr, Epstein SE. Abnormal endothelium-dependent vascular relaxation in patients with essential hypertension. N Engl J Med. (1990) 323:22–7. doi: 10.1056/NEJM199007053230105
43. Cardillo C, Kilcoyne CM, Quyyumi AA, Cannon RO 3rd, Panza JA. Selective defect in nitric oxide synthesis may explain the impaired endothelium-dependent vasodilation in patients with essential hypertension. Circulation. (1998) 97:851–6. doi: 10.1161/01.CIR.97.9.851
44. Yuhanna IS, Zhu Y, Cox BE, Hahner LD, Osborne-Lawrence S, Lu P, et al. High-density lipoprotein binding to scavenger receptor-BI activates endothelial nitric oxide synthase. Nat Med. (2001) 7:853–7. doi: 10.1038/89986
45. Pereira AC, Sposito AC, Mota GF, Cunha RS, Herkenhoff FL, Mill JG, et al. Endothelial nitric oxide synthase gene variant modulates the relationship between serum cholesterol levels and blood pressure in the general population: new evidence for a direct effect of lipids in arterial blood pressure. Atherosclerosis. (2006) 184:193–200. doi: 10.1016/j.atherosclerosis.2005.03.035
46. Liao JK, Shin WS, Lee WY, Clark SL. Oxidized low-density lipoprotein decreases the expression of endothelial nitric oxide synthase. J Biol Chem. (1995) 270:319–24. doi: 10.1074/jbc.270.1.319
47. Chapman MJ, Sposito AC. Hypertension and dyslipidaemia in obesity and insulin resistance: pathophysiology, impact on atherosclerotic disease and pharmacotherapy. Pharmacol Ther. (2008) 117:354–73. doi: 10.1016/j.pharmthera.2007.10.004
Keywords: lipids, hypertension, ischemic stroke, interaction, cohort study, dyslipidemia
Citation: Wei L, Sun J, Xie H, Zhuang Q, Wei P, Zhao X, Chen Y, Dong J, Li M, Chen C, Yang S and Shen C (2022) Interaction Analysis of Abnormal Lipid Indices and Hypertension for Ischemic Stroke: A 10-Year Prospective Cohort Study. Front. Cardiovasc. Med. 9:819274. doi: 10.3389/fcvm.2022.819274
Received: 21 November 2021; Accepted: 18 February 2022;
Published: 11 March 2022.
Edited by:
Anne-Clémence Vion, INSERM U1087 L'unité de recherche de l'institut du thorax, FranceReviewed by:
Chongke Zhong, Soochow University, ChinaCopyright © 2022 Wei, Sun, Xie, Zhuang, Wei, Zhao, Chen, Dong, Li, Chen, Yang and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chong Shen, c2NAbmptdS5lZHUuY24=; Song Yang, c3RhZmYwNTJAeXhwaC5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.