- 1Department of Clinical Epidemiology and Center of Evidence Based Medicine, The First Hospital of China Medical University, Shenyang, China
- 2Department of Clinical Epidemiology, The Fourth Affiliated Hospital of China Medical University, Shenyang, China
Background: Many epidemiological studies have investigated the relationship between occupational noise and hypertension, but with conflicting findings. This study aimed to assess the relationship between occupational noise exposure and the risk of hypertension.
Methods: A case-control study was conducted to explore hypertension predictors, and then sensitivity analysis was performed based on propensity score matching (PSM). Data were collected from participants' annual physical examinations and occupational noise exposure measurements. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated using logistic regression analysis. A restricted cubic spline (RCS) function was used to fit the dose-effect relationship.
Results: 500 cases and 4,356 controls were included in the study. Multivariate logistic regression showed that an increase in the level of occupational noise [range 68–102 dB(A)] of 1 dB(A), corresponded to an increase in hypertension risk of 8.3% (OR: 1.083, 95% CI: 1.058–1.109). Compared to the first quartile, the risk of hypertension in the fourth quartile was 1.742 (95% CI: 1.313–2.310). After applying PSM to minimize bias, we obtained a population of 500 cases and 1,000 controls. Noise level was significantly associated with the risk of hypertension. In addition, the RCS curve showed the risk of hypertension was relatively stable until a predicted noise level of around 80 dB(A) and then started to increase rapidly afterward (Pnonlinear = 0.002).
Conclusions: Occupational noise exposure was significantly associated with hypertension risk and there was a positively correlated dose-response relationship.
Introduction
Noise exposure is a common occupational hazard. Noise exposure not only adversely affects health, but also increases the risk of diseases such as hearing loss (1), ischemic heart disease (2), mental distress, and sleep disturbance (3). To protect workers, an occupational exposure limit has been set for the workplace (standard GBZ2.2-2007) of 85 dB(A) (4). However, even if occupational noise exposure does not exceed this limit, increased incidences of chronic diseases such as hypertension have been shown among workers as revealed by annual physical examinations (5). Hypertension is a serious medical condition associated with increased disease risk to the heart, brain, kidneys, and other organ systems. The burden of hypertension disproportionately affects workers in low and middle-income countries, with two-thirds of cases being found there, largely due to recent increases in risk factors in these populations (6). Previous studies have focused on the typical risk factors for hypertension, such as salt intake (7), smoking (8), and obesity (9), with some studies also addressing the impact of noise exposure on the incidence and development of hypertension (10–15).
Evidence from animal and human studies has suggested hyperactivity of the sympathetic nervous system to be a possible mechanism for the association between noise exposure and hypertension (16). The sympathetic nervous system plays an important role in long-term blood pressure regulation in both normotension and hypertension (17). Noise exposure increases sympathetic activity triggering the release of stress hormones, such as epinephrine and norepinephrine, which act on the corresponding vascular receptors to enhance the contractility of resistance arterioles and increase blood pressure (18, 19). In addition, elevated stress hormone levels trigger the inflammatory and oxidative stress pathways by activating the nicotinamide adenine dinucleotide phosphate oxidase uncoupling of endothelial/neuronal nitric oxide synthase, thereby inducing endothelial and neuronal dysfunction (20).
Some epidemiological studies have suggested associations between traffic noise and hypertension, with one study relating aircraft noise and road traffic noise to an increased risk of hypertension (10, 11). However, epidemiological investigations conducted in the working population have not yet reached a consistent conclusion (12–15). Differences in findings have been attributed to differences in study design, sample sizes and baseline characteristics, and the influence of confounding factors. Meta-analyses have been used to summarize the relationship between occupational noise exposure and the risk of hypertension. However, their conclusions have been limited. Meta-analyses conducted by Wang et al. (21) and Yang et al. (22) included only Chinese literature and Chinese workers. Different study designs (cross-sectional studies, cohort studies, and case-control studies) were included in the three meta-analyses (23–25), which may indirectly explain the results. Recent meta-analyses have been limited by the overall low methodological quality of the included epidemiological studies, with only three of the 24 studies having a low risk of bias (26).
The purpose of this study was to explore the relationship between occupational noise exposure and hypertension risk, to provide a theoretical basis for improving conditions for factory workers and promoting workplace protection.
Methods
This was a case-control study. It was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines (27) (Supplementary Table S1).
Study Design and Population
Male workers were recruited from a modern automobile manufacturing facility in Shenyang. Participants underwent occupational health examinations between July and October 2013. The inclusion criteria of participants were as follows: (1) Those working in places where occupational noise may exist; (2) Those with a cumulative duration of noise exposure of ≥1 year; (3) Those who were physically healthy. Participants were excluded if they were new employees, worked in an office space free of occupational noise (e.g., finance department, management department, etc.), or those who suffered from coronary heart disease, liver disease, kidney disease, or any endocrine disease. Hypertension was defined as a systolic blood pressure of ≥140 mmHg and or a diastolic blood pressure of ≥90 mmHg (2018 ESC/ESH Practice Guidelines) (28). Participants who met the criteria for hypertension were assigned to the case group, otherwise, they were placed in the control group.
This study was approved by the medical scientific research ethics committee of the First Affiliated Hospital of China Medical University (No. AF-SOP-07-1.0-01). All procedures performed in the study complied with the ethical standards of the institution, the National Research Committee, and the 1964 Helsinki Declaration and its subsequent amendments, or similar ethical standards.
Data Collection
The patients and the public were not involved in the design and analysis of this study. Demographic and clinical examination data were extracted from the management system of the medical examination center. Occupational noise exposure was measured in the workplace where the members of factory personnel were located, and measurements were undertaken by an occupational health assessment institution with the relevant safety assessment qualification.
Basic participant information was collected by two trained interviewers using a questionnaire survey that included their age, family history of hypertension (yes/no), smoking status (yes/no), job role, and duration in post. Smoking was defined as at least 1 cigarette per day for a year or more.
Clinical examination and blood sample collection were conducted by a healthcare professional. The clinical examination included height (m), weight (kg), body mass index (BMI), blood pressure (mmHg), listening test (normal/abnormal), and pulmonary function (normal/abnormal). Normal pulmonary function was defined using the ratio of forced expiratory volume in 1 s (FEV1) to forced vital capacity (FVC) taking a value of >80 %. Height and weight were measured using an automatic measuring instrument, and body mass index (BMI) was calculated as weight/height2 (kg/m2). Blood pressure was measured in the upper left arm after 5–10 m of rest in a seated position using an automated device (HEM-746C, Omron, Japan). Each of the above was measured twice, and the mean of the two measurements was used in the analysis. Blood tests were conducted using an automatic biochemical instrument operated by trained technicians, including total cholesterol (TC), triglyceride (TG), high-density lipoprotein (HDL), and low-density lipoprotein (LDL) levels.
Occupational noise exposure was measured by occupational safety inspection professionals, using a statistical noise analyzer (AWA6218; Beijing Xihua Instrument Technology Co., Ltd.). Actual noise levels were recorded according to the normalization of the equivalent continuous A-weighted sound pressure level to a nominal 8-hour working day (LEX, 8h).
Statistical Analysis
In the presence of any missing data, multiple imputation was used to complete the dataset. Continuous variables were shown as median and inter-quartile ranges (25, 75%), and categorical variables were shown as frequencies (%). Mann-Whitney U-tests and chi-square tests, respectively, were used to compare the distributions of continuous and categorical variables between the two groups.
The odds ratio (OR) and 95% confidence interval (CI) of each variable were calculated using logistic regression. A univariate model was used to describe the linear effects of continuous variables. The continuous variables that were included in the corresponding risk models were transformed into categorical variables by selecting the corresponding critical values to ensure the clinically relevant balance between the groups (29). For occupational noise, the critical value was <85 dB(A), and ≥85 dB(A). For age, thresholds of <24, 24–25, 26–29 and ≥30 years were used. For BMI, the critical value was <18.55, 18.55-23.98, and ≥23.99 kg/m2. For heart rate, the critical value was <60, 60–100, and ≥100 beats per minute. For TG, the critical value was <1.70, 1.70–2.25, and ≥2.26 mmol/L. For TC, the critical value was <5.18, 5.18-6.21, and ≥6.22 mmol/L. For LDL, the critical value was <3.37, 3.37–4.13, and ≥4.14 mmol/L. For HDL, the critical value was <1.04, 1.04–1.54, and ≥1.55 mmol/L (30). Years of working at the facility were included as a continuous variable. Smoking status (reference: none), family history (reference: none), pulmonary function (reference: normal), and hearing (reference: normal) were also included in the risk model.
To explore the accuracy of using occupational noise as a predictor of hypertension, the association was explored according to the inter-quartile range of occupational noise levels [ ≤ 76.4 dB(A), 76.41–78.8 dB(A), 78.81–80.90 dB(A), and >80.90 dB(A)]. Finally, Restricted cubic splines (RCS) with knots at the 25, 50, and 75th percentiles of the distribution were used to assess the dose-effect relationship between them, with 80 dB(A) as the reference group. A Spearman correlation test was performed to evaluate the association between occupational noise level and hypertension.
As participants were not randomly assigned to case and control groups, therefore, we used propensity score matching (PSM) to minimize the impact of confounds on the sensitivity analysis (31, 32). We then calculated the propensity score of each participant using multivariate logistic regression modeling. A nearest-neighbor matching method was then used, making the ratio between the case group and control group 1:2, that is, each 1 participant from the case group was matched to 2 participants in the control group with similar propensity scores. The balance of the matched model was assessed using the standardized mean differences between the two groups (33). Finally, the corresponding OR and 95% CI of noise exposure on the risk of hypertension were calculated using univariate logistic regression.
Statistical analyses were conducted using SPSS version 25 (Armonk, NY: IBM Corp.) (34), except for spline fitting, which was performed using SAS version 9.4 (SAS Institute, Cary, NC). A two-sided P-value < 0.05 was considered statistically significant.
Result
Demographic Characteristics
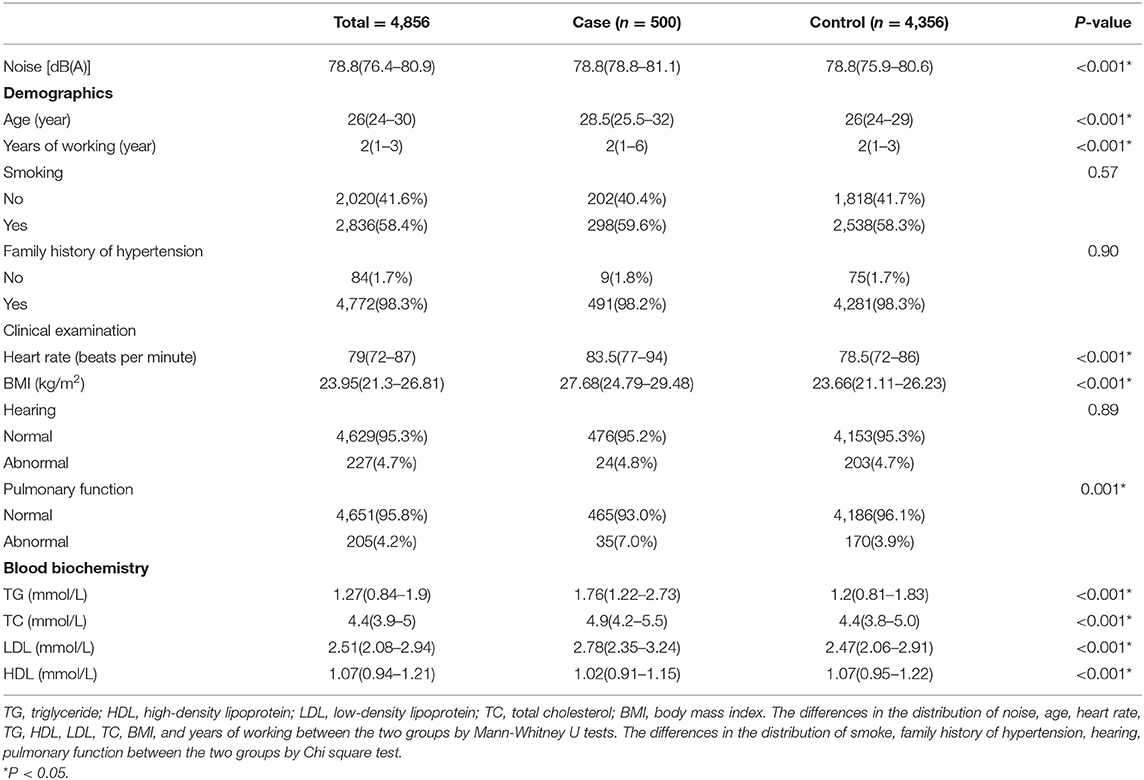
Table 1 shows the participant characteristics of the case and control groups across the entire study cohort. There were 500 cases and 4,356 controls. Noise exposure level, age, TG, TC, LDL, BMI, heart rate, years working at the facility, and pulmonary function were higher in the case group than in the control group (P < 0.05). HDL was lower in the case group than in the control group (P < 0.05). Smoking, family history of hypertension, and hearing level did not significantly differ between the two groups (P > 0.05).
Identify Predictors of Hypertension
Independent predictors of hypertension in the entire participant cohort were identified using logistic regression models with the original value for each variable (Supplementary Table S2). In the multivariate logistic regression, an increase in occupational noise exposure level of 1 dB(A) was associated with an increased hypertension risk of 8.3% (OR: 1.083, 95% CI: 1.058–1.109). Age, heart rate, and BMI were independent predictors of the risk of hypertension.
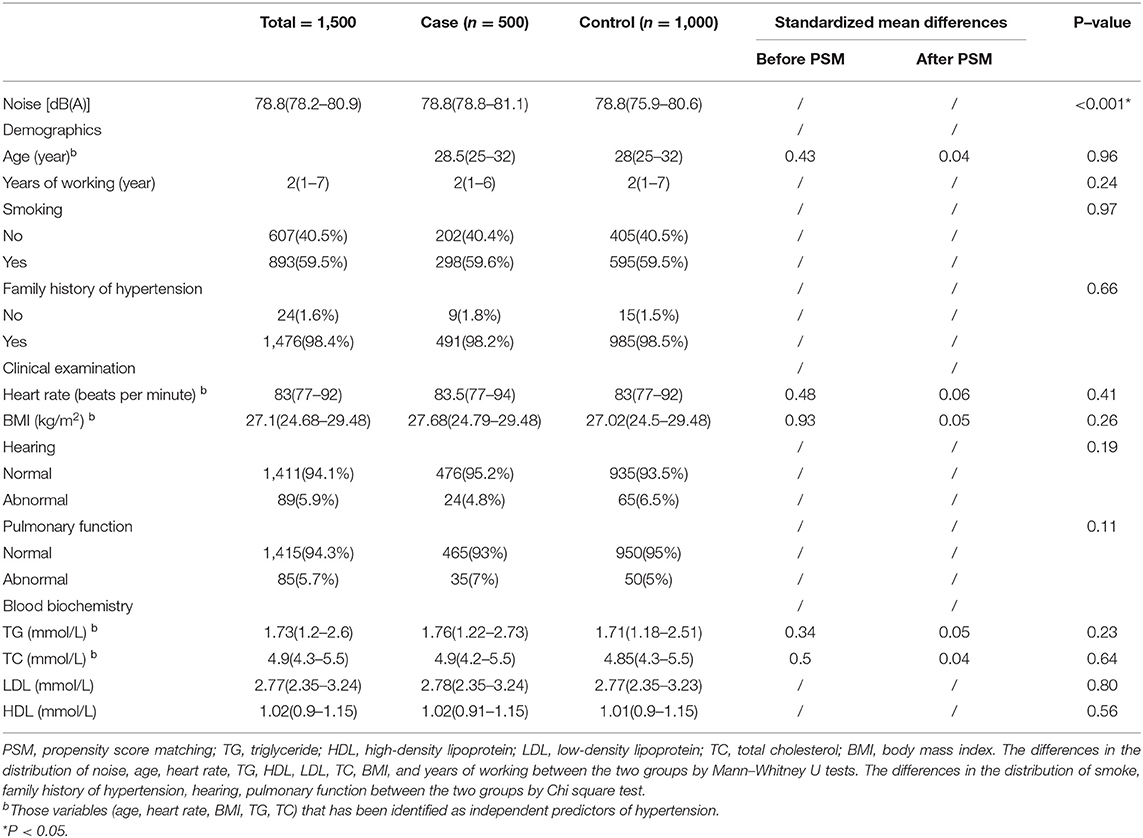
Table 2 shows the independent predictors of hypertension in the entire cohort identified by analyzing the nonlinear effects of the continuous variables. Multivariate logistic regression showed that exposure to occupational noise ≥85 dB(A) was significantly associated with the risk of hypertension (OR: 4.917, 95%CI: 2.920–8.279). When occupational noise level was analyzed as a categorical variable, the risk of having hypertension in the fourth quartile was 1.742 (95% CI: 1.313–2.310), compared to the first quartile. In addition, age, heart rate, BMI, TG, and TC were independent predictors of hypertension.
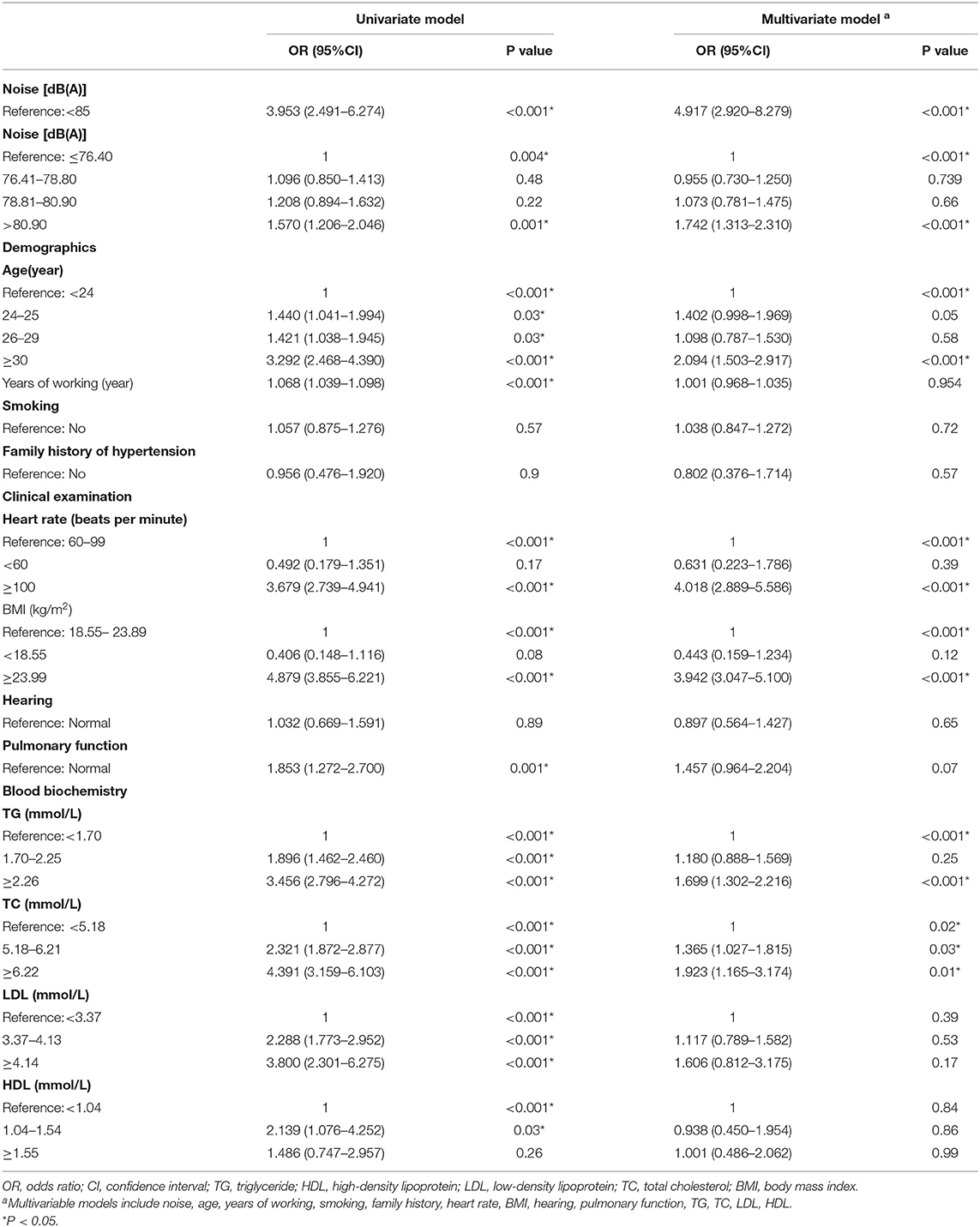
Table 2. The OR and 95% CI of the relationship between classified variables and hypertension in all participants.
Sensitivity Analysis
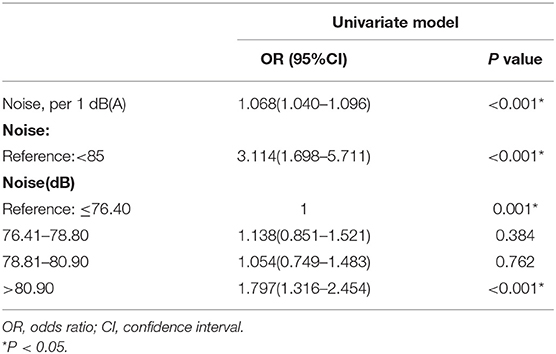
PSM was used for sensitivity analysis to minimize the effects of confounding factors. The baseline characteristics of participants after PSM are shown in Table 3. When occupational noise was analyzed as either a continuous or categorical variable, it was significantly associated with the risk of hypertension, consistent with the results of the other analyses performed (Table 4).
Dose Effect Relationship Between Noise and Hypertension
The Spearman correlation test showed that the correlation between occupational noise exposure and hypertension was significant at the 0.01 level (2-tailed). Subsequently, the RCS curve showed a positively correlated nonlinear dose-response relationship between noise exposure and hypertension (Pnonlinear = 0.002; Figure 1). The risk of hypertension was relatively stable until a predicted occupational noise level of around 80 dB(A) and then started to increase rapidly afterward.
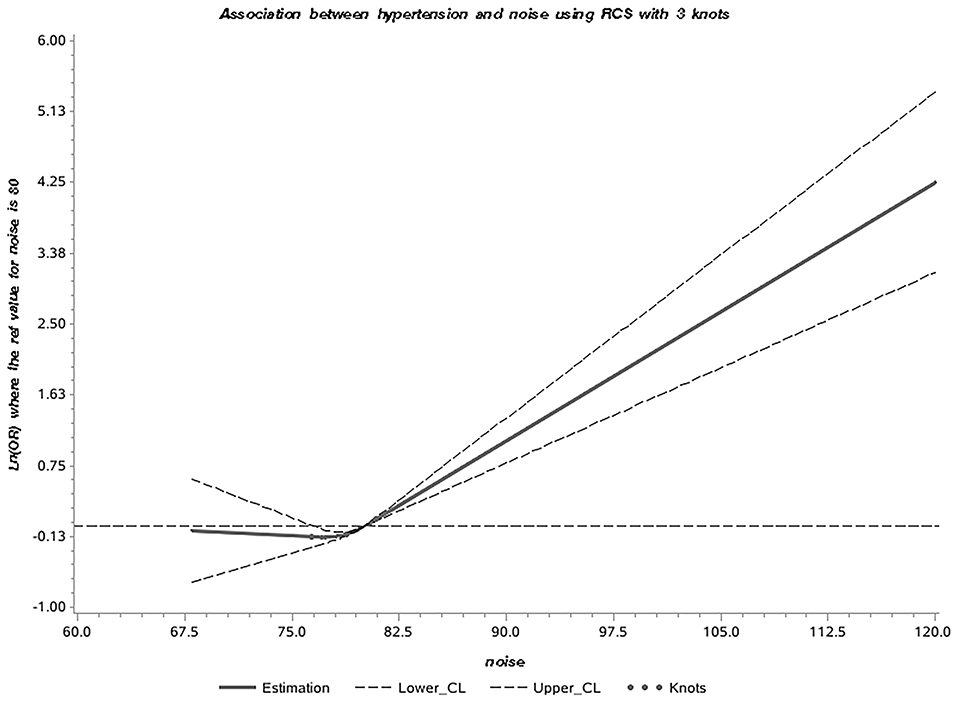
Figure 1. Dose effect relationship between occupational noise and hypertension in entire participants.
Discussion
Main Results and Description
We used a case-control study design to explore predictors of hypertension. Independent of whether occupational noise was analyzed as a continuous or categorical variable, there was a nonlinear dose-response relationship between it and hypertension.
Literature Review
We found that occupational noise exposure was associated with an increased risk of hypertension. Previous studies have reported that occupational noise exposure increases the risk of hypertension. A cross-sectional study reported this in steelworkers (OR: 2.03, 95% CI: 1.15–3.58) (12), Bolm et al. (26) conducted a meta-analysis of 24 studies and concluded that the risk of hypertension increased 1.77-fold (95% CI 1.36–2.29) for employees exposed to occupational noise levels of 80–85 dB(A), and increased 3.50-fold (95% CI 1.56–7.86) for employees exposed at 85–90 dB(A). However, Tessier et al. (13) and Stokholm et al. (14) reported an absence of any such association. The inconsistency of these findings may be attributed to the noise exposures reported in their studies not being high enough to detect an effect. In addition, the present results show a nonlinear dose-response relationship between occupational noise and the risk of hypertension. For occupational noise exposures in the range 68–80 dB(A), the risk of hypertension was relatively stable. Exposures above 80 dB(A) were associated with a risk of hypertension that increased rapidly with noise exposure level. Lin et al. (15) also reported a curved exposure-response pattern between occupational noise and hypertension, whereby the risk of hypertension increased for exposures between 82 and 106 dB(A), and then sharply decreased for exposures over 107 dB(A). This may be related to the extensive use of personal protective equipment in people exposed to high levels of occupational noise, thereby reducing the incidence of hypertension.
Study Strengths and Limitations
Hypertension is a consequence of many factors working together. The influence of potential confounding factors on research findings must be considered when analyzing the impact of noise exposure on the risk of hypertension. Multifactor regression analysis is the most commonly used method that adjusts for confounding factors, but collinearity between variables can lead to instabilities in such a model (35). Firstly, we used PSM to balance the distributions of potentially confounding variables between participant groups by matching participants in the case group with those from the control group, thereby reducing the error (36). Secondly, we used RCR regression to flexibly model the association between occupational noise and the risk of hypertension. As such, we obtained a more intuitive dose-effect relationship curve.
Our study also had some limitations. Firstly, we have no information about the use of antihypertensive drugs within the participant cohort, which may provide a confounding factor to determining the association between occupational noise exposure and hypertension. Secondly, we did not set the caliper value for the PSM, potentially leading to a deviation in the results (37). However, the balance achieved between the groups after PSM suggests that the model was stable. In addition, noise exposure and blood pressure measurements were collected at a single time point, so it is not possible to infer any causal relationship between noise exposure and hypertension. Prospective longitudinal studies will be needed to explore the causal relationship between noise exposure and hypertension.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
This study has been approved by the medical scientific research Ethics Committee of the First Affiliated Hospital of China Medical University (No. AF-SOP-07-1.0-01). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
XW, CL, and BZ contributed to conception and design of the study. XZ and YS organized the database. BZ and XW performed the statistical analysis. CL wrote the first draft of the manuscript. XW, CL, YS, and XZ wrote sections of the manuscript. XW, CL, DZ, and YL revised various parts of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.803695/full#supplementary-material
References
1. Zhou J, Shi Z, Zhou L, Hu Y, Zhang M. Occupational noise-induced hearing loss in China: a systematic review and meta-analysis. BMJ Open. (2020) 10:e039576. doi: 10.1136/bmjopen-2020-039576
2. Pyko A, Andersson N, Eriksson C, de Faire U, Lind T, Mitkovskaya N, et al. Long-term transportation noise exposure and incidence of ischaemic heart disease and stroke: a cohort study. Occup Environ Med. (2019) 76:201–7. doi: 10.1136/oemed-2018-105333
3. Beutel ME, Brahler E, Ernst M, Klein E, Reiner I, Wiltink J, et al. Noise annoyance predicts symptoms of depression, anxiety and sleep disturbance 5 years later. Findings from the Gutenberg Health Study. Eur J Public Health. (2020) 30:516–21. doi: 10.1093/eurpub/ckaa015
4. Occupational Exposure Limits for Hazardous Factors in the Workplace Part 2: Physical Factors. Beijing: China Science Publishing & Media Ltd. (CSPM) (2007). p. 14p:A4.
5. Zhao S, He D, Zhang H, Hou T, Yang C, Ding W, et al. Health study of 11,800 workers under occupational noise in Xinjiang. BMC Public Health. (2021) 21:460. doi: 10.1186/s12889-021-10496-3
6. Hypertension. Available at: https://www.who.int/health-topics/hypertension/#tab=tab_1 (accessed on September 1, 2021).
7. Rust P, Ekmekcioglu C. Impact of Salt Intake on the Pathogenesis and Treatment of Hypertension. Adv Exp Med Biol. (2017) 956:61–84. doi: 10.1007/5584_2016_147
8. Gloria-Bottini F, Banci M, Neri A, Magrini A, Bottini E. Smoking and hypertension: Effect of adenosine deaminase polymorphism. Clin Exp Hypertens. (2019) 41:548–51. doi: 10.1080/10641963.2018.1516776
9. Becton LJ, Shatat IF, Flynn JT. Hypertension and obesity: epidemiology, mechanisms and clinical approach. Indian J Pediatr. (2012) 79:1056–61. doi: 10.1007/s12098-012-0777-x
10. Zeeb H, Hegewald J, Schubert M, Wagner M, Droge P, Swart E, et al. Traffic noise and hypertension - results from a large case-control study. Environ Res. (2017) 157:110–7. doi: 10.1016/j.envres.2017.05.019
11. Seidler A, Wagner M, Schubert M, Droge P, Romer K, Pons-Kuhnemann J, et al. Aircraft, road and railway traffic noise as risk factors for heart failure and hypertensive heart disease-A case-control study based on secondary data. Int J Hyg Environ Health. (2016) 219:749–58. doi: 10.1016/j.ijheh.2016.09.012
12. Zhou F, Shrestha A, Mai S, Tao Z, Li J, Wang Z, et al. Relationship between occupational noise exposure and hypertension: A cross-sectional study in steel factories. Am J Ind Med. (2019) 62:961–8. doi: 10.1002/ajim.23034
13. Tessier-Sherman B, Galusha D, Cantley LF, Cullen MR, Rabinowitz PM, Neitzel RL. Occupational noise exposure and risk of hypertension in an industrial workforce. Am J Ind Med. (2017) 60:1031–8. doi: 10.1002/ajim.22775
14. Stokholm ZA, Bonde JP, Christensen KL, Hansen AM, Kolstad HA. Occupational noise exposure and the risk of hypertension. Epidemiology. (2013) 24:135–42. doi: 10.1097/EDE.0b013e31826b7f76
15. Lin YT, Chen TW, Chang YC, Chen ML, Hwang BF. Relationship between time-varying exposure to occupational noise and incident hypertension: A prospective cohort study. Int J Hyg Environ Health. (2020) 226:113487. doi: 10.1016/j.ijheh.2020.113487
16. Said MA, El-Gohary OA. Effect of noise stress on cardiovascular system in adult male albino rat: implication of stress hormones, endothelial dysfunction and oxidative stress. Gen Physiol Biophys. (2016) 35:371–7. doi: 10.4149/gpb_2016003
17. Joyner MJ, Charkoudian N, Wallin BG A. sympathetic view of the sympathetic nervous system and human blood pressure regulation. Exp Physiol. (2008) 93:715–24. doi: 10.1113/expphysiol.2007.039545
18. Munzel T, Daiber A, Steven S, Tran LP, Ullmann E, Kossmann S, et al. Effects of noise on vascular function, oxidative stress, and inflammation: mechanistic insight from studies in mice. Eur Heart J. (2017) 38:2838–49. doi: 10.1093/eurheartj/ehx081
19. Schmidt FP, Basner M, Kroger G, Weck S, Schnorbus B, Muttray A, et al. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur Heart J. (2013) 34:3508-14a. doi: 10.1093/eurheartj/eht269
20. Hahad O, Prochaska JH, Daiber A, Muenzel T. Environmental noise-induced effects on stress hormones, oxidative stress, and vascular dysfunction: key factors in the relationship between cerebrocardiovascular and psychological disorders. Oxid Med Cell Longev. (2019) 2019:4623109. doi: 10.1155/2019/4623109
21. Wang D, Zhou M, Li W, Kong W, Wang Z, Guo Y, et al. Occupational noise exposure and hypertension: the Dongfeng-Tongji Cohort Study. J Am Soc Hypertens. (2018) 12:71–9 e5. doi: 10.1016/j.jash.2017.11.001
22. Yang Y, Zhang E, Zhang J, Chen S, Yu G, Liu X, et al. Relationship between occupational noise exposure and the risk factors of cardiovascular disease in China: A meta-analysis. Medicine (Baltimore). (2018) 97:e11720. doi: 10.1097/MD.0000000000011720
23. Rabiei H, Ramezanifar S, Hassanipour S, Gharari N. Investigating the effects of occupational and environmental noise on cardiovascular diseases: a systematic review and meta-analysis. Environ Sci Pollut Res Int. (2021) 28:62012–29. doi: 10.1007/s11356-021-16540-4
24. Fu W, Wang C, Zou L, Liu Q, Gan Y, Yan S, et al. Association between exposure to noise and risk of hypertension: a meta-analysis of observational epidemiological studies. J Hypertens. (2017) 35:2358–66. doi: 10.1097/HJH.0000000000001504
25. Tomei G, Fioravanti M, Cerratti D, Sancini A, Tomao E, Rosati MV, et al. Occupational exposure to noise and the cardiovascular system: a meta-analysis. Sci Total Environ. (2010) 408:681–9. doi: 10.1016/j.scitotenv.2009.10.071
26. Bolm-Audorff U, Hegewald J, Pretzsch A, Freiberg A, Nienhaus A, Seidler A. Occupational Noise and Hypertension Risk: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. (2020) 17:6281. doi: 10.3390/ijerph17176281
27. Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. (2007) 4:e297. doi: 10.1371/journal.pmed.0040297
28. Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension (vol 39, pg 3021, 2018). Eur Heart J. (2019) 40:475. doi: 10.1093/eurheartj/ehy686
29. de Francisco ALM, Varas J, Ramos R, Merello JI, Canaud B, Stuard S, et al. Proton Pump Inhibitor Usage and the Risk of Mortality in Hemodialysis Patients. Kidney Int Rep. (2018) 3:374–84. doi: 10.1016/j.ekir.2017.11.001
30. Junren Zhu, Runlin Gao, Shuiping Zhao, Guoping Lu, Dong Zhao, Jianjun Li. Guidelines for the prevention and treatment of dyslipidemia in Chinese adults (revised in 2016). Chin J Health Manage. (2017) 11:7-28 %@1674-0815%L11-5624/R%WCNKI.
31. Staffa SJ, Zurakowski D. Five Steps to Successfully Implement and Evaluate Propensity Score Matching in Clinical Research Studies. Anesth Analg. (2018) 127:1066–73. doi: 10.1213/ANE.0000000000002787
32. Varas J, Perez-Saez MJ, Ramos R, Merello JI, de Francisco ALM, Luno J, et al. Returning to haemodialysis after kidney allograft failure: a survival study with propensity score matching. Nephrol Dial Transplant. (2019) 34:667–72. doi: 10.1093/ndt/gfy215
33. Austin PC. Goodness-of-fit diagnostics for the propensity score model when estimating treatment effects using covariate adjustment with the propensity score. Pharmacoepidemiol Drug Saf. (2008) 17:1202–17. doi: 10.1002/pds.1673
34. Thoemmes, F,. Propensity Score Matching in SPSS. Available at: http://arxiv.org/abs/1201.6385 (accessed on December 2, 2021).
35. Wilson A, Zigler CM, Patel CJ, Dominici F. Model-averaged confounder adjustment for estimating multivariate exposure effects with linear regression. Biometrics. (2018) 74:1034–44. doi: 10.1111/biom.12860
36. Benedetto U, Head SJ, Angelini GD, Blackstone EH. Statistical primer: propensity score matching and its alternatives. Eur J Cardiothorac Surg. (2018) 53:1112–7. doi: 10.1093/ejcts/ezy167
Keywords: hypertension, noise, dose effect relationship, epidemiology, risk factors
Citation: Wu X, Li C, Zhang X, Song Y, Zhao D, Lan Y and Zhou B (2022) The Impact of Occupational Noise on Hypertension Risk: A Case-Control Study in Automobile Factory Personnel. Front. Cardiovasc. Med. 9:803695. doi: 10.3389/fcvm.2022.803695
Received: 03 November 2021; Accepted: 25 January 2022;
Published: 17 February 2022.
Edited by:
Yuli Huang, Southern Medical University, ChinaReviewed by:
Denis Vinnikov, Al-Farabi Kazakh National University, KazakhstanJavier Varas, Novartis, Spain
Copyright © 2022 Wu, Li, Zhang, Song, Zhao, Lan and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Zhou, emhvdWJvQGNtdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Xiaomei Wu
Xiaomei Wu Chaoxiu Li
Chaoxiu Li Xiaohong Zhang
Xiaohong Zhang Yumeng Song
Yumeng Song Dan Zhao
Dan Zhao YueYan Lan
YueYan Lan Bo Zhou
Bo Zhou