- 1Australasian College of Sport and Exercise Physicians, Melbourne, VIC, Australia
- 2Agnes Ginges Centre for Molecular Cardiology, Centenary Institute and The University of Sydney, Sydney, NSW, Australia
- 3Clinical Research Department, Baker Heart and Diabetes Institute, Melbourne, VIC, Australia
- 4Faculty of Medicine and Health, The University of Sydney, Sydney, NSW, Australia
- 5Department of Physiotherapy, Centre for Health, Exercise and Sports Medicine, Melbourne School of Health Sciences, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Carlton, VIC, Australia
Aims: Cardiac rehabilitation (CR) is an evidence-based intervention promoting risk factor modification following coronary artery disease events but the relative benefits for patient subgroups is not clear. This review synthesizes the available evidence on the effectiveness of modern CR programs and determines outcomes for age, sex and prior level of fitness.
Methods: MEDLINE, CINAHL, and EMBASE were examined for RCT and cohort studies involving exercise prescription or phase II or III CR following Myocardial Infarction (MI), Percutaneous Coronary Intervention (PCI) and cardiac surgery from January 2010 to February 2021. Outcomes assessed included peakVO2max, 6-min walk test and Metabolic Equivalent of Task. Meta-regression was used to determine CR impact for change in fitness and age and sex influences.
Results: The mean age of study participants was 59.5 years and 82.7% were male. Females, younger people and those of average or above cardiorespiratory fitness were substantially under-represented in data and attendance, with 13% of study groups with a mean age <55 years. At entry, 73% were below average for fitness vs. age-matched normative values. Fitness improved across all groups following CR with no evidence of sex or age independently affecting outcomes.
Conclusions: Modest improvements in fitness in all groups were shown, but the benefits of CR can be far greater. A modern, innovative approach to CR will likely lead to more substantial benefits. This may require a “Precision Medicine” model which tailors exercise prescription to different populations to ensure all CR participant's needs are met. This will ensure that CR is more flexible and accessible for all.
Introduction
Cardiovascular disease (CVD) is a leading contributor to global morbidity and mortality, causing approximately one third of total deaths annually (1). Mortality rates in high-income countries range from 20 to 50% (2, 3), with the worldwide disease burden from CVD being approximately 20% (1).
Cardiac rehabilitation (CR) is a multidisciplinary, evidence-based intervention (4), composed of a multifaceted set of interventions that aim to address common, modifiable risk factors for coronary artery disease (5). CR programs include risk factor education, behavior change and psychological support, but perhaps most importantly, exercise (5). Modern CR programs including early moderate intensity aerobic exercise (6) or high intensity training (7, 8) are well validated, safe and encouraged in current CR guidelines (9, 10).
Most international exercise guidelines focus on aerobic training as part of CR (11). There are significant variations in the way this is prescribed with regards to frequency, intensity, duration and type, as well as the length of the programs and whether resistance training is included (11). Guidelines tend to be generalisable in order to be applied to all patients, with variation minimized in exercise prescription between different clinical conditions and patients (11).
Although coronary heart disease and myocardial infarction (MI) predominantly affects older adults, young men or women can suffer MI. This carries significant morbidity, psychological and financial effects and high disease-adjusted life year (DALY) burdens (12). The prevalence of the disease in men and women aged between 45 and 54 years in England in 2019 was 2.7% (13), although other studies have shown this figure to be as high as 4% in people aged ≤40 years (14). A study in Melbourne, Australia, found that 20% of MI admissions were younger than 55 years (15). Evidence points toward younger CR patients having a higher rate of non-participation and dropout in CR (16). Secondary prevention is of utmost importance, particularly in younger people. Mortality in young patients with MI is as high as 30% at 15-year follow-up (17). Also of note, over a 14-year time period from 2003 to 2017 in England, while prevalence of coronary heart disease decreased by 25–43% in age groups aged over 55 years, there was no change in prevalence in the 44–54 years age group (13).
Women represent 36.3% of AMI presentations (18). Studies have shown that significantly fewer women subsequently access CR than men (19, 20), and those who do are less likely to complete the full duration of the program (21). Ritchey et al. (4) found that <1 in 5 women who are offered CR attend available programs. Women are not only less likely to receive evidence-based management, including revascularisation, preventative medications and CR, but they also often have poorer long-term outcomes (22).
Boyer et al. (23) showed that the characteristics of acute myocardial infarction (AMI) patients was changing in their study between 2003 and 2008. Their data showed an increasing proportion of AMI patients represented the 45 to 65-year-old age group in both males and females.
With this growing evidence pointing toward an increasing proportion of comparatively younger cardiac patients, as well as a lack of uptake of CR in females and younger people, we hypothesized that a similar trend would also be seen in patients entering CR from an average or above average fitness level for their age.
This study aimed to examine the effectiveness of modern (since 2010). CR programs, but perhaps more importantly, whether they examined for benefit in an increasingly heterogenous group of patients regardless of age, sex and prior level of fitness. The study also sought to assess whether the demographics of cardiac rehabilitation participants is changing in tandem with the changes in demographics seen in sufferers of AMI.
Methods
This study was performed according to the “PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions” (24).
Search Strategy
The literature search was performed using the MEDLINE, CINAHL, and EMBASE databases from January 2010 to February 2021. Search terms included: acute coronary syndrome, myocardial ischemia, coronary artery disease, heart valve disease, cardiovascular disease, cardiac event, coronary artery bypass graft, percutaneous coronary intervention, angioplasty, stent, valve repair, valve prosthesis, valve replacement, cardiac surgery, cardiac catheterisation, cardiac rehabilitation, exercise training and secondary prevention. The full search strategy is included in the Supplementary Material.
Inclusion/Exclusion Criteria
Studies were included if they satisfied the following criteria: (i) original research published in English, (ii) contemporary, that is, published after January 2010, (iii) study population was adults over 18 years, (iv) studied Phase II (after discharge from hospital) or phase III CR programs (supervised or unsupervised outpatient CR), (v) described CR programs post myocardial infarction, PCI or cardiac surgery. Exclusion criteria were: (i) studies using only Phase I CR (in-patient, post event), (ii) inadequately described the exercise/rehabilitation protocol used, (iii) had fewer than 10 participants.
Study Selection
Two researchers (MS and JF) screened the searched articles by title and abstract and all studies meeting the inclusion criteria were reviewed by full text. Any issues with eligibility were resolved by discussion with a third researcher (JO).
Data Extraction
Data were extracted from the studies onto an Excel (Microsoft Corporation, USA) spreadsheet for analysis. Data extracted included author, year of publication, country of study, study design, number of participants, age, sex ratios, indication for CR, level of fitness at entry measured by baseline cardiorespiratory function tests, supervision level, CR setting, phase of rehabilitation, exercise program type, intensity and duration, primary and secondary outcome measures and dropout rates. Assessment of study methodological quality (type of study, level of evidence, performance of a power analysis, treatment allocation, blinding, dropout rates and methodological flaws) was performed. Only studies with level of evidence IV or greater were included to minimize bias. This is shown in Table 1.
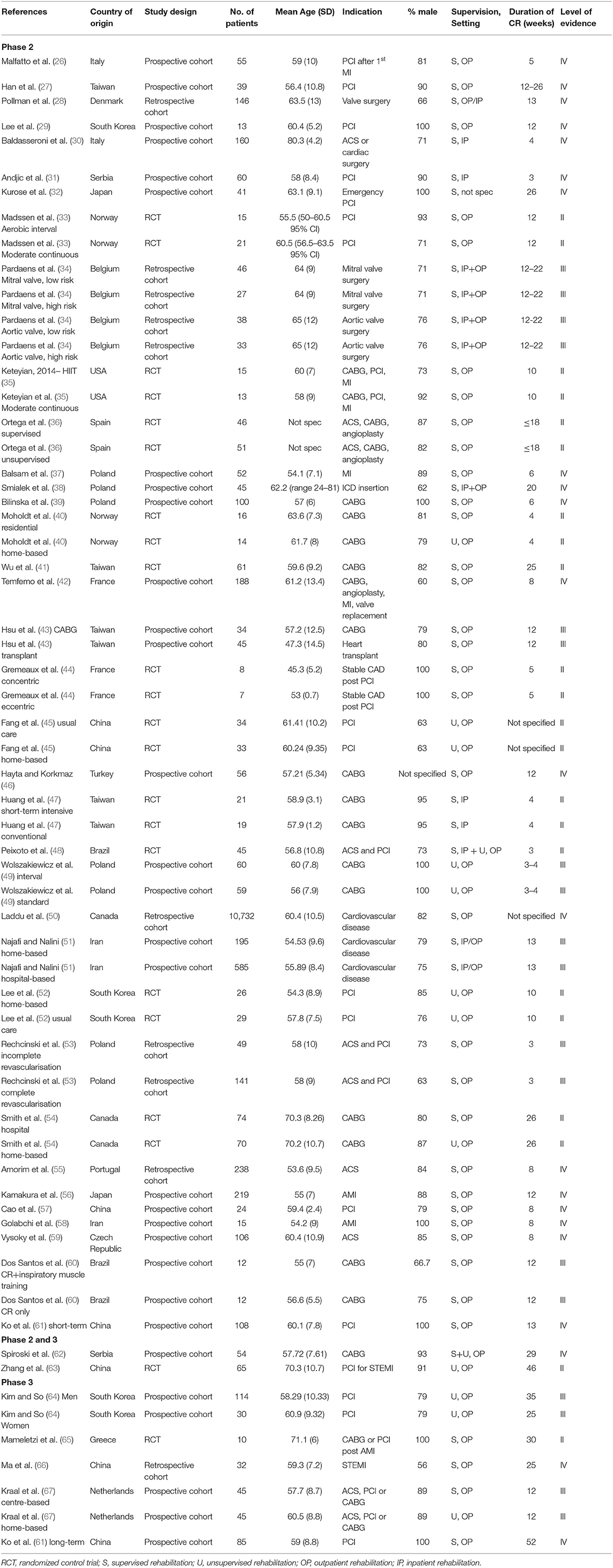
Table 1. Summary of study groups included within meta-analysis, with study types, key demographic data, CR delivery type and indication for CR. Level of evidence grading based on (25).
Statistical Analyses
Statistical analysis was performed using Stata software (Version 14.0). Data from studies using the same outcome measures peak VO2max, 6-min walk test (6MWT) and Metabolic Equivalent of Task (METs) was pooled and analyzed with 95% confidence intervals (CIs) reported to assess for change in cardiorespiratory fitness from baseline to exit from rehabilitation. Where studies compared two different CR methods rather than a control group, both exercise protocols were included separately in the analysis. Where studies utilized two or more cardiorespiratory outcome measures, all were included. Heterogeneity assessed using an I2 test and a fixed effects model was used. A meta-regression analysis was performed to determine the effect of other factors, specifically age and sex.
Results
Study Characteristics and Patient Characteristics
The initial search identified 2,726 studies (Figure 1). A total of 23 duplicates were removed, and 2,565 records were excluded based on title and/or abstract screening, leaving 138 for full-text review. A further 96 articles were excluded due to lack of exercise prescription, no cardiac event, having only Phase I CR, no outcome measures to assess change in cardiorespiratory status, or were protocols or review articles. Thus 42 articles were available for quantitative analysis, of which 13 were randomized controlled trials (33, 35, 36, 40, 41, 44, 45, 47, 48, 52, 54, 63, 65) and 29 were cohort studies (26–32, 34, 37–39, 42, 43, 46, 49–51, 53, 55–62, 64, 66, 67). Included papers are shown in Table 1, together with study results and the level of evidence of the study. Studies were conducted primarily in Europe (21 studies) and Asia (16 studies) but also included Canada (2) and Brazil (2) and the USA (1).
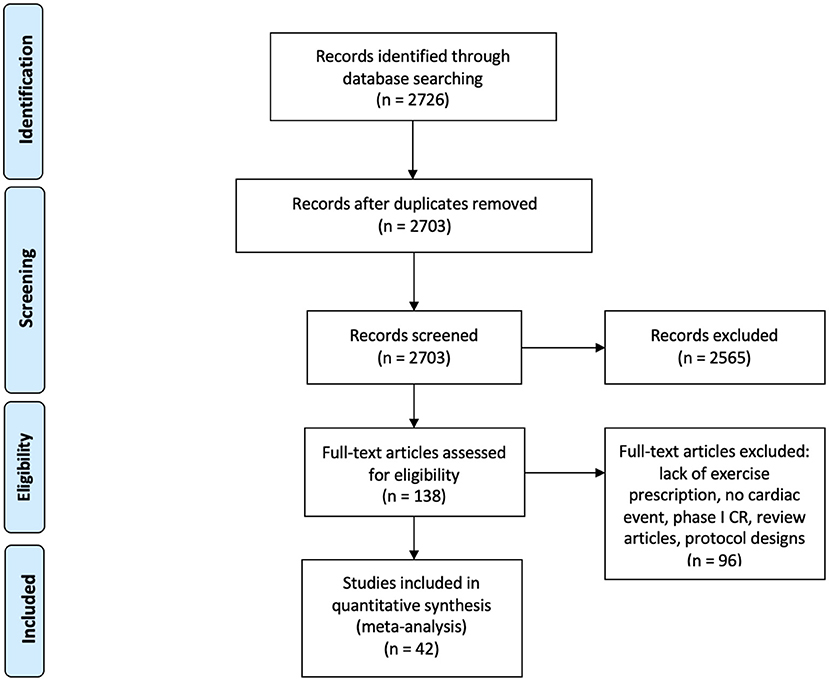
Figure 1. Preferred reporting items for systematic reviews and meta-analyses flow diagram of study selection.
A total of 14,683 patients were included in the study data. The mean age of study participants was 59.5 years (range of means 45.3–80.3 years). Eighteen studies included comparison of differing exercise protocols (including one that separated into four study groups), creating 62 groups of patients that completed CR. Of the study groups 8/60 (13%) had a mean age <55 years [one study encompassing two groups did not report mean age of participants (36)]. The mean percentage of male participants within the study groups was 82.7%. In total, 46/61 (75%) had ≥75% of participants being male (one study did not specify the sex breakdown of study participants).
Baseline level of fitness was examined by assessing values for peak VO2max, 6-minute walk test (6MWT) and METs on entry into CR, shown in Table 2. Mean baseline levels of cardiorespiratory function were: peakVO2 23 ml/kg/min (age-based normal value = 25.1 ml/kg/min), 6MWT 420.5m (normal = 555) and baseline METs 7 (normal = 7). 27% of study groups had a mean average cardiorespiratory function level below age-matched normative values (68–70).
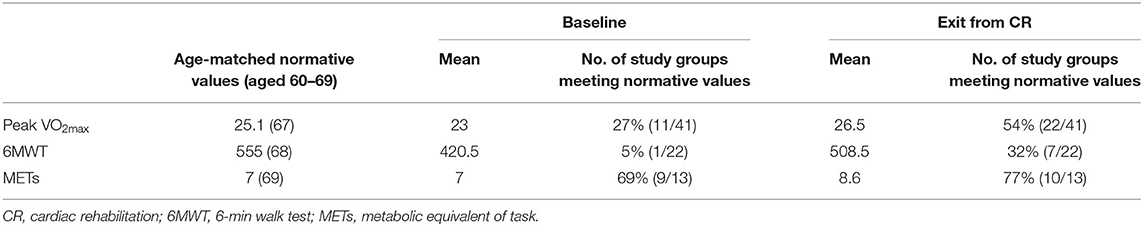
Table 2. Cardiorespiratory fitness levels on entry and exit from CR alongside normative values for community dwelling individuals aged 60–69 years.
Peak VO2 was utilized by 28 studies (26–44, 56, 57, 59–62, 64, 65, 67), 12 studies examined 6MWT (34, 44–49, 60, 61, 63, 64, 66) and 9 studies utilized METs based on formal testing (50–55, 57–59). Multiple outcome measures were used in 7 studies (34, 44, 57, 59–61, 64). Dropout rate was specified in 16 of the studies (29, 33, 35, 36, 39–42, 44, 45, 51–54, 64, 65). The rate varied from 2 to 75%, with a mean dropout rate of 19.3%.
The duration of CR programs varied from 3 to 52 weeks, with a mean duration of 14.8 weeks. The prescribed programs are shown in Supplementary Table 1. The type of exercise prescribed varied, and included: walking (outdoor or treadmill), stationary bike, stationary stepping, stair climbing, swimming, arm ergometer, elliptical trainer, cross-country skiing, rowing and gymnastics. In some studies, strength training, calisthenics, or flexibility training were also included, but this was not examined in this study. Frequency of exercise was on average 3 sessions per week (range 2–10), with an average time of 38 min (range 10–90) min per session. Intensity levels varied between groups and were expressed as either: a percentage of VO2peak (5 groups, average 59–75% of VO2peak) a percentage of maximum or peak heart rate (11 groups, average 71–82% of maximum HR), a percentage of heart rate reserve (HRR) (13 groups, average 53.5–78% of HRR) or exercise at anaerobic or ventilatory threshold levels (6 groups). Nine study groups specified interval training, with the remainder focused on steady state training. Three studies were determined to be high-intensity interval training (HIIT) when defined as ≥85% of VO2max (71).
Cardiorespiratory fitness increased in all measures assessed across all study groups examined in this study. Change in peakVO2max was assessed in a total of 2,141 patients, with an observed change of 3.23 ml/kg/min (2.86–3.60, 95% confidence interval). Mean change in 6MWT was examined in 999 patients, with a mean change of 86.98 m (64.54–109.42, 95% confidence interval) on exiting CR. The utilization of METs to assess change in fitness was used in 12,248 patients in total, showing a mean average improvement in METs of 1.53 METs (1.28–1.78, 95% confidence interval) from entry to exit from CR (Figure 2).
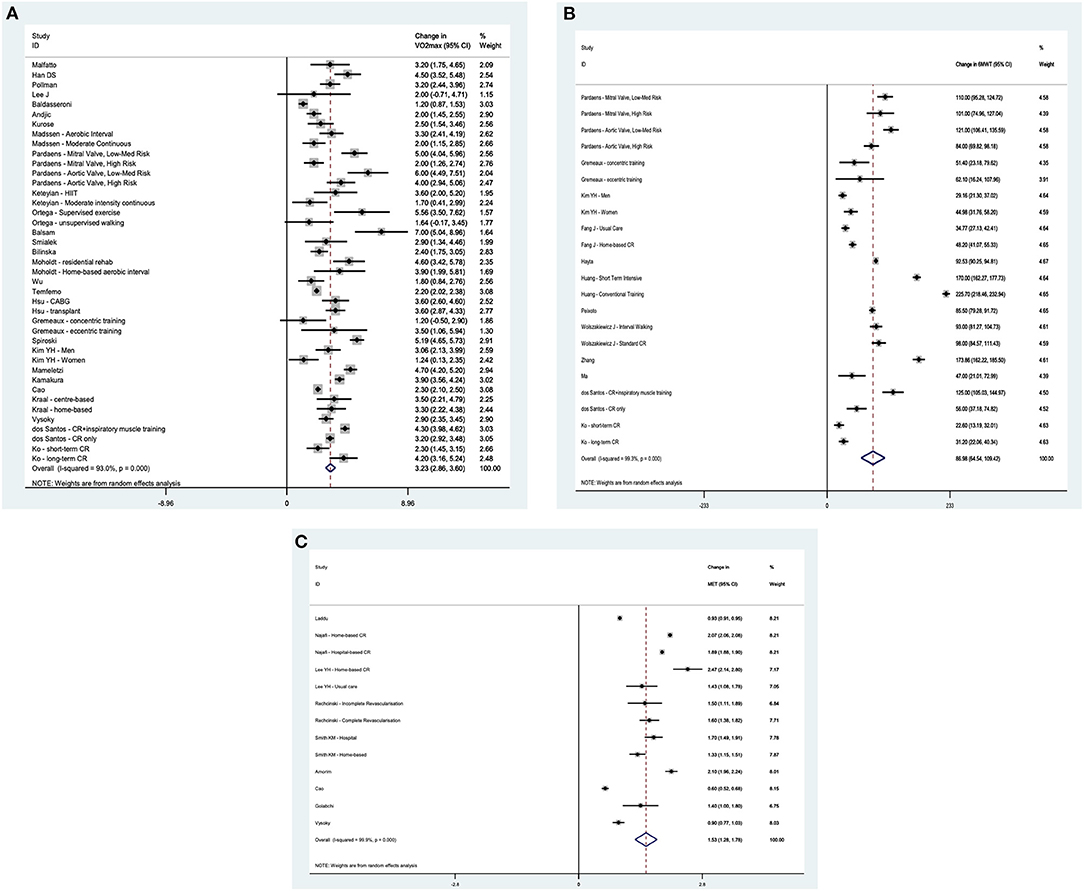
Figure 2. (A) Forest plot showing changes in VO2max in phase II and III cardiac rehabilitation programs. (B) Forest plot showing changes in 6MWT in phase II and III cardiac rehabilitation programs. (C) Forest plot showing changes in METs in phase II and III cardiac rehabilitation programs.
The proportion of patients meeting population age and sex referenced normative values for cardiorespiratory fitness increased across each of the three domains. On entry to CR, 27% (11/41) of study groups had a mean peakVO2max at the level or above age-matched normative values. This increased to 54% (22/41) on exit from CR. Improvements were also seen in 6MWT from 5% (1/22 study groups) to 32% (7/22 study groups) and METs from 69% (9/13 study groups) to 77% (10/13 study groups).
A further meta-regression analysis was performed to assess the independent effects of age and sex on change in cardiorespiratory fitness with CR. For each outcome measure, age and proportion of male participants had no significant impact upon improvement in cardiorespiratory function following CR. The results of this analysis are shown in Table 3.
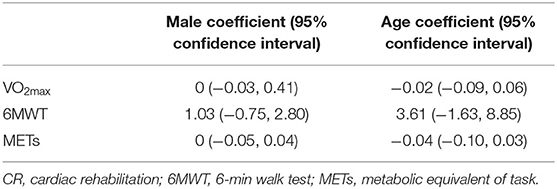
Table 3. Meta-regression analysis of the independent effects of age and sex on change in VO2max, 6MWT and METs following CR.
Discussion
This study presents a comprehensive review of the characteristics of modern CR attendees and study participants and the wide variations in how exercise is prescribed for patients. Our meta-analysis utilizes data from 42 studies, encompassing four continents over the past 11 years and involving 14,683 patients. Our results provide evidence that cardiac rehabilitation significantly improves the cardiorespiratory performance of attendees. It also demonstrates that within the dataset, the average CR patient is 60 years old, male and with low baseline cardiorespiratory fitness. The mean dropout rate in the studies examined in this review was 19.3%, which is concerning that we are potentially not meeting the needs for 1 in 5 patients. Whilst there is variability in the frequency, intensity, type and duration of CR programs, it may be that modern CR programs are focused for the mean average patient rather than tailored for individual needs.
Sex
Lower uptake of CR in women compared to men has been identified in multiple studies (4, 19–21). Similarly, our study showed that only 17% of patients completing CR were female. This is despite 36.3% of patients suffering AMI being female (18), which would be represented the AMI and PCI aspects of this patient cohort. In addition, three-quarters of study groups had a male to female ratio of >3:1. Reasons previously attributed for this discrepancy have included: inadequate CR education and referral, transport and health system reasons, and competing demands (such as caregiver responsibilities) (72). However, even after age and covariate adjustment, women were found to be 9% less likely to attend CR and 13% less likely to complete CR after commencement (4).
Some efforts have been made to improve CR uptake and completion among female cardiac patients. One commonly used approach is to have sex-specific or women-only CR programs (22). This can lead to greater adherence (73), improved mental health outcomes (74) and comparable functional outcomes when compared to mixed sex CR (75), as well as improved satisfaction from participants (76). These classes more commonly offer alternative forms of exercise, such as dance and yoga. However, as an example in Australia, only 1% of programs offer women-only classes (22). Home-based or community-based programs have also been suggested as a potential improvement, as these have been shown to be equally effective as traditional CR (72) and may circumvent some of the potential barriers to attendance for women.
Age
Previous studies have shown that younger age is associated with a higher drop-out rate (77). There is also evidence that older patients are more likely to complete CR (78, 79). This study appears to support these findings. The mean age of subjects completing CR in the groups analyzed was 59.5 years, but the average ages of study groups were closely centered around this point, showing little variability. Only 13% of study groups had a mean age <55 years, when this age group represents 23% of patients suffering AMI (80). As a result, when assessing the efficacy of CR programs, our data indicate that the research is skewed toward the needs of those aged older than 55.
In Australia and the UK, exercise recommendations for cardiac patients are largely toward light- to moderate-intensity aerobic exercise (81–83). Lower intensity exercise is easier to implement, particularly within restricted resource situations and is more acceptable to older adults and those with physical limitations (11), but this could be a significant deterrent to younger, more athletic patients, for whom the program is “too easy” (effectively detraining). Exercise interventions in coronary artery disease patients that recommend moderate to vigorous intensity exercise have shown greater improvements in cardiorespiratory fitness and cardiac risk factors than lower intensity interventions (11), as well as being safe and well accepted. Applying these measures to younger patients may lead to better uptake and completion, and better health outcomes.
Fitness
Our study shows that the entry-level baseline level of fitness for patients completing CR was lower than that of normative data for sedentary 60–69 year-olds. We found that 73% of study groups were below average compared to their sedentary matched counterparts. That is, the majority of CR patients are below average fitness for their age.
It can be argued that acute events such as MI, PCI and cardiac surgery would be expected to acutely lower these cardiorespiratory functional measures. However, these low values may also represent drop-out or failure of inclusion of patients coming from a high level of baseline fitness capacity, and that these patients are disproportionately represented in the 19.3% of dropout cases from CR. Although this group may have lower risk for future cardiac events, the importance of transitioning them back to an acceptable level of function is high. A lack of guidance on how to progress back to normal function may increase the risk of further cardiac issues in this patient cohort.
Exercise Prescription
The average CR program lasted 15 weeks and included cardiovascular training with 3 sessions per week. The average duration of each session was 38 min. Intensity levels were on average 59–75% of VO2peak, 71–82% of maximum HR, 53.5–78% of HRR or at anaerobic or ventilatory thresholds. Only 16% of groups were specified as interval training, with the remainder focused on steady state training. HIIT programs represented only 5% of prescribed programs.
Despite this study only including phase II or III CR programs, there was great variability in the programs prescribed to patients following cardiac events. This variability encompassed duration of programs, type of exercise program, frequency and duration of sessions as well as the intensity level and individualization of rehabilitation. This variation in prescription of exercise programs makes drawing conclusions for the type of rehabilitation that works optimally for different subsets of cardiac rehabilitation very difficult.
Effectiveness of Modern CR
Cardiorespiratory fitness outcomes increased across all study groups examined in this study. Mean improvement in cardiorespiratory function was 3.23 ml/kg/min for VO2max, 86.98 m for 6MWT and 1.53 METs. The results of this study mirror those of a multitude of others showing that over the time period of CR, cardiorespiratory outcome measures improve on average in all participants.
Meta-regression analysis found that neither age nor the proportion of females to males in study groups had any significant impact upon improvement in cardiorespiratory function following CR. This highlights the importance of CR and its effectiveness for all patients, as well as the benefits that can be attained regardless of age and sex. However, it raises the question of whether this improvement could be increased further and whether rehabilitation is challenging enough or tailored enough to the patients involved.
Survival of the (Not So) Fittest
This study displays the outcomes of CR in those who complete the rehabilitation process. This study compares the demographics of these patients to those eligible to complete CR and shows that younger, female and moderate-to-high fitness individuals are under-represented. CR appears to largely meet the needs of male, older and low fitness individuals, with either a failure to be referred, a failure to attend or a failure to complete rehabilitation in those outside of these demographics. It may be that due to rehabilitation being tailored to the more unfit members of the cohort, those of higher fitness feel that their needs are not met and drop out.
Limitations
This study has a number of limitations. First, it examines CR research literature which includes both CR programs and research studies rather than a snapshot of CR programs themselves solely. Examining demographic trends within these data are beneficial and has been performed previously, but to our knowledge, no assessment of this demographic data has been performed on research study participants to this point. It is also important to reflect on the need for research looking at these specified groups and whether they benefit from rehabilitation as much as the more studied cohorts of males, sedentary and older patients.
Although this systematic review included all available literature, there were a small number of studies using each individual cardiorespiratory outcome measure resulting in high heterogeneity. Therefore, we have included only the three most widely reported outcome measures to minimize this heterogeneity. Additionally, regarding the delivery of cardiac rehabilitation, there is considerable variation particularly in the duration of cardiac rehabilitation. This varies greatly from study-to-study and country-to-country, leading to different effect sizes. The variation in the way that cardiac rehabilitation is prescribed and delivered in terms of frequency, intensity, type, and time, also means that there is unavoidable heterogeneity in results.
Most studies included did not specify baseline level of physical function and the level of physical activity prior to commencement of CR. Only 8/60 (13%) of studies specified a previous physical activity level. Baseline cardiorespiratory function testing was used for this purpose but may not adequately describe how physically active a rehabilitation participant was prior to commencement in CR. When grouped among other participants of low cardiac fitness, it will be difficult to ascertain whether the benefit gained from CR is greater or smaller than the mean for those who were previously physically active.
Dropout rate amongst studies was difficult to accurately determine as some studies only examined patients who completed CR whereas others included dropout rates from the commencement of CR. Whether these dropout rates preferentially affect younger, female and fitter patients is impossible to conclusively ascertain from this data. This is a potential area of future research, alongside further investigation into the reasons behind the poorer completion rate of each of these subgroups.
Cardiorespiratory assessment measures also appeared to be variable. In assessing baseline level of cardiorespiratory fitness, the percentage of study groups meeting age-matched normative values varied depending on which of the cardiorespiratory measures were used [peak VO2max (27%), 6MWT (5%) and METs (69%)]. This may reflect inaccuracies in the normative values but may also show the inaccuracy of cardiorespiratory function testing in general, particularly with 6MWT and METs.
Future Directions–From Efficacy to an Effective Intervention
This study highlights a number of concerns regarding the equity of CR. There appears to be a lack of research and exercise programs focused on the needs of female, young and fit patients when recovering from AMI, PCI or cardiac surgery. Taken together, this indicates large gaps in CR, with the possibility of patients “falling through the cracks” in recovering from a major life event. It also represents a potential risk of increased future cardiac events if the needs of these patients are not met.
In order to improve CR completion, it is important to address the reasons behind a lack of uptake and a lack of completion of CR in these patients. We need to ensure that CR is made more accessible and suitable to a broader range of people, as well as more appealing to those who are referred. By making CR more personalized, we can change CR from the current model of modest efficacy to an effective therapy.
Our opinion on how this is achieved is through a more patient-centric approach. Commencing any form of exercise is a two-stage process: motivation, as well as of performance. By addressing the goals, interests and motivations of the patient, greater long-term self-efficacy can be fostered. Moving away from the current paternalistic model of care does not have detrimental effects on patient outcomes and can be cost-effective, decrease fear and enhance motivation (45, 52, 84).
The future will involve a model of care that is more personalized and may be that a triage model is utilized involving clinical determinants of health as well as goals, risk factors and social determinants. Smart technology will allow a more specific, patient-centered approach, which can work better for those with time-constraints, whilst reducing stress and giving equivalent benefits to supervised training (45, 52). This can be done remotely and reach patients outside of suburban areas. Risk factors for coronary events appear to be changing, with a greater burden from sedentary behavior and lower physical fitness. By using more innovative methods to improve activity, risk factor modification can be sustainably improved.
Conclusions
This study shows that there is a striking absence of females, younger people and those of average or above cardiorespiratory fitness in CR programs. As such, we do not currently understand the optimal method for prescribing exercise in rehabilitation for these patients and must do better at adapting methods for their needs, to make cardiac rehabilitation fit for purpose.
In this study, CR showed modest improvements in cardiorespiratory fitness for all demographic groups, but with a paucity of data in some subgroups. This leads us to believe that there is the potential for improvement in outcomes. A modern, innovative process will likely lead to greater benefits. This “Precision Medicine” model of exercise prescription may assist in this aim for improvement in secondary prevention goals for all participants, whilst making CR more flexible, more accessible and more easily scheduled into modern-day life. This tailored approach, with the inclusion of adapting programs to be specific to the needs, goals and enjoyment of participants, can lead to the integration of exercise and activity into daily life long-term, which is the most effective method of long-term prevention of cardiovascular morbidity and mortality.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
MS, JO, and JF ran systematic review and assessed articles. MS, JO, JF, AL, and RG aided in writing various sections of the article. All authors contributed to the article and approved the submitted version.
Funding
JO supported by a Postdoctoral Fellowship (Award Reference No. 104809) from the National Heart Foundation of Australia.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer PQ declared a shared affiliation, with no collaboration, with one of the authors JO and RG to the handling editor at the time of the review.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We sincerely thank Dr. Hussain Khan (Australasian College of Sports and Exercise Physicians, Australia) and Quan Huynh, Ph.D. (Baker Heart and Diabetes Institute, Melbourne, Australia) for their help with the statistical analysis. We wholeheartedly thank Susie Moreton and Sandy Gill (Epworth Healthcare, Australia) for their support with the search strategy and literature search.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.764882/full#supplementary-material
References
1. Mendis S, Puska P, Norrving B, World Health O, World Heart F, World Stroke O. Global Atlas on Cardiovascular Disease Prevention and Control / Edited by: Shanthi Mendis... [et al.]. Geneva: World Health Organization (2011).
2. Bjarnason-Wehrens B, McGee H, Zwisler AD, Piepoli MF, Benzer W, Schmid JP, et al. Cardiac rehabilitation in Europe: results from the European cardiac rehabilitation inventory survey. Eur J Cardiovasc Prev Rehabil. (2010) 17:410–8. doi: 10.1097/HJR.0b013e328334f42d
3. Grace SL, Bennett S, Ardern CI, Clark AM. Cardiac rehabilitation series: Canada. Prog Cardiovasc Dis. (2014) 56:530–5. doi: 10.1016/j.pcad.2013.09.010
4. Ritchey MD, Maresh S, McNeely J, Shaffer T, Jackson SL, Keteyian SJ, et al. Tracking cardiac rehabilitation participation and completion among medicare beneficiaries to inform the efforts of a national initiative. Circ Cardiovasc Qual Outcomes. (2020) 13:e005902. doi: 10.1161/CIRCOUTCOMES.119.005902
5. Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, et al. Exercise standards for testing and training: a scientific statement from the American heart association. Circulation. (2013) 128:873–934. doi: 10.1161/CIR.0b013e31829b5b44
6. Hirschhorn AD, Richards DA, Mungovan SF, Morris NR, Adams L. Does the mode of exercise influence recovery of functional capacity in the early postoperative period after coronary artery bypass graft surgery? a randomized controlled trial. Interact Cardiovasc Thorac Surg. (2012) 15:995–1003. doi: 10.1093/icvts/ivs403
7. Quindry JC, Franklin BA, Chapman M, Humphrey R, Mathis S. Benefits and risks of high-intensity interval training in patients with coronary artery disease. Am J Cardiol. (2019) 123:1370–7. doi: 10.1016/j.amjcard.2019.01.008
8. Taylor JL, Holland DJ, Spathis JG, Beetham KS, Wisløff U, Keating SE, et al. Guidelines for the delivery and monitoring of high intensity interval training in clinical populations. Prog Cardiovasc Dis. (2019) 62:140–6. doi: 10.1016/j.pcad.2019.01.004
9. Pengelly J, Pengelly M, Lin KY, Royse C, Karri R, Royse A, et al. Exercise parameters and outcome measures used in cardiac rehabilitation programs following median sternotomy in the elderly: a systematic review and meta-analysis. Heart Lung Circ. (2019) 28:1560–70. doi: 10.1016/j.hlc.2019.05.098
10. Piepoli MF, Corrà U, Adamopoulos S, Benzer W, Bjarnason-Wehrens B, Cupples M, et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. core components, standards and outcome measures for referral and delivery: a policy statement from the cardiac rehabilitation section of the European association for cardiovascular prevention & rehabilitation endorsed by the committee for practice guidelines of the European society of cardiology. Eur J Prev Cardiol. (2014) 21:664–81. doi: 10.1177/2047487312449597
11. Price KJ, Gordon BA, Bird SR, Benson AC. A review of guidelines for cardiac rehabilitation exercise programmes: is there an international consensus? Eur J Prev Cardiol. (2016) 23:1715–33. doi: 10.1177/2047487316657669
12. Egred MVG, Davis GK Myocardial infarction in young adults. Postgrad Med J. (2005) 81:741–5. doi: 10.1136/pgmj.2004.027532
14. Fournier JA, Sánchez A, Quero J, Fernández-Cortacero JA, González-Barrero A. Myocardial infarction in men aged 40 years or less: a prospective clinical-angiographic study. Clin Cardiol. (1996) 19:631–6. doi: 10.1002/clc.4960190809
15. Loughnan ME, Nicholls N, Tapper NJ. Demographic, seasonal, and spatial differences in acute myocardial infarction admissions to hospital in Melbourne Australia. Int J Health Geogr. (2008) 7:42. doi: 10.1186/1476-072X-7-42
16. Resurrección DM, Moreno-Peral P, Gómez-Herranz M, Rubio-Valera M, Pastor L, de Almeida JMC, et al. Factors associated with non-participation in and dropout from cardiac rehabilitation programmes: a systematic review of prospective cohort studies. Eur J Cardiovasc Nurs. (2019) 18:38–47. doi: 10.1177/1474515118783157
17. Cole JH, Sperling LS, Weintraub WS. Long-term follow-up of coronary artery disease presenting in young adults. J Am Coll Cardiol. (2003) 41:521–8. doi: 10.1016/S0735-1097(02)02862-0
18. Freisinger E, Sehner S, Malyar NM, Suling A, Reinecke H, Wegscheider K. Nationwide routine-data analysis of sex differences in outcome of acute myocardial infarction. Clin Cardiol. (2018) 41:1013–21. doi: 10.1002/clc.22962
19. Colella TJ, Gravely S, Marzolini S, Grace SL, Francis JA, Oh P, et al. Sex bias in referral of women to outpatient cardiac rehabilitation? a meta-analysis. Eur J Prev Cardiol. (2015) 22:423–41. doi: 10.1177/2047487314520783
20. Samayoa L, Grace SL, Gravely S, Scott LB, Marzolini S, Colella TJ. Sex differences in cardiac rehabilitation enrollment: a meta-analysis. Can J Cardiol. (2014) 30:793–800. doi: 10.1016/j.cjca.2013.11.007
21. Oosenbrug E, Marinho RP, Zhang J, Marzolini S, Colella TJ, Pakosh M, et al. Sex differences in cardiac rehabilitation adherence: a meta-analysis. Can J Cardiol. (2016) 32:1316–24. doi: 10.1016/j.cjca.2016.01.036
22. Turk-Adawi KI, Pola MS, Lopez-Jimenez F, Adawi A, Sadeghi M, Grace S. Women-only cardiac rehabilitation delivery around the world. Heart Lung Circ. (2020) 75:1969. doi: 10.1016/S0735-1097(20)32596-1
23. Boyer NL, Laskey WK, Cox M, Hernandez A, Peterson ED, Bhatt D, et al. Trends in clinical, demographic, and biochemical characteristics of patients with acute myocardial infarction from 2003 to 2008: a report from the American heart association get with the guidelines coronary artery disease program. J Am Heart Assoc. (2012) 1:e001206. doi: 10.1161/JAHA.112.001206
24. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. (2009) 6:e1000100. doi: 10.1371/journal.pmed.1000100
25. Ackley BJ, Swan BA, Ladwig G, Tucker S. Evidence-Based Nursing Care Guidelines: Medical-Surgical Interventions. St. Louis, MO: Mosby Elsevier (2008). p. 7
26. Malfatto G, Revera M, Branzi G, Ciambellotti F, Giglio A, Blengino S, et al. A brief period of intensive cardiac rehabilitation improves global longitudinal strain and diastolic function after a first uncomplicated myocardial infarction. Acta Cardiol. (2017) 72:284–91. doi: 10.1080/00015385.2017.1305196
27. Han DS, Hsiao MY, Wang TG, Chen SY, Yang WS. Relation between serum myokines and phase II cardiac rehabilitation. Medicine. (2017) 96:e6579. doi: 10.1097/MD.0000000000006579
28. Pollmann AGE, Frederiksen M, Prescott E. Cardiac rehabilitation after heart valve surgery: improvement in exercise capacity and morbidity. J Cardiopulm Rehabil Prev. (2017) 37:191–8. doi: 10.1097/HCR.0000000000000208
29. Lee J, Song Y, Lindquist R, Yoo Y, Park E, Lim S, et al. Nontraditional cardiac rehabilitation in Korean patients with coronary artery disease. Rehabil Nurs J. (2017) 42:191–8. doi: 10.1002/rnj.268
30. Baldasseroni S, Pratesi A, Francini S, Pallante R, Barucci R, Orso F, et al. Cardiac rehabilitation in very old adults: effect of baseline functional capacity on treatment effectiveness. J Am Geriatr Soc. (2016) 64:1640–5. doi: 10.1111/jgs.14239
31. Andjic M, Spiroski D, Ilic Stojanovic O, Vidakovic T, Lazovic M, Babic D, et al. Effect of short-term exercise training in patients following acute myocardial infarction treated with primary percutaneous coronary intervention. Eur J Phys Rehabil Med. (2016) 52:364–9.
32. Kurose S, Iwasaka J, Tsutsumi H, Yamanaka Y, Shinno H, Fukushima Y, et al. Effect of exercise-based cardiac rehabilitation on non-culprit mild coronary plaques in the culprit coronary artery of patients with acute coronary syndrome. Heart Vessel. (2016) 31:846–54. doi: 10.1007/s00380-015-0681-1
33. Madssen E, Moholdt T, Videm V, Wisloff U, Hegbom K, Wiseth R. Coronary atheroma regression and plaque characteristics assessed by grayscale and radiofrequency intravascular ultrasound after aerobic exercise. Am J Cardiol. (2014) 114:1504–11. doi: 10.1016/j.amjcard.2014.08.012
34. Pardaens S, Moerman V, Willems AM, Calders P, Bartunek J, Vanderheyden M, et al. Impact of the preoperative risk and the type of surgery on exercise capacity and training after valvular surgery. Am J Cardiol. (2014) 113:1383–9. doi: 10.1016/j.amjcard.2014.01.413
35. Keteyian SJ, Hibner BA, Bronsteen K, Kerrigan D, Aldred HA, Reasons LM, et al. Greater improvement in cardiorespiratory fitness using higher-intensity interval training in the standard cardiac rehabilitation setting. J Cardiopulm Rehabil Prev. (2014) 34:98–105. doi: 10.1097/HCR.0000000000000049
36. Ortega R, Garcia-Ortiz L, Torcal J, Echevarria P, Vargas-Machuca C, Gomez A, et al. Supervised exercise for acute coronary patients in primary care: a randomized clinical trial. Fam Pract. (2014) 31:20–9. doi: 10.1093/fampra/cmt059
37. Balsam P, Glowczynska R, Zaczek R, Szmit S, Opolski G, Filipiak KJ. The effect of cycle ergometer exercise training on improvement of exercise capacity in patients after myocardial infarction. Kardiol Pol. (2013) 71:1059–64. doi: 10.5603/KP.2013.0261
38. Smialek J, Lelakowski J, Majewski J. Efficacy and safety of early comprehensive cardiac rehabilitation following the implantation of cardioverter-defibrillator. Kardiol Pol. (2013) 71:1021–8. doi: 10.5603/KP.2013.0256
39. Bilinska M, Kosydar-Piechna M, Mikulski T, Piotrowicz E, Gasiorowska A, Piotrowski W, et al. Influence of aerobic training on neurohormonal and hemodynamic responses to head-up tilt test and on autonomic nervous activity at rest and after exercise in patients after bypass surgery. Cardiol J. (2013) 20:17–24. doi: 10.5603/CJ.2013.0004
40. Moholdt T, Bekken Vold M, Grimsmo J, Slordahl SA, Wisloff U. Home-based aerobic interval training improves peak oxygen uptake equal to residential cardiac rehabilitation: a randomized, controlled trial. PLoS ONE. (2012) 7:e41199. doi: 10.1371/journal.pone.0041199
41. Wu YT, Wu YW, Hwang CL, Wang SS. Changes in diastolic function after exercise training in patients with and without diabetes mellitus after coronary artery bypass surgery. a randomized controlled trial. Eur J Phys Rehabil Med. (2012) 48:351–60.
42. Temfemo A, Chlif M, Mandengue SH, Lelard T, Choquet D, Ahmaidi S. Is there a beneficial effect difference between age, gender, and different cardiac pathology groups of exercise training at ventilatory threshold in cardiac patients? Cardiol J. (2011) 18:632–8. doi: 10.5603/CJ.2011.0026
43. Hsu CJ, Chen SY, Su S, Yang MC, Lan C, Chou NK, et al. The effect of early cardiac rehabilitation on health-related quality of life among heart transplant recipients and patients with coronary artery bypass graft surgery. Transplant Proc. (2011) 43:2714–7. doi: 10.1016/j.transproceed.2011.04.025
44. Gremeaux V, Duclay J, Deley G, Philipp JL, Laroche D, Pousson M, et al. Does eccentric endurance training improve walking capacity in patients with coronary artery disease? a randomized controlled pilot study. Clin Rehabil. (2010) 24:590–9. doi: 10.1177/0269215510362322
45. Fang J, Huang B, Xu D, Li J, Au WW. Innovative application of a home-based and remote sensing cardiac rehabilitation protocol in chinese patients after percutaneous coronary intervention. Telemed J E Health. (2019) 25:288–93. doi: 10.1089/tmj.2018.0064
46. Hayta E, Korkmaz O. Cardiac rehabilitation increases the reliability of the 6-minute walk test in patients after coronary artery bypass graft surgery. Heart Surgery Forum. (2017) 20:E247–E51. doi: 10.1532/hsf.1737
47. Huang SC, Wong MK, Lin PJ, Tsai FC, Chu JJ, Wu MY, et al. Short-term intensive training attenuates the exercise-induced interaction of mono-1/2 cells and platelets after coronary bypass in cardiac patients. Thromb Haemost. (2017) 117:1761–71. doi: 10.1160/TH17-03-0184
48. Peixoto TC, Begot I, Bolzan DW, Machado L, Reis MS, Papa V, et al. Early exercise-based rehabilitation improves health-related quality of life and functional capacity after acute myocardial infarction: a randomized controlled trial. Can J Cardiol. (2015) 31:308–13. doi: 10.1016/j.cjca.2014.11.014
49. Wolszakiewicz J, Piotrowicz E, Foss-Nieradko B, Dobraszkiewicz-Wasilewska B, Piotrowicz R. A novel model of exercise walking training in patients after coronary artery bypass grafting. Kardiol Pol. (2015) 73:118–26. doi: 10.5603/KP.a2014.0165
50. Laddu D, Ozemek C, Lamb B, Hauer T, Aggarwal S, Stone JA, et al. Factors associated with cardiorespiratory fitness at completion of cardiac rehabilitation: identification of specific patient features requiring attention. Can J Cardiol. (2018) 34:925–32. doi: 10.1016/j.cjca.2018.03.015
51. Najafi F, Nalini M. Hospital-based versus hybrid cardiac rehabilitation program in coronary bypass surgery patients in western Iran: effects on exercise capacity, risk factors, psychological factors, and quality of life. J Cardiopulm Rehabil Prev. (2015) 35:29–36. doi: 10.1097/HCR.0000000000000087
52. Lee YH, Hur SH, Sohn J, Lee HM, Park NH, Cho YK, et al. Impact of home-based exercise training with wireless monitoring on patients with acute coronary syndrome undergoing percutaneous coronary intervention. J Korean Med Sci. (2013) 28:564–8. doi: 10.3346/jkms.2013.28.4.564
53. Rechcinski T, Kalowski M, Kasprzak JD, Trzos E, Kurpesa M. Beneficial effects of cardiac rehabilitation in patients with incomplete revascularization after primary coronary angioplasty. Eur J Phys Rehabil Med. (2013) 49:785–91.
54. Smith KM, McKelvie RS, Thorpe KE, Arthur HM. Six-year follow-up of a randomised controlled trial examining hospital versus home-based exercise training after coronary artery bypass graft surgery. Heart. (2011) 97:1169–74. doi: 10.1136/hrt.2010.202036
55. Amorim H, Cadilha R, Parada F, Rocha A. Progression of aerobic exercise intensity in a cardiac rehabilitation program. Rev Port Cardiol. (2019) 38:281–6. doi: 10.1016/j.repc.2018.07.009
56. Kamakura T, Kawakami R, Nakanishi M, Ibuki M, Ohara T, Yanase M, et al. Efficacy of out-patient cardiac rehabilitation in low prognostic risk patients after acute myocardial infarction in primary intervention era. Circ J. (2011) 75:315–21. doi: 10.1253/circj.CJ-10-0813
57. Cao RY, Zheng H, Mi Q, Li Q, Yuan W, Ding Y, et al. Aerobic exercise-based cardiac rehabilitation in Chinese patients with coronary heart disease: study protocol for a pilot randomized controlled trial. Trials. (2018) 19:363. doi: 10.1186/s13063-018-2771-8
58. Golabchi A, Basati F, Kargarfard M, Sadeghi M. Can cardiac rehabilitation programs improve functional capacity and left ventricular diastolic function in patients with mechanical reperfusion after ST elevation myocardial infarction? : a double-blind clinical trial. ARYA Atheroscler. (2012) 8:125–9.
59. Vysoký R, Fiala J, Dosbaba F. Bat'alik L, Nehyba S, Ludka O. Preventive training programme for patients after acute coronary event– correlation between selected parameters and age groups. Cent Eur J Public Health. (2015) 23:208–13. doi: 10.21101/cejph.a4125
60. Dos Santos TD, Pereira SN, Portela LOC, Cardoso DM, Lago PD, Dos Santos Guarda N, et al. Moderate-to-high intensity inspiratory muscle training improves the effects of combined training on exercise capacity in patients after coronary artery bypass graft surgery: a randomized clinical trial. Int J Cardiol. (2019) 279:40–6. doi: 10.1016/j.ijcard.2018.12.013
61. Ko DH, Lee K, Chung J. Effects of long-term and short-term Cardiac Rehabilitation programs on cardiovascular risk factors and physical fitness after Percutaneous Coronary Intervention. J Mens Health. (2020) 6:29–37. doi: 10.15586/jomh.v16i3.253
62. Spiroski D, Andjic M, Stojanovic OI, Lazovic M, Dikic AD, Ostojic M, et al. Very short/short-term benefit of inpatient/outpatient cardiac rehabilitation programs after coronary artery bypass grafting surgery. Clin Cardiol. (2017) 40:281–6. doi: 10.1002/clc.22656
63. Zhang Y, Cao H, Jiang P, Tang H. Cardiac rehabilitation in acute myocardial infarction patients after percutaneous coronary intervention: a community-based study. Medicine. (2018) 97:e9785. doi: 10.1097/MD.0000000000009785
64. Kim YH, So WY. Gender differences in home-based cardiac rehabilitation of post-percutaneous coronary intervention patients. Aging Clin Exp Res. (2019) 31:249–55. doi: 10.1007/s40520-018-0951-8
65. Mameletzi D, Kouidi E, Koutlianos N, Deligiannis A. Effects of long-term exercise training on cardiac baroreflex sensitivity in patients with coronary artery disease: a randomized controlled trial. Clin Rehabil. (2011) 25:217–27. doi: 10.1177/0269215510380825
66. Ma L, Xiong X, Yan L, Qu J, Hujie G, Ma Y, et al. Home-based exercise is associated with improved cardiac functional performance in patients after acute myocardial infarction. J Int Med Res. (2020) 48:300060520977637. doi: 10.1177/0300060520977637
67. Kraal JJ, Van den Akker-Van Marle ME, Abu-Hanna A, Stut W, Peek N, Kemps HM. Clinical and cost-effectiveness of home-based cardiac rehabilitation compared to conventional, centre-based cardiac rehabilitation: results of the FIT@Home study. Eur J Prev Cardiol. (2017) 24:1260–73. doi: 10.1177/2047487317710803
68. Kaminsky LA, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing: data from the fitness registry and the importance of exercise national database. Mayo Clin Proc. (2015) 90:1515–23. doi: 10.1016/j.mayocp.2015.07.026
69. Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: six-minute walk test, berg balance scale, timed up & go test, and gait speeds. Phys Ther. (2002) 82:128–37. doi: 10.1093/ptj/82.2.128
70. Jetté MSK, Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol. (1990) 13:555–65. doi: 10.1002/clc.4960130809
71. Ballesta-García I, Martínez-González-Moro I, Ramos-Campo DJ, Carrasco-Poyatos M. High-intensity interval circuit training versus moderate-intensity continuous training on cardiorespiratory fitness in middle-aged and older women: a randomized controlled trial. Int J Environ Res Public Health. (2020) 17:1805. doi: 10.3390/ijerph17051805
72. Resurrección DM, Motrico E, Rubio-Valera M, Mora-Pardo JA, Moreno-Peral P. Reasons for dropout from cardiac rehabilitation programs in women: a qualitative study. PLoS ONE. (2018) 13:e0200636. doi: 10.1371/journal.pone.0200636
73. Gunn E, Bray SR, Mataseje L, Aquila E. Psychosocial outcomes and adherence in a Women's only exercise and education cardiac rehabilitation program. J Cardiopulm Rehabil Prev. (2007) 27:345. doi: 10.1097/01.HCR.0000291377.52385.9d
74. Midence L, Arthur HM, Oh P, Stewart DE, Grace SL. Women's health behaviours and psychosocial well-being by cardiac rehabilitation program model: a randomized controlled trial. Can J Cardiol. (2016) 32:956–62. doi: 10.1016/j.cjca.2015.10.007
75. Grace SL, Midence L, Oh P, Brister S, Chessex C, Stewart DE, Arthur HM. Cardiac rehabilitation program adherence and functional capacity among women: a randomized controlled trial. Mayo Clin Proc. (2016) 91:140–8. doi: 10.1016/j.mayocp.2015.10.021
76. Grace SL, Racco C, Chessex C, Rivera T, Oh P. A narrative review on women and cardiac rehabilitation: program adherence and preferences for alternative models of care. Maturitas. (2010) 67:203–8. doi: 10.1016/j.maturitas.2010.07.001
77. Mikkelsen T, Korsgaard Thomsen K, Tchijevitch O. Non-attendance and drop-out in cardiac rehabilitation among patients with ischaemic heart disease. Dan Med J. (2014) 61:A4919.
78. Martin BJ, Hauer T, Austford LD, Knudtson ML, Arena R, Meldrum DA, Aggarwal S, Stone JA. Cardiac rehabilitation: characteristics of those who drop out after initiating a program. Circulation. (2018) 128:A17051. doi: 10.1161/circ.128.suppl_22.A17051
79. Sarrafzadegan N, Rabiei K, Shirani S, Kabir A, Mohammadifard N, Roohafza H. Drop-out predictors in cardiac rehabilitation programmes and the impact of sex differences among coronary heart disease patients in an Iranian sample: a cohort study. Clin Rehabil. (2007) 21:362–72. doi: 10.1177/0269215507072193
80. Rosengren A, Wallentin L, Simoons M, Gitt AK, Behar S, Battler A, et al. Age, clinical presentation and outcome of acute coronary syndromes in the euroheart acute coronary syndrome survey. Eur Heart J. (2006) 27:789–95. doi: 10.1093/eurheartj/ehi774
81. Probert H, Barritt H, Breen S, Buckley J, Burgess L, Graham K, et al. Standards for Physical Activity and Exercise in the Cardiovascular Population 3rd ed. Manchester: Association of Chartered Physiotherapists in Cardiac Rehabilitation (2015).
82. Network SIG. Cardiac Rehabilitation: A National Clinical Guideline. Edinburgh: Scottish Intercollegiate Guidelines Network. (2015). Available online at: http://www.scotphn.net/wp-content/uploads/2015/11/Cardiac_Rehabilitation.pdf (accessed December 13, 2020).
83. Association NHFoAaACR. Recommended Framework for Cardiac Rehabilitation National Heart Foundation of Australia. (2019). Available online at: http://www.heartfoundation.org.au (accessed December 13, 2020).
Keywords: exercise, exercise prescription, cardiac rehabilitation, women, young, risk factors
Citation: Smith M, Orchard J, La Gerche A, Gallagher R and Fitzpatrick J (2022) Fit, Female or Fifty–Is Cardiac Rehabilitation “Fit” for Purpose for All? A Systematic Review and Meta-Analysis With Meta-Regression. Front. Cardiovasc. Med. 9:764882. doi: 10.3389/fcvm.2022.764882
Received: 26 August 2021; Accepted: 07 March 2022;
Published: 29 March 2022.
Edited by:
Nicola Mumoli, ASST Ovest Milanese, ItalyReviewed by:
Jing Kang, University of Leeds, United KingdomPierre Qian, The University of Sydney, Australia
Karen Søgaard, University of Southern Denmark, Denmark
Copyright © 2022 Smith, Orchard, La Gerche, Gallagher and Fitzpatrick. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martin Smith, bWFydGluLnNtaXRoJiN4MDAwNDA7ZHJtYXJ0aW5zbWl0aC5jb20uYXU=
 Martin Smith
Martin Smith Jessica Orchard
Jessica Orchard Andre La Gerche
Andre La Gerche Robyn Gallagher4
Robyn Gallagher4