- Department of Cardiology, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, China
Background: The optimal revascularization strategy in patients with ST-segment elevation myocardial infarction (STEMI) complicating by cardiogenic shock (CS) remains controversial. This study aims to evaluate the clinical outcomes of multivessel percutaneous coronary intervention (MV-PCI) compared to culprit vessel-only PCI (CO-PCI) for the treatment, only in patients with STEMI with CS.
Methods: A comprehensive literature search was conducted. Studies assessed the efficacy outcomes of short (in-hospital or 30 days)/long-term mortality, cardiac death, myocardial reinfarction, repeat revascularization, and safety outcomes of stroke, bleeding, acute renal failure with MV-PCI vs. CO-PCI in patients with STEMI with CS were included. The publication bias and sensitivity analysis were also performed.
Results: A total of 15 studies were included in this meta-analysis. There was no significant difference in short- and long-term mortality in patients treated with MV-PCI compared to CO-PCI group [odds ratio (OR) = 1.17; 95% confidence interval (CI), 0.92–1.48; OR = 0.86; 95% CI, 0.58–1.28]. Similarly, there were no significant differences in cardiac death (OR = 0.67; 95% CI, 0.44–1.00), myocardial reinfarction (OR = 1.24; 95% CI, 0.77–2.00), repeat revascularization (OR = 0.75; 95% CI, 0.40–1.42), bleeding (OR = 1.53; 95% CI, 0.53–4.43), or stroke (OR = 1.42; 95% CI, 0.90–2.23) between the two groups. There was a higher risk in acute renal failure (OR = 1.33; 95% CI, 1.04–1.69) in patients treated with MV-PCI when compared with CO-PCI.
Conclusion: This meta-analysis suggests that there may be no significant benefit for patients with STEMI complicating CS treated with MV-PCI compared with CO-PCI, and patients are at increased risk of developing acute renal failure after MV-PCI intervention.
Introduction
Cardiogenic shock (CS) occurs in 6–12% of patients with ST-segment elevation myocardial infarction (STEMI) and is associated with increased mortality (1–3). Previous randomized study has suggested that early revascularization in patients with acute myocardial infarction (AMI) with CS could improve the short/long-term survival rate (4). However, there remains high mortality at 40–50% despite the increasing use of early revascularization with percutaneous coronary intervention (PCI) among these patients (2). It was reported that most patients with STEMI with CS have underlying multivessel coronary artery disease (CAD), which is associated with worse outcomes (5–7). Previous randomized controlled trials (RCTs) have suggested that multivessel PCI (MV-PCI) is associated with improved clinical outcomes compared with culprit-vessel only PCI (CO-PCI), but these trials did not comprise patients with CS (8–11). Meanwhile, limited randomized data exist regarding the treatment effect of MV-PCI compared with CO-PCI for patients with STEMI with CS. The United States guidelines suggest that due to pump failure, for patients with STEMI with CS, PCI of a severe stenosis in a large non-infarct artery might improve hemodynamic stability and should be considered during the primary procedure (12). Similarly, the European guidelines on myocardial revascularization state that during STEMI, MV-PCI should be considered in patients with CS in the presence of multiple, critical stenosis or highly unstable lesions, and whether there is persistent ischemia after PCI on the supposed culprit lesion remains unclear (13).
However, the supporting evidence is largely based on pathophysiology considerations and extrapolation of data from clinical trials that included patients with hemodynamically stable STEMI, but not on non-randomized studies in patients with CS. Observational studies have revealed conflicting results when comparing MV-PCI vs. CO-PCI in AMI patients with CS (1, 14–26). In addition, several observational studies have also included patients with STEMI and non-STEMI (NSTEMI), which have different clinical profile, treatment, and outcomes (1, 15, 17, 18, 24). Furthermore, prior meta-analyses have included studies in patients with or without shock when comparing the clinical outcomes of MV-PCI vs. CO-PCI (27, 28). Data for patients with STEMI with CS alone may still be inadequate.
Therefore, we reconducted a systematic review and meta-analysis to investigate the clinical outcomes of MV-PCI compared to CO-PCI for the treatment only in patients with STEMI with CS.
Methods
Data Sources and Search Strategy
Two authors (Bingquan Xiong and Qiang She) systematically searched the databases of PubMed, Web of Science, and Medicine for related articles published in English language before December 1, 2020. We used the following keywords: “percutaneous coronary intervention,” “PCI,” “ST-segment elevation myocardial infarction,” “STEMI,” “myocardial infarction,” “cardiogenic shock,” and “multivessel disease” for the search. We included the studies that met the following criteria: (1) studies included patients presented with STEMI and CS, (2) studies comparing the clinical outcomes of MV-PCI vs. CO-PCI, (3) studies that included more than 10 cases in each treatment group, and (4) studies where, at minimum, reported data of interest on short-term mortality for each group. We excluded studies that met any one of the following criteria: (1) review articles, (2) duplicate publication, and (3) abstract or conference publications. In addition, the reference lists of retrieved articles were manually searched for potentially relevant articles. Any difference in article assessments between the two authors was resolved by group discussion. The present study was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (29).
Data Extraction and Quality Assessment
Two authors (Bingquan Xiong and Qiang She) independently extracted the data using a standardized approach, and disagreements were resolved by consensus. Data were collected as follows: study and patient characteristics, baseline clinical characteristics, interventional details, data of clinical outcomes, and follow-up duration. We assessed the quality of included studies using the Newcastle–Ottawa scale (NOS), which assigns a star to each item based on the three domains: selection of study groups (4 criteria), comparability of groups (1 criterion), and ascertainment of outcome/exposure (3 criteria) (30).
Definition and Endpoints
The CO-PCI was defined as PCI confined to culprit vessel lesions only. The MV-PCI was defined as PCI confined to the culprit vessel lesions and ≥ 1 non-culprit vessel lesions. The number of additional PCI received was comparable between the two groups. Multivessel disease (MVD) was defined as the angiographic detection of significant stenosis (≥50% of lumen diameter) in at least one major non-infarct-related artery. As for the follow-up time, the short term was defined as the time period until hospital discharge or 30 days following the index hospitalization, whereas the long term was defined as the time period extending ≥6 months after index hospitalization. The interest primary outcome was short-term all-cause mortality in this study. Secondary efficacy outcomes included long-term mortality, cardiac death, myocardial reinfarction, and repeat revascularization. Secondary safety outcomes were stroke, bleeding, and renal failure. Since the follow-up time of short term and long term was different across studies, we used the longest available follow-up data from each study for the outcomes of interest in our analysis.
Statistical Analysis
All the extracted data were pooled to estimate the combined odds ratio (OR) and 95% confidence interval (CI) using the random or fixed-effects models, based on whether there is the existence of heterogeneity. We conducted the sensitivity analysis by recalculating the combined effect estimates after omitting one study at a time (leave-one-out method). The presence of heterogeneity was assessed using I2 statistics and the Cochrane Q tests, when values of I2 > 50% and p ≤ 0.1 for the Cochrane Q test were considered as the existence of substantial heterogeneity. Publication bias was assessed using Egger’s regression test and visual inspection of asymmetry in funnel plots. All the statistical tests were two-tailed, and p < 0.05 was considered as statistically significant. We conducted all the analyses using the STATA version 14 (StataCorp LP, College Station, TX, United States).
Results
Characteristics of the Included Studies
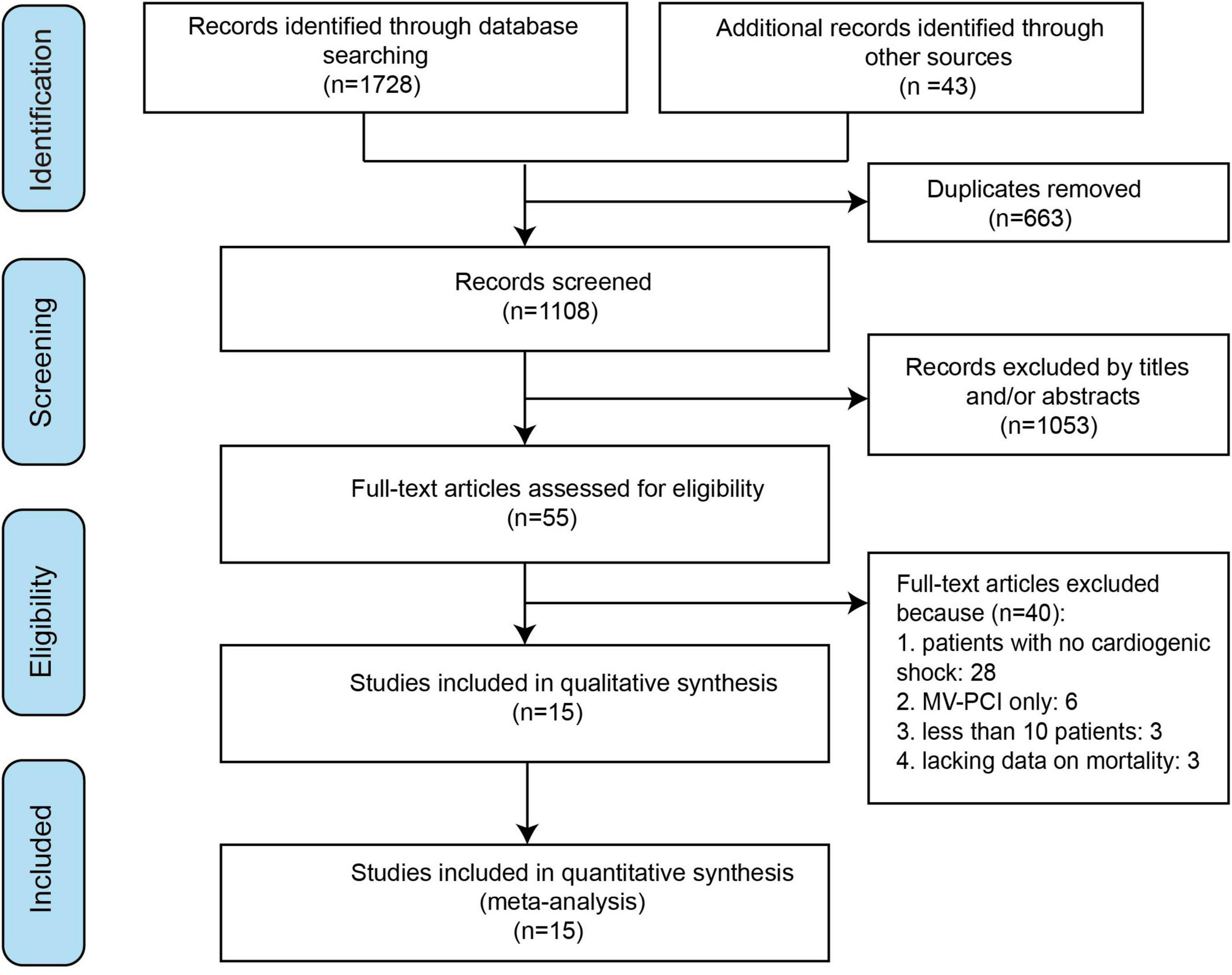
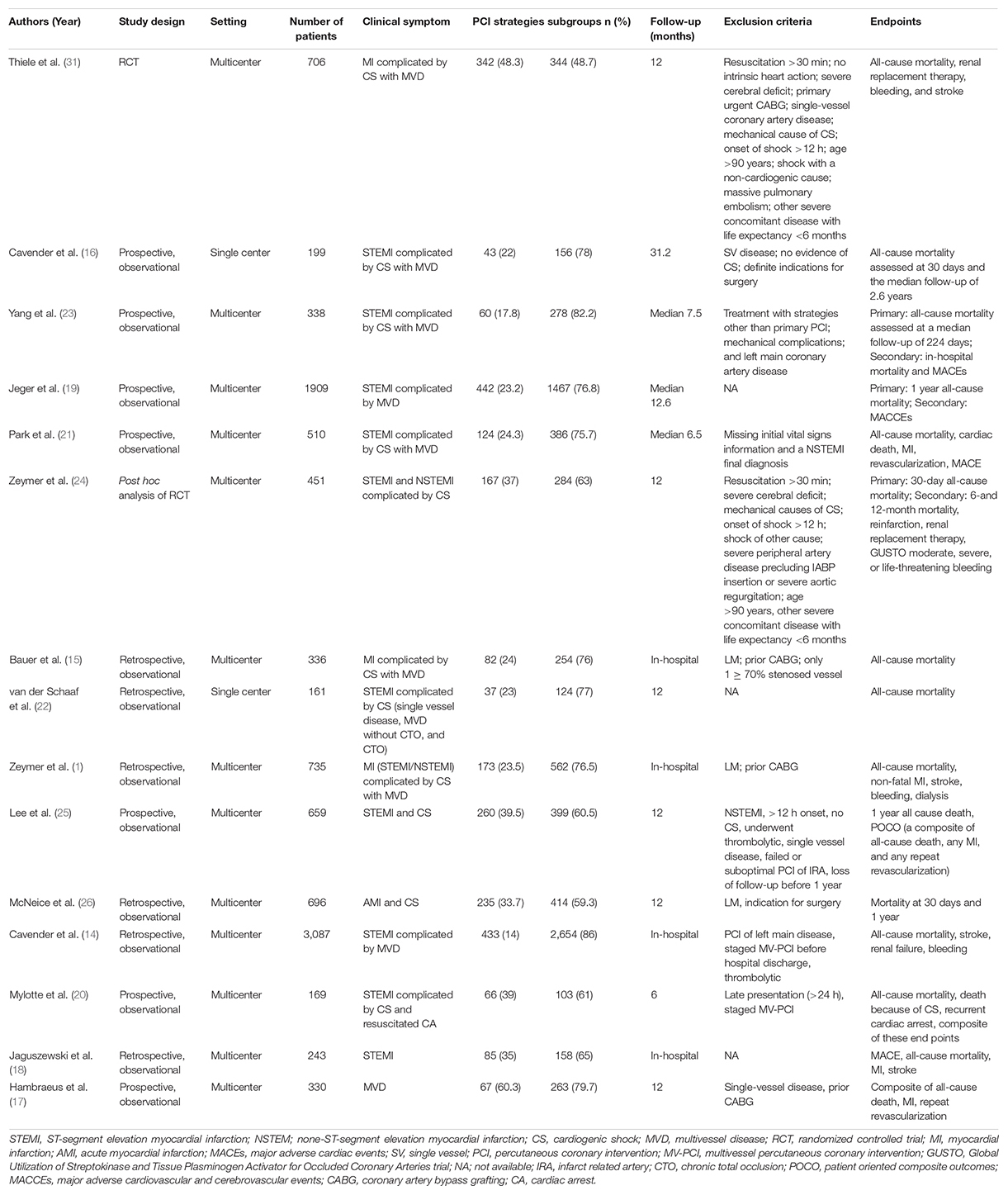
A total of 15 studies were finally included in the meta-analysis (1, 14–26, 31). The detailed study selection process is shown in Figure 1. Table 1 summarizes the characteristics of the included individual studies. Among the 15 studies, 1 was an RCT, 1 was a post hoc analysis of RCT, 6 were retrospective, and 7 were prospective. Of the 13 non-randomized studies, 2 studies were from single center, whereas the remaining studies were from national multicenter registries. The definitions of MVD and CS were somewhat different. A total of 4 patients in CO-PCI group received coronary artery bypass graft (CABG) (23), whereas 6 patients in MV-PCI group received scheduled non-urgent CABG (20). Three and 1 patients in MV-PCI group received repeat PCI on target vessel and on non-target vessel, respectively. And 9 patients in CO-PCI group received repeat PCI on non-target vessel (23). However, there was no difference in the incidence rate of repeated PCI and CABG after routine PCI treatment between the two groups (23). The baseline characteristics of patient for the treatment groups of MV-PCI and CO-PCI are comparable and are summarized in Table 2.

Table 2. Baseline characteristics according to treatment strategy reported in the individual studies.
Efficacy Outcomes
A total of 13 studies reported the data on primary efficacy endpoint of short-term all-cause mortality. There was no statistically significant difference in short-term mortality with MV-PCI compared with CO-PCI (OR = 1.17, 95% CI = 0.92–1.48, p < 0.01, I2 = 63%; Figure 2). We found that there might be publication bias for all-cause short-term mortality (Supplementary Figure 1; Egger’s test: p = 0.006). There were 10 studies reporting the outcome of long-term mortality and 5 studies reporting cardiac death. No significant difference in long-term mortality (OR = 0.86, 95% CI = 0.58–1.28, p < 0.01, I2 = 74%; Figure 3) and a borderline significant difference in cardiac death (OR = 0.67, 95% CI = 0.44–1.00, p = 0.23, I2 = 60%; Figure 4) were found between MV-PCI and CO-PCI groups. Furthermore, there might be no publication bias for long-term mortality (Supplementary Figure 2; Egger’s test: p = 0.860) and myocardial reinfarction (Supplementary Figure 3; Egger’s test: p = 0.991). Data on repeat revascularization and myocardial reinfarction were reported in 7 and 9 studies, respectively. No statistically significant difference in the risk of myocardial reinfarction (OR = 1.24, 95% CI = 0.77–2.00, p = 0.65, I2 = 0%; Figure 5) or repeat revascularization (OR = 0.75, 95% CI = 0.40–1.42, p < 0.01, I2 = 75%; Figure 6) was found between the two groups. There was publication bias for the secondary efficacy endpoints of repeat revascularization (Supplementary Figure 4; Egger’s test: p = 0.532) and cardiac death (Supplementary Figure 5; Egger’s test: p = 0.587).

Figure 2. Short-term mortality with multivessel (MV) vs. culprit vessel-only (CO) percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock (CS).
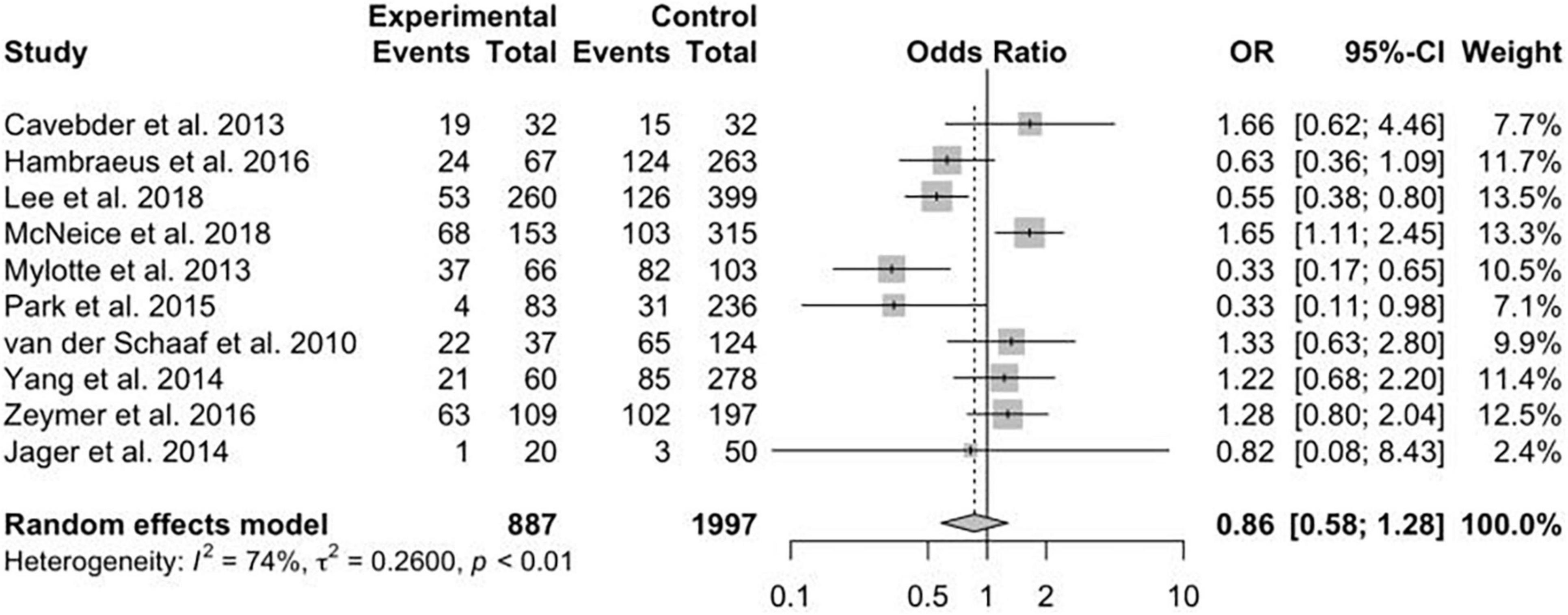
Figure 3. Long-term mortality with multivessel (MV) vs. culprit vessel-only (CO) percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock (CS).
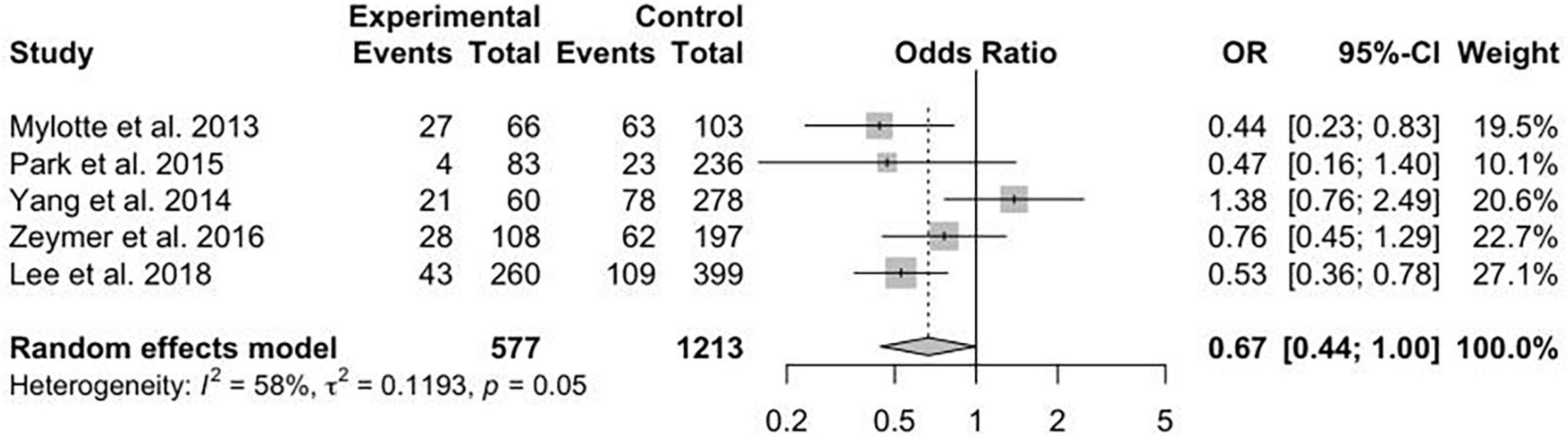
Figure 4. Cardiac death with multivessel (MV) vs. culprit vessel-only (CO) percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock (CS).
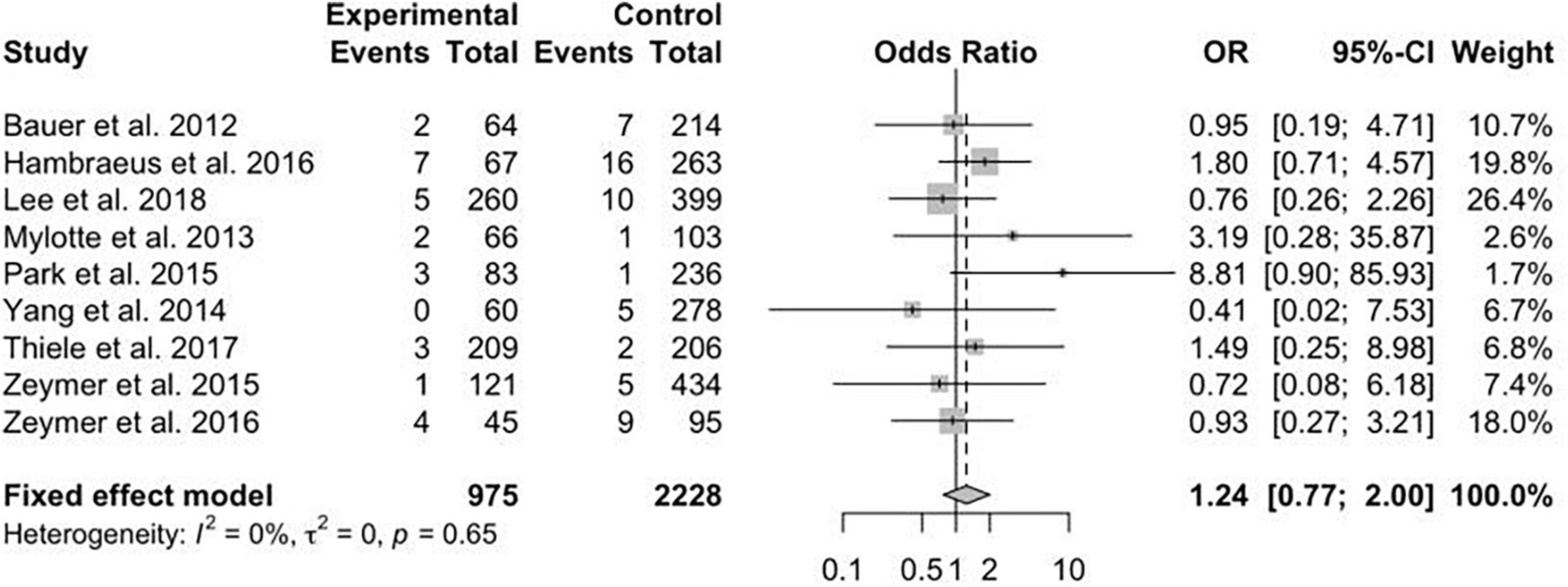
Figure 5. Myocardial reinfarction (MI) with multivessel (MV) vs. culprit vessel-only (CO) percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock (CS).

Figure 6. Repeat revascularization reinfarction (MI) with multivessel (MV) vs. culprit vessel-only (CO) percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock (CS).
Sensitivity analyses were performed for the efficacy outcomes to assess the robustness of result using the leave-one-out method. It was demonstrated that excluding a single study did not significantly alter the overall outcomes for long-term mortality, cardiac death, myocardial reinfarction, and repeat revascularization. However, for short-term mortality, excluding the study of Mylotte et al. (20) changed the statistical significance of the overall pooled estimate (OR = 1.31; 95% CI, 1.10–1.57; Supplementary Figures 6–10).
Safety Outcomes
The data concerning renal failure has been reported in 9 studies. There was a statistically significant higher risk of acute renal failure in patients treated with MV-PCI compared with CO-PCI (OR = 1.33; 95% CI, 1.04–1.69; p = 0.74, I2 = 0%; Figure 7). The safety outcome of bleeding was reported in 8 studies, and no statistically significant difference was found between MV-PCI and CO-PCI (OR = 1.53; 95% CI, 0.53–4.43; p < 0.01, I2 = 90%; Figure 8). Finally, stroke was reported in 9 studies, and no significant difference was found between the two groups (OR = 1.42; 95% CI, 0.90–2.23; p = 0.71, I2 = 0%; Figure 9). Publication bias was observed for the safety outcome of bleeding (Supplementary Figure 11; Egger’s test: p = 0.069), but no publication bias was found about renal failure (Supplementary Figure 12; Egger’s test: p = 0.281) and stroke (Supplementary Figure 13; Egger’s test: p = 0.587).
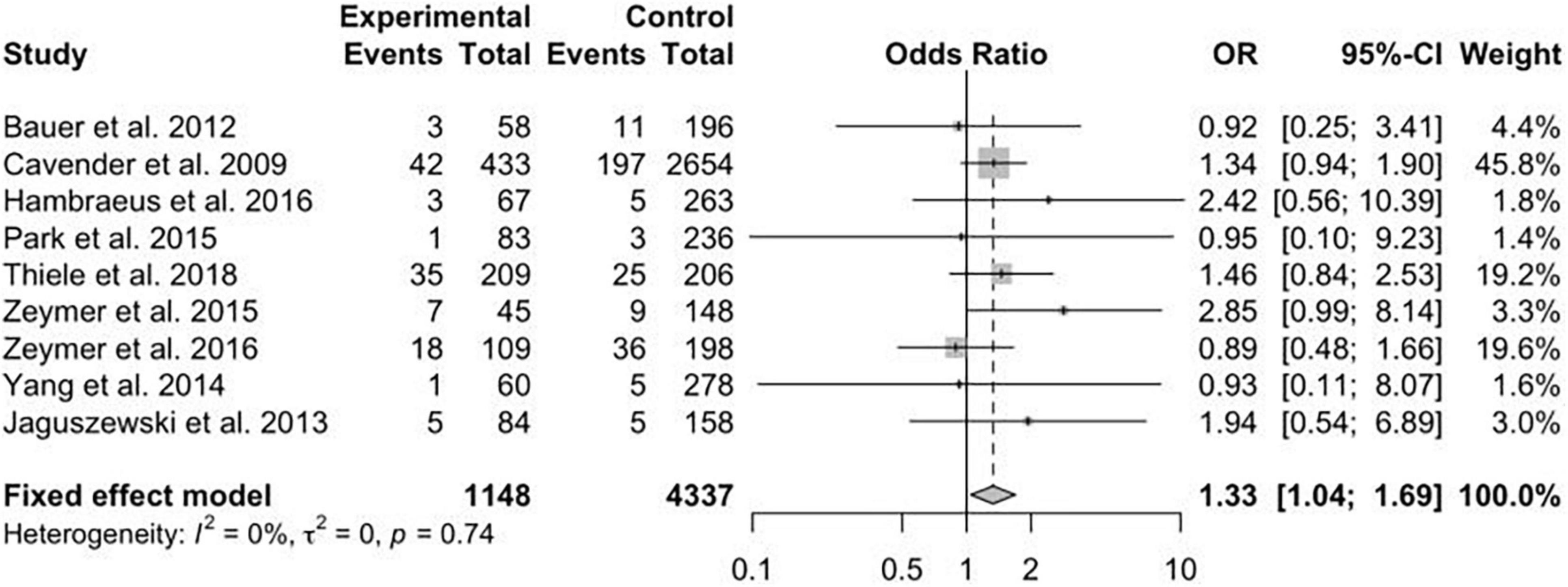
Figure 7. Renal failure with multivessel (MV) vs. culprit vessel-only (CO) percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock (CS).
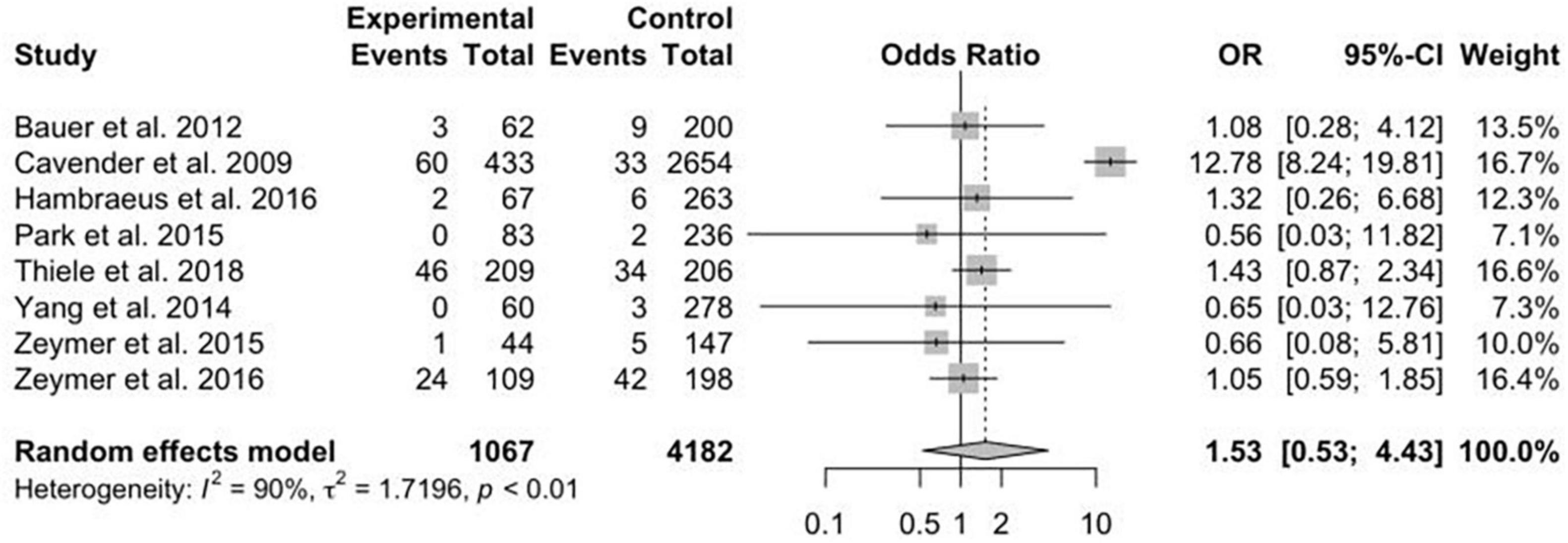
Figure 8. Bleeding with multivessel (MV) vs. culprit vessel-only (CO) percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock (CS).
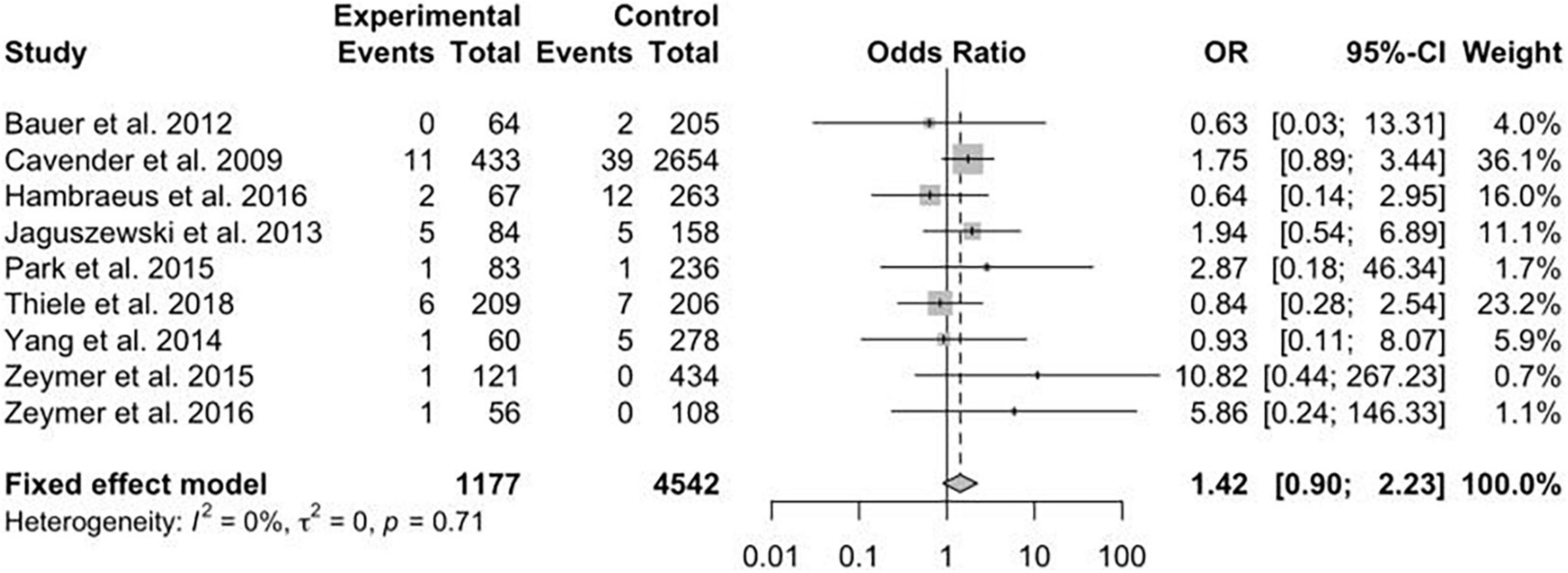
Figure 9. Stroke with multivessel (MV) vs. culprit vessel-only (CO) percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock (CS).
Sensitivity analyses were performed on the safety outcomes of renal failure, bleeding, and stroke to assess the robustness of results. Excluding a single study did not significantly alter the overall results of bleeding and stroke. However, for renal failure, excluding the study of Cavender et al. (14) and Thiele et al. (31) affects the statistical significance of the overall pooled estimates (OR = 1.32; 95% CI, 0.95–1.57 and OR = 1.30; 95% CI, 0.99–1.70; Supplementary Figures 14–16).
Discussion
This meta-analysis including 15 studies has suggested that there is no significant difference in the efficiency outcomes of short/long-term mortality, revascularization, myocardial reinfarction, and safety outcomes of bleeding and stroke in patients with STEMI complicated by CS treated with MV-PCI compared to CO-PCI. Our results were supported by previous meta-analysis (32), which demonstrated that there was no statistical difference of any efficiency or safety outcomes between the two groups, although they focused on patients with AMI with CS. Our study also revealed that MV-PCI could increase the risk of acute renal failure, and this result has been supported by the newly published study (33). However, another meta-analysis (34) indicated that the incidence of MI and revascularization were significantly reduced, but all-cause death was not affected by the revascularization strategy. Previous meta-analyses concerning this topic have reported inconsistent results. The study of Kolte et al. (35) showed that there was no difference in short/long-term outcomes in the two groups, whereas another study (36) reported higher short-term mortality in the MV-PCI treatment group. However, the two studies did not include RCTs data, and the second study included all patients with AMI without separating patients with STEMI and NSTEMI.
At present, it is still a controversial issue about the optimal revascularization strategy in patients with STEMI complicated by CS. Theoretically speaking, MV-PCI of non-culprit arteries may improve survival rate of patients with AMI through limiting infarct size and preserving left ventricular function. However, in our study, immediate MV-PCI did not decrease the short/long-term mortality in patients with STEMI complicated by CS, compared with CO-PCI. The non-statistical difference may be due to the difference of baseline characteristics between the two groups and inability to adjust for patient and operator characteristics, as almost all the included studies were non-randomized. And patients who underwent MV-PCI were sicker and were prone to have adverse outcomes, which could counteract the potential benefit of MV-PCI. Nevertheless, two previous trials reported that there was no difference in all-cause mortality among patients with STEMI without CS between MV-PCI and CO-PCI treatment groups (10, 11). During our search process of study selection, few studies were found to evaluate the efficacy and safety of CO-PCI compared to MV-PCI treatment among patients with AMI. However, these studies focused on different populations [AMI and CS (32, 36–38); AMI, CS, and MVD (39); and STEMI and MVD (40)], thus gave different conclusions and could not provide optimal strategies for patients with STEMI with CS. In addition, the location of culprit lesion may be one of the sources of heterogeneity in mortality. Lee et al. (25) reported that compared with IRA-only PCI group, the all-cause mortality of indicated culprit in the MVP group decreased [left main or left anterior descending (LAD) culprit: hazard ratio (HR) = 0.53 (0.36–0.77); left circumflex artery (LCX) or right coronary artery (RCA) culprit: HR = 0.57 (0.32–1.02)]. However, Jaguszewski et al. (18) found that when left main is the diseased vessel, there was no difference in the in-hospital mortality between single-vessel PCI group and multivessel PCI group. More data from RCTs with large sample are needed to investigate the relationship between the location of culprit lesions and mortality.
Both RCTs and meta-analyses of RCTs have shown that there is a significant reduction in repeat revascularization in patients with STEMI without CS with MV-PCI when compared with CO-PCI (11, 41, 42). This may be because complete revascularization leads to subsequent improved ventricular function and a lower subsequent incidence of heart failure (20, 32). However, no significant difference in reinfarction or repeat revascularization was found in patients with STEMI with CS in the two groups, and this result was also supported by previous meta-analysis, which focused on patients with STEMI with CS (34). There is a fact that 100% of patients who were treated with MV-PCI would undergo additional revascularization of the non-infarct-related arteries upfront, and this may influence the endpoint of repeat revascularization. In patients with STEMI without CS, MV-PCI did not increase the risks of bleeding and stroke (9–11, 41). For patients aged 75 years and older with MI (either STE or NSTE), functionally guided complete revascularization may reduce the occurrence of the composite patient-oriented endpoint of all-cause death, MI, stroke, and ischemia-driven revascularization (42). On the contrary, we found higher rates of renal failure with MV-PCI compared with CO-PCI in patients with STEMI with CS. As reported, presentation with STEMI and CS is associated with 2- to 3-fold higher risk of developing acute kidney injury after PCI (43). In addition, Park et al. (21) found the risk of contrast-induced nephropathy was 9.08 times higher in the MV-PCI group than in the CO-PCI group. This together with the use of higher amounts of contrast during MV-PCI may explain the statistically association between MV-PCI and acute renal failure compared with CO-PCI, but there is a lack of data for analyzing the problem quantitatively.
Finally, some limitations should be acknowledged in this study. First, we only included one RCT study in the meta-analysis, further high-quality RCTs, which decrease the selection bias and unmeasured confounding maximally, are needed to support our results. Second, heterogeneity across studies raise from the different entry criteria, study population, and follow-up time that limit the conclusions’ generalization. Finally, the definition of efficiency and safety outcomes varied among included studies, which could also introduce heterogeneity.
Conclusion
This study suggests that there is no additional benefit in either efficiency outcomes of short/long-term mortality, revascularization, myocardial reinfarction, or safety outcomes of bleeding and stroke in patients with STMEI complicated by CS treated with MV-PCI, compared to CO-PCI. In addition, MV-PCI may increase the risk of acute renal failure. Nonetheless, further RCTs with high quality are needed in the real world to provide optimal revascularization strategy.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
BX and HY provided the idea and wrote this manuscript. YZ, WY, and YH verified the analytical methods. QS encouraged all authors to finish this report. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer YL declared a past collaboration with one of the authors QS to the handling editor.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.735636/full#supplementary-material
References
1. Zeymer U, Hochadel M, Thiele H, Andresen D, Schühlen H, Brachmann J, et al. Immediate multivessel percutaneous coronary intervention versus culprit lesion intervention in patients with acute myocardial infarction complicated by cardiogenic shock: results of the ALKK-PCI registry. Eurointervention. (2015) 11:280–5. doi: 10.4244/EIJY14M08_04
2. Kolte D, Khera S, Aronow WS, Mujib M, Palaniswamy C, Sule S, et al. Trends in incidence, management, and outcomes of cardiogenic shock complicating ST-elevation myocardial infarction in the United States. J Am Heart Assoc. (2014) 3:e000590. doi: 10.1161/JAHA.113.000590
3. Anderson ML, Peterson ED, Peng SA, Wang TY, Ohman EM, Bhatt DL, et al. Differences in the profile, treatment, and prognosis of patients with cardiogenic shock by myocardial infarction classification: a report from NCDR. Circ Cardiovasc Qual Outcomes. (2013) 6:708–15. doi: 10.1161/CIRCOUTCOMES.113.000262
4. Hochman JS, Sleeper LA, Webb JG, Dzavik V, Buller CE, Aylward P, et al. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA. (2006) 295:2511–5. doi: 10.1001/jama.295.21.2511
5. Sanborn TA, Sleeper LA, Webb JG, French JK, Bergman G, Parikh M, et al. Correlates of one-year survival inpatients with cardiogenic shock complicating acute myocardial infarction: angiographic findings from the SHOCK trial. J Am Coll Cardiol. (2003) 42:1373–9. doi: 10.1016/s0735-1097(03)01051-9
6. Wong SC, Sanborn T, Sleeper LA, Webb JG, Pilchik R, Hart D, et al. Angiographic findings and clinical correlates in patients with cardiogenic shock complicating acute myocardial infarction: a report from the SHOCK trial registry. SHould we emergently revascularize occluded coronaries for cardiogenic shocK? J Am Coll Cardiol. (2000) 36:1077–83. doi: 10.1016/s0735-1097(00)00873-1
7. Thiele H, Desch S, Piek JJ, Stepinska J, Oldroyd K, Serpytis P, et al. Multivessel versus culprit lesion only percutaneous revascularization plus potential staged revascularization in patients with acute myocardial infarction complicated by cardiogenic shock: design and rationale of CULPRIT-SHOCK trial. Am Heart J. (2016) 172:160–9. doi: 10.1016/j.ahj.2015.11.006
8. Bhatt DL. Do we really know the CvLPRIT in Myocardial infarction? or just stent all lesions? J Am Coll Cardiol. (2015) 65:973–5. doi: 10.1016/j.jacc.2014.12.037
9. Engstrom T, Kelbaek H, Helqvist S, Hofsten DE, Klovgaard L, Holmvang L, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3-PRIMULTI): an open-label, randomised controlled trial. Lancet. (2015) 386:665–71. doi: 10.1016/s0140-6736(15)60648-1
10. Gershlick AH, Khan JN, Kelly DJ, Greenwood JP, Sasikaran T, Curzen N, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol. (2015) 65:963–72. doi: 10.1016/j.jacc.2014.12.038
11. Wald DS, Morris JK, Wald NJ, Chase AJ, Edwards RJ, Hughes LO, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med. (2013) 369:1115–23. doi: 10.1056/nejmoa1305520
12. O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation. (2013) 127:e362–425.
13. Kolh P, Windecker S, Alfonso F, Collet JP, Cremer J, Falk V, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European society of cardiology (ESC) and the European association for cardio–thoracic surgery (EACTS). Developed with the special contribution of the European association of percutaneous cardiovascular interventions (EAPCI). Eur J Cardio Thorac Surg. (2014) 46:517–92.
14. Cavender MA, Milford-Beland S, Roe MT, Peterson ED, Weintraub WS, Rao SV. Prevalence, predictors, and in-hospital outcomes of non-infarct artery intervention during primary percutaneous coronary intervention for ST-segment elevation myocardial infarction (from the national cardiovascular data registry). Am J Cardiol. (2009) 104:507–13. doi: 10.1016/j.amjcard.2009.04.016
15. Bauer T, Zeymer U, Hochadel M, Möllmann H, Weidinger F, Zahn R, et al. Use and outcomes of multivessel percutaneous coronary intervention in patients with acute myocardial infarction complicated by cardiogenic shock (from the EHS-PCI registry). Am J Cardiol. (2012) 109:941–6. doi: 10.1016/j.amjcard.2011.11.020
16. Cavender MA, Rajeswaran J, DiPaola L, Houghtaling P, Kiernan MS, Rassi AN, et al. Outcomes of culprit versus multivessel PCI in patients with multivessel coronary artery disease presenting with ST-elevation myocardial infarction complicated by shock. J Invasive Cardiol. (2013) 25:218–24.
17. Hambraeus K, Jensevik K, Lagerqvist B, Lindahl B, Carlsson R, Farzaneh-Far R, et al. Long-term outcome of incomplete revascularization after percutaneous coronary intervention in SCAAR (Swedish coronary angiography and angioplasty registry). JACC Cardiovasc Interv. (2016) 9:207–15. doi: 10.1016/j.jcin.2015.10.034
18. Jaguszewski M, Radovanovic D, Nallamothu BK, Lüscher TF, Urban P, Eberli FR, et al. Multivessel versus culprit vessel percutaneous coronary intervention in ST-elevation myocardial infarction: is more worse? Eurointervention. (2013) 9:909–15. doi: 10.4244/EIJV9I8A153
19. Jeger R, Jaguszewski M, Nallamothu BN, Lüscher TF, Urban P, Pedrazzini GB, et al. Acute multivessel revascularization improves 1-year outcome in ST-elevation myocardial infarction: a nationwide study cohort from the AMIS Plus registry. Int J Cardiol. (2014) 172:76–81. doi: 10.1016/j.ijcard.2013.12.083
20. Mylotte D, Morice MC, Eltchaninoff H, Garot J, Louvard Y, Lefèvre T, et al. Primary percutaneous coronary intervention in patients with acute myocardial infarction, resuscitated cardiac arrest, and cardiogenic shock: the role of primary multivessel revascularization. JACC Cardiovasc Interv. (2013) 6:115–25. doi: 10.1016/j.jcin.2012.10.006
21. Park JS, Cha KS, Lee DS, Shin D, Lee HW, Oh JH, et al. Culprit or multivessel revascularisation in ST-elevation myocardial infarction with cardiogenic shock. Heart. (2015) 101:1225–32. doi: 10.1136/heartjnl-2014-307220
22. van der Schaaf RJ, Claessen BE, Vis MM, Hoebers LP, Koch KT, Baan J Jr., et al. Effect of multivessel coronary disease with or without concurrent chronic total occlusion on one-year mortality in patients treated with primary percutaneous coronary intervention for cardiogenic shock. Am J Cardiol. (2010) 105:955–9. doi: 10.1016/j.amjcard.2009.11.014
23. Yang JH, Hahn JY, Song PS, Song YB, Choi SH, Choi JH, et al. Percutaneous coronary intervention for nonculprit vessels in cardiogenic shock complicating ST-segment elevation acute myocardial infarction. Crit Care Med. (2014) 42:17–25. doi: 10.1097/CCM.0b013e3182a2701d
24. Zeymer U, Werdan K, Schuler G, Zahn R, Neumann FJ, Fürnau G, et al. Editor’s choice– impact of immediate multivessel percutaneous coronary intervention versus culprit lesion intervention on 1-year outcome in patients with acute myocardial infarction complicated by cardiogenic shock: results of the randomised IABP-SHOCK II trial. Eur Heart J Acute Cardiovasc Care. (2017) 6:601–9. doi: 10.1177/2048872616668977
25. Lee JM, Rhee TM, Hahn JY, Kim HK, Park J, Hwang D, et al. Multivessel percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction with cardiogenic shock. J Am Coll Cardiol. (2018) 71:844–56.
26. McNeice A, Nadra IJ, Robinson SD, Fretz E, Ding L, Fung A, et al. The prognostic impact of revascularization strategy in acute myocardial infarction and cardiogenic shock: insights from the British Columbia cardiac registry. Catheter Cardiovasc Interv. (2018) 92:E356–67. doi: 10.1002/ccd.27648
27. Bainey KR, Mehta SR, Lai T, Welsh RC. Complete vs culprit-only revascularization for patients with multivessel disease undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review and meta-analysis. Am Heart J. (2014) 167:1–14.e2. doi: 10.1016/j.ahj.2013.09.018
28. Vlaar PJ, Mahmoud KD, Holmes DR Jr, van Valkenhoef G, Hillege HL, van der Horst IC, et al. Culprit vessel only versus multivessel and staged percutaneous coronary intervention for multivessel disease in patients presenting with ST-segment elevation myocardial infarction: a pairwise and network meta-analysis. J Am Coll Cardiol. (2011) 58:692–703. doi: 10.1016/j.jacc.2011.03.046
29. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1.
30. Zhang Y, Cheng J, Li Y, He R, Choudhry AA, Jiang J, et al. Suicidality among patients with asthma: a systematic review and meta-analysis. J Affect Disord. (2019) 256:594–603. doi: 10.1016/j.jad.2019.06.031
31. Thiele H, Akin I, Sandri M, Fuernau G, de Waha S, Meyer-Saraei R, et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. (2017) 377:2419–32.
32. Khan MS, Siddiqi TJ, Usman MS, Riaz H, Khan AR, Murad MH, et al. Meta-analysis comparing culprit vessel only versus multivessel percutaneous coronary intervention in patients with acute myocardial infarction and cardiogenic shock. Am J Cardiol. (2019) 123:218–26. doi: 10.1016/j.amjcard.2018.09.039
33. Thiele H, Akin I, Sandri M, de Waha-Thiele S, Meyer-Saraei R, Fuernau G, et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. (2018) 379:1699–710.
34. Pavasini R, Biscaglia S, Barbato E, Tebaldi M, Dudek D, Escaned J, et al. Complete revascularization reduces cardiovascular death in patients with ST-segment elevation myocardial infarction and multivessel disease: systematic review and meta-analysis of randomized clinical trials. Eur Heart J. (2020) 41:4103–10. doi: 10.1093/eurheartj/ehz896
35. Kolte D, Sardar P, Khera S, Zeymer U, Thiele H, Hochadel M, et al. Culprit vessel-only versus multivessel percutaneous coronary intervention in patients with cardiogenic shock complicating ST-segment-elevation myocardial infarction: a collaborative meta-analysis. Circ Cardiovasc Interv. (2017) 10:e005582. doi: 10.1161/CIRCINTERVENTIONS.117.005582
36. de Waha S, Jobs A, Eitel I, Pöss J, Stiermaier T, Meyer-Saraei R, et al. Multivessel versus culprit lesion only percutaneous coronary intervention in cardiogenic shock complicating acute myocardial infarction: a systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care. (2018) 7:28–37. doi: 10.1177/2048872617719640
37. Kundu A, Sardar P, Kakouros N, Fisher DZ, Malhotra R, Kolte D, et al. Outcomes of multivessel vs culprit lesion-only percutaneous coronary intervention in patients with acute myocardial infarction complicated by cardiogenic shock: evidence from an updated meta-analysis. Catheterv Cardiovasc Interv. (2019) 94:70–81. doi: 10.1002/ccd.28062
38. Khalid MF, Khan AA, Khattak F, Ayub MT, Bagai J, Mukherjee D, et al. Culprit vessel only versus multivessel percutaneous coronary intervention in acute myocardial infarction with cardiogenic shock: a systematic review and meta-analysis. Cardiovasc Revascular Med. (2018) 20:956–64. doi: 10.5005/jp/books/12834_22
39. Tarantini G, D’Amico G, Tellaroli P, Colombo C, Brener SJ. Meta-analysis of the optimal percutaneous revascularization strategy in patients with acute myocardial infarction, cardiogenic shock, and multivessel coronary artery disease. Am J Cardiol. (2017) 119:1525–31. doi: 10.1016/j.amjcard.2017.02.028
40. Zhang D, Song X, Lv S, Yuan F, Xu F, Zhang M, et al. Culprit vessel only versus multivessel percutaneous coronary intervention in patients presenting with ST-segment elevation myocardial infarction and multivessel disease. PLoS One. (2014) 9:e92316. doi: 10.1371/journal.pone.0092316
41. Elgendy IY, Wen X, Mahmoud A, Bavry AA. Complete versus culprit-only revascularization for patients with multi-vessel disease undergoing primary percutaneous coronary intervention: an updated meta-analysis of randomized trials. Catheter Cardiovasc Interv. (2016) 88:501–5. doi: 10.1002/ccd.26322
42. Biscaglia S, Guiducci V, Santarelli A, Amat Santos I, Fernandez-Aviles F, Lanzilotti V, et al. Physiology-guided revascularization versus optimal medical therapy of nonculprit lesions in elderly patients with myocardial infarction: rationale and design of the FIRE trial[J]. Am Heart J. (2020) 229:100–9. doi: 10.1016/j.ahj.2020.08.007
43. Anantha Narayanan M, Reddy YN, Sundaram V, Reddy YN, Baskaran J, Agnihotri K, et al. What is the optimal approach to a non- culprit stenosis after ST-elevation myocardial infarction – conservative therapy or upfront revascularization? An updated meta-analysis of randomized trials. Int J Cardiol. (2016) 216:18–24. doi: 10.1016/j.ijcard.2016.04.054
Keywords: myocardial infarction, cardiogenic shock, percutaneous coronary intervention, meta-analysis, clinical outcomes
Citation: Xiong B, Yang H, Yu W, Zeng Y, Han Y and She Q (2022) Multivessel vs. Culprit Vessel-Only Percutaneous Coronary Intervention for ST-Segment Elevation Myocardial Infarction in Patients With Cardiogenic Shock: An Updated Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 9:735636. doi: 10.3389/fcvm.2022.735636
Received: 03 July 2021; Accepted: 28 February 2022;
Published: 15 April 2022.
Edited by:
Joo Myung Lee, Sungkyunkwan University School of Medicine, South KoreaReviewed by:
Gianluca Campo, University Hospital of Ferrara, ItalyYingrui Li, University of Heidelberg, Germany
Copyright © 2022 Xiong, Yang, Yu, Zeng, Han and She. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiang She, cXNoZTk4QGNxbXUuZWR1LmNu
 Bingquan Xiong
Bingquan Xiong Huiping Yang
Huiping Yang Yue Han
Yue Han Qiang She
Qiang She