- 1School of Physical Education, Jinan University, Guangzhou, China
- 2Institute for Healthcare Artificial Intelligence Application, Guangdong Second Provincial General Hospital, Guangzhou, China
- 3Faculty of Data Science, City University of Macau, Macao, Macao SAR, China
- 4Guangzhou Sport University, Guangzhou, China
- 5Guangdong Women and Children Hospital, Guangzhou, China
- 6Division of Physical Education, Guangdong University of Finance and Economics, Guangzhou, China
- 7School of Education, City University of Macau, Macao, Macao SAR, China
- 8School of Data Science, City University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 9Department of Industrial Engineering and Management, School of Mechanical Engineering, Shanghai Jiao Tong University, Shanghai, China
- 10Syns Institute of Educational Research, Hong Kong, Hong Kong SAR, China
- 11School of Public Health, Sun Yat-Sen University, Guangzhou, China
- 12Department of Health Medicine, Guangdong Second Provincial General Hospital, Guangzhou, China
- 13UNC Project-China, UNC Global, School of Medicine, The University of North Carolina, Chapel Hill, NC, United States
- 14Zhuhai College of Science and Technology, Zhuhai, China
- 15ZCST Health and Medicine Industry Research Institute, Zhuhai, China
Background: Cardiovascular disease (CVD) and cancer are the first and second causes of death in over 130 countries across the world. They are also among the top three causes in almost 180 countries worldwide. Cardiovascular complications are often noticed in cancer patients, with nearly 20% exhibiting cardiovascular comorbidities. Physical exercise may be helpful for cancer survivors and people living with cancer (PLWC), as it prevents relapses, CVD, and cardiotoxicity. Therefore, it is beneficial to recommend exercise as part of cardio-oncology preventive care.
Objective: With the progress of deep learning algorithms and the improvement of big data processing techniques, artificial intelligence (AI) has gradually become popular in the fields of medicine and healthcare. In the context of the shortage of medical resources in China, it is of great significance to adopt AI and machine learning methods for prescription recommendations. This study aims to develop an interpretable machine learning-based intelligent system of exercise prescription for cardio-oncology preventive care, and this paper presents the study protocol.
Methods: This will be a retrospective machine learning modeling cohort study with interventional methods (i.e., exercise prescription). We will recruit PLWC participants at baseline (from 1 January 2025 to 31 December 2026) and follow up over several years (from 1 January 2027 to 31 December 2028). Specifically, participants will be eligible if they are (1) PLWC in Stage I or cancer survivors from Stage I; (2) aged between 18 and 55 years; (3) interested in physical exercise for rehabilitation; (4) willing to wear smart sensors/watches; (5) assessed by doctors as suitable for exercise interventions. At baseline, clinical exercise physiologist certificated by the joint training program (from 1 January 2023 to 31 December 2024) of American College of Sports Medicine and Chinese Association of Sports Medicine will recommend exercise prescription to each participant. During the follow-up, effective exercise prescription will be determined by assessing the CVD status of the participants.
Expected outcomes: This study aims to develop not only an interpretable machine learning model to recommend exercise prescription but also an intelligent system of exercise prescription for precision cardio-oncology preventive care.
Ethics: This study is approved by Human Experimental Ethics Inspection of Guangzhou Sport University.
Clinical trial registration: http://www.chictr.org.cn, identifier ChiCTR2300077887.
1 Introduction
Globally, cardiovascular disease (CVD) ranks as the first leading cause of death, while cancer ranks as the second in around 130 countries (1). These two factors are also among the top three killers in almost 180 countries worldwide (2). People living with cancer (PLWC) usually exhibit cardiovascular complications resulting from so-called “cardio-toxicity” (3) (which is defined as any heart damage arising from cancer treatments) as well as the overlap of risk factors of cancer and CVD, including an unbalanced fat diet, alcohol abuse, and physical inactivity (4).
Interventions using some common prevention strategies for these risk factors exist. For example, regularly engaging in physical activity (i.e., exercise prescription) is an efficient prevention strategy for cardio-oncology (5) because physical exercise can reduce not only cardio-toxicity but also the adverse effects of chemotherapy, including lymphoedema, fatigue, and immunological disorders (6). As a result, among PLWC or cancer survivors, physical exercise is a valuable tool for CVD prevention. Therefore, it is beneficial to recommend exercise prescription in cardio-oncology preventive care (5).
Artificial Intelligence (AI) has been widely employed in healthcare and medicine, especially since great advancements in deep learning algorithms and significant improvements to big data processing techniques (7). The fields of mental health (8), internal medicine (9), infectious diseases control (10), heart failure (11, 12), and diabetes (13), among others employ AI. In the context of the shortage of medical resources in China, developing prescription recommendation systems using AI and machine learning methods is promising (14). Wang et al. have proposed a reinforcement learning-based dynamic prescription recommendation system (15).
As for a dynamic recommendation system of exercise prescription, Tuka and Linhart discussed the possibility of utilizing AI and machine learning approaches for personalized exercise prescription recommendations for patients (16). More specifically, Chen et al. presented a hierarchical learning framework for Chinese kids’ physical exercise prescription (17). However, there is no existing studies have examined machine learning-based exercise prescription recommendations for cardio-oncology preventive care. Therefore, we aim to develop an interpretable machine learning-based intelligent system of exercise prescription for cardio-oncology preventive care and present the study protocol.
2 Methods and analysis
2.1 Design
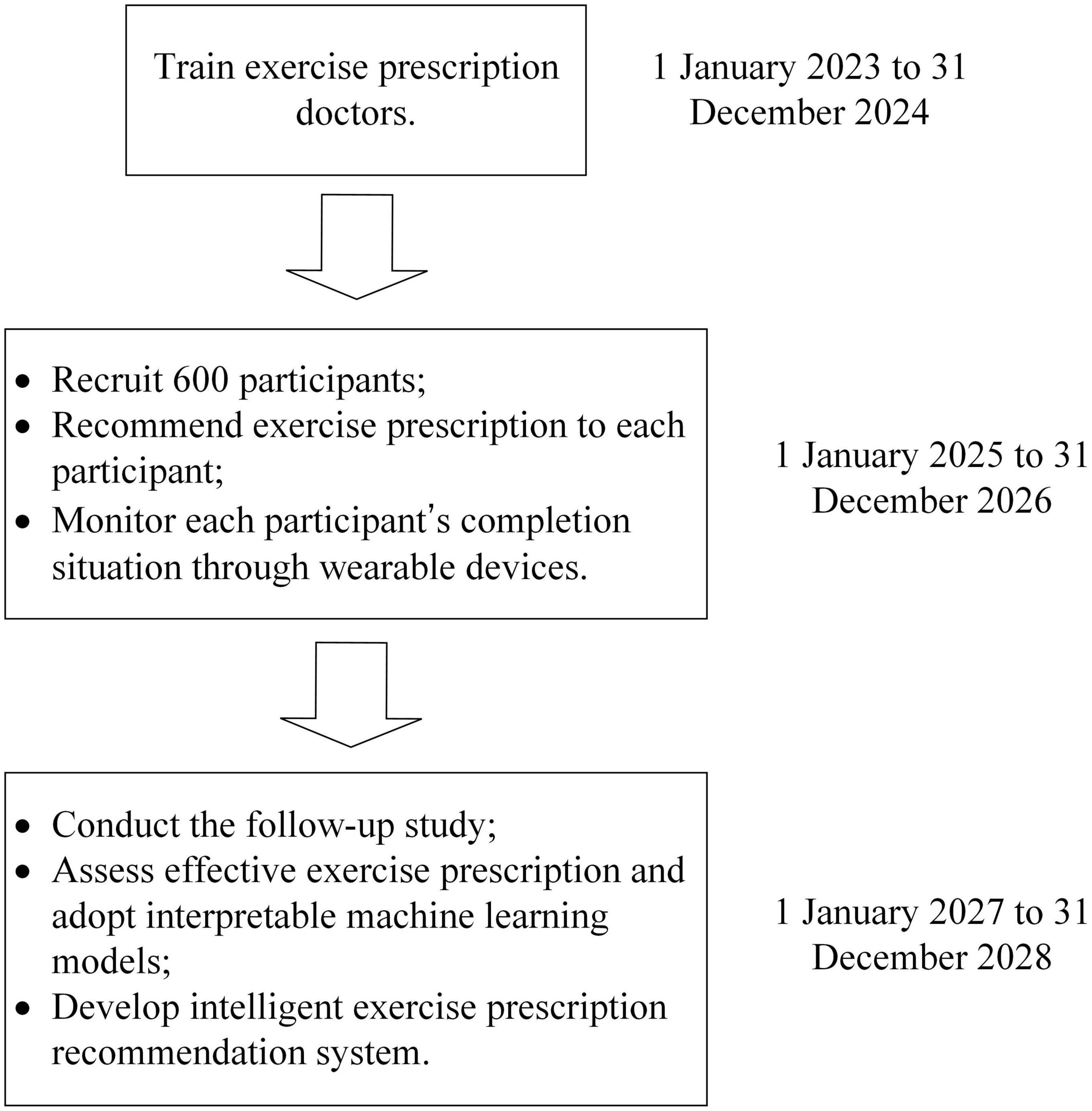
This will be a cohort study with retrospective machine learning modeling. The study timeline is presented in Figure 1.
From 1 January 2023 to 31 December 2024, we will train our exercise prescription doctors in the training program for clinical exercise physiologist (CEP). This training program is jointly supported by American College of Sports Medicine (ACSM) and Chinese Association of Sports Medicine (CASM). Candidates who are admitted to this training program should either hold a bachelor’s degree (or above) in medicine/public health or have at least 3-year professional clinical experience in healthcare. Additionally, candidates are supposed to have a vast knowledge of physical education and sports training as well. In this training program, candidates need to complete reading materials, online courses, offline tutorials, practice, and examinations. The offline training activities will take place at Zhuhai, China, where a certificated training base of ACSM-CASM CEP programs locates on. After completion of all modules, our exercise prescription doctors will be certificated jointly by ACSM and CASM as CEP. From 1 January 2025 to 31 December 2026, we will recruit 600 participants who are PLWC (in Stage I) or cancer survivors (from Stage I) for this study. The baseline characteristics including demographics, cancer-related information, exercise habits and lifestyle, health-related physical fitness, and CVD-related items will be collected based on physical examination or biomedical testing, where necessary. Then the exercise prescription doctors certificated by ACSM-CASM will recommend exercise prescription to each participant based on the abovementioned variables. During the 2-year exercise intervention period, we will monitor each participant’s completion status through wearable devices, which can record one’s physical activity every day. Additionally, our health management team will keep track of participants every week to ensure their adherence. We will undertake the follow-up study between 1 January 2027 and 31 December 2028, re-examining CVD-related items for all participants. Finally, effective exercise prescription will be assessed based on the changes in CVD-related items from the baseline to the follow-up, and interpretable machine learning models will be adopted in effective exercise prescription. The intelligent exercise prescription recommendation system will be developed based on some machine learning models with both good interpretability and high performance.
2.2 Selection of subjects
This protocol involving human participants was reviewed and approved by the Ethics Committee of Guangzhou Sport University. The participants will be provided with their written informed consent to participate in this study.
2.2.1 Inclusion criteria
Participants will be eligible if they are (1) PLWC in Stage I or cancer survivors from Stage I; (2) aged between 18 and 55 years; (3) interested in physical exercise for rehabilitation; (4) willing to wear smart sensors/watches; (5) assessed by doctors as suitable for exercise interventions.
2.2.2 Exclusion criteria
Participants will be ineligible for inclusion if they have: (1) current or recent serious sports injuries; or (2) existing severe CVD; or (3) other conditions that may not be suitable for exercise interventions, as assessed by doctors.
2.3 The sample size
We will recruit 600 participants for this study. Generally, the minimum sample size for machine learning modeling is 200 (18). We estimate the loss rate in the follow-up is 47% according to a finding that 53% cancer survivors do not follow the recommended physical activity guidelines (19). We infer that 65% of exercise prescriptions will be assessed as effective for cardio-oncology preventive care after the follow-up and used for machine learning modeling. This assumed value is based on the effectiveness rate of exercise prescriptions in reducing the risk of cardiovascular events among cancer patients (20). Therefore, at least 200÷65%÷53%=580.55 participants are needed. As a result, we decide to recruit 600 participants in the baseline to ensure the guarantee the minimum sample size for machine learning modeling at last.
2.4 The baseline and follow-up
In the baseline and the follow-up, five aspects of characteristics/variables will be collected: demographics, cancer-related information, exercise habits and lifestyle, health-related physical fitness (21), and CVD-related items. Table 1 illustrates these variables in detail.
Specifically, demographics, cancer-related information, exercise habits and lifestyle, and health-related physical fitness are used for exercise prescriptions, while CVD-related items are used to evaluate the effectiveness of exercise prescriptions after comparing them with the follow-up data.
2.5 Interventional methods
The interventional method for all participants is the exercise prescription, prescribed by our ACSM-CASM certificated exercise prescription doctors. The exercise intervention strategies are prescribed based on each participant’s baseline characteristics including demographics, cancer-related information, exercise habits and lifestyle, and health-related physical fitness.
From the professional perspective, exercise prescription doctors will determine the exercise dose considering three aspects: frequency, duration, and intensity (26). To be specific, doctors prescribe an exercise dose such as “3 times of exercise per week, 150 minutes in total, in moderate intensity” or “5 times of exercise per week, 75 minutes for each time, in high-intensity.” Frequency is the number of times of exercise per week, duration is the length of time in total, and intensity is decided to be high, moderate, or low. Furthermore, we can employ the concept of metabolic equivalent of task (MET) in exercise dose when considering frequency, duration, and intensity (54). For example, the above-mentioned two exercise doses are equivalent to each other, and both represent 7.5 MET-h/week.
During the 2-year exercise intervention period, wearable devices will be applied to monitor each participant’s completion status. In addition, our professional health management team (including certificated CEPs by ACSM-CASM programs and several assistants who hold a degree in public health, sports training, physical education, social work or psychology) will keep track of participants every week to ensure their adherence. The employment of wearable devices will be charged a deposit fee at the beginning which will be returned after the follow-up. Participants who are kept in track by our health management team during these 2 years will be given sports equipment (e.g., badminton rackets, yoga mats, foam rollers) for free every 6 months.
2.6 Data analysis and interpretable learning
Effective exercise prescriptions will be selected based on pre- and post-intervention data analysis of CVD-related items. For example, if the blood pressure variability decreases or at least does not increase, the exercise prescription can be considered effective. We will employ interpretable machine learning models to the learnings on exercise prescription recommendations for all effective prescriptions.
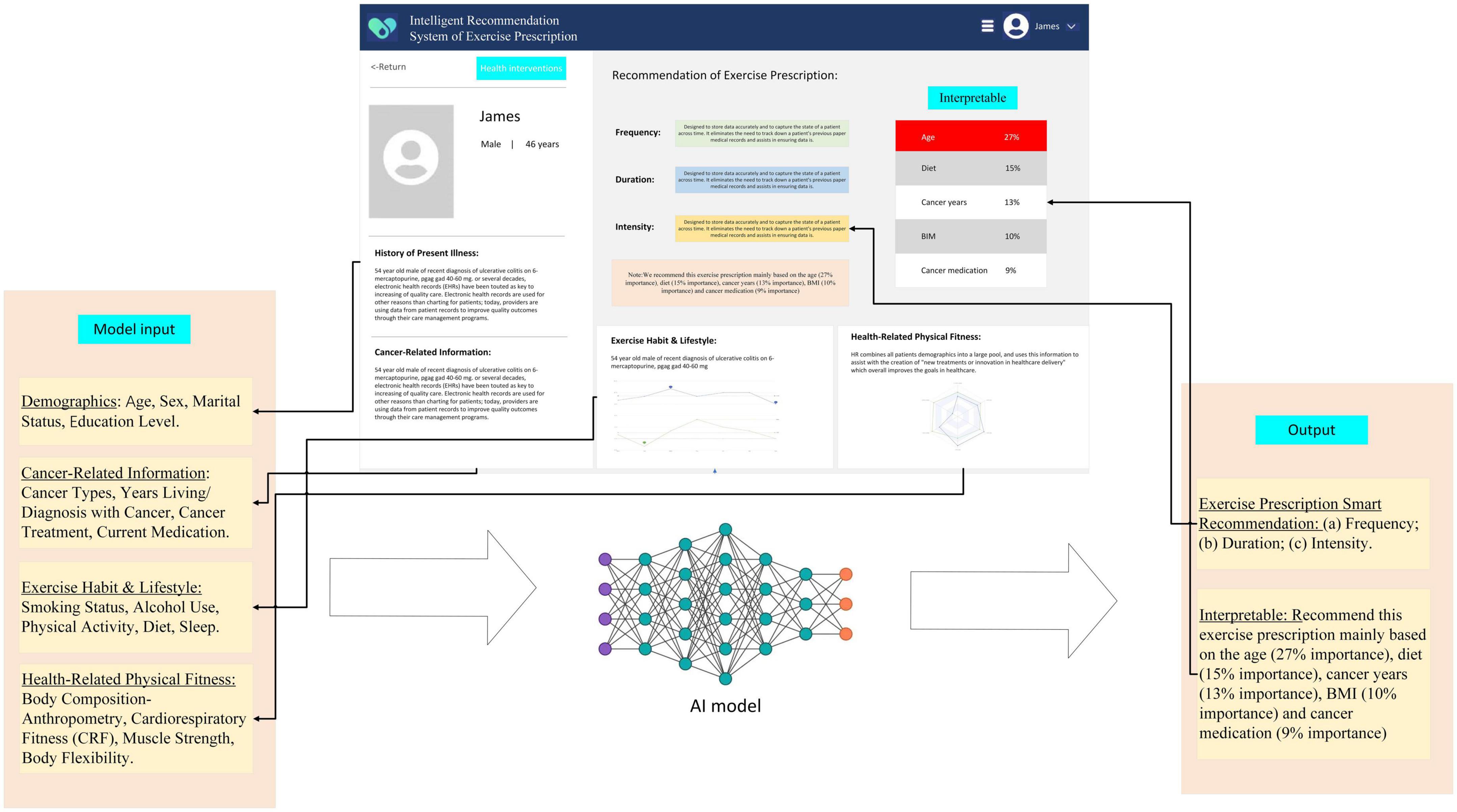
Demographics, cancer-related information, exercise habits and lifestyle, health-related physical fitness will be input variables, while frequency, duration, and intensity of exercise prescription will be output variables. We formulate the prescription learning process as a machine learning classification task. Explainable machine learning models such as logistics regression, support vector machine, decision tree, random forest, k-nearest neighbor, and naive Bayes classifiers will be utilized. Specifically, in the logistics regression machine learning model, the estimated values of coefficients and their standard deviations, P-values, and 95% confidence intervals, will provide us with the interpretability. The process of feature selection and kernels when using support vector machine may reveal the model interpretability (55). Figure presentation of trees and importance ranking of features for decision tree and random forest can lead to good explanations (56). In k-nearest neighbor algorithm, showing the k-nearest neighbors might also be explainable (57). As for Naive Bayes, it can be interpreted on the modular level and the conditional probability, then thus it will be very clear for us to understand how much each feature contributes toward a certain class prediction (58). Generally, these machine learning models may all have good potential for interpretability.
Some deep learning models will also be employed to evaluate the classification performance (accuracy, precision, recall, F-1 score, area under curve) in fivefold cross-validations, comparing them with the above-mentioned explainable machine learning models. Explanations of deep neural networks can be challenging (59), and hence to ensure that our deep learning models (convolutional neural networks, eXtreme gradient boosting, multilayer perceptron, deep residual network, DeepGBM) are more interpretable, an explainability tool named SHapley Additive exPlanations (SHAP), (60) will also be included. Recent advances in interpretability study for deep learning models have demonstrated the explainable potential for such models utilizing SHAP. For example, Zhao et al. proposed a novel SHAP scores computing algorithm for convolutional neural networks in classification (61). Meng et al. developed an integrated framework with better interpretability based on SHAP and eXtreme gradient boosting (62).
Since the intervention duration will be 2 years, there might be a great chance of loss-to-follow-up. Therefore, we set our sample size as 600 instead of 580, to cope with a higher loss rate or lower effectiveness rate than our initial estimations. If the final sample size for machine learning modeling still fails to reach the minimum bound (18), we will employ some few-shot learning algorithms (63) in such small size machine learning task to deal with this potential problem.
2.7 Intelligent system development
Considering both the model performance and the model interpretability, the intelligent exercise prescription recommendation system will be developed based on some machine learning models with both good interpretability and high performance. Figure 2 depicts an example of this intelligent system. It is noteworthy that our designed intelligent system will explain why it recommends specific exercise prescriptions.
3 Discussion
All cancer patients need to consider a multidisciplinary approach during treatment, which includes physical training, psychological support, and lifestyle advice (26). The concept of cardio-oncology rehabilitation has been introduced by both the American Heart Association and the American Cancer Society (64). Cardio-oncology rehabilitation is to identify PLWC who are at high risk for cardiac dysfunction as well. Physical activity intervention, that is exercise prescription, is an important component of cardio-oncology rehabilitation and can prevent or moderate cardiovascular events in cancer patients or survivors. It has been demonstrated that heterogeneous responses to the same physical training can enhance cardio-respiratory fitness in cancer therapy (65). There is some theoretical and experimental evidence as to why physical exercise can help reduce cardiovascular events in cancer patients or survivors. For example, the so-called “cancer-induced cardiac cachexia,” which refers to a multi-organ/tissue syndrome affecting the brain, liver, and heart, can exist in cancer patients because of the tumor environment (66). Previous studies have revealed that physical exercise can restore muscle strength and improve endurance, thus counteracting cardiac cachexia (67). Exercise prescription can act as an aid and therapy for cardio-oncology preventive care. Therefore, our study on interpretable machine learning of exercise prescription for cardio-oncology prevention is of significance.
Some limitations of our study need to be mentioned. First, only PLWC in cancer Stage I or cancer survivors from cancer Stage I are taken into account. Although considering more participants (e.g., expansion to Stage II or Stage III) may improve our approach’s coverage, we decide to focus on participants with milder intensities of cancer. Second, there is always a trade-off between model interpretability and model performance. Black-box deep learning models may outperform explainable machine learning models in evaluation metrics such as accuracy and area under curve (AUC). Therefore, we plan to adopt both in this study and select a balanced one for intelligent system development. Third, we will only employ internal cross-validation methods in training and testing as an initial validation choice. To fill in this gap, after the interpretable machine learning-based intelligent system of exercise prescription has been developed and used in real case for a period, we will then conduct a quasi-experimental trial for external validation in another study, just like other machine learning-based medical studies did for external validation (68–70). Furthermore, with external validation and more dataset in the future, we can continuously update the intelligent system of exercise prescription through dynamic optimization of parameters of the interpretable machine learning model.
In conclusion, physical exercise is a promising interventional strategy for cancer patients or survivors during and after medical treatment and may also be effective in counteracting some adverse effects of the tumor environment or drugs on their cardiovascular system. When prescribing exercise, we need to take the cancer patients’ or survivors’ individual characteristics, cancer drugs/medications, personal lifestyle history, and health-related physical fitness into consideration. Such a tailored exercise prescription process can be learned by interpretable models using machine learning approaches and can generate an intelligent recommendation system of exercise prescription for cardio-oncology preventive care in the future.
Ethics statement
The protocol has received approval from the Ethics Inspection of the Ethical Review Board of Guangzhou Sport University (Ethics Approval ID: 20232022-41). The patients/participants provided their written informed consent to participate in this study.
Author contributions
TG, HR, FJ, and XT conceived the study and drafted the manuscript. FJ and XT were involved in the study design and methodology. WMC and WBC supervised the study. SH, DL, YX, KC, YW, YZ, HD, ZX, WMC, and WBC provided the insightful ideas and critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Fundamental Research Funds for the Central Universities [21JNQN14], by Doctoral Workstation Foundation of Guangdong Second Provincial General Hospital [2023BSGZ014], and by Guangzhou Science and Technology Project [SL2022A04J01130]. The APC Fee was supported by the Health and Medicine Industry Research Institute, Zhuhai College of Science and Technology.
Acknowledgments
We acknowledge the guest editor and reviewers. We thank the professional editing institution for the proofreading service from native speakers which is recommended by Frontiers.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bray F, Laversanne M, Cao B, Varghese C, Mikkelsen B, Weiderpass E, et al. Comparing cancer and cardiovascular disease trends in 20 middle-or high-income countries 2000–19: a pointer to national trajectories towards achieving Sustainable Development goal target 3.4. Cancer Treat Rev. (2021) 100:102290. doi: 10.1016/j.ctrv.2021.102290
2. Bray F, Laversanne M, Weiderpass E, Soerjomataram I. The ever-increasing importance of cancer as a leading cause of premature death worldwide. Cancer. (2021) 127:3029–30. doi: 10.1002/cncr.33587
3. Dong M, Yu T, Zhang Z, Zhang J, Wang R, Tse G, et al. ICIs-related cardiotoxicity in different types of cancer. J Cardiovasc Dev Dis. (2022) 9:203. doi: 10.3390/jcdd9070203
4. Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation. (2016) 133:1104–14. doi: 10.1161/CIRCULATIONAHA.115.020406
5. Wang HL, Cousin L, Fradley MG, Donovan KA, Smith B, Szalacha L, et al. Exercise Interventions in cardio-oncology populations: a scoping review of the literature. J Cardiovasc Nurs. (2021) 36:385–404. doi: 10.1097/JCN.0000000000000664
6. Schmielau J, Rick O, Reuss-Borst M, Kalusche-Bontemps EM, Steimann M. Rehabilitation of cancer survivors with long-term toxicities. Oncol Res Treat. (2017) 40:764–71. doi: 10.1159/000485187
7. Rajpurkar P, Chen E, Banerjee O, Topol EJ. AI in health and medicine. Nat Med. (2022) 28:31–8. doi: 10.1038/s41591-021-01614-0
8. Xu Z, Zhang Q, Li W, Li M, Yip PSF. Individualized prediction of depressive disorder in the elderly: a multitask deep learning approach. Int J Med Inform. (2019) 132:103973. doi: 10.1016/j.ijmedinf.2019.103973
9. Xu Z, Cheng W, Li Z, Tse G, Jing F, Lian W, et al. Mass screening for low bone density using basic check-up items. IEEE Transactions on Computational Social Systems. Manhattan, NJ: IEEE (2022). p. 1–8. doi: 10.1109/TCSS.2022.3176652
10. Jing F, Ye Y, Zhou Y, Ni Y, Yan X, Lu Y, et al. Identification of key influencers for secondary distribution of HIV self-testing among Chinese MSM: a machine learning approach. Medrxiv [preprint]. (2021): doi: 10.1101/2021.04.19.21255584
11. Tse G, Zhou J, Woo SWD, Ko CH, Lai RWC, Liu T, et al. Multi-modality machine learning approach for risk stratification in heart failure with left ventricular ejection fraction ≤ 45%. ESC Heart Fail. (2020) 7:3716–25. doi: 10.1002/ehf2.12929
12. Ren H, Sun Y, Xu C, Fang M, Xu Z, Jing F, et al. Predicting acute onset of heart failure complicating acute coronary syndrome: an explainable machine learning approach. Curr Probl Cardiol. (2022) 48:101480. doi: 10.1016/j.cpcardiol.2022.101480
13. Zhou J, Liu X, Chou OH, Li L, Lee S, Wong WT, et al. Lower risk of gout in sodium glucose cotransporter 2 (SGLT2) inhibitors versus dipeptidyl peptidase-4 (DPP4) inhibitors in type-2 diabetes. Rheumatology (Oxford). (2022):keac509. [Epub ahead of print]. doi: 10.1093/rheumatology/keac509
14. Liu C, Liu X, Wu F, Xie M, Feng Y, Hu C. Using artificial intelligence (Watson for Oncology) for treatment recommendations amongst Chinese patients with lung cancer: feasibility study. J Med Internet Res. (2018) 20:e11087. doi: 10.2196/11087
15. Wang L, Zhang W, He X, Zha H. Supervised reinforcement learning with recurrent neural network for dynamic treatment recommendation. Proceedings of the 24th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining. New York, NY: ACM (2018). p. 2447–56. doi: 10.1145/3219819.3219961
16. Tuka V, Linhart A. Personalised exercise prescription: finding the best for our patients. Eur J Prevent Cardiol. (2020) 27:1366–8. doi: 10.1177/2047487319884376
17. Chen G, Song G, Wu Q. A hierarchical learning framework for Chinese kids physical exercise prescription. Proceeding of the 2017 International Conference on Machine Learning and Cybernetics (ICMLC). Vol. 1. Manhattan, NJ: IEEE (2017). p. 279–84. doi: 10.1109/ICMLC.2017.8107777
18. Cui Z, Gong G. The effect of machine learning regression algorithms and sample size on individualized behavioral prediction with functional connectivity features. Neuroimage. (2018) 178:622–37. doi: 10.1016/j.neuroimage.2018.06.001
19. Blanchard CM, Courneya KS, Stein K. Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. J Clin Oncol. (2008) 26:2198–204. doi: 10.1200/JCO.2007.14.6217
20. Palomo A, Ray RM, Johnson L, Paskett E, Caan B, Jones L, et al. Associations between exercise prior to and around the time of cancer diagnosis and subsequent cardiovascular events in women with breast cancer: a Women’s Health Initiative (WHI) analysis. J Am Coll Cardiol. (2017) 69:1774–1774. doi: 10.1016/S0735-1097(17)35163-X
21. Liguori G, American College of Sports Medicine [ACSM]. ACSM’s Guidelines for Exercise Testing and Prescription. Philadelphia, PA: Lippincott Williams & Wilkins (2020).
22. Ingram DK. Age-related decline in physical activity: generalization to nonhumans. Med Sci Sports Exerc. (2000) 32:1623–9. doi: 10.1097/00005768-200009000-00016
23. Parker BA, Kalasky MJ, Proctor DN. Evidence for sex differences in cardiovascular aging and adaptive responses to physical activity. Eur J Appl Physiol. (2010) 110:235–46. doi: 10.1007/s00421-010-1506-7
24. Pettee KK, Brach JS, Kriska AM, Boudreau R, Richardson CR, Colbert LH, et al. Influence of marital status on physical activity levels among older adults. Med Sci Sports Exerc. (2006) 38:541–6. doi: 10.1249/01.mss.0000191346.95244.f7
25. Shaw BA, Spokane LS. Examining the association between education level and physical activity changes during early old age. J Aging Health. (2008) 20:767–87. doi: 10.1177/0898264308321081
26. D’Ascenzi F, Anselmi F, Fiorentini C, Mannucci R, Bonifazi M, Mondillo S. The benefits of exercise in cancer patients and the criteria for exercise prescription in cardio-oncology. Eur J Prevent Cardiol. (2021) 28:725–35. doi: 10.1177/2047487319874900
27. Luan X, Tian X, Zhang H, Huang R, Li N, Chen P, et al. Exercise as a prescription for patients with various diseases. J Sport Health Sci. (2019) 8:422–41. doi: 10.1016/j.jshs.2019.04.002
28. Codima A, das Neves Silva W, de Souza Borges AP, de Castro G. Exercise prescription for symptoms and quality of life improvements in lung cancer patients: a systematic review. Support Care Cancer. (2021) 29:445–57. doi: 10.1007/s00520-020-05499-6
29. Kirkham AA, Bonsignore A, Bland KA, McKenzie DC, Gelmon KA, Van Patten CL, et al. Exercise prescription and adherence for breast cancer: one size does not FITT all. Med Sci Sports Exerc. (2018) 50:177–86. doi: 10.1249/MSS.0000000000001446
30. Hayes SC, Spence RR, Galvão DA, Newton RU. Australian association for exercise and sport science position stand: optimising cancer outcomes through exercise. J Sci Med Sport. (2009) 12:428–34. doi: 10.1016/j.jsams.2009.03.002
31. Sweegers MG, Altenburg TM, Chinapaw MJ, Kalter J, Verdonck-de Leeuw IM, Courneya KS, et al. Which exercise prescriptions improve quality of life and physical function in patients with cancer during and following treatment? A systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. (2018) 52:505–13. doi: 10.1136/bjsports-2017-097891
32. Kaczynski AT, Manske SR, Mannell RC, Grewal K. Smoking and physical activity: a systematic review. Am J Health Behav. (2008) 32:93–110. doi: 10.5993/AJHB.32.1.9
33. Dodge T, Clarke P, Dwan R. The relationship between physical activity and alcohol use among adults in the United States: a systematic review of the literature. Am J Health Promot. (2017) 31:97–108. doi: 10.1177/0890117116664710
34. Van Holle V, De Bourdeaudhuij I, Deforche B, Van Cauwenberg J, Van Dyck D. Assessment of physical activity in older Belgian adults: validity and reliability of an adapted interview version of the long International Physical Activity Questionnaire (IPAQ-L). BMC Public Health. (2015) 15:433. doi: 10.1186/s12889-015-1785-3
35. Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act. (2012) 9:1–30. doi: 10.1186/1479-5868-9-78
36. Millen AE, Midthune D, Thompson FE, Kipnis V, Subar AF. The National Cancer Institute diet history questionnaire: validation of pyramid food servings. Am J Epidemiol. (2006) 163:279–88. doi: 10.1093/aje/kwj031
37. World Health Organization [WHO]. Global Strategy on Diet, Physical Activity and Health. Geneva: World Health Organization (2004).
38. Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
39. Semplonius T, Willoughby T. Long-term links between physical activity and sleep quality. Med Sci Sports Exerc. (2018) 50:2418–24. doi: 10.1249/MSS.0000000000001706
40. Antonio J, Kenyon M, Ellerbroek A, Carson C, Burgess V, Tyler-Palmer D, et al. Comparison of Dual-Energy X-Ray Absorptiometry (DXA) versus a Multi-frequency Bioelectrical Impedance (InBody 770) device for body composition assessment after a 4-week hypoenergetic diet. J Funct Morphol Kinesiol. (2019) 4:23. doi: 10.3390/jfmk4020023
41. Brodie D, Moscrip V, Hutcheon R. Body composition measurement: a review of hydrodensitometry, anthropometry, and impedance methods. Nutrition. (1998) 14:296–310. doi: 10.1016/S0899-9007(97)00474-7
42. Bandyopadhyay A. Validity of Cooper’s 12-minute run test for estimation of maximum oxygen uptake in male university students. Biol Sport. (2015) 32:59–63. doi: 10.5604/20831862.1127283
43. Grant S, Corbett K, Amjad AM, Wilson J, Aitchison T. A comparison of methods of predicting maximum oxygen uptake. Br J Sports Med. (1995) 29:147–52. doi: 10.1136/bjsm.29.3.147
44. Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. (2011) 40:423–9. doi: 10.1093/ageing/afr051
45. Jaric S. Muscle strength testing. Sports Med. (2002) 32:615–31. doi: 10.2165/00007256-200232100-00002
46. Baltaci G, Un N, Tunay V, Besler A, Gerçeker S. Comparison of three different sit and reach tests for measurement of hamstring flexibility in female university students. Br J Sports Med. (2003) 37:59–61. doi: 10.1136/bjsm.37.1.59
47. Horsfall I, Champion SM, Watson CH. The development of a quantitative flexibility test for body armour and comparison with wearer trials. Appl Ergon. (2005) 36:283–92. doi: 10.1016/j.apergo.2005.01.005
48. Arroll B, Beaglehole R. Does physical activity lower blood pressure: a critical review of the clinical trials. J Clin Epidemiol. (1992) 45:439–47. doi: 10.1016/0895-4356(92)90093-3
49. Xu X, Meng X, Oka SI. Long-term habitual vigorous physical activity is associated with lower visit-to-visit systolic blood pressure variability: insights from the SPRINT trial. Am J Hypertens. (2021) 34:463–6. doi: 10.1093/ajh/hpaa198
50. Jensen MT, Suadicani P, Hein HO, Gyntelberg F. Elevated resting heart rate, physical fitness and all-cause mortality: a 16-year follow-up in the Copenhagen Male Study. Heart. (2013) 99:882–7. doi: 10.1136/heartjnl-2012-303375
51. Hein H, Panhuyzen-Goedkoop N, Corrado D, Hoffmann E, Biffi A, Delise P, et al. Recommendations for participation in leisure-time physical activity and competitive sports in patients with arrhythmias and potentially arrhythmogenic conditions Part I: supraventricular arrhythmias and pacemakers. Eur J Prevent Cardiol. (2006) 13:475–84. doi: 10.1097/01.hjr.0000216543.54066.72
52. Upshaw JN, Hubbard RA, Hu J, Brown JC, Smith AM, Demissei B, et al. Physical activity during and after breast cancer therapy and associations of baseline physical activity with changes in cardiac function by echocardiography. Cancer Med. (2020) 9:6122–31. doi: 10.1002/cam4.3277
53. Hosseini SRA, Hejazi K. The effects of Ramadan fasting and physical activity on blood hematological-biochemical parameters. Iranian J Basic Med Sci. (2013) 16:845.
54. Mendes MDA, Da Silva I, Ramires V, Reichert F, Martins R, Ferreira R, et al. Metabolic equivalent of task (METs) thresholds as an indicator of physical activity intensity. PLoS One. (2018) 13:e0200701. doi: 10.1371/journal.pone.0200701
55. Navia-Vázquez A, Parrado-Hernández E. Support vector machine interpretation. Neurocomputing. (2006) 69:1754–9. doi: 10.1016/j.neucom.2005.12.118
56. Marchese Robinson RL, Palczewska A, Palczewski J, Kidley N. Comparison of the predictive performance and interpretability of random forest and linear models on benchmark data sets. J Chem Inform Model. (2017) 57:1773–92. doi: 10.1021/acs.jcim.6b00753
57. Rajani NF, Krause B, Yin W, Niu T, Socher R, Xiong C. Explaining and improving model behavior with k nearest neighbor representations. arXiv [preprint]. (2020):
58. Ridgeway G, Madigan D, Richardson T, O’Kane J. Interpretable boosted naïve bayes classification. KDD-98 Proceedings. New York, NY: ACM (1998). p. 101–4.
59. Zhang Q, Wu YN, Zhu SC. Interpretable convolutional neural networks. Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (8827-8836). Manhattan, NJ: IEEE (2018). doi: 10.1109/CVPR.2018.00920
60. Van den Broeck G, Lykov A, Schleich M, Suciu D. On the tractability of SHAP explanations. J Artificial Intell Res. (2022) 74:851–86. doi: 10.1613/jair.1.13283
61. Zhao W, Joshi T, Nair VN, Sudjianto A. Shap values for explaining CNN-based text classification models. arXiv [Preprint]. (2020):
62. Meng Y, Yang N, Qian Z, Zhang G. What makes an online review more helpful: an interpretation framework using XGBoost and SHAP values. J Theor Appl Electron Comm Res. (2020) 16:466–90. doi: 10.3390/jtaer16030029
63. Wang Y, Yao Q, Kwok JT, Ni LM. Generalizing from a few examples: a survey on few-shot learning. ACM Comput Surveys (CSUR). (2020) 53:1–34. doi: 10.1145/3386252
64. Gilchrist SC, Barac A, Ades PA, Alfano CM, Franklin BA, Jones LW, et al. Cardio-oncology rehabilitation to manage cardiovascular outcomes in cancer patients and survivors: a scientific statement from the American Heart Association. Circulation. (2019) 139:e997–1012. doi: 10.1161/CIR.0000000000000679
65. Scott JM, Nilsen TS, Gupta D, Jones LW. Exercise therapy and cardiovascular toxicity in cancer. Circulation. (2018) 137:1176–91. doi: 10.1161/CIRCULATIONAHA.117.024671
66. Argilés JM, Busquets S, López-Soriano FJ, Costelli P, Penna F. Are there any benefits of exercise training in cancer cachexia? J Cachexia Sarcopenia Muscle. (2012) 3:73–6. doi: 10.1007/s13539-012-0067-5
67. Antunes JMM, Ferreira RM, Moreira-Gonçalves D. Exercise training as therapy for cancer-induced cardiac cachexia. Trends Mol Med. (2018) 24:709–27. doi: 10.1016/j.molmed.2018.06.002
68. Churpek MM, Carey KA, Edelson DP, Singh T, Astor BC, Gilbert ER, et al. Internal and external validation of a machine learning risk score for acute kidney injury. JAMA Netw Open. (2020) 3:e2012892. doi: 10.1001/jamanetworkopen.2020.12892
69. Lu Y, Ni Y, Wang Q, Jing F, Zhou Y, He X, et al. Effectiveness of sexual health influencers identified by an ensemble machine learning model in promoting secondary distribution of HIV self-testing among men who have sex with men in China: study protocol for a quasi-experimental trial. BMC Public Health. (2021) 21:1772. doi: 10.1186/s12889-021-11817-2
70. Plante TB, Blau AM, Berg AN, Weinberg AS, Jun IC, Tapson VF, et al. Development and external validation of a machine learning tool to rule out COVID-19 among adults in the emergency department using routine blood tests: a large, multicenter, real-world study. J Med Internet Res. (2020) 22:e24048. doi: 10.2196/24048
Keywords: exercise prescription, machine learning, cardio-oncology, physical activity, interpretable artificial intelligence, prescription recommendation
Citation: Gao T, Ren H, He S, Liang D, Xu Y, Chen K, Wang Y, Zhu Y, Dong H, Xu Z, Chen W, Cheng W, Jing F and Tao X (2023) Development of an interpretable machine learning-based intelligent system of exercise prescription for cardio-oncology preventive care: A study protocol. Front. Cardiovasc. Med. 9:1091885. doi: 10.3389/fcvm.2022.1091885
Received: 07 November 2022; Accepted: 12 December 2022;
Published: 01 December 2023.
Edited by:
Jiandong Zhou, Nuffield Department of Medicine, Medical Sciences Division, University of Oxford, United KingdomReviewed by:
Yuxin Ni, Boston University, United StatesYabin Wen, Macau University of Science and Technology, Macao SAR, China
Copyright © 2023 Gao, Ren, He, Liang, Xu, Chen, Wang, Zhu, Dong, Xu, Chen, Cheng, Jing and Tao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fengshi Jing, ZmVuZ3NoaS5qaW5nQG1lZC51bmMuZWR1; Xiaoyu Tao, ZXBpLmRlcmVrdGFvQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share senior authorship
 Tianyu Gao
Tianyu Gao Hao Ren2,3†
Hao Ren2,3† Shan He
Shan He Yuxin Zhu
Yuxin Zhu Zhongzhi Xu
Zhongzhi Xu Weibin Cheng
Weibin Cheng Fengshi Jing
Fengshi Jing Xiaoyu Tao
Xiaoyu Tao