
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 10 January 2023
Sec. Cardiac Rhythmology
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.1077992
This article is part of the Research Topic Systems Biology and Data-Driven Machine Learning-Based Models in Personalized Cardiovascular Medicine View all 17 articles
 Menglu Lin1†
Menglu Lin1† Yangyang Bao1†
Yangyang Bao1† Zunhui Du1†
Zunhui Du1† Yanting Zhou2
Yanting Zhou2 Ning Zhang1
Ning Zhang1 Changjian Lin1
Changjian Lin1 Yinyin Xie2
Yinyin Xie2 Ruihong Zhang2
Ruihong Zhang2 Qiheng Li1
Qiheng Li1 Jinwei Quan1
Jinwei Quan1 Tingfang Zhu1
Tingfang Zhu1 Yuan Xie3
Yuan Xie3 Cathy Xu1
Cathy Xu1 Yun Xie1
Yun Xie1 Yue Wei1
Yue Wei1 Qingzhi Luo1
Qingzhi Luo1 Wenqi Pan1
Wenqi Pan1 Lingjie Wang1
Lingjie Wang1 Tianyou Ling1
Tianyou Ling1 Qi Jin1
Qi Jin1 Liqun Wu1*
Liqun Wu1* Tong Yin2*
Tong Yin2* Yucai Xie1*
Yucai Xie1*Background: There are controversies on the pathophysiological alteration in patients with atrial fibrillation (AF) undergoing pulmonary vein isolation using different energy sources.
Objectives: We evaluated the changes in plasma proteins in acute phase post-ablation in patients receiving cryoballoon ablation, radiofrequency balloon ablation, or radiofrequency ablation.
Methods: Blood samples from eight healthy controls and 24 patients with AF were taken on the day of admission, day 1, and day 2 post-ablation and analyzed by the Olink proximity extension assay. Proteins were identified and performed with enrichment analysis. Protein–protein interaction network and module analysis were conducted using Cytoscape software.
Results: Of 181 proteins, 42 proteins in the cryoballoon group, 46 proteins in the radiofrequency balloon group, and 43 proteins in the radiofrequency group significantly changed after ablation. Most of the proteins altered significantly on the first day after ablation. Altered proteins were mainly involved in cytokine–cytokine receptor interaction. Both balloon-based ablations showed a similar shift toward enhancing cell communication and regulation of signaling while inhibiting neutrophil chemotaxis. However, radiofrequency ablation presented a different trend. Seed proteins, including osteopontin, interleukin-6, interleukin-10, C-C motif ligand 8, and matrix metalloproteinase-1, were identified. More significant proteins associated with hemorrhage and coagulation were selected in balloon-based ablations by machine learning.
Conclusion: Plasma protein response after three different ablations in patients with AF mainly occurred on the first day. Radiofrequency balloon ablation shared similar alteration in protein profile as cryoballoon ablation compared with radiofrequency ablation, suggesting that lesion size rather than energy source is the determinant in pathophysiological responses to the ablation.
Atrial fibrillation (AF) is the most common arrhythmia around the world, which can cause a variety of clinical outcomes, such as stroke, heart failure, and cardiovascular mortality. The two main strategies of treatment are anti-arrhythmic drugs and catheter ablation. Although the primary treatment for AF is pharmacology therapy, it has limited effectiveness (1). Previous studies have demonstrated that catheter ablation outperforms drug therapy in terms of recurrence rate and quality of life in long term (2–4). Accordingly, catheter ablation is recommended by the most recent guidelines (5, 6).
Currently, radiofrequency (RF) ablation and cryoballoon (CB) ablation are the most common techniques to treat AF, with no significant difference in terms of safety or efficacy (7, 8). Experimental data suggested that the use of cryoablation is different from radiofrequency ablation due to its preservation of the extracellular matrix and reduction of endothelial and thrombus formation (9–11). In clinical studies, however, there was a comparable increase in markers of cell damage, platelet activation, and inflammatory response between CB and RF ablation (12, 13). Radiofrequency balloon (RB) ablation, also called hot balloon ablation, is an emerging approach for AF ablation with favorable safety and effectiveness (14, 15). However, there are few data about the biomarkers’ changes compared to the CB or RF ablation.
In order to resolve the controversy, we utilized a new proteomic assay platform—Olink proximity extension assay, which has been widely applied in the biomarker discovery of the cardiovascular disease field (16, 17), to assess the change in 181 different proteins during the acute post-procedure phase from the cryoballoon ablation group and irrigated-tip RF catheter ablation group. We also introduced the RB ablation group into comparison to avoid alteration resulting from lesion size rather than energy sources (18).
After the Institutional Review Committee and Ethics Committee approved the study, 24 patients diagnosed with paroxysmal or persistent AF at our institution who gave informed written consent were included, in which pulmonary vein isolation was performed with the CB catheter (Arctic Front Advance Cardiac Cryoablation Catheter, Medtronic), RB catheter (HELIOSTAR™ Balloon Ablation Catheter, Biosense Webster Inc.), or RF catheter (NaviStar™RMT, ThermoCool™; Biosense Webster, CA, USA). In our study, all patients met the following inclusion criteria: (1) Non-valvular AF or flutter. The exclusion criteria were as follows: (1) <18 or >80 years old; (2) history of left atrial surgery; (3) transesophageal echocardiography-witnessed left atrial thrombus; (4) uncontrolled hyperthyroidism; (5) pregnancy; (6) history of obstructive sleep apnea syndrome; and (7) history of myocardial infarction, percutaneous coronary intervention, heart surgery, transient ischemic attack, or stroke within 3 months before the procedure. Patients were treated with oral anticoagulation at least 1 month before the ablation procedure. During the procedure, 100-IU/kg heparin was administered to maintain an activated clotting time of ≥300 s. Eight healthy controls were also enrolled as a comparison. A blood sample of 2 ml from the peripheral vein was taken and added to the ethylene diamine tetraacetic acid (EDTA) anticoagulant tube on three-time points, the admission day, day 1 (D1), and day 2 (D2) after ablation. The samples were immediately centrifuged and frozen at −80°C until analysis. All the patients were monitored by the telemetry electrocardiogram during hospitalization, and electrocardiogram data were collected for analysis.
The proteomic analyses were performed at the National Research Center for Translational Medicine, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine. The Olink multiplex cardiovascular disease III and inflammation panels comprise 184 proteins. Three protein markers were available on both panels, resulting in 181 unique markers. Samples were run in duplicates. The limit of detection (LOD) was defined as three standard deviations above the background, and values below this limit were reported as <LOD. The results from each assay were rendered as normalized log2 protein expression (NPX) data, which are relative values, and one-unit higher NPX represents a doubling of the measured protein concentration. NPX values for proteins with >75% of measurements below LOD were removed from the analysis.
Statistical analysis was performed using GraphPad Prism nine software and SPSS 25. Normally distributed continuous variables were shown as mean ± SD. Categorical variables were shown as counts and percentages. Categorical variables were compared with the chi-square test. Wilcoxon matched-pairs signed-rank test was used to assess differences for each analyte before and after ablation. The Kruskal–Wallis H-test was used to assess differences in the clinical characteristics and the levels of analytes according to the ablation type. A P-value of <0.05 was considered statistically significant.
Heatmap was plotted by http://www.bioinformatics.com.cn, a free online platform for data analysis and visualization. The protein interaction, the gene ontology (GO) functional, and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis in the network were performed by Search Tool for the Retrieval of Interacting Genes (STRING, version 11.5) database with the threshold of false discovery rate (FDR) <0.05. The required confidence (combined score) >0.4 was used as the cutoff criterion. In addition, the Molecular Complex Detection (MCODE) plugin in Cytoscape (version 3.7.1) was used to screen the significant modules and seed protein in the protein–protein interaction (PPI) network (degree cutoff = 2, node cutoff = 0.2, k-core = 2, and max. depth = 100). Moreover, enrichment analysis for the proteins involved in the most significant module was conducted using the STRING online tool. LASSO logistic regression model was fitted with the glmnet R package. Feature contributions to the models were visualized using the regression coefficients. The random forest model was fitted with random Forest and caret R packages according to Jack Gisby et al. with slight modifications (19). The 4-fold cross-validation that was repeated 100 times was used to estimate the model accuracy. Mtry value was calculated as the square root of the number of features. The random forest feature was extracted using the R randomForestExplainer package. Benjamini–Hochberg adjustment was applied to the p-value calculated by the model, and an adjusted value of 0.05 was indicated as the significance threshold. Multiway importance plot was replotted via R package ggplot2.
A total of 32 persons were included in this study, of which eight were controls and eight received CB, RB, or RF ablation, respectively. The baseline characteristics of 32 participants are presented in Table 1. There were no significant differences in ages, gender, laboratory values, past medical history, and the history of medication apart from the use of anticoagulants (p < 0.01).
All the patients were monitored by the telemetry electrocardiogram during the hospitalization. The recurrent atrial arrhythmia after ablation has no significant differences in the three groups, although four patients presented AF or premature atrial contraction in the CB group, compared with two patients in the RB and RF groups, respectively (p = 0.472, Figure 1).
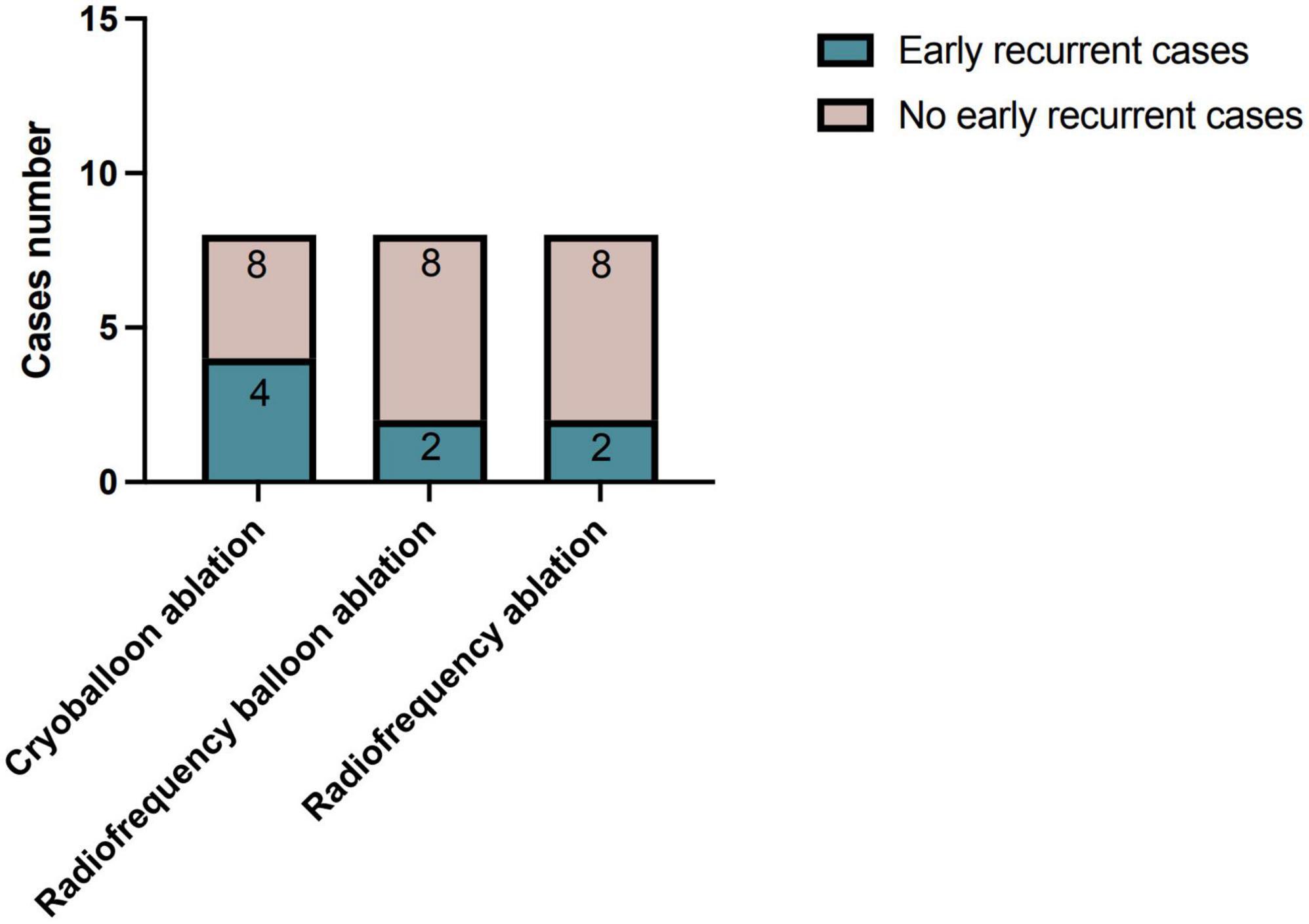
Figure 1. Early recurrence of atrial arrhythmia post-different ablations during hospitalization. The early recurrent cases of atrial arrhythmia post-ablations were not significantly different between three ablation groups (p = 0.472).
A total of 181 unique proteins in two panels were tested, and 19 (10.5%) analytes were removed with over 75% of samples below LOD. Table 2 shows the biomarkers that showed significant differences before and after ablation using three different methods. Forty-two proteins (19 increased and 24 decreased), 46 proteins (21 increased and 25 decreased), and 43 proteins (13 increased and 30 decreased) showed significant changes in the CB, RB, and RF groups, respectively (Supplementary Figure 4).
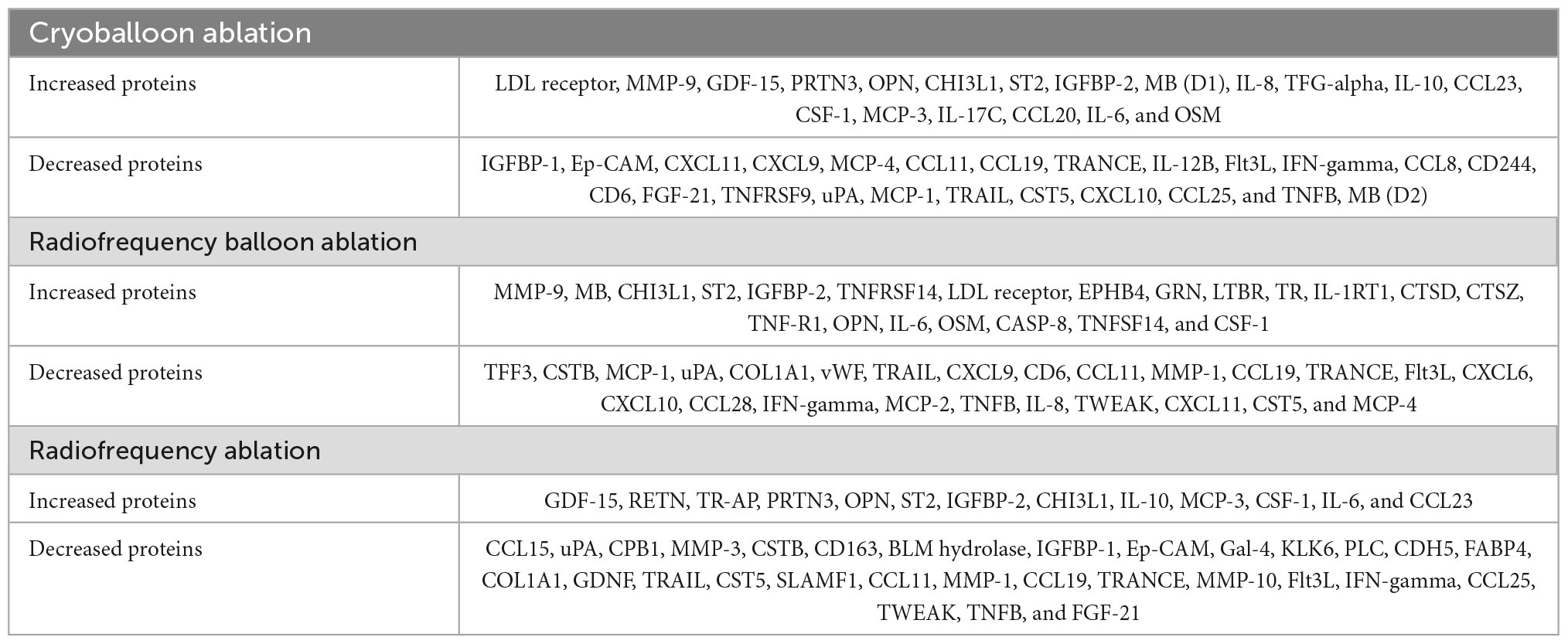
Table 2. Significantly altered proteins before and after ablation were sorted by three different techniques.
The heatmaps of the altered proteins in three groups before and after ablation are shown in Figure 2, which indicates that the change in proteins in the acute phase was mainly on D1 post-ablation, especially in CB and RB groups.
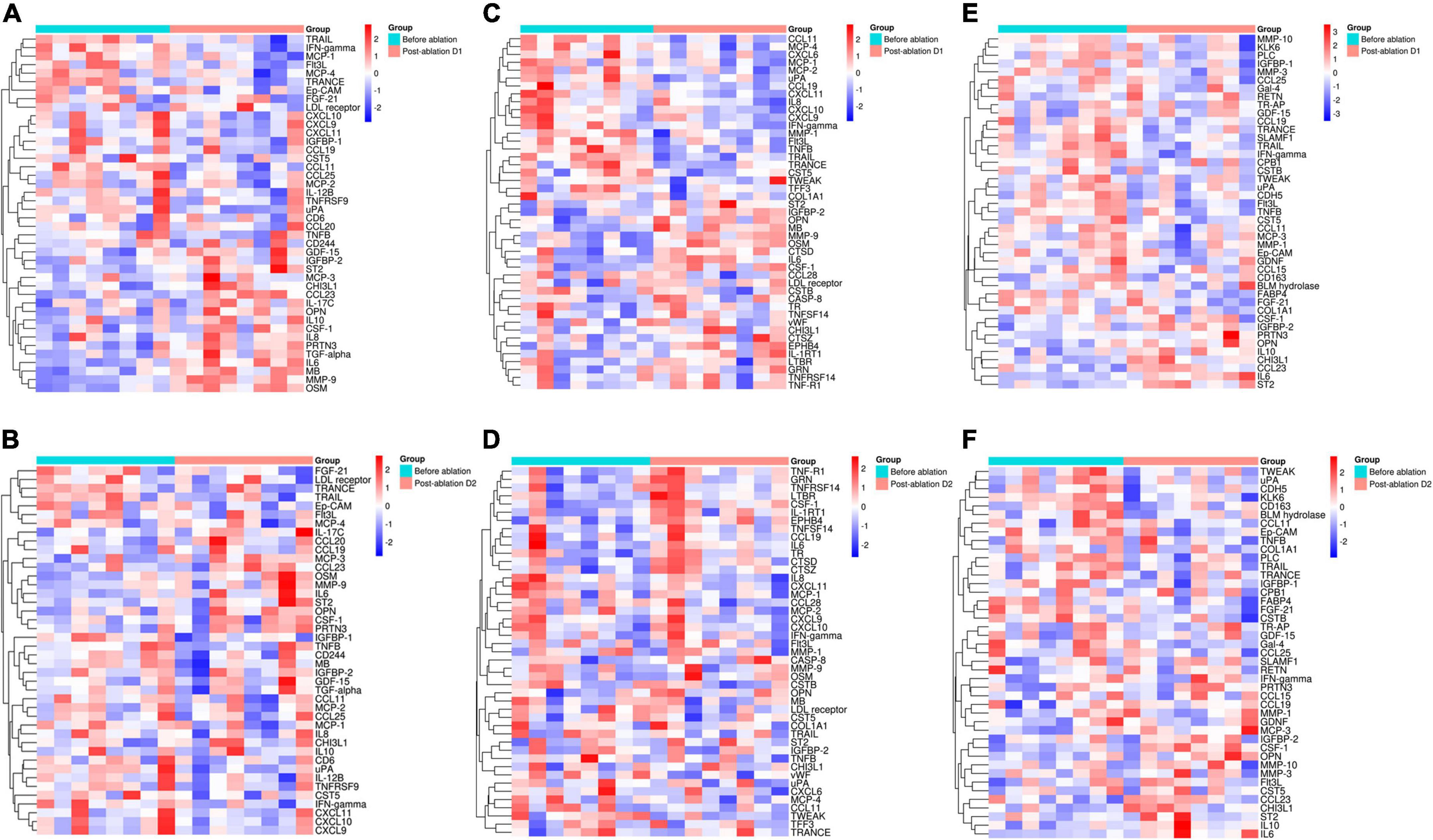
Figure 2. Heatmap of altered proteins before and after ablation. Most of the altered proteins changed on the first day after ablation. The heatmap of the altered proteins before and after ablation D1 and D2 in the cryoballoon group (A,B), the radiofrequency balloon group (C,D), and the radiofrequency group (E,F) (red: high expression and blue: low expression).
Based on the altered proteins and the STRING database, we constructed the PPI network for the increased and decreased proteins separately in three groups (Supplementary Figures 1–3). The top KEGG pathways of altered proteins in different groups are shown in Figure 3. There was no distinguishment because the altered proteins in three groups were mainly enriched in cytokine–cytokine receptor interaction and viral protein interaction with cytokine and cytokine receptor.
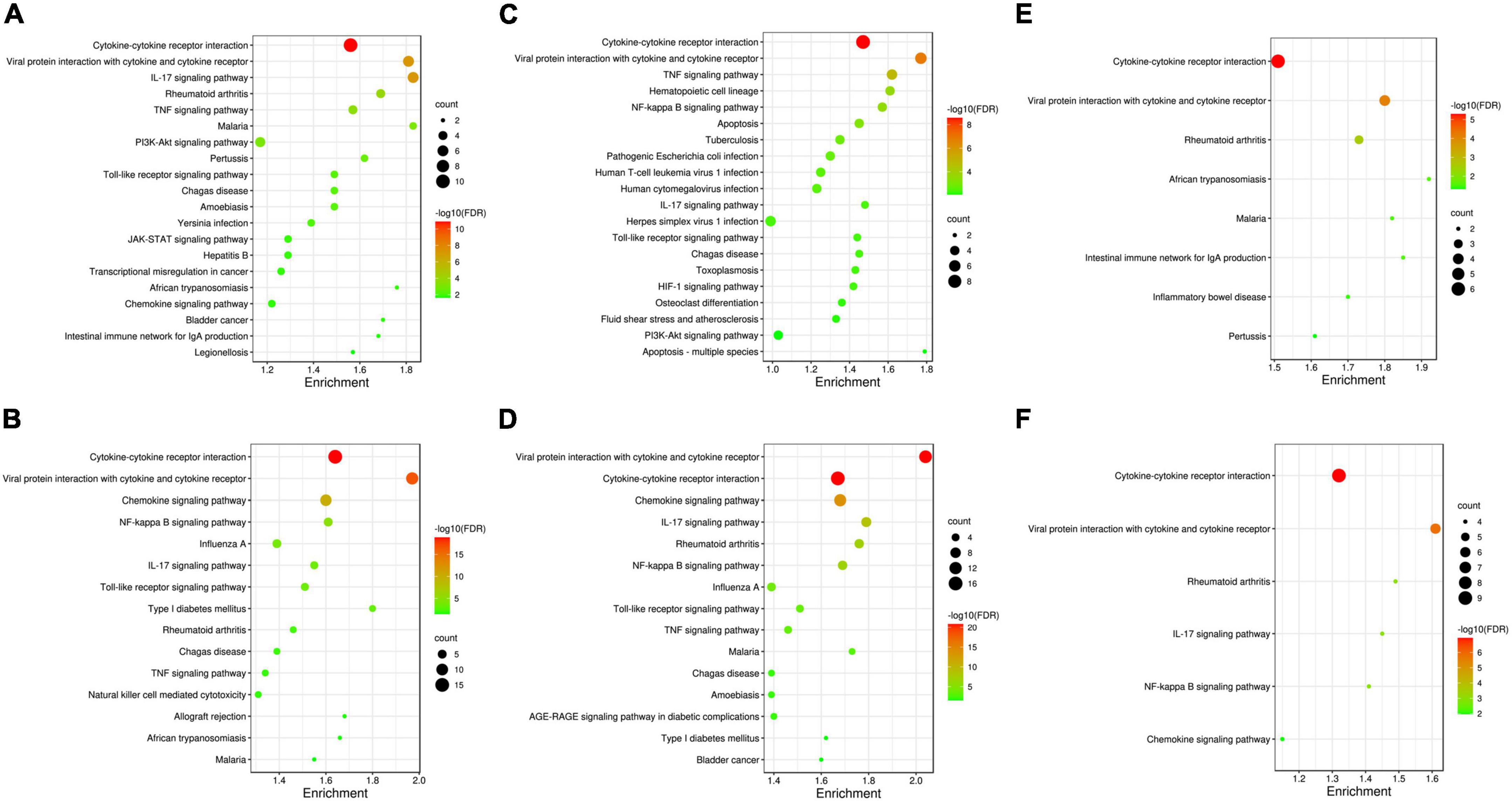
Figure 3. Kyoto encyclopedia of genes and genomes pathways analysis of altered proteins in three ablation groups. Altered proteins in three groups are all mainly enriched in cytokine–cytokine receptor interaction and viral protein interaction with cytokine and cytokine receptor. (A,B) The top 20 KEGG pathways enriched for the increased proteins and decreased proteins in the cryoballoon ablation group; (C,D) the top 20 KEGG pathways enriched for the increased proteins and decreased proteins in the radiofrequency balloon ablation group; (E,F) the all KEGG pathways enriched for the increased proteins and decreased proteins in the radiofrequency ablation group. The sizes of the bubbles are illustrated from big to small in descending order of the number of potential targets involved in the pathways.
In order to more accurately elucidate the protein change pattern after different ablations, we used the MCODE plugin in the Cytoscape software to conduct module analysis on the PPI network and obtained a potential protein functional module with the best score, as shown in Figure 4. Furthermore, the GO enrichment analysis for six significant modules (Supplementary Tables 1–5) showed a similar biological process in CB and RB groups. Proteins involved in the most significant module for the decreased proteins were both enriched in the neutrophil chemotaxis (Tables 3, 4). Proteins in the most significant module for the increased proteins in the CB group mainly enriched in the cytokine-mediated signaling pathway (Table 3), which is part of cell communication and regulation of signaling, the two major positively regulated biological processes in the RB group (Table 4). However, as seen in Table 5, the cytokine-mediated signaling pathway was downregulated in the RF group.
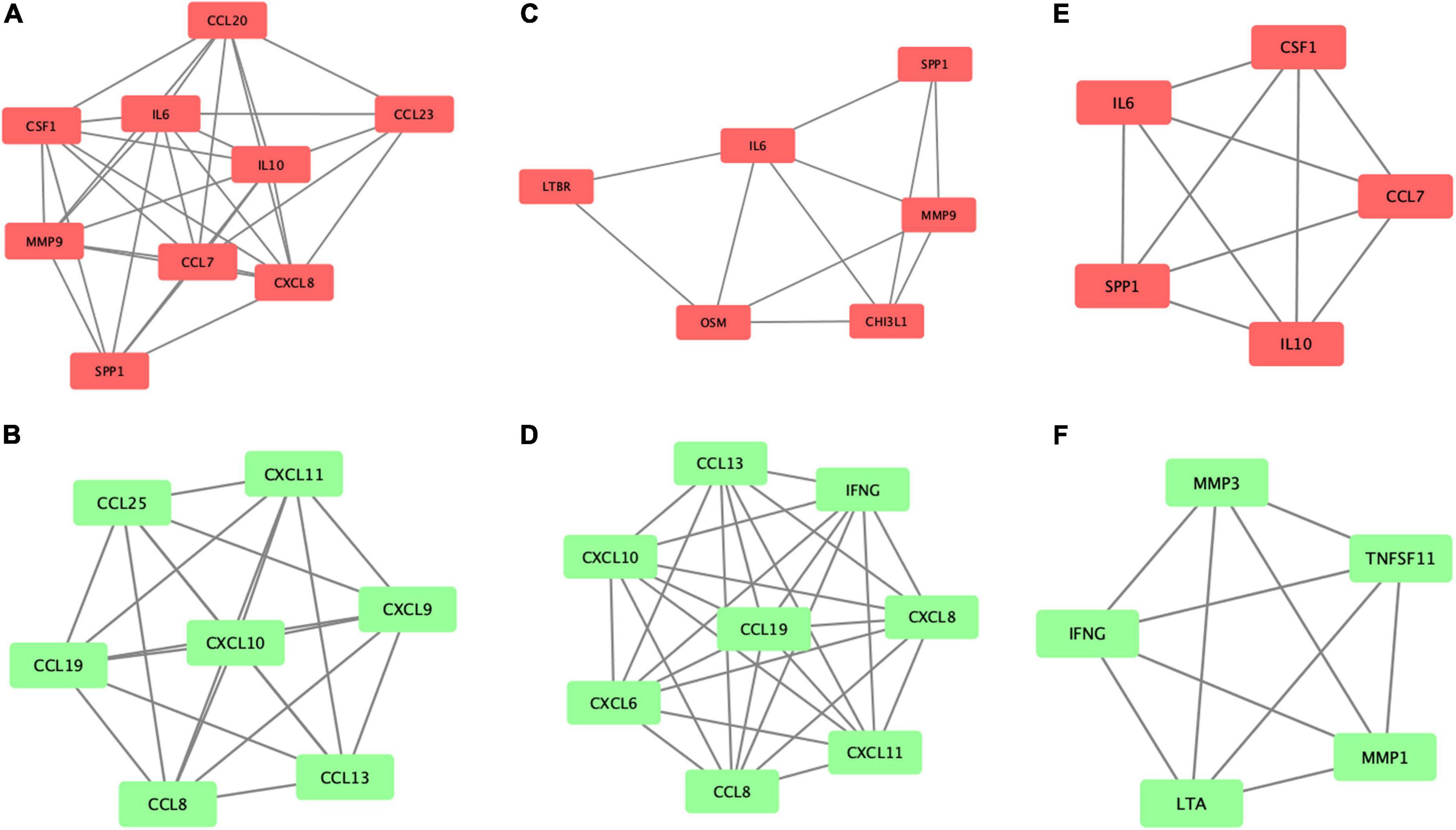
Figure 4. Potential functional modules with the best score in the PPI network. The most significant module for the increased proteins (A) and decreased proteins (B) in the cryoballoon group; (C,D) in the radiofrequency balloon group and (E,F) in the radiofrequency group, respectively. The significant modules were analyzed by using MCODE plugin, and then module networks were visualized using Cytoscape software.
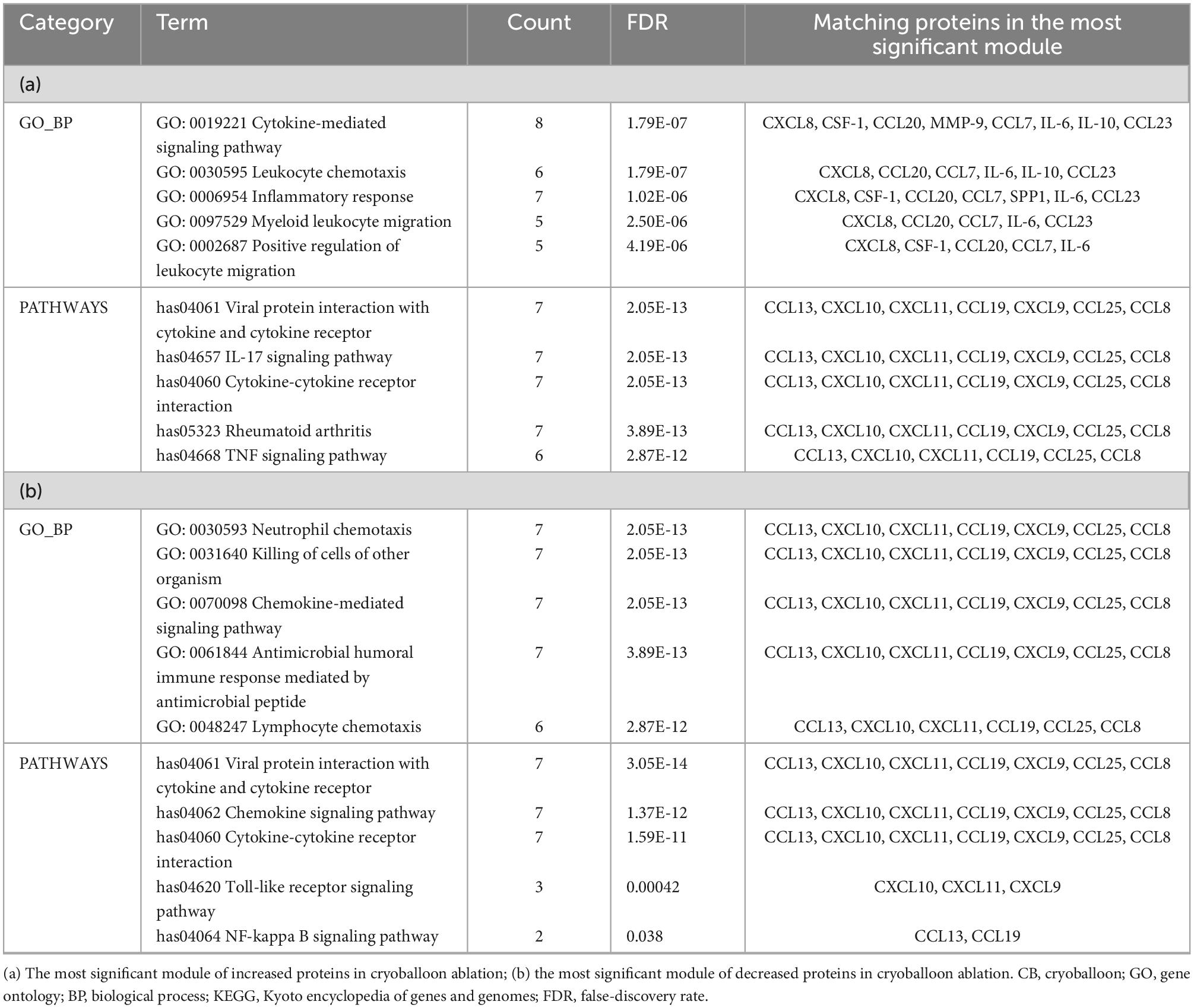
Table 3. GO_BP and KEGG pathways enriched in the most significant module in the CB group (only top five listed).
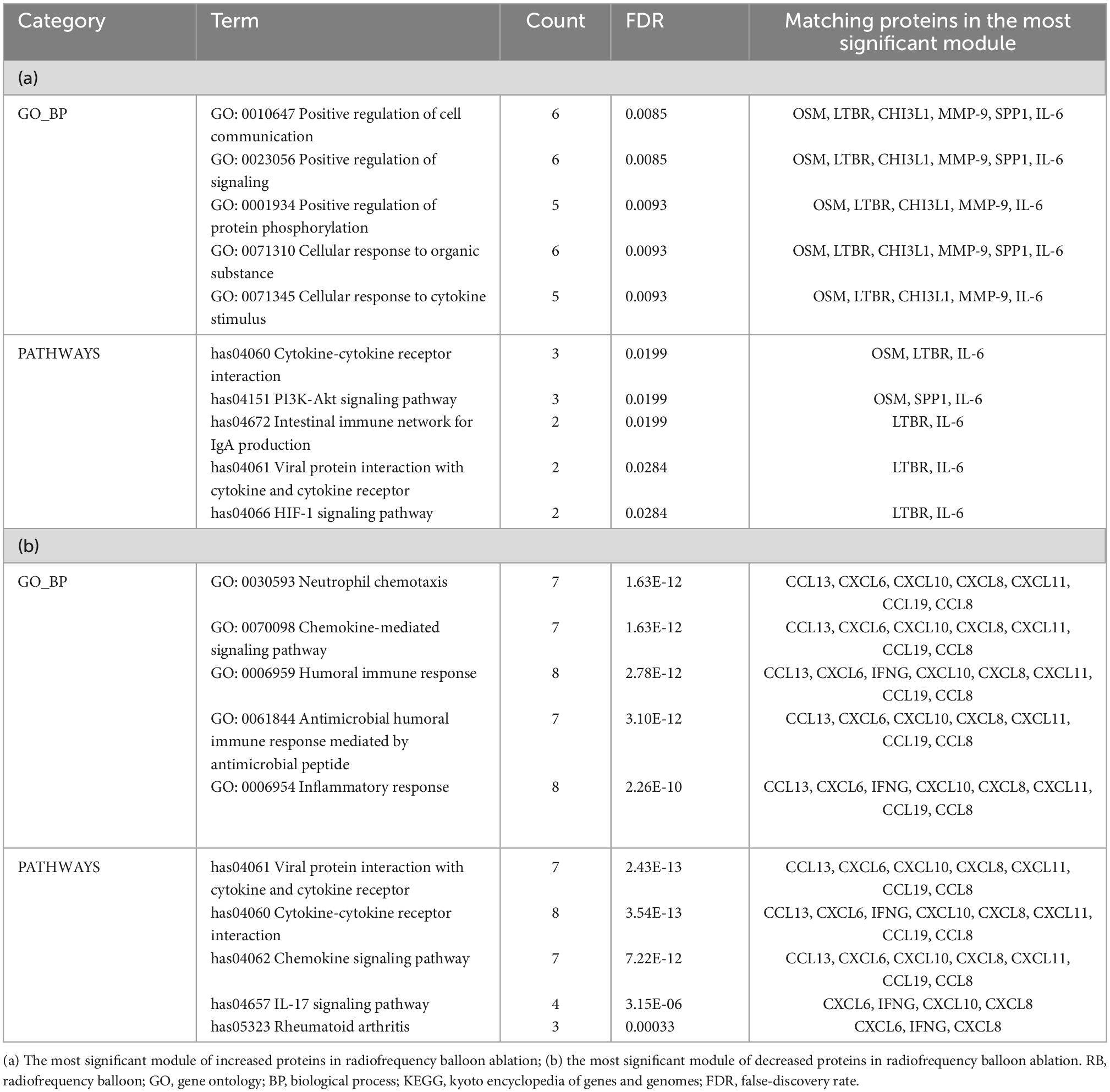
Table 4. GO_BP and KEGG pathways enriched in the most significant module in the RB group (only top five listed).
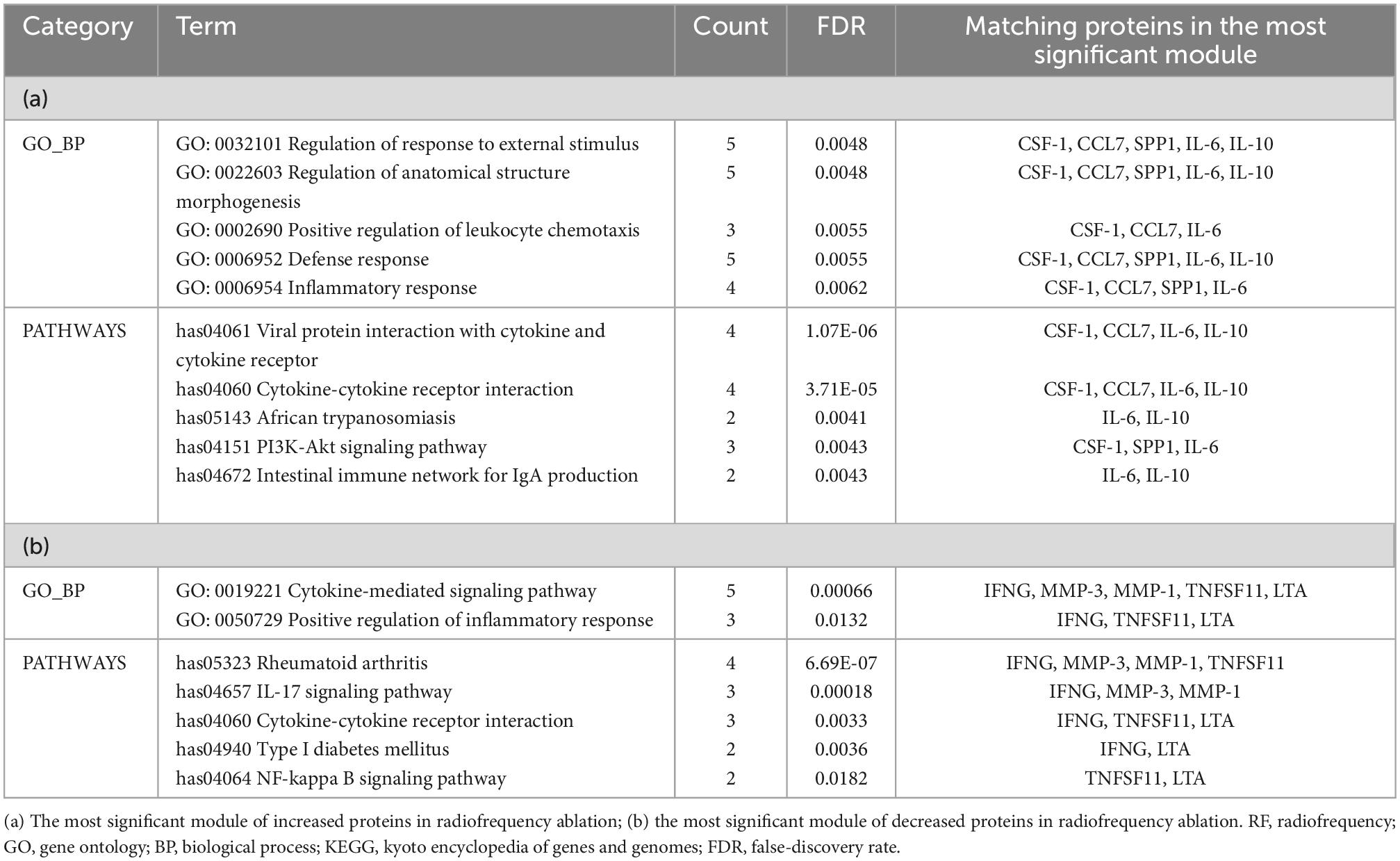
Table 5. GO_BP and KEGG pathways enriched in the most significant module in the RF group (only top five listed).
The MCODE application also provided the highest dense protein complex as the seed protein from the potential functional module, which helps to identify the potential markers for further study in three different techniques. The seed protein of the increased proteins was osteopontin (OPN), also known as secreted phosphoprotein 1, in the CB group and interleukin-6 (IL-6) in the RB group. For patients who received RF ablation, the seed increased protein was IL-10.
Among the proteins decreased after ablation, the seed protein was C-C motif ligand 8 (CCL8), also known as monocyte chemoattractant protein-2, in both CB and RB groups. Differently, the seed protein was matrix metalloproteinase-1 (MMP-1) in the RF group.
The change in OPN, IL-6, IL-10, CCL8, and MMP-1 levels at three-time points in three ablation groups and the control group are shown in Figure 5, with a comparable measurement between the groups. No significant difference was observed in these proteins at baseline between the control group and three ablation groups as well, which can exclude the disease-related effect on the change in proteins.
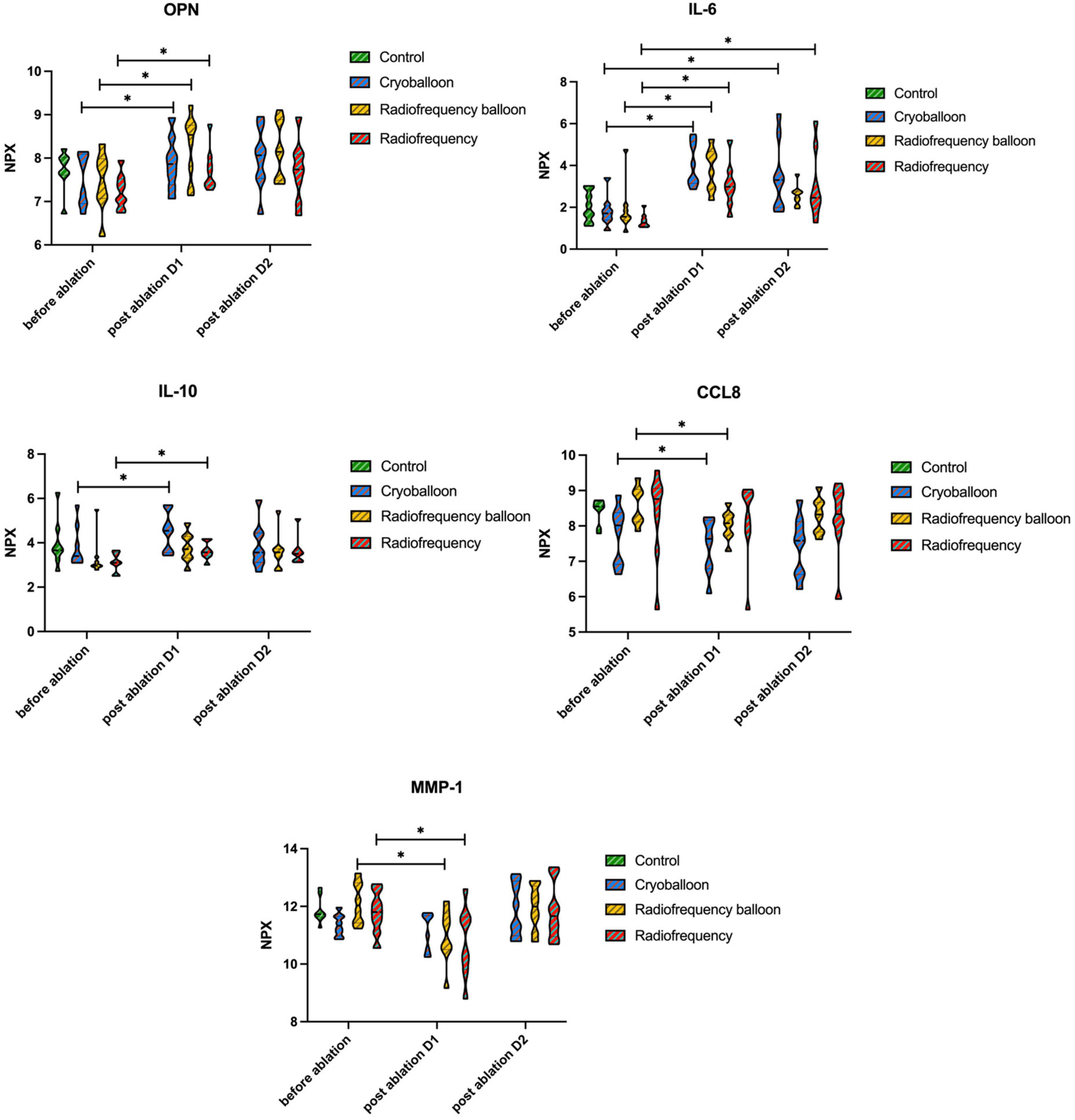
Figure 5. Levels of seed proteins before and after ablation. No differences were seen between the groups at any time point. Differences before and after ablation were assessed with the Wilcoxon signed-rank test. P-values are given for comparison within the group between different time points. OPN, osteopontin, seed-increased protein in the CB group; IL-6, interleukin-6, seed-increased protein in the RB group; IL-10, interleukin-10, seed-increased protein in the RF group; CCL8, C-C motif ligand 8, seed decreased protein in CB and RB groups; MMP-1, matrix metalloproteinase-1, seed decreased protein in the RF group. NPX, normalized protein expression. *P < 0.05.
As shown in Table 6, we identified some altered proteins associated with hemorrhage and coagulation. Proteins changes that increased thrombus formation risk after ablation were noted for OPN and urokinase-type plasminogen activator (uPA) in all groups, along with trefoil factor 3 (TFF3) in the RB group and MMP-1 in the RF group. Proteins changes that caused higher bleeding risk after ablation, include growth/differentiation factor 15, myeloblastin (PRTN3), collagen alpha-1 (I) chain, tumor necrosis factor receptor 1 (TNF-R1), ephrin type-B receptor 4 (EPHB4), and von Willebrand factor (vWF). We also conducted LASSO logistic regression and random forest to select significant proteins (Figure 6). Interestingly, two proteins (uPA and PRTN3) in the CB group and three proteins (vWF, uPA, and EPHB4) in the RB group were also the significant proteins selected by LASSO logistic regression and random forest, among which only PRTN3 was related to hemorrhage and coagulation in the RF group. No significant differences in the levels of these proteins were found between three groups (Figure 7).
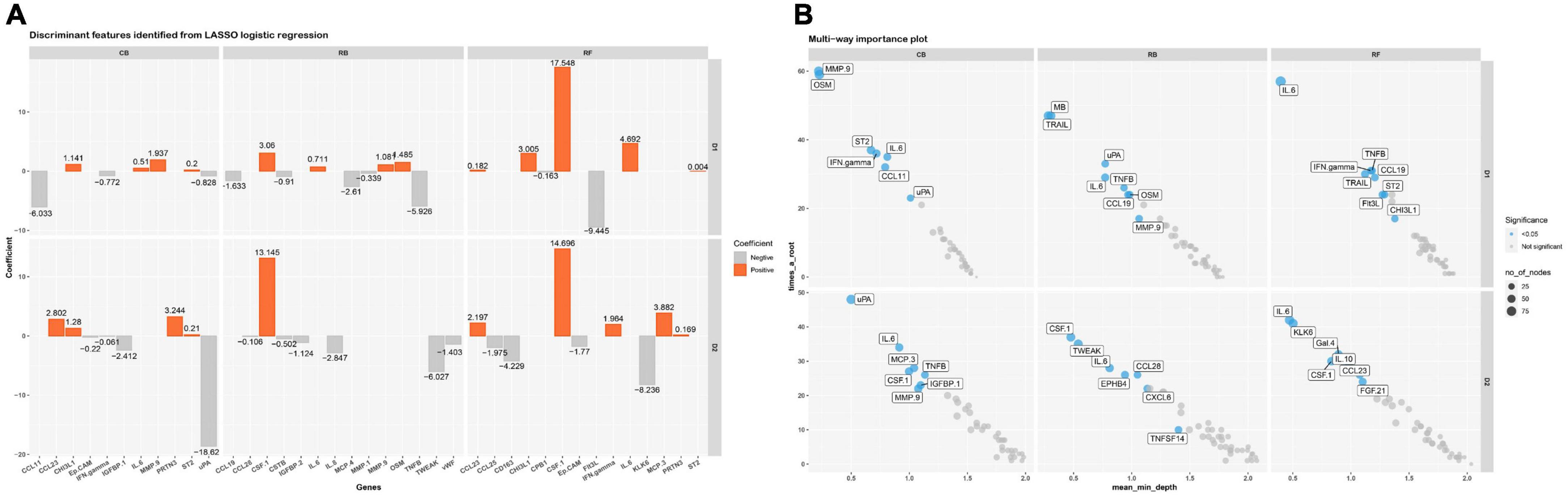
Figure 6. LASSO logistic regression and random forest of altered proteins in three ablation groups. (A) Significant proteins selected by LASSO logistic regression before and after ablation D1 and D2 in three ablation groups; (B) significant proteins selected by random forest before and after ablation D1 and D2 in three ablation groups.
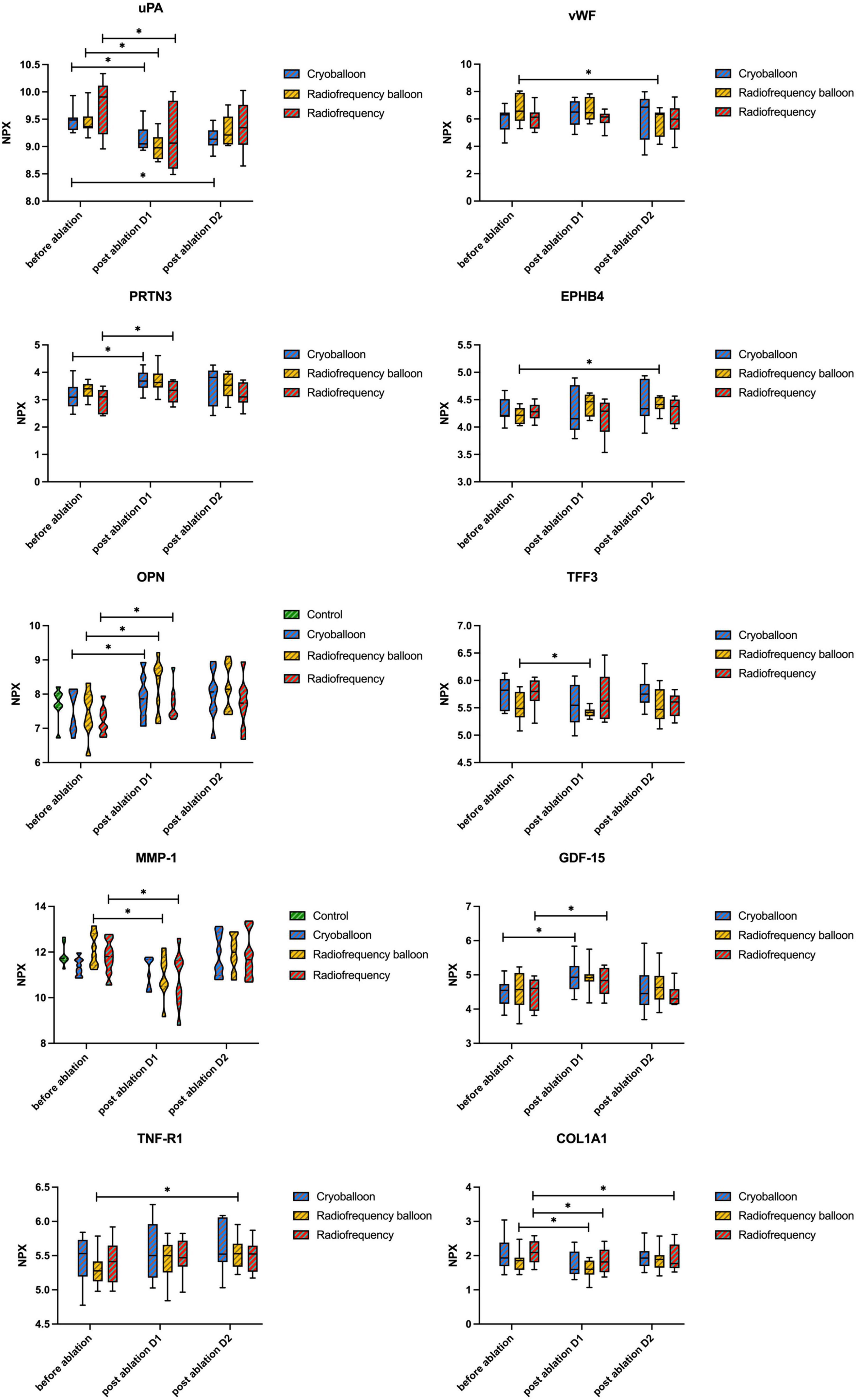
Figure 7. Levels of proteins associated with hemorrhage and coagulation activity. No differences were seen between the groups at any time point. Differences before and after ablation were assessed with the Wilcoxon signed-rank test. P-values are given for comparison within the group between different time points. uPA, urokinase-type plasminogen activator; TFF3, trefoil factor 3; GDF-15, growth/differentiation factor 15; PRTN3, myeloblastin; COL1A1, collagen alpha-1(I) chain; TNF-R1, tumor necrosis factor receptor 1; EPHB4, ephrin type-B receptor 4; vWF, von Willebrand factor; NPX, normalized protein expression; *P < 0.05. Note that the levels of OPN and MMP-1 are shown in Figure 5.
In this study, we analyzed a total of 181 different plasma proteins from eight control patients and 24 patients with AF before and after interventional ablation using three different techniques. Most of the proteins changed significantly on the first day after ablation. Although clinical studies demonstrated that same-day discharge is safe with a comparable rate of complications in the long term in patients with an overnight stay after ablation (20, 21), the pathophysiological alterations recover until the overnight stay in patients with AF undergoing pulmonary vein isolation. Given that plasma proteins changed mainly limited on the first day after three different ablations, it would be safer for patients to be discharged overnight.
Pathway analysis indicated that the proteins that changed after ablation in the acute phase were mainly in cytokine–cytokine receptor interaction in three groups. Interestingly, the module analysis and enrichment analysis indicated that CB and RB groups showed similar trends in cell communication, the regulation of signaling, and neutrophil chemotaxis. Specifically, the cytokine-mediated signaling pathway in the CB group was upregulated significantly. As part of cell communication and regulation of signaling, this signaling pathway was also positively regulated in the RB group (Supplementary Table 3). However, the cytokine-mediated signaling pathway was downregulated in the RF group. Meanwhile, neutrophil chemotaxis was inhibited in both balloon-based ablations (Tables 3, 4) but not in the RF group. To our knowledge, this phenomenon was not noted in previous studies.
We also found that both balloon-based ablations shared a similar response to inflammation, while radiofrequency ablation showed different tendencies to inflammatory response as indicated by different seed proteins after ablation. In the CB group, OPN was the most important increased protein after ablation. OPN is a matricellular protein that contributes to acute inflammation by increasing the production of IL-6, IL-12, IL-17, and interferon-gamma (IFN-γ) and inhibiting the expression of IL-10 (22). Since RB ablation is a new technique, there are few comparative studies about markers of inflammation between RB and CB ablation or RF ablation. However, the high risk of inflammation in the RB group was indicated by the seed protein IL-6 in our study. Such a finding was consistent with a previous image study, which describes the regional inflammation pattern occurring after CB ablation and RB ablation in the human left atrium using positron emission tomography (23). The upregulated expression of IL-6 by OPN has been demonstrated in inflammatory disease (24). Thus, IL-6 may trigger IL-6 trans-signaling, contributing to the upregulation of OPN in THP-1 macrophages (25). Of note, higher IL-6 concentrations can also play a role in regulating leukocyte infiltration by suppressing neutrophil recruitment (26). Neutrophil activation, as reflected by the seed protein CCL8 (27, 28), displayed a similar decreased trend in the CB and RB group in this study. While in the RF group, IL-10 generally recognized as an anti-inflammatory cytokine, was the seed protein of increased proteins in our study. The new report demonstrated that mature neutrophils could potentially dampen local inflammation by IL-10 production (29).
There is no obvious explanation for why these proteins altered significantly, but it could be related to larger lesion size and injury. Previous studies have shown that endothelial injury is related to inflammatory biomarkers, including OPN and IL-6 (30, 31). High levels of IL-6 are also associated with vascularization in sites of inflammation and with wound healing (32, 33). The higher inflammatory tendency in balloon-based ablation might show that the endothelial surface is kept less intact after balloon lesion than what is seen after irrigated RF ablation.
Although this study noted comparable levels of inflammatory markers in the acute phase between the CB and RF ablation, which is supported by other publications (34, 35), the different inflammatory effects of seed proteins indicates greater local inflammatory response in the balloon-based ablation. Along with similar enrichment analysis, these results suggest that pathophysiological response in the acute phase after ablation is more likely to be affected by the lesion size rather than the energy source.
Thromboembolism events are uncommon but one of the most feared complications of AF ablation. By using a new proteomic assay, we identified some proteins which are different from the common-used biomarkers in previous studies, such as D-dimer and P-selection.
As shown in Table 6, radiofrequency energy affected greater numbers of proteins, indicating a stronger impact on hemorrhage and coagulation activity. This finding is consistent with previous studies showing a higher rate of thrombus formation after RF than after CB ablation (11, 36). However, current data are lacking to define the prevalence of thromboembolism in patients received RB ablation. Compared with the CB group, both radiofrequency energy groups affected one more protein that could increase the risk of thrombus. As the most important decreased protein in the RF group in our study, MMP-1 plays an important role in the occurrence and development of a deep venous thrombus (37, 38), and also in regulating prothrombotic state in patients with AF (39). TFF3 is a protective marker of underlying myocyte damage/ischemia and is moderately correlated with ischemic stroke in patients with AF (40, 41). We also noticed the bleeding tendency with the lower level of vWF after RB ablation, which is commonly increased after CB and RF ablation (13, 42). In an explorative study, TNF-R1 and EPHB4 were independently associated with major bleedings in patients with AF (43), also suggesting higher hemorrhage risk in RB ablation.
Interestingly, results from LASSO logistic regression and random forest presented a different explanation for proteins associated with hemorrhage and coagulation. Among the significant proteins selected in three groups by LASSO logistic regression and random forest, respectively, only one protein in the RF group was associated with hemorrhage and coagulation activity, compared with two related proteins in the CB group and three in the RB group. Although RF ablation affected more proteins associated with thrombus and bleeding events, they are not characteristic enough to distinguish RF from other techniques. The underlying reason for a greater impact on hemorrhage and coagulation activity in balloon-based ablation groups shown in two novel bioinformatic analyses could be attributed to the larger ablation lesion.
In clinical practice, the basis for the selection of ablation technologies for pulmonary vein isolation in patients with AF remains unclear, especially with the emergence of a new technique RB. A recent clinical study showed that all ablation technologies facilitate safe and efficient pulmonary vein isolation, with slight differences in the procedural data and complications (44). To replenish previous clinical studies, the similar alteration of two balloon-based ablations in protein profile in our study provided the pathophysiological evidence from protein levels to support the application of RB in the clinic.
This study was limited to the proteins provided by the Olink panel and the evaluation period. Thus, most of the investigated proteins are still not clearly related to the clinical event, although they are useful for the pathophysiological understanding of the ablation lesion mechanism. Finally, the size of this explorative study was small and, as such, did not have enough power to show minor differences between the three ablation techniques.
Multiple plasma proteins were differently expressed after catheter ablation using different techniques, especially on the first day after ablation, suggesting that longer monitoring is not needed in patients with AF undergoing uncomplicated catheter ablation. The pattern of the protein change during the acute phase is mainly affected by the lesion size according to the similar enrichment analysis in the most significant module of CB and RB ablation. We also identified some important plasma proteins that could be of potential interest to future studies.
By comparison, balloon-based ablation (CB and RB) showed a higher tendency of inflammation and had more influence on hemorrhage and coagulation activity. Further studies of these biomarkers and clinical events in patients with AF who received different ablations are warranted.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by the Ruijin Hospital Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
ML: data curation-lead, formal analysis-lead, investigation-equal, methodology-equal, validation-equal, visualization-equal, and writing—original draft, review, and editing-equal. YB: conceptualization-lead, investigation-equal, methodology-equal, validation-equal, and writing—original draft, review, and editing-equal. ZD: conceptualization-supporting, data curation-supporting, investigation-equal, methodology-equal, validation-equal, and writing—original draft, review, and editing-equal. NZ, CL, YX, YW, QZL, WP, TL, and QJ: methodology-equal. YYX: conceptualization-supporting and methodology-equal. YZ and RZ: methodology-equal and visualization-equal. QHL: investigation-equal and validation-equal. JQ, TZ, and CX: investigation-equal. YAX, LJW, and LQW: writing—review and editing-equal. TY: conceptualization-supporting, funding acquisition-equal, supervision-equal, and writing—review and editing-equal. YCX: conceptualization-supporting, data curation-supporting, funding acquisition-equal, supervision-equal, and writing—review and editing-equal. All authors contributed to the article and approved the submitted version.
This study was supported by the National Natural Science Foundation of China (grant number: 81570234) and the National Research Center for Translational Medicine Shanghai Open Project, TMSK-2021-508.
We are grateful to the patients who participated in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.1077992/full#supplementary-material
AF, atrial fibrillation; CB, cryoballoon; RB, radiofrequency balloon; RF, radiofrequency; PPI, protein–protein interaction; LOD, limit of detection; NPX, normalized protein expression; GO, gene ontology; KEGG, Kyoto encyclopedia of genes and genomes; FDR, false discovery rate.
1. Goudis C, Vasileiadis I, Liu T. Epicardial adipose tissue and atrial fibrillation: pathophysiological mechanisms, clinical implications, and potential therapies. Curr Med Res Opin. (2018) 34:1933–43. doi: 10.1080/03007995.2018.1462786
2. Cosedis Nielsen J, Johannessen A, Raatikainen P, Hindricks G, Walfridsson H, Kongstad O, et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med. (2012) 367:1587–95.
3. Packer D, Mark D, Robb R, Monahan K, Bahnson T, Poole J, et al. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA. (2019) 321:1261–74. doi: 10.1001/jama.2019.0693
4. Khan A, Khan S, Sheikh M, Khuder S, Grubb B, Moukarbel G. Catheter ablation and antiarrhythmic drug therapy as first- or second-line therapy in the management of atrial fibrillation: systematic review and meta-analysis. Circ Arrhythm Electrophysiol. (2014) 7:853–60.
5. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax J, Blomstrom-Lundqvist C, et al. Corrigendum to: 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European association for cardio-thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European heart rhythm association (EHRA) of the ESC. Eur Heart J. (2021) 42:4194. doi: 10.1093/eurheartj/ehab648
6. January C, Wann L, Calkins H, Chen L, Cigarroa J, Cleveland J Jr., et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the american college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation. (2019) 140:e125–51. doi: 10.1161/CIR.0000000000000665
7. Andrade J, Champagne J, Dubuc M, Deyell M, Verma A, Macle L, et al. Cryoballoon or radiofrequency ablation for atrial fibrillation assessed by continuous monitoring: a randomized clinical trial. Circulation. (2019) 140:1779–88.
8. Wang Y, Wang W, Yao J, Chen L, Yi S. Second-generation cryoballoon vs. contact-force sensing radiofrequency catheter ablation in atrial fibrillation: a meta-analysis of randomized controlled trials. J Interv Card Electrophysiol. (2021) 60:9–19. doi: 10.1007/s10840-020-00893-w
9. Ohkawa S, Hackel D, Mikat E, Gallagher J, Cox J, Sealy W. Anatomic effects of cryoablation of the atrioventricular conduction system. Circulation. (1982) 65:1155–62.
10. van Oeveren W, Crijns H, Korteling B, Wegereef E, Haan J, Tigchelaar I, et al. Blood damage, platelet and clotting activation during application of radiofrequency or cryoablation catheters: a comparative in vitro study. J Med Eng Technol. (1999) 23:20–5.
11. Khairy P, Chauvet P, Lehmann J, Lambert J, Macle L, Tanguay J, et al. Lower incidence of thrombus formation with cryoenergy versus radiofrequency catheter ablation. Circulation. (2003) 107:2045–50.
12. Herrera Siklody C, Arentz T, Minners J, Jesel L, Stratz C, Valina C, et al. Cellular damage, platelet activation, and inflammatory response after pulmonary vein isolation: a randomized study comparing radiofrequency ablation with cryoablation. Heart Rhythm. (2012) 9:189–96. doi: 10.1016/j.hrthm.2011.09.017
13. Malmborg H, Christersson C, Lonnerholm S, Blomstrom-Lundqvist C. Comparison of effects on coagulation and inflammatory markers using a duty-cycled bipolar and unipolar radiofrequency pulmonary vein ablation catheter vs. a cryoballoon catheter for pulmonary vein isolation. Europace. (2013) 15:798–804. doi: 10.1093/europace/eus411
14. Schilling R, Dhillon G, Tondo C, Riva S, Grimaldi M, Quadrini F, et al. Safety, effectiveness, and quality of life following pulmonary vein isolation with a multi-electrode radiofrequency balloon catheter in paroxysmal atrial fibrillation: 1-year outcomes from SHINE. Europace. (2021) 23:851–60. doi: 10.1093/europace/euaa382
15. Reddy V, Schilling R, Grimaldi M, Horton R, Natale A, Riva S, et al. Pulmonary vein isolation with a novel multielectrode radiofrequency balloon catheter that allows directionally tailored energy delivery: short-term outcomes from a multicenter first-in-human study (RADIANCE). Circ Arrhythm Electrophysiol. (2019) 12:e007541. doi: 10.1161/CIRCEP.119.007541
16. Joshi A, Rienks M, Theofilatos K, Mayr M. Systems biology in cardiovascular disease: a multiomics approach. Nat Rev Cardiol. (2021) 18:313–30.
17. Verdonschot J, Ferreira J, Pellicori P, Brunner-La Rocca H, Clark A, Cosmi F, et al. Proteomic mechanistic profile of patients with diabetes at risk of developing heart failure: insights from the HOMAGE trial. Cardiovasc Diabetol. (2021) 20:163. doi: 10.1186/s12933-021-01357-9
18. Kurose J, Kiuchi K, Fukuzawa K, Takami M, Mori S, Suehiro H, et al. Lesion characteristics between cryoballoon ablation and radiofrequency ablation with a contact force-sensing catheter: late-gadolinium enhancement magnetic resonance imaging assessment. J Cardiovasc Electrophysiol. (2020) 31:2572–81. doi: 10.1111/jce.14664
19. Gisby J, Clarke C, Medjeral-Thomas N, Malik T, Papadaki A, Mortimer P, et al. Longitudinal proteomic profiling of dialysis patients with COVID-19 reveals markers of severity and predictors of death. eLife. (2021) 10:e64827. doi: 10.7554/eLife.64827
20. Field M, Goldstein L, Corriveau K, Khanna R, Fan X, Gold M. Same-day discharge after catheter ablation in patients with atrial fibrillation in a large nationwide administrative claims database. J Cardiovasc Electrophysiol. (2021) 32:2432–40. doi: 10.1111/jce.15193
21. Prasitlumkum N, Cheungpasitporn W, Chokesuwattanaskul R, Kewcharoen J, Tokavanich N, Navaravong L, et al. Comparison between same-day discharge and overnight stay after atrial fibrillation ablation: systematic review and meta-analysis. Pacing Clin Electrophysiol. (2021) 44:2054–66. doi: 10.1111/pace.14380
22. Lund S, Giachelli C, Scatena M. The role of osteopontin in inflammatory processes. J Cell Commun Signal. (2009) 3:311–22.
23. Kiuchi K, Fukuzawa K, Mori S, Watanabe Y, Hirata K. Feasibility of imaging inflammation in the left atrium post AF ablation using PET technology. JACC Clin Electrophysiol. (2017) 3:1466–7. doi: 10.1016/j.jacep.2017.02.004
24. Yang Y, Gao S, Zhang F, Luo W, Xue J, Lei G. Effects of osteopontin on the expression of IL-6 and IL-8 inflammatory factors in human knee osteoarthritis chondrocytes. Eur Rev Med Pharmacol Sci. (2014) 18:3580–6.
25. Uchibori T, Matsuda K, Shimodaira T, Sugano M, Uehara T, Honda T. IL-6 trans-signaling is another pathway to upregulate osteopontin. Cytokine. (2017) 90:88–95. doi: 10.1016/j.cyto.2016.11.006
26. Hurst S, Wilkinson T, McLoughlin R, Jones S, Horiuchi S, Yamamoto N, et al. Il-6 and its soluble receptor orchestrate a temporal switch in the pattern of leukocyte recruitment seen during acute inflammation. Immunity. (2001) 14:705–14. doi: 10.1016/s1074-7613(01)00151-0
27. Asano K, Takahashi N, Ushiki M, Monya M, Aihara F, Kuboki E, et al. Intestinal CD169(+) macrophages initiate mucosal inflammation by secreting CCL8 that recruits inflammatory monocytes. Nat Commun. (2015) 6:7802. doi: 10.1038/ncomms8802
28. Shaath H, Vishnubalaji R, Elkord E, Alajez N. Single-cell transcriptome analysis highlights a role for neutrophils and inflammatory macrophages in the pathogenesis of severe COVID-19. Cells. (2020) 9:2374. doi: 10.3390/cells9112374
29. Bergmann C, Salyer C, Beckmann N, Caldwell C. Intraperitoneal Neutrophil IL-10 production is promoted by interferon gamma in a murine model of sepsis model in the acute phase of sepsis. Biochem Biophys Res Commun. (2020) 530:278–84. doi: 10.1016/j.bbrc.2020.07.089
30. Batko K, Krzanowski M, Gajda M, Dumnicka P, Fedak D, Woziwodzka K, et al. Endothelial injury is closely related to osteopontin and TNF receptor-mediated inflammation in end-stage renal disease. Cytokine. (2019) 121:154729. doi: 10.1016/j.cyto.2019.05.016
31. Montgomery A, Tam F, Gursche C, Cheneval C, Besler K, Enns W, et al. Overlapping and distinct biological effects of IL-6 classic and trans-signaling in vascular endothelial cells. Am J Physiol Cell Physiol. (2021) 320:C554–65. doi: 10.1152/ajpcell.00323.2020
32. Catar R, Witowski J, Zhu N, Lucht C, Derrac Soria A, Uceda Fernandez J, et al. IL-6 trans-signaling links inflammation with angiogenesis in the peritoneal membrane. J Am Soc Nephrol. (2017) 28:1188–99. doi: 10.1681/ASN.2015101169
33. Mateo R, Reichner J, Albina J. Interleukin-6 activity in wounds. Am J Physiol. (1994) 266(6 Pt 2):R1840–4.
34. Antolic B, Pernat A, Cvijic M, Zizek D, Jan M, Sinkovec M. Radiofrequency catheter ablation versus balloon cryoablation of atrial fibrillation: markers of myocardial damage, inflammation, and thrombogenesis. Wien Klin Wochenschr. (2016) 128:480–7. doi: 10.1007/s00508-016-1002-0
35. Bin Waleed K, Yin X, Yang X, Dai B, Liu Y, Wang Z, et al. Short and long-term changes in platelet and inflammatory biomarkers after cryoballoon and radiofrequency ablation. Int J Cardiol. (2019) 285:128–32. doi: 10.1016/j.ijcard.2019.02.054
36. Herrera Siklody C, Deneke T, Hocini M, Lehrmann H, Shin D, Miyazaki S, et al. Incidence of asymptomatic intracranial embolic events after pulmonary vein isolation: comparison of different atrial fibrillation ablation technologies in a multicenter study. JACC. (2011) 58:681–8. doi: 10.1016/j.jacc.2011.04.010
37. Trivedi V, Boire A, Tchernychev B, Kaneider N, Leger A, O’Callaghan K, et al. Platelet matrix metalloprotease-1 mediates thrombogenesis by activating PAR1 at a cryptic ligand site. Cell. (2009) 137:332–43. doi: 10.1016/j.cell.2009.02.018
38. Zhang T, Li Q, Wang L, Li G. Expression variations and clinical significance of MMP-1, MMP-2 and inflammatory factors in serum of patients with deep venous thrombosis of lower extremity. Exp Ther Med. (2019) 17:181–6. doi: 10.3892/etm.2018.6922
39. Marin F, Roldan V, Climent V, Garcia A, Marco P, Lip G. Is thrombogenesis in atrial fibrillation related to matrix metalloproteinase-1 and its inhibitor, TIMP-1? Stroke. (2003) 34:1181–6. doi: 10.1161/01.STR.0000065431.76788.D9
40. Liu S, Tefft B, Roberts D, Zhang L, Ren Y, Li Y, et al. Cardioprotective proteins upregulated in the liver in response to experimental myocardial ischemia. Am J Physiol Heart Circ Physiol. (2012) 303:H1446–58.
41. Hijazi Z, Wallentin L, Lindback J, Alexander J, Connolly S, Eikelboom J, et al. Screening of multiple biomarkers associated with ischemic stroke in atrial fibrillation. J Am Heart Assoc. (2020) 9:e018984.
42. Hajas O, Bagoly Z, Toth N, Urbancsek R, Kiss A, Kovacs K, et al. Intracardiac fibrinolysis and endothelium activation related to atrial fibrillation ablation with different techniques. Cardiol Res Pract. (2020) 2020:1570483. doi: 10.1155/2020/1570483
43. Siegbahn A, Lindback J, Hijazi Z, Aberg M, Alexander J, Eikelboom J, et al. Multiplex protein screening of biomarkers associated with major bleeding in patients with atrial fibrillation treated with oral anticoagulation. J Thromb Haemost. (2021) 19:2726–37.
Keywords: proteomics, bioinformatics, Olink, atrial fibrillation, catheter ablation
Citation: Lin M, Bao Y, Du Z, Zhou Y, Zhang N, Lin C, Xie Y, Zhang R, Li Q, Quan J, Zhu T, Xie Y, Xu C, Xie Y, Wei Y, Luo Q, Pan W, Wang L, Ling T, Jin Q, Wu L, Yin T and Xie Y (2023) Plasma protein profiling analysis in patients with atrial fibrillation before and after three different ablation techniques. Front. Cardiovasc. Med. 9:1077992. doi: 10.3389/fcvm.2022.1077992
Received: 23 October 2022; Accepted: 19 December 2022;
Published: 10 January 2023.
Edited by:
Jedrzej Kosiuk, Helios Clinic Köethen, GermanyReviewed by:
Li-Da Wu, Nanjing Medical University, ChinaCopyright © 2023 Lin, Bao, Du, Zhou, Zhang, Lin, Xie, Zhang, Li, Quan, Zhu, Xie, Xu, Xie, Wei, Luo, Pan, Wang, Ling, Jin, Wu, Yin and Xie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yucai Xie,  ZHJ4aWV5dWNhaUAxNjMuY29t; Tong Yin,
ZHJ4aWV5dWNhaUAxNjMuY29t; Tong Yin,  eWludG9uZzAxMDFAMTYzLmNvbQ==; Liqun Wu,
eWludG9uZzAxMDFAMTYzLmNvbQ==; Liqun Wu,  d3VsaXF1bjg5QGhvdG1haWwuY29t
d3VsaXF1bjg5QGhvdG1haWwuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.