- 1Department of Cardiac Surgery, University Hospital Bonn, Bonn, Germany
- 2Department of Cardiac Surgery, Heart Center Siegburg, Siegburg, Germany
Introduction: Minimally invasive approach in cardiac surgery has gained popularity. In order to reduce surgical trauma in coronary surgery minimally invasive direct coronary artery bypass (MIDCAB) has already been established. This technique has been introduced for revascularisation of isolated left anterior descending (LAD). It can also be performed for hybrid revascularisation procedure in multi-vessel disease.
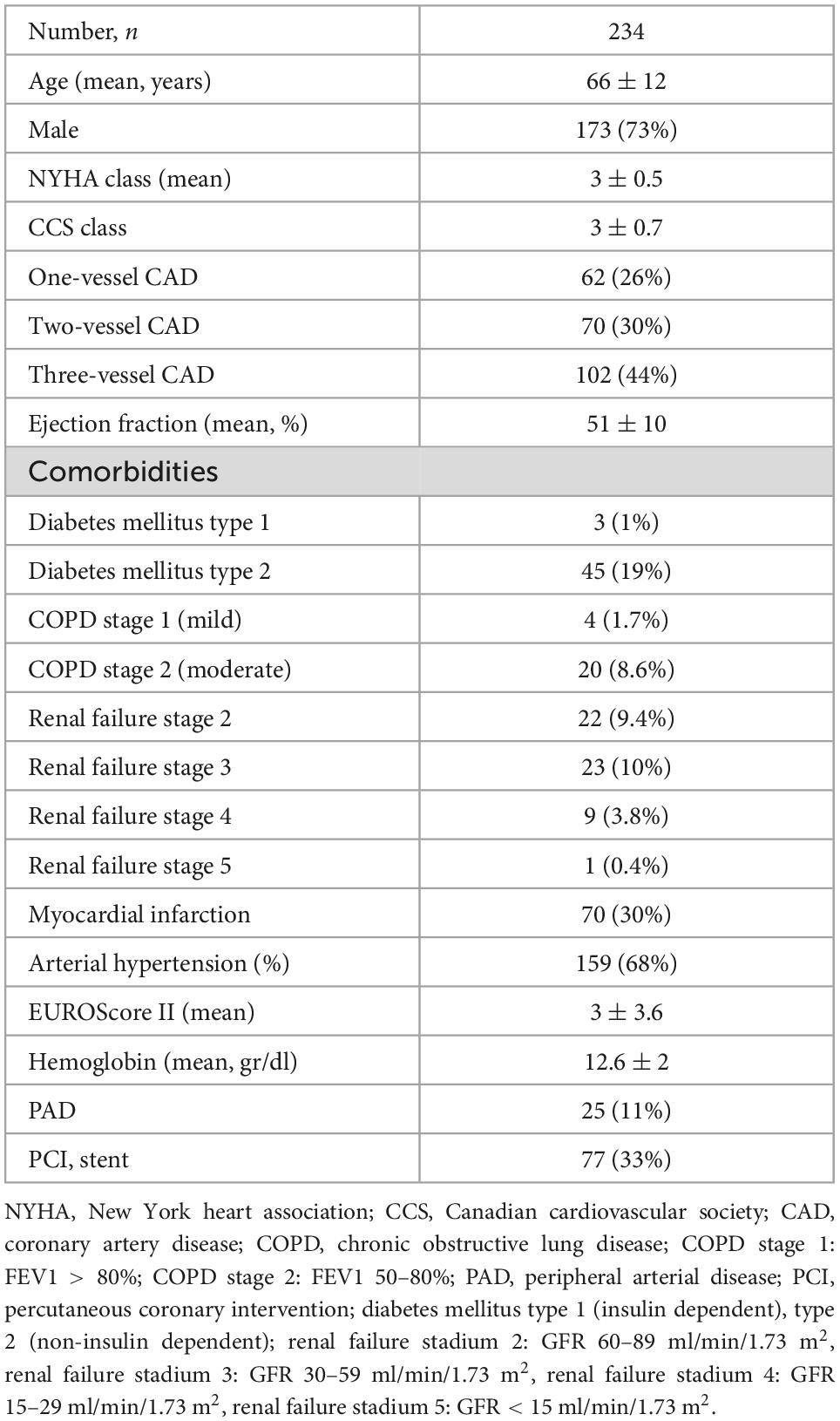
Methods: From 2017 to 2021, 234 patients received MIDCAB operation in our heartcenter 73% were male. Most of the patients had two or three vessel disease (74%). The average age of the patients was 66 ± 12 years mean. The left internal mammary artery (LIMA) was anastomosed to the LAD through left minithoracotomy approach. Multi-vessel MIDCAB (MV-MIDCAB) including two anastomoses (T-graft to LIMA with additional saphenous vein graft) was done in 15% (n = 35).
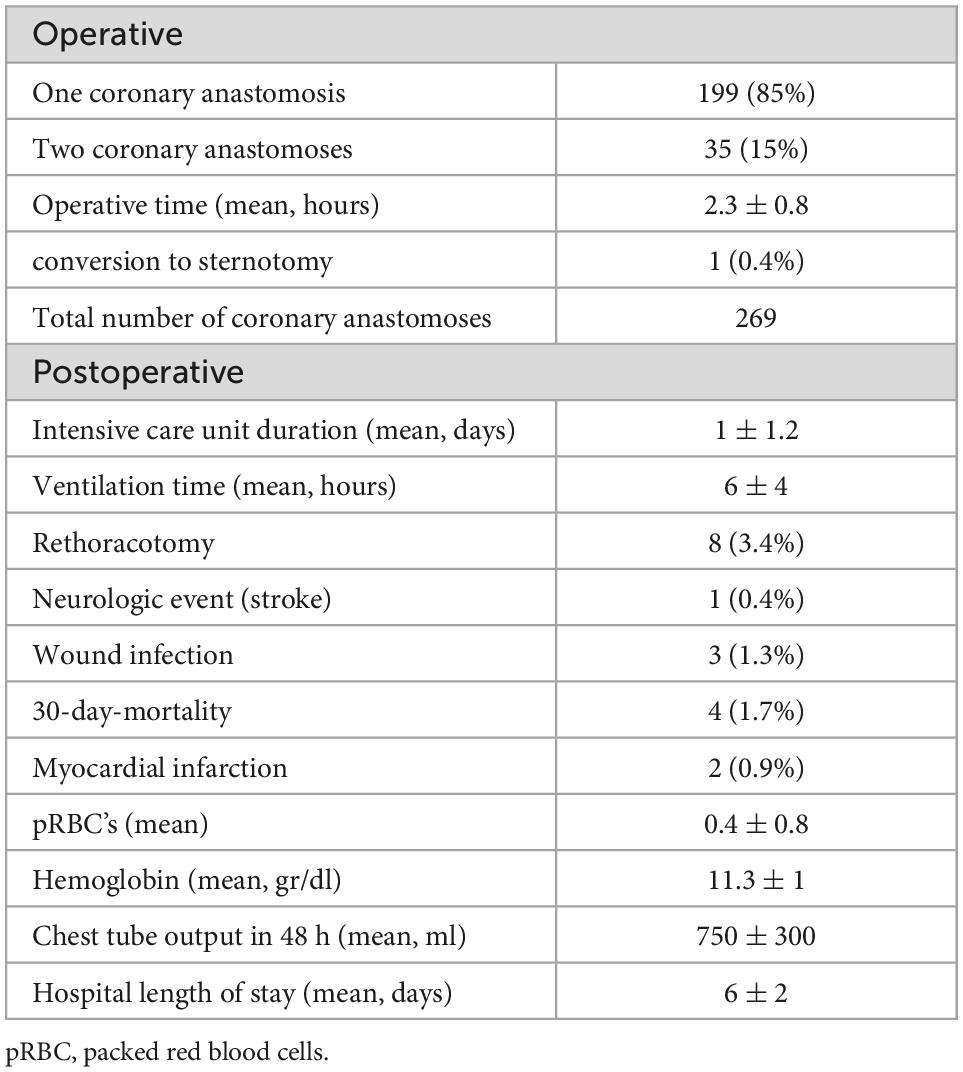
Results: The average operation time was 2.3 ± 0.8 h mean. The 30-day mortality was 1.7% (n = 4). The average amount of packed red blood cells (pRBC) that was given intra- and postoperatively was 0.4 ± 0.8 units mean. The mean intensive care unit stay (ICU) was 1 ± 1.2 days. Three patients (1.3%) had wound infection postoperatively. The rate of neurologic complications was 0.4% (n = 1). Two patients (0.9%) had myocardial infarction and received coronary re-angiography perioperatively including stent implantation of the right coronary artery.
Discussion: The MIDCAB procedure is a safe and less traumatic procedure for selected patients with proximal LAD lesions. It is also an option for hybrid procedure in multi-vessel disease. The ICU stay and application of pRBC’s are low. Our MIDCAB results show a good postoperative clinical outcome. However, follow-up data are necessary to evaluate long-term outcome.
Introduction
Minimally invasive cardiac surgery for the treatment of valve disease is well-established. Coronary artery bypass grafting (CABG) via minimally invasive approach is an outstanding evolution in cardiac surgery. Since the first beating heart anastomosis was described by Kollesov in 1967 (1) the Off-pump bypass surgery technique has been developed continuously during the past decades. Minimally invasive direct coronary artery bypass (MIDCAB) grafting was presented in the 1990s by Calafiore and Subramanian (2, 3). Today it is an important part of the cardiac surgery armamentarium in centers of excellence. MIDCAB procedure is a revascularization strategy for the treatment of left anterior descending (LAD) disease. It can also be applied as a hybrid coronary revascularization (HCR) in the setting of incomplete surgical revascularization for high-risk patients. These patients usually undergo postoperative interventional percutaneous coronary intervention (PCI). In selected patients multi-vessel MIDCAB is feasible to treat lesions of LAD, diagonal branch or circumflex artery. Less surgical trauma, reduced operative bleeding, and fast recovery are associated with MIDCAB approach (4–6). Despite the advantages of MIDCAB procedure this technique has not been widespread in the routine cardiac surgery field. It might be related to the fact that MIDCAB remains technically challenging due to limited access to the surgical situs and limitation of exposure of the heart (5). Another reason could be that CABG and PCI are indexed for class IA category for treatment of isolated proximal LAD lesions in the guidelines on myocardial revascularization (7). Therefore the desicions of heartteams play an important role to enclose the suitable patients for this minimally invasive procedure.
Patients and methods
Study population
From 2017 to 2021, 234 patients underwent MIDCAB procedure in Heartcenter Siegburg and University Hospital Bonn. 27% were female. The majority of patients had two or three vessel disease (74%). Patients’ mean age was 66 ± 12 years. The left internal mammary artery (LIMA) was anastomosed to the LAD via left minithoracotomy approach in all patients. MV-MIDCAB with two anastomoses (additional saphenous vein graft as T-graft to LIMA) was performed in 35 patients (15%). The patients’ preoperative characteristics are summarized in Table 1.
This retrospective study was approved by the local ethics committee (#446/21).
Patient selection criteria
Suitable patients for MIDCAB were discussed in a heartteam for the surgical/hybrid procedure. Inclusion criteria were significant stenosis or occlusion of the proximal or medial LAD for single vessel revascularization. The diagonal branch or ramus intermedius were targets for multi-vessel revascularization. For HCR the right coronary artery and/or circumflex artery were treated with PCI postoperatively. Exclusion criteria were former chest radiation or left thoracotomy (for lung or breast surgery), stenosis of the left subclavian artery, emergency operation, and/or hemodynamically instable patients, or redo CABG.
Surgical technique
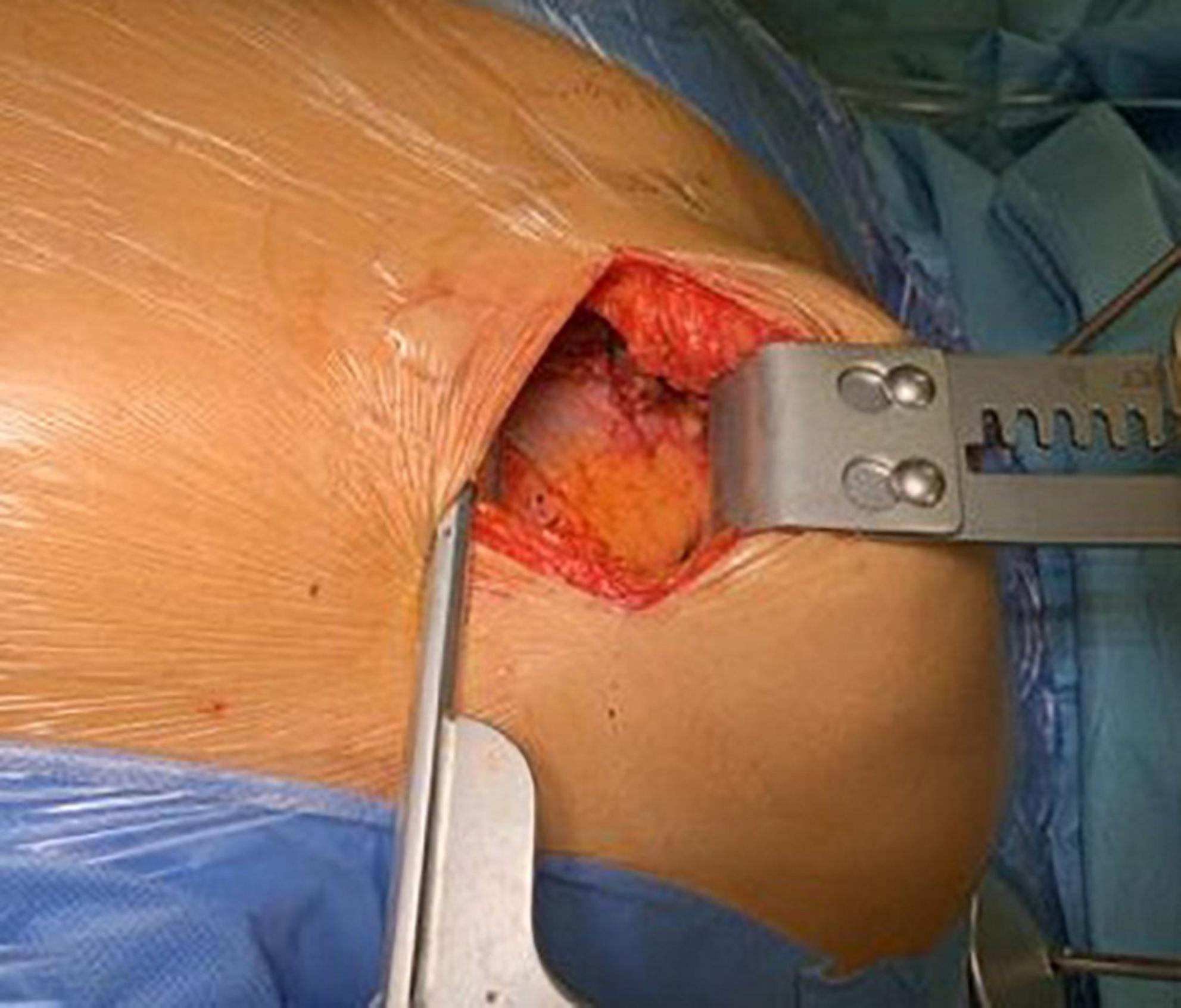
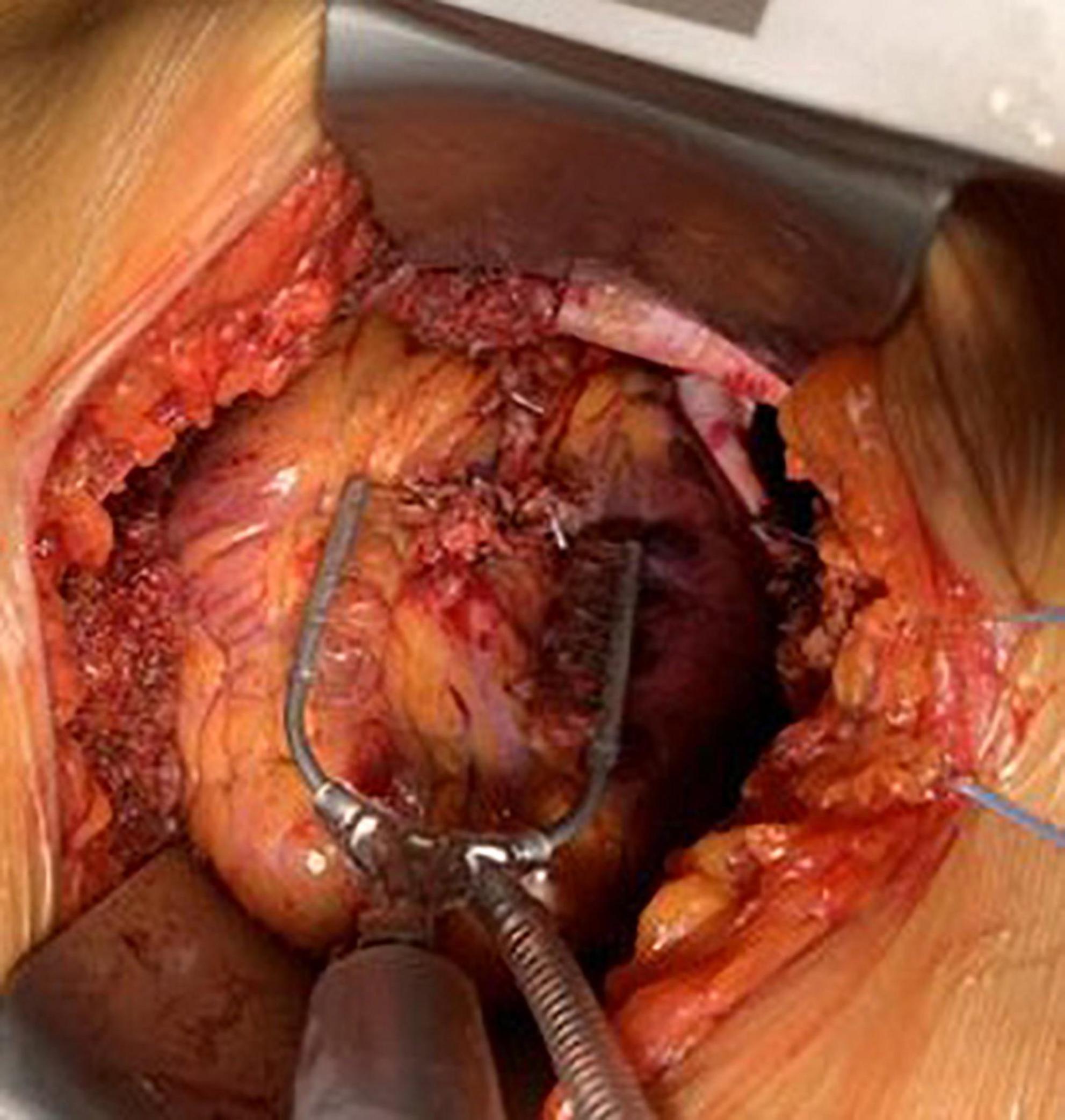
Patients were placed in a supine position, with 30° elevation of the left thorax. Intubation was established with a double-way endotracheal tube. A 5–8 cm long left submammary or supramammary skin incision was done, and the left pleural space was entered through the 4th or 5th intercostal space. The left lung was deflated. With the help of a MICS retractor for LIMA (lifting retractor, Geister, Tuttlingen, Germany) a pedicled LIMA graft was harvested (Figure 1). Systemic heparinization was initiated, the pericardium was opened, and the LAD was identified. The distal anastomosis was performed Off-pump with the help of a vacuum tissue stabilizer (Octopus Evolution, Medtronic, Minneapolis, USA) and an intracoronary shunt (Medtronic, Minneapolis, USA). A traction suture with tourniquet was placed with 4/0 polypropylene to the proximal part of the LAD. Air/saline insufflation was used to achieve a bloodless operation field. Bypass flow was measured routinely intraoperatively. In MV-MIDCAB a small segment of saphenous vein was harvested from the lower leg. The venous graft was anastomosed to the target vessel in a same manner. Finally the proximal anastomosis (T-Graft to LIMA) was performed. If necessary a heart positioner was applied for better exposition (Starfish Evo, Medtronic, Minneapolis, USA). Protamin was administered 1:1, a thorax drain was placed into the left pleura and thoracotomy was closed.
Statistical analysis
Statistical analyses were calculated with the biometrically analysis of sampling software (BIAS 11.06, Frankfurt, Germany). Categorical data were presented as percentages and continuous data were illustrated as mean value ± standard deviation.
Results
The majority of patients (85%) received single bypass LIMA to LAD in MIDCAB technique (Figure 2). A total of 15% underwent MV-MIDCAB with LIMA to LAD and saphenous vein (T-Graft) to the diagonal branch (Figure 3). The operative and perioperative results are illustrated in Table 2. The mean operation time was 2.3 ± 0.8 h. Conversion to sternotomy was necessary in one patient (0.4%) who had myocardial ischemia postoperatively. The RCA could not be treated with PCI. Therefore the patient underwent sternotomy for additional bypass to the right coronary artery (RCA) at the first postoperative day. The applied amount of packed red blood cells (pRBC) were 0.4 ± 0.8 units. The average intensive care unit stay (ICU) were 1 ± 1.2 days. One patient (0.4%) presented with a minor stroke postoperatively. Myocardial infarction was observed in two patients (0.9%) who underwent coronary re-angiography perioperatively and stent intervention of the right coronary artery. There was no operative death. The 30-day mortality was 1.7% (n = 4). Cause of death were multi organ failure (n = 1), low output syndrome (n = 2), and sepsis due to pneumonia (n = 1). Rethoracotomy for bleeding (via left thoracotomy approach) was necessary in eight patients (3.4%). Wound revision due to superficial wound infection was required in three patients (1.3%).
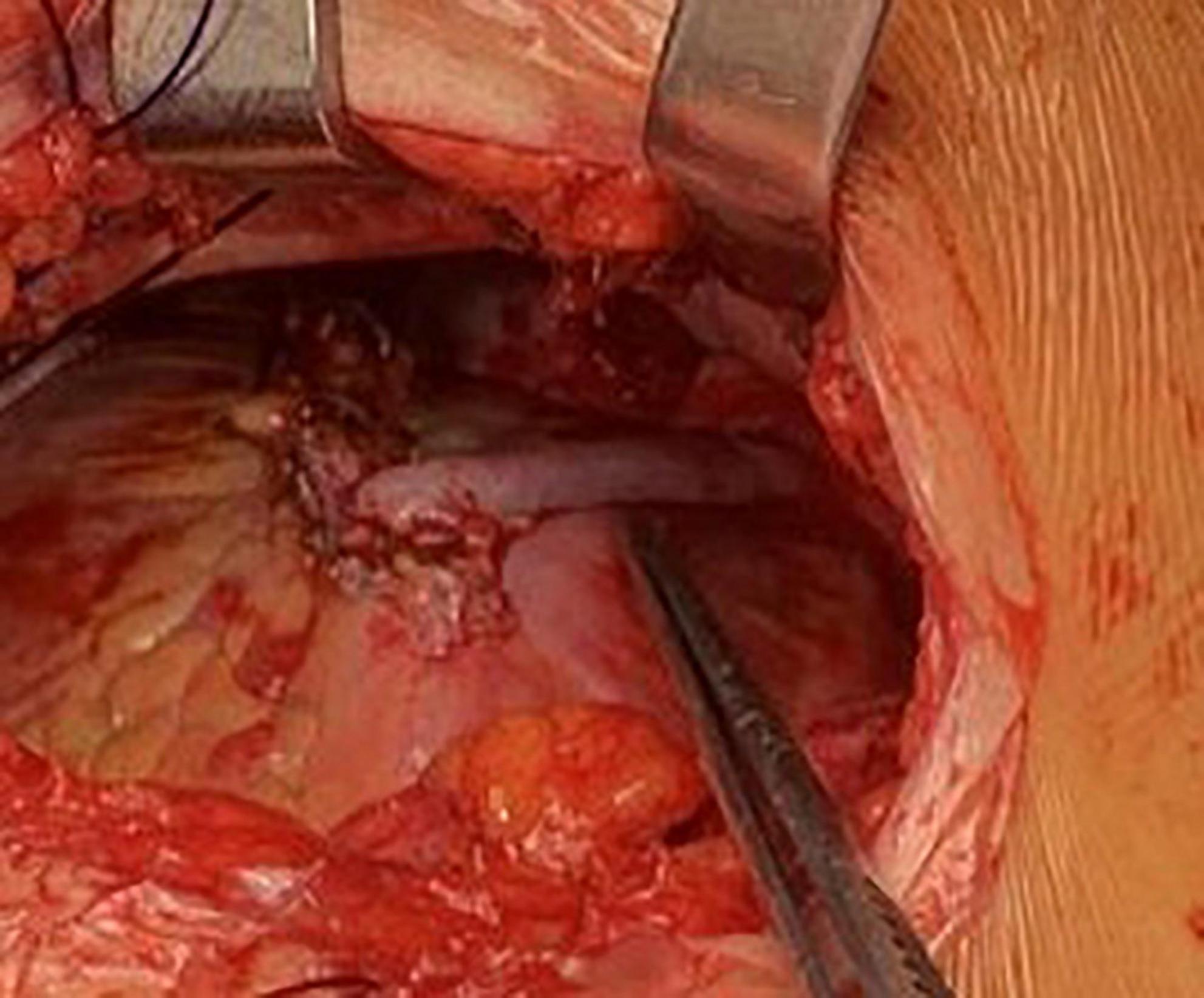
Figure 3. Multivessel-MIDCAB, LIMA, to LAD and saphenous vein (T-graft) to diagonal branch anastomoses.
Discussion
Minimally invasive direct coronary artery bypass procedure offers a good solution for patients with isolated proximal LAD stenosis. The avoidance of sternotomy and cardiopulmonary bypass (CPB) in the MIDCAB setting has been associated with faster recovery, less bleeding, and fewer transfusions (8). An important strategy for MIDCAB revascularization is a careful patient selection that should be discussed in a heartteam. A LAD diameter < 1.5 mm, diffuse disease, or intramural position of the LAD are reported to be exclusion criteria for MIDCAB (9). Also unfavorable anatomical conditions like obesity, former chest radiation, left thoracotomy (for lung or breast surgery), or stenosis of the left subclavian artery make MIDCAB unsuitable for these patients. Emergent cases and/or hemodynamically instable patients should be also excluded. In the early beginning of the MIDCAB era this technique was predominantly applied in patients with isolated lesions of the LAD. Nowadays it is an attractive option for HCR in multi vessel disease particularly in high-risk patients with several comorbidities. MIDCAB for HCR is reported to be associated with a favorable clinical outcome including lower major adverse cardiovascular and cerebral events (MACCE) and repeat revascularization rates compared with multivessel PCI (10). In our series 40% of the patients underwent HCR. The 30-day mortality was 1.7% (n = 4) that is comparable to the published data of other centers (5, 10–12). Conversion to sternotomy (without cardiopulmonary bypass) was necessary in one patient (0.4%) that is acceptable and similar to published data (5, 10). We observed one (0.4%) neurological event (minor stroke) postoperatively that is low. The applied amount of pRBC were 0.4 ± 0.8 units. The average ICU stay was 1 ± 1.2 days that is short. These findings are similar to the reported results of other MIDCAB performing centers regarding less required blood transfusions and a short ICU stay (5, 13). Although MIDCAB is a challenging technique, it can be performed safely with low complication rates by experienced Off-pump coronary artery bypass (OPCAB) surgeons (11, 13, 14). In selected patients MIDCAB procedure is a good revascularization strategy as described in the following studies. Indja et al. reported that MIDCAB for LAD remains superior to first- or second-generation PCI with DES regarding long-term freedom from myocardial infarction and survival (15). Aziz et al. presented a meta-analysis including 12 studies (1,952 patients) comparing MIDCAB with PCI for single vessel LAD revascularization (16). They could show that there was a higher rate of recurrent angina, need for repeat revascularization and incidence of MACCE with PCI at midterm follow up. Blazek et al. reported the 10-year follow-up results of a randomized trial comparing MIDCAB with bare-metal stenting for stenosis of the LAD (17). They found out that there were no significant differences in the endpoints death and myocardial infarction. However, a significant higher repeat target vessel revascularisation rate was observed in the PCI group (34 vs. 11%, p < 0.01). Similar results are described in the propensity matched study of Hannan et al. (18). They observed a significantly lower repeat revascularization rate in patients undergoing CABG vs. PCI with DES (7.09 vs. 12.98%, p = 0.0007) in isolated proximal LAD disease at 3-years follow-up. The decision of heartteams plays an important role to enclose the suitable patients for this minimally invasive procedure. There are only a few studies dealing with benefits and late outcomes of heartteam decisions regarding patients with CAD. Domingues et al. report about their experience regarding heartteam recommendations for 1,000 patients with CAD (19). They observed a 5-year mortality rate of 3% for patients with 1 vessel disease with or without proximal LAD involvement. Despite the heartteam recommendation was largely in accordance with the clinical guidelines the timing for treatment could have been further optimized (19). It is mandatory to set up a multidisciplinary heartteam to determine criteria moving a patient for MIDCAB approach. The surgical view regarding the feasibility of minimally invasive approach with/without hybrid strategy in CAD is essential. Therefore the role of cardiac surgeons in heartteam meetings is crucial. The advantage of a hybrid procedure is the revascularization of multiple territories without a large surgical trauma. To set an example, the RCA territory can be treated with PCI afterward MIDCAB LIMA to LAD has been performed. In the most cases it is not possible to reach the RCA via left minithoracotomy in off-pump technique. The rate of hybrid procedures in CAD is increasing. Van den Eynde et al. published the results of a systematic review and meta-analysis regarding HCR versus PCI in 27041 patients (20). They observed that HCR was associated with significantly lower rates of myocardial infarction and target vessel revascularization in comparison to PCI. Therefore HCR strategy is gaining popularity in many experienced heart centers as it is a valid alternative to multivessel PCI.
Minimally invasive cardiac surgery can compete with interventional cardiology and offers outstanding results. Although MIDCAB is technically demanding our postoperative results demonstrate that this procedure is safe and feasible (21). Optimal patient selection and an experienced surgical team are mandatory.
Minimally invasive direct coronary artery bypass for selected patients with proximal LAD lesions and in multi-vessel disease is a safe procedure with a low 30-day mortality and good clinical outcome. Intra- and perioperative application of pRBC’s and ICU stay are low. The trauma and incision is small with a good cosmetic result. However, long-term clinical follow up data are necessary to strengthen our thesis.
Limitations
The study has a retrospective design. A control group, e.g., On-pump CABG, was not added. Follow-up data are not included yet as further investigations are ongoing.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the University Hospital Bonn. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
NM and EA analyzed the data. NM, EA, and SS structured the manuscript giving contribute to tables, figures, and text editing. FB revisited the article implementing the final manuscript form. All authors contributed to the manuscript production and in the final revision.
Acknowledgments
The abstract of this manuscript was presented in part at the annual meeting of the German Society of Thoracic-, Heart- and Vascular Surgery in February 2022 (21).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kolessov V. Mammary artery-coronary artery anastomosis as method of treatment for angina pectoris. J Thorac Cardiovasc Surg. (1967) 54:535–44. doi: 10.1016/S0022-5223(19)43061-4
2. Calafiore A, Di Giammarco G, Teodori G, Brosco G, DÀnnunzio E, Barsotti A, et al. Left anterior descending coronary artery grafting via left anterior small thoracotomy without cardiopulmonary bypass. Ann Thorac Surg. (1996) 61:1658–65. doi: 10.1016/0003-4975(96)00187-7
3. Subramanian V, McCabe J, Geller C. Minimally invasive direct oronary artery bypass grafting: two-year clinical experience. Ann Thorac Surg. (1997) 64:1648–53. doi: 10.1016/s0003-4975(97)01099-0
4. Al-Ruzzeh S, Mazrani W, Wray J, Modine T, Nakamura K, Bustami M, et al. The clinical outcome and quality of life following minimally invasive direct coronary artery bypass surgery. J Card Surg. (2004) 19:12–6. doi: 10.1111/j.0886-0440.2004.04003.x
5. Tekin A, Arslan Ü. Perioperative outcomes in minimally invasive direct coronary artery bypass versus off-pump coronary artery bypass with sternotomy. Videosurg Miniinv. (2017) 12:285–90. doi: 10.5114/wiitm.2017.67679
6. Yang M, Xiao L, Gao Z, Zhou J. Clinical effect and prognosis of off-pump minimally invasive direct coronary artery bypass. Med Sci Monit. (2017) 23:1123–8. doi: 10.12659/msm.902940
7. Neumann F, Sousa-Uva M, Ahlsson A, Alfonso F, Banning A, Benedetto U, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. (2019) 40:87–165. doi: 10.1093/eurheartj/ehy394
8. Ruel M, Une D, Bonatti J, McGinn J. Minimally invasive coronary artery bypass grafting: is it time for the robot? Curr Opin Cardiol. (2013) 28:639–45. doi: 10.1097/HCO.0b013e3283653fd1
9. Diegeler A, Matin M, Falk V, Binner C, Walther T, Autschbach R, et al. Indication and patient selection in minimally invasive and “off-pump” coronary artery bypass grafting. Eur J Cardiothorac Surg. (1999) 16:S79–82. doi: 10.1016/s1010-7940(99)00194-3
10. Harskamp R. Current state and future direction of hybrid coronary revascularization. Curr Opin Cardiol. (2015) 30:643–9. doi: 10.1097/HCO.0000000000000223
11. Cremer J, Schoettler J, Thiem A, Grothusen C, Hoffmann G. The MIDCAB approach in its various dimensions. HSR Proc Intensive Care Cardiovasc Anesth. (2011) 3:249–53.
12. Endo Y, Nakamura Y, Kuroda M, Ito Y, Hori T. The utility of a 3D endoscope and robot-assisted system for MIDCAB. Ann Thorac Cardiovasc Surg. (2019) 25:200–4. doi: 10.5761/atcs.oa.18-00254
13. Van Praet K, Kofler M, Nazari Shafti T, Abd El Al A, van Kampen A, Amabile A. Minimally invasive coronary revascularisation surgery: a focused review of the available literature. Interv Cardiol. (2021) 16:e08. doi: 10.15420/icr.2021.05
14. Detter C, Reichenspurner H, Boehm D, Thalhammer M, Raptis P, Schütz A, et al. Minimally invasive direct coronary artery bypass grafting (MIDCAB) and off-pump coronary artery bypass grafting (OPCAB): two techniques for beating heart surgery. Heart Surg Forum. (2002) 5:157–62.
15. Indja B, Woldendorp K, Black D, Bannon P, Wilson M, Vallely M. Minimally invasive surgical approaches to left main and left anterior descending coronary artery revascularization are superior compared to first- and second-generation drug-eluting stents: a network meta-analysis. Eur J Cardiothorac Surg. (2020) 57:18–27. doi: 10.1093/ejcts/ezz184
16. Aziz O, Rao C, Singh Panesar S, Jones C, Morris S, Darzi A, et al. Meta-analysis of minimally invasive internal thoracic artery bypass versus percutaneous revascularisation for isolated lesions of the left anterior descending artery. BMJ. (2007) 334:617. doi: 10.1136/bmj.39106.476215.BE
17. Blazek S, Holzhey D, Jungert C, Borger M, Fuernau G, Desch S, et al. Comparison of bare-metal stenting with minimally invasive direct bypass surgery for stenosis of the left anterior descending coronary artery: 10-year follow-up of a randomized trial. JACC Cardiovasc Interv. (2013) 6:20–6. doi: 10.1016/j.jcin.2012.09.008
18. Hannan E, Zhong Y, Walford G, Holmes D, Venditti F, Berger P, et al. Coronary artery graft bypass surgery versus drug-eluting stent for patients with isolated proximal left anterior descending disease. JACC. (2014) 64:2717–26. doi: 10.1016/j.jacc.2014.09.074
19. Domingues C, Milojevic M, Thuijs DJ, Van Mieghem N, Daemen J, Van Domburg R, et al. Heart team decision making and long-term outcomes for 1000 consecutive cases of coronary artery disease. Interact Cardiovasc Thorac Surg. (2019) 28:206–13. doi: 10.1093/icvts/ivy237
20. Van den Eynde J, Pompeu Sa M, De Groote S, Amabile A, Sicouri S, Ramlawi B. Hybrid coronary revascularization versus percutaneous coronary intervention: a systematic review and meta-analysis. Int J Cardiol Heart Vasc. (2021) 37:100916. doi: 10.1016/j.ijcha.2021.100916
Keywords: minimally invasive, off-pump surgery, minithoracotomy, hybrid procedure, left anterior descending
Citation: Monsefi N, Alaj E, Sirat S and Bakhtiary F (2023) Postoperative results of minimally invasive direct coronary artery bypass procedure in 234 patients. Front. Cardiovasc. Med. 9:1051105. doi: 10.3389/fcvm.2022.1051105
Received: 22 September 2022; Accepted: 22 December 2022;
Published: 10 January 2023.
Edited by:
Nikolaos Bonaros, Medical University of Innsbruck, AustriaReviewed by:
Pietro Giorgio Malvindi, Marche Polytechnic University, ItalyCem Alhan, Acıbadem University, Turkey
Copyright © 2023 Monsefi, Alaj, Sirat and Bakhtiary. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nadejda Monsefi,  bmFkZWpkYS5tb25zZWZpQHVrYm9ubi5kZQ==
bmFkZWpkYS5tb25zZWZpQHVrYm9ubi5kZQ==
 Nadejda Monsefi
Nadejda Monsefi Eissa Alaj
Eissa Alaj Sami Sirat2
Sami Sirat2