
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Cardiovasc. Med., 10 January 2023
Sec. Coronary Artery Disease
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.1036274
This article is part of the Research TopicCase Reports in Coronary Artery Disease: 2022View all 10 articles
 Qiang Niu1†
Qiang Niu1† Yunhe Zhao1†
Yunhe Zhao1† Haiying Li1
Haiying Li1 Qilei Wang1
Qilei Wang1 Haijun Zhu1
Haijun Zhu1 Chenglong Bi1
Chenglong Bi1 Hui Zhang1
Hui Zhang1 Jian Wang1
Jian Wang1 Cheng Cheng1
Cheng Cheng1 Beibei Song1
Beibei Song1 Chengwei Jin1
Chengwei Jin1 Ming Lv2*
Ming Lv2* Bo Li1*
Bo Li1*The right coronary artery (RCA) originating from the left anterior descending artery (LAD) is a very rare variation of coronary artery anomaly. This kind of anomaly is usually considered to be clinically benign. Here, we present an acute myocardial infarction patient with a single coronary artery (SCA), in whom the LAD and RCA are both occlusive at the same time. He suffered from ventricular fibrillation, cardiogenic shock, and severe bradyarrhythmias many times. Fortunately, this patient survived from death through our effective medical procedures.
Coronary artery anomalies are present at birth, and they are relatively uncommon findings in coronary angiography. Rarely, only one coronary artery originates from the aortic trunk supplying the entire heart; as a rare variation, a single coronary artery (SCA) arises from the left sinus of Valsalva, and the right coronary artery (RCA) originates from the left anterior descending artery (LAD) (1, 2). This kind of anomaly is usually considered to be clinically benign (1). Here, we report the case of a patient with acute myocardial infarction and a SCA in whom the LAD and RCA were both occluded at the same time. This report is the first such an anomaly associated with a variety of serious complications. The patient underwent percutaneous coronary intervention two times to the LAD/RCA bifurcated lesion and finally completed revascularization half a year after symptom onset.
The patient was a 76-year-old man with a history of cerebral infarction. He was admitted to the emergency room because of sudden and severe chest pain over the previous 3 h. The first electrocardiography showed obvious ST elevation in V2–V4 (Figure 1), and his troponin I level was > 80 pg/ml, which exceeded the laboratory’s testing limit. The first blood pressure was 67/40 mmHg, and a high dose of dopamine and noradrenaline is used to maintain adequate blood pressure. Then, the patient suffered from sudden cardiac arrest and ventricular fibrillation several times, and chest compressions and electric defibrillation were performed urgently over the course of diagnosis and treatment. We decided to perform emergency coronary angiography. During coronary angiography, the left coronary ostium was located normally. Selective left coronary angiography demonstrated a normal left main coronary artery, ostial LAD occlusion, and 40% ostial left circumflex artery (LCX) lesions (Figure 2A). Multiple attempts to cannulate the right coronary ostium were unsuccessful. As the blood pressure could not be maintained merely depending on the use of vasopressor drugs, intra-aortic balloon pump (IABP) was performed to hold the blood pressure and prevent ischemia-reperfusion injury.
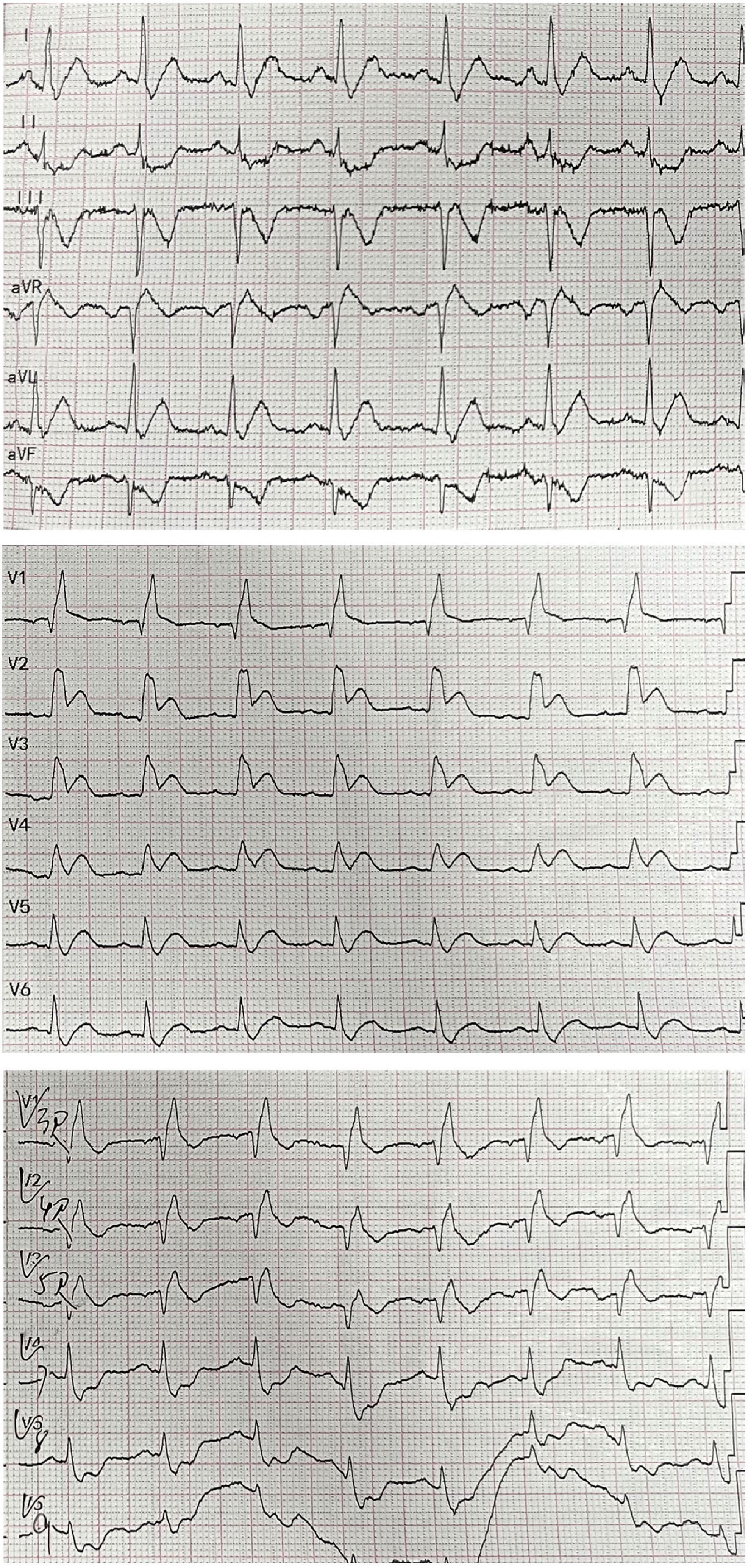
Figure 1. A 18-lead electrocardiogram of the patient showing ST elevation in V2–V4 leads with widespread inverted T-waves in inferior, posterior, and right ventricular leads.
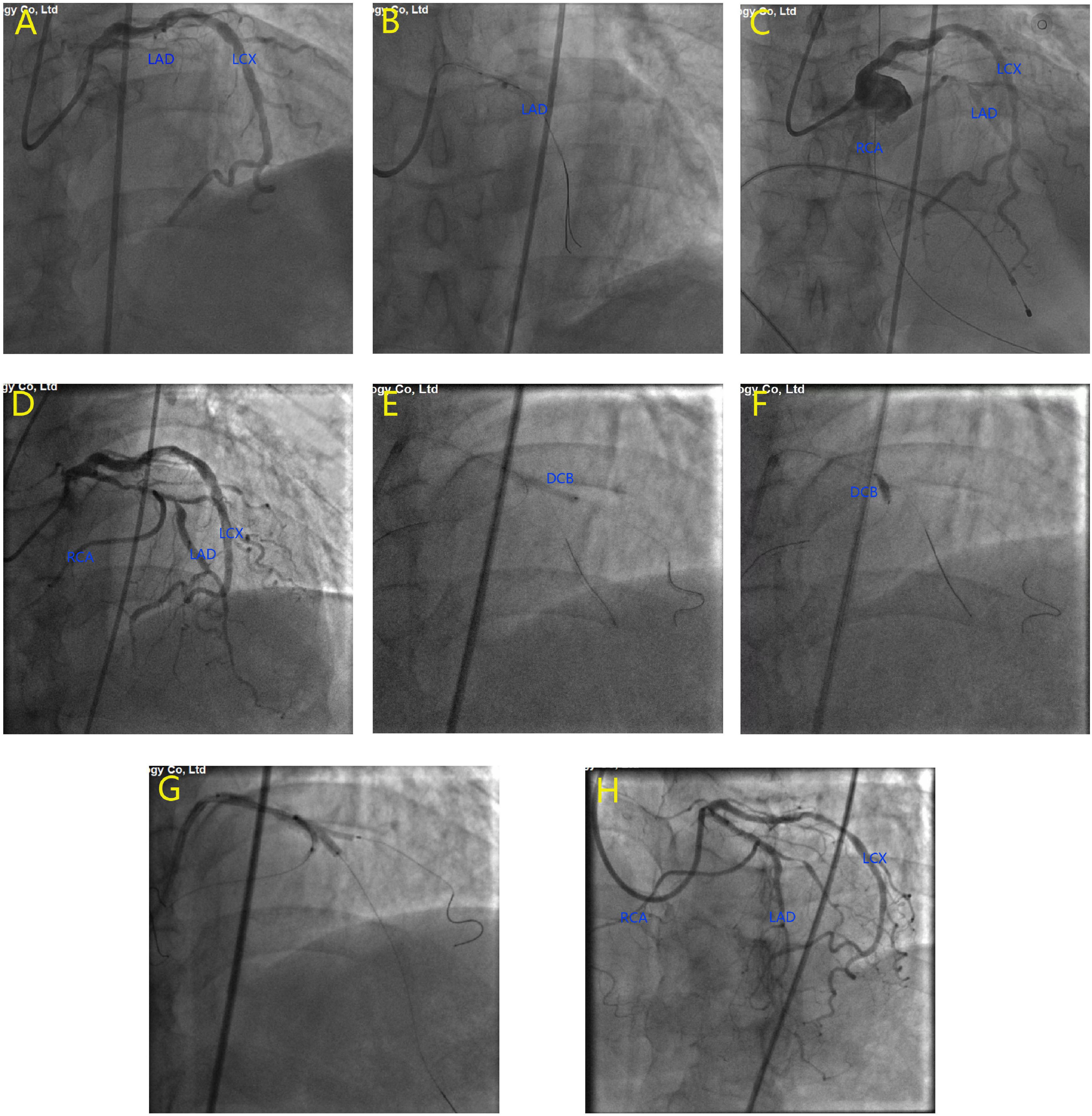
Figure 2. Emergency coronary angiography at the onset of acute myocardial infarction. The results showed that the proximal left anterior descending artery (LAD) was completely occluded (A). Balloon dilatation was performed on the occlusive site (B). TIMI grade 3 flow was restored in LAD and right coronary artery (RCA) (C). The second coronary angiography at 4 months after myocardial infarction. The results showed high-grade lesion at the proximal LAD, as well as at LAD/RCA bifurcation and LAD/diagonal bifurcation (D). Drug-eluting balloons were used to dilate the diagonal branch (E) and the RCA (F). A drug-eluting stent in LAD and 2 balloons in D1 and RCA were dilated simultaneously for kissing balloon inflation (G). Final imaging results after procedure (H).
With the aid of IABP, a guide wire was used to cross the occluding lesion of the LAD, and TIMI grade 3 blood flow was achieved after balloon angioplasty. We found that the left circumflex is the dominant artery and RCA originated from the middle of the LAD (Figures 2B, C). As the ECG monitor showed a ventricular rate of 36 and iii° AV block occurred, we performed a temporary pacemaker. Due to massive thrombosis in the coronary arteries and unstable vital signs, we decided to stop the operation and initiate intensive antithrombotic therapy. After 2 weeks of therapy, the patient’s vital signs stabilized, his chest pain disappeared, and his heart failure improved. We gradually removed the IABP, temporary pacemaker, and vasopressors. Then, coronary artery bypass surgery (CABG) or re-percutaneous coronary intervention (PCI) was recommended for the patient, but he and his family rejected this recommendation.
Four months after discharge, the patient was advised again to undergo coronary angiography, and the results showed complex and severe triple bifurcated lesions, with 90% ostial LAD lesions, 80% ostial D1 lesions, and 70% ostial RCA lesions (Figure 2D). Following coronary angiography, we discussed the revascularization strategy. Two Sion blue wires were passed down the LAD, D1, and anomalous RCA, and two 2.5 × 20 mm drug-coated balloons were deployed in the D1 and RCA (Figures 2E, F). Then, the LAD/RCA/D1 bifurcation was treated with a 3.0 × 36 mm (10 atm) drug-eluting stent (DES) placed in the LAD and two Maverick 2.0 × 20 mm (6 atm) balloons placed in the D1 and RCA (Figure 2G), which were dilated simultaneously for kissing balloon inflation. Then, a proximal optimization technique (POT) was performed with a Quantum Maverick 3.0 × 15 mm high-pressure balloon placed in the LAD. With no symptoms of discomfort, PCI was completed, and the outcomes were satisfactory (Figure 2H). After 3 days, the patient was discharged home on aspirin, ticagrelor, and rosuvastatin. After a 1-month follow-up, we performed computed tomography angiography (CTA) of the coronary artery. Through CTA, we confirmed that the anomalous RCA originated from the middle of the LAD (Figure 3). It passed between the aorta and pulmonary artery in the group of L-II variants (1).
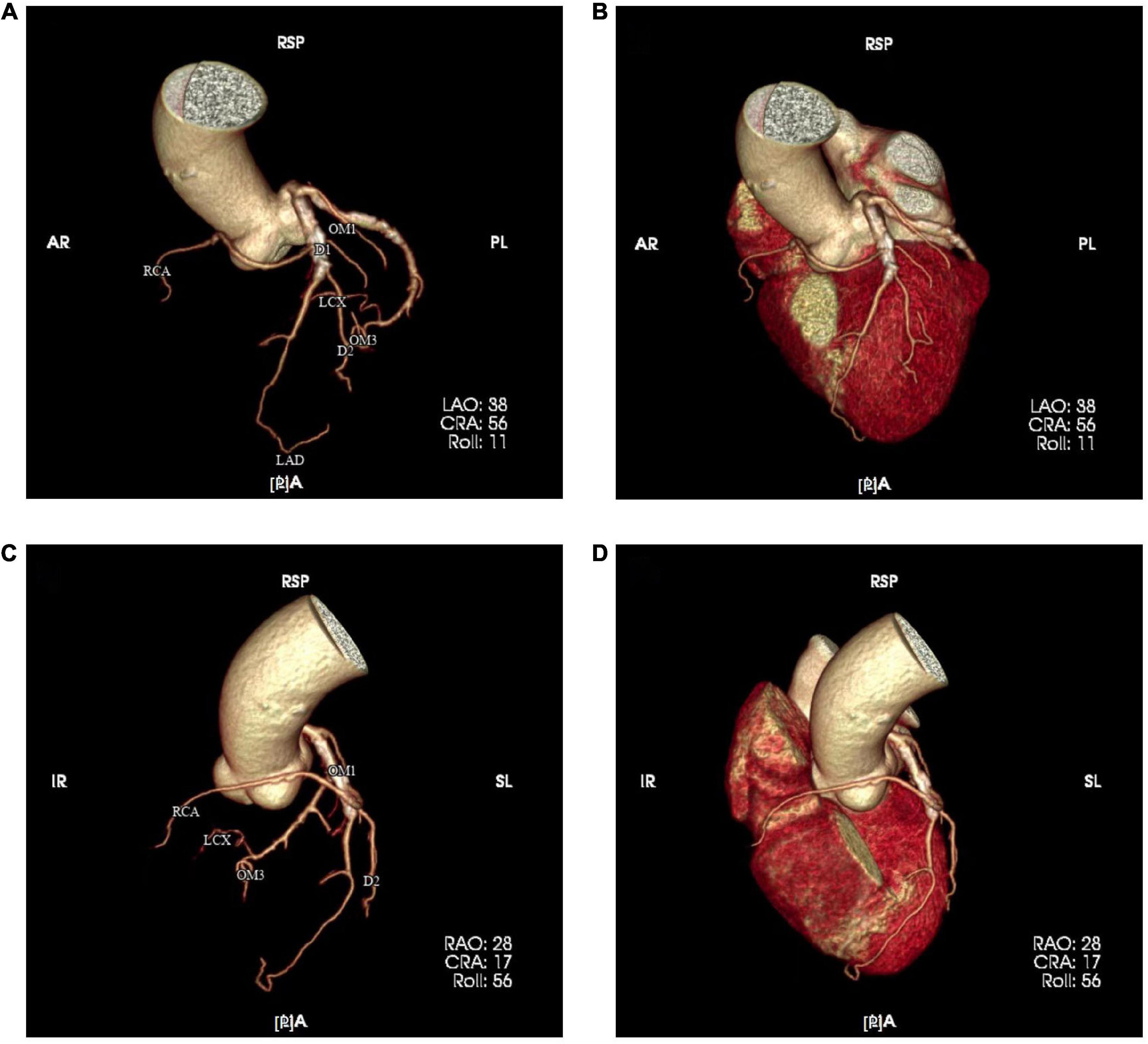
Figure 3. Coronary computed tomography angiography (CTA) was re-examined one month after PCI and resulting images (A–D) confirmed the anomalous origin of the right coronary artery.
In previous studies, we learned that approximately 1.3% of the population has coronary artery anomalies (1), and these anomalies are found in 0.2 to 1.3% of patients undergoing coronary angiography and 0.3% of autopsy series (3). Coronary artery anomalies are considered to be the second most common cause of sudden cardiac death among young athletes. While an SCA, first defined by Hyrtl in (4), is a rare congenital anomaly, it occurs in approximately 0.024 to 0.066% of individuals (5). The first antemortem diagnosis was made by means of coronary angiography in 1967 (6).
To date, an increasing number of associated cases of an SCA have been reported, including an SCA arising from the LSV or RSV. Most of the published SCA case reports describe an RCA originating from the proximal or middle segment of the LAD, and this kind of anomaly was well-recognized as being clinically benign (1). Besides that, when the anomalous coronary artery courses between the aorta and pulmonary trunk, it is considered a malignant course and may cause sudden death (7). Here, we present a symptomatic case associated with the RCA originating from the LAD, and we did not find a similar case by searching PubMed. In such patients, LAD stenosis will also influence blood flow in the RCA. In the worst-case scenario, LAD stenosis can instantly cause simultaneous occlusion of both the LAD and RCA, resulting in a high risk of death and a poor prognosis. This 76-year-old man suffered from ventricular fibrillation, cardiogenic shock, and severe bradyarrhythmia many times throughout the diagnostic and treatment process; thus, this patient experienced all serious adverse events associated with LAD stenosis. Fortunately, this patient survived with the use of IABP, a temporary cardiac pacemaker, and an emergency operation. Many people survive such a complicated lesion. Selective revascularization was performed with DES and DCB 4 months later, and the patient was discharged from the hospital. We will continue to pay attention to the patient’s prognosis in the future.
Once a coronary artery anomaly is found in a patient, it is recommended that early preventive or even early treatment measures must be taken if there are lesions with a common origin, as seen in this patient. As the common origin is equivalent to LM, in the case of occlusion, the consequences would be severe and possibly fatal.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Yamanaka O, Hobbs R. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. (1990) 21:28–40. doi: 10.1002/ccd.1810210110
2. Villa RB, Morís C, Muñiz AL, Hernández LC, Román LS, Alvarez VB, et al. Anomalías congénitas de las arterias coronarias del adulto descritas en 31 años de estudios coronariográficos en el principado de asturias: principales características angiográficas y clínicas. Rev Esp de Cardiol. (2001) 54:269–81.
3. Balghith M. Anomalous origin of the right coronary artery from the proximal left anterior descending artery and a single coronary artery anomaly: three case reports. J Saudi Heart Assoc. (2013) 25:43–6. doi: 10.1016/j.jsha.2012.05.002
4. Hyrtl J. Einige in chirurgicscher hinsicht wichtige gefassvariateten. Med Jahrb Osterr Staats. (1841) 33:17–38.
5. Desmet W, Vanhaecke J, Vrolix M, Van de Werf F, Piessens J, Willems J, et al. Isolated single coronary artery: a review of 50,000 consecutive coronary angiographies. Eur Heart J. (1992) 13:37–40. doi: 10.1093/oxfordjournals.eurheartj.a060117
6. Halperin I, Penny J, Kennedy R. Single coronary artery: antemortem diagnosis in a patient with congestive heart failure. Am J Cardiol. (1967) 19:424–7. doi: 10.1016/0002-9149(67)90456-0
Keywords: AMI, percutaneous coronary intervention (PCI), anomaly, drug-coated balloon (DCB), ventricular fibrillation (VF)
Citation: Niu Q, Zhao Y, Li H, Wang Q, Zhu H, Bi C, Zhang H, Wang J, Cheng C, Song B, Jin C, Lv M and Li B (2023) Case report: Treatment of a patient with STEMI and cardiogenic shock caused by RCA originating from LAD. Front. Cardiovasc. Med. 9:1036274. doi: 10.3389/fcvm.2022.1036274
Received: 04 September 2022; Accepted: 19 December 2022;
Published: 10 January 2023.
Edited by:
Tommaso Gori, Johannes Gutenberg University Mainz, GermanyReviewed by:
Roberto Spina, Gosford Hospital, AustraliaCopyright © 2023 Niu, Zhao, Li, Wang, Zhu, Bi, Zhang, Wang, Cheng, Song, Jin, Lv and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Li,  bGlib3N1Ym1pdEAxNjMuY29t; Ming Lv,
bGlib3N1Ym1pdEAxNjMuY29t; Ming Lv,  MTM4NjQzNzkzOTlAMTI2LmNvbQ==
MTM4NjQzNzkzOTlAMTI2LmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.