
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 20 December 2022
Sec. Coronary Artery Disease
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.1020488
This article is part of the Research Topic Current Trends and Approaches in the Comprehensive Evaluation of Coronary Artery Disease View all 19 articles
 Dongze Li1†
Dongze Li1† Xiaoli Chen1†
Xiaoli Chen1† Fanghui Li2
Fanghui Li2 Yu Jia1
Yu Jia1 Zhilin Li1
Zhilin Li1 Yi Liu1
Yi Liu1 Lei Ye1
Lei Ye1 Yongli Gao1
Yongli Gao1 Wei Zhang1
Wei Zhang1 Hong Li1
Hong Li1 Rui Zeng2
Rui Zeng2 Zhi Wan1
Zhi Wan1 Zhi Zeng1*
Zhi Zeng1* Yu Cao1*
Yu Cao1*Background: As a validated assessment tool for functional disability (activities of daily living), the Barthel index (BI) assessed initially at admission has the potential to stratify patients with high-risk acute coronary syndrome (ACS). Dynamic trajectory evaluation of functional capacity in hospitals may provide more prognostic information. We aimed to establish a novel dynamic BI-based risk stratification program (DBRP) during hospitalization to predict outcomes among ACS patients.
Methods: A total of 2,837 ACS patients were included from the Retrospective Multicenter Study for Early Evaluation of Acute Chest Pain. The DBRP rating (low, medium, and high-risk categories) was calculated from dynamic BI at admission and discharge. The primary outcome was all-cause mortality, and the secondary outcome was cardiac mortality.
Results: Of all the included patients, 312 (11%) died during a median follow-up period of 18.0 months. Kaplan–Meier analysis revealed that the cumulative mortality was significantly higher in patients in the higher risk category according to the DBRP. Multivariable Cox regression analysis indicated that, compared to the low-risk category, the higher risk category in the DBRP was an independent strong predictor of all-cause mortality after adjusting for confounding factors (medium-risk category: hazard ratio [HR]: 1.756, 95% confidence interval [95% CI]: 1.214–2.540; P = 0.003; high-risk category: HR: 5.052, 95% CI: 3.744–6.817; P < 0.001), and the same result was found for cardiac mortality.
Conclusion: The DBRP was a useful risk stratification tool for the early dynamic assessment of patients with ACS.
Clinical trial registration: [http://www.chictr.org.cn], identifier [ChiCTR1900024657].
Acute coronary syndrome (ACS) is a life-threatening emergent condition of coronary artery disease mainly caused by coronary plaque rupture with relatively high mortality and morbidity (1). Risk stratification in patients with ACS facilitates treatment decisions and improves survival rates (1–4). Current guidelines regarding ACS management emphasize the importance of risk assessment for identifying patients with a higher mortality risk requiring more aggressive care and therapy, selecting the optimal care site, and matching therapeutic intensity with risk (1, 5, 6). Previous studies indicated that risk evaluation based on the Global Registry of Acute Coronary Events (GRACE) or thrombolysis in myocardial infarction (TIMI) risk scores have been well-implemented for and proved to be clinically beneficial to patients with ACS, and the ACS guidelines recommend that the GRACE score should be completed within 24 h and re-evaluated before discharge to guide the management of ACS (5–9).
Nearly 38% of in-hospital deaths occur within the first 24 h of symptom onset in patients with AMI; therefore, early, rapid, and dynamic risk assessment identifying high-risk patients is necessary to guide treatment decisions in the emergency department (ED) (10). However, assessment using these risk scores, including GRACE or TIMI, is relatively time consuming and cannot be completed without a medical examination because these scoring systems consist of components including biomarkers of myocardial and other related organ injuries. In addition, the condition of patients with ACS can change rapidly, and the continuous dynamic assessment of ACS patients may provide more prognostic information during the whole course of ACS (11). With this in mind, current scoring systems cannot also immediately stratify patients out of hospitals or during hospitalization, and realize the timely revision of their risk level. This suggests the need for simpler, more accurate dynamic assessment and better treatment decision tools or algorithms to guide individual healthcare during the pre-hospital, admission, in-hospital, and discharge settings.
Activities of daily living (ADL), as a basic functional capacity marker assessed by the Barthel Index (BI) score based on difficulty degrees of daily activities without any laboratory or imaging examination results, has gained interest in recent years as a prognostic indicator in patients with cardiovascular emergency conditions (12, 13). Performance of the ADL assessment is nowadays feasible in the ambulance and, therefore, the functional capacity assessment can be completely obtained in the pre-hospital, in-hospital, or even discharge settings. A previous study indicated that the initial ADL assessed by the BI at the ED has the potential to stratify high-risk patients with ACS, and independently associated with mortality, however, the accuracy was inferior to that of the GRACE score (12). In addition, patients with ACS would receive optimal drug therapy and/or PCI during hospitalization, patient’s ADL should be improved if patients responded well to the treatment therapy, and maybe the elevated change in ADL assessed by BI scores during hospitalization suggested that the improvement of myocardial ischemia or less complications after treatment in hospital. It is possible that the continuous dynamic assessment of functional capacity trajectories may provide more prognostic information for patients with ACS. However, the assessment of functional status at admission or the deterioration in functional status during hospitalization has received little consideration and has not been studied as a potential risk prognostic tool for risk stratification of ACS. Therefore, we conducted this multicenter retrospective cohort study to establish a novel dynamic BI-based risk stratification program (DBRP) based on functional capacity trajectories during hospitalization for long-term outcomes and evaluate the prediction efficiency of this risk assessment tool in patients with ACS.
The Retrospective Evaluation of Acute Chest Pain (REACP) study is a multicenter, retrospective study including a cohort of patients with acute chest pain (ACP) who were admitted to EDs from seven tertiary hospitals in China from January 2017 to December 2019 (clinicaltrials.gov, identifier: ChiCTR1900024657) (12, 14). This study was conducted to elucidate the development of fatal chest pain (ACS, aortic dissection, and pulmonary embolism) and the risk factors in the suspected population. This study was conducted in accordance with the Declaration of Helsinki and approved by local or central institutional review.
In this study, we aimed to establish a novel DBRP based on admission and hospital-acquired BI score for risk stratification in ACS patients. The inclusion criteria were as follows: age greater than 18 years, first-time diagnosis of ST-segment elevation myocardial infarction (STEMI) or non-STEMI (NSTEMI), and unstable angina (UA), less than 12 h between the onset of symptoms and ED admission, and treatment with coronary angiography or primary percutaneous coronary intervention in the hospital. The exclusion criteria were as follows: accompanied by the identified disabled (including previous stroke, severe valvular heart disease, heart failure, chronic obstructive pulmonary disease, rheumatological diseases, trauma diseases, and other diseases with possible impact in BI assessment), malignant tumors, pregnancy, end-stage hepatopathy, or renal failure at admission. A diagram demonstrating the election of patients is shown in Figure 1.
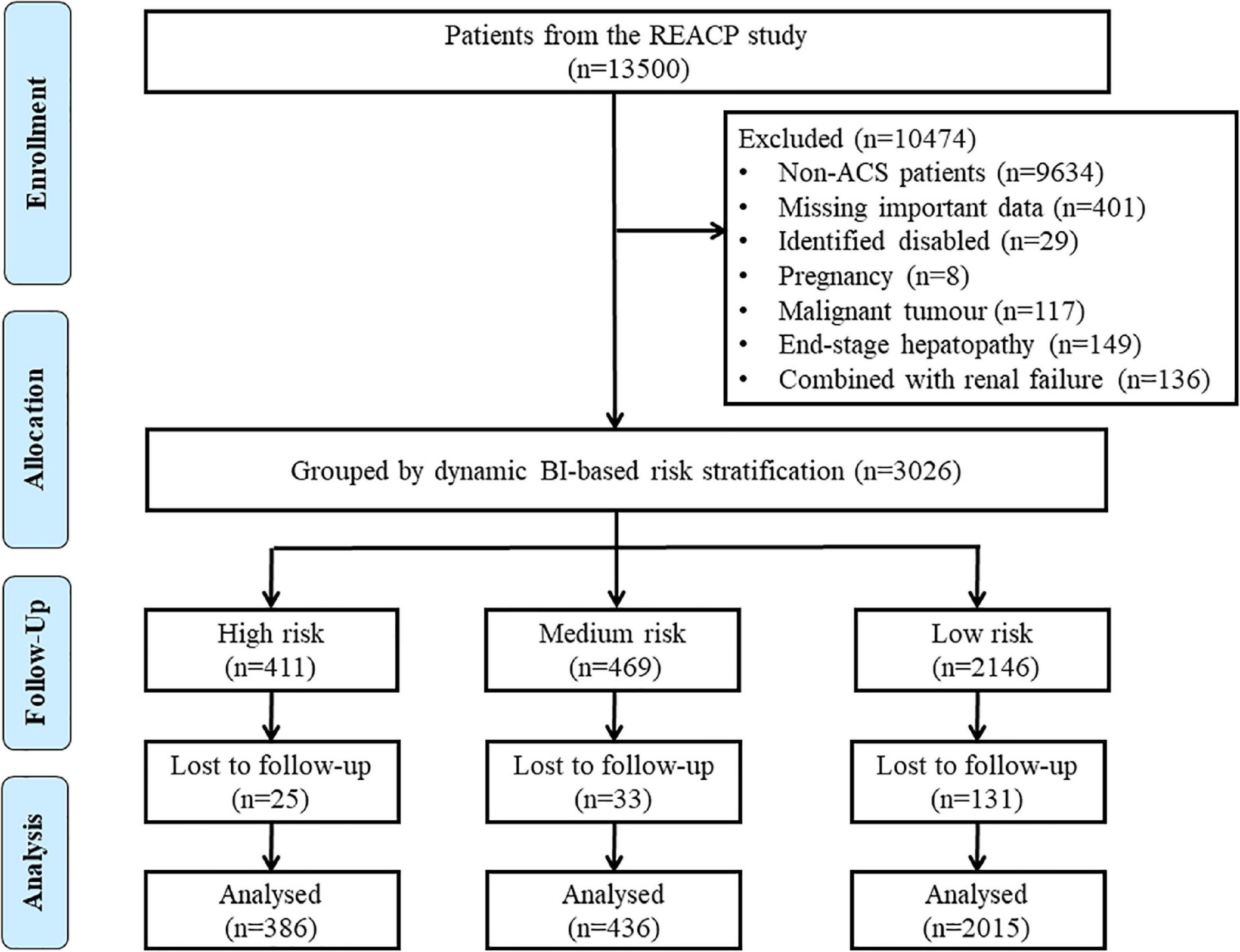
Figure 1. Flow chart of the enrollment of participants in the study. ACS, acute coronary syndrome; BI, Barthel index; REACP, the multicentre retrospective evaluation of acute chest pain study.
In this study, the BI scores of ACS patients were assessed by trained nurses at admission and discharge. The details of evaluating BI scores were described in our previous study (12). Briefly, the BI score comprises 10 items: feeding, toilet use, bathing, grooming, dressing, bowel and bladder control, chair transferring, stair climbing, and ambulating. Each item is scored proportionally, and a given number of points are assigned to each level or rank. The admission and discharge BI assessments were conducted according to responses from the ACS patient or a family member. We divided the BI score into three different level categories according to the standard BI grouping method: high disability caused by ADL (0–40), considered high risk, moderate disability caused by ADL (41–60), considered medium risk, low disability caused by ADL (61–100), considered low risk (12).
We obtained demographic data, characteristic details, and clinical features of the patients from the database of the REACP study, including medical histories, vital signs, electrocardiograms, troponin I/T, myocardial enzymes, liver and renal function, coronary angiography (CAG) findings, echocardiography findings, inpatient complications, pre-hospital and in-hospital treatment and discharge medication. Standard case report forms were used to collect these data; the details were described in our previous publications (3, 4, 12, 15, 16).
In this study, we established a novel DBRP consisting of the low, medium, and high-risk categories, based on admission BI, discharge BI and the changes between the two. In terms of the BI changes, “largely improved” was defined as two levels of improvement; for example, BI changes from the high risk (0–40) to the low-risk category (61–100); “slightly improved” was defined as one level of improvement; for example, BI changes from the high-risk category (0–40) to the medium-risk category (41–60); “largely declined” was defined as two levels of worsening; for example, BI changes from low risk (61–100) to high risk (0–40); “slightly declined” was defined as one level of worsening; for example, BI changes from the medium risk (41–60) to the high-risk category (0–40); “no change” was defined as the risk group at discharge BI remaining the same as that on admission. In particular, for dead patients within hospitalization, the BI at discharge was signed to high risk (0–40). The detailed rules for risk stratification based on the DBRP are described in Figure 2.
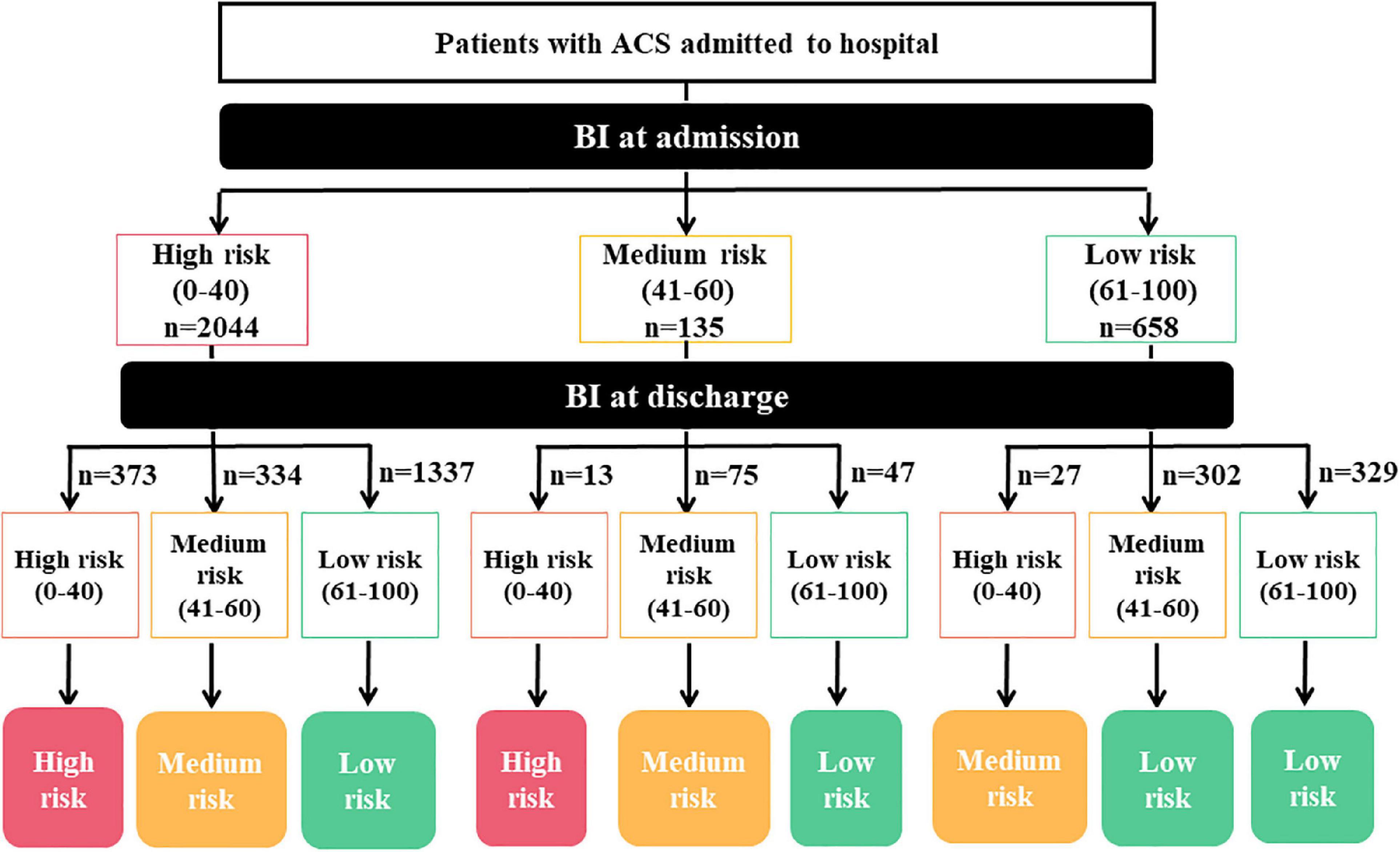
Figure 2. Diagram of the detailed rules for dynamic BI-based risk stratification. BI, Barthel index.
The primary endpoint of this study was all-cause mortality, confirmed through a combination of hospital medical records and telephone contact with the patient’s family members. The secondary outcome was cardiac death, identified based on hospital record reviews for identified hospitalizations and through phone interviews. All reported events were reviewed and verified by the outcome assessment committee of the REACP study.
Parametric continuous variables are expressed as means ± standard deviations (SD) and non-parametric continuous variables as medians with interquartile ranges. Categorical variables are reported as frequencies and percentages. Parametric patient characteristics were compared using one-way analysis and non-parametric variables using the Kruskal–Wallis H test. Categorical variables were compared using Fisher’s exact test or chi-square test.
The Kaplan–Meier survival analysis and log-rank tests were performed to calculate and compare the cumulative survival of ACS patients with different risk levels. Cox proportional hazards models were used to investigate the relationship between risk levels according to dynamic BI-based risk stratification and time-to-mortality. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using the multivariate Cox regression model after adjusting for potential influencing factors. The sensitivity, specificity, accuracy, positive predictive value (PPV), negative predictive value (NPV), and Cohen’s Kappa coefficient were calculated to evaluate the predictive efficiency of DBRP and GRACE score. Receiver operating characteristic (ROC) analyses for the DBRP and GRACE score were performed, and differences in mortality between these indicators were compared using the area under the curve (AUC) values with the method of DeLong et al. (17).
Subgroup analysis was performed to test the robustness of the association between the Dynamic BI-based risk stratification score and the all-cause mortality. A two-tailed P-value < 0.05 was considered significant for all tests. Statistical analyses were performed using SPSS version 22.0 (IBM Corp, Armonk, NY, USA) and R Statistical Software (v4.1.2; R Core Team 2021) (18).
A total of 2,837 ACS patients were enrolled with an average age of 65.5 ± 13.0 years. Of these participants, 2,121 (74.7%) were male. According to the dynamic BI-based risk stratification program (DBRP), patients were divided into three groups: the high-risk (n = 386, 13.6%), medium risk (n = 436, 15.4%), and low-risk groups (n = 2,015, 71.0%). During a median follow-up period of 18.0 (10.3–24.2) months, a total of 312 (11.0%) patients died, of whom 237 (8.3%) died due to cardiac causes. The baseline characteristics of patients in these three groups are described and compared in Table 1. Compared to those in the low-risk group, participants in the high-risk group were older, had lower body mass indexes (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), left ventricular ejection fraction (LVEF), triglycerides, total cholesterol, and low-density lipoprotein (LDL), and had higher heart rates, fibrinogen, blood glucose, creatinine, BUN, N-terminal pro-B-type natriuretic peptide (NT-proBNP), cardiac troponin T, creatinine kinase, CK-MB levels, GRACE scores, and Genisini scores, and were more likely to have chronic obstructive pulmonary disease (COPD) and Killip classes ≥ 2. Several common inflammatory and thrombus indicators, namely white blood cells (WBC), neutrophil, C-reactive protein (CRP), interleukin 6, neutrophil-to-lymphocyte ratio (NRL), and D-dimer, were significantly higher in the high-risk category of DBRP than in the low-risk category (NLR, P = 0.009; all others, P < 0.001).
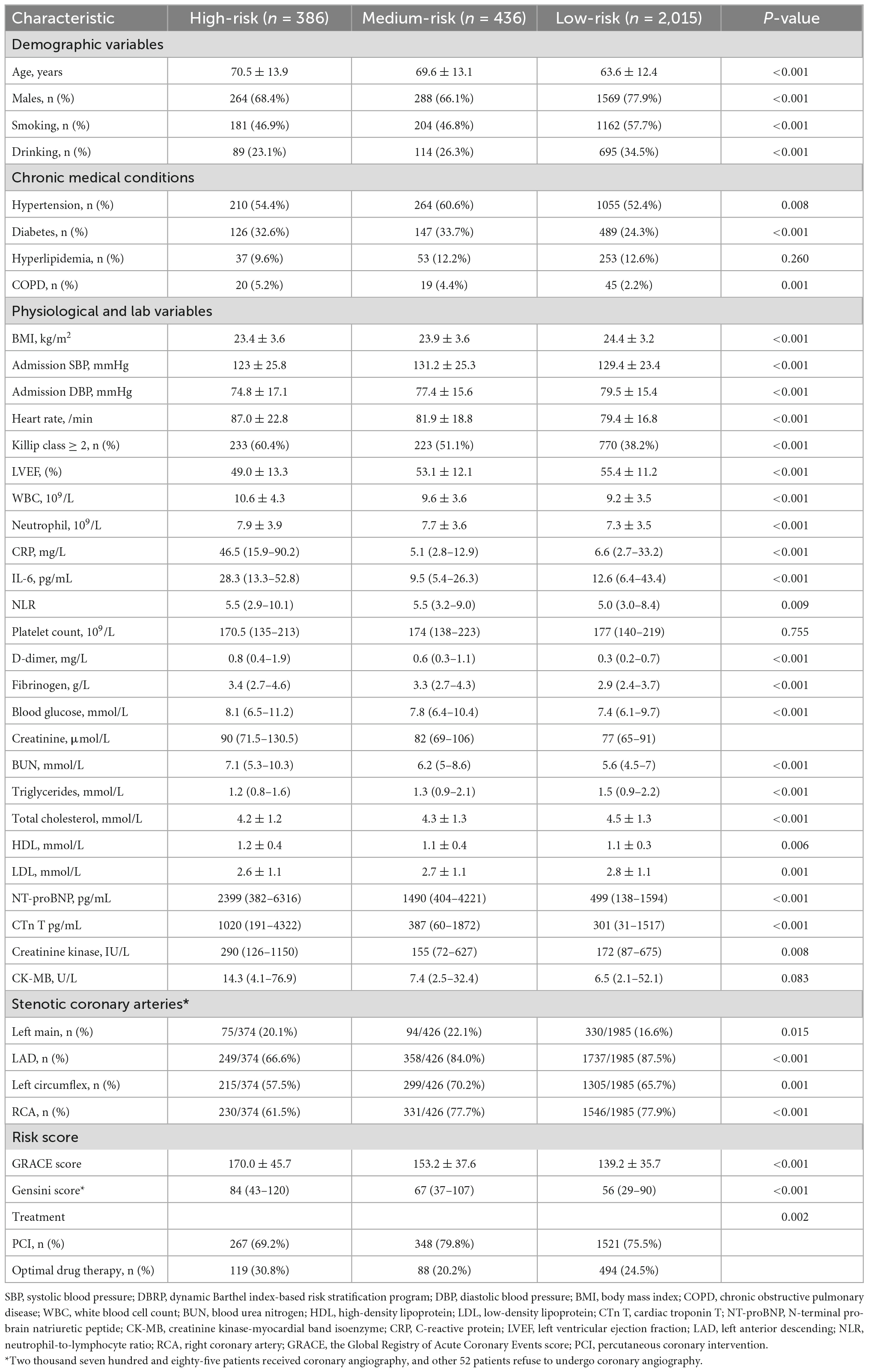
Table 1. Relationships between baseline clinical characteristics and the DBRP in patients with acute coronary syndrome.
Kaplan–Meier analysis (Figure 3) revealed that the cumulative mortality was significantly higher in patients in the higher risk category according to the DBRP, regardless of STEMI and non-ST segment elevation acute coronary syndrome (NST-ACS), in both all-cause mortality and cardiac mortality (P < 0.001 for all). Multivariable Cox regression analysis further indicated compared to participants with the low-risk category, the higher risk category in the DBRP was an independent strong predictor of both all-cause mortality and cardiac mortality after eliminating confounding factors (all-cause mortality: medium-risk category: HR: 1.756, 95% CI: 1.214–2.540; P = 0.003; high-risk category: HR: 5.052, 95% CI: 3.744–6.817; P < 0.001; cardiac mortality: medium-risk category: HR: 1.865, 95% CI: 1.252–2.779; P = 0.002; high-risk category: HR: 4.780, 95% CI: 3.423–6.673; P < 0.001; Table 2).
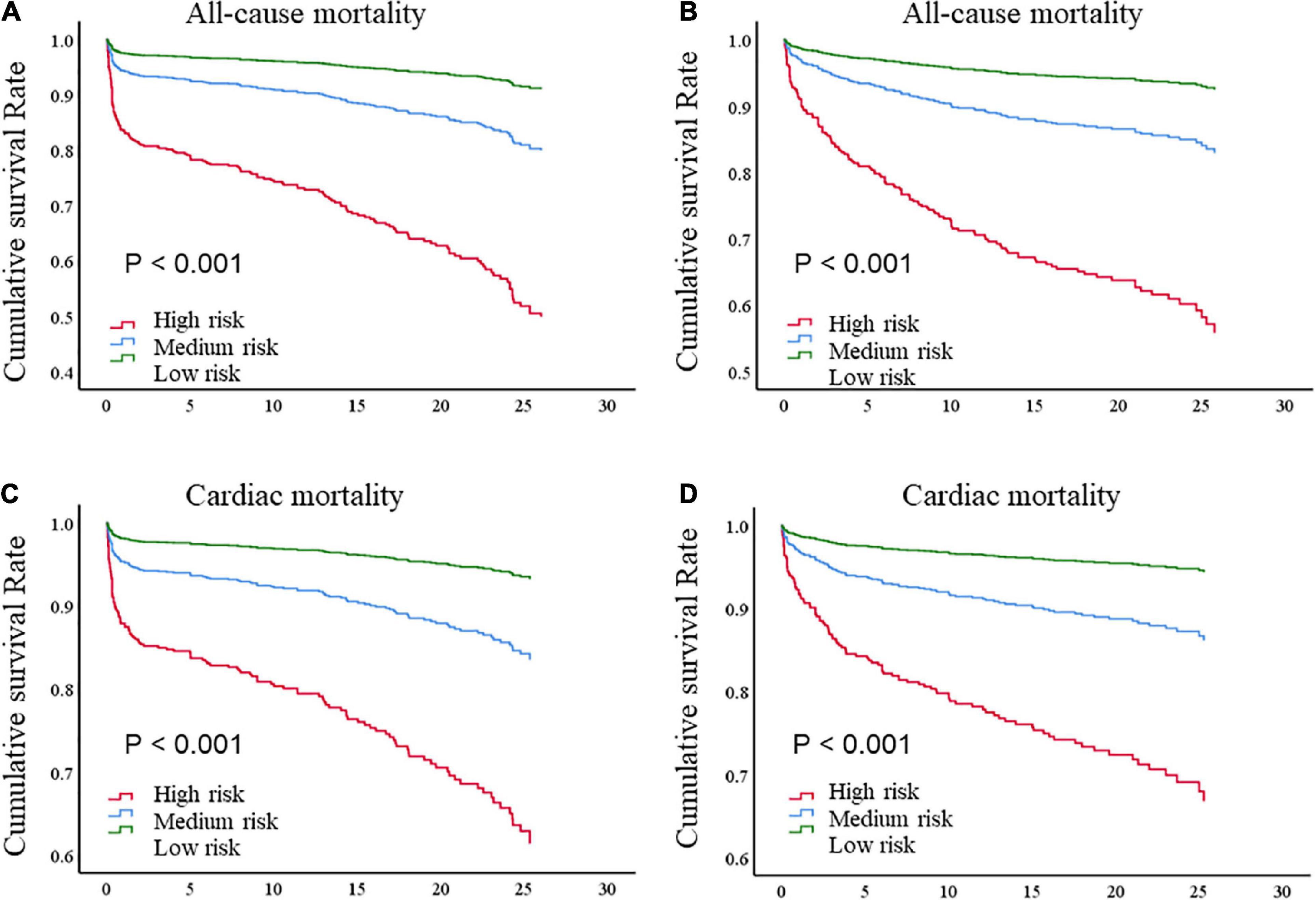
Figure 3. Kaplan–Meier survival curve of (A) all-cause death for STEMI patients; (B) all-cause death for NST-ACS patients; (C) cardiac death for STEMI patients; (D) cardiac death for NST-ACS patients; by risk levels according to dynamic BI-based risk stratification. BI, Barthel index; STEMI, ST-segment elevation myocardial infarction; NST-ACS, non-ST elevation acute coronary syndrome.
The sensitivity, specificity, accuracy, PPV, and NPV for mortality of the dynamic BI-based risk stratification, when high-risk was taken as the cut point, were 42.0, 89.9, 84.6, 33.9, and 92.6%, respectively. And the Cohen’s Kappa coefficient was 0.289 (95%CI: 0.240–0.338, P < 0.001). When medium-risk was used as the cutoff point, the sensitivity, specificity, accuracy, PPV, and NPV for mortality of the dynamic BI-based risk stratification were 60.6, 74.9, 73.4, 23.0, and 93.9%, respectively. The Cohen’s Kappa coefficient was 0.207 (95% CI: 0.171–0.242, P < 0.001). We also evaluated the predictive efficiency of the GRACE score, using guideline-recommended 140 and 108 as cutoff points, respectively. The specific results were shown in Table 3. The AUC generated using the ROC curve analysis found no significant differences in AUCs for all-cause mortality between the DBRP (low, medium, and high risk) and GRACE score (140 and 108 as cutoff points) (AUC, 0.700 vs. 0.698, P > 0.05), however, the AUC of GRACE score (AUC, 0.791, P < 0.001) was higher than that of categorical DBRP for all-cause mortality.
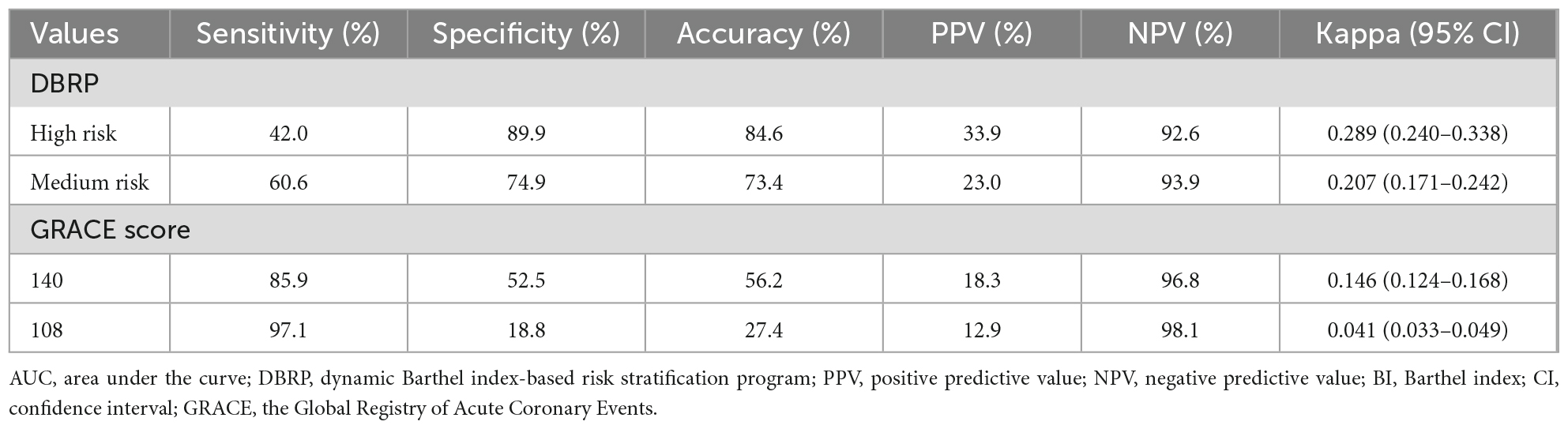
Table 3. Predictive efficiency for mortality of the DBRP and GRACE score in acute coronary syndrome patients.
We carried out subgroup analysis by grouping patients according to gender, age, BMI, SBP, DBP, heart rate, WBC, cardiac troponin T, NT-proBNP, Killip class, GRACE score, and ACS type. Patients in the high-risk group had the lowest cumulative survival rates of all-cause mortality in each subgroup (Table 4).
This study established a novel dynamic BI-based risk stratification program (DBRP) using admission and discharge BI, and the changes between them for risk assessment in ACS patients and investigated whether the DBRP was efficient in predicting the prognosis of patients with ACS. Our findings demonstrated that the DBRP could accurately predict the prognosis of ACS patients. Patients with high and medium risks were correlated with an increased risk of all-cause mortality and cardiac mortality compared to those with low risk. Higher risk independently predicted a worse prognosis in ACS patients.
Our previous study demonstrated that the BI scores assessed at admission were a valuable prognostic predictor for patients with ACS, predicting all-cause mortality and cardiac mortality both in-hospital and during follow-up (12). According to the BI scores at admission, the HR for mortality of patients in the high-risk group is twice that of patients in the low-risk group. One study focusing on older ACS patients (≥85 years) found that the BI scores assessed at discharge were correlated with 1-year mortality in these patients (13). However, the development of the disease process is ever-changing; thus, dynamic assessment may provide more valuable information (11).
The BI score at admission reflects the ADL of patients before medical intervention, which shows the initial status of the patient after the onset of illness, while the BI score assessed at discharge reflects the ADL of patients after receiving medical intervention, indicating the patient’s current status. The change between these two indices provided information on disease development and therapeutic effects. The DBRP comprehensively evaluates these three items, which may more accurately predict the prognosis of ACS patients. In addition, the elevated change in ADL assessed by BI scores during hospitalization suggested that the improvement of myocardial ischemia or less complications after treatment in hospital. Therefore, In this study, we took the dynamic changes of ADL functional status into consideration and established a relatively more accurate risk stratification tool for ACS patients.
As described in our previous research, ADL representing patients’ physical functional status is correlated with several pathophysiological states, including inflammatory processes, aging status, and frailty (19–23). These factors are all essential considerations in the occurrence and development of cardiovascular disease (24–28). Also, the results of our study showed that several common inflammatory and thrombus indicators were significantly higher among patients in the high-risk category of DBRP than in the low-risk category, which may further explain an underlying mechanism. Prior studies have demonstrated that the indicators related to the various pathophysiological conditions involved in the pathogenesis of cardiovascular disease or myocardial injury may provide more prognostic information (3, 29–31). Being a validated evaluation tool for ADL, the BI score is highly likely to play a role in the risk stratification and prognosis prediction of ACS patients.
As the performance of the evaluation of ADL is nowadays feasible in the ambulance, the BI score can be completely obtained in the pre-hospital setting. The scale is considered easy to use, with good reliability and sensitivity to change, mainly in predicting the ADL functional status. The DBRP established in the present study is based on the changes between admission and discharge BI scores, and it has been proved that dynamic monitoring may provide more information and guide clinical decision-making, no matter the patient’s physiological indices or functional status (32–35). Thus, the continuous dynamic evaluation of BI scores may provide more prognostic information for patients with ACS. According to our results, the risk of mortality was five times greater in the high-risk category than the low-risk category of DBRP. Furthermore, in patients with different levels of cardiovascular risk factors, the DBRP had a stable prognostic value. This result is far better than that of our previous study, in which risk stratification was carried out based on the BI score at admission alone (12).
The GRACE score is a guideline-recommended risk stratification for patients with ACS, comprising several factors, including demographic data, heart and other organ damage related to ACS, and has been widely used in clinical practice (36). The results of this study show that the DBRP had relatively better specificity, accuracy, PPV, and consistency than the GRACE score in predicting mortality in ACS patients, and no significant differences in the AUCs for all-cause mortality were observed between the DBRP and GRACE score (as categorical data). The DBRP provides additional geriatric-related signals reported to predict outcomes beyond age and standard risk factors (37). Currently, the ACS patients with geriatric conditions account for an increasing proportion of total patients, making it all the more important to consider the relevant indicators (38). Thus, the DBRP is indeed necessary because it may provide prognostic information not provided by the GRACE score, and combining these two indicators may illustrate comprehensive and systematic information. Furthermore, the BI score is routinely evaluated orally by nurses in hospital settings in China, which does not increase the burden on doctors, and has been widely accepted by both physicians and patients. Importantly, in the early evaluation of ACS patients, the participation of nurses can promote physician-nurse collaboration, subsequently leading to a more efficient and comprehensive evaluation. The latest European Society of Cardiology consensus statement demonstrated that the active participation of well-trained nurses can be beneficial to the risk stratification of patients (5). In addition, as a ADL assessment tool, the BI score consists of 10 items that relate to ADL without any medical examination results, and is considered easy to use mainly in predicting the functional outcomes.
There are several limitations to this study. Firstly, retrospective as this study was, large, multicenter, and prospective studies are needed to further verify the validity of these results. Secondly, we only collected BI scores at one time point after admission, while multiple collections may provide more prognostic information. Thirdly, whether subsequent clinical interventions according to the DBRP can improve the prognosis of ACS patients was not investigated in this study, and this would be an interesting point to further explore in the future.
This study established a risk stratification tool based on dynamic BI scores and demonstrated that this dynamic BI-based risk stratification program might help identify high-risk patients and provide useful prognostic information for patients with ACS. As such, it could be applied in clinical practice for ACS patients for early risk warning and clinical decision guidance.
The original contributions presented in this study are included in this article/supplementary material, further inquiries can be directed to the corresponding authors.
DL, ZZ, and YC conceived the study design. DL, XC, YJ, FL, ZL, YL, WZ, LY, HL, and YG collected the epidemiological and clinical data. DL, XC, YJ, YL, and ZL summarized data and performed the statistical analysis. DL, FL, and YC interpreted the data and drafted the manuscript. ZZ and RZ participated in the design of the study, acquired the data, and helped to revise the manuscript. All authors accepted responsibility for the entire content of this submitted manuscript and approved submission.
This work was financially supported by grants from National Key Research and Development Program of China (Nos. 2020AAA0105000 and 2020AAA0105005), Sichuan Science and Technology Program (Nos. 2022YFS0279, 2021YFQ0062, and 2022JDRC0148), Sichuan Provincial Health Commission (No. ZH2022-101), and Sichuan University West China Nursing Discipline Development Special Fund Project (Nos. HXHL20017, HXHL20046, and HXHL21016).
We thank all the participants of this project and investigators for collecting the data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ACS, acute coronary syndrome; ACP, acute chest pain; ADL, activities of daily living; AUC, area under the curve; BI, Barthel index; DBRP, dynamic Barthel index-based risk stratification program; ED, emergency department; GRACE, Global Registry of Acute Coronary Events; NSTEMI, non-ST-segment elevation myocardial infarction; NST-ACS, non-ST elevation acute coronary syndrome; REACP, retrospective evaluation of acute chest pain; STEMI, ST-segment elevation myocardial infarction; TIMI, thrombolysis in myocardial infarction; UA, unstable angina.
1. Ibanez B, James S, Agewall S, Antunes M, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC). Eur Heart J. (2018) 39:119–77. doi: 10.1093/eurheartj/ehx393
2. O’Donoghue M, Morrow D, Cannon C, Jarolim P, Desai N, Sherwood M, et al. Multimarker risk stratification in patients with acute myocardial infarction. J Am Heart Assoc. (2016) 5:e002586. doi: 10.1161/jaha.115.002586
3. Li F, Li D, Yu J, Jia Y, Jiang Y, Chen X, et al. Prognostic value of the nutritional risk screening 2002 scale in patients with acute myocardial infarction: insights from the retrospective multicenter study for early evaluation of acute chest pain. J Cardiovasc Nurs. (2021) 36:546–55. doi: 10.1097/jcn.0000000000000786
4. Yu J, Li D, Jia Y, Li F, Jiang Y, Zhang Q, et al. Nutritional risk screening 2002 was associated with acute kidney injury and mortality in patients with acute coronary syndrome: insight from the REACP study. Nutr Metab Cardiovasc Dis. (2021) 31:1121–8. doi: 10.1016/j.numecd.2020.12.028
5. Stepinska J, Lettino M, Ahrens I, Bueno H, Garcia-Castrillo L, Khoury A, et al. Diagnosis and risk stratification of chest pain patients in the emergency department: focus on acute coronary syndromes. A position paper of the acute cardiovascular care association. Eur Heart J Acute Cardiovasc Care. (2020) 9:76–89. doi: 10.1177/2048872619885346
6. Wong G, Welsford M, Ainsworth C, Abuzeid W, Fordyce C, Greene J, et al. 2019 canadian cardiovascular society/canadian association of interventional cardiology guidelines on the acute management of ST-elevation myocardial infarction: focused update on regionalization and reperfusion. Can J Cardiol. (2019) 35:107–32. doi: 10.1016/j.cjca.2018.11.031
7. Tamis-Holland J, Jneid H, Reynolds H, Agewall S, Brilakis E, Brown T, et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the american heart association. Circulation. (2019) 139:e891–908. doi: 10.1161/cir.0000000000000670
8. Lim M, Eagle K, Gore J, Anderson F Jr., Dabbous O, Mehta R, et al. Treating patients with acute coronary syndromes with aggressive antiplatelet therapy (from the global registry of acute coronary events). Am J Cardiol. (2005) 96:917–21. doi: 10.1016/j.amjcard.2005.05.047
9. Hall M, Bebb O, Dondo T, Yan A, Goodman S, Bueno H, et al. Guideline-indicated treatments and diagnostics, GRACE risk score, and survival for non-ST elevation myocardial infarction. Eur Heart J. (2018) 39:3798–806. doi: 10.1093/eurheartj/ehy517
10. Ohman E, Topol E, Califf R, Bates E, Ellis S, Kereiakes D, et al. An analysis of the cause of early mortality after administration of thrombolytic therapy. The thrombolysis angioplasty in myocardial infarction study group. Coron Artery Dis. (1993) 4:957–64. doi: 10.1097/00019501-199311000-00002
11. Chang W, Boersma E, Granger C, Harrington R, Califf R, Simoons M, et al. Dynamic prognostication in non-ST-elevation acute coronary syndromes: insights from GUSTO-IIb and PURSUIT. Am Heart J. (2004) 148:62–71. doi: 10.1016/j.ahj.2003.05.004
12. Li F, Li D, Yu J, Jia Y, Jiang Y, Chen T, et al. Barthel index as a predictor of mortality in patients with acute coronary syndrome: better activities of daily living, better prognosis. Clin Interv Aging. (2020) 15:1951–61. doi: 10.2147/cia.S270101
13. Higuchi S, Kabeya Y, Matsushita K, Taguchi H, Ishiguro H, Kohshoh H, et al. Barthel index as a predictor of 1-year mortality in very elderly patients who underwent percutaneous coronary intervention for acute coronary syndrome: better activities of daily living, longer life. Clin Cardiol. (2016) 39:83–9. doi: 10.1002/clc.22497
14. Li D, Cheng Y, Yu J, Jia Y, Li F, Zhang Q, et al. Early risk stratification of acute myocardial infarction using a simple physiological prognostic scoring system: insights from the REACP study. Eur J Cardiovasc Nurs. (2021) 20:147–59. doi: 10.1177/1474515120952214
15. Jia Y, Li H, Li D, Li F, Li Q, Jiang Y, et al. Prognostic value of braden scale in patients with acute myocardial infarction: from the retrospective multicenter study for early evaluation of acute chest pain. J Cardiovasc Nurs. (2020) 35:E53–61. doi: 10.1097/jcn.0000000000000735
16. Jia Y, Gao Y, Li D, Cao Y, Cheng Y, Li F, et al. Geriatric nutritional risk index score predicts clinical outcome in patients with acute ST-segment elevation myocardial infarction. J Cardiovasc Nurs. (2020) 35:E44–52. doi: 10.1097/jcn.0000000000000674
17. DeLong E, DeLong D, Clarke-Pearson D. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. (1988) 44:837–45.
18. R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing (2021). Available online at: https://www.R-project.org
19. Noz M, Hartman Y, Hopman M, Willems P, Tack C, Joosten L, et al. Sixteen-week physical activity intervention in subjects with increased cardiometabolic risk shifts innate immune function towards a less proinflammatory State. J Am Heart Assoc. (2019) 8:e013764. doi: 10.1161/jaha.119.013764
20. Duggal N, Niemiro G, Harridge S, Simpson R, Lord J. Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity? Nat Rev Immunol. (2019) 19:563–72. doi: 10.1038/s41577-019-0177-9
21. Bier N, Belchior Pda C, Paquette G, Beauchemin É, Lacasse-Champagne A, Messier C, et al. The instrumental activity of daily living profile in aging: a feasibility study. J Alzheimers Dis. (2016) 52:1361–71. doi: 10.3233/jad-150957
22. Costenoble A, Knoop V, Vermeiren S, Vella R, Debain A, Rossi G, et al. Comprehensive overview of activities of daily living in existing frailty instruments: a systematic literature search. Gerontologist. (2021) 61:e12–22. doi: 10.1093/geront/gnz147
23. Op Het Veld L, Beurskens A, de Vet H, van Kuijk S, Hajema K, Kempen G, et al. The ability of four frailty screening instruments to predict mortality, hospitalization and dependency in (instrumental) activities of daily living. Eur J Ageing. (2019) 16:387–94. doi: 10.1007/s10433-019-00502-4
24. Swirski F, Nahrendorf M. Leukocyte behavior in atherosclerosis, myocardial infarction, and heart failure. Science. (2013) 339:161–6. doi: 10.1126/science.1230719
25. Li D, Zhao L, Yu J, Zhang W, Du R, Liu X, et al. Lipoprotein-associated phospholipase A2 in coronary heart disease: review and meta-analysis. Clin Chim Acta. (2017) 465:22–9. doi: 10.1016/j.cca.2016.12.006
26. Veerasamy M, Edwards R, Ford G, Kirkwood T, Newton J, Jones D, et al. Acute coronary syndrome among older patients: a review. Cardiol Rev. (2015) 23:26–32. doi: 10.1097/crd.0000000000000016
27. Campo G, Maietti E, Tonet E, Biscaglia S, Ariza-Solè A, Pavasini R, et al. The assessment of scales of frailty and physical performance improves prediction of major adverse cardiac events in older adults with acute coronary syndrome. J Gerontol A Biol Sci Med Sci. (2020) 75:1113–9. doi: 10.1093/gerona/glz123
28. Uchmanowicz I, Lisiak M, Wleklik M, Gurowiec P, Kałużna-Oleksy M. The relationship between frailty syndrome and quality of life in older patients following acute coronary syndrome. Clin Interv Aging. (2019) 14:805–16. doi: 10.2147/cia.S204121
29. Li D, Ye L, Yu J, Deng L, Liang L, Ma Y, et al. Significance of the thrombo-inflammatory status-based novel prognostic score as a useful predictor for in-hospital mortality of patients with type B acute aortic dissection. Oncotarget. (2017) 8:79315–22. doi: 10.18632/oncotarget.18105
30. Du R, Li D, Yu J, Ma Y, Zhang Q, Zeng Z, et al. Association of platelet to lymphocyte ratio and risk of in-hospital mortality in patients with type B acute aortic dissection. Am J Emerg Med. (2017) 35:368–70. doi: 10.1016/j.ajem.2016.11.003
31. Li D, Chen Y, Jia Y, Tong L, Tong J, Wang W, et al. CoV-2-induced immune dysregulation and myocardial injury risk in china: insights from the ERS-COVID-19 study. Circulation Res. (2020) 127:397–9. doi: 10.1161/circresaha.120.317070
32. Shekelle P, Pane J, Agniel D, Shi Y, Rumball-Smith J, Haas A, et al. Assessment of variation in electronic health record capabilities and reported clinical quality performance in ambulatory care clinics, 2014-2017. JAMA Netw Open. (2021) 4:e217476. doi: 10.1001/jamanetworkopen.2021.7476
33. Neoh M, Abu Zaid Z, Mat Daud Z, Md Yusop N, Ibrahim Z, Abdul Rahman Z, et al. Changes in nutrition impact symptoms, nutritional and functional status during head and neck cancer treatment. Nutrients. (2020) 12:1225. doi: 10.3390/nu12051225
34. Smith S, Madden A. Body composition and functional assessment of nutritional status in adults: a narrative review of imaging, impedance, strength and functional techniques. J Hum Nutr Diet. (2016) 29:714–32. doi: 10.1111/jhn.12372
35. Bowen M. Monitoring functional status using a wearable real-time locating technology. Nurs Outlook. (2020) 68:727–33. doi: 10.1016/j.outlook.2020.04.012
36. Granger C, Goldberg R, Dabbous O, Pieper K, Eagle K, Cannon C, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. (2003) 163:2345–53. doi: 10.1001/archinte.163.19.2345
37. Sanchis J, Bonanad C, Ruiz V, Fernández J, García-Blas S, Mainar L, et al. Frailty and other geriatric conditions for risk stratification of older patients with acute coronary syndrome. Am Heart J. (2014) 168:784–91. doi: 10.1016/j.ahj.2014.07.022
Keywords: acute coronary syndrome, trajectory, functional capacity, risk stratification, activities of daily living
Citation: Li D, Chen X, Li F, Jia Y, Li Z, Liu Y, Ye L, Gao Y, Zhang W, Li H, Zeng R, Wan Z, Zeng Z and Cao Y (2022) Evaluation of risk stratification program based on trajectories of functional capacity in patients with acute coronary syndrome: The REACP study. Front. Cardiovasc. Med. 9:1020488. doi: 10.3389/fcvm.2022.1020488
Received: 16 August 2022; Accepted: 02 December 2022;
Published: 20 December 2022.
Edited by:
Gianluca Rigatelli, Hospital Santa Maria della Misericordia of Rovigo, ItalyReviewed by:
Roberto Franco Enrico Pedretti, MultiMedica Scientific and Technological Pole, MultiMedica (IRCCS), ItalyCopyright © 2022 Li, Chen, Li, Jia, Li, Liu, Ye, Gao, Zhang, Li, Zeng, Wan, Zeng and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu Cao, ✉ Y2FveXVAd2Noc2N1LmNu; Zhi Zeng, ✉ emVuZ3poaTIwMTNAcXEuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.