- 1Division of Cardiology, Department of Clinical and Molecular Medicine, Azienda Ospedaliera Universitaria Sant’Andrea, Sapienza University of Rome, Rome, Italy
- 2Cardiology Unit, Madre Giuseppina Vannini Hospital, Rome, Italy
- 3Cardiovascular Disease Unit, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) Ospedale Policlinico San Martino, Genoa, Italy
- 4Department of Internal Medicine, University of Genoa, Genoa, Italy
It has been reported that patients affected by takotsubo syndrome (TTS) with a concurrent diagnosis of cancer suffer from greater mortality as compared to their non-cancer counterpart. It remains unclear whether TTS worsens the prognosis of cancer patients as well. Aim of this study was to compare outcomes of cancer patients with and without TTS. We combined data from two independent cohorts: one consisted of a prospective multicentre TTS registry; the second cohort consisted of all oncologic patients from two Cardio-Oncology Outpatient Clinics, who did not have cardiovascular conditions at the time of the cardio-oncologic visit. From the TTS registry, we selected patients with cancer (cancer-TTS patients). Next, we matched these patients with those from the cardio-oncologic cohort (cancer non-TTS patients) in a 1:2 fashion by age, sex, and type and cancer staging. Study endpoint was all-cause mortality. Among 318 TTS patients, 42 (13%) had a concurrent diagnosis of cancer. Characteristics of cancer-TTS patients and of the 84 matched cancer non-TTS subjects were comparable with the exception of diabetes mellitus, which was more common in cancer non-TTS patients. All-cause mortality was similar between cancer-TTS and cancer non-TTS patients. At Cox regression analysis TTS was not associated with mortality (OR 1.4, 95% CI 0.6–3.3, p = 0.43). Our findings show that even in the presence of acute heart failure due to TTS, the prognosis of oncologic patients is driven by the malignancy itself. Our results may prove useful for integrated management of cardio-oncologic patients.
Introduction
The profile of patients affected by takotsubo syndrome (TTS) is characterized by the presence of several cardiovascular and non-cardiovascular comorbidities, among which cancer is one of the most frequent (1, 2). It has been largely acknowledged that these comorbidities are the main drivers of prognosis in TTS, especially in the long-term (3). In particular, patients affected by TTS with a concurrent diagnosis of cancer have been reported to suffer from greater mortality, both in the short and long-term, as compared to their non-cancer counterpart (2, 4, 5). On the other hand, it remains unclear whether TTS worsens the prognosis of cancer patients.
Methods
To assess the impact of TTS on cancer mortality, we combined the data from two independent cohorts. One consisted of 318 TTS patients enrolled in a prospective multicentre registry at S. Andrea Hospital, Sapienza University and Madre Giuseppina Vannini Hospital, both in Rome, Italy, since September 1, 2006 (6). Data were extracted from the registry on December 1, 2021. TTS was defined according to the European Society of Cardiology Heart Failure Association criteria (7). The second cohort was extrapolated from an all-comer population evaluated at two Cardio-Oncology Outpatient Clinics (IRCCS Ospedale Policlinico San Martino, Genova, Italy and S. Andrea Hospital, Sapienza University, Rome, Italy) since January 1, 2015. This latter cohort consisted of 1,024 oncologic patients referred for a baseline Cardio-Oncologic evaluation, who did not have cardiovascular conditions at the time of the cardio-oncologic visit.
From the TTS registry, we selected patients with either active cancer or cancer diagnosed within 5 years before the TTS event, hereafter defined as cancer-TTS patients. Next, we matched these patients with those from the cardio-oncologic cohort (cancer non-TTS patients) in a 1:2 fashion by age, sex and type and cancer staging (i.e., metastatic vs. non-metastatic).
Statistical analysis was performed with SPSS version 25. Continuous variables were compared by Student’s t-test; categorical variables by chi-squared test. The influence of TTS on all-cause mortality in cancer patients was assessed by means of Cox regression analysis and the Kaplan Meier method. Follow-up time was calculated from TTS or cancer diagnosis up to last evaluation or death, whichever came first. Secondarily, we also studied the relationship between cancer and all-cause mortality in the TTS cohort. For this analysis, follow-up began at the time of TTS diagnosis. A two-sided p-value < 0.05 was considered statistically significant. The study was conducted in compliance with the Declaration of Helsinki. As an observational retrospective study, it did not need full Ethics Committee approval; an informed consent for the use of medical data for research purposes was obtained from all participants.
Results
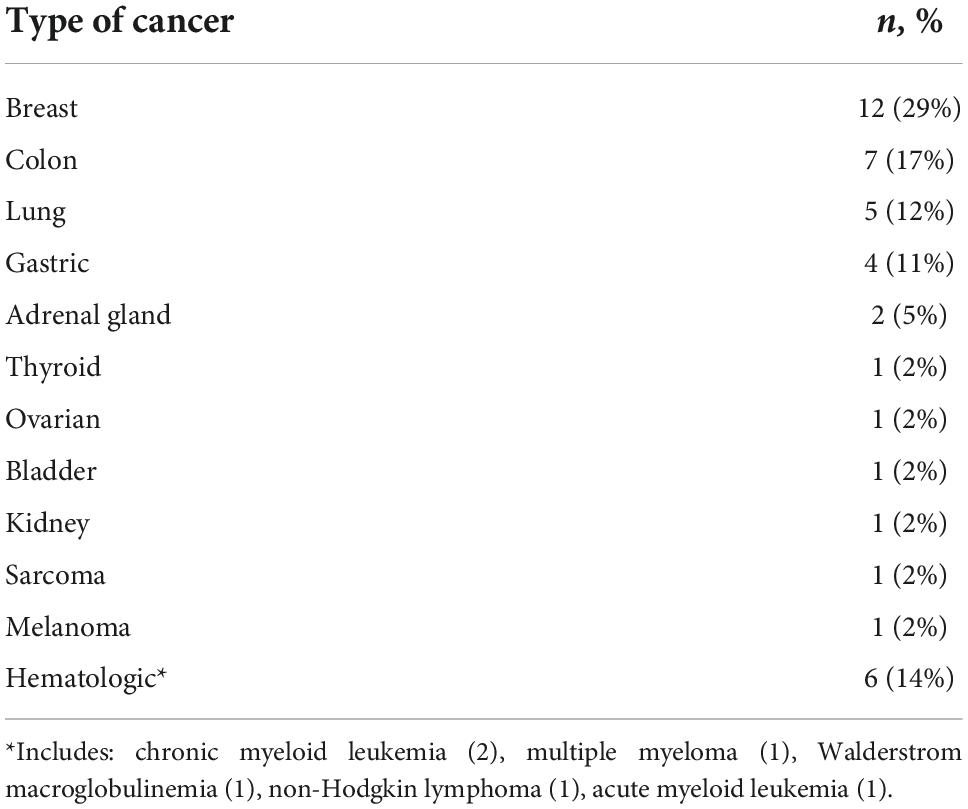
Among 318 TTS patients (285 [90%] females, aged 72 ± 11 years, mean left ventricular ejection fraction: 40 ± 9%), 42 (13%) had a concurrent diagnosis of cancer. Types of cancer are reported in Table 1.
Influence of takotsubo syndrome on oncologic patients’ mortality
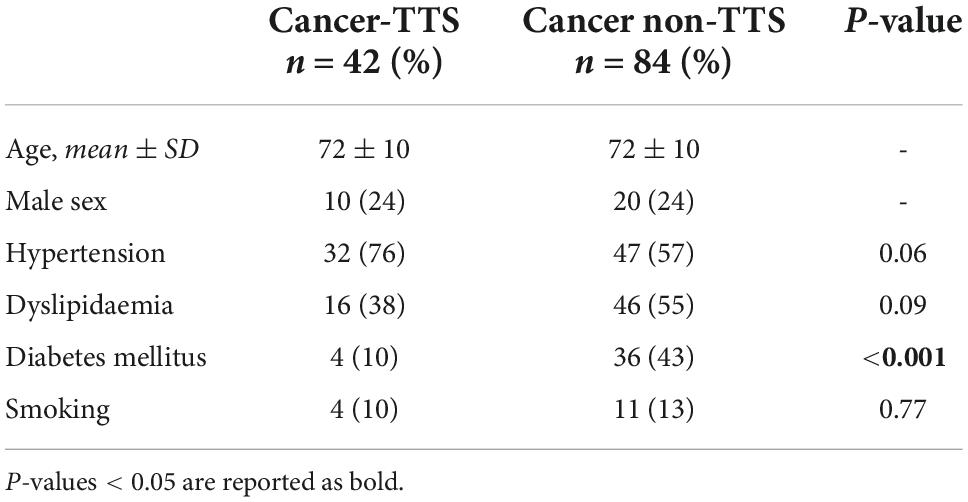
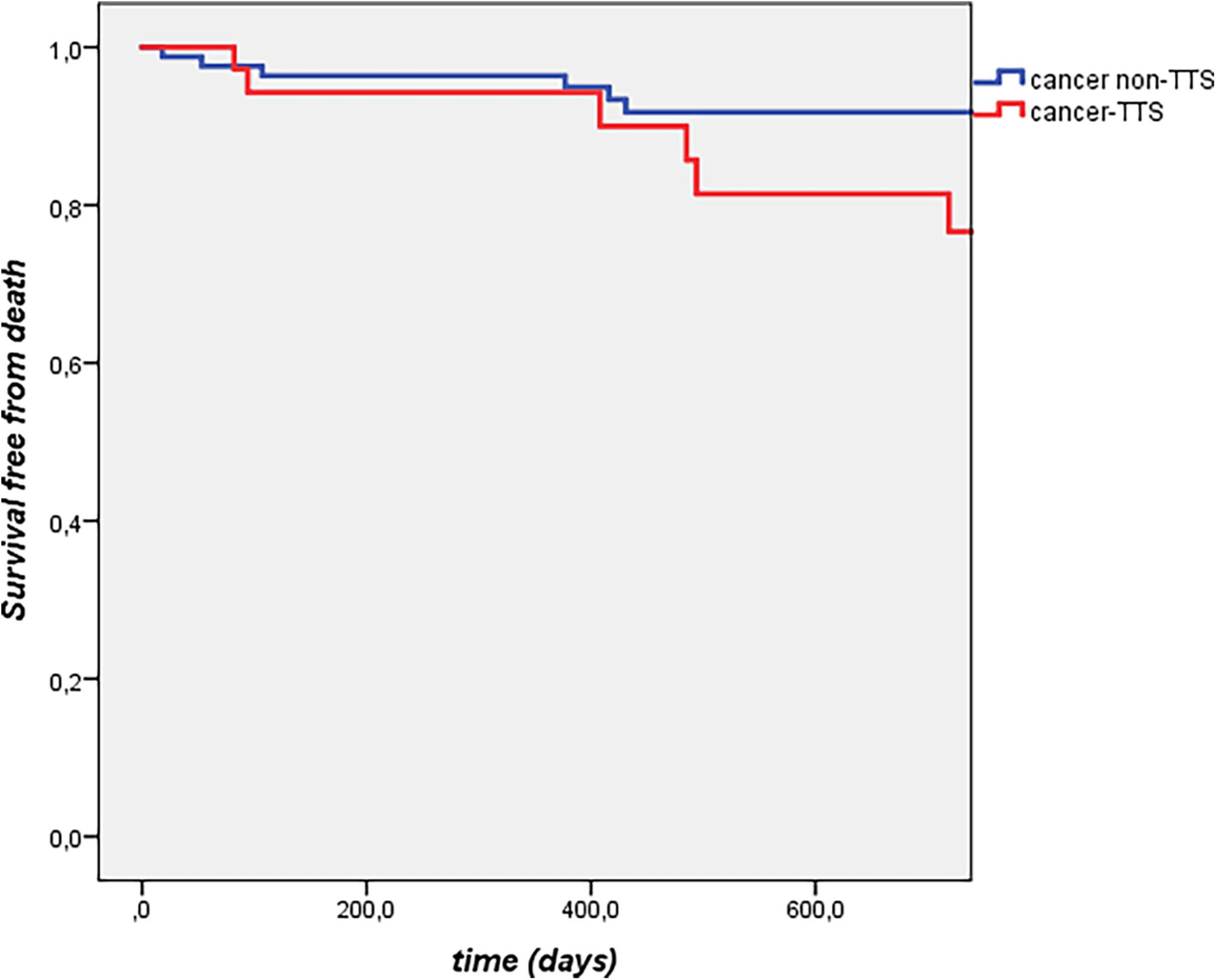
Features of cancer-TTS patients and of the 84 matched cancer non-TTS subjects are reported in Table 2. Arterial hypertension, dyslipidaemia, and smoking were similarly distributed between the two groups, whilst diabetes mellitus was more common in cancer non-TTS patients. Length of follow-up was comparable in the two groups (median: 1.2 [0.2–3.3] vs. 1.9 [1.0–3.3] years, p = 0.08). All-cause mortality was similar between cancer-TTS and cancer non-TTS patients, with a 1-year incidence of 4.8 vs. 3.5%, respectively. At Cox regression analysis, TTS was not associated with mortality (OR 1.4, 95% CI 0.6–3.3, p = 0.43; p log = 0.43, Figure 1).
Influence of cancer on takotsubo syndrome patients’ mortality
There were no significant differences between TTS patients with and without cancer in terms of age, sex, cardiovascular risk factors, type of trigger, left ventricular ejection fraction at presentation and presence of atrial fibrillation (p > 0.05 for all, data not shown). During a median follow-up of 2.7 [0.5–6.5] years, 42 patients died, 10 (23.8%) with and 32 (11.6%) without cancer (p = 0.03). A diagnosis of cancer was associated with all-cause mortality at Cox regression analysis (OR 4.6, 95% CI 2.2–9.7, p < 0.0001), even after adjustment for age and sex (OR 3.1, 95% CI 1.3–6.9, p = 0.01).
Discussion
Takotsubo syndrome does not influence the long-term prognosis of cancer patients. Our findings show that cancer-TTS and cancer non-TTS patients have a similar incidence of mortality, suggesting that even in the presence of an acute cardiovascular event (acute heart failure due to TTS), the prognosis of oncologic patients with active cancer is not substantially modified and that it is the malignancy that drives the outcome (8). In addition, our data confirm that TTS patients with cancer have a greater mortality as compared to TTS patients without, as already shown in previous studies (2, 4, 5). Long-term mortality in TTS is known to be burdened by non-cardiovascular comorbidities and, hence, non-cardiovascular deaths (2, 3, 9).
In real-world practice cardiovascular comorbidities or acute events are frequently perceived as debilitating when caring for a cancer patient (10). This may impact management and treatments (which may be halted, influencing the oncologic prognosis), and is particularly true in the case of heart failure (11), but has been postulated also in TTS (4, 12). Nevertheless, since the prevalence of malignancy in heart failure and in TTS is not low, as seen also in our cohort (11, 13, 14), and similarly is the prevalence of cardiovascular conditions and risk factors in oncologic patients (10), an integrated approach caring for bidirectional cardiovascular and oncologic needs appears fundamental, though frequently challenging to be pursued (15). In fact, dedicated guidelines for management of cancer patients in cardiovascular settings are lacking, and oncologic patients are often under-represented or not adequately phenotyped in cardiovascular clinical trials, and viceversa (11, 13, 16).
In this perspective, the fact that real-world cancer-TTS patients do not have a worse prognosis as compared to cancer non-TTS ones, might reassure oncologists who in their practice encounter patients experiencing, or who had experienced, an acute cardiovascular event as TTS. Moreover, given the clinical and epidemiological scenario depicted above, our findings further highlight the importance of collaboration between specialists, with the aim of not to undertreat cancer patients with cardiovascular comorbidities.
We acknowledge some shortcomings of our analysis. The registries from which the two matched groups have been extracted partly span different years. Moreover, the TTS one is a prospective registry, while cancer non-TTS patients were extracted from a retrospective cohort. Information about therapies and frailty or performance status in cancer patients were not available for all patients and thus were not included in the analysis. Finally, the two matched groups have a small size, possibly influencing statistical calculations. Our results should thus be considered hypothesis-generating, and we warrant replication in other cohorts. However, to our knowledge this is the first registry study comparing long-term outcome of TTS patients with cancer, with an oncologic counterpart, rather than with patients without cancer. Our considerations are not necessarily generalizable to any cardiovascular event outside the TTS context, and each one (i.e., acute myocardial infarction) likely deserves dedicated analyses. Nevertheless, it has frequently been reported that cardiovascular conditions in cancer patients are overlooked or undertreated (10). Given the significant improvements in cardiovascular and oncologic treatments, such a simplistic management is not anymore justified in clinical practice and needs to be addressed by the scientific community.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to GT, Z2lhY29tby50aW5pbWVsYXRvQHVuaXJvbWExLml0; LA, bHVjYS5hcmNhcmk4OEBnbWFpbC5jb20=.
Author contributions
GT and LA contributed to conception of the study. GT, LA, PS, BM, PA, and LC contributed to the design of the study. GT, LA, and MS organized the database. GT performed the statistical analysis and wrote the first draft of the manuscript. All authors contributed to manuscript revision and read and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Stepien K, Nowak K, Szlosarczyk B, Nessler J, Zalewski J. Clinical characteristics and long-term outcomes of MINOCA accompanied by active cancer: a retrospective insight into a cardio-oncology center registry. Front Cardiovasc Med. (2022) 9:785246. doi: 10.3389/fcvm.2022.785246
2. Möller C, Stiermaier T, Graf T, Eitel C, Thiele H, Burgdorf C, et al. Prevalence and long-term prognostic impact of malignancy in patients with takotsubo syndrome. Eur J Heart Fail. (2018) 20:816–8. doi: 10.1002/ejhf.868
3. Pelliccia F, Parodi G, Greco C, Antoniucci D, Brenner R, Bossone E, et al. Comorbidities frequency in takotsubo syndrome: an international collaborative systematic review including 1109 patients. Am J Med. (2015) 128:654.e11–9. doi: 10.1016/j.amjmed.2015.01.016
4. Cammann VL, Sarcon A, Ding KJ, Seifert B, Kato K, Di Vece D, et al. Clinical features and outcomes of patients with malignancy and takotsubo syndrome: observations from the international takotsubo registry. J Am Heart Assoc. (2019) 8:e010881. doi: 10.1161/JAHA.118.010881
5. Sattler K, El-Battrawy I, Lang S, Zhou X, Schramm K, Tülümen E, et al. Prevalence of cancer in takotsubo cardiomyopathy: short and long-term outcome. Int J Cardiol. (2017) 238:159–65. doi: 10.1016/j.ijcard.2017.02.093
6. Arcari L, Cacciotti L, Limite LR, Russo D, Sclafani M, Semeraro R, et al. Clinical characteristics of patients with takotsubo syndrome recurrence: an observational study with long-term follow-up. Int J Cardiol. (2021) 329:23–7. doi: 10.1016/j.ijcard.2020.12.047
7. Lyon AR, Bossone E, Schneider B, Sechtem U, Citro R, Underwood SR, et al. Current state of knowledge on takotsubo syndrome: a position statement from the taskforce on takotsubo syndrome of the heart failure association of the European society of cardiology: current state of knowledge on takotsubo syndrome. Eur J Heart Fail. (2016) 18:8–27. doi: 10.1002/ejhf.424
8. Giza DE, Lopez-Mattei J, Vejpongsa P, Munoz E, Iliescu G, Kitkungvan D, et al. Stress-induced cardiomyopathy in cancer patients. Am J Cardiol. (2017) 120:2284–8. doi: 10.1016/j.amjcard.2017.09.009
9. Limite LR, Arcari L, Cacciotti L, Russo D, Musumeci MB. Cardiogenic shock in takotsubo syndrome: a clue to unravel what hides behind the curtain? JACC Heart Fail. (2019) 7:175–6. doi: 10.1016/j.jchf.2018.11.003
10. Tini G, Sarocchi M, Tocci G, Arboscello E, Ghigliotti G, Novo G, et al. Arterial hypertension in cancer: the elephant in the room. Int J Cardiol. (2019) 281:133–9. doi: 10.1016/j.ijcard.2019.01.082
11. Ameri P, Canepa M, Anker MS, Belenkov Y, Bergler-Klein J, Cohen-Solal A, et al. Cancer diagnosis in patients with heart failure: epidemiology, clinical implications and gaps in knowledge. Eur J Heart Fail. (2018) 20:879–87. doi: 10.1002/ejhf.1165
12. Keramida K, Farmakis D, Filippatos G. Cancer and takotsubo syndrome: from rarity to clinical practice. ESC Heart Fail. (2021) 8:4365–9. doi: 10.1002/ehf2.13741
13. Tini G, Bertero E, Signori A, Sormani MP, Maack C, De Boer RA, et al. Cancer mortality in trials of heart failure with reduced ejection fraction: a systematic review and meta-analysis. J Am Heart Assoc. (2020) 9:e016309. doi: 10.1161/JAHA.119.016309
14. Brunetti ND, Tarantino N, Guastafierro F, De Gennaro L, Correale M, Stiermaier T, et al. Malignancies and outcome in takotsubo syndrome: a meta-analysis study on cancer and stress cardiomyopathy. Heart Fail Rev. (2019) 24:481–8. doi: 10.1007/s10741-019-09773-6
15. Tini G, Ameri P, Buzzatti G, Sarocchi M, Murialdo R, Guglielmi G, et al. Diversity of cardiologic issues in a contemporary cohort of women with breast cancer. Front Cardiovasc Med. (2021) 8:654728. doi: 10.3389/fcvm.2021.654728
Keywords: takotsubo (stress) cardiomyopathy, cardio-oncology, cancer, CV health, heart failure
Citation: Tini G, Arcari L, Sclafani M, Spallarossa P, Camastra G, Battistoni A, Autore C, Volpe M, Musumeci B, Ameri P and Cacciotti L (2022) Exploring the influence of takotsubo syndrome on oncologic patients’ mortality. Front. Cardiovasc. Med. 9:1020078. doi: 10.3389/fcvm.2022.1020078
Received: 15 August 2022; Accepted: 17 October 2022;
Published: 02 November 2022.
Edited by:
Aaron L. Sverdlov, University of Newcastle, AustraliaReviewed by:
Jaroslaw Zalewski, Jagiellonian University Medical College, PolandIvan J. Nuñez Gil, Hospital Clínico San Carlos, Spain
Efstratios Koutroumpakis, University of Texas MD Anderson Cancer Center, United States
Copyright © 2022 Tini, Arcari, Sclafani, Spallarossa, Camastra, Battistoni, Autore, Volpe, Musumeci, Ameri and Cacciotti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giacomo Tini, Z2lhY29tby50aW5pbWVsYXRvQHVuaXJvbWExLml0
 Giacomo Tini
Giacomo Tini Luca Arcari
Luca Arcari Matteo Sclafani1
Matteo Sclafani1 Paolo Spallarossa
Paolo Spallarossa Allegra Battistoni
Allegra Battistoni Camillo Autore
Camillo Autore Massimo Volpe
Massimo Volpe Pietro Ameri
Pietro Ameri