- 1Clinic for Cardiology, University Clinical Center of Serbia, Belgrade, Serbia
- 2School of Medicine, University of Belgrade, Belgrade, Serbia
- 3Department of Health Promotion, Mother and Child Care, Internal Medicine and Medical Specialties (ProMISE), University of Palermo, Palermo, Italy
- 4Royal Brompton & Harefield NHS Foundation Trust, London, United Kingdom
- 5Serbian Academy of Sciences and Arts, Belgrade, Serbia
- 6Department of Internal Medicine, Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia
- 7Dedinje Cardiovascular Institute, Belgrade, Serbia
Background: The COMET-CTO trial was a randomized prospective study that assessed long-term follow-up in patients with chronic total occlusion (CTO) in coronary arteries treated with percutaneous coronary intervention (PCI) or with optimal medical therapy (OMT). During the 9-month follow-up, the incidence of major adverse cardiac events (MACE) did not differ between the two groups; no death or myocardial infarction (MI) was observed. There was a significant difference in quality of life (QoL), assessed by the Seattle Angina Questionnaire (SAQ), in favor of the PCI group. Here we report long-term follow-up results (56 ± 12 months).
Methods: Between October 2015 and May 2017, a total of 100 patients with CTO were randomized into two groups of 50 patients: PCI CTO or OMT group. The primary endpoint of the current study was the incidence of MACE defined as cardiac death, MI, and revascularization [PCI or coronary artery bypass graft (CABG)]. As the secondary exploratory outcome, we analyzed all the cause-mortality rate.
Results: Out of 100 randomized patients, 92 were available for long-term follow-up (44 in the PCI group and 48 in the OMT group). The incidence of MACE did not differ significantly between the two groups (p = 0.363). Individual components of MACE were distributed, respectively: cardiac death (OMT vs. PCI group, 6 vs. 3, p = 0.489), MI (OMT vs. PCI group, 1 vs. 0, p = 1), and revascularization (PCI: OMT vs. PCI group, 2 vs. 2, p = 1; CABG: OMT vs. PCI group, 1 vs. 1, p = 1). There was no significant difference between the two groups regarding the individual component of MACE. Six patients died from non-cardiac causes [five deaths were reported in the OMT group and one death in the PCI group (p = 0.206)]. Kaplan-Meier survival curves for MACE did not differ significantly between the study groups (log-rank 0.804, p = 0.370). Regarding the secondary exploratory outcome, a total of 15 patients died at 56 ± 12 months (11 in the OMT and 4 in the PCI group) (p = 0.093). The Kaplan-Meier survival curves for all-cause mortality rates did not differ significantly between the two groups (log rank 3.404, p = 0.065). There were no statistically significant differences between OMT and PCI groups in all five SAQ domains. There was a significant improvement in three SAQ domains in the PCI group: PL (p < 0.001), AF (p = 0.007), and QoL (p = 0.001).
Conclusion: After 56 ± 12 months of follow-up, the incidence of MACE, as well as QoL measured by SAQ, did not differ significantly between the PCI and OMT groups.
Introduction
Recanalization of chronic total occlusions (CTO) of the coronary arteries is certainly one of the most technically demanding procedures in interventional cardiology. Furthermore, between 15 and 20% of patients who have an indication for coronary angiography have a CTO of at least one blood vessel (1–3). However, a significantly lower percentage of these patients are candidates for percutaneous coronary intervention (4, 5). Over the years observational studies have proven that successful recanalization of CTO is associated with improved patient symptoms, quality of life, and long-term survival compared with failed recanalization (6–8). According to the observational, non-randomized data, under elective circumstances, long-term benefits of successful percutaneous coronary intervention (PCI) of CTO have been suggested: improved survival, reduced need for coronary artery bypass grafting (CABG), and a better survival of future myocardial infarctions (MI) related to non-CTO arteries (9, 10). Several randomized studies also assessed the long-term treatment outcomes of patients with CTO; however, their initial results were slightly controversial including major adverse cardiovascular events (MACE) (11–13).
COMET–CTO was one of the first randomized studies that assessed the quality of life (QoL) in patients with CTO allocated to PCI of CTO or to optimal medical therapy (OMT). The primary endpoint of the study was the QoL assessed by the Seattle Angina Questionnaire (SAQ). The results showed that there was a significant improvement in QoL in patients with one CTO on the main coronary blood vessel in patients treated with percutaneous recanalization of CTO when compared to patients randomized to OMT only (14). However, during the 9-month follow-up, the incidence of MACE was very low, with no cardiac death or MI. Therefore, the aim of this study was to determine the long-term treatment outcome (>4 years) of patients with chronic total coronary artery occlusion previously randomized to PCI of the CTO plus OMT or just to OMT. This would be one of the first research papers on this topic in elective patients.
Materials and methods
The study design, methods (including the sample size calculation), and results were described previously (14). The study was registered on ClinicalTrials.gov (NCT02964975). Shortly, the study was designed as an open-label, randomized, prospective study which included patients with a single chronically occluded epicardial coronary artery. Between October 2015 and May 2017, 100 patients were randomized into two groups (50 pts in each group) after signing the informed consent. They participated in the study and completed the SAQ at baseline and after the 9-month follow-up. The first group was randomized to PCI of CTO with OMT and the second group of patients was randomized to OMT only.
During the long-term follow-up, patients were contacted to assess their clinical status and their adverse events. All events were recorded in the appropriate database. For the patients we were unable to reach, information was obtained from their cardiologists, general practitioners, or hospital records. The mean follow-up time was 56 ± 12 months. The primary clinical composite endpoint was the incidence of MACE, defined as cardiovascular death, nonfatal MI, and coronary revascularization (PCI or CABG). For the secondary exploratory outcomes, we analyzed the all cause-mortality rate (15). Cardiac death was defined according to the Academic Research Consortium (ARC) criteria. MI was defined with symptoms of cardiac ischemia and a troponin level of at least one value above the 99th percentile upper reference limit according to the recent guidelines (16).
Statistical analysis
All the data were analyzed with the statistical program SPSS version 21 (SPSS, Chicago, IL). Continuous variables are presented as the mean ± SD. Categorical variables are presented as frequencies and proportions. Differences in continuous variables were assessed with Student’s t-test or the Mann–Whitney U test, following the Kolmogorov–Smirnov test. Differences in categorical variables were compared using the chi-squared test when appropriate (expected frequencies > 5; otherwise, Fisher’s exact test was used). Changes in all five components of the SAQ were tested using repeated-measures analysis of variance for each factor. SAQ domains at the baseline and after the FUP were entered as within-subject variables, whereas the study group was entered as the between-subject variable.
Results
Nine-month results
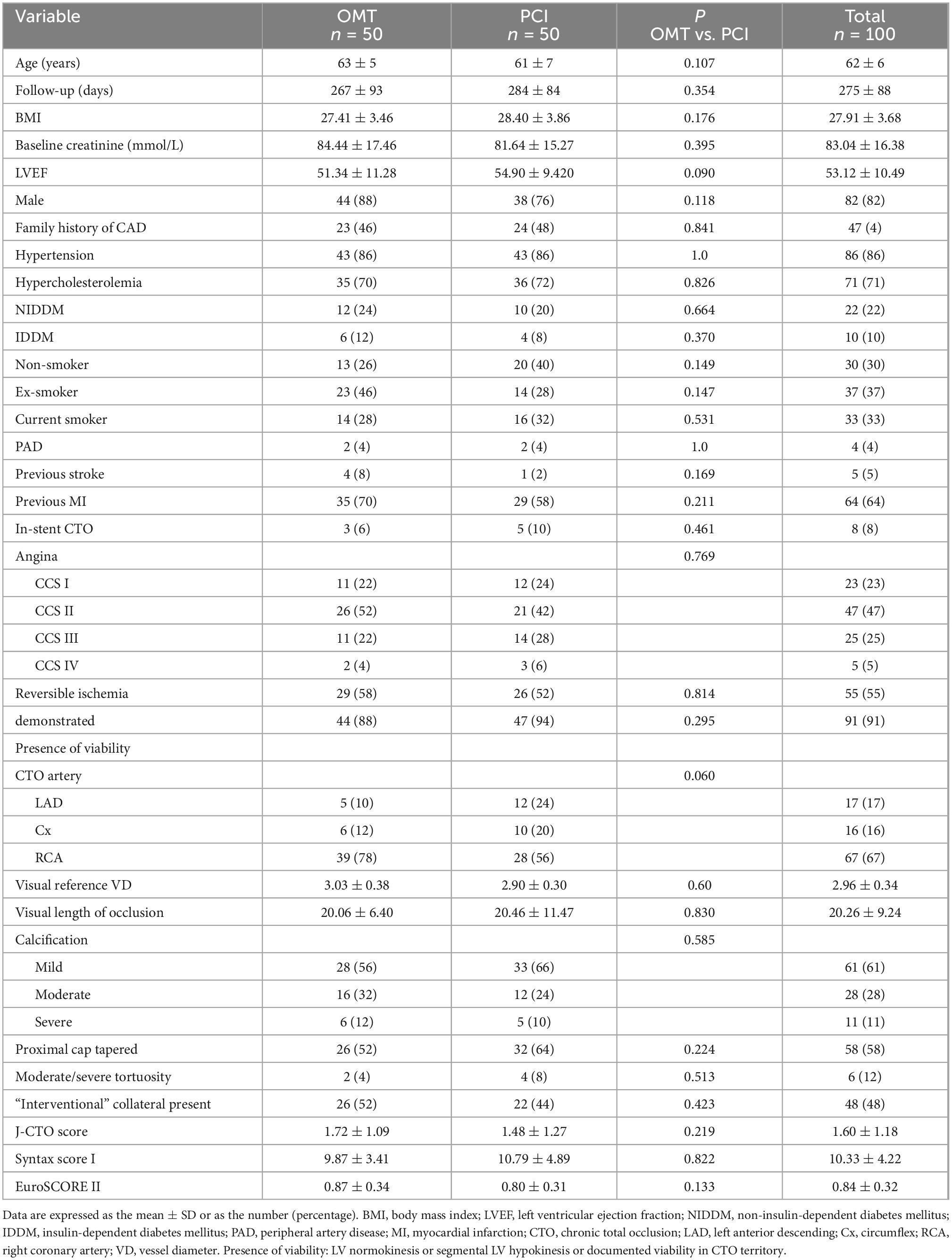
In terms of baseline characteristics, the compared groups were similar (14). Patient and lesion characteristics did not differ significantly between the groups at baseline (Table 1). The mean follow-up was 275 ± 88 days. In the PCI CTO group, 94% of patients had a successful recanalization of the occlusion. The mean number of implanted drug-eluting stents per lesion was 1.78 ± 1.02, while the mean stent diameter was 2.98 ± 0.35 mm. The mean length of implanted stents was 46.84 ± 26.80 mm. This study observed a significant improvement in QoL (in all five domains of the SAQ) in patients treated with PCI of CTO plus OMT when compared with patients treated with OMT only.
Long-term outcomes
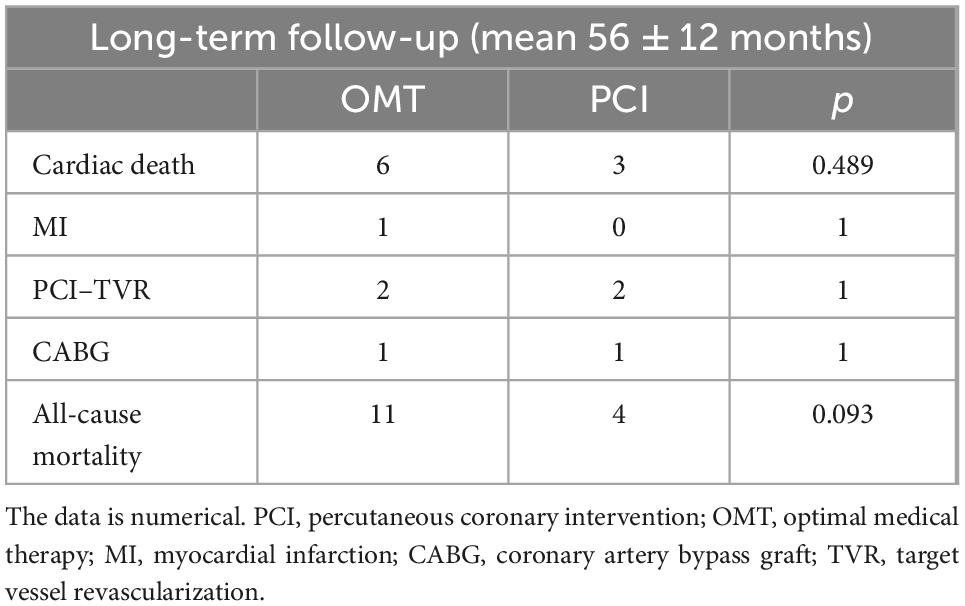
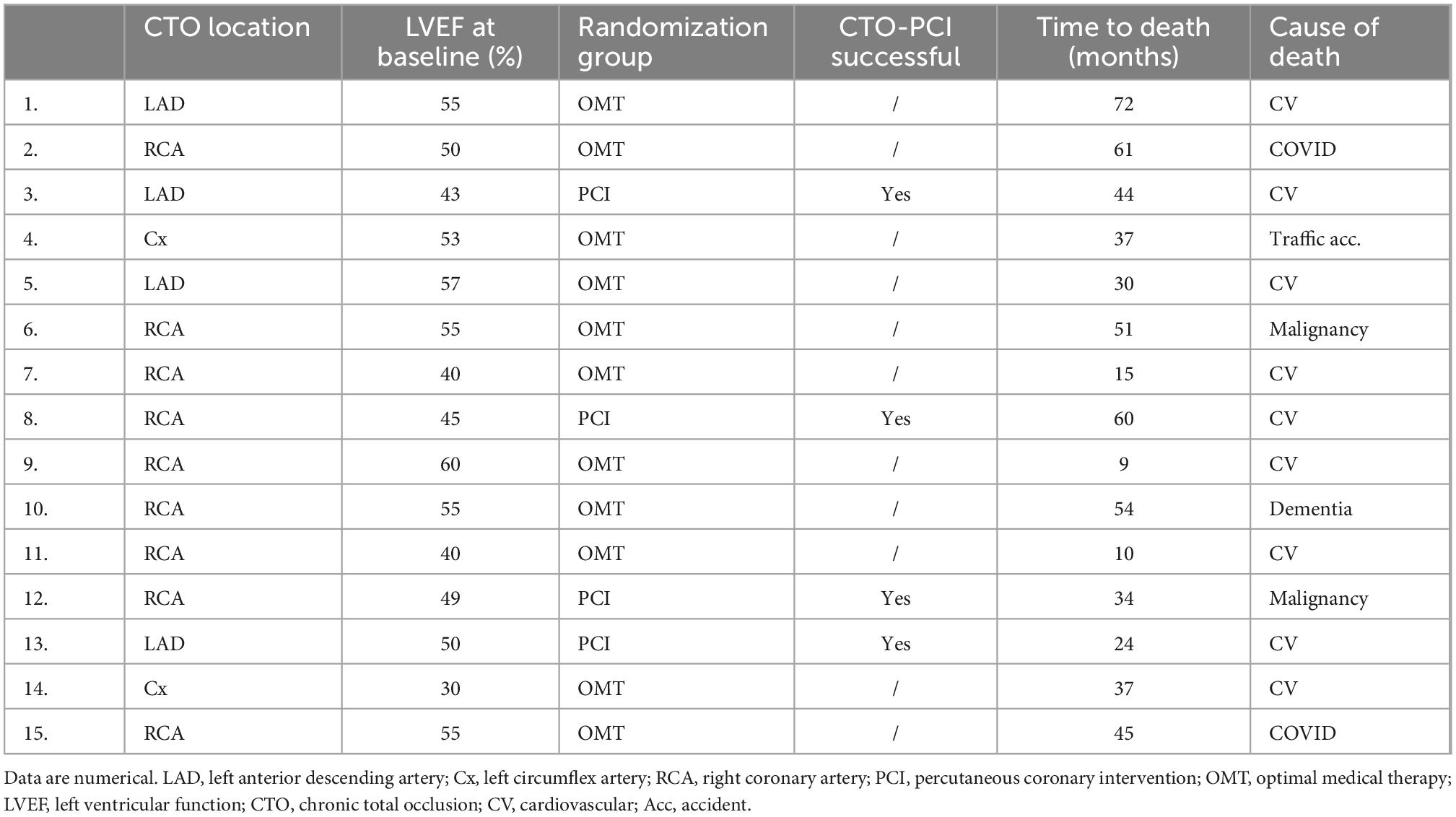
Out of 100 randomized patients, 92 were available for long-term follow-up (44 in PCI and 48 in OMT group). During the long-term follow-up, a total of 15 patients died (11 in the OMT group and 4 in the PCI group) (p = 0.093) (Table 2).
The incidence of MACE did not differ significantly between the two groups (p = 0.363). There was no statistically significant difference between the two groups regarding cardiac death, MI, or revascularization (Table 2). From the non-cardiac causes of death in the OMT group, there were five deaths, and in the PCI group, there was one death (p = 0.206). The causes of death along with some of the baseline characteristics are shown in Table 3.
The Kaplan–Meier survival curves for the MACE did not differ significantly between the two groups (Figure 1, p = 0.370). In addition, the Kaplan–Meier survival curves for all-cause mortality also did not differ significantly between the two groups (Figure 2, p = 0.065).
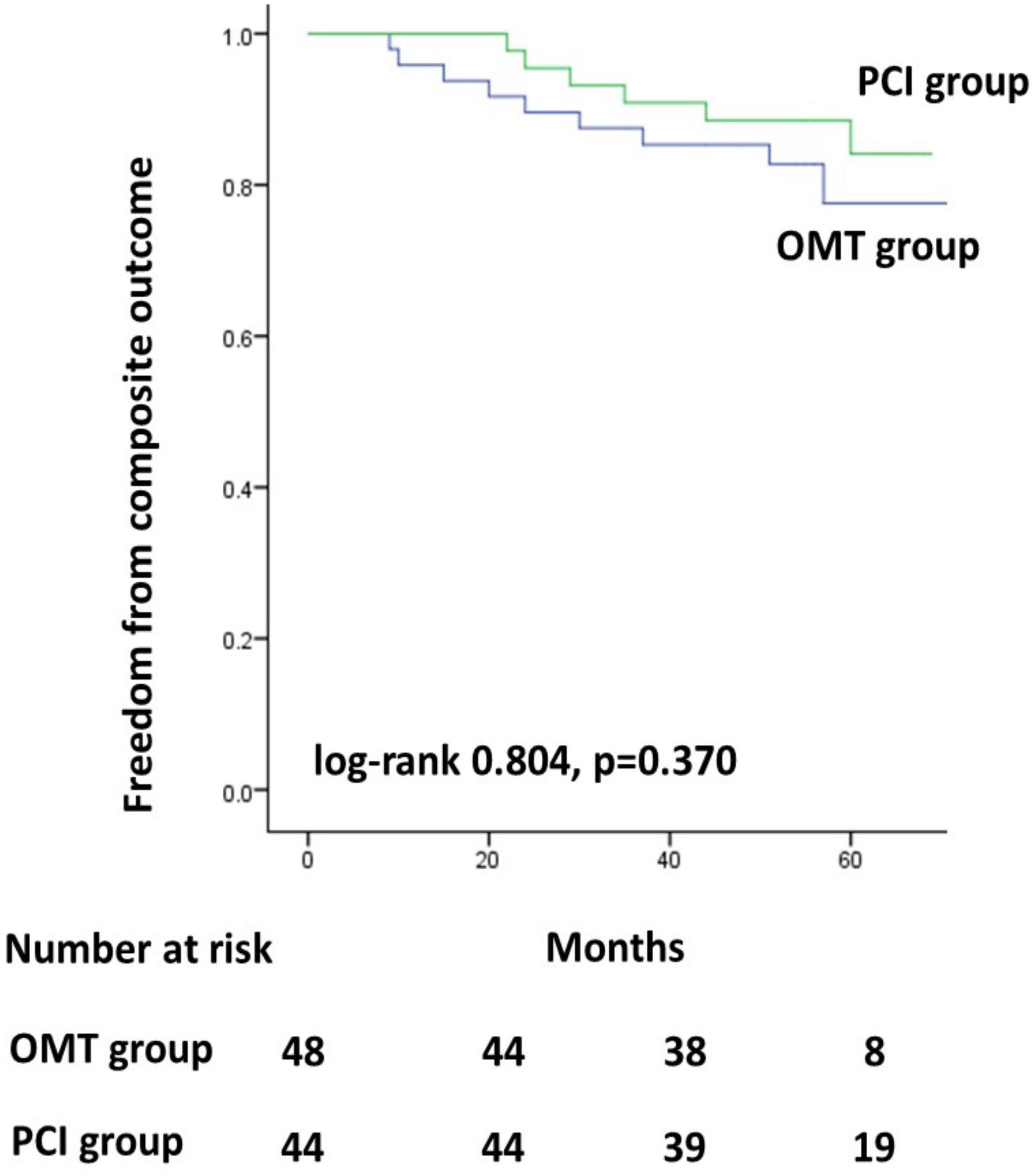
Figure 1. Kaplan–Meier survival curves for the MACE. PCI, percutaneous coronary intervention; OMT, optimal medical therapy.
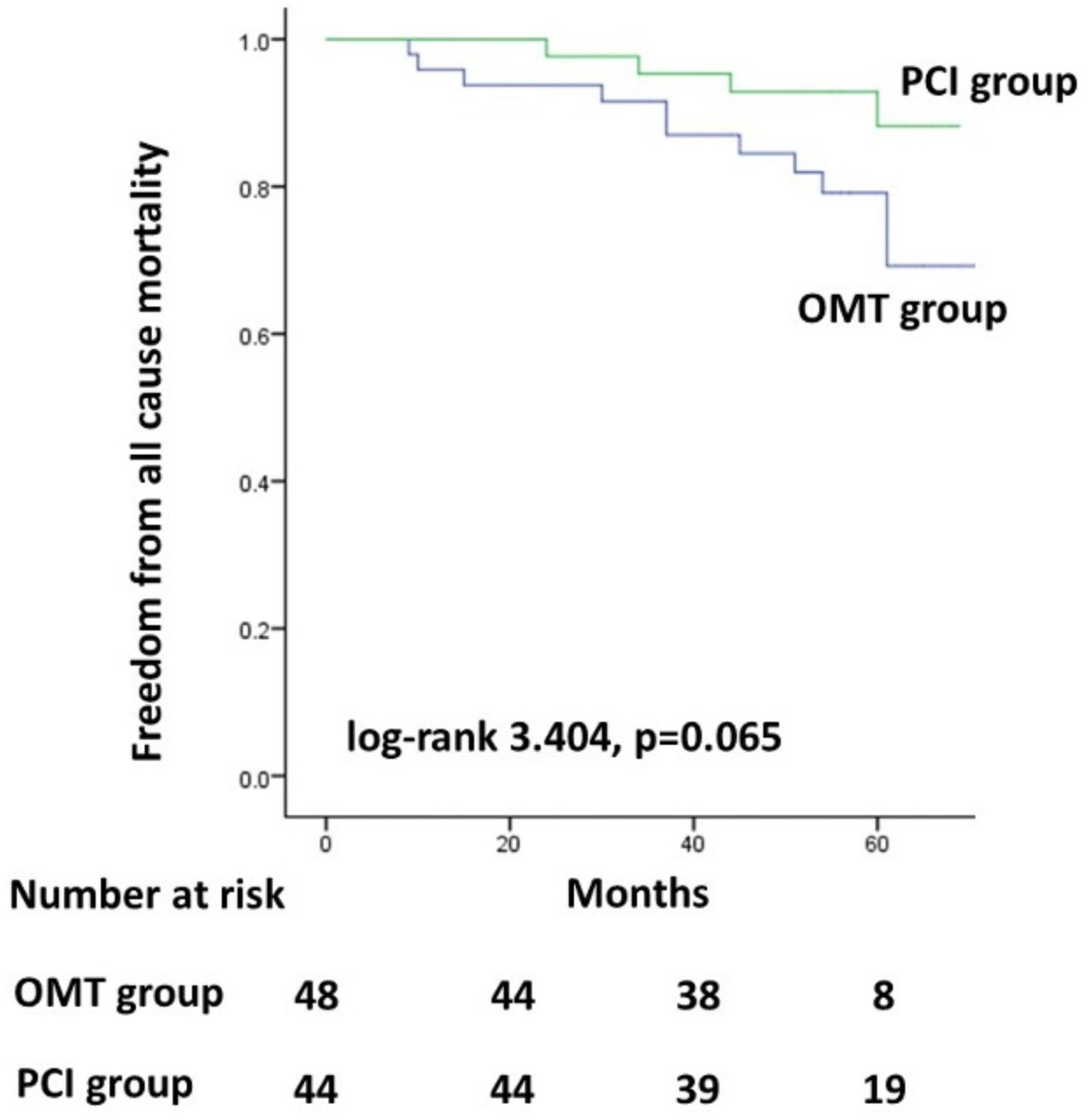
Figure 2. Kaplan–Meier survival curves for all-cause mortality. PCI, percutaneous coronary intervention; OMT, optimal medical therapy.
After the initial FUP where we had a total of three events (one CABG in the PCI group and two cross-overs in the OMT group due to anginal complaints), during the long-term FUP, there was no statistically significant difference in revascularization between the two groups (PCI: OMT vs. PCI group, 2 vs. 2, p = 1; CABG: OMT vs. PCI group, 1 vs. 1, p = 1).
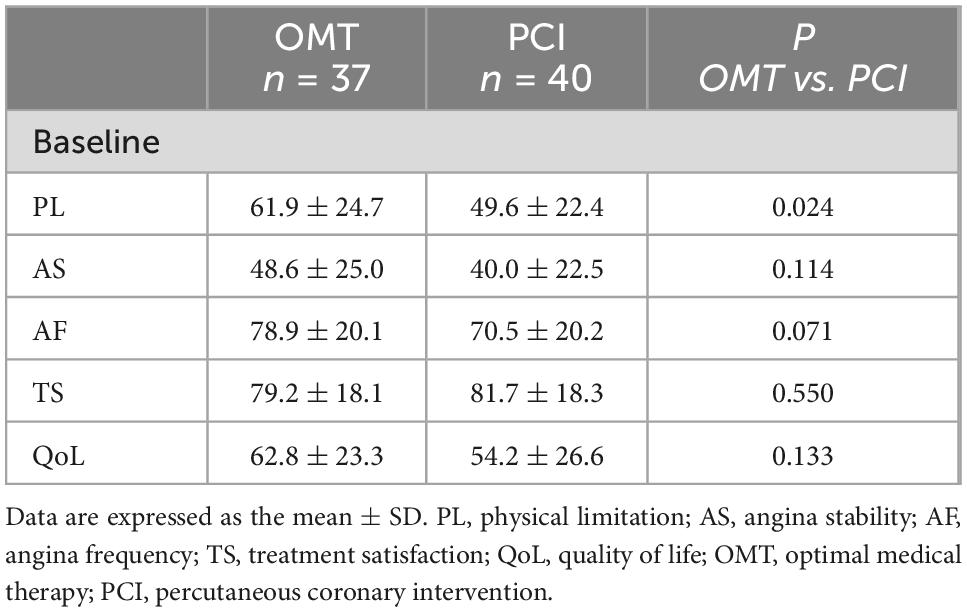
A total of 40 patients were analyzed for the SAQ in the PCI group and 37 patients in the OMT group. The scores for the five angina symptom domains at the FUP and their changes from the pre-procedural scores are reported in Figure 3. Baseline scores for a total of 77 patients were not different between the two groups, except for PL (PCI group 49.6 ± 22.4 vs. OMT group 61.9 ± 24.7, p = 0.024) (Table 4). During the FUP, there were no statistically significant differences between groups in all five SAQ domains (Figure 3). There was a significant improvement in three SAQ domains in the PCI group: PL (p < 0.001), AF (p = 0.007), and I-QoL (p = 0.001) (Figure 3).
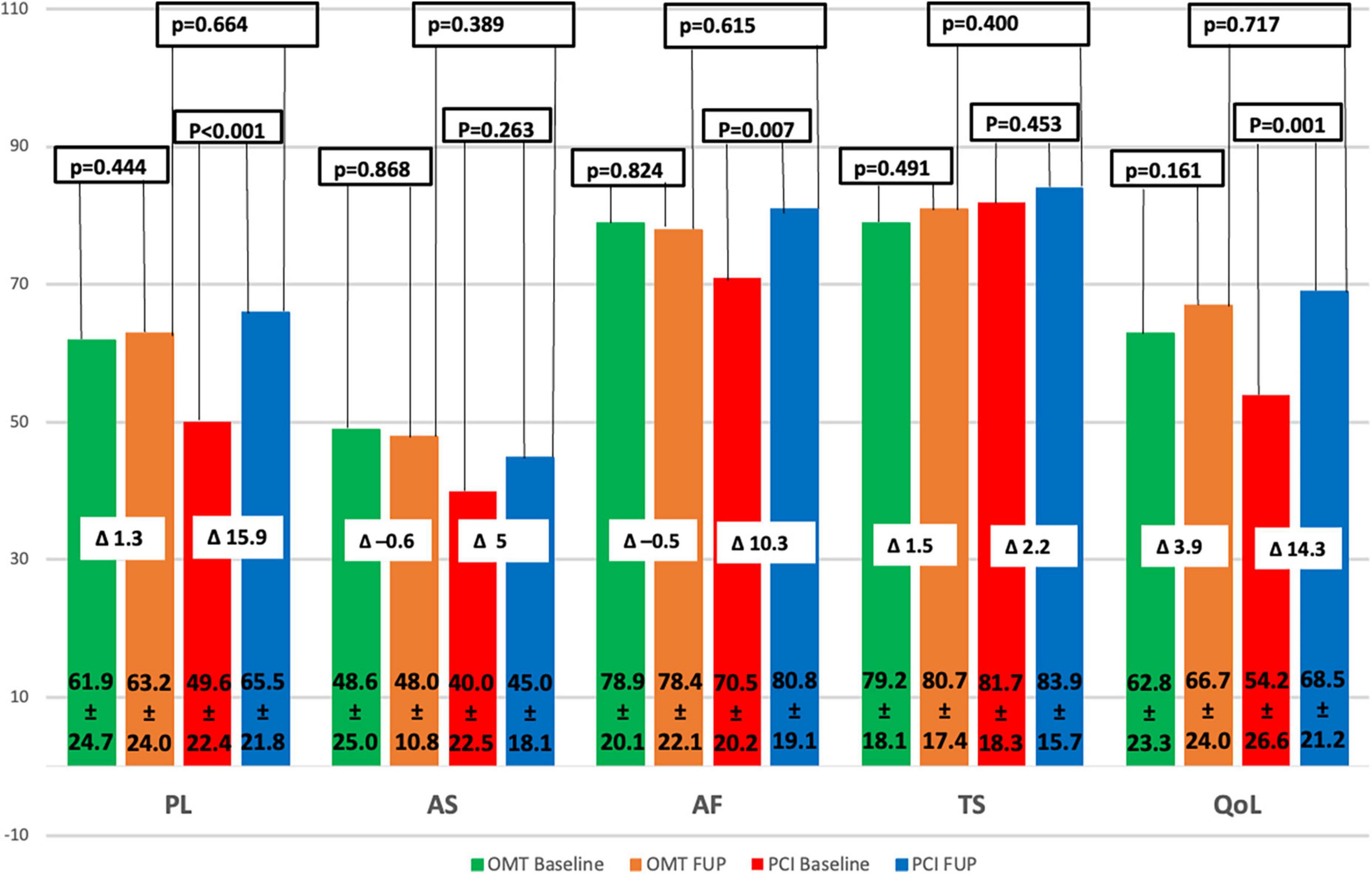
Figure 3. SAQ subscale changes. QoL, quality of life; PL, physical limitation; AS, angina stability; AF, angina frequency; TS, treatment satisfaction; PCI, percutaneous coronary intervention; OMT, optimal medical therapy; FUP, follow-up. Δ: difference between f-up and baseline mean values.
Discussion
To the best of our knowledge, COMET-CTO is a randomized study in elective CTO patients with the longest follow-up. The study has demonstrated that there was a trend to significantly lower all-cause mortality in the PCI group (p = 0.065). MACE and all the individual components of MACE did not differ significantly during the average 4.7 years of follow-up.
This study showed that QoL improved significantly in the PCI group of patients compared to the patients assigned to OMT alone. During the short-term follow-up, we observed no deaths, MIs, stent thrombosis, or strokes. However, we observed low rates of revascularization in both groups of patients. The present study extended the previous clinical outcomes from the COMET-CTO trial.
The EURO-CTO trial included 407 patients with CTO (randomization 2:1—OMT with CTO PCI or OMT, respectively) (11). In the group of patients who underwent PCI CTO, they had a significant improvement in the frequency of angina and QoL (p = 0.003 and p = 0.007), while in our study, we had a statistically significant improvement in all five domains of the SAQ. Also, the MACE rate was very similar in the EURO CTO and COMET-CTO trial during the initial follow-up.
EXPLORE (13) and DECISION-CTO (12) are two randomized studies published on this topic that did not confirm a significant reduction in MACE in the revascularized CTO group compared to the OMT group. Several things need to be addressed in both studies. Out of the 1,284 patients originally planned, only 65% (834) of the patients were included in the DECISION-CTO study. There were difficulties observed in recruiting patients which led to the main reason for the premature termination of the study. Furthermore, the significant cross-over between the two study groups (approximately one in five patients) was probably caused by the fact that PCI of non-CTO lesion was left on operator discretion before PCI of CTO. Hence, the majority of PCI of non-CTO lesions were performed after the PCI of CTO (77% of patients had multi-vessel disease).
However, overall mortality in the PCI group was lower than in the OMT group (3.0 vs. 4.4% at the 3-year follow-up and 4.5 vs. 7.9% at the 5-year follow-up). These figures did not reach statistical significance which is similar to our results.
Furthermore, in the DECISION-CTO trial, the number of patients at risk was significantly lower at the 5-year than at the 3-year follow-up (12). This could mean that the follow-up was incomplete or that a large number of patients were lost during the follow-up period. Otherwise, it is very possible that the difference would have been significant. Precisely, due to all the above-mentioned facts, the opinion of many experts in the field of CTO is that the DECISION-CTO study should not be considered as definitely negative for the primary endpoint.
In the EXPLORE trial, the MACE (composite of cardiac death, myocardial infarction, and CABG) rate did not differ significantly between the groups (13.5 vs. 12.3%, p = 0.93), during the median follow-up of 3.9 years. This finding is consistent with our results. An increasing trend without statistical significance was observed in the overall mortality of the CTO PCI group (12.9 vs. 6.9%, P = 0.11). These results should be interpreted with caution due to the small absolute number of events. Also, we cannot rule out a possibly harmful effect of PCI CTO within 7 days of an acute myocardial infarction.
Two large prospective registers, Canadian (17) and Korean (18) registers, were published in the recent years which evaluated CTO revascularization using a long-term follow-up. In the Canadian Multicenter Chronic Total Occlusion Registry 1,624 patients were assigned either to the CTO revascularized group or to the group where no revascularization of the CTO artery was performed. In the group where CTO was revascularized, there was a significantly lower mortality rate at 10 years (22.7 vs. 36.6%), lower revascularization rates (14.0 vs. 22.8%), and a shorter acute coronary syndrome hospitalizations (10.0 vs. 16.6%).
The Korean registry is a single center register with patients with CTO classified into two groups, PCI CTO (n = 883) or OMT group (n = 664), depending on the initial treatment strategy. Patients were enrolled during the period from 2003 to 2012 with typical angina or a positive functional test. At the end of the 3-year follow-up, there was no significant difference between the groups in terms of mortality due to a cardiac cause. However, between 3 and 10 years of follow-up, there was a significantly lower mortality in the revascularized group (8.3 vs. 16.6%; HR, 0.43 [95% CI, 0.27–0.71]; P < 0.001).
Furthermore, it is observed that the results of randomized studies and prospective registries are more similar for MACE when it comes to long-term follow-up.
In COMET CTO initial result of significant difference in QoL in favor of the PCI group after 9 months of F-up for all five SAQ domains, vanished during the next 4 years. In contrast, ISCHEMIA trial showed that QoL assessed by SAQ was significantly improved after 36 months of FUP (19). This discrepancy could be in a part explained by the fact that the number of patients available for QoL assessment decreased to 77 by time [numerically more patients died in the OMT group (11 pts) than in PCI group (4 pts)]. Bearing this in mind, it is not insignificant to emphasize that, in our trial, SAQ scores were numerically higher in four domains at the end of long-term FUP.
Limitations
This is a prospective randomized study conducted in a single center. This study does not have statistical power to detect differences in the incidence of major adverse cardiovascular events between the examined groups (which was considered as a secondary endpoint).
Conclusion
In patients with a single CTO treated by percutaneous coronary intervention with OMT (study group) in comparison with a group of patients only treated with OMT (control group), there was no difference observed in long-term MACE or other clinical events between the two groups. Similarly, SAQ data showed that QoL did not differ significantly between OMT and PCI groups. Further research is needed to clarify and evaluate this important area.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Medical Ethical Committee of the University Clinical Center of Serbia. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SJ, SS, and MBT contributed to drafting of the manuscript, analysis and interpretation of data, and discussions on the results. SJ, DM, MRD, MB, SA, and MPD collected the data. SS, SJ, AG, VV, GS, MVT, BB, MO, DO, and MN revised the final revision and final approval of the manuscript. All authors provided critical feedback and contributed to the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fefer P, Knudtson M, Cheema A, Galbraith P, Osherov A, Yalonetsky S, et al. Current perspectives on coronary chronic total occlusions: the Canadian multicenter chronic total occlusions registry. J Am Coll Cardiol. (2012) 59:991–7. doi: 10.1016/j.jacc.2011.12.007
2. Gössl M, Faxon D, Bell M, Holmes D, Gersh B. Complete versus incomplete revascularization with coronary artery bypass graft or percutaneous intervention in stable coronary artery disease. Circ Cardiovasc Interv. (2012) 5:597–604. doi: 10.1161/CIRCINTERVENTIONS.111.965509
3. Kahn J. Angiographic suitability for catheter revascularization of total coronary occlusions in patients from a community hospital setting. Am Heart J. (1993) 126:561–4. doi: 10.1016/0002-8703(93)90404-W
4. Azzalini L, Jolicoeur E, Pighi M, Millán X, Picard F, Tadros V, et al. Epidemiology, management strategies, and outcomes of patients with chronic total coronary occlusion. Am J Cardiol. (2016) 118:1128–35. doi: 10.1016/j.amjcard.2016.07.023
5. Brilakis E, Banerjee S, Karmpaliotis D, Lombardi W, Tsai T, Shunk K, et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National Cardiovascular Data Registry). JACC Cardiovasc Interv. (2015) 8:245–53. doi: 10.1016/j.jcin.2014.08.014
6. Galassi A, Werner G, Boukhris M, Azzalini L, Mashayekhi K, Carlino M, et al. Percutaneous recanalisation of chronic total occlusions: 2019 consensus document from the EuroCTO club. Eurointervention. (2019) 15:198–208. doi: 10.4244/EIJ-D-18-00826
7. Teramoto T, Tsuchikane E, Yamamoto M, Matsuo H, Kawase Y, Suzuki Y, et al. Successful revascularization improves long-term clinical outcome in patients with chronic coronary total occlusion. Int J Cardiol Heart Vasc. (2017) 14:28–32. doi: 10.1016/j.ijcha.2016.11.001
8. Stojkovic S, Juricic S, Dobric M, Nedeljkovic M, Vukcevic V, Orlic D, et al. Improved propensity-score matched long-term clinical outcomes in patients with successful percutaneous coronary interventions of coronary chronic total occlusion. Int Heart J. (2018) 59:719–26. doi: 10.1536/ihj.17-360
9. Christakopoulos G, Christopoulos G, Carlino M, Jeroudi O, Roesle M, Rangan BV, et al. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol. (2015) 115:1367–75. doi: 10.1016/j.amjcard.2015.02.038
10. Hoebers L, Claessen B, Elias J, Dangas G, Mehran R, Henriques J. Meta-analysis on the impact of percutaneous coronary intervention of chronic total occlusions on left ventricular function and clinical outcome. Int J Cardiol. (2015) 187:90–6. doi: 10.1016/j.ijcard.2015.03.164
11. Werner G, Martin-Yuste V, Hildick-Smith D, Boudou N, Sianos G, Gelev V, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. (2018) 39:2484–93. doi: 10.1093/eurheartj/ehy220
12. Lee S, Lee P, Ahn J, Park D, Yun S, Han S, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion: the DECISION-CTO trial. Circulation. (2019) 139:1674–83. doi: 10.1161/CIRCULATIONAHA.118.031313
13. Henriques J, Hoebers L, Råmunddal T, Laanmets P, Eriksen E, Bax M, et al. Percutaneous intervention for concurrent chronic total occlusions in patients with STEMI: the EXPLORE trial. J Am Coll Cardiol. (2016) 68:1622–32. doi: 10.1016/j.jacc.2016.07.744
14. Juricic S, Tesic M, Galassi A, Petrovic O, Dobric M, Orlic D, et al. Randomized controlled comparison of optimal medical therapy with percutaneous recanalization of chronic total occlusion (COMET-CTO). Int Heart J. (2021) 62:16–22. doi: 10.1536/ihj.20-427
15. Ybarra L, Rinfret S, Brilakis E, Karmpaliotis D, Azzalini L, Grantham J, et al. Definitions and clinical trial design principles for coronary artery chronic total occlusion therapies: CTO-ARC consensus recommendations. Circulation. (2021) 143:479–500. doi: 10.1161/CIRCULATIONAHA.120.046754
16. Thygesen K, Alpert J, Jaffe A, Chaitman B, Bax J, Morrow D, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. (2019) 40:237–69. doi: 10.1093/eurheartj/ehy856
17. Strauss B, Knudtson M, Cheema A, Galbraith P, Elbaz-Greener G, Abuzeid W, et al. Canadian multicenter chronic total occlusion registry: ten-year follow-up results of chronic total occlusion revascularization. Circ Cardiovasc Interv. (2021) 14:e010546. doi: 10.1161/CIRCINTERVENTIONS.121.010546
18. Park T, Lee S, Choi K, Lee J, Yang J, Song Y, et al. Late survival benefit of percutaneous coronary intervention compared with medical therapy in patients with coronary chronic total occlusion: a 10-year follow-up study. J Am Heart Assoc. (2021) 10:e019022. doi: 10.1161/JAHA.120.019022
Keywords: percutaneous coronary intervention, chronic total occlusion, optimal medical therapy, outcomes, long-term follow-up
Citation: Juricic SA, Stojkovic SM, Galassi AR, Stankovic GR, Orlic DN, Vukcevic VD, Milasinovic DG, Aleksandric SB, Tomasevic MV, Dobric MR, Nedeljkovic MA, Beleslin BD, Dikic MP, Banovic MD, Ostojic MC and Tesic MB (2023) Long-term follow-up of patients with chronic total coronary artery occlusion previously randomized to treatment with optimal drug therapy or percutaneous revascularization of chronic total occlusion (COMET-CTO). Front. Cardiovasc. Med. 9:1014664. doi: 10.3389/fcvm.2022.1014664
Received: 08 August 2022; Accepted: 20 December 2022;
Published: 09 January 2023.
Edited by:
Sabato Sorrentino, University of Magna Graecia, ItalyReviewed by:
Manel Sabate, Hospital Clinic of Barcelona, SpainBimmer Claessen, Amsterdam University Medical Center, Netherlands
Copyright © 2023 Juricic, Stojkovic, Galassi, Stankovic, Orlic, Vukcevic, Milasinovic, Aleksandric, Tomasevic, Dobric, Nedeljkovic, Beleslin, Dikic, Banovic, Ostojic and Tesic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sinisa M. Stojkovic,  c3N0b2prb3ZpQG10cy5ycw==
c3N0b2prb3ZpQG10cy5ycw==
 Stefan A. Juricic
Stefan A. Juricic Sinisa M. Stojkovic
Sinisa M. Stojkovic Alfredo R. Galassi
Alfredo R. Galassi Goran R. Stankovic
Goran R. Stankovic Dejan N. Orlic
Dejan N. Orlic Vladan D. Vukcevic
Vladan D. Vukcevic Dejan G. Milasinovic
Dejan G. Milasinovic Srdjan B. Aleksandric
Srdjan B. Aleksandric Miloje V. Tomasevic1,6
Miloje V. Tomasevic1,6 Milan R. Dobric
Milan R. Dobric Branko D. Beleslin
Branko D. Beleslin Marko D. Banovic
Marko D. Banovic Miodrag C. Ostojic
Miodrag C. Ostojic Milorad B. Tesic
Milorad B. Tesic