
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 17 January 2022
Sec. Cardiovascular Epidemiology and Prevention
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.800222
 Qinghao Zhao1
Qinghao Zhao1 Haiyan Xu1*†
Haiyan Xu1*† Xuan Zhang1
Xuan Zhang1 Yunqing Ye1
Yunqing Ye1 Qiuting Dong1
Qiuting Dong1 Rui Fu1
Rui Fu1 Hui Sun1
Hui Sun1 Xinxin Yan1
Xinxin Yan1 Xiaojin Gao1
Xiaojin Gao1 Jingang Yang2
Jingang Yang2 Yang Wang2
Yang Wang2 Yuejin Yang1*† on behalf of the CAMI Registry investigators
Yuejin Yang1*† on behalf of the CAMI Registry investigatorsBackground: With the growing burden of non-ST-elevation myocardial infarction (NSTEMI), developing countries face great challenges in providing equitable treatment nationwide. However, little is known about hospital-level disparities in the quality of NSTEMI care in China. We aimed to investigate the variations in NSTEMI care and patient outcomes across the three hospital levels (province-, prefecture- and county-level, with decreasing scale) in China.
Methods: Data were derived from the China Acute Myocardial Infarction Registry on patients with NSTEMI consecutively registered between January 2013 and November 2016 from 31 provinces and municipalities throughout mainland China. Patients were categorized according to the hospital level they were admitted to. Multilevel generalized mixed models were fitted to examine the relationship between the hospital level and in-hospital mortality risk.
Results: In total, 8,054 patients with NSTEMI were included (province-level: 1,698 patients; prefecture-level: 5,240 patients; county-level: 1,116 patients). Patients in the prefecture- and county-level hospitals were older, more likely to be female, and presented worse cardiac function than those in the province-level hospitals (P <0.05). Compared with the province-level hospitals, the rate of invasive strategies was significantly lower in the prefecture- and county-level hospitals (65.3, 43.3, and 15.4%, respectively, P <0.001). Invasive strategies were performed within the guideline-recommended timeframe in 25.4, 9.7, and 1.7% of very-high-risk patients, and 16.4, 7.4, and 2.4% of high-risk patients in province-, prefecture- and county-level hospitals, respectively (both P <0.001). The use of dual antiplatelet therapy in the county-level hospitals (87.2%) remained inadequate compared to the province- (94.5%, P <0.001) and prefecture-level hospitals (94.5%, P <0.001). There was an incremental trend of in-hospital mortality from province- to prefecture- to county-level hospitals (3.0, 4.4, and 6.9%, respectively, P-trend <0.001). After stepwise adjustment for patient characteristics, presentation, hospital facilities and in-hospital treatments, the hospital-level gap in mortality risk gradually narrowed and lost statistical significance in the fully adjusted model [Odds ratio: province-level vs. prefecture-level: 1.23 (0.73–2.05), P = 0.441; province-level vs. county-level: 1.61 (0.80–3.26), P = 0.182; P-trend = 0.246].
Conclusions: There were significant variations in NSTEMI presentation and treatment patterns across the three hospital levels in China, which may largely explain the hospital-level disparity in in-hospital mortality. Quality improvement initiatives are warranted, especially among lower-level hospitals.
Non-ST-elevation myocardial infarction (NSTEMI) is a major cause of death worldwide, and its incidence continues to rise in both developing and developed countries (1–4). The application of evidence-based treatment is an effective approach to reduce mortality from NSTEMI (5, 6). Over the past decades, there has been a declining trend in the in-hospital mortality of NSTEMI in some countries, primarily due to enhanced compliance with guideline-recommended management (2, 3, 7).
Despite the rapidly growing burden, quality improvement initiatives for NSTEMI care remain inadequate compared with the comprehensive efforts to improve the care for patients with ST-elevation myocardial infarction (STEMI). Recent data from Europe have reported significant hospital-level variations in the quality of NSTEMI care, with widespread suboptimal use of guideline-recommended management (7, 8). Developing countries, particularly China, may face greater challenges in providing optimal and equitable treatment across the nation due to the vast geographic area and uneven economic development (9). However, there is limited information concerning the hospital-level disparities in NSTEMI care provision, treatment patterns, and patient outcomes in China. Filling this gap will provide valuable insight for policymakers, hospital administrators, and clinical practitioners in China and other countries at a similar stage of development.
The public hospital system in China follows a traditional structure based on the Chinese government's vertical administrative model, consisting of three levels (province, prefecture, and county) in the order of decreasing scale and level (Figure 1). Province-level hospitals are usually university-affiliated academic hospitals in the capital cities of each province; prefecture-level hospitals are located in the medium-sized cities; county-level hospitals service the smallest cities usually adjacent to rural areas. In general, the bed numbers, availability of hospital facilities and staffing ratios of specialists to generalists decrease as the hospital level decreases. Thus, hospital-level comparisons of NSTEMI management are appropriate and would provide a good picture of the hierarchical performance of the healthcare system in China. Based on the China AMI (CAMI) Registry, a nationwide multicenter prospective observational study for AMI care across the three hospital levels, this study aimed to investigate the hospital-level variations in NSTEMI care and patient outcomes in China.
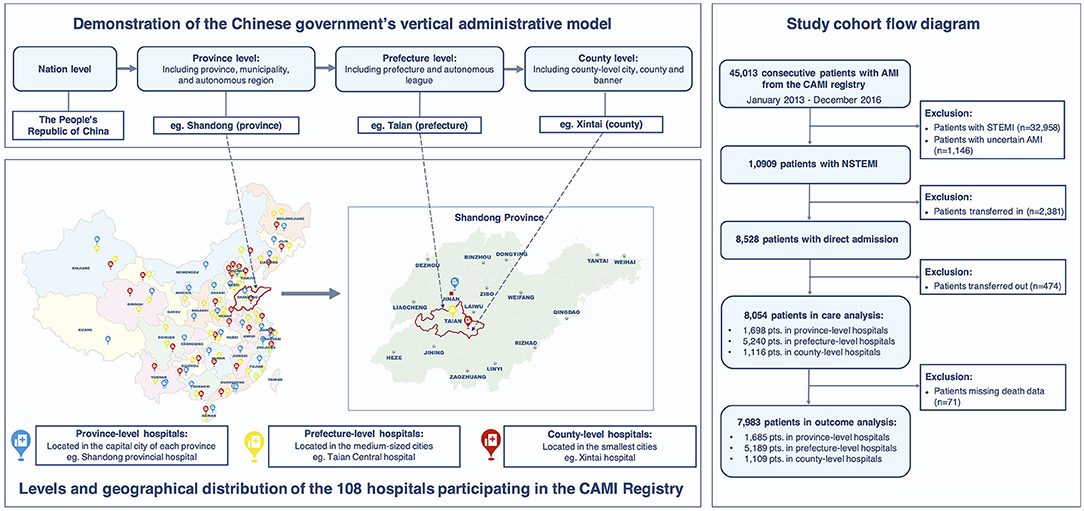
Figure 1. Demonstration of the levels and geographical distribution of the hospitals participating in the CAMI Registry and study cohort flow diagram. The Chinese public hospital system follows a three-level structure based on the Chinese government's vertical administrative model: province-level hospitals (located in the capital cities of each province, Blue marker), prefecture-level hospitals (located in the medium-sized cities, Yellow marker), and county-level hospitals (located in the smallest cities, Red marker), in the order of decreasing scale and level. The CAMI Registry included 108 hospitals covering the three hospital levels from 31 provinces and municipalities throughout Mainland China.
The study design of the CAMI Registry has been described previously (10). In brief, the CAMI registry is a prospective, nationwide, multicenter, observational study for AMI care in China. 108 hospitals from 31 provinces and municipalities throughout Mainland China participated since January 2013 (Supplementary Table 1). The participating sites were instructed to enroll consecutive patients with a primary diagnosis of AMI, with a standardized set of variables and standard definitions. The registry included 31 province-level hospitals, 45 prefecture-level hospitals, and 32 county-level hospitals with a wide geographical distribution, covering both urban and rural areas (Figure 1). These hospitals are the largest or the central hospitals in their administrative regions; therefore, a representative sample of local healthcare quality is ensured. In the province-, prefecture- and county-level hospitals, the median bed number in the cardiology units was 122, 83, and 47, respectively; the availability rate of the cardiac-coronary care unit (CCU) was 100, 96, and 78%, respectively; the availability rate of the catheterization laboratory was 100, 93, and 44%, respectively.
The CAMI Registry consecutively enrolled patients with a primary diagnosis of AMI, including STEMI and NSTEMI, who were admitted within 7 days of symptoms onset. The final diagnosis of NSTEMI must meet the 3rd Universal Definition for Myocardial Infarction (11). Type 4a and 5 AMIs were not eligible. Data collection and quality control are detailed in Supplementary Methods. This project was approved by the Institution Review Board Central Committee at Fuwai Hospital, National Center for Cardiovascular Diseases of China. Written informed consent was obtained from all the eligible patients.
In total, 10,909 patients with a confirmed diagnosis of NSTEMI were consecutively enrolled from January 2013 to December 2016. To avoid referral bias and obtain true pre-hospital information, we excluded 2,381 patients who were transferred in and 474 patients who were transferred out. Thus, 8,054 patients with direct admission were included in the core cohort for the care analysis. Moreover, after further exclusion of 71 patients with missing data on death, 7,983 patients were included in the analysis of in-hospital outcomes (Figure 1).
The key variable in NSTEMI care was the use of an invasive strategy, i.e., coronary angiography with subsequent revascularization if necessary. We analyzed the procedure timing based on the risk criteria mandating invasive strategy proposed by the current ESC and AHA/ACC guidelines (5, 6). Patients were classified into the very-high-risk category (recommending an immediate invasive strategy <2 h from admission) if they presented with hemodynamic instability or cardiogenic shock, recurrent or ongoing chest pain refractory to medical treatment, life-threatening arrhythmias or cardiac arrest, mechanical complications, acute heart failure, or recurrent dynamic ST-T wave changes. Other patients were classified in the high-risk category (recommending an early invasive strategy <24 h from admission) due to the changes in cardiac biomarkers compatible with AMI. Revascularization procedures, intra-aortic balloon pump (IABP), and medications during hospitalization were also assessed. The primary outcome was in-hospital mortality. Secondary outcomes included in-hospital heart failure, cardiogenic shock, severe arrhythmias, re-infarction, cerebrovascular accident or stroke, and non-intracranial hemorrhage bleeding (detailed definitions in Supplementary Methods).
Patient characteristics, presentation, treatment, and in-hospital outcomes were compared across the three hospital levels. The normality of continuous data was tested using the Shapiro-Wilk test. Continuous variables with a non-normal distribution were expressed as the median and interquartile range (IQR) and compared using the non-parametric Kruskal-Wallis H-test. Categorical variables were presented as percentages with 95% confidence intervals (CIs) and compared using the Chi-square test. The Cochran-Armitage test was performed to examine trends in the crude rates of outcomes across the three hospital levels. To account for within-hospital clustering, we fitted multilevel generalized mixed models with hospitals as a random effect to evaluate the association between the hospital level and in-hospital mortality, adjusting for confounders as a fixed effect. To comprehensively adjust for potential confounders and avoid model over-fitting, the variables included in the adjustment models were carefully chosen. We initially examined all baseline variables by univariate analyses (Supplementary Table 8). Baseline variables with P < 0.05 in the univariate analyses or with clinical relevance reported in the previous studies were selected (12–14). The following variables were stepwise incorporated to fit the model 1-6: Model 1 adjusting for patient characteristics (age, sex, hypertension, diabetes, prior myocardial infarction, prior heart failure); Model 2 adjusting for Model 1 plus medical contact (onset-to-arrival time, means of transport); Model 3 adjusting for Model 2 plus clinical status at admission (anterior-wall infarction, systolic blood pressure, heart rate, cardiogenic shock, heart failure, cardiac arrest, Killip class); Model 4 adjusting for Model 3 plus hospital facilities (coronary care unit availability, coronary catheter lab availability); Model 5 adjusting for Model 4 plus the use of medications (aspirin, P2Y12-receptor inhibitors, statin, β-blocker, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker) and IABP; Model 6 adjusting for Model 5 plus the use of invasive strategies. We reported the odds ratios (ORs) with 95% CIs and tested the linear trend across the three hospital levels in each model. In-hospital mortality was also compared across the three hospital levels in the subgroups categorized by the guideline-recommended risk criteria and the use of invasive strategies. All variables were missing <10% and the multivariate analyses were based on the complete data. We also performed multiple imputations using a Markov chain Monte Carlo algorithm for the missing values and performed multivariate analyses based on the imputed data for sensitivity analyses (15). Statistical significance was set at two-tail P < 0.05. All analyses were performed using R 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
Of the 8,054 NSTEMI patients with direct admission, 1,698, 5,240, and 1,116 patients were admitted to province-, prefecture-, and county-level hospitals, respectively. As shown in Table 1 and Supplementary Table 3, compared with patients in the province-level hospitals, patients in the prefecture- and county-level hospitals were older, and more likely to be female and have a history of stroke, but less likely to be obese, or have smoking habits, diabetes, dyslipidemia, prior revascularization procedures, and peripheral artery diseases (all P < 0.05). Patients in the prefecture- and county-level hospitals were less likely to present ≤ 24 h after symptoms onset, with less frequency to use ambulance transportations compared to those in the province-level hospitals (both P < 0.001). At admission, more patients in the prefecture- and county-level hospitals presented with heart failure, cardiogenic shock, and Killip class III/IV compared with those in the province-level hospitals (all P < 0.05). The proportion of very-high-risk patients did not differ significantly across the three hospital levels (P = 0.285).
Compared to the province-level hospitals, the rate of invasive strategies (coronary angiography with subsequent revascularization if necessary) was significantly lower in the prefecture-level and county-level hospitals [65.3% (63.0–67.6%), 43.3% (42.0–44.7%) and 15.4% (13.2–17.5%), respectively, P < 0.001] (Table 2). Among the province-, prefecture- and county-level hospitals, 25.4% (21.9-28.9%), 9.7% (8.4-11.1%), and 1.7% (0.4-2.9%) of very-high-risk patients, and 16.4% (14.2-18.6%), 7.4% (6.5–8.3%), and 2.4% (1.2–3.5%) of high-risk patients were treated with invasive strategies within the guideline-recommended timeframe, respectively (<2 h for very-high-risk; <24 h for high-risk) (both P < 0.001 and P-trend < 0.001, Figure 2) (5, 6). During hospitalization, 57.2% (53.2–61.2%), 28.1% (26.0–30.2%), and 7.5% (5.0–10.1%) of very-high-risk patients, and 51.5% (48.5–54.5%), 34.1% (32.4–35.7%), and 13.4% (10.8–16.0%) of high-risk patients underwent revascularization in the province-, prefecture- and county-level hospitals, respectively (P < 0.001 and P-trend < 0.001, Figure 3). IABP was used more frequently in the province-level hospitals than in the prefecture- and county-level hospitals (P < 0.001). The overall use of dual antiplatelet therapy was 93.5%. However, this rate was much lower in the county-level hospitals [87.2% (85.3–89.2%)] than in the province-level [94.5% (93.4–95.6%), P < 0.001] and prefecture-level hospitals [94.5% (93.9–95.2%), P < 0.001]. Statin, β-blocker, and angiotensin-converting enzyme inhibitor/angiotensin receptor blocker (ACEI/ARB) were prescribed in 96.9, 71.7, and 63.9% of overall patients, respectively. Similarly, the use of these drugs was much lower in the county-level hospitals (93.7, 69.4, and 65.5%, respectively) compared with the province-level hospitals (97.5, 77.3, and 67.3%, respectively. All P < 0.05) (Table 2).
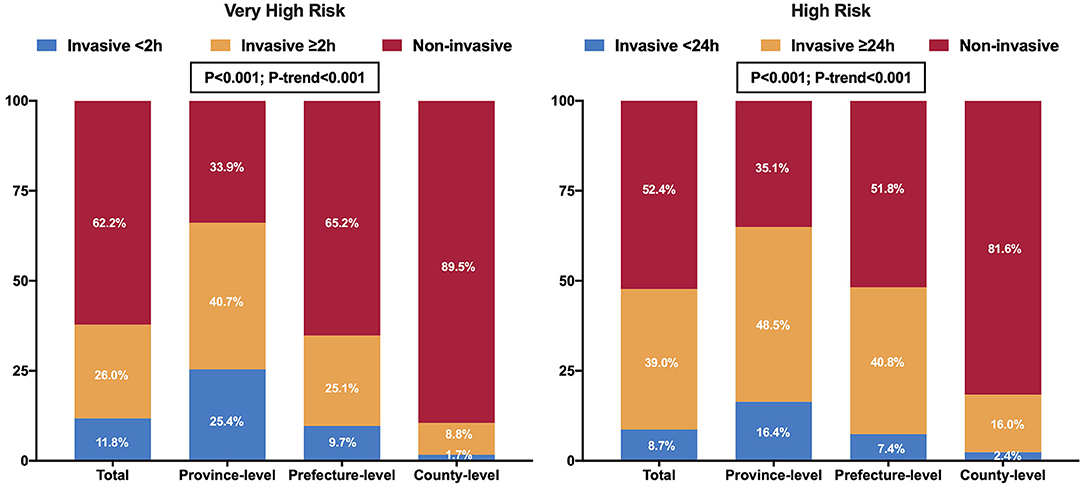
Figure 2. Utilization and timing of invasive strategies in patients with NSTEMI according to the guideline-recommended risk criteria among the three hospital levels in China.
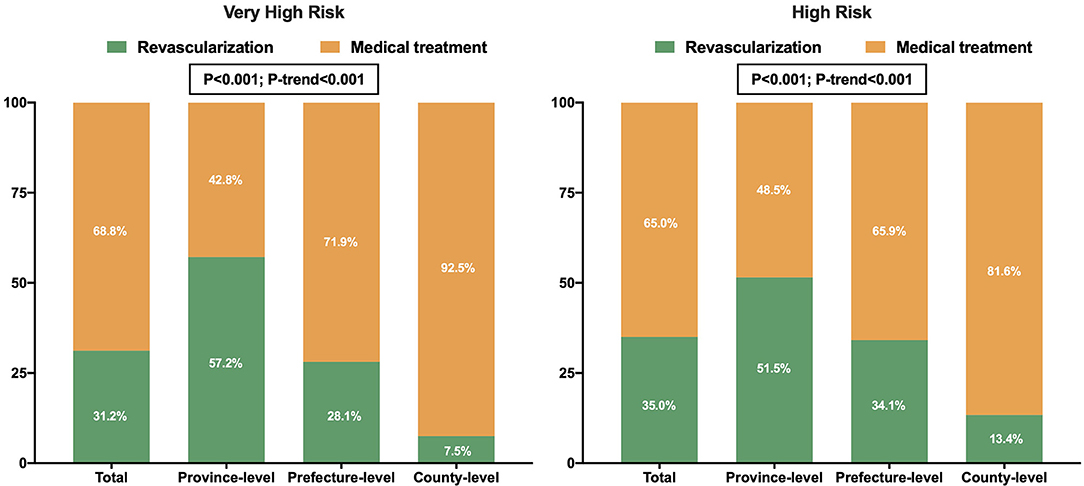
Figure 3. Revascularization rates in patients with NSTEMI according to the guideline-recommended risk criteria among the three hospital levels in China.
There was an incremental trend of in-hospital mortality from the province- to prefecture- to county-level hospitals [3.0% (2.2–3.8%), 4.4% (3.8–4.9%), 6.9% (5.4–8.4%), P-trend < 0.001, Figure 4]. Compared to the province-level hospitals, the odds of in-hospital mortality were 1.62 (95% CI: 1.03–2.56, P = 0.038) and 2.50 (95% CI: 1.49–4.17, P < 0.001) times higher for the prefecture- and county-level hospitals, respectively. This disparity persisted in the subset of very-high-risk patients (P = 0.001) and high-risk patients (P = 0.033), but was not significant in the subset of patients undergoing invasive strategies [0.7% (0.2–1.3%), 1.2% (0.7–1.6%), 1.2% (0–2.8%), P = 0.447] (Supplementary Table 6). There were similar increasing trends in the incidence of heart failure, cardiogenic shock, and severe arrhythmia across the three hospital levels (all P < 0.001 and P-trend < 0.001, Figure 4).
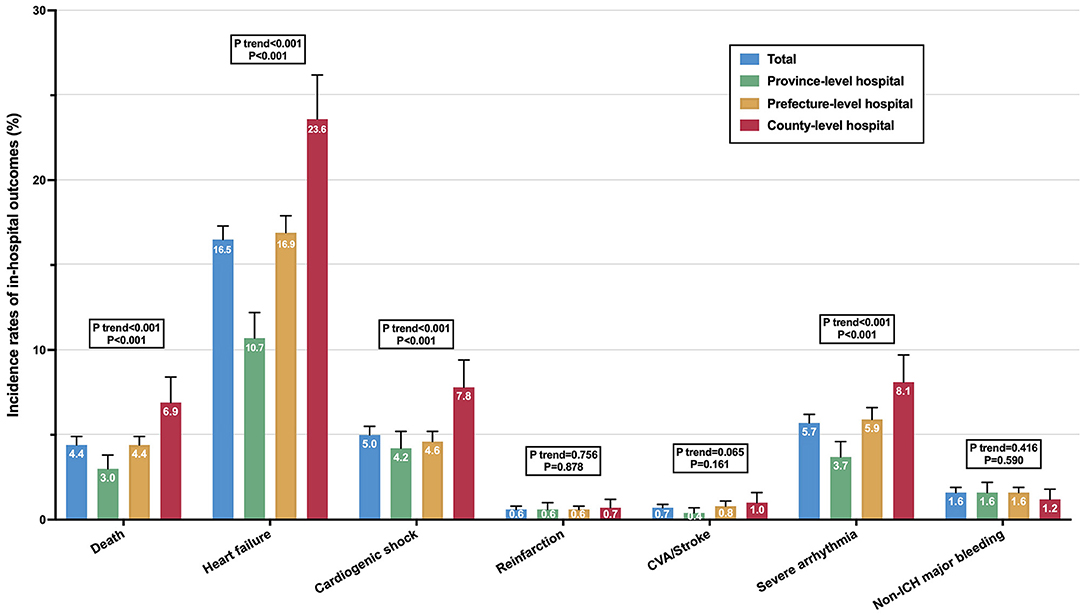
Figure 4. Incidence of in-hospital outcomes in patients with NSTEMI among the three hospital levels in China. The error bars indicate the 95% confidence interval of the sampling errors.
As Figure 5 shows, after adjustment for patient characteristics and presentation (Model 1–3), there was no significant difference in mortality risk between the province- and prefecture-level hospitals [OR (95% CI): 1.37 (0.85–2.20), P = 0.198], but the remarkable disparity between the province- and county-level hospitals persisted [OR (95% CI): 1.84 (1.07–3.17), P = 0.028]. After additional adjustment for hospital facilities and the use of medications and IABP (Model 4–5), county-level hospitals were still significantly associated with a higher mortality risk compared with the province-level hospitals [OR (95% CI): 2.08 (1.05–4.14), P = 0.036]. However, after adding invasive strategies to the model (Model 6), the gap in mortality risk between the province- and county-level hospitals remarkably narrowed, resulting in a loss of statistical significance [OR (95% CI): 1.61 (0.80–3.26), P = 0.182; P-trend = 0.246]. Similar results were observed in the sensitivity analysis based on the multiple imputation data (Supplementary Table 9). Furthermore, the use of invasive strategies was identified as the strongest protective factor for mortality of NSTEMI, as attested by its largest Wald Chi-square statistics in the fully adjusted model [OR (95% CI): 0.20 (0.13–0.31), P < 0.001, Wald Chi-square = 51.961, Supplementary Table 10].
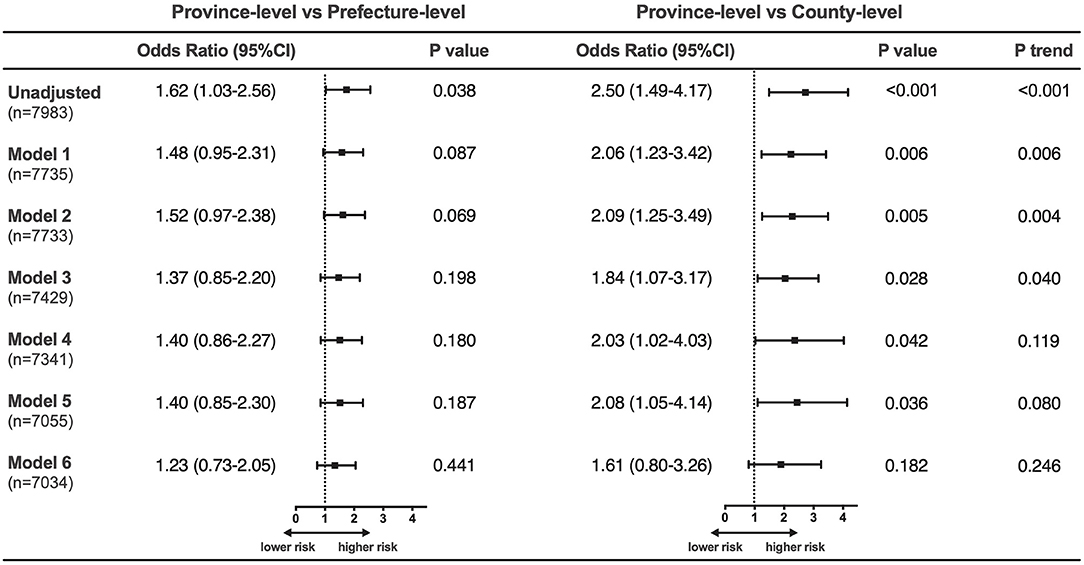
Figure 5. Adjusted in-hospital mortality risk in patients with NSTEMI among the three hospital levels. Model 1 adjusting for patient characteristics (age, sex, hypertension, diabetes, prior myocardial infarction, prior heart failure); Model 2 adjusting for Model 1 plus medical contact (onset-to-arrival time, means of transport); Model 3 adjusting for Model 2 plus clinical status at admission (anterior-wall infarction, systolic blood pressure, heart rate, cardiogenic shock, heart failure, cardiac arrest, Killip class); Model 4 adjusting for Model 3 plus hospital facilities (coronary care unit availability, coronary catheter lab availability); Model 5 adjusting for Model 4 plus the use of medications (aspirin, P2Y12-receptor inhibitors, statin, β-blocker, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker) and intra-aortic balloon pump; Model 6 adjusting for Model 5 plus the use of invasive strategies.
This study is the first national report on the hospital-level differences in NSTEMI care and patient outcomes in China. The key findings are as follows: First, invasive strategies were underused and markedly delayed in the current management of NSTEMI, especially in lower-level hospitals. Second, the overall use of dual antiplatelet therapy was high, but more improvements in county-level hospitals are desirable. Third, there was an incremental trend of in-hospital mortality with decreasing hospital levels. The hospital-level disparity in mortality could be largely explained by the wide variations in patient presentation and treatment patterns between hospitals, particularly in terms of available invasive strategies. These findings shed light on the challenges that China currently faces, and could not only serve as a basis for improving healthcare quality in China but hold valuable insights for other developing countries.
The invasive strategies have a central role in NSTEMI care (5, 6). However, the overall rate of invasive strategies in China was low (44.1%), which was markedly lower than the rate in Canada (60.2%), Denmark (63.3%), the United States (79.6%), and South Korea (91.3%) (16–18). Although the province-level hospitals showed a comparable rate of 65.3%, the prominently low rate at 15.4% in the county-level hospitals pulled the average down. There may be several reasons for the limited use of invasive strategies in lower-level hospitals. First, PCI capability varied across the three hospital levels. In our study, the catheterization laboratory was available in 44% of the county-level hospitals compared to 100% of the province-level hospitals. The lack of PCI facilities and interventional specialists directly limits the number of interventional procedures. Second, physicians in lower-level hospitals tended to adopt a more conservative strategy for patients with complex and critical conditions. We observed an inverse relationship between the revascularization rates and patient risk stratification in the prefecture- and county-level hospitals, with a similar risk-treatment paradox reported in previous studies (16, 19, 20). This paradox may be due to concerns about procedure-related complications and inadequate clinical expertise (21). Third, some subjective factors of patients, such as affordability concerns, may have also influenced the decision for or against invasive strategies, especially in lower-level hospitals (9).
Current guidelines strongly endorse the use of an early invasive strategy within 24 h of admission in patients with NSTEMI to reduce ischemic complications and length of in-hospital stay (5, 6). In particular, the invasive strategy should be performed within 2 h if the patient meets the very-high-risk criteria (5). Our study observed substantial in-hospital delays, with only 11.8% of very-high-risk patients and 8.7% of high-risk patients meeting the time targets. This rate is similar to the recent findings of a national registry in the United Kingdom (16.4%) (22), suggesting that delayed application of invasive strategies is a common issue in NSTEMI management. There may be a common time delay in identifying patients with NSTEMI due to their frequent presentation of atypical symptoms and lack of definite electrocardiographic changes. Time delays may also result from the decision-making process for invasive strategies because many NSTEMI patients have type-2 AMI for whom evidence-based treatment is still lacking (22, 23). Moreover, some time-consuming processes, including patient consent provision (patient factor) and preparations for the PCI procedure (hospital factor), may further exacerbate in-hospital delays.
Dual antiplatelet therapy, consisting of aspirin and P2Y12-receptor inhibitor, is the cornerstone of the medical management of AMI (5, 6). The China-PEACE study described a remarkable improvement in the use of evidence-based antiplatelet therapy for patients with AMI in China, with aspirin use increasing from 86.5 to 90.0% and clopidogrel use increasing from 45.7 to 79.8%, from 2006 to 2011 (24, 25). Our data collected between 2013 and 2016 showed that the use of aspirin and P2Y12-receptor inhibitor in patients with NSTEMI reached 95.6 and 96.4%, respectively. These results are comparable to the rates in developed healthcare systems (18, 22). However, the use of dual antiplatelet therapy in the county-level hospitals (87.2%) remained inadequate compared to the province- and prefecture-level hospitals (both 94.5%). The overall use of other guideline-recommended medications, including statin, β-blocker, and ACEI/ARB, was similar to that reported by the registries in Italy, Switzerland, the United States, and South Korea (18, 26, 27). However, when categorized by hospital levels, the use of statin, β-blocker and ACEI/ARB was much lower in the county-level hospitals compared with the province-level hospitals (all P < 0.05). Since few county-level hospitals are tertiary hospitals staffed with cardiovascular specialists, the lack of practitioners with condition-specific expertise may explain the underuse of evidence-based medical therapies in county-level hospitals (24, 25).
Notably, there was a significant disparity in the in-hospital mortality across the three hospital levels, with the highest mortality rate (6.9%) in the county-level hospitals while the lowest rate (3.0%) in the province-level hospitals. This disparity in mortality can only be partially explained by patient-level variations, as the remarkable differences in mortality risk between province- and county-level hospitals persisted, albeit attenuated, after adjusting for patient characteristics and presentation. Of greater importance, factors related to in-hospital care, including hospital facilities, as well as the use of medications, IABP, and invasive strategies, may be more critical determinants of in-hospital mortality. As these factors were stepwise incorporated into the model, the gap in mortality risk between hospitals gradually narrowed. However, it was not until the inclusion of invasive strategies into the model that the disparity in mortality risk between province- and county-level hospitals lost statistical significance. In the fully adjusted model, invasive strategies also had the greatest weight on in-hospital mortality (Supplementary Table 10). Moreover, in the subset of patients who underwent invasive strategies, the mortality rate was remarkably low, ranging from 0.7 to 1.2%, with no significant variations across the three hospital levels. These evidences suggest the crucial role of invasive strategies in determining mortality associated with NSTEMI. Thus, in the contemporary management of NSTEMI, addressing the inequalities in the application of invasive strategies and enhancing the rate of invasive strategies in lower-level hospitals are critical to narrow the hospital-level disparities in mortality.
As mentioned above, for future improvement in NSTEMI care in China, it is of prime importance to reduce the hospital-level inequalities in applying invasive strategies. To achieve this, more investments in the construction and staffing of catheterization laboratories are necessary to provide basic PCI facilities, thereby promoting the use of invasive strategies in lower-level hospitals. Developing regional medical combination networks with optimized processes of timely transferal of patients to PCI-capable hospitals is also a very cost-efficient approach to increase the access to PCI (28, 29). Moreover, greater emphasis should be placed on the intensive training and technical support for the interventional cardiologists in lower-level hospitals, for improving clinical practice and adapting evidence-based therapies. Beginning in 2015, China has been undertaking a major healthcare reform to build a tiered healthcare delivery system, aiming to strengthen the infrastructure in lower-level hospitals, and more importantly, developing medical alliances (30). In this model, the leading hospitals in each alliance not only serve as a centralized location for training programs and fast-track referrals, but also share responsibilities, resources, management, and economic interests with their alliance members (30). This model may help address the gaps in medical resource allocation in China and provide valuable insights for other countries at a similar point of development.
This study has certain limitations. First, as not all hospitals participated in this national registry, we could not collect all cases of NSTEMI in China. However, to objectively reflect the quality of NSTEMI care in the Chinese public medical system, our study was uniquely designed to include the hospitals across the three levels rather than the binary comparisons between urban-rural or tertiary-secondary hospitals. Therefore, our comparisons were more consistent with the medical practice pattern and administrative model in China, and can well reflect the hierarchical performance of the Chinese public medical system. Second, as an observational study, the possibility of residual measured and unmeasured confounders may be present. However, we used multilevel mixed models to account for within-hospital clustering and adjust for comprehensive variables relating to multiple facets of presentation and care to minimize bias. Third, the CAMI Registry is a hospital-based registry study that enrolled the patients admitted to hospitals but did not include outpatients. Therefore, we could only estimate the in-hospital mortality of NSTEMI but could not assess the out-of-hospital mortality.
In this large nationwide analysis of hospital-level differences in NSTEMI care and patient outcomes in China, we found that patient presentation and treatment patterns varied widely across the three hospital levels, which may largely explain the hospital-level disparities in the in-hospital mortality rates. Invasive strategies played a key role in determining mortality associated with NSTEMI. Thus, it is crucial to reduce the hospital-level inequalities in applying invasive strategies and to increase the rate of invasive strategies in patients with NSTEMI. In this scenario, national initiatives and investments in quality improvement, with a particular focus on lower-level hospitals, are warranted for the delivery of optimal and equitable care for patients with NSTEMI. Our findings provide valuable insights for policymakers and medical professionals in China and other developing countries, informing future strategies for healthcare quality improvement and medical resource allocation.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Institution Review Board Central Committee at Fuwai Hospital, National Center for Cardiovascular Diseases of China. The patients/participants provided their written informed consent to participate in this study.
YYa and HX conceived the study. QZ and HX developed the study methodology. QZ edited the initial draft of the manuscript. XZ, QD, RF, HS, XY, XG, JY, and YW were involved in the study implement, data collection, and data audit. YYa, HX, and YYe critically revised the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
This work was supported by the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences [Grant no. CIFMS2016-I2M-1-009] and National Twelfth Five-year Science and Technology Support Projects by Ministry of Science and Technology of China [Grant no. 2011BAI11B02].
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank Stephen D. Wiviott and Marc S. Sabatine at The TIMI Study Group and Eric Peterson and Ying Xian at DCRI for their tremendous contribution on the design and implementation of the CAMI Registry. We also appreciate all the investigators of CAMI Registry for their contributions to this collaboration.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.800222/full#supplementary-material
NSTEMI, Non-ST-elevation myocardial infarction; STEMI, ST-elevation myocardial infarction; AMI, acute myocardial infarction; CCU, cardiac-coronary care unit; IABP, intra-aortic balloon pump; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting.
1. Yeh RW, Sidney S, Chandra M, Sorel M, Selby J V, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. (2010) 362:2155–65. doi: 10.1056/NEJMoa0908610
2. Khera S, Kolte D, Aronow WS, Palaniswamy C, Subramanian KS, Hashim T, et al. Non-ST-elevation myocardial infarction in the United States: Contemporary trends in incidence, utilization of the early invasive strategy, and in-hospital outcomes. J Am Heart Assoc. (2014) 3:1–19. doi: 10.1161/JAHA.114.000995
3. Freisinger E, Fuerstenberg T, Malyar NM, Wellmann J, Keil U, Breithardt G, et al. German nationwide data on current trends and management of acute myocardial infarction: discrepancies between trials and real-life. Eur Heart J. (2014) 35:979–88. doi: 10.1093/eurheartj/ehu043
4. Murugiah K, Wang Y, Nuti SV, Li X, Li J, Zheng X, et al. Are non-ST-segment elevation myocardial infarctions missing in China? Eur Hear J Qual Care Clin Outcomes. (2017) 3:319–27. doi: 10.1093/ehjqcco/qcx025
5. Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent st-segment elevation. Eur Heart J. (2016) 37:267–315. doi: 10.1093/eurheartj/ehv320
6. Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, Holmes DR, et al. 2014 AHA/ACC Guideline for the management of patients with non–ST-elevation acute coronary syndromes. J Am Coll Cardiol. (2014) 64:e139–228. doi: 10.1016/j.jacc.2014.09.017
7. Dondo TB, Hall M, Timmis AD, Yan AT, Batin PD, Oliver G, et al. Geographic variation in the treatment of non-ST-segment myocardial infarction in the English National Health Service: a cohort study. BMJ Open. (2016) 6:e011600. doi: 10.1136/bmjopen-2016-011600
8. Chung SC, Sundström J, Gale CP, James S, Deanfield J, Wallentin L, et al. Comparison of hospital variation in acute myocardial infarction care and outcome between Sweden and United Kingdom: population based cohort study using nationwide clinical registries. BMJ. (2015) 351:h3913. doi: 10.1136/bmj.h3913
9. Xu H, Yang Y, Wang C, Yang J, Li W, Zhang X, et al. Association of hospital-level differences in care with outcomes among patients with acute ST-segment elevation myocardial infarction in China. JAMA Netw Open. (2020) 3:e2021677. doi: 10.1001/jamanetworkopen.2020.21677
10. Xu H, Li W, Yang J, Wiviott SD, Sabatine MS, Peterson ED, et al. The China Acute Myocardial Infarction (CAMI) registry: a national long-term registry-research-education integrated platform for exploring acute myocardial infarction in China. Am Heart J. (2016) 175:193–201. doi: 10.1016/j.ahj.2015.04.014
11. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, Vasileva EY. Task force for the universal definition of myocardial infarction. third universal definition of myocardial infarction. Nat Rev Cardiol. (2012) 9:620–33. doi: 10.1038/nrcardio.2012.122
12. McNamara RL, Kennedy KF, Cohen DJ, Diercks DB, Moscucci M, Ramee S, et al. Predicting in-hospital mortality in patients with acute myocardial infarction. J Am Coll Cardiol. (2016) 68:626–35. doi: 10.1016/j.jacc.2016.05.049
13. Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. (2003) 163:2345–53. doi: 10.1001/archinte.163.19.2345
14. Antman EM, Cohen M, Bernink PJLM, McCabe CH, Horacek T, Papuchis G, et al. The TIMI risk score for unstable angina/non–ST elevation MI. JAMA. (2000) 284:835. doi: 10.1001/jama.284.7.835
15. Martin AD, Quinn KM, Park JH. MCMCpack: Markov chain monte carlo in R. J Stat Softw. (2011) 42:1–21. doi: 10.18637/jss.v042.i09
16. Gyenes GT, Yan AT, Tan M, Welsh RC, Fox KAA, Grondin FR, et al. Use and timing of coronary angiography and associated in-hospital outcomes in Canadian non-st-segment elevation myocardial infarction patients: insights from the Canadian global registry of acute coronary events. Can J Cardiol. (2013) 29:1429–35. doi: 10.1016/j.cjca.2013.04.035
17. Mårtensson S, Gyrd-Hansen D, Prescott E, Andersen PK, Zwisler ADO, Osler M. Trends in time to invasive examination and treatment from 2001 to 2009 in patients admitted first time with non-ST elevation myocardial infarction or unstable angina in Denmark. BMJ Open. (2014) 4:e004052. doi: 10.1136/bmjopen-2013-004052
18. Kang HJ, Simon D, Wang TY, Alexander KP, Jeong MH, Kim HS, et al. The contemporary use of angiography and revascularization among patients with non-ST-segment elevation myocardial infarction in the United States compared with South Korea. Clin Cardiol. (2015) 38:708–14. doi: 10.1002/clc.22475
19. Zia MI, Goodman SG, Peterson ED, Mulgund J, Chen AY, Langer A, et al. Paradoxical use of invasive cardiac procedures for patients with non-ST segment elevation myocardial infarction: An international perspective from the CRUSADE initiative and the Canadian ACS Registries I and II. Can J Cardiol. (2007) 23:1073–9. doi: 10.1016/S0828-282X(07)70876-0
20. Yang Q, Wang Y, Liu J, Liu J, Hao Y, Smith SC, et al. Invasive management strategies and antithrombotic treatments in patients with non-ST-segment-elevation acute coronary syndrome in China: findings from the improving CCC project (Care for Cardiovascular Disease in China). Circ Cardiovasc Interv. (2017) 10:1–9. doi: 10.1161/CIRCINTERVENTIONS.116.004750
21. Saar A, Marandi T, Ainla T, Fischer K, Blöndal M, Eha J. The risk-treatment paradox in non-ST-elevation myocardial infarction patients according to their estimated GRACE risk. Int J Cardiol. (2018) 272:26–32. doi: 10.1016/j.ijcard.2018.08.015
22. Rashid M, Curzen N, Kinnaird T, Lawson CA, Myint PK, Kontopantelis E, et al. Baseline risk, timing of invasive strategy and guideline compliance in NSTEMI: nationwide analysis from MINAP. Int J Cardiol. (2020) 301:7–13. doi: 10.1016/j.ijcard.2019.11.146
23. Baron T, Hambraeus K, Sundström J, Erlinge D, Jernberg T, Lindahl B. Type 2 myocardial infarction in clinical practice. Heart. (2015) 101:101–6. doi: 10.1136/heartjnl-2014-306093
24. Gao Y, Masoudi FA, Hu S, Li J, Zhang H, Li X, et al. Trends in early aspirin use among patients with acute myocardial infarction in China, 2001-2011: the China PEACE-Retrospective AMI study. J Am Heart Assoc. (2014) 3:1–10. doi: 10.1161/JAHA.114.001250
25. Zhang L, Desai NR, Li J, Hu S, Wang Q, Li X, Masoudi FA, et al. National quality assessment of early clopidogrel therapy in Chinese patients with acute myocardial infarction (AMI) in 2006 and 2011: insights from the China patient-centered evaluative assessment of cardiac events (PEACE)-retrospective AMI study. J Am Heart Assoc. (2015) 4:1–10. doi: 10.1161/JAHA.115.001906
26. Colivicchi F, Di Fusco SA, Gulizia MM, de Luca L, Geraci G, Nardi F, et al. Risk stratification and secondary prevention post-myocardial infarction: Insights from the EYESHOT Post-MI study. J Cardiovasc Med. (2021) 22:278–85. doi: 10.2459/JCM.0000000000001132
27. Schoenenberger AW, Radovanovic D, Windecker S, Iglesias JF, Pedrazzini G, Stuck AE, et al. Temporal trends in the treatment and outcomes of elderly patients with acute coronary syndrome. Eur Heart J. (2016) 37:1304–11. doi: 10.1093/eurheartj/ehv698
28. Topol EJ, Kereiakes DJ. Regionalization of care for acute ischemic heart disease: a call for specialized centers. Circulation. (2003) 107:1463–6. doi: 10.1161/01.CIR.0000063680.45780.A0
29. Concannon TW, Kent DM, Normand SL, Newhouse JP, Griffith JL, Cohen J, et al. Comparative effectiveness of ST-segment-elevation myocardial infarction regionalization strategies. Circ Cardiovasc Qual Outcomes. (2010) 3:506–13. doi: 10.1161/CIRCOUTCOMES.109.908541
Keywords: non-ST elevated acute myocardial infarction, in-hospital care, invasive strategies, medications, healthcare quality, outcome
Citation: Zhao Q, Xu H, Zhang X, Ye Y, Dong Q, Fu R, Sun H, Yan X, Gao X, Yang J, Wang Y and Yang Y (2022) Current Status and Hospital-Level Differences in Care and Outcomes of Patients With Acute Non-ST-Segment Elevation Myocardial Infarction in China: Insights From China Acute Myocardial Infarction Registry. Front. Cardiovasc. Med. 8:800222. doi: 10.3389/fcvm.2021.800222
Received: 22 October 2021; Accepted: 17 December 2021;
Published: 17 January 2022.
Edited by:
Pietro Scicchitano, University of Bari Medical School, ItalyReviewed by:
Irene R. Degano, Centro de Investigación Biomédica en Red en Enfermedades Cardiovasculares (CIBERCV), SpainCopyright © 2022 Zhao, Xu, Zhang, Ye, Dong, Fu, Sun, Yan, Gao, Yang, Wang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haiyan Xu, eHVoYWl5YW5AZnV3YWlob3NwaXRhbC5vcmc=; Yuejin Yang, eWFuZ3lqZndAMTI2LmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.