
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 04 November 2021
Sec. Heart Valve Disease
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.766430
This article is part of the Research Topic Bicuspid Aortic Valve: From pathophysiological mechanisms, imaging diagnosis to clinical treatment methods View all 14 articles
Background: The population is aging and advances in multimodal imaging and transcatheter valve intervention have been prominent in the past two decades. This study investigated temporal trends in demographic characteristics, use of multimodal imaging, treatments, and outcomes in patients with bicuspid aortic valve (BAV).
Methods and Results: A total of 1,497 patients (male 71.7%, 57 ± 14 years old) first diagnosed with BAV between January 2003 and December 2020, in a single tertiary center were divided into three groups according to year of diagnosis: group 1 (2003–2008, n = 269), group 2 (2009–2014, n = 594), and group 3 (2015–2020, n = 634). The patients' demographic characteristics, comorbidities, BAV morphology, BAV function, BAV-related disease, use of multimodal diagnostic imaging, treatment modality for BAV, and clinical outcomes were compared among the three groups. The ages at diagnosis and at the time of surgery/intervention increased considerably from group 1 to 3. The patients' comorbidity index also increased progressively. The proportion of non-dysfunctional BAV and significant AS increased, while that of significant AR decreased. The frequency of infective endocarditis as an initial presentation significantly decreased over time. Additionally, the use of multimodal imaging increased markedly in the most recent group. The results also indicated increasing trends in the use of bioprosthetic valves and transcatheter aortic valve replacement. Overall and cardiovascular survival rates improved from group 1 to 3 (log rank p < 0.001).
Conclusions: For the past two decades, remarkable temporal changes have occurred in patient characteristics, use of multimodal diagnostic imaging, choice of treatment modality, and clinical outcomes in patients with BAV.
Bicuspid aortic valve (BAV) is the most common congenital heart valve disease, and the burden of BAV disease is greater than for other congenital anomalies (1–3). BAV can present in diverse spectrum and affect valve function from non-dysfunctional to severe aortic stenosis (AS) or severe aortic regurgitation (AR) (4–6). In addition, BAV often is accompanied by aortopathy, other congenital defects, cardiomyopathies, or infective endocarditis (IE) (7–9). In the past two decades, echocardiographic surveillance of asymptomatic subjects has increased, and multimodality imaging has been developed and applied in heart valve diseases (10, 11). Recently, transcatheter aortic valve replacement (AVR) has been expanded to young age and low risk groups, and treatment methods in BAV patients have diversified (12–14). In addition, the incidence of IE as a first manifestation in BAV patients is expected to decrease as socioeconomic status improves (15). Therefore, this study aimed to investigate temporal trends in demographic characteristics, use of multimodal imaging, treatment modality, and clinical outcomes in patients with BAV from a large Korean registry.
We systemically analyzed a single-center Korean registry that consisted of 1,497 consecutively enrolled BAV patients 19 years of age or older. This retrospective and prospective registry contains echocardiographic data and clinical information from medical records of the patients from January 2003 to December 2020, in Severance Cardiovascular Hospital, Seoul, Korea. All patients were diagnosed with BAV through transthoracic echocardiography, and additional diagnostic imaging was performed according to the clinical judgement of the physician. When there was discrepancy between imaging tests, we determined exclusion after comprehensive consideration of all imaging studies and intraoperative findings. There were 14 exclusions in this study. The Institutional Review Board of Severance Hospital approved this study, which was conducted in compliance with the Declaration of Helsinki. The need for informed consent was waived.
Baseline characteristics at the time of diagnosis were age, sex, height, weight, body mass index, and comorbidities. The Charlson comorbidity index was calculated to determine patient risk (16). All participants in the study population underwent comprehensive transthoracic echocardiography. All echocardiographic studies were performed using commercially available equipment and were analyzed retrospectively without knowledge of the clinical data. Standard 2-dimensional and Doppler measurements were performed, and the severity of BAV dysfunction was assessed based on the American Society of Echocardiography guidelines (17, 18).
Congenital BAV was diagnosed when only two cusps were identified unequivocally in systole and diastole in the short-axis view, with a clear “fish-mouth” appearance during systole, as previously described (5–8). Type 1 was confirmed based on congenital fusion of the right and left coronary cusps; Type 2 was confirmed based on a congenital fusion of the right and non-coronary cusps; Type 3 was confirmed based on a congenital fusion of the non-coronary and left coronary cusps; Type 0 was confirmed for cases without raphe, which also is referred to as “true type” BAV. The severity of AS and AR was assessed using an integrated approach (17, 18). Patients that had at least moderate AS or moderate AR were classified as significant AS or significant AR, respectively, and others were classified with non-dysfunctional BAV (5, 6).
All measurements of the aorta were performed on the QRS complex of the electrocardiogram according to recommendations (19). The dimensions of the Valsalva sinuses were measured perpendicularly to the right and left (or non-) aortic sinuses. The sinotubular junction was measured where the aortic sinuses met the tubular aorta. The AA was measured 2 cm distal to the sinotubular junction. The presence of aortopathy was defined as an ascending aorta diameter ≥37 mm (6, 7, 20). A maximum dimension of the ascending aorta ≥45 mm was defined as severe aortopathy (6). Concomitant congenital defects including ventricular septal defect, atrial septal defect, patent foramen ovale, and patent ductus arteriosus were investigated. Concomitant cardiomyopathy was defined as specific cardiomyopathies such as hypertrophic cardiomyopathy, noncompaction cardiomyopathy, and idiopathic dilated cardiomyopathy (8). A diagnosis of IE was determined according to modified Duke criteria (21).
We investigated whether transesophageal echocardiography (TEE) and MDCT were performed in addition to transthoracic echocardiography. Diagnostic multimodal imaging was performed based on the clinician's judgement. Surgery or intervention was conducted according to the guidelines at time of diagnosis, based on patient symptoms, cardiac function, and BAV function and clinician decision. Eligibility for transcatheter AVR was determined by a multidisciplinary heart team.
The study population was divided into three groups according to year of diagnosis with six-year increments: group 1 (2003–2008, n = 269), group 2 (2009–2014, n = 594), and group 3 (2015–2020, n = 634). The baseline characteristics, ages at diagnosis and at the time of surgery or intervention, use of multimodality imaging, number of surgeries or interventions, and survival from all-cause death and cardiovascular death were compared among the groups.
The index date was the time of the first BAV diagnosis. Death information was collected by medical records. Cardiovascular death was defined as death due to worsening heart failure, acute coronary syndrome, cerebrovascular accidents, or sudden cardiac death. The cause of death was determined based on the death certificate.
Categorical variables are expressed as percentage or frequency and compared using the χ2 test or Fisher's exact test. Continuous variables are expressed as mean ± standard deviation. The Cochran–Armitage and Jonckheere–Terpstra methods were used to test trends in nominal and categorical variables across time periods. Survival from all-cause death and cardiovascular death was estimated using the Kaplan–Meier method and compared by Log-rank test. A probability value (P-value) <0.05 was considered statistically significant. Statistical analyses were conducted using R version 4.1.0 (The R Foundation for Statistical Computing; www.R-project.org).
During the study period, a total of 1,497 patients (male 71.7%, 56.5 ± 14.3 years old) was diagnosed with BAV. The absolute numbers of patients diagnosed with BAV in groups 1, 2, and 3 were 269, 594, and 634, respectively. Baseline characteristics of the study population are shown in Table 1.
Patient demographics indicated that age at diagnosis increased significantly from group 1 to group 3 (P for trend < 0.001), and sex distribution was not significantly different between groups according to diagnosis year, with males accounting for more than 70% of all groups. From group 1 to 3, a tendency for an increase in body mass index was observed (P for trend = 0.036). Analysis of patient comorbidities indicated that the more recent patients experienced more frequent hypertension and dyslipidemia, and the Charlson comorbidity index increased in this group (P for trend = 0.029). Analysis of BAV morphology indicated that type 1 was dominant in all groups, and there was no difference according to group. In terms of BAV function, the diagnosis of non-dysfunctional BAV increased in groups 2 and 3 compared to group 1 (P for trend=0.039), the proportion of significant AR decreased (P for trend = 0.002), and the significant AS increased steadily (P for trend = 0.039; Figure 1A). In terms of BAV-associated disease, about half of the patients had aortopathy, and about one-quarter had severe aortopathy, with no significant trends observed over time (Figure 1B). From group 1 to 3, the prevalence of infective endocarditis significantly decreased (P for trend = 0.010; Figure 1B). Detection of congenital defects increased (P for trend = 0.002) and likely was attributable to the increased use in additional diagnostic imaging from groups 1 to 3. In group 3, TEE and MDCT were used in 38.6 and 33.9% of patients, respectively (Figure 2).
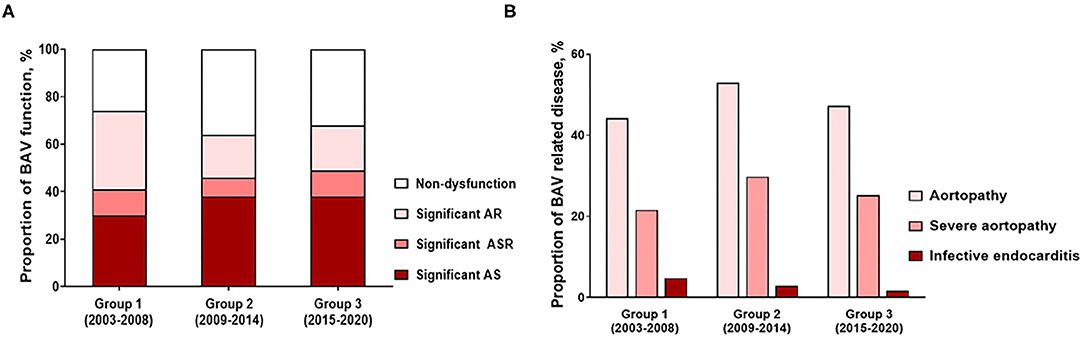
Figure 1. Temporal trends of (A) proportion of BAV function and (B) proportion of BAV-related disease.
Table 2 shows treatment characteristics for the three groups of the study population. There was an increasing trend in age at surgery or intervention between groups (P for trend < 0.001; Figure 3A). The mean age at surgery or intervention in group 1 was 55 years, while that in group 3 was 62 years. The proportion of patients older than 70 years at surgery or intervention remarkably increased (P for trend = 0.003) and reached about 25% in groups 2 and 3. In terms of indications for surgery or intervention, surgery due to severe AR or infective endocarditis decreased over time (P for trend = 0.024, 0.027, respectively).
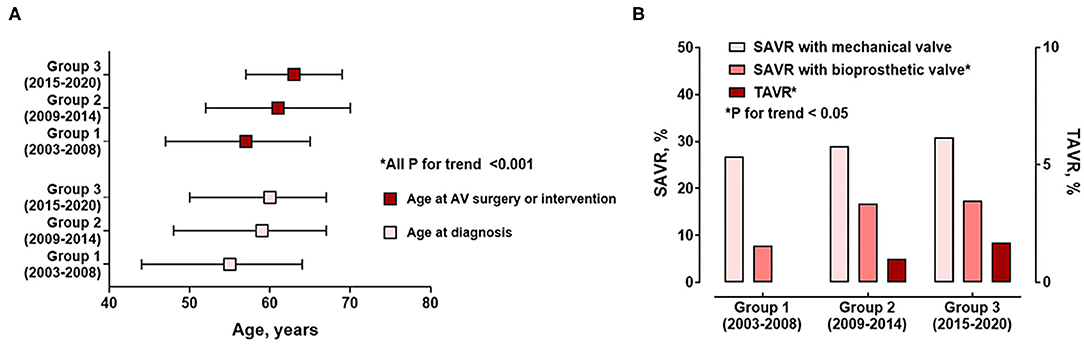
Figure 3. Temporal trends of (A) ages at diagnosis and AV surgery or interventions and (B) treatment methods.
As age at surgery increased from group 1 to 3, surgical AVR using bioprosthetic valves significantly increased (P for trend = 0.002). In addition, transcatheter AVR gradually increased over time (P for trend = 0.024; Figure 3B). The results indicate that there were more frequent concomitant surgeries such as coronary artery bypass for patients diagnosed and treated more recently (P for trend = 0.002). During the 3.8 years (interquartile range 1.0–6.9 years) of follow-up, all-cause death and cardiovascular death significantly decreased from group 1 to group 3 (both log-rank P < 0.001; Figure 4).
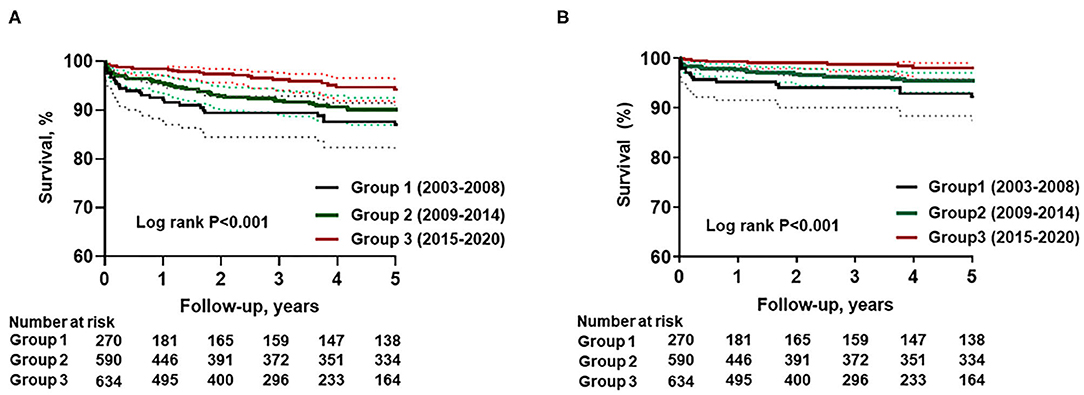
Figure 4. Temporal trends in clinical outcomes: (A) survival from all-cause death, (B) survival from cardiovascular death.
The principal findings of this study were as follow: (1) a significant temporal increase was observed in both age at the time of diagnosis and age at the time of surgery or intervention; (2) over time, the proportions of non-dysfunctional BAV and significant AS increased and significant AR decreased in patients with BAV; (3) a temporal change in the incidence of infective endocarditis was observed in patients with BAV; (4) surgical AVR using bioprosthetic valve and transcatheter AVR increased; (5) the frequency of additional diagnostic imaging, such as TEE or MDCT, remarkably increased in patients with BAV; and (6) there was a recent significant improvement in all-cause and cardiovascular death among all patients diagnosed with BAV. Understanding these temporal changes and trends in patient characteristics, BAV function, diagnosis, treatment, and outcome will be important for further diagnostic and treatment advances.
BAV is the most common adult congenital heart defect and has associated increased risk for severe AS or AR, thoracic aortic disease or acquired complications such as IE (1–4, 22, 23). Because BAV is congenital, BAV-related diseases typically manifest at an early age. Therefore, the majority of previous studies has reported a mean age of about 40 years (24). Significant bicuspid AS usually occurs earlier than tricuspid AS and is reported in their 50s and 60s (25). In patient with BAV, AR is more common at a young age, whereas AS usually presents later in life (26). In this study, the mean age at diagnosis was 56.5 years, and the mean age increased over about two decades. Furthermore, the mean age at surgery or intervention was 61.6 years, and 24.5% of patients in the more recent group were older than 70 years. In addition, as the global burden of calcified aortic valve disease increased, the proportion of significant AR decreased while that of significant AS increased from group 1 to 3, likely related to the increase in age for the general population (27). As ages of patients at diagnosis and at surgery or intervention increased, the treatment strategy for BAV dysfunction also changed. In this study, 35.6% of patients in group 3 underwent AVR with bioprosthetic valves. Increased use of bioprosthetic valves was an expected finding because of the increasing aging trend in patient with BAV. In addition, as the comorbidities of patients increased, the surgical risk also increased, as did the demand for transcatheter AVR. This study showed increasing trend of transcatheter AVR in BAV patients after its launch in 2011, in Korea.
The diagnosis of non-dysfunctional BAV had increased in this study. In Korea, the number of TTE as screening tool is continuously increasing (28). The increased number of exam might enable early diagnosis of BAV and related disease in general population.
The present study also showed a decreasing trend for prevalence of IE as the first manifestation of BAV disease. The rate of IE was 1.7% in group 3, and the incidence of IE in BAV has been reported around 2%, which was comparable to our results (9, 24). A recent report from the United States showed decreasing trend of native valve endocarditis but that of increased prosthetic valve and device-related endocarditis (15). These trends might be derived from increased echocardiographic surveillance for BAV and improved socioeconomic status over time.
Multimodality imaging has become increasingly important because BAV is not only a valve disease, but also is associated with other diseases such as aortopathy and cardiomyopathies (6–8, 10). The first diagnostic tool of choice to evaluate heart valves was transthoracic echocardiography because it is easy to use and noninvasive. Recently, MDCT has been used as a complement to echocardiography for diagnosing heart valve disease and preoperative evaluation (18, 29, 30). In patients with BAV, MDCT can provide accurate information about the BAV and adjacent structural abnormalities including the aorta, concomitant anomalies, or combined coronary artery disease (10, 11). Furthermore, in the era of transcatheter AVR, the use of multimodal imaging is becoming an increasingly essential part of routine clinical practice, particularly for BAV patients with significant AS (10, 31). The patients with BAV had chance of concomitant cardiomyopathies. They had different flow dynamics from the patients with tricuspid aortic valve (32). Furthermore, myocardial fibrosis has been reported as important prognostic factor in BAV related disease such as AS or AR (33, 34). Cardiac magnetic resonance might be useful in patients with BAV and related disease (8, 35). The results of this study indicate that the use of multimodal imaging has increased, and that this approach can detect concomitant disease such as congenital defects based on the overall trends in diagnostic imaging in patients with BAV.
This study also showed clinical outcome improvements in the more recent group despite an increase in mean age with a higher comorbidity index. There are several factors that could impact these results. Notably, as the proportion of non-dysfunctional BAV increased in group 3, it is possible that fewer clinical events were diagnosed because those events likely were attributable to previously undetected non-dysfunctional BAV in patients. In addition, recent advances in diagnostic imaging, surgical techniques (36), medical systems such as a multidisciplinary approach, and application of transcatheter AVR in patients with high surgical risk might influence the improved clinical outcomes in patients with BAVs.
Our study had several limitations. First, this study was conducted at a single tertiary center by comprehensively reviewing retrospective and prospective data; therefore, selection and referral bias were inevitable, and our results could not be generalized. The proportions of significant BAV dysfunction and severe aortopathy were higher than reported in previous studies (24, 26). The clinical follow-up duration for the study population was relatively short. Seconds, the study subjects were diagnosed based on TTE, so there might be inevitable limitations and bias for the morphologic evaluation of BAV, particularly severely calcified aortic valve. However, as this study had additional imaging studies performed by clinician's judgement and consisted of a large-scale population, we believe this potential bias would not change our main findings. Additionally, it is difficult to generalize and apply these temporal trends to other societies or countries because if differing social and medical environmental factors. Despite these limitations, we believe that the data from this large Korean registry will be helpful to understand the characteristics, diagnosis, treatment, and outcomes for BAV patients over the past two decades. Further, some of the temporal trends might be applicable to other societies.
In past two decades, there have been remarkable temporal changes in patients with BAV. Patient characteristics, proportion of BAV dysfunction, diagnosis, and treatment strategy have changed, and the demand for bioprosthetic valves has increased. Temporal trends were observed with improvements of clinical outcomes in patients with BAV.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Severance Hospital, Yonsei University College of Medicine. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
KK and CS contributed to the conception, design of the work, and drafted the manuscript. D-YK, JS, and IC assisted in data collection and analysis. G-RH and J-WH contributed to the review and revision of the manuscript. All authors contributed to the article and approved the submitted version.
This research was supported from the Korean Cardiac Research Foundation (202103-02).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AR, aortic regurgitation; AS, aortic stenosis; AVR, aortic valve replacement; BAV, bicuspid aortic valve; IE, infective endocarditis; MDCT, multidetector computed tomography; TEE, transesophageal echocardiography.
1. Ward C. Clinical significance of the bicuspid aortic valve. Heart. (2000) 83:81–5. doi: 10.1136/heart.83.1.81
2. Sillesen AS, Vogg O, Pihl C, Raja AA, Sundberg K, Vedel C, et al. Prevalence of bicuspid aortic valve and associated aortopathy in newborns in Copenhagen, Denmark. JAMA. (2021) 325:561–7. doi: 10.1001/jama.2020.27205
3. Siu SC, Silversides CK. Bicuspid aortic valve disease. J Am Coll Cardiol. (2010) 55:2789–800. doi: 10.1016/j.jacc.2009.12.068
4. Braverman AC, Guven H, Beardslee MA, Makan M, Kates AM, Moon MR. The bicuspid aortic valve. Curr Probl Cardiol. (2005) 30:470–522. doi: 10.1016/j.cpcardiol.2005.06.002
5. Lee SY, Shim CY, Kim D, Cho I, Hong GR, Ha JW, et al. Factors determining aortic valve dysfunction in Korean subjects with a bicuspid aortic valve. Am J Cardiol. (2017) 119:2049–55. doi: 10.1016/j.amjcard.2017.03.038
6. Song S, Seo J, Cho I, Hong GR, Ha JW, Shim CY. Progression and outcomes of non-dysfunctional bicuspid aortic valve: longitudinal data from a large korean bicuspid aortic valve registry. Front Cardiovasc Med. (2020) 7:603323. doi: 10.3389/fcvm.2020.603323
7. Lee SY, Shim CY, Hong GR, Seo J, Cho I, Cho IJ, et al. Association of aortic phenotypes and mechanical function with left ventricular diastolic function in subjects with normally functioning bicuspid aortic valves and comparison to subjects with tricuspid aortic valves. Am J Cardiol. (2015) 116:1547–54. doi: 10.1016/j.amjcard.2015.08.017
8. Jeong H, Shim CY, Kim D, Choi JY, Choi KU, Lee SY, et al. Prevalence, characteristics, and clinical significance of concomitant cardiomyopathies in subjects with bicuspid aortic valves. Yonsei Med J. (2019) 60:816–23. doi: 10.3349/ymj.2019.60.9.816
9. Zegri-Reiriz I, de Alarcon A, Munoz P, Martinez Selles M, Gonzalez-Ramallo V, Miro JM, et al. Infective endocarditis in patients with bicuspid aortic valve or mitral valve prolapse. J Am Coll Cardiol. (2018) 71:2731–40. doi: 10.1016/j.jacc.2018.03.534
10. Galian-Gay L, Rodriguez-Palomares J, Guala A, Michelena HI, Evangelista A. Multimodality imaging in bicuspid aortic valve. Prog Cardiovasc Dis. (2020) 63:442–51. doi: 10.1016/j.pcad.2020.06.003
11. Kim D, Shim CY, Kim YJ, Nam K, Hong GR, Lee SH, et al. Differences in flow-gradient patterns between severe bicuspid aortic stenosis and severe tricuspid aortic stenosis- mechanistic insight from multimodal imaging. Circ J. (2019) 84:119–26. doi: 10.1253/circj.CJ-19-0702
12. Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O'Hair D, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. (2019) 380:1706–15. doi: 10.1056/NEJMoa1816885
13. Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. (2019) 380:1695–705. doi: 10.1056/NEJMoa1814052
14. Tarantini G, Fabris T. Transcatheter aortic valve replacement for bicuspid aortic valve stenosis: a practical operative overview. Circ Cardiovasc Interv. (2021) 14:e009827. doi: 10.1161/CIRCINTERVENTIONS.120.009827
15. Toyoda N, Chikwe J, Itagaki S, Gelijns AC, Adams DH, Egorova NN. Trends in infective endocarditis in California and New York State, 1998-2013. JAMA. (2017) 317:1652–60. doi: 10.1001/jama.2017.4287
16. Brusselaers N, Lagergren J. The Charlson Comorbidity Index in registry-based research. Methods Inf Med. (2017) 56:401–6. doi: 10.3414/ME17-01-0051
17. Zoghbi WA, Adams D, Bonow RO, Enriquez-Sarano M, Foster E, Grayburn PA, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the american society of echocardiography developed in collaboration with the society for cardiovascular magnetic resonance. J Am Soc Echocardiogr. (2017) 30:303–71. doi: 10.1016/j.echo.2017.01.007
18. Baumgartner H, Hung J, Bermejo J, Chambers JB, Edvardsen T, Goldstein S, et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the european association of cardiovascular imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. (2017) 30:372–92. doi: 10.1016/j.echo.2017.02.009
19. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. (2015) 28:1–39.e14. doi: 10.1016/j.echo.2014.10.003
20. Della Corte A, Bancone C, Quarto C, Dialetto G, Covino FE, Scardone M, et al. Predictors of ascending aortic dilatation with bicuspid aortic valve: a wide spectrum of disease expression. Eur J Cardiothorac Surg. (2007) 31:397–404; discussion 404–5. doi: 10.1016/j.ejcts.2006.12.006
21. Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. (2000) 30:633–8. doi: 10.1086/313753
22. Verma S, Siu SC. Aortic dilatation in patients with bicuspid aortic valve. N Engl J Med. (2014) 370:1920–9. doi: 10.1056/NEJMra1207059
23. Kiyota Y, Della Corte A, Montiero Vieira V, Habchi K, Huang CC, Della Ratta EE, et al. Risk and outcomes of aortic valve endocarditis among patients with bicuspid and tricuspid aortic valves. Open Heart. (2017) 4:e000545. doi: 10.1136/openhrt-2016-000545
24. Masri A, Svensson LG, Griffin BP, Desai MY. Contemporary natural history of bicuspid aortic valve disease: a systematic review. Heart. (2017) 103:1323–30. doi: 10.1136/heartjnl-2016-309916
25. Roberts WC, Ko JM. Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation. (2005) 111:920–5. doi: 10.1161/01.CIR.0000155623.48408.C5
26. Tzemos N, Therrien J, Yip J, Thanassoulis G, Tremblay S, Jamorski MT, et al. Outcomes in adults with bicuspid aortic valves. JAMA. (2008) 300:1317–25. doi: 10.1001/jama.300.11.1317
27. Coffey S, Roberts-Thomson R, Brown A, Carapetis J, Chen M, Enriquez-Sarano M, et al. Global epidemiology of valvular heart disease. Nat Rev Cardiol. (2021). doi: 10.1038/s41569-021-00570-z
28. Chung SH, Lee HJ, Kim HS, Oh J-Y. Health insurance benefit criteria and quality assurance policies of diagnostic ultrasound services in other countries. Health Policy Manag. (2014) 24:109–19. doi: 10.4332/KJHPA.2014.24.2.109
29. Choi JY, Suh YJ, Seo J, Choi KU, Hong GR, Lee S, et al. Structural and functional characteristics of mitral paravalvular leakage identified by multimodal imaging and their implication on clinical presentation. J Clin Med. (2021) 10:222. doi: 10.3390/jcm10020222
30. Kim IC, Chang S, Hong GR, Lee SH, Lee S, Ha JW, et al. Comparison of cardiac computed tomography with transesophageal echocardiography for identifying vegetation and intracardiac complications in patients with infective endocarditis in the era of 3-dimensional images. Circ Cardiovasc Imaging. (2018) 11:e006986. doi: 10.1161/CIRCIMAGING.117.006986
31. Jilaihawi H, Chen M, Webb J, Himbert D, Ruiz CE, Rodes-Cabau J, et al. A bicuspid aortic valve imaging classification for the TAVR era. JACC Cardiovasc Imaging. (2016) 9:1145–58. doi: 10.1016/j.jcmg.2015.12.022
32. Hope MD, Meadows AK, Hope TA, Ordovas KG, Reddy GP, Alley MT, et al. Images in cardiovascular medicine. Evaluation of bicuspid aortic valve and aortic coarctation with 4D flow magnetic resonance imaging. Circulation. (2008) 117:2818–9. doi: 10.1161/CIRCULATIONAHA.107.760124
33. Bing R, Cavalcante JL, Everett RJ, Clavel MA, Newby DE, Dweck MR. Imaging and impact of myocardial fibrosis in aortic stenosis. JACC Cardiovasc Imaging. (2019) 12:283–96. doi: 10.1016/j.jcmg.2018.11.026
34. Malahfji M, Senapati A, Tayal B, Nguyen DT, Graviss EA, Nagueh SF, et al. Myocardial scar and mortality in chronic aortic regurgitation. J Am Heart Assoc. (2020) 9:e018731. doi: 10.1161/JAHA.120.018731
35. Bohbot Y, Renard C, Manrique A, Levy F, Marechaux S, Gerber BL, et al. Usefulness of cardiac magnetic resonance imaging in aortic stenosis. Circ Cardiovasc Imaging. (2020) 13:e010356. doi: 10.1161/CIRCIMAGING.119.010356
Keywords: bicuspid aortic valve, trend, diagnosis, imaging, treatment, outcome
Citation: Kim K, Kim D-Y, Seo J, Cho I, Hong G-R, Ha J-W and Shim CY (2021) Temporal Trends in Diagnosis, Treatments, and Outcomes in Patients With Bicuspid Aortic Valve. Front. Cardiovasc. Med. 8:766430. doi: 10.3389/fcvm.2021.766430
Received: 29 August 2021; Accepted: 13 October 2021;
Published: 04 November 2021.
Edited by:
Mao Chen, Sichuan University, ChinaReviewed by:
Dhrubajyoti Bandyopadhyay, New York Medical College, United StatesCopyright © 2021 Kim, Kim, Seo, Cho, Hong, Ha and Shim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chi Young Shim, Y3lzcHJzQHl1aHMuYWM=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.